Abstract
Background
In 1997, the National Hockey League (NHL) and NHL Players’ Association (NHLPA) launched a concussion program to improve the understanding of this injury. We explored initial postconcussion signs, symptoms, physical examination findings and time loss (i.e., time between the injury and medical clearance by the physician to return to competitive play), experienced by male professional ice-hockey players, and assessed the utility of initial postconcussion clinical manifestations in predicting time loss among hockey players.
Methods
We conducted a prospective case series of concussions over seven NHL regular seasons (1997–2004) using an inclusive cohort of players. The primary outcome was concussion and the secondary outcome was time loss. NHL team physicians documented post-concussion clinical manifestations and recorded the date when a player was medically cleared to return to play.
Results
Team physicians reported 559 concussions during regular season games. The estimated incidence was 1.8 concussions per 1000 player-hours. The most common postconcussion symptom was headache (71%). On average, time loss (in days) increased 2.25 times (95% confidence interval [CI] 1.41–3.62) for every subsequent (i.e., recurrent) concussion sustained during the study period. Controlling for age and position, significant predictors of time loss were postconcussion headache (p < 0.001), low energy or fatigue (p = 0.01), amnesia (p = 0.02) and abnormal neurologic examination (p = 0.01). Using a previously suggested time loss cut-point of 10 days, headache (odds ratio [OR] 2.17, 95% CI 1.33–3.54) and low energy or fatigue (OR 1.72, 95% CI 1.04–2.85) were significant predictors of time loss of more than 10 days.
Interpretation
Postconcussion headache, low energy or fatigue, amnesia and abnormal neurologic examination were significant predictors of time loss among professional hockey players.
Concussion has been defined as a pathophysiologic process affecting the brain and induced by traumatic forces.1–3 Concussions are common in ice hockey.4–14 It has been estimated that 1.6 to 3.8 million sports- and recreation-related traumatic brain injuries occur in the United States each year.15 Although most signs and symptoms resolve over time when concussive injuries are recognized and managed appropriately, concussions can be career-ending.4,12,16
In 1997, the National Hockey League (NHL) and NHL Players Association (NHLPA) launched the NHL-NHLPA Concussion Program to examine concussion from a scientific perspective and to better understand its natural history and contribute new knowledge to the field.17 The objectives of our study were to determine rates of concussion and trends related to concussion in the NHL, to descriptively explore initial postconcussion signs, symptoms, physical examination findings and time loss (i.e., time between the injury and medical clearance by the physician to return to competitive play), and to assess the utility of initial postconcussion clinical manifestations as predictors of time loss among male professional ice-hockey players.
Methods
Study design, participants and setting
This study was a prospective case series involving concussions among an inclusive cohort of male professional ice-hockey players from all NHL teams competing during the hockey seasons of 1997–1998 to 2003–2004.
Approved by the NHL, the NHLPA and the Office of Medical Bioethics of the University of Calgary, this study used NHL team physicians who were mandated by the league to document all concussions sustained during regular season games from 1997–1998 to 2003–2004. Physicians used standardized injury report forms; the 2002–2003 Physician Evaluation Form is presented in Appendix 1 (available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
The team physicians were present at all regular season games and consistently documented initial postconcussion signs, symptoms and physical examination findings over the seven years of study. Physicians also recorded the date when a player was medically cleared to return to play, which provided a marker of concussion severity (via time loss from participation). This clearance date served as a best estimate of when a player had completely recovered from his concussion and was able to return to unrestricted competition. Additional details of the study methods are provided in Appendix 2 (available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
Outcome measures
The main outcome variable was concussion (for the definition of concussion as used in this study, see Box 1). The secondary outcome variable was time loss. Time loss was defined as the period of competitive playing time lost by a study participant as a result of concussion, and was measured in days from the date of injury to the date on which the team physician medically cleared a player to return to unrestricted competition. The NHL-NHLPA Concussion Program did not adopt a concussion grading scale or return-to-play guideline. Rather, team physicians managed concussions according to their own clinical judgment, as suggested in the literature on concussion.1–3,18,19
Box 1: Definition of concussion.
