Abstract
Background
Osteoporosis is highly prevalent in the nursing home (NH) populations but medications that increase bone mineral density are used infrequently. Prior research finds few patient characteristics predict treatment. NH characteristics have been associated with prescription of some medications. We examined associations of NH-level characteristics with osteoporosis treatment in elderly patients admitted to a NH after a fracture.
Method
We conducted a cohort study of patients with hip, wrist and humeral fractures admitted to a NH in NJ. They were followed for 12 months from 1999–2004. Possible NH-level predictors of receiving osteoporosis treatment were assessed in mixed multivariable models to account for clustering within individual NHs.
Results
Of the 2,838 post-fracture patients identified from 180 NH’s, 156 (5.5%) were prescribed an osteoporosis medication. There was wide variation in treatment between individual NHs (0–40%), which was substantially reduced after adjusting for patient case-mix. Several patient characteristics did associate with osteoporosis treatment -- female gender (odds ratio (OR) 2.56, 95% confidence interval (CI) 1.42, 4.61), younger age per year (OR 0.98 95%CI 0.96, 0.99), white race (OR 2.37 95%CI 1.23, 4.56) and prior history of fracture (OR 4.41 95%CI 1.04, 18.73). However no NH characteristics significantly associate with treatment (profit status, NH chain member, occupancy rate, and bed size).
Conclusion
NH characteristics did not predict pharmacological treatment of osteoporosis. Further studies of osteoporosis prescribing in NHs need to consider other types of variables as possible correlates of prescribing.
Keywords: osteoporosis, nursing home, pharmacological treatment
1. INTRODUCTION
Osteoporosis is widespread in nursing home (NH) populations with a prevalence of 80% in some cohort studies. Fracture prevention is a critical issue, with the incidence of fracture increased from 5 to 11 times compared to age-matched community dwelling elderly patients. Furthermore, hip and other osteoporosis fractures increase the risk of subsequent fractures in NH patients. NH patients who sustain fractures have increased healthcare utilization, even 12 months after the fracture. Strategies for fracture prevention have largely focused on fall prevention, however the impact on fracture reduction is unclear. Low bone mineral density (BMD) is a significant predictor of fracture in NH patients. Widely available medications improve BMD, with some evidence of effectiveness in NH residents. Despite the relative safety of these medications they are poorly utilized in this population.
In prior work, we examined patient-level predictors of prescribing osteoporosis medications in patients admitted to a NH after a fracture. We found few characteristics predicted receipt of an osteoporosis medication, suggesting possible variation at the level of the NH. Organizational characteristics of nursing homes have long been shown to influence resident outcome in many domains such as physical restraints, vaccination, staff turn over, and feeding tube use. Organizational characteristics have also been associated with medication utilization. Anti-psychotic medication use has been linked to larger NHs and those with reduced resources, as is the case with the use of long-acting benzodiazepines. Anti-depressant use has also been shown to be associated with larger NHs and in those that employed full time physicians.
Only one prior study has examined the influence of NH characteristics on the prescription of osteoporosis medications, reporting non-urban/surburban location and female gender were associated with treatment. We conducted a cohort study using previously collected data to determine the correlation between organizational NH characteristics and prescribing for osteoporosis in patients admitted to a NH after fracture.
2. METHOD
2.1 Study Population
The study cohort was identified from individuals enrolled in New Jersey Medicaid and Pharmaceutical Assistance for the Aged and Disabled programs (PAAD) from 1999 thru 2004. The PAAD program is a state specific drug benefit program for elderly and disabled citizens. Most beneficiaries are aged over 65 years. There is no deductible or maximum cost; however there is a $2 co-payment per prescription. The New Jersey Medicaid program has no maximum benefit, no deductible, nor co-payment and there were no restrictions on prescribing during the study period from either program.
