Abstract
Objective
The goal of this work was to evaluate a possible improvement in ultrasound coverage for a dual-modality breast imaging system in the mammographic geometry.
Methods
A pilot study was performed to evaluate use of a rubber dam to retain ultrasound gel and improve imaging coverage at the breast periphery on a combined imaging system consisting of an ultrasound scanner and a digital x-ray tomosynthesis unit. Several dams were constructed to encompass the shapes of various sizes of compressed breasts. Visual tracings of the breast-to-paddle contact area and breast periphery were made for 8 breasts to estimate coverage area. Two readers independently reviewed the resulting images and were asked to rate overall breast image quality.
Results
The percentages of breast in contact with the paddle were larger (P <0.01) and the linear dimensions of breast in contact with the paddle were bigger (P <0.05) using the rubber dam than without it. With the dam the mean estimated area of the breast in contact with the paddle increased 14%, while the mean increase in the fraction of the total breast area in contact with paddle was 30%. The difference was due to the mean total projected area of the breast decreasing 12% as the dam was pressed against it. The image quality of automated ultrasound with the rubber dam was consistently judged to be superior to that without the dam.
Conclusions
This method can enhance the absolute and percentage area of the breast in contact with the paddle, reducing noncontact gaps at the breast periphery. Gently pressing the breast periphery with the dam inserted toward the chest wall improves coverage in automated breast ultrasound scanning.
Keywords: Breast cancer screening, Multimodality, Automated ultrasound, 3-D imaging
Introduction
Ultrasound has been found to be a valuable adjunct to mammography in the characterization of breast lesions.1,2 However, conventional ultrasound imaging is performed freehand in a different geometry than mammography, which can make it difficult to correlate lesions between the two modalities. Studies have shown that at least 10% of the time, lesions found in the ultrasound images do not correspond with those in the mammograms.3 False positives are a particular problem when searching for secondary masses and for detection in high risk or screening populations. 4,5
A combined X-ray/ultrasound system addresses these problems by first taking a 3-dimensional (3D) digital x-ray image (tomosynthesis) of a compressed breast, then scanning a high frequency (9 to 12 MHz) ultrasonic transducer across a special dual-modality compression paddle while the breast is still under compression. This creates coregistered 3D X-ray and 3D ultrasound images in the same imaging geometry.6,7 Dual-mode whole-breast imaging also exhibits significant potential for advanced X-ray and ultrasound modes which would provide additional information about breast tissues that is not available from conventional ultrasound and mammography. For example, in its current configuration, X-ray Digital Breast Tomosynthesis (DBT) replaces single projection digital mammography in the combined system for 3D delineation of tissue structures and better correlation with the 3D ultrasound.8 Initial results of the fusion of pulse echo Automated Breast Ultrasound (ABU) and of DBT are promising, although there remain technical issues of breast coverage and some acoustic coupling artifacts in the ABU. 8, 9
A major source of the coverage problems in performing automated ultrasound scans in a dual-modality system is that there can be an appreciable air gap between the compression paddle and the breast surface near the breast periphery.8, 10, 11 In our previous work, we employed a viscous gel that was manually distributed with a syringe at the breast periphery to address the air gap problem.8 In most of our patient studies where needed, we also taped a thin strip of plastic film around the breast periphery to act as a dam to keep the viscous gel in place. However, the effects of these dams were not quantified nor reported. The dams employed in the present study are made of butyl rubber to provide an absorptive, minimally reflecting surface to minimize artifactual reflections.
Materials and methods
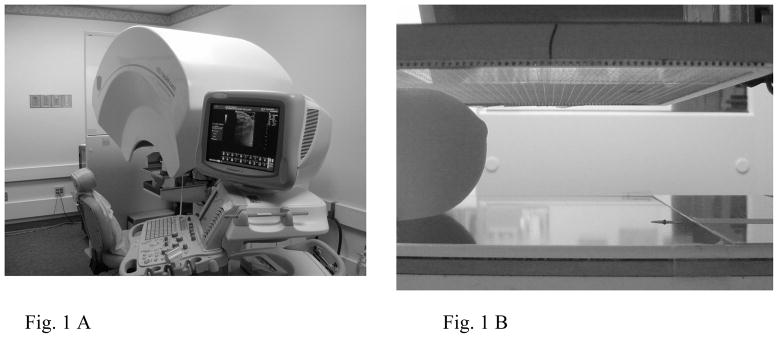
This study was approved by the institutional review board and informed consent was obtained from all subjects. Trials were performed on a combined system consisting of a GE LOGIQ 9 ultrasound system (GE Health Systems, Milwaukee, WI) and a second-generation GE/University of Michigan research DBT unit (Fig. 1). A linear matrix array ultrasound transducer (GE M12L) operating at a center frequency of 12 MHz was translated across a compression paddle with a motorized transducer carriage. This automated breast ultrasound scanning system was developed jointly with GE.
