Abstract
Objectives. To assess whether any benefits from adjunctive homeopathic intervention in patients with RA are due to the homeopathic consultation, homeopathic remedies or both.
Methods. Exploratory double-blind, randomized placebo-controlled trial conducted from January 2008 to July 2008, in patients with active stable RA receiving conventional therapy. Eighty-three participants from three secondary care UK outpatient clinics were randomized to 24 weeks of treatment with either homeopathic consultation (further randomized to individualized homeopathy, complex homeopathy or placebo) or non-homeopathic consultation (further randomized to complex homeopathy or placebo). Co-primary outcomes: ACR 20% improvement (ACR20) criteria and patient monthly global assessment (GA). Secondary outcomes: 28-joint DAS (DAS-28), tender and swollen joint count, disease severity, pain, weekly patient and physician GA and pain, and inflammatory markers.
Results. Fifty-six completed treatment phase. No significant differences were observed for either primary outcome. There was no clear effect due to remedy type. Receiving a homeopathic consultation significantly improved DAS-28 [mean difference 0.623; 95% CI 0.1860, 1.060; P = 0.005; effect size (ES) 0.70], swollen joint count (mean difference 3.04; 95% CI 1.055, 5.030; P = 0.003; ES 0.83), current pain (mean difference 9.12; 95% CI 0.521, 17.718; P = 0.038; ES 0.48), weekly pain (mean difference 6.017; 95% CI 0.140, 11.894; P = 0.045; ES 0.30), weekly patient GA (mean difference 6.260; 95% CI 0.411, 12.169; P = 0.036; ES 0.31) and negative mood (mean difference − 4.497; 95% CI −8.071, −0.923; P = 0.015; ES 0.90).
Conclusion. Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable RA.
Trial registration. Current controlled trials, http://www.controlled-trials.com/, ISRCTN09712705.
Keywords: Clinical trial, Homeopathy, Rheumatoid arthritis, Consultation
Introduction
RA is a chronic inflammatory disease of unknown aetiology with a worldwide prevalence of 1% [1]. DMARDs are toxic and of variable efficacy; combination therapy seems to be most effective [2]. Homeopathy is a popular complementary medical intervention [complementary and alternative medicine (CAM)] for chronic conditions with patients reporting considerable satisfaction [3], but its use engenders much debate [4]. A meta-analysis evaluating homeopathy for RA (three trials employing individualized [5–7] and one using complex homeopathy [8, 9]) identified an odds ratio of 2.0 [10] favouring homeopathy in spite of contradictory evidence for the specific efficacy of homeopathy over placebo [11]; homeopathic intervention appears to be clinically beneficial for RA. There is no commonly accepted mechanism for ultra-molecular dilutions and it has been suggested that any clinical benefit results from the placebo effects attributable to the clinical consultations rather than the remedies but this has not been formally assessed.
There is evidence for the therapeutic benefits of the consultation process on health outcomes in both conventional medicine and CAM [12, 13]. These contextual effects include factors that are not the active components of the treatment but are inherent within the whole treatment package [12–15]. Research into the homeopathic consultation has identified contextual factors such as empathy and empowerment [16], which may mediate the homeopathic process. Homeopathy consultations involve a complete exploration of the patient’s emotional, spiritual and physical well-being to enable treatment of the whole person not just the illness.
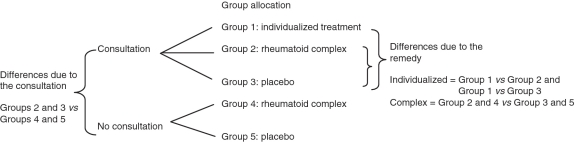
We utilized a five-arm design (Fig. 1) to identify where clinical benefits arose. Patients receiving a consultation were randomly prescribed individualized homeopathy, a fixed combination of remedies (complex homeopathy) or placebo. Those not receiving consultation received either complex homeopathy or placebo. There is evidence for employing both individualized [5–7] and complex homeopathic [8, 9] approaches in RA. Individualized or classical homeopathy is based on identifying the totality of individualized symptoms using the law of similars by matching the clinical picture of the patient to one particular remedy [17]. Complex homeopathy involves homeopathic mixtures of commonly prescribed remedies for specific problems and can be used without a consultation. The aim was to identify whether therapeutic benefits were attributable to the homeopathic remedy, the homeopathic consultation or both. The trial was exploratory as we wished to explore how the consultation process may potentially be eliciting clinical benefit using relevant measures.
Fig. 1.
Study design showing randomization scheme and specific contrasts.
Methods
Design
This was a multi-centred placebo-controlled randomized double-blind exploratory clinical trial assessing homeopathy (remedy ± consultation) as an adjunctive treatment for RA.
Setting and participants
Participants from rheumatology outpatient departments at three hospitals in the UK, meeting the inclusion/exclusion criteria (Table 1), were recruited from January 2006 to July 2008; we recruited adults formally diagnosed with RA for at least 2 years, who had had relatively stable disease but some disease activity on entry (DAS > 2.6). Ethical approval was obtained [multi-centre research ethics committee, Scotland A (05/MRE00/30) and from the local research ethics committees]. Patients provided written informed consent.
Table 1.
Eligibility criteria and process of randomization and treatment allocation
| Eligibility criteria | |
|---|---|
| Inclusion criteria | Exclusion criteria |
| Aged >18 years | Severe RA (functional status Class IV) |
| Diagnosis of RA for >2 years [1987 ACR guidelines | Taking biological DMARDS, e.g. anti-TNF |
| Current disease activity: minimum DAS-28 score >2.6 | Severe comorbidities that would affect their RA |
| Patient GA score of ≥30 mm | Used homeopathy for <3 months |
| Stable medication for >3 months | Pregnant or breastfeeding |
| Participated in an investigational trial within 45 days before enrolment. | |
| Randomization details | |
|---|---|
| Allocation sequence generation: separate randomization codes for each study site were generated by computer program by the study statistician using a block size of 5 as follows: C1, C2, C3, N2, N3 [where C = consultation and N = no consultation and 1, 2, 3 are the three treatments (1 = individual, 2 = complex and 3 = placebo)]. At all sites, patients were randomly allocated to one of the treatment groups at a ratio of 1 : 1 : 1 : 1 : 1 between the five treatment arms; at each site, each enrolled patient was assigned the next sequentially ordered sealed envelope reporting the randomization code. | |
| Allocation concealment: randomization was a two-staged process using sealed envelopes. The first envelope was opened by the study nurse once the patient passed baseline screening to identify allocation to consultation or no consultation. Randomization to consultation/no consultation was therefore not blinded. When the patient returned for treatment visits, the enclosed sealed second envelope was opened by staff unrelated to the study trial to identify the patient’s treatment allocation; this was faxed to the independent off-site pharmacist to allocate the correct medication. Randomization to treatment allocation was therefore blinded to patients and all study staff. |
Randomization
Patients were randomized into five groups (Fig. 1). Randomization is described in Table 1. Of the five groups, three received a homeopathic consultation (Groups 1–3) and two (Groups 4 and 5) did not. The consultation groups were further randomized to individualized treatment (Group 1), a homeopathic complex for RA (Group 2) or placebo (Group 3).
Non-consultation participants were allocated complex (Group 4) or placebo (Group 5); individualized homeopathy can only be prescribed through a consultation. The study design enabled the following comparisons:
Contrast 1: the effect of the consultation; by comparing the consultation and non-consultation groups; Groups 2 and 3 vs Groups 4 and 5. Those receiving individualized homeopathic treatment were excluded because there was no direct comparison for the non-consultation group.