We examined a database of all beneficiaries of PAAD who also have concurrent Medicaid eligibility. Subjects who sustained a hip, wrist or humeral fracture and were then admitted to a NH within 30 days after discharge from an acute care facility were potentially eligible for the study cohort. This method has been used in our prior work. Fractures were identified using diagnosis codes from the International Classification of Diseases Ninth Revision (ICD-9) combined with procedural codes using a previously validated algorithm. We required patients to be in the NH for at least 30 days. Patients also were required to have a minimum of 1 prescription filled per month for the 12-month period.
Patients were excluded if they did not fill any prescription or have a Medicare claim in the two 6 month periods preceding the index fracture to ensure uniform medication eligibility during which co-variate assessment occurred. Finally patients were eliminated from the cohort if they could not be linked to an identified NH or were in NH’s with <10 fracture patients. This allowed a large enough sample to make valid inferences about individual NHs as performed previously in a similar paper. Patients with prior use of an osteoporosis medication were also eliminated to understand the relationship of new prescribing for osteoporosis independent of prior use. Patients were followed for a 12-month period after NH entry until one of the following occurred: prescription filled for osteoporosis, death, discharge from NH or end of the study period.
2.2 Predictors of Treatment
Patient covariate assessment occurred 12 months preceding the index fracture. A modified Charlson co-morbidity index score was calculated from diagnostic information from the International Classification of Diseases Ninth Revision. We created variables by reviewing specific codes and combining them with filled prescriptions during the previous 12 months. These included a history of falls, dementia, osteoporosis, prior oral glucocorticoid use, and prior BMD exam.
NH characteristics were obtained from the On-line Survey and Certification Report (OSCAR) database and the Minimum Data Set (MDS) repository from 2003. Examples of the available information from this database includes Medicare identification number for each facility, staffing information, number of certified beds and whether the NH was a member of chain. Because our cohort was collected over a 6 year period we only used those variables with minimal variation over time. Nursing home covariates examined were bed size, occupancy rate, profit status, and chain status.
2.3 Statistical Analysis
The dependent variable was receipt of any osteoporosis medication. Medications included as osteoporosis treatments were all bisphosphonates (intravenous and oral), raloxifene, teriparatide, calcitonin and non vaginal hormone replacement therapy. Individual medications were not differentiated. Calcium and vitamin D utilization information was not available in the pharmacy claims database.
The proportion of treated patients per NH was examined. We then calculated the mean proportion and the 95% confidence interval for each of the individual nursing homes. These proportions were adjusted for patient characteristics.
Patient and NH characteristics were assessed as potential predictors of receipt of medication. We used non linear mixed effect models including both patient and NH characteristics as fixed and random effects of the NH, accounting for clustering of patients within NH’s. We compared models using the cross validated estimate of R2. This approach has been used previously to measure the variability explained by clinic and physician factors in clustered data. Analyses were performed using R Statistical Software version 2.7.0 (R foundation for Statistical Computing Vienna Austria) and SAS version 9.1 software (SAS Institute Inc, Cary, North Carolina).
3. RESULTS
3.1 Study Population and NH Characteristics
Of the 2,838 NH residents in 180 NH identified, 84% were female and the mean age was 83.7 years with 84% female. Most (94%) were hip fractures. Over 60% of the cohort had a history of prior fracture, or fall and 60.9% had dementia. Only 5.5% (n=156) received any osteoporosis medication during the 12-months after fracture across the 6 year study period. Table 1 displays the patient characteristics.
Table 1.
Characteristics of Study Population
| Characteristic | Number of Patients (%) n=2838 |
|---|---|
| Mean Age, (years) (±SD) | 83.7 (9.6) |
| Female | 2375 (83.7) |
| White | 2438 (87.5) |
| PAAD¶ | 334 (11.8) |
| Length of NH* stay, (in days) | 237.5 [74,364] |
| Hip Fracture | 2671 (94.1) |
| Prior BMD Exam† | 17 (0.60) |
| Prior Fall | 1845 (65.0) |
| Prior Fracture | 2341 (82.5) |
| Dementia | 1728 (60.9) |
| Osteoporosis | 20 (0.7) |
| PUD/GERD§ | 529 (18.6) |
| Glucocorticoids | 193 (6.8) |
NH denotes nursing home
BMD denotes bone mineral density
Peptic Ulcer Disease/ Gastroesophageal Reflex Disease
Pharmaceutical Assistance for the Aged and Disabled
Table 2 shows the characteristics of the study NHs as compared with all other NH’s in the state. Of the NHs included in the study, 69% were for profit homes while only 31% were part of a chain. Almost 90% had a high occupancy rate as well. The study NHs were reflective of overall state NH characteristics. The median number of patients per NH included in our study was 15 (inter-quartile range 11–45)
Table 2.