For the 1997–1998 to 2001–2002 NHL regular seasons, a reportable injury was defined as any traumatically induced alteration in brain function characterized or manifested by one or more of the following:
Alteration of awareness of consciousness (including but not limited to loss of consciousness), “ding,” having one’s “bell rung,” being dazed or stunned, having a sensation of “wooziness,” “fogginess,” seizures or any type of amnesia;
Any signs or symptoms consistent with brain injury or postconcussion syndrome, including but not limited to one or more of the following: headache, vertigo, light-headedness, loss of balance, unsteadiness, syncope, near-syncope, cognitive dysfunction, memory dysfunction, difficulty concentrating, sleep disturbance, hearing difficulty, ringing in the ears (tinnitus), blurred vision, double vision (diplopia), personality change, drowsiness, lethargy, fatigue and inability to perform daily activities;
Transient or persistent neurologic signs;
Symptoms or signs as outlined above after a suspected or diagnosed head injury or concussion that occurs during or after a return to activity.
For the 2002–2003 and 2003–2004 NHL regular seasons, the following definition by the Vienna Concussion in Sport Agreement Statement was used in the NHL-NHLPA Concussion Program:
“Concussion is defined as a complex pathophysiologic process affecting the brain, induced by traumatic biomechanical forces. Concussion results in a graded set of clinical syndromes that may or may not involve loss of consciousness or memory dysfunction. Concussion typically results in a functional disturbance with the rapid onset of short-lived impairment of neurologic function that resolves spontaneously.”1
The independent variables of interest were age, position, recurrent concussion during the study period, and initial postconcussion symptoms, signs and neurologic examination findings. Because there was variability across seasons in which symptoms were included on the physician evaluation forms, only those symptoms that remained consistent from season to season were included in the analyses (Appendix 3, available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
Statistical analysis
Descriptive univariable and bivariable summary statistics were provided for the independent and dependent variables. Concussion rates were calculated as the number of regular-season, game-related concussions per 100 players per season. The incidence density or average incidence rate of concussion was calculated as the number of instances of concussion (allowing for re-entry into the study of a participant who had fully recovered) divided by the sum of estimated individual athlete-exposure time. The athlete-exposure calculation is shown in Appendix 2 (available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
Univariable logistic regression was fitted to explore potential predictors (initial postconcussion signs, symptoms and abnormal neurologic examination findings) of time loss. A 10-day time loss cut-point was used as a marker to retrospectively distinguish concussion severity (≤ 10 v. > 10 days); this marker has been supported in the literature for adult male sport participants.3,20–23 Multivariable logistic regression was fitted, adjusting for age (in years) and position (i.e., centre, wing, defense or goalie). Sensitivity analysis was also performed by treating time loss (in days) as a continuous outcome. In such case, a linear regression model was fitted to identify potential significant predictors of time loss. A selected (type 1 error) level of 0.05 was used for all analyses.
Results
Primary outcome variable
There were 559 physician-diagnosed, regular-season, in-game concussions among NHL team players reported during the seven years of study. The mean number of concussions per year was 80, with an overall game rate of 5.8 concussions per 100 players per season (Table 1). The estimated incidence density was 1.8 concussions per 1000 game player-hours. A χ2 analysis showed a significant difference in concussion proportions across seasons (p = 0.001).
Table 1:
Frequency and rate of concussion in National Hockey League (NHL) regular season games per 100 players (1997–2004)
| NHL regular season | Frequency of concussion | Players, no. | Rate of concussion per 100 players |
|---|---|---|---|
| 1997–98 | 56 | 1218 | 4.6 |
| 1998–99 | 88 | 1249 | 7.0 |
| 1999–00 | 66 | 1347 | 4.9 |
| 2000–01 | 109 | 1419 | 7.7 |
| 2001–02 | 96 | 1470 | 6.5 |
| 2002–03 | 72 | 1457 | 4.9 |
| 2003–04 | 72 | 1459 | 4.9 |
| Overall | 559 | 9619 | 5.8 |
Secondary outcome variable
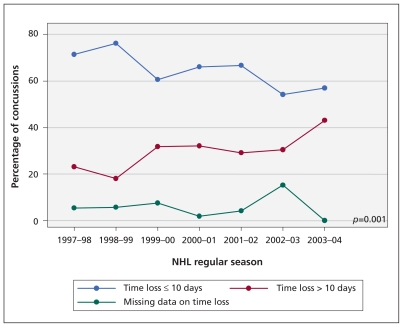
Individual postconcussion time loss ranged from 0 to 342 days, with a median time loss of six days per concussion (interquartile range [IQR] 2–13). Of the 529 instances of concussion for which information on time loss was recorded, 69% (363/529) missed up to 10 days of unrestricted competition, whereas 31% (166/529) missed more than 10 days because of their concussion. The percentage of instances of concussion that resulted in more than 10 days of time loss ranged from 19% to 43% per season (Figure 1).