Contrast 2: the effect of the complex treatment; comparing Groups 2 and 4 with Groups 3 and 5.
Contrast 3: the difference in effect between individualized treatment and complex; comparing Groups 1 and 2.
Contrast 4: the effect of individualized remedy; comparing Groups 1 and 3.
Study procedures
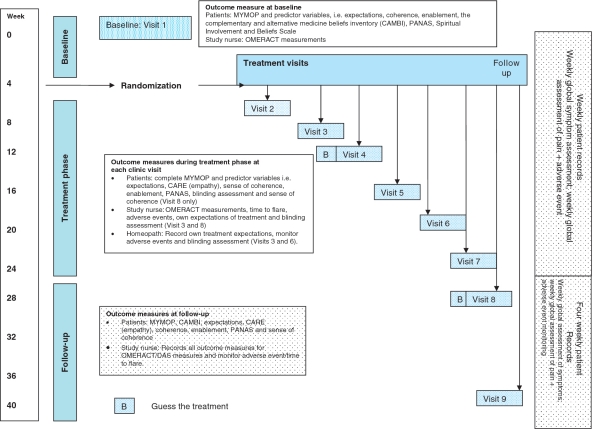
Participants with active disease were recruited from consultant lists and remained on their conventional medication throughout but were withdrawn if their DMARD was changed or if they received >80 mg of steroids in total during the treatment period. Figure 2 outlines the study procedures; all clinics were held in secondary care. Patients were screened at baseline clinic (Visit 1) then randomized. The trial period was 40 weeks; patients attended for seven further clinic visits on a 4 weekly basis during treatment (Visits 2–8); follow-up was Week 40 (Visit 9). All clinic visits were standardized; all participants saw a study nurse where assessments and outcome measures were recorded. Participants randomized to consultation additionally received a homeopathic consultation from Visits 2–6 inclusive (first consultation was 1 h with 30-min follow-ups). Two qualified experienced non-medical homeopaths (each with 15 years experience, classically trained) prescribed individualized homeopathic treatment at each visit mirroring normal practice. In between clinic visits, patients also completed weekly diaries recording pain, global assessment (GA) and adverse events. Further details of the intervention using standardized homeopathic reporting guidelines [18] can be obtained from the authors.
Fig. 2.
Study procedures.
Interventions
Trial medication
This was posted to participants after clinic Visits 2–7 by an off-site homeopathic pharmacist, in accordance with randomization allocation and taken twice daily during the treatment phase; this dosing regimen is appropriate in chronic conditions such as RA [19]. The interventions were:
Individualized homeopathy prescribed as tablets (Group 1 only). The homeopaths prescribed from the entire homeopathic repertoire. A post-analysis review confirmed that all individualized homeopathy was prescribed at ultra-molecular doses (all fifty millesimal potency scale potencies).
A standardized commercial homeopathic complex (Groups 2 and 4) previously reported as efficacious for RA [8, 9]; Rheumaselect (Dreluso, Hessisch Oldendorf Germany). The complex was a liquid taken 20 drops/dose twice daily. It contains Rhus Toxicodendron D4, Bryonia cretica D4, Strychnos nux-vomica D4, Berberis vulgaris D4 and Ledum palustre D4 in 20 ml. Two placebos were prepared identical in colour, taste and consistency to the homeopathic tablets and complex (Groups 3 and 5).
The homeopathic consultation
Consultations were conducted as in normal practice. The process of the consultation was standardized in that specific topics were covered (e.g. detailed clinical history, current symptoms and medication, assessment of emotional and mental states, etc.) to identify the relevant information to prescribe. The content of the consultations varied between patients and between consultations; homeopathic intervention is individualized and patient centred and led by the patient’s narratives. Details of the homeopathic consultations are reported in our nested qualitative study (Brien et al., 2010, submitted for publication).
Allocation concealment
Patients and study staff were aware of consultation allocation but were all blinded to treatment allocation. All patients received one bottle of tablets (individualized remedy or placebo as appropriate) and a bottle of liquid (either homeopathic complex or equivalent placebo) with a standardized dosing frequency ensuring blinding. All preparations were indistinguishable in appearance, taste and smell. The security of the blinding process was assessed by asking participants, homeopaths and the study nurse to guess which treatment they believed the participant received at Visits 4 and 8.
Outcome assessment
The two primary outcome measures were: (i) the proportion of patients meeting the ACR 20% improvement criteria (ACR20 response) based on the OMERACT [20]. ACR20 [21] is a validated rheumatological composite measure giving a binary outcome of treatment success (achieved or not achieved). (ii) Improvement in the patient’s GA of health [100-mm visual analogue scale (VAS)]. The GA is the patient’s response to ‘considering all the ways your arthritis affects you, please make a vertical line to show how well you are now’ with the terminators ‘disease completely inactive’ and ‘disease severely active’. This is considered the most sensitive variable of all the OMERACT measures in detecting symptom change [22]. A clinically significant improvement is a minimum 35% change from baseline to the end of treatment [23].
A number of secondary outcomes were employed:
The DAS-28 is a continuous summary measure recording changes in disease activity over time developed by the EULAR [24]. It is the standard European research outcome measure comparable with the ACR criteria [25]. It includes both objective (ESR or CRP and swollen joints count) and subjective (tender joint counts and patient GA score) measures.
Individual measures included within the ACR20.
A 15% improvement in the Measure Yourself Medical Outcome Profile [26].
Changes in mood assessed with positive and negative affect scale (PANAS) [27].
Changes in weekly pain and patient GA (100-mm VAS).
Adverse events were recorded at clinic visits (study nurse) and between visits (patient recorded) using standardized forms.
Potential predictors of treatment outcome were: patient, study nurse and homeopath (for consultation group only) expectations of outcome (100-mm VAS); sense of coherence scale to assess the degree to which patients feel their life makes sense, is manageable and meaningful [28]; patients spirituality using the Spiritual Involvement and Beliefs Scale [29]; patient’s attitudes to and beliefs about CAM [30]; participant’s assessment of empathy using the Consultation and Relational Empathy (CARE) [31]; degree of enablement using Patient Enablement Instrument [32]; and baseline mood (PANAS) [27]. ‘Guess the treatment’ was recorded by nurses, patients and homeopaths during (Visit 4) and after treatment phase (Visit 8) as a measure of the security of blinding.
Sample size
No study has previously determined the effect size (ES) of the consultation or how relative this effect is to the specific treatment effect. The power calculation was estimated on the dichotomous primary outcome, ACR20 [33]. We required 110 participants (22 per arm) to detect a 30% difference in ACR20 for active vs placebo treatment and for consultation vs no consultation, using a 5% significance level with 80% power from baseline to end of treatment, allowing for a 20% loss to follow-up.
Statistical analyses
All analyses were completed on an intention to treat (ITT) basis using two-sided 5% significance levels. The randomization code was broken by the statistician after data entry was completed, the primary outcome determined and any data queries resolved. Logistic regression analysis assessed dichotomous data and analysis of covariance assessed continuous data comparing changes in scores from baseline to the end of treatment. Means (s.d.) are determined and, where appropriate, 95% CIs are quoted. Longitudinal analysis using first-order autoregressive correlation structure and generalized estimating equations (Stata version 10.1, 2009, StataCorp, College Station, TX) was used to fit models to the treatment scores for the relevant secondary outcome measures adjusting for baseline and other covariates. No missing values were imputed for longitudinal analysis since this method fits all available data to the model; thus data on patients who withdrew were included in the analysis to the point of withdrawal.