Characteristics of study NHs as compared with non-study NH in NJ
| Nursing Home Characteristic | Study Nursing Homes n=180 (%) | NJ Nursing Homes n=143 (%) | p value |
|---|---|---|---|
| Certified Number of Beds* | |||
| 1–100 | 5 (2.7) | 59 (42.5) | <.0001 |
| 101–300 | 167(92.7) | 77 (55.4) | |
| ≥301 | 8 (4.4) | 3 (2.2) | |
| %Occupied Beds* | |||
| 1–80 | 20 (11.1) | 18 (13.5) | |
| ≥80 | 160 (88.9) | 115 (86.5) | 0.52 |
| Chain | |||
| Yes | 56 (31.1) | 57 (39.9) | |
| No | 124 (68.9) | 86 (60.1) | 0.10 |
| Ownership Status | |||
| Owner for profit | 125 (69.4) | 95 (66.4) | |
| Government/ Not for Profit | 55 (30.6) | 48 (33.6) | 0.56 |
Missing certified bed data for 4 non-study NHs and missing occupied beds data for 10 non-study NHs.
3.2 Predictors of Treatment
We examined several multilevel models: a model with patient characteristics alone, patient characteristics combined with a random effect for NH, and then finally patient and NH characteristics with a random effect for NH. Results from these models did not dramatically improve with additional covariates. Table 3 shows the model accounting for fixed patient and NH effects with a random effect for the individual nursing home.
Table 3.
Patient and NH Characteristics Associated With Receipt of Osteoporosis Medications.
| Variable | Adjusted OR (95%Confidence Interval) |
|---|---|
| Patient Characteristic | |
| Demographics | |
| Age | 0.98 (.96, 0.99) |
| Female | 2.56 (1.42, 4.61) |
| White | 2.37 (1.23, 4.56) |
| PAAD (reference Medicaid) | 0.84 (0.49, 1.47) |
| Co-morbidities | |
| Prior diagnosis of Osteoporosis | 0.89 (0.11, 7.03) |
| Prior Glucocorticoid Use | 1.48 (0.82, 2.66) |
| Prior GERD/H2 blocker | 1.33 (0.89, 2.00) |
| Prior Fracture | 4.41 (1.04, 18.73) |
| Prior Fall | 1.00 (0.69, 1.44) |
| Dementia | 0.99 (0.70,1.42) |
| Modified Charlson Co-morbidity Index | 0.98 (0.65, 1.34) |
| NH Characteristic | |
| Bed Size | |
| 1–100 | 1.00 |
| 101–300 | 1.40 (0.30, 6.58) |
| ≥301 | 1.81 (0.34, 9.63) |
| Chain | |
| Yes | 1.00 |
| No | 0.82 (0.53, 1.26) |
| Ownership Status | |
| Government/Non-Profit | 1.00 |
| For Profit | 1.24 (0.81, 1.88) |
| Occupancy Rate | |
| 1–80% | 0.83 (0.47, 1.46) |
| >80% | 1.00 |
Multilevel models (see Table 3) indicated several patient-level variables were significant predictors of osteoporosis treatment: female gender (odds ratio (OR) 2.56 95% Confidence Interval (CI) 1.42, 4.61), younger age, per year (OR 0.98 95%CI 0.96, 0.99), white race (OR 2.37 95%CI 1.23, 4.56) and a history of prior fracture (OR 4.41 95%CI 1.04, 18.73). No NH-level characteristics correlated with osteoporosis treatment. Larger size NHs seemed to be more likely to treat patients; however bed size was not a statistically significant predictor of osteoporosis treatment.