Figure 1:
Comparison of distribution of time loss by percentage of concussions and regular season of play.
Independent variables of interest
The median age of players sustaining concussion was 27 years (IQR 24–30 [range 18–41] years). One hundred sixty-two (30.5%) of the concussions were sustained by centremen, 167 (31.4%) by defencemen, 179 (33.6%) by wingers and 24 (4.5%) by goalies. Information on position was missing for 27 instances. Given that there are generally two defencemen, two wingers and one centreman on the ice at any given time, the proportion of concussions sustained by centremen was about twice that of defencemen and wingers. During the seven years of study, 368 instances of concussion (69.2%) were the first concussive event (median time loss 6 [IQR 2–13] days), 116 instances (21.8%) were the second concussive event (median time loss 8 [IQR 3–14] days), 32 instances (6.02%) were the third concussive event (median time loss 9 [IQR 4–22] days), 12 instances (2.26%) were the fourth concussive event (median time loss 7 [IQR 5–9] days), and 4 instances (0.75%) were the fifth concussive event (median time loss 31 [IQR 12–106] days).
A Kruskal–Wallis test showed a significant difference in median time loss across different levels of recurrent concussion (p = 0.007). A linear regression analysis adjusted for age and position showed that, on average, time loss increased 2.25 times (95% confidence interval [CI] 1.41–3.62) for every subsequent (i.e., recurrent) concussion sustained during the study period.
Table 2 highlights summary statistics for the consistently recorded initial postconcussion signs, symptoms and physical examination findings for the 559 instances of concussion. The most common postconcussion symptom reported was headache (71%), followed by dizziness (34%), nausea (24%), neck pain (23%), low energy or fatigue (22%), and blurred vision (22%). Amnesia (either anterograde or retrograde) was experienced in 21% of instances of concussion, whereas loss of consciousness was reported in 18% of instances (mean period of loss of consciousness 19.3 [range 1–300] seconds). Neurologic examination findings were abnormal in 13% of cases.
Table 2:
Summary medical statistics for 559 instances of game-related concussion sustained over seven consecutive National Hockey League (NHL) regular seasons (1997–2004)
| Variable* | Yes | % present |
|---|---|---|
| Symptoms† (n = 533) | ||
| Headache | 378 | 70.9 |
| Dizziness | 181 | 34.0 |
| Nausea | 126 | 23.6 |
| Neck pain | 122 | 22.9 |
| Low energy or fatigue | 119 | 22.3 |
| Blurred vision | 117 | 21.9 |
| Light sensitivity | 52 | 9.8 |
| Nervousness or anxiety | 40 | 7.5 |
| Irritability | 39 | 7.3 |
| Vomiting | 23 | 4.3 |
| Amnesia (n = 534) | 110 | 20.6 |
| Loss of consciousness (n = 537) | 98 | 18.2 |
| Abnormal physical examination (n = 518) | 93 | 17.9 |
| Head, ears, eyes, nose, throat | 27 | 13.8 |
| Cervical spine | 11 | 5.7 |
| Cardiorespiratory | 0 | 0.0 |
| Abnormal neurologic examination (n = 519) | 65 | 12.5 |
| Cerebellar examination | 19 | 10.2 |
| Tandem gait | 27 | 8.7 |
| Rhomberg | 6 | 4.6 |
| Vestibular-ocular reflex | 8 | 4.4 |
| Finger-nose-finger | 3 | 2.2 |
| Eye motion | 2 | 1.5 |
| Cranial nerve | 3 | 0.8 |
| Visual Field | 1 | 0.7 |
| Motor examination | 1 | 0.5 |
| Deep tendon reflex | 0 | 0.0 |
| Sensory examination | 0 | 0.0 |
| Pronator drift | 0 | 0.0 |
Instances for which variable-specific data were missing were as follows: symptoms = 26, amnesia = 25, loss of consciousness = 22, abnormal physical examination = 41, abnormal neurologic examination = 40.