The four contrasts were evaluated on each outcome measure to assess particular comparisons. To avoid problems of multiple testing, only the four specified contrasts were examined and significance levels between 5 and 2% were treated with caution. ESs, i.e. standardized mean score differences, adjusted for baseline differences are reported where appropriate. Adverse events were reported using descriptive statistics. Assessment of blinding (by ‘guess the treatment’) was done by chi-squared test.
Results
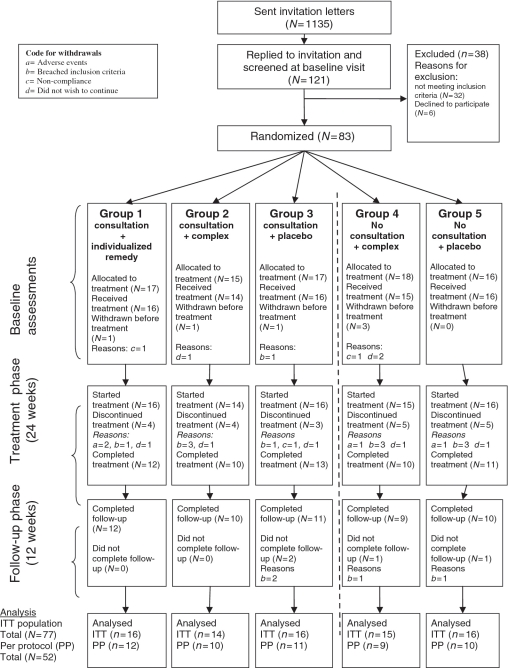
Participant flow is shown in Fig. 3. A total of 83 participants were randomized to treatment, of which 6 patients dropped out after randomization before treatment; 77 patients were included into the ITT. No group differences were observed between those who withdrew between randomization and end of treatment. Patients withdrew commonly for i.m. steroid injections, flare [n (%) = 8 (9.6)], or when they wanted to discontinue [n (%) = 9 (10.8)]. Baseline characteristics of the ITT population did not significantly differ for any variable (Table 2). Mean baseline DAS-28 was 4.54 (range 2.62–7.37) with 25 (32%) patients having a high level of disease activity (DAS-28 > 5.1).
Fig. 3.
Patient flow.
Table 2.
Baseline characteristics of patients allocated to treatment group (ITT population including withdrawals)
| Consultation-type allocation | Consultation |
No consultation |
|||
|---|---|---|---|---|---|
| Medication-type allocation | Individual | Complex | Placebo | Complex | Placebo |
| Treatment group | 1 (n = 16) | 2 (n = 14) | 3 (n = 16) | 4 (n = 15) | 5 (n = 16) |
| Females, n (%) | 13 (81.3) | 9 (64.3) | 13 (81.3) | 11 (73.3) | 8 (50.0) |
| Age, years | 62.19 (13.71) | 63.43 (11.65) | 65.75 (11.70) | 60.33 (14.90) | 64.88 (9.52) |
| Duration of arthritis in years | 10.75 (7.54) | 12.14 (9.91) | 12.44 (12.61) | 8.20 (6.39) | 11.44 (9.44) |
| Number of other medical complaints | 1.75 (1.48) | 1.53 (1.73) | 2.13 (2.22) | 1.56 (1.82) | 1.25 (2.05) |
| Number of RA medication on entry to study | 1.88 (1.15) | 2.36 (0.84) | 1.75 (0.93) | 2.27 (0.70) | 2.19 (1.05) |
| Baseline rheumatological measures | |||||
| DAS-28a (range 0–10) | 4.69 (0.84) | 4.23 (1.12) | 4.87 (0.96) | 4.68 (0.97) | 4.21 (1.09) |
| Swollen joint count (range 0–28) | 4.06 (3.30) | 4.43 (4.13) | 6.94 (7.32) | 2.93 (2.37) | 3.56 (2.68) |
| Tender joint count (range 0–28) | 8.06 (5.90) | 5.86 (8.48) | 7.94 (7.31) | 7.13 (6.36) | 6.13 (7.24) |
| Pain VAS (0–100) | 36.88 (19.72) | 46.57 (14.04) | 38.94 (16.10) | 39.27 (18.38) | 42.06 (21.38) |
| CRP, mg/l | 14.73 (20.00) | 11.62 (9.78) | 9.52 (8.29) | 15.00 (14.02) | 8.22 (5.46) |
| ESR, mm/h | 25.67 (11.35) | 18.29 (10.78) | 28.00 (15.71) | 30.00 (22.83) | 19.56 (13.72) |
| Other measures | |||||
| HAQ (range 1–3) | 1.21 (0.68) | 1.21 (0.76) | 1.19 (0.68) | 1.38 (0.61) | 1.34 (0.69) |
| Patient GA (VAS, range 0–100) | 45.94 (13.20) | 55.21 (13.54) | 49.81 (10.82) | 51.13 (13.09) | 55.13 (18.24) |
| Physician GA (VAS, range 0–100) | 41.94 (12.6) | 45.93 (12.7) | 45.94 (9.7) | 44.93 (12.7) | 41.75 (18.3) |
| Positive mood (PANAS; range 10–50) | 30.63 (7.82) | 31.14 (9.57) | 31.56 (9.08) | 28.73 (8.56) | 33.31 (6.49) |
| Negative mood (PANAS; range 10–50) | 20.75 (7.78) | 16.57 (4.99) | 17.94 (8.53) | 15.93 (4.48) | 19.50 (6.80) |
| Measure yourself medical outcome profile (range 0–6) | 3.57 (1.00) | 3.55 (0.73) | 3.44 (0.72) | 3.47 (0.66) | 3.72 (0.82) |
| Patient expectations of treatment (range 0–10) | 4.31 (0.95) | 4.79 (0.43) | 4.94 (0.68) | 4.67 (1.05) | 5.00 (0.37) |
| Homeopath expectations of treatment (consultation groups only; range 0–10) | 4.25 (1.13) | 4.14 (0.86) | 4.25 (1.13) | NA | NA |
| Physician expectation of treatment (range 0–10) | 4.75 (0.58) | 4.93 (0.27) | 4.88 (0.62) | 4.93 (0.26) | 4.69 (0.48) |
| Spirituality (range 22–154) | 84.88 (18.70) | 82.43 (12.24) | 79.60 (18.68) | 81.27 (16.55) | 84.38 (24.11) |
| Sense of coherence (range 3–15) | 8.56 (1.59) | 8.93 (1.82) | 8.69 (1.54) | 8.73 (1.94) | 8.94 (1.88) |
| Attitudes to, and beliefs about CAMb | |||||
| Natural treatment (range 0–36) | 34.38 (5.81) | 34.64 (5.83) | 36.19 (4.71) | 31.47 (7.05) | 32.81 (5.91) |
| Participation in treatment (range 0–30) | 26.38 (4.81) | 27.43 (5.20) | 26.44 (4.57) | 27.73 (5.04) | 27.73 (4.03) |
| Holistic health (range 0–36) | 31.93 (3.45) | 29.71 (5.01) | 31.73 (5.26) | 29.60 (3.50) | 31.44 (5.72) |
Values are means (s.d.) or number of patients (%) unless otherwise stated. aDAS is calculated by DAS-28 = 0.56 × sqrt(tender28) + 0.28 × sqrt(swollen28) + 0.70 × ln(ESR) + 0.014 × GH. A cut-off level of DAS = 1.6 or a DAS-28 = 2.6 corresponded with being in remission following the ARA criteria. bA higher positive score indicates more positive belief.
