Abstract
Liver diseases are an increasingly common cause of morbidity and mortality; new approaches for investigation of mechanisms of liver diseases and identification of therapeutic targets are emergent. Lipid rafts (LRs) are specialized domains of cellular membranes that are enriched in saturated lipids; they are small, mobile, and are key components of cellular architecture, protein partition to cellular membranes, and signaling events. LRs have been identified in the membranes of all liver cells, parenchymal and non-parenchymal; more importantly, LRs are active participants in multiple physiological and pathological conditions in individual types of liver cells. This article aims to review experimental-based evidence with regard to LRs in the liver, from the perspective of the liver as a whole organ composed of a multitude of cell types. We have gathered up-to-date information related to the role of LRs in individual types of liver cells, in liver health and diseases, and identified the possibilities of LR-dependent therapeutic targets in liver diseases.
Keywords: Hepatocytes, Stellate cells, Kupffer cells, Endothelial cells, Signaling, Therapeutic, Viral, Hepatitis C virus, Metabolism
INTRODUCTION
The liver is the largest parenchymal organ of the body and has a multitude of important and complex functions; among the most notable are the metabolism of fat, proteins, and carbohydrates, synthesis and secretion of bile, microelement recycling and detoxification of products resulting from body metabolism (bilirubin, ammonia, etc.) and from exogenous toxins (drugs, alcohol and environment)[1]. The liver is also an immune[2] and an endocrine[3,4] organ and functions as a blood capacitance reservoir[5,6]. To accomplish these many assignments, the liver accommodates a wide variety of cell types, including those that call liver “home”, namely liver progenitor cells, hepatocytes, Kupffer cells (KCs), stellate cells (SCs) and the cellular components of vasculature, and those that use the liver as a temporary and/or terminal station, such as blood cells[1,7]. Liver diseases are the 10th leading cause of death and account for significant morbidity across the entire age and gender spectrum of the US population[8,9]. The mechanisms of liver diseases are extensively researched but not fully understood. More recently, research data have emerged proposing that some pathogenic mechanisms, such as inflammation, tissue death and regeneration, and organ remodeling, are shared across a large spectrum of liver diseases of distinct etiologies[10-14], with the suggestion that common denominators of cell structure or function may be involved. Here we have focused on a common denominator of the cellular structure, the lipid rafts (LRs), as players in liver physiology and pathology.
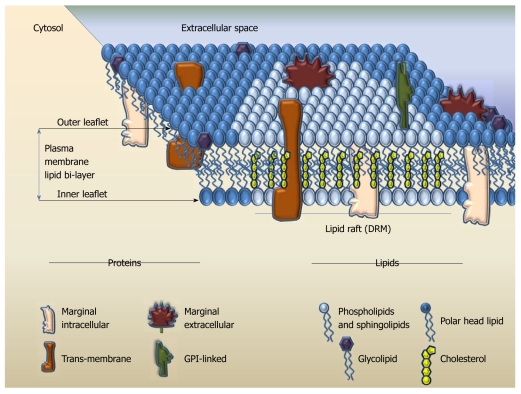
Cellular membranes separate each cell and define their entity. The main components of the cellular membrane are lipids and proteins[15]. Structurally, the membrane lipid molecules consist of a polar globular head and a straight non-polar hydrophobic backbone region. Each row of lipids aligns in a leaflet at the level of globular heads and hydrophobic areas of the leaflet attract similarly charged structures, such as the straight region of another lipid layer. Thus, the plasma membrane (PM) consists of two leaflets with the non-polar regions pointing inward and the polar heads pointing to the water rich-zones (intra- and extra-cellular spaces); architecturally this structure portrays a lipid bilayer[16] (Figure 1). Besides serving as warrant of cellular identity and integrity, the lipid bilayer assures that the membrane is flexible. At lower temperatures, the lipid bilayer forms a gel state and is tightly packed; as the temperature rises the bilayer favors tri-dimensional movement of the lipid molecules and the interior space between the two leaflets becomes more fluid. It is the gel/fluid exchange state that allows horizontal and vertical movement of lipids, and also of other components of the membrane[15-17]. Proteins are embedded into the lipid bilayer, either by spanning through, as trans-membrane integral structures that could cross in a single- or multi-pass fashion, or as attached structures; the latter exist as peripheral proteins, attached to the membrane exclusively on either the extracellular or cytosolic face, or as glycosylphosphatidylinositol (GPI)-anchored proteins on the extracellular face of the membrane[18]. At the end of the 20th century, the LR hypothesis of cellular membrane function emerged: this proposed that certain regions of the lipid bilayer modify their chemical composition to become more rigid, thus allowing some membrane proteins to physically segregate depending on their interaction with the bilayer components and with other proteins[19,20]. This theory combined the biological knowledge about cellular activation and the biochemical knowledge about protein folding with biophysical approaches to the dynamic cellular membrane structure and attempted to answer the puzzling question about how proteins cluster and what contributes to signal transduction.