Fig. 1.
A, Dual modality combined system consisting of a GE LOGIQ 9 ultrasound system and a second-generation GE digital tomosynthesis unit. B, Breast-simulating phantom illustrating an air gap between the phantom and the compression paddle at the periphery.
The subject was seated comfortably throughout the scan to minimize motion artifacts and fatigue, and the breast was positioned between the compression paddle and digital X-ray detector. Instead of the solid TPX (polymethylpentene) compression paddle described previously6–9, a fiber mesh paddle similar to a fine mesh tennis racquet was used in this study12. This new paddle, similar to but with a finer mesh than one recently published, makes acoustic coupling easier and better between the transducer and the breast surface. An evaluation of various mesh paddle designs for our dual modality system will be presented in the near future. A compression force of approximately 4 to 8 dN was typically used with the dual-modality system to minimize subject discomfort while stabilizing the breast. Eight breasts of 4 female healthy volunteers were imaged with this combined system. The ages of the 4 healthy volunteers ranged from 45 to 54 years (mean, 51 years). Two automated scans of each breast were performed. One scan was conducted without using rubber dam. For the second scan the rubber dam was deployed around the breast periphery and pushed a little toward the chest wall. Bubble-free ultrasound gel was employed as the coupling medium between the transducer and the breast surface through the fiber mesh compression paddle for craniocaudal (CC) views.
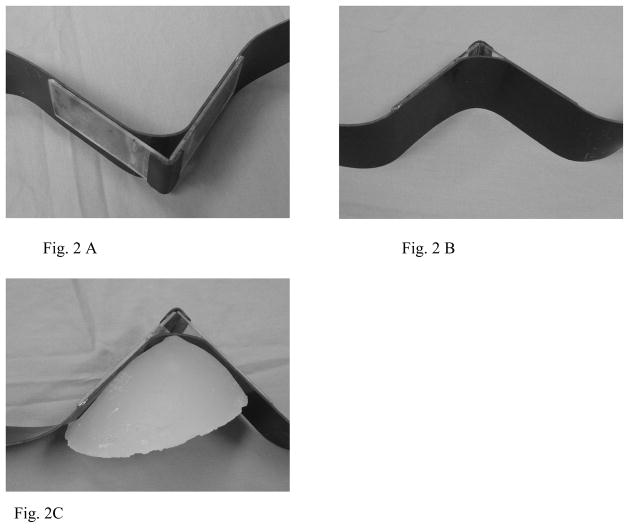
Rubber dams were constructed by adhering two 0.2 cm thick plastic sheets to a strip of 0.15 cm thick butyl rubber. The dams were made to mimic the shape of the breast (Fig. 2). Rubber is advantageous because it can reduce artifacts by absorbing ultrasound reflections, but is too soft to use by itself. Plastic, on the other hand, is hard and maintains its structure, but lends itself to artifacts. The combination of rubber supported by a plastic backing maintains the advantages of both materials. Six dams were constructed to accommodate an angle range from 30° to 120° with heights of 2.0, 2.5, 3.5, 4.0, 5.0, and 6.0 cm. The variable angle of the V shape and height differences of these dams accommodate the different breast sizes of patients.
Fig. 2.
Rubber dams constructed by adhering two 0.2 cm thick plastic sheets to a strip of 0.15 cm thick butyl rubber and a rubber hinge (A,B). The inside shape adequately mimics that of the breast in this lateral view (C) as well as other views.
To estimate the fraction of the breast surface area that was in contact with the compression paddle, we employed a method described previously.8 In brief, thin transparency film was placed on the compression paddle. Using a marking pen, the technologist made visual tracings of the paddle-to-breast contact regions and the outer breast borders on those transparencies. The tracings were drawn for 8 breasts both with and without using a rubber dam. The tracings were then digitized with a flatbed scanner and analyzed using a public domain computer program ImageJ (http://rsb.info.nih.gov/ij/docs/intro.html). The contact and outer breast contours were traced by hand in ImageJ, and the areas calculated using the measure function. Also, the lengths of the gaps between the border of the contact region and the outer border of the breast in the tracings were measured at 5 different angles (30, 60, 90, 120 and 150º).