3.3 Treatment Variation Between Nursing Homes
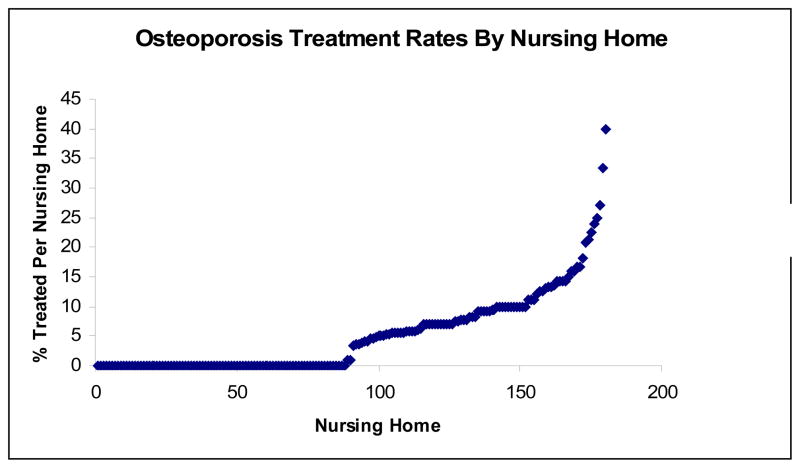
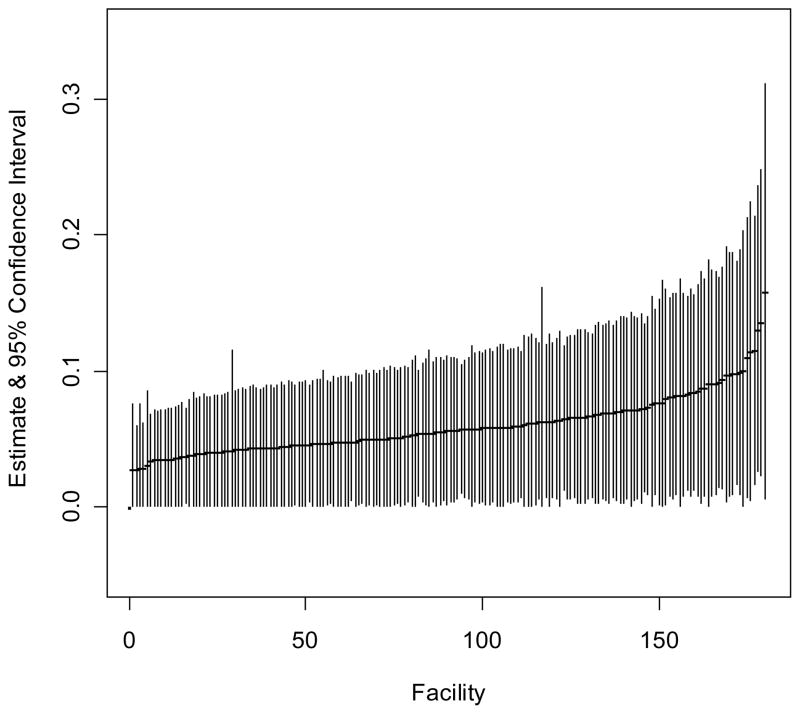
There was significant variation in treatment rates ranging 0 to 40%. Figure 1 displays the distribution of treatment rates per NH. We then adjusted each NH for patient case mix using covariates previously described. Figure 2 displays the median predicted probability and 95% confidence interval for the “average patient” of receiving an osteoporosis medication in each NH. The estimates were additionally adjusted for facility specific characteristics described in table 2. The overlapping confidence intervals indicate no statistically significant difference in the predicted probability of receiving an osteoporosis medication between NH facilities.
Figure 1.
Each point represents a NH and they are ordered according to the rate of treatment.