Includes only the 10 initial postconcussion symptoms for which data were consistently recorded across seasons.
In 69% of instances of concussion, between one and three of the 10 consistently documented symptoms were experienced, whereas in 20% of instances, four or more symptoms were experienced. Symptoms other than those consistently documented over the seven years of study were experienced in 11% of instances (Appendix 4, available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
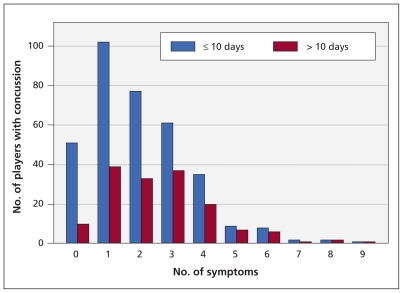
Figure 2 shows the distribution of symptoms in players who experienced time loss of more than 10 days and those who experienced time loss of less than 10 days. A linear regression analysis adjusted for age and position showed that, on average, time loss increased 1.89 times (95% CI 1.53–2.34) for each additional postconcussion symptom experienced.
Figure 2:
Distribution of symptoms in players who experienced time loss of more than 10 days and those who experienced time loss of less than 10 days. Consistently documented initial postconcussion symptoms were headache, nausea, neck pain, fatigue or low energy, irritability, nervousness or anxiety, blurred vision, photophobia or sensitivity to light, dizziness and vomiting.
Univariable logistic regression analysis showed that headache, loss of consciousness, low energy or fatigue, and light sensitivity were significant predictors of time loss greater than 10 days. Controlling for age and position, headache (odds ratio [OR] 2.17, 95% CI 1.33–3.54) and low energy or fatigue (OR 1.72, 95% CI 1.04–2.85) remained significant predictors in the multiple regression setting (Table 3).
Table 3:
Unadjusted and adjusted multivariable logistic regression analyses of potential predictors of time loss greater than 10 days among players with concussion
| Predictors of time loss (> 10 days v. ≤ 10 days) | Unadjusted analysis | Multivariable analysis, adjusted* | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Headache | 2.23 | 1.40–3.56 | 0.001 | 2.17 | 1.33–3.54 | 0.002 |
| Low energy or fatigue | 1.86 | 1.18–2.93 | 0.008 | 1.72 | 1.04–2.85 | 0.03 |
| Loss of consciousness | 1.70 | 1.04–2.78 | 0.034 | 1.69 | 0.97–2.94 | 0.06 |
| Amnesia | 1.41 | 0.88–2.26 | 0.16 | 1.26 | 0.73–2.19 | 0.41 |
| Dizziness | 1.25 | 0.83–1.89 | 0.28 | 0.86 | 0.55–1.36 | 0.53 |
| Nausea | 1.24 | 0.79–1.94 | 0.35 | 0.91 | 0.55–1.53 | 0.73 |
| Neck pain | 1.13 | 0.72–1.79 | 0.59 | 0.95 | 0.58–1.55 | 0.84 |
| Blurred vision | 1.09 | 0.69–1.73 | 0.96 | 0.98 | 0.60–1.60 | 0.94 |
| Light sensitivity | 1.88 | 1.02–3.46 | 0.043 | 1.61 | 0.82–3.13 | 0.17 |
| Nervousness or anxiety | 1.49 | 0.74–3.03 | 0.27 | 1.00 | 0.44–2.26 | 0.99 |
| Irritability | 1.21 | 0.56–2.59 | 0.63 | 0.76 | 0.32–1.82 | 0.55 |
| Vomiting | 1.40 | 0.53–3.69 | 0.50 | 1.21 | 0.41–3.56 | 0.73 |
| Abnormal neurologic exam | 1.44 | 0.83–2.51 | 0.19 | 1.24 | 0.69–2.23 | 0.47 |
Note: CI = confidence interval, OR = odds ratio.