For both the “with” and “without” dam cases, after the contours were traced, the transparencies were removed and ultrasound gel was distributed over the breast using a syringe. The ultrasound translation system was lowered to the compression paddle so the transducer was in contact with the gel/breast, and 3D ultrasound images were acquired. Two readers independently reviewed the 3D ultrasound images in a blinded study. The images were displayed using the ImageJ program. The readers were asked to rate overall breast image quality, especially the breast coverage and image artifacts, on a scale of 1–5 with 1 being ‘Much better image quality without rubber dam’, 3 being ‘Equivalent image quality’ and 5 being ‘Much better image quality with rubber dam’.
Statistical analyses were performed with Excel (Microsoft Corporation, Redmond, WA). Breast coverage-related parameters were calculated and reported as mean ± SD (standard deviation). The coverage-related parameters derived from the scans using a rubber dam and those derived from the scans not using the dam were compared by a paired two-tailed Student’s t test. The level of significance was set to 0.05.
Results
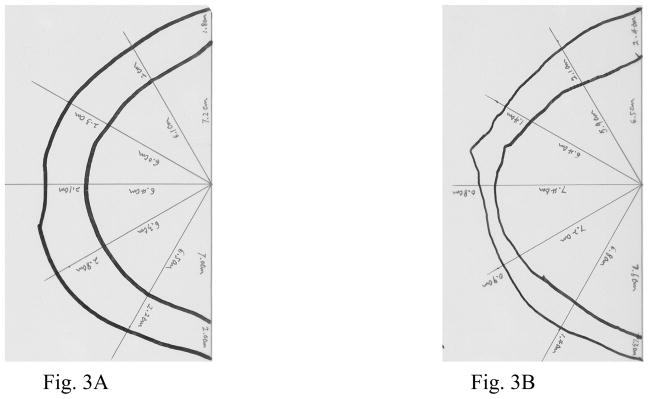
An example of the visual traces of the breast-paddle contact areas and breast outer boundaries for the “with” and “without” dam cases are shown in Figure 3.
Fig. 3.
Visual tracings of regions of the breast in contact with the paddle (inner curves) and outer breast borders in the same breast. A, without rubber dam the percentage of the breast area in contact with the paddle is smaller, about 55.2%. B, using rubber dam with slight compression force, the percentage of the breast area in contact with the paddle is larger, approximate 70%.
The linear dimensions of the gaps between the border of the contact region and the outer border of the breast in the tracings for the “with” and “without” dam cases are listed in Table 1.. For the 8 breasts in this study, the linear dimensions of the breast in contact with the paddle were larger, the noncontact gaps at the breast periphery were smaller, and the percentages of the breast linear dimensions in contact with the paddle were larger using rubber dam than those of without using the dam at all 5 different angles. Furthermore, the differences in noncontact gaps at the breast periphery and percentages of breast in contact with paddle between using a rubber dam and without using it were all statistically significant (P < 0.05).
Table 1.
Linear Dimensions of the Gaps at the Breast Periphery from Visual Tracings
| Angle | Breast in Contact With Paddle, cm
|
Noncontact Gaps at the Breast Periphery, cm
|
Percentages of Breast in Contact with Paddle, %
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| without dam | with dam | P | without dam | with dam | P | without dam | with dam | P | |
| 30° | 6.19±1.86 | 6.54±2.16 | 0.14 | 1.76±0.36 | 1.00±0.67 | 0.01 | 75.9±5.7 | 85.8±9.9 | 0.01 |
| 60° | 5.55±2.12 | 5.80±2.16 | 0.21 | 1.76±0.39 | 0.96±0.36 | 0.001 | 74.5±7.4 | 84.3±8.0 | 0.002 |
| 90° | 5.30±2.06 | 5.65±2.17 | 0.08 | 1.75±0.43 | 0.96±0.32 | 0.006 | 74.3±4.5 | 84.2±6.3 | 0.008 |
| 120° | 5.33±2.07 | 5.79±2.38 | 0.04 | 1.81±0.55 | 0.91±0.40 | 0.008 | 73.6±6.2 | 84.5±9.0 | 0.01 |
| 150° | 5.91±1.99 | 6.46±1.88 | 0.08 | 1.83±0.66 | 1.00±0.52 | 0.01 | 75.4±9.2 | 86.0±7.0 | 0.01 |
Values are mean ± SD
The percentages of the breast area in contact with the compression paddle from the visual tracings are listed in Table 2. There were significant differences in breast area in contact with paddle and total breast area between using a rubber dam and without using it (P < 0.05 and P <0.01, respectively). The breast areas in contact with paddle were larger (69.9 ± 46.7 cm2 vs. 61.2 ± 42.3 cm2 ) and total breast areas were smaller (88.5 ± 48.5 cm2 vs. 99.1 ± 49.1 cm2 ) using rubber dam than those of without using it. A significant difference was also found in the percentages of the breast area in contact with the paddle between using rubber dam and without using it (P < 0.01). The percentage of the breast area in contact with the paddle was approximately 75.9% ± 8.8% (range, 64.3%–90.4%) with rubber dam usage, and 59.0% ± 9.2% (range, 48.3%–79.5%) without it.