Blinding of treatment allocation assessed by ‘guess the treatment’ was secure for the study nurse (Visit 4: χ2 = 1.41, degrees of freedom (df) = 2, P = 0.494; Visit 8: χ2 = 2.93, df = 2, P = 0.231) and subjects (Visit 4: χ2 = 0.67, df = 2, P = 0.717; Visit 8: χ2 = 3.77, df = 2, P = 0.152). The homeopaths were unable to guess treatment and thought more patients received individualized treatment when they were receiving either complex or placebo (Stuart Maxwell test, Visit 3: χ2 = 7.40, df = 2, P = 0.025) confirming blinding was secure.
Primary outcomes
Table 3 reports the number of patients per group achieving the ACR20 and 35% improvement in the patient GA. Logistic regression analyses of all randomized patients for the four contrasts are reported in Table 4. No significant differences were identified for the effects of consultation or treatment allocation for either of these primary outcomes.
Table 3.
Primary outcome measures: number of patients achieving an ACR20 and 35% improvement in patient GA
| Consultation-type allocation | Consultation |
No consultation |
|||
|---|---|---|---|---|---|
| Medication-type allocation | Individual | Complex | Placebo | Complex | Placebo |
| Treatment group allocation | 1 | 2 | 3 | 4 | 5 |
| No. of completers | 16 | 14 | 16 | 15 | 16 |
| No. of completers who achieved ACR20, n (%) | 5 (31.3) | 2 (14.3) | 5 (31.2) | 2 (13.3) | 2 (12.5) |
| No. of completers who achieved 35% patient GA, n (%) | 6 (37.5) | 6 (42.9) | 6 (37.5) | 4 (26.7) | 6 (37.5) |
Table 4.
Logistic regression analyses for the primary outcomes: ACR20 and 35% improvement in patient GAa
| Contrast | Contrasts evaluated |
Odds ratio | s.e. | 95% Cl | P-value | |
|---|---|---|---|---|---|---|
| Groups 2 and 3 | Groups 4 and 5 | |||||
| Consultation vs no consultation | n = 30 | n = 31 | ||||
| No. of patients who achieved ACR20, n (%) | 7 (23.3) | 4 (12.9) | 0.404 | 0.298 | 0.095, 1.714 | 0.219 |
| No. of patients who achieved 35% patient GA, n (%) | 12 (40.0) | 10 (32.2) | 0.725 | 0.424 | 0.231, 2.280 | 0.582 |
| Groups 2 and 4 | Groups 3 and 5 | |||||
|---|---|---|---|---|---|---|
| Complex vs placebo | n = 29 | n = 32 | ||||
| No. of patients who achieved ACR20, n (%) | 4 (13.8) | 7 (21.9) | 2.050 | 1.494 | 0.492, 8.548 | 0.324 |
| No. of patients who achieved 35% patient GA, n (%) | 10 (34.5) | 12 (37.5) | 1.142 | 0.652 | 0.373, 3.497 | 0.816 |
| Group 1 | Group 2 | |||||
|---|---|---|---|---|---|---|
| Individual vs complex | n = 16 | n = 14 | ||||
| No. of patients who achieved ACR20, n (%) | 5 (31.3) | 2 (14.3) | 0.258 | 0.259 | 0.036, 1.842 | 0.177 |
| No. of patients who achieved 35% patient GA, n (%) | 6 (37.5) | 6 (42.9) | 1.076 | 0.863 | 0.224, 5.181 | 0.927 |
| Group 1 | Group 3 | |||||
|---|---|---|---|---|---|---|
| Individual vs placebo | n = 16 | n = 16 | ||||
| No. of patients who achieved ACR20, n (%) | 5 (31.3) | 5 (31.2) | 1.262 | 1.045 | 0.249, 6.394 | 0.778 |
| Number of patients who achieved 35% patient GA, n (%) | 6 (37.5) | 6 (37.5) | 1.047 | 0.811 | 0.229, 4.781 | 0.953 |
aAdjusted for practitioner, baseline disease severity, baseline disease activity, sex, age, duration of illness, number of medications for RA and number of other medical complaints.
Secondary outcomes
The mean score differences for all secondary outcomes of completers from baseline to end of treatment are reported in Table 5. Also shown in Table 5 are the number of patients per group achieving a 15% reduction in Measure Yourself Medical outcome profile (MYMOP). The percentages are based on all 77 ITT patients; there were no significant group differences.
Table 5.
Secondary outcome measures after 24 weeks of treatment: mean differences (s.d.) between end of treatment and baselinea
| Consultation-type allocation | Consultation |
No consultation |
|||
|---|---|---|---|---|---|
| Medication-type allocation | Individual | Complex | Placebo | Complex | Placebo |
| Group number | 1 | 2 | 3 | 4 | 5 |
| Rheumatological measuresb | |||||
| DAS-28 | |||||
| Mean (s.d.) | −0.92 (1.56) | −0.74 (0.78) | −0.98 (1.28) | −0.02 (0.92) | −0.30 (0.77) |
| n | 12 | 9 | 12 | 9 | 11 |
| Swollen joint count | |||||
| Mean (s.d.) | −2.83 (4.59) | −2.44 (2.74) | −4.00 (6.51) | 1.89 (6.98) | −1.45 (2.66) |
| n | 12 | 9 | 12 | 9 | 11 |
| Tender joint count | |||||
| Mean (s.d.) | −4.00 (8.10) | −1.22 (2.99) | −2.83 (5.56) | −1.00 (3.67) | −0.73 (3.77) |
| n | 12 | 9 | 12 | 9 | 11 |
| Current pain (VAS) | |||||
| Mean (s.d.) | −3.75 (18.83) | −15.56 (27.36) | −8.00 (27.15) | 2.33 (19.07) | −7.40 (30.72) |
| n | 12 | 9 | 11 | 9 | 10 |
| CRP, mg/l | |||||
| Mean (s.d.) | −4.50 (27.67) | −3.31 (9.29) | 2.18 (13.74) | −4.10 (8.98) | −1.54 (6.53) |
| n | 11 | 9 | 12 | 8 | 11 |
| ESR, mm/h | |||||
| Mean (s.d.) | −0.36 (6.27) | −3.00 (11.55) | 0.73 (18.70) | −4.87 (4.94) | −3.00 (7.62) |
| n | 11 | 9 | 11 | 8 | 10 |
| HAQ | |||||
| Mean (s.d.) | −0.24 (0.69) | −0.19 (0.35) | −0.24 (0.50) | −0.26 (0.43) | −0.06 (0.16) |
| n | 12 | 9 | 12 | 10 | 11 |
| Patient GA | |||||
| Mean (s.d.) | −14.50 (17.96) | −18.22 (28.49) | −13.31 (26.28) | −4.11 (24.55) | −22.36 (28.82) |
| n | 12 | 9 | 13 | 9 | 11 |
| Physician GA | |||||
| Mean (s.d.) | −9.75 (14.99) | −20.00 (19.16) | −12.92 (20.38) | −3.78 (34.98) | −7.36 (26.84) |
| n | 12 | 9 | 13 | 9 | 11 |
| Other measuresb | |||||
| Positive mood | |||||
| Mean (s.d.) | 5.58 (6.49) | 3.33 (11.20) | 2.33 (8.55) | −1.50 (6.06) | −0.45 (5.73) |
| n | 12 | 9 | 12 | 10 | 11 |
| Negative moodb | |||||
| Mean (s.d.) | −4.25 (5.96) | −2.78 (2.68) | −5.75 (9.35) | 1.88 (2.23) | −3.00 (2.76) |
| n | 12 | 9 | 12 | 10 | 11 |
| MYMOP | |||||
| Mean (s.d.) | −0.96 (0.95) | −1.00 (0.86) | −1.55 (1.37) | −0.62 (1.29) | −1.07 (0.90) |
| n | 10 | 9 | 12 | 9 | 9 |
| Number of patients who achieved 15% MYMOP, n (%) | 8 (50.0) | 7 (50.0) | 10 (62.5) | 5 (33.3) | 7 (43.8) |
| Weekly pain scores (VAS) | |||||
| Mean (s.d.) | −5.67 (19.85) | −11.2 (27.06) | −5.80 (23.42) | 0.57 (9.96) | 11.16 (29.06) |
| n | 9 | 5 | 10 | 7 | 6 |
| Weekly GA | − | ||||
| Mean (s.d.) | −6.00 (14.98) | 8.60 (21.42) | −8.2 (28.41) | −2.14 (10.54) | −16.29 (24.55) |
| n | 9 | 5 | 10 | 7 | 7 |
aThe data reported are for completed patients only. bA negative sign indicates improvement except for the positive mood construct of the PANAS, where a positive sign indicates improvement. The negative mood construct of the PANAS was adjusted accordingly so that a negative sign indicates improvement.