Adjusted for age (in years) and player position.
Sensitivity analysis was performed by treating time loss as a continuous outcome. Log-transformation of time loss was applied because of a highly right-skewed distribution, with 41 cases requiring a change in time loss from 0 days to 0.00001 days to avoid exclusion of these cases during the transformation. Controlling for age and position, significant predictors of time loss in the multivariable linear model included headache (p < 0.001), low energy or fatigue (p = 0.01), amnesia (p = 0.02) and abnormal neurologic examination findings (p = 0.01) (Appendix 5, available at www.cmaj.ca/cgi/content/full/cmaj.092190/DC1).
Postconcussion actions
Table 4 shows the distribution of postconcussion actions with associated time loss and the percentage of instances of concussion that resulted in time loss greater than 10 days. In 70% (369/529) of instances, the players with concussion were removed from play during the regular season game in which they sustained the concussion (median time loss 7 [IQR 3–12, range 0–185] days; time loss greater than 10 days 31% [115/369]).
Table 4:
Distribution of postconcussion actions with associated time loss* and percentage of instances of concussion in which time loss was more than 10 days
| Postconcussion action | Frequency | % | Median time loss, d | Interquartile range | % > 10 days |
|---|---|---|---|---|---|
| Continued to play without evaluation and retrospectively diagnosed with concussion | 56 | 10.59 | 2.5 | 0.0–11.5 | 26.8 |
| Evaluated or observed and returned to play | 44 | 8.32 | 0.0 | 0.0–4.0 | 13.6 |
| Evaluated and removed from play | 369 | 69.75 | 7.0 | 3.0–12.0 | 31.2 |
| Admitted to hospital | 24 | 4.54 | 16.5 | 8.5–31.5 | 70.8 |
| Data not available | 36 | 6.81 | 8.0 | 3.5–14.5 | 36.1 |
| Total | 529 | 100.00 |
Data on time loss was missing for 30 instances of concussion.
In 8% of instances of concussion (44/529), the players were evaluated or observed and returned to play in the same game. Although the median time loss was 0 (IQR 0–4, range 0–342) days for these players, 14% (6/44) subsequently experienced more than 10 days of time loss. In 25 instances (57%), the players did not miss any subsequent time after being evaluated and returned to play in the same game. Of note, there was no report of loss of consciousness, amnesia or abnormal physical or neurologic examination findings among any of the players who were evaluated or observed and returned to play in the same game.
In 11% of instances of concussion (56/529), the players continued to play (because the injury was not observed or was not reported by the player) and then later reported symptoms to the medical staff after the game (median time loss 2.5 [IQR 0–11.5, range 0–275] days; time loss greater than 10 days 27% [15/56]).
In 5% of instances of concussion (24/529), the players were sent to hospital (28/531) (median time loss 16.5 days [IQR 8.5–31.5, range 0–100] days; time loss greater than 10 days 71%). Among patients sent to hospital, 63% (15/24) experienced loss of consciousness (p < 0.001) and 54% (13/24) experienced either anterograde or retrograde amnesia (p = 0.001).
Interpretation
Rates of concussion in NHL regular-season games declined from a peak of 7.7 concussions per 100 players during the 2000–2001 season to 4.9 per 100 players during the 2003–2004 season. Possible explanations for this finding include the following: more conservative management or return-to-play decisions by physicians; increase in the NHL in the severity of concussions (i.e., longer time to complete resolution of postconcussion symptoms); failure by players to report symptoms for fear of being held out of games; reporting by players of only severe symptoms; use by NHL team physicians of higher thresholds for diagnosis of concussion; or increasing use of neuropsychological testing results before making return-to-play decisions.
Using modelling techniques for multiple regression, several initial postconcussion clinical manifestations were found to be significant predictors of time loss (headache, low energy or fatigue, amnesia, and abnormal neurologic examination). These findings are of use to physicians, medical support staff, players, coaches and management, given that they have prognostic utility for assessing concussion severity at the time of injury.