Figure 2.
Each point represents the predicted probability of receiving osteoporosis medication by individual NH. The predicted probability was estimated for the average nursing home patient with the following characteristics: age 86, female, white, Charlson Score=3, no prior steroids, no previous peptic ulcer gastro-esophageal reflux disease or osteoporosis, has prior fracture, falls, and dementia, no prior BMD test, on Medicaid. Each NH may vary with respect to number of beds, ownership, neighborhood, occupancy, and for profit status.
4. DISCUSSION
We conducted a cohort study of 2,838 elderly patient with recent fractures admitted to a total of 180 individual nursing homes and found only 5.5% of all subjects received an osteoporosis medication within a 12 month period. In prior work we found few significant patient-level predictors of receipt of medication. Only female gender and prior use of osteoporosis medication were associated with prescription of osteoporosis medication. In this cohort, prior history of fracture, female sex and younger age were significant patient level characteristics predictive of receipt of medication. Bed size, profit status, chain status and the occupancy rate did not significantly predict osteoporosis treatment. There was a wide variation between individual homes with rates of treatment ranging from 0 to 40% despite few predictive factors. Although when patient mix was adjusted for, the probability of receiving treatment did not vary significantly between NHs.
Prior studies, report a strong association between gender and osteoporosis treatment. Other studies have also reported racial disparities in osteoporosis care and younger patients with prior fractures are more likely to be treated. Few studies examined the influence of facility characteristics on osteoporosis prescribing however. One prior study examining 867 patients in 67 NH found a level of treatment variation from 0 to 85%. They found urban location was associated with treatment. The outcome however was inclusive of calcium, vitamin D and hip protectors. It is surprising in our study examining a larger cohort and greater number of facilities that the variation between nursing homes was reduced when adjusting for patient characteristics.
Variation in NH care has been demonstrated in a number of diverse areas, encompassing end of life care and advance care planning, staff turnover and pressure ulcer care. Practices in medication prescribing also vary, the emphasis however has been psychotropic medications due to governmental and public pressure coupled with intrinsic vulnerability of the institutionalized elderly. Little is known about variation in prescribing for secondary prevention of fractures. Prescribing for osteoporosis has been known to vary in a number of settings including community practices, and hospital settings. In addition treatment varies among populations with different secondary causes of osteoporosis. Variation has been explained in part by physician differences such as specialty training, and larger patient volume. While our study adjusted for patient case mix we did not examine physician characteristics or nursing staff levels which may play a role in the large variation we see within facility.
Prescribing in nursing homes is complex, with patient functionality, goals of care, family dynamics and patient wishes considered. Furthermore, there are regulatory standards, performance measures and state oversight which may influence care. Physicians practicing in this vulnerable population are subject to scrutiny, however NH patients at high risk of future fractures should be given consideration for osteoporosis treatment beyond calcium and vitamin D. Prescription of widely available osteoporosis medication remains low with little explanation by patient characteristics or NH organizational characteristics. Interventions to improve to treatment in the NH environment have been largely unsuccessful. This is reflective of a need for a deeper understanding of the prescribing culture surrounding osteoporosis allowing for more effective interventions to be designed. The influence of physician characteristics, regulatory oversight and perhaps performance measures need to be studied.
There were several limitations in this study. Our study only included 55% of all NH’s in one state, as a result of stringent selection criteria and data sources, the results may not be truly representative. However the characteristics of the study NHs as compared to all NHs in the state were similar, limiting this possibility. We only examined organizational characteristics with minimal variation over time. More dynamic features such as staffing level and staffing ratios may be of interest in the future, especially as specific directions need to be followed for some medications (oral bisphosphonates) necessitating close patient observation. However bisphosphonate side effects were not perceived as barriers for treatment in a small survey of medical and nursing directors. We did not have vitamin D or calcium use data which is an important and well tolerated treatment in this population, nor did we have functional data specifically nutritional, cognitive, mobility status, which may influence fracture risk and thus treatment. Finally the study was conducted retrospectively based on data collected for insurance payment purposes. Thus, our analyses were confined to a limited number of potential predictors.