Table 2.
Percentage of Breast Area in Contact with the Compression Paddle from Visual Tracings
| Breast NO. | Area in Contact with Paddle, cm2 |
Total Breast Area, cm2 |
Breast Area in Contact with Paddle, %
|
Increase in Fraction of Breast Area, % | |||
|---|---|---|---|---|---|---|---|
| without dam | with dam | without dam | with dam | without dam | with dam | ||
| 1 | 63.49 | 74.31 | 115.07 | 106.18 | 55.2 | 70 | 26.8 |
| 2 | 52.67 | 64.89 | 109.01 | 82.17 | 48.3 | 79 | 63.6 |
| 3 | 66.03 | 81.18 | 110.19 | 94.5 | 59.9 | 85.9 | 43.4 |
| 4 | 159.23 | 174.53 | 200.25 | 193 | 79.5 | 90.4 | 13.7 |
| 5 | 49.61 | 62.22 | 85.62 | 83.95 | 57.9 | 74.1 | 28 |
| 6 | 46.39 | 46.85 | 81.13 | 68.29 | 57.2 | 68.6 | 19.9 |
| 7 | 22.79 | 29.42 | 43.16 | 39.38 | 52.8 | 74.7 | 41.5 |
| 8 | 29.68 | 25.88 | 48.52 | 40.26 | 61.2 | 64.3 | 5.1 |
With the dam the mean estimated area of the breast in contact with the paddle increased 14.4% ± 14.3%, while the mean increase in the fraction of the total breast area in contact with paddle was 30.2% ± 18.7%. The difference was due to the mean total projected area of the breast decreasing 11.7% ± 7.6% as the dam was pressed against it.
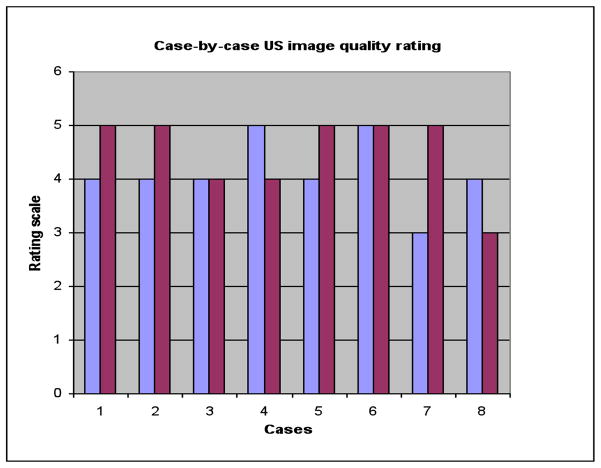
Figure 4 compares the relative image quality obtained with the automated ultrasound scanning system using a rubber dam surrounding the breast periphery and without using it. The rubber dam significantly improved breast coverage because it reduces gel slippage away from the breast periphery.
Fig. 4.