Rheumatology measures: DAS-28 and individual OMERACT variables
Longitudinal analysis adjusted for significant covariates for each contrast for all patients randomized, are reported in Table 6.
Table 6.
Secondary outcome analysis: contrast estimates after 24 weeks of treatment with 95% CIs, significance achieved and ESs (s: pooled s.d.)a
| Contrasts | Contrast 1 Groups (2 and 3) vs (4 and 5) | Contrast 2 Groups (2 and 4) vs (3 and 5) | Contrast 3 Group 1 vs 2 | Contrast 4 Group 1 vs 3 |
|---|---|---|---|---|
| Treatment comparisons | Consultation vs no consultation | Complex remedy vs placebo | Individualized remedy vs complex remedy | Individualized remedy vs placebo |
| Rheumatological measures | ||||
| DAS-28 | ||||
| Estimate (95% CI) | 0.623 (0.186, 1.060) | 0.125 (−0.316, 0.566) | −0.085 (−0.704, 0.534) | 0.181 (−0.408, 0.769) |
| P-value | 0.005* | 0.579 | 0.787 | 0.547 |
| ES (s = 0.888) | 0.702 | 0.141 | −0.096 | 0.204 |
| Swollen joint count | ||||
| Estimate (95% CI) | 3.043 (1.055, 5.030) | −1.110 (–3.120, 0.900) | −1.021 (−3.845, 1.804) | −0.061 (−2.721, 2.599) |
| P-value | 0.003* | 0.279 | 0.479 | 0.964 |
| ES (s = 3.667) | 0.830 | −0.303 | −0.278 | −0.017 |
| Tender joint count | ||||
| Estimate (95% CI) | 1.343 (0.845, 3.531) | 0.3189 (−1.875, 2.513) | 1.469 (−1.634, 4.573) | 1.498 (−1.428, 4.425) |
| P-value | 0.229 | 0.776 | 0.353 | 0.316 |
| ES (s = 5.243) | 0.256 | 0.061 | 0.280 | 0.286 |
| Current pain (VAS) | ||||
| Estimate (95% CI) | 9.120 (0.521, 17.718) | 2.838 (−5.837, 11.512) | −8.534 (−20.687, 3.618) | −2.973 (−14.425, 8.480) |
| P-value | 0.038* | 0.521 | 0.169 | 0.611 |
| ESs = 18.96 | 0.481 | 0.150 | −0.450 | −0.157 |
| CRP, mg/l | ||||
| Estimate (95% CI) | −0.202 (−6.246, 5.842) | 0.905 (−5.170, 6.980) | −2.393 (−10.948, 6.162) | 0.950 (−7.182, 9.083) |
| P-value | 0.948 | 0.770 | 0.584 | 0.819 |
| ES (s = 11.74) | −0.017 | 0.077 | −0.204 | 0.081 |
| ESR, mm/h | ||||
| Estimate (95% CI) | −2.263 (−6.982, 2.456) | 2.326 (−2.383, 7.034) | −1.238 (−7.692, 5.216) | 2.781 (−3.46, −9.017) |
| P-value | 0.347 | 0.333 | 0.707 | 0.382 |
| ES (s = 14.56) | −0.155 | 0.160 | −0.085 | 0.191 |
| HAQ | ||||
| Estimate (95% CI) | 0.088 (−0.052, 0.229) | −0.017 (−0.158, 0.123) | 0.020 ( = 0.180, 0.220) | −0.012 (−0.200, 0.176) |
| P-value | 0.218 | 0.810 | 0.844 | 0.903 |
| ES (s = 0.333) | 0.264 | −0.051 | 0.060 | −0.036 |
| Patient GA | ||||
| Estimate (95% CI) | 8.102 (−0.785, 16.988) | 0.540 (−8.408, 9.487) | −8.600 (−21.215, 4.016) | 0.669 (−11.201, 12.540) |
| P-value | 0.074 | 0.906 | 0.182 | 0.912 |
| ES (s = 18.86) | 0.430 | 0.029 | −0.456 | 0.035 |
| Physician GA | ||||
| Estimate (95% CI) | 6.392 (−2.494, 15.276) | 1.298 (−7.628, 10.224) | −7.580 (−20.191, 5.032) | −3.197 (−15.058, 8.665) |
| P-value | 0.159 | 0.776 | 0.239 | 0.597 |
| ES (s = 17.56) | 0.364 | 0.074 | −0.432 | −0.182 |
| Other measures | ||||
| Positive mood | ||||
| Estimate (95% CI) | 4.041 (−0.772, 8.853) | −1.152 (−5.962, 3.657) | 3.970 (−3.802, 11.741) | 4.006 (−2.008, 10.021) |
| P-value | 0.098 | 0.631 | 0.308 | 0.186 |
| ES (s = 7.031) | 0.575 | −0.164 | 0.565 | 0.570 |
| Negative mood | ||||
| Estimate (95% CI) | −4.497 (−8.071, −0.923) | 3.385 (−0.338, 7.108) | −1.634 (−7.297, 4.028) | 2.228 (−6.536, 2.081) |
| P-value | 0.015* | 0.074 | 0.563 | 0.302 |
| ES (s = 5.024) | −0.895 | 0.674 | −0.325 | 0.443 |
| MYMOP | ||||
| Estimate (95% CI) | −0.288 (−1.011, 0.435) | 0.287 (−0.407, 0.982) | 0.248 (−0.916, 1.412) | 0.573 (−0.332, 1.478) |
| P-value | 0.424 | 0.407 | 0.668 | 0.207 |
| ES (s = 1.012) | −0.284 | 0.283 | 0.245 | 0.566 |
| Weekly pain scores (VAS) | ||||
| Estimate (95% CI) | 6.017 (0.140, 11.894) | −1.518 (−7.429, 4.394) | −5.560 (−1.413, 3.008) | −4.512 (−12.265, 3.240) |
| P-value | 0.045* | 0.615 | 0.203 | 0.254 |
| ES (s = 20.02) | 0.301 | −0.076 | −0.278 | −0.225 |
| Weekly GA | ||||
| Estimate (95% CI) | 6.260 (0.411, 12.169) | −3.820 (−9.726, 2.085) | −6.904 (−15.457, 1.648) | −10.415 (−18.163, −2.667) |
| P-value | 0.036* | 0.205 | 0.114 | 0.008* |
| ESs = 20.02 | 0.313 | −0.191 | −0.345 | −0.520 |
aAdjusted for practitioner, baseline disease severity, baseline disease activity, sex, age, duration of illness, number of medications for RA, number of other medical complaints and corresponding baseline assessments. *P > 0.05. DAS is calculated by DAS-28 = 0.56 × sqrt(tender28) + 0.28 × sqrt(swollen28) + 0.70 × ln(ESR) + 0.014 × GH.