The rate of prescribing for osteoporosis remains low in this high risk population. Organizational NH-level characteristics do not predict treatment. Thus, targeting NHs for improvement may require identifying a NH based on its prior prescribing rates. Alternatively, quality measures for NHs may be useful to identify poor performers. If quality improvement measures are to be successful, a better understanding is required to understand the complexities that surround recognition and treatment of osteoporosis. While treatment may not be appropriate for all, there is probably under-utilization and under-treatment of this endemic disease. Further research is needed to understand prescribing, the role of physicians and regulatory oversight.
Footnotes
Conflict of Interest: Dr Parikh was supported T32 AG023480-05 through Harvard Medical School/Division of Gerontology. Beth Israel Deaconess Medical Center, Boston during writing of this manuscript. Dr Solomon is supported by K24 AR055989. The sponsor had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
M. Alan Brookhart, Email: abrookhart@partners.org.
Margaret Stedman, Email: mstedman2@partners.org.
Jerry Avorn, Email: javorn@partners.org.
Helen Mogun, Email: mogun@boss.bwh.harvard.edu.
Daniel H Solomon, Email: dsolomon@partners.org.
References
- 1.Zimmerman SI, Girman CJ, Buie VC, Chandler J, Hawkes W, Martin A, Holder L, Hebel JR, Sloane PD, Magaziner J. The prevalence of osteoporosis in nursing home residents. Osteoporos Int. 1999;9:151–7. doi: 10.1007/s001980050129. [DOI] [PubMed] [Google Scholar]
- 2.Cali CM, Kiel DP. An epidemiologic study of fall-related fractures among institutionalized older people. J Am Geriatr Soc. 1995;43:1336–40. doi: 10.1111/j.1532-5415.1995.tb06610.x. [DOI] [PubMed] [Google Scholar]
- 3.Rudman IW, Rudman D. High rate of fractures for men in nursing homes. Am J Phys Med Rehabil. 1989;68:2–5. doi: 10.1097/00002060-198902000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Lyles KW, Schenck AP, Colon-Emeric CS. Hip and other osteoporotic fractures increase the risk of subsequent fractures in nursing home residents. Osteoporos Int. 2008;19:1225–33. doi: 10.1007/s00198-008-0569-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmerman S, Chandler JM, Hawkes W, Sloane PD, Hebel JR, Magaziner J, Martin AR, Girman CJ. Effect of fracture on the health care use of nursing home residents. Arch Intern Med. 2002;162:1502–8. doi: 10.1001/archinte.162.13.1502. [DOI] [PubMed] [Google Scholar]
- 6.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003:CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 7.Chandler JM, Zimmerman SI, Girman CJ, Martin AR, Hawkes W, Hebel JR, Sloane PD, Holder L, Magaziner J. Low bone mineral density and risk of fracture in white female nursing home residents. Jama. 2000;284:972–7. doi: 10.1001/jama.284.8.972. [DOI] [PubMed] [Google Scholar]
- 8.Greenspan SL, Schneider DL, McClung MR, Miller PD, Schnitzer TJ, Bonin R, Smith ME, DeLucca P, Gormley GJ, Melton ME. Alendronate improves bone mineral density in elderly women with osteoporosis residing in long-term care facilities. A mkrandomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002;136:742–6. doi: 10.7326/0003-4819-136-10-200205210-00009. [DOI] [PubMed] [Google Scholar]
- 9.Boonen S, McClung MR, Eastell R, El-Hajj Fuleihan G, Barton IP, Delmas P. Safety and efficacy of risedronate in reducing fracture risk in osteoporotic women aged 80 and older: implications for the use of antiresorptive agents in the old and oldest old. J Am Geriatr Soc. 2004;52:1832–9. doi: 10.1111/j.1532-5415.2004.52506.x. [DOI] [PubMed] [Google Scholar]