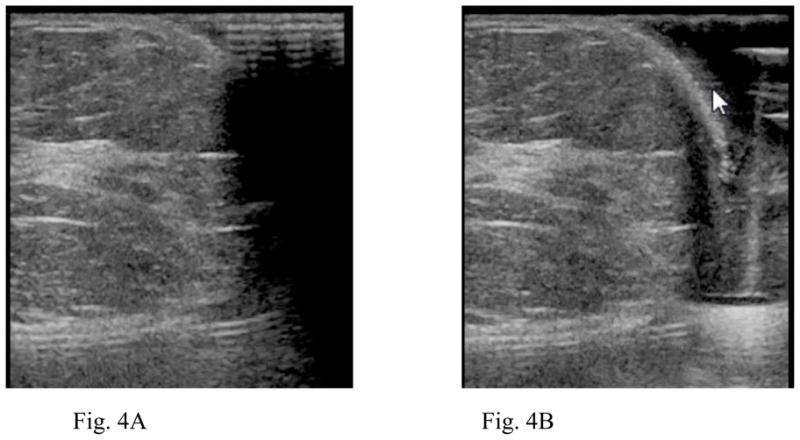
A, Single slice of a gray scale image volume without rubber dam around the breast border. B, Same image slice, using rubber dam surrounding the breast periphery, the rubber dam significantly improved breast coverage.
The image quality of automated ultrasound using a rubber dam was consistently judged to be superior to that without using it as the readers expressed a mean preference of 4.3 on a scale of 1 to 5, with 5 being ‘much better image quality with a rubber dam’. Figure 5 shows the two readers’ ratings of the ultrasound image quality.
Fig. 5.
Ultrasound image quality ratings for 8 cases by two readers. A scale of 1 to 5 was used, where a rating of 1 was equivalent to ‘Much better image quality without rubber dam’ and a rating of 5 was equivalent to ‘Much better image quality with rubber dam’.
Discussion
Ultrasound has been a valuable supplement to mammography in characterizing and even detecting breast lesions in high-risk women, including particularly those with mammographically dense breasts.2, 4, 13,14 Automated ultrasound in our current implementation in the mammographic geometry probably cannot yet entirely replace clinical hand ultrasound scans for screening purposes because of the presence of air bubbles in the coupling medium, the lack of full breast volume coverage, possibly less than optimal acquisition due to the practical limitation of employing only one or two (e.g., CC and MLO) views of tissues of interest in the 3D scans, and the reduced compression when the whole breast is compressed. However, less interpretation is required at the time of scanning and anatomic correlation of ultrasound with mammography or tomosynthesis aids the radiologist’s evaluation of a suspicious mass in the human breast and raises the confidence level of his or her assessment.
As discussed in a previous study,8 if gel does not liberally fill the gaps between the breast and the compression paddle at the breast periphery, ultrasound coverage can be limited to only half of the total breast area for the combined x-ray/ultrasound imaging system. Coverage of the periphery can be critical because 73% of malignant lesions in breasts of women under 50 have been found at the periphery of the breast, as defined by a zone 1 cm wide within the subcutaneous fat or anterior to the retromammary fat.15
Use of the here-introduced rubber dam enhanced the percentages of breast (tissue) area in contact with the paddle by 30%, without changing the compressed breast thickness. Use of the dam resisted gel slippage, and (probably) reduced reverberations in the gel by absorbing some of the extraneous ultrasound. Retained gel at the periphery of the breast allowed better imaging of the subareolar region. The overall image quality of automated ultrasound using the introduced rubber dam was consistently judged to be superior to that without using it. The gel could be easily dispensed to the breast periphery when using the rubber dam with (probable) reduction in air bubbles as well. The variable angle (shape) capability and height differences of the rubber dams accommodate the different breast sizes. The dam can be easily pushed toward the chest wall and as long as the pushing against the breast is not too forceful, posterior movement of breast tissues outside of the ultrasound scanning range is not likely, and spatial correlation between structures in the ABU and the DBT, taken before deployment of the dam, are not affected greatly.
Finally, it should be noted that in our study, artifact reflections were sometimes observed in the ABU images with the dams. These reflections arise due to grazing incidence of the ultrasonic waves on the flat rubber surface of the dam. The reflections could be reduced by utilizing a sawtooth or other rough pattern on the rubber surface. Also in this study, some variability in measurements was caused by the protective cowling for the tomosynthesis, though particular care was taken to reposition the same breast consistently. We are in the process of replacing the current cowling with a more ergonomic one.
In summary, the rubber dam method in ABU in the mammographic geometry increases breast coverage by shaping the breast and retaining gel at the periphery to reduce noncontact gaps. The image quality of automated ultrasound using the rubber dam was superior to that without its use.