Contrast 1: effects due to homeopathic consultation
Receiving a homeopathic consultation resulted in significant improvement over time in DAS-28 compared with no consultation [mean group difference (s.e.) 0.623 (0.223); 95% CI 0.186, 1.06; P = 0.005; ES 0.70]. In addition, receiving a homeopathic consultation was significantly associated with reduction in the number of swollen joints (group difference 3.04; 95% CI 1.055, 5.030; P = 0.003; ES 0.83) and current pain (group difference 9.12; 95% CI 0.521, 17.718; P = 0.038; ES 0.48) compared with those not receiving a consultation.
Contrasts 2–4: effects due to treatment allocation
No significant differences due to treatment were identified for any rheumatology measures for either Contrast 2, 3 or 4.
Other secondary outcomes
Longitudinal analysis adjusted for significant covariates for each contrast are reported in Table 6.
Contrast 1: effects due to consultation
Receiving a homeopathic consultation compared with no consultation significantly reduced weekly pain (group difference 6.017; 95% CI 0.140, 11.894; P = 0.045; ES = 0.30), improved patient GA (group difference 6.260; 95% CI 0.411, 12.169; P = 0.036; ES = 0.31) and negative mood (group difference −4.497; 95% CI −8.071, −0.923; P = 0.028; ES = 0.90).
Contrasts 2–4: effects due to treatment allocation
Patients receiving placebo compared with individualized homeopathy, reported significantly improved patient GA (group difference −10.415; 95% CI −18.163, −2.667; P = 0.008; ES = 0.52). No other significant effects were identified.
Adverse events
The number and type of most frequently reported adverse events recorded during the study are reported in Table 7. No significant differences were identified between treatment groups. Four serious adverse events (SAEs) all unrelated to the study medication were reported during the trial. One SAE during treatment phase related to a patient in Group 1 who experienced a fractured femur. The three SAEs during follow-up were: mild heart attack, Group 4; admission to hospital for stomach pains related to conventional rheumatological medication, Group 2; and fractured metacarpal, Group 2. Common adverse reactions reported included upper respiratory tract infections, diarrhoea and vomiting, headaches, mouth ulcers and skin rashes.
Table 7.
Adverse eventsa during treatment and follow-up per treatment groupb
| Consultation allocation | Consultation |
No consultation |
||||
|---|---|---|---|---|---|---|
| Medication-type allocation | Individualized | Complex | Placebo | Complex | Placebo | |
| Treatment group | 1 | 2 | 3 | 4 | 5 | Total |
| Total adverse eventsa, n | 72 | 55 | 58 | 60 | 37 | 282 |
| SAEs, n | 1 | 2 | 0 | 1 | 0 | 4 |
| Non-serious adverse events, n | 71 | 53 | 58 | 59 | 37 | 278 |
| Patient attribution of adverse event to study medication, n (%) | 16 (22.2) | 22 (40.0) | 15 (25.9) | 19 (48.7) | 18 (31.7) | 90 (31.9) |
aIncludes all adverse events during treatment phase. bDoes not include worsening RA.
Predictor variables
Expectations (patients, nurses and clinicians), attitude to or beliefs about CAM, coping style, sense of coherence and patient spirituality did not predict outcome for the primary variables. Patients receiving homeopathic consultation, compared with no consultation, reported significantly higher scores at the first consultation for empathy (CARE; mean difference 3.36; 95% CI 0.81, 5.92; P = 0.010; ES 0.66) and enablement (mean difference 3.56; 95% CI 2.17, 4.94; P < 0.001; ES1.27). These consultation group differences were sustained to the end of the consultation visits. Neither variable predicted changes in either primary outcomes or DAS-28.
Comment
Homeopathic intervention in patients with chronic, active but relatively stable RA has significant clinical benefits that are attributable mainly to the homeopathic consultation process. There appeared to be no specific benefit from the homeopathic remedies themselves. Although no significant group differences in either of the primary outcomes were observed, statistical and clinically relevant improvements did occur for those receiving consultations in some equally valuable and relevant secondary outcomes. The homeopathic consultation, regardless of treatment allocation, significantly improved standard objective markers of RA: DAS-28 (the EULAR equivalent of the ACR20) and swollen joint count. Minimizing disease activity reduces radiological progression and improves long-term functional outcome [34]. The ESs on objective rheumatological markers are significant and substantial (>0.70) comparable to other adjunctive conventional disease-modifying agents over similar periods of time [35, 36]. As such, these data provide robust evidence that receiving homeopathic consultations is efficacious in RA.
Under-recruitment resulted in lower patient numbers than those required based on the a priori power calculation, but post hoc analysis confirmed that sufficient patients were recruited to obtain 80% power to detect the observed and significant changes in DAS-28 between consultation and no consultation. The significant reduction in DAS-28 demonstrates proof of concept in that the homeopathic consultation appears to be the main active ingredient within homeopathy. Subjective indices such as current pain, weekly pain, weekly GA and negative mood demonstrate the same trend for improvement with homeopathic consultation, but these data need to be interpreted more cautiously because of multiple testing.
This is the first study to identify that the benefits of homeopathy are attributable to the consultation. The findings confirm previous work demonstrating that therapeutic benefits do arise from processes within the homeopathic consultation involving communication skills, empathy, hopefulness, enablement and narrative competence [16, 37, 38]. The homeopathic consultation necessitates a very detailed understanding of the patient and is a unique and personalized approach. The placebo effects of the homeopathic consultation may well be specific to this therapy possibly being dependent on the ritual of the collaborative and highly individualized consultation necessary to identify a homeopathic remedy and the associated symbolic meaning response for that patient [14]. The observed ESs ranging from 0.30 to 0.90 are larger than those observed for other non-pharmacological interventions such as cognitive behavioural therapy [39]. Our currently unpublished nested qualitative study (Brien et al., 2010, submitted for publication) exploring the patients’ experiences of the homeopathic consultation, offers further important insights consistent with the quantitative changes we report.