- 10.Parikh S, Mogun H, Avorn J, Solomon DH. Osteoporosis medication use in nursing home patients with fractures in 1 US state. Arch Intern Med. 2008;168:1111–5. doi: 10.1001/archinte.168.10.1111. [DOI] [PubMed] [Google Scholar]
- 11.Jachna CM, Shireman TI, Whittle J, Ellerbeck EF, Rigler SK. Differing patterns of antiresorptive pharmacotherapy in nursing facility residents and community dwellers. J Am Geriatr Soc. 2005;53:1275–81. doi: 10.1111/j.1532-5415.2005.53401.x. [DOI] [PubMed] [Google Scholar]
- 12.Phillips CD, Hawes C, Mor V, Fries BE, Morris JN, Nennstiel ME. Facility and area variation affecting the use of physical restraints in nursing homes. Med Care. 1996;34:1149–62. doi: 10.1097/00005650-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Castle NG. Differences in nursing homes with increasing and decreasing use of physical restraints. Med Care. 2000;38:1154–63. doi: 10.1097/00005650-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Bardenheier B, Shefer A, McKibben L, Roberts H, Bratzler D. Characteristics of long-term-care facility residents associated with receipt of influenza and pneumococcal vaccinations. Infect Control Hosp Epidemiol. 2004;25:946–54. doi: 10.1086/502325. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell SL, Teno JM, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. Jama. 2003;290:73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 16.Ruths S, Straand J, Nygaard HA. Psychotropic drug use in nursing homes--diagnostic indications and variations between institutions. Eur J Clin Pharmacol. 2001;57:523–8. doi: 10.1007/s002280100348. [DOI] [PubMed] [Google Scholar]
- 17.Sorensen L, Foldspang A, Gulmann NC, Munk-Jorgensen P. Determinants for the use of psychotropics among nursing home residents. Int J Geriatr Psychiatry. 2001;16:147–54. doi: 10.1002/1099-1166(200102)16:2<147::aid-gps286>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 18.Hughes CM, Lapane KL, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing homes. Med Care. 2000;38:1164–73. doi: 10.1097/00005650-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Svarstad BL, Mount JK. Chronic benzodiazepine use in nursing homes: effects of federal guidelines, resident mix, and nurse staffing. J Am Geriatr Soc. 2001;49:1673–8. doi: 10.1046/j.1532-5415.2001.t01-1-49278.x. [DOI] [PubMed] [Google Scholar]
- 20.Lapane KL, Hughes CM. Which organizational characteristics are associated with increased management of depression using antidepressants in US nursing homes? Med Care. 2004;42:992–1000. doi: 10.1097/00005650-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Colon-Emeric C, Lyles KW, Levine DA, House P, Schenck A, Gorospe J, Fermazin M, Oliver K, Alison J, Weisman N, Xie A, Curtis JR, Saag K. Prevalence and predictors of osteoporosis treatment in nursing home residents with known osteoporosis or recent fracture. Osteoporos Int. 2006 doi: 10.1007/s00198-006-0260-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ray WA, Griffin MR, Fought RL, Adams ML. Identification of fractures from computerized Medicare files. J Clin Epidemiol. 1992;45:703–14. doi: 10.1016/0895-4356(92)90047-q. [DOI] [PubMed] [Google Scholar]
- 23.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 24.Brookhart MA, Solomon DH, Wang P, Glynn RJ, Avorn J, Schneeweiss S. Explained variation in a model of therapeutic decision making is partitioned across patient, physician, and clinic factors. J Clin Epidemiol. 2006;59:18–25. doi: 10.1016/j.jclinepi.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Solomon DH, Brookhart MA, Gandhi TK, Karson A, Gharib S, Orav EJ, Shaykevich S, Licari A, Cabral D, Bates DW. Adherence with osteoporosis practice guidelines: a multilevel analysis of patient, physician, and practice setting characteristics. Am J Med. 2004;117:919–24. doi: 10.1016/j.amjmed.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 26.Alam NM, Archer JA, Lee E. Osteoporotic fragility fractures in African Americans: under-recognized and undertreated. J Natl Med Assoc. 2004;96:1640–5. [PMC free article] [PubMed] [Google Scholar]