In 27% percent of instances of concussion in which the player continued to play without game-time medical evaluation, more than 10 days of time loss resulted. Possible explanations include the following: the injury of the players was not observed or recognized; the players did not report their symptoms to medical staff; symptoms may not have been present at the time of the event and only occurred after the game; or players simply did not recognize their symptoms because of their concussion. It is becoming more apparent that athletes with acute concussion experience functional or cognitive impairment and reduced reaction times.24–26 It is possible that continued exertion in the immediate postconcussion period may exacerbate the injury or increase a player’s susceptibility to further injury, which may ultimately increase severity and prolong recovery.
Our results suggest that, on average, time loss significantly increased for every subsequent (repeat) concussion sustained during the study period, as well as for each increase in the number of postconcussion symptoms experienced. This finding is consistent with others reported in the literature21,22,27,28 and suggests that more conservative or precautionary measures should be taken in the presence of such factors.
Estimating concussion severity and subsequent time loss from athletic participation at the time of injury has been a daunting task for health care professionals. Because there are presently no direct prognostic measures of concussion severity or concussion resolution, severity can only be determined in retrospect, when symptoms have completely resolved (during rest and postexertion) and cognitive function has returned to baseline. Although several studies have advanced the understanding of the natural history of concussion and recovery from it,21,26–31 we are not aware of any prospective studies that have been conducted to specifically assess the predictive utility of initial postconcussion clinical manifestations for time loss in a cohort of male professional ice-hockey players.
Limitations
Our study had limitations. First, underreporting of concussion diagnosis by physicians may have occurred but could not be measured. Second, it is unknown if different reporting and return-to-play thresholds existed among physicians of different teams. Third, there was no systematic collection of data on practice-, exhibition- and playoff-related concussions, so the accuracy and completeness of reporting for these injuries could not be ascertained. Fourth, the NHL-NHLPA Concussion Program evolved over the seven-year period of our study, and only those signs, symptoms and physical examination findings that remained consistent from season to season were included in the analyses.
Fifth, it was not clear exactly when specific symptoms occurred or recurred after the initial concussive event in instances in which players with concussion continued to play or those in which they returned to play after evaluation or observation. Sixth, prior history of concussion was not collected on the physician evaluation forms. Thus, we could comment only on recurrent concussions observed during the seven years of study. Seventh, the sensitivity analysis treating time loss as a continuous variable in the linear regression model identified more significant predictors than the logistic model that used a 10-day time loss cut-point as a marker of concussion severity. This is a limitation of dichotomizing continuous variables that often results in loss of information. Eighth, we collected information on the basis of instances of concussion and not individual players. Hence, we were not able to adjust our analyses for clustering of multiple concussions within players.
Lastly, this study had a descriptive observational epidemiologic design, and therefore, it cannot provide detailed insights into the underlying biology or pathophysiology of concussions. Although we can be certain only that the results of this study are generalizable to adult male professional ice-hockey players, it is plausible that similar findings would be observed for adult men with concussion in nonprofessional hockey as well as other contact or collision sports. It is unknown whether similar results would be observed for children, women or concussions not related to sports.
Conclusion
This large prospective case series of concussions contributes to the understanding of the natural history of concussion by prospectively documenting the frequency of initial postconcussion clinical manifestations and time loss experienced by male professional ice-hockey players. Using modelling techniques for multiple regression, four initial postconcussion clinical manifestations (headache, low energy or fatigue, amnesia, and abnormal neurologic examination) were found to be significant predictors of time loss among male professional ice-hockey players. Our results suggest that more should be done to educate all involved with the sport about the potential adverse effects associated with continuing to play while symptomatic, failing to report symptoms to medical staff and failure to recognize or evaluate any suspected concussion. Our findings also suggest that more conservative or precautionary measures should be taken in the immediate postconcussion period, particularly when an athlete reports or experiences a post-concussion headache, low energy or fatigue, amnesia, recurrent concussion or many different postconcussion symptoms, or when the athlete has an abnormal neurologic examination.