There were two major limitations to this study; it was underpowered for dichotomous outcomes due to under-recruitment and a slightly higher rate of attrition than anticipated (27% compared with 20%). However, it was adequately powered for continuous variables and comparisons using Contrasts 1 and 2, but not Contrasts 3 and 4, which measured single groups. The second limitation relates to the assessment of clinical activity in RA when employing adjunctive treatments. There is no gold standard for measuring clinical activity in RA [40]. Both ACR20 and DAS-28 are widely used and valid outcome measures that monitor change in disease activity. The DAS-28 has the additional advantage in that it can assess current disease activity so is commonly used in clinical practice [41]. The ACR20 is a binary outcome so is less sensitive than DAS-28 in detecting treatment differences in stable RA populations [42, 43]. The patients included in this trial were well managed conventionally; therefore, identifying a positive DAS-28 but negative ACR20 is not unexpected or unreasonable and has been reported in previous trials assessing adjunctive therapy [44]. Furthermore, the a priori power calculation was based on a trial identifying a 30% group difference between DMARD treated vs no treatment [33] but as patients in this trial received standard DMARDs, the groups are not comparable. At the time of the study’s conception, DMARDs were not in such widespread clinical use but as all the patients in this study had modified disease more modest changes would be expected in response to any adjunctive treatment. In retrospect, DAS-28 would have been the most appropriate primary outcome given the study population. Within these limitations, we consider these data to be rigorous and robust. This was a multi-centre trial and the homeopathy intervention was pragmatic reflecting normal clinical practice. Blinding was secure and no group differences in baseline characteristics were identified that could confound outcome. Finally, we identified that the study design was feasible.
The use of randomized controlled trials (RCTs) to assess the effectiveness of complex interventions has been criticized [45] as the specific and non-specific effects may not be additive, but could interact in a more complex fashion. These results suggest that we can effectively model the major components of clinical interactions and identify the clinical benefits attributable to each of them using an RCT. Further investigation is warranted to identify the ESs of the specific beneficial elements of the homeopathic consultation and investigate whether they could be employed by other clinicians to maximize patient benefit.
This trial was not designed to be definitive or prove the effectiveness of ultra-molecular medication, but to identify the relative ESs of the two most important components within homeopathy: the medication and the consultation. Given the magnitude of these effects and the lack of reported side effects, the impact of the homeopathic consultation is of clinical relevance to patients and clinicians alike. A further study, powered to identify consultation effects, is needed to confirm the benefit of homeopathic consultations in this population.
Acknowledgements
We thank the participants, the homeopaths, June Daniels and Hugh Harrison; the study nurses Julia Taylor, Alexandra Burch, Gill Horsfield, Sarah Smith, Lyndsey Goulston and Christiane Fernadez for their assistance with data collection; the rheumatologists; Brandon’s homeopathic pharmacy; the Wellcome Trust Clinical Research Facility, Southampton University Hospital Trust; Francis Treuherz, homeopath for help with technical homeopathic queries; and Professor Paul Little and Dr Selwyn Richards for reviewing the manuscript.
Contributors: S.B. contributed to the study design, study management, analysis and interpretation and led the writing of the manuscript. L.L. contributed to the study design, interpretation and writing of the manuscript. P.P. led the statistical analysis and contributed to the interpretation and the writing of the manuscript. C.McD. led the data collection and study management and contributed to the writing of the manuscript; G.L. contributed to the study design, analysis, interpretation and writing of the manuscript. All authors had full access to the data and reports. All authors agreed to submit for publication. S.B., G.L. and P.P. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: This work was supported by the National Institute of Health Research (PDA04/CAMs2/02 to S.B. and project funding), the Samueli Institute, USA (for project funding), the Southampton Complementary Medicine Research Trust (for project funding) the Rufford Maurice Laing Foundation (to G.L.), Dreluso Pharmazeutika GmBH (complex homeopathic medication); and National Health Service Fund for Science (Poole R+D Hospital Trust; for study nurse and blood tests). L.L., P.P. and C.M. received no funding for this study. The funders had no role in the study design or management, data collection, analysis and interpretation, writing of the report or the manuscript.
Disclosure statement: The authors have declared no conflicts of interest.
Footnotes
See page 1007 for the editorial comment on this article (doi:10.1093/rheumatology/keq265)
References
- 1.Hochberg MS, Spector TD. Epidemiology of rheumatoid arthritis: update. Epidemiological Rev. 1990;12:247–52. doi: 10.1093/oxfordjournals.epirev.a036058. [DOI] [PubMed] [Google Scholar]
- 2.Klareskog L, van der Heijde D, de Jager JP, et al. Therapeutic effects of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double blind randomised controlled trial. Lancet. 2004;363:675–81. doi: 10.1016/S0140-6736(04)15640-7. [DOI] [PubMed] [Google Scholar]
- 3.Witt CM, Ludtke R, Baur R, Willich SN. Homeopathic medical practice; long term results of a cohort study with 3981 patients. BMC Public Health. 2005;5:115. doi: 10.1186/1471-2458-5-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samarasekera U. Pressure grows against homoeopathy in the UK. Lancet. 2007;370:1677–8. doi: 10.1016/s0140-6736(07)61708-5. [DOI] [PubMed] [Google Scholar]
- 5.Gibson RG, Gibson S, MacNeill AD, et al. Homeopathic therapy in rheumatoid arthritis: evaluation by double-blind clinical therapeutic trial. Br J Clin Pharmacol. 1980;9:553–9. doi: 10.1111/j.1365-2125.1980.tb05840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andrade L, Ferraz MB, Atra E, et al. A randomized controlled trial to evaluate the effectiveness of homeopathy in rheumatoid arthritis. Scand J Rheumatol. 1991;20:205–8. doi: 10.3109/03009749109103022. [DOI] [PubMed] [Google Scholar]
- 7.Fisher P, Scott D. A randomised controlled trial of homeopathy in rheumatoid arthritis. Rheumatology. 2001;50:1052–5. doi: 10.1093/rheumatology/40.9.1052. [DOI] [PubMed] [Google Scholar]
- 8.Köhler T. Proof of efficacy of homeopathy against rheumatoid arthritis. A randomised double blind trial by independent doctors. Der Kassenarzt. 1991;13:48–52. [Google Scholar]
- 9.Wiesenauer M, Gaus W. Proof of efficacy of homeopathy against rheumatoid arthritis. A randomised double blind trial by independent doctors. Aktuelle Rheumatologie. 1991;16:1–9. [Google Scholar]
- 10.Linde K, Clausius N, Ramirez G, et al. Are the clinical effects of homoeopathy placebo effects? A meta-analysis of placebo-controlled trials. Lancet. 1997;350:834–43. doi: 10.1016/s0140-6736(97)02293-9. [DOI] [PubMed] [Google Scholar]
- 11.Shang A, Huwiler-Müntener, Nartey KL, et al. Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy. Lancet. 2005;366:726–32. doi: 10.1016/S0140-6736(05)67177-2. [DOI] [PubMed] [Google Scholar]