- 27.Block AE, Solomon DH, Cadarette SM, Mogun H, Choudhry NK. Patient and physician predictors of post-fracture osteoporosis management. J Gen Intern Med. 2008;23:1447–51. doi: 10.1007/s11606-008-0697-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colon-Emeric C, Lyles KW, Levine DA, House P, Schenck A, Gorospe J, Fermazin M, Oliver K, Alison J, Weisman N, Xie A, Curtis JR, Saag K. Prevalence and predictors of osteoporosis treatment in nursing home residents with known osteoporosis or recent fracture. Osteoporos Int. 2007;18:553–9. doi: 10.1007/s00198-006-0260-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mor V, Papandonatos G, Miller SC. End-of-life hospitalization for African American and non-Latino white nursing home residents: variation by race and a facility’s racial composition. J Palliat Med. 2005;8:58–68. doi: 10.1089/jpm.2005.8.58. [DOI] [PubMed] [Google Scholar]
- 30.Castle NG, Mor V. Advance care planning in nursing homes: pre- and post- Patient Self-Determination Act. Health Serv Res. 1998;33:101–24. [PMC free article] [PubMed] [Google Scholar]
- 31.Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. Gerontologist. 2006;46:62–73. doi: 10.1093/geront/46.1.62. [DOI] [PubMed] [Google Scholar]
- 32.Rudman D, Slater EJ, Richardson TJ, Mattson DE. The occurrence of pressure ulcers in three nursing homes. J Gen Intern Med. 1993;8:653–8. doi: 10.1007/BF02598281. [DOI] [PubMed] [Google Scholar]
- 33.Saadi H, Litaker D, Mills W, Kippes C, Richmond B, Licata A. Practice variation in the diagnosis and treatment of osteoporosis: a case for more effective physician education in primary care. J Womens Health Gend Based Med. 1999;8:767–71. doi: 10.1089/152460999319093. [DOI] [PubMed] [Google Scholar]
- 34.Mudano A, Allison J, Hill J, Rothermel T, Saag K. Variations in glucocorticoid induced osteoporosis prevention in a managed care cohort. J Rheumatol. 2001;28:1298–305. [PubMed] [Google Scholar]
- 35.Peat ID, Healy S, Reid DM, Ralston SH. Steroid induced osteoporosis: an opportunity for prevention? Ann Rheum Dis. 1995;54:66–8. doi: 10.1136/ard.54.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hughes CM, Lapane K, Watson MC, Davies HT. Does organisational culture influence prescribing in care homes for older people? A new direction for research. Drugs Aging. 2007;24:81–93. doi: 10.2165/00002512-200724020-00001. [DOI] [PubMed] [Google Scholar]
- 37.Duque G, Mallet L, Roberts A, Gingrass S, Kremer R, Sainte-Marie LG, Kiel DP. To treat or not to treat, that is the question: proceedings of the Quebec symposium for the treatment of osteoporosis in long-term care institutions, Saint-Hyacinthe, Quebec, November 5, 2004. J Am Med Dir Assoc. 2007;8:e67–73. doi: 10.1016/j.jamda.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 38.Colon-Emeric CS, Lyles KW, House P, Levine DA, Schenck AP, Allison J, Gorospe J, Fermazin M, Oliver K, Curtis JR, Weissman N, Xie A, Saag KG. Randomized trial to improve fracture prevention in nursing home residents. Am J Med. 2007;120:886–92. doi: 10.1016/j.amjmed.2007.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colon-Emeric CS, Casebeer L, Saag K, Allison J, Levine D, Suh TT, Lyles KW. Barriers to providing osteoporosis care in skilled nursing facilities: perceptions of medical directors and directors of nursing. J Am Med Dir Assoc. 2004;5:361–6. doi: 10.1097/01.JAM.0000141950.34986.EE. [DOI] [PubMed] [Google Scholar]