Supplementary Material
Acknowledgements
The authors acknowledge the following individuals, groups and funding organizations: the National Hockey League (NHL), the National Hockey League Players Association (NHLPA), the NHL team physicians, athletic therapists and athletic trainers who collected information for the NHL-NHLPA Concussion Program, members of the previous NHL Concussion Program Committee (including Dave Dryden, Dr. Mark Lovell and Kristen Hawn), the current NHL-NHLPA Concussion Working Group (including Dr. Ruben Echemendia (Chair), Dr. Mark Aubry, Dr. Paul Comper, Julie Grand, Jim McCrossin and Rob Zamuner), the Alberta Heritage Foundation for Medical Research and the Alberta Provincial CIHR Training Program in Bone and Joint Health.
See related commentary by Sojka on page 887 and at www.cmaj.ca/cgi/doi/10.1503/cmaj.110504 and analysis article by Johnson on page 921 and at www.cmaj.ca/cgi/doi/10.1503/cmaj.110282.
Footnotes
Competing interests: Brian Benson is on contract with the NHL as a concussion data analyst and publication consultant. Willem Meeuwisse is a medical consultant for the National Hockey League (NHL). John Rizos is a medical consultant for the NHL Players Association. Charles Burke is a team physician for the Pittsburgh Penguins NHL club.
This article has been peer reviewed.
Contributors: Brian Benson was the principal investigator and takes responsibility for the integrity of the data and accuracy of the data analysis. Brian Benson, Willem Meeuwisse, John Rizos and Charles Burke had full access to all of the data, and contributed to the design of the study and the interpretation of the results. Brian Benson contributed to the analysis of the data. Jian Kang was responsible for technical aspects of the data analysis and participated in data interpretation. Brian Benson and Jian Kang contributed to the drafting of the manuscript, and Willem Meeuwisse, John Rizos and Charles Burke critically reviewed it. All of the authors approved the final version of the manuscript submitted for publication.
Funding: The Alberta Heritage Foundation for Medical Research and The Alberta Provincial CIHR Training Program in Bone and Joint Health provided financial support as part of the principal investigator’s Doctorate Program in Epidemiology, Department of Community Health Sciences, Faculty of Medicine, University of Calgary.
References
- 1.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the first International Conference on Concussion in Sport, Vienna 2001. Clin J Sport Med 2002;12:6–11 [DOI] [PubMed] [Google Scholar]
- 2.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd international conference on concussion in sport, Prague 2004. Clin J Sport Med 2005;15:48–55 [DOI] [PubMed] [Google Scholar]
- 3.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport, 3rd International Conference on Concussion in Sport, held in Zurich, November 2008. Clin J Sports Med 2009;19:185–200 [DOI] [PubMed] [Google Scholar]
- 4.Cantu RC. Reflections on head injuries in sport and the concussion controversy [editorial]. Clin J Sport Med 1997;7:83–4 [DOI] [PubMed] [Google Scholar]
- 5.Goodman D, Gaetz M, Meichenbaum D. Concussion in hockey: There is cause for concern. Med Sci Sports Exerc 2001;33:2004–9 [DOI] [PubMed] [Google Scholar]
- 6.Stuart MJ, Smith A. Injuries in junior A ice hockey: a three-year prospective study. Am J Sports Med 1995;23:458–61 [DOI] [PubMed] [Google Scholar]
- 7.Safety in youth ice hockey: the effects of body checking. American Academy of Pediatrics. Committee on Sports Medicine and Fitness Pediatrics 2000;105(3 Pt 1):657–58 [DOI] [PubMed] [Google Scholar]
- 8.Molsa JJ, Tegner Y, Alaranta H, et al. Spinal cord injuries in ice hockey in Finland and Sweden from 1980–1996. Int J Sports Med 1999;20:64–7 [DOI] [PubMed] [Google Scholar]
- 9.Marchie A, Cusimano M. Bodychecking and concussions in ice hockey: Should our youth pay the price? CMAJ 2003;169:124–8 [PMC free article] [PubMed] [Google Scholar]