Acknowledgments
This work was supported in part by American Public Health Service grant R01 CA91713. Others contributing recently to the combined system used in this project were: Andrea Schmitz, MS (GE Global Research); Gerald L. LeCarpentier, PhD, Ganesh Narayanasamy, MS, Sumedha P. Sinha MS, and Marilyn Roubidoux, MD (Department of Radiology, Health System, University of Michigan)
Abbreviations
- 3D
3-dimensional
- ABU
automated breast ultrasound
- DBT
digital breast tomosynthesis
- CC
craniocaudal
References
- 1.Jackson VP. The role of ultrasound in breast imaging. Radiology. 1990;177:305–311. doi: 10.1148/radiology.177.2.2217759. [DOI] [PubMed] [Google Scholar]
- 2.Taylor KJ, Merritt C, Piccoli C, et al. Ultrasound as a complement to mammography and breast examination to characterize breast masses. Ultrasound Med Biol. 2002;28:19–26. doi: 10.1016/s0301-5629(01)00491-4. [DOI] [PubMed] [Google Scholar]
- 3.Conway WF, Hayes CW, Brewer WH. Occult breast masses: Use of mammographic localizing grid for US evaluation. Radiology. 1991;181:143–146. doi: 10.1148/radiology.181.1.1653441. [DOI] [PubMed] [Google Scholar]
- 4.Kolb TM, Lichy J, Newhouse JH. Occult cancer in women with dense breasts: Detection with screening ultrasound: Diagnostic yield and tumor characteristics. Radiology. 1998;207:191–198. doi: 10.1148/radiology.207.1.9530316. [DOI] [PubMed] [Google Scholar]
- 5.Berg WA. Rationale for a trial of screening breast ultrasound: American College of Radiology Imaging Network (ACRIN) 6666. AJR. 2003;180:1225–1228. doi: 10.2214/ajr.180.5.1801225. [DOI] [PubMed] [Google Scholar]
- 6.Kapur A, Carson PL, Eberhard J, et al. Combination of digital mammography with semiautomated 3D breast ultrasound. Technol Cancer Res Treat. 2004;3:325–334. doi: 10.1177/153303460400300402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Booi RC, Krucker JF, Goodsitt MM, et al. Evaluating thin compression paddles for mammographically compatible ultrasound. Ultrasound Med Biol. 2007;33:472–482. doi: 10.1016/j.ultrasmedbio.2006.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinha SP, Goodsitt MM, Roubidoux MA, et al. Automated ultrasound scanning on a dual-modality breast imaging system: Coverage and motion issues and solutions. J Ultrasound Med. 2007;26:645–655. doi: 10.7863/jum.2007.26.5.645. [DOI] [PubMed] [Google Scholar]
- 9.Sinha SP, Roubidou MA, Helvie MA, Nees AV, Goodsitt MM, LeCarpentie GL, Fowlkes JB, Chaleck CL, Carson PL. Multi-modality 3D breast imaging with X-Ray tomosynthesis and automated ultrasound. Procs 29th Ann Internat Conf IEEE Engineering Med Biol Soc; 2007. pp. 1335–1338. [DOI] [PubMed] [Google Scholar]
- 10.Kotsianos-Hermle D, Wirth S, Fischer T, et al. First clinical use of a standardized three-dimensional ultrasound for breast Imaging. Eur J Radiol. 2008 doi: 10.1016/j.ejrad.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Shipley JA, Duck FA, Goddard DA, et al. Automated quantitative volumetric breast ultrasound data-acquisition system. Ultrasound Med Biol. 2005;31:905–917. doi: 10.1016/j.ultrasmedbio.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Blane CE, Goodsitt MM, Grimm JC, Pavlik J, March D, Ong JT, Blacklaw L, Helvie MA. New Compression Paddle for Wire Localization in Mammography. Acad Radiol. 2010;17(2):142–145. doi: 10.1016/j.acra.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 13.Moss HA, Britton PD, Flower CDR, et al. How reliable is modern breast imaging in differentiating benign from malignant breast lesions in the symptomatic population? Clinical Radiology. 1999;54:676–682. doi: 10.1016/s0009-9260(99)91090-5. [DOI] [PubMed] [Google Scholar]
- 14.Berg WA, Blume JD, Cormack JB, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008;299:2151–2163. doi: 10.1001/jama.299.18.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stacey-Clear A, McCarthy KA, Hall DA, et al. Mammographically detected breast cancer: location in women under 50 years old. Radiology. 1993;186:677–680. doi: 10.1148/radiology.186.3.8381550. [DOI] [PubMed] [Google Scholar]