- 12.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2002;357:757. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- 13.Walach H. Placebo and placebo effects - a concise review. Focus Altern Complement Ther. 2003;8:178–87. [Google Scholar]
- 14.Moerman D, Jonas W. Deconstructing the placebo effect and finding the meaning response. Ann Intern Med. 2002;136:471–6. doi: 10.7326/0003-4819-136-6-200203190-00011. [DOI] [PubMed] [Google Scholar]
- 15.Hyland M. A tale of two therapies: psychotherapy and complementary and alternative medicine and the human effect. Clin Med. 2005;5:361–7. doi: 10.7861/clinmedicine.5-4-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mercer SW. Practitioner empathy, patient enablement and health outcomes of patients attending the Glasgow Homeopathic Hospital: a retrospective and prospective comparison. Wien Med Wochenschr. 2005;155:498–501. doi: 10.1007/s10354-005-0229-6. [DOI] [PubMed] [Google Scholar]
- 17.Burch A, Dibb B, Brien S. Understanding homeopathic decision-making: a qualitative study. Forsch Komplementärmed. 2008;15:218–25. doi: 10.1159/000138511. [DOI] [PubMed] [Google Scholar]
- 18.Dean ME, Coulter MK, Fisher P, Jobst K, Walach H. Reporting data on homeopathic treatments (RedHot): a supplement to CONSORT. Forschende Komplementärmedizin [Research in Complementary Medicine] 2006;13:368–71; Homeopathy 2007;96:42–45. J Altern Complement M. 2007;13:19–24. doi: 10.1159/000097073. [DOI] [PubMed] [Google Scholar]
- 19.Hahnemann S. In: The chronic diseases their peculiar nature and their homoeopathic cure. New Delhi, India: B Jain Publishers Ltd; 1837. Concerning the technical part of homeopathy §248 and 280. [Google Scholar]
- 20.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–55. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 21.Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38:727–35. doi: 10.1002/art.1780380602. [DOI] [PubMed] [Google Scholar]
- 22.Gotzsche P. Sensitivity of effect variables in rheumatoid arthritis: a meta-analysis of 130 placebo controlled NSAID trials. J Clin Epidemiol. 1990;43:1313–8. doi: 10.1016/0895-4356(90)90097-9. [DOI] [PubMed] [Google Scholar]
- 23.Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcome: development, scoring and evaluation of rheumatoid arthritis. J Rheumatol. 1993;20:561–5. [PubMed] [Google Scholar]
- 24.van Gestel AM, Prevoo ML, van’t Hof MA, van Rijswijk MH, van de Putte LB, van Riel PL. Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism Criteria. Arthritis Rheum. 1996;39:34–40. doi: 10.1002/art.1780390105. [DOI] [PubMed] [Google Scholar]
- 25.van Gestel AM, Anderson JJ, van Riel PL, et al. ACR and EULAR improvement criteria have comparable validity in rheumatoid arthritis trials American College of Rheumatology European League of Associations for Rheumatology. J Rheumatol. 1999;26:705–11. [PubMed] [Google Scholar]
- 26.Paterson C. Measuring outcome in primary care: a patient-generated measure, MYMOP, compared to the SF-36 health survey. Br Med J. 1996;312:1016–20. doi: 10.1136/bmj.312.7037.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Person Soc Psych. 1988;55:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 28.Schumann A, Hapke U, Meyer C, Rumpf HJ, John U. Measuring sense of coherence with only three items: a useful tool for population surveys. Br J Health Psych. 2003;8:409–21. doi: 10.1348/135910703770238275. [DOI] [PubMed] [Google Scholar]
- 29.Hatch RL, Naberhaus DS, Halmich LK, Burg MA. Spiritual involvement and beliefs scale: development and testing of a new instrument. J Fam Pract. 1998;46:476–86. [PubMed] [Google Scholar]
- 30.Bishop F, Yardley L, Lewith G. Developing a measure of treatment beliefs: the complementary and alternative medicine beliefs inventory. Complement Ther Med. 2005;2:144–9. doi: 10.1016/j.ctim.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Mercer SW, Maxwell M, Heaney D, Watt G. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21:699–705. doi: 10.1093/fampra/cmh621. [DOI] [PubMed] [Google Scholar]
- 32.Howie JGR, Heaney DJ, Maxwell M, Walker JJ, Freeman GK, Rai H. Quality at general practice consultations: cross sectional survey. Br Med J. 1999;319:738–53. doi: 10.1136/bmj.319.7212.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strand V, Cohen S, Schiff M, et al. Treatment of rheumatoid arthritis with leflunomide compared with placebo. Arch Int Med. 1999;159:2542–50. doi: 10.1001/archinte.159.21.2542. [DOI] [PubMed] [Google Scholar]
- 34.Fries JF, Williams CA, Morfeld D, Singh G, Sibley J. Reduction of long-term disability in patients with rheumatoid arthritis by disease-modifying antirheumatic drug-based treatment strategies. Arthritis Rheum. 1996;39:616–22. doi: 10.1002/art.1780390412. [DOI] [PubMed] [Google Scholar]
- 35.McCarey DW, McInnes PB, Madhok R, et al. Trial of atorvastatin in rheumatoid arthritis (TARA): double-blind, randomised placebo-controlled trial. Lancet. 2004;363:2015–21. doi: 10.1016/S0140-6736(04)16449-0. [DOI] [PubMed] [Google Scholar]
- 36.van Vollenhoven RF, Ernestam S, Harju A, Bratt J, Klareskog L. Etanercept versus etanercept plus methotrexate: a registry-based study suggesting that the combination is clinically more efficacious. Arthritis Res Ther. 2003;5:R347–51. doi: 10.1186/ar1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hartog C. Elements of effective communication – rediscoveries from homeopathy. Patient Educ Counc. 2009;77:172–8. doi: 10.1016/j.pec.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 38.Thompson T, Weiss M. Homeopathy - what are the active ingredients? An exploratory study using the UK Medical Research Council's framework for the evaluation of complex interventions. BMC Complement Altern Med. 2006;6:37. doi: 10.1186/1472-6882-6-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Astin JA, Beckner W, Soeken K, Hochberg MC, Berman B. Psychological interventions for rheumatoid arthritis: a meta-analysis of randomized controlled trials. Arthritis Rheum. 2002;47:291–302. doi: 10.1002/art.10416. [DOI] [PubMed] [Google Scholar]
- 40.Pincus T, Sokka T. Quantitative measures for assessing rheumatoid arthritis in clinical trials and clinical care. Best Pract Res Clin Rheumatol. 2003;17:753–81. doi: 10.1016/s1521-6942(03)00077-9. [DOI] [PubMed] [Google Scholar]
- 41.van Riel PL, Schumacher HR., Jr How does one assess early rheumatoid arthritis in daily clinical practice? Best Pract Res Clin Rheumatol. 2001;15:67–76. doi: 10.1053/berh.2000.0126. [DOI] [PubMed] [Google Scholar]
- 42.Pincus T, Amara I, Koch GG. Continuous indices of core data set measures in rheumatoid arthritis clinical trials. Lower responses to placebo than seen with categorical response with the American College of Rheumatology 20% criteria. Arthritis Rheum. 2005;52:1031–6. doi: 10.1002/art.20995. [DOI] [PubMed] [Google Scholar]
- 43.Felson DT, Zhang B, Siegal JN. Trials in rheumatoid arthritis: choosing the right outcome measure when minimal disease is achievable. Ann Rheum Dis. 2008;67:580–3. doi: 10.1136/ard.2007.079632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zanette SD, Born IG, Brenol JC, Xavier RM. A pilot study of acupuncture as adjunctive treatment of rheumatoid arthritis. Clin Rheumatol. 2008;27:627–35. doi: 10.1007/s10067-007-0759-y. [DOI] [PubMed] [Google Scholar]
- 45.Weatherley-Jones E, Thompson EA, Thomas KJ. The placebo-controlled trial as a test of complementary and alternative medicine: observations from research experience of individualised homeopathic treatment. Homeopathy. 2004;93:186–9. doi: 10.1016/j.homp.2004.06.002. [DOI] [PubMed] [Google Scholar]