- 10.Emery CA, Meeuwisse WH, McAllister JR. A survey of sport participation, sport injury and sport safety practices in adolescents. Clin J Sport Med 2006;16:20–6 [DOI] [PubMed] [Google Scholar]
- 11.Benson BW, Mohtadi NG, Rose MS, et al. Head and neck injuries among ice hockey players wearing full face shields vs half face shields. JAMA 1999;282:2328–32 [DOI] [PubMed] [Google Scholar]
- 12.Wennberg RA, Tator CH. National Hockey League reported concussions, 1986–87 to 2001–02. Can J Neurol Sci 2003;30:206–9 [DOI] [PubMed] [Google Scholar]
- 13.Benson BW, Rose MS, Meeuwisse WH. The impact of face shield use on concussions in ice hockey: a multivariate analysis. Br J Sports Med 2002;36:27–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agel J, Dompier T, Dick R, et al. Descriptive epidemiology of collegiate men’s ice hockey injuries: National Collegiate Athletic Association injury surveillance system, 1988–1989 through 2003–2004. J Athl Train 2007;42:241–8 [PMC free article] [PubMed] [Google Scholar]
- 15.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury. J Head Trauma Rehabil 2006;21:375–8 [DOI] [PubMed] [Google Scholar]
- 16.Wennberg RA, Tator CH. Concussion incidence and time lost from play in the NHL during the past 10 years. Can J Neurol Sci 2008;35:647–51 [DOI] [PubMed] [Google Scholar]
- 17.Meeuwisse W, Burke C, Benson B. NHL concussion program: a 5-year prospective study [abstract]. Clin J Sport Med 2003;13:380 [Google Scholar]
- 18.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association Position Statement: management of sport-related concussion. J Athl Train 2004;39:280–97 [PMC free article] [PubMed] [Google Scholar]
- 19.Cantu RC, Herring S, Putukian M. Correspondance: concussion. N Engl J Med 2007;356:1787–9 [DOI] [PubMed] [Google Scholar]
- 20.Broglio SP, Peutz TW. The effect of sport concussion on neurocognitive function, self-report symptoms and postural control: a meta-analysis. Sports Med 2008;38:53–7 [DOI] [PubMed] [Google Scholar]
- 21.Iverson G. Predicting slow recovery from sport-related concussion: the new simple-complex distinction. Clin J Sport Med 2007;17:31–7 [DOI] [PubMed] [Google Scholar]
- 22.Lau B, Lovell M, Collins M, et al. Neurocognitive and symptom predictors of recovery in high school athletes. Clin J Sport Med 2009;19:216–21 [DOI] [PubMed] [Google Scholar]
- 23.Makdissi M. Is the simple versus complex classification of concussion a valid and useful differentiation? Br J Sports Med 2009;43(Suppl 1):i23–7 [DOI] [PubMed] [Google Scholar]
- 24.Warden DL, Bleiberg J, Cameron KL, et al. Persistent prolongation of simple reaction time in sports concussion. Neurology 2001;57:524–6 [DOI] [PubMed] [Google Scholar]
- 25.Collie A, Makdissi M, Maruff P, et al. Cognition in the days following concussion: comparison of symptomatic versus asymptomatic athletes. J Neurol Neurosurg Psychiatry 2006;77:241–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: The NCAA Concussion Study. JAMA 2003;290:2556–63 [DOI] [PubMed] [Google Scholar]
- 27.Collins MW, Iverson GL, Lovell MR, et al. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med 2003;13:222–9 [DOI] [PubMed] [Google Scholar]
- 28.McCrory PR, Ariens T, Berkovic SF. The nature and duration of acute concussive symptoms in Australian football. Clin J Sport Med 2000;10:235–8 [DOI] [PubMed] [Google Scholar]
- 29.Casson IR, Viano DC, Powell JW, et al. Twelve years of national football league concussion data. Sports Health 2010;2:471–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Erlanger D, Kaushik T, Cantu R, et al. Symptom-based assessment of the severity of a concussion. J Neurosurg 2003;98:477–84 [DOI] [PubMed] [Google Scholar]
- 31.Lovell MR, Iverson GL, Collins MW, et al. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med 1999;9:193–8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.