Figure 1.
The theoretical model of lipid bilayer and lipid rafts in cellular membranes. GPI: Glycosylphosphatidylinositol; DRM: Detergent-resistant domain.
LRS: STRUCTURE, FUNCTIONS AND RESEARCH METHODOLOGY
LR structure and functions
LRs are areas of cellular membranes with a signature composition rich in sphingolipids and cholesterol phospholipids. Saturated fatty acids are preferentially enriched in the side chains of the membrane phospholipids, which allows closer packing and thus increased rigidity, more order, and less fluidity of the LRs compared to the surrounding membrane[15,19-21]. LRs act as a unique platform that aids co-localization of proteins involved in sensing (receptors), reacting (pores) and triggering/sustaining cell activation (intracellular signaling pathways) (Figure 1). Besides their structural signature, LRs exhibit two more unique characteristics: they are small, ranging from several to about 500 nm, and are dynamic, with a variable life span in the order of milliseconds (msec). It is not fully understood whether the LRs form and disintegrate constantly or maintain a longer lifespan when a cell is in its steady state, because a relatively constant number/composition of proteins can be identified in the LRs at this stage. However, once the cell is activated, the LRs undergo a radical change in composition by adding or eliminating certain proteins and thus accommodating the cellular needs for formation of signaling platform in a matter of msec. While they are well documented to be in the PM of the cells, it has been suggested that LRs can also reside in the intracellular structures, such as endoplasmic reticulum (ER), peroxisomes, mitochondria, and endosomes[22-26]; to date it is not clear whether such findings are truly due to LR presence in these intracellular compartments or if they are an artifact of LR isolation/investigation techniques. LRs are present throughout the entire evolutionary chain, from the viruses and bacteria[27] to mammals; the purpose of the LR in evolution is yet to be fully understood.
LR research methodology
Studying the LRs is challenging. With sizes ranging up to 500 nm in diameter, the LRs are beyond the resolution of optical microscopes. For this reason the overlay of one or more stains tagged to the proteins of interest revealing a significant co-localization with the coalesced LRs, labeled indirectly with a fluorescent choleratoxin B, is usually suggestive but never a definite indication of the LR localization of the studied proteins. In addition to being small, the rafts diffuse in msec across the cell membrane and thus require additional efforts for timely detection. The transmission electron microscope can analyze a 5-nanometer-thick cell membrane and captures short time frames; the more dynamic and short-lived rafts can only be observed with advanced imaging techniques such as atomic force microscopy (AFM)[28]. Fluorescence lifetime spectroscopy, including Förster resonance energy transfer (FRET), is becoming more accepted in the LR research field due to the fact that the capacity of energy transfer in FRET is about the size of the rafts and it occurs in the range of msec, thus covering both the size and the life span of the LR. Single point microscopic decay and fluorescence lifetime imaging microscopy are often used in combination with FRET for more comprehensive analysis of LR-related time-sensitive processes[29]. Flow cytometry analysis of LRs is emerging; however, it provides very limited resolution both for the size and for the timing of LR-localized events[30]. Fluorescence correlation and cross-correlation spectroscopy (FCS/FCCS) deliver information of fluorophore mobility and dynamics of lateral heterogeneity in the membrane and can be used in single or multiple colors[31]. Single particle tracking (SPT) can be employed to define the translational trajectory of very small particles, including quantum dots, to identify cluster size confinement based on intensity. The thinning out clusters while conserving stoichiometry of labeling (TOCCSL) technique is employed for LR analysis because of its proficiency in discriminating between clusters and monomers[32]. The additional advantage of FRET, FCS/FCCS, SPT and TOCCSL is their high spatial/temporal resolution, and thus their ability to register rafts as they form and dissociate in time. Labeling of living cells with the fluorescent probe 6-acyl-2-dimethylaminonapthalene (Laurdan), which exhibits a 50-nm red shift as membranes undergo phase transition from gel to fluid due to altered water penetration into the lipid bilayer, followed by two-photon microscopy, is often used as another indirect method of LR visualization[33].
Translocation of proteins to or from the LRs is often analyzed by sucrose-density gradient fractionation of the membranes and subsequent Western blot analysis; LRs are defined by their insolubility in diverse nonionic detergents [thus named detergent-resistant domains (DRMs)] and by floating in the low-density sucrose fractions (interface between 5% and 30%) upon ultracentrifugation[34]. Diverse detergents can be employed, yielding diverse composition of DRMs[34-39]. Furthermore, some researchers construct step sucrose gradients and further sub-divide the DRMs into light and intermediately-light fractions, which may have distinct protein composition. It is still debatable as to how closely the DRMs represent the true identity of the LRs; however, this method yields consistent results and is the only one available that allows enrichment and analysis of large protein complexes at reasonable cost and using old-fashioned technology.
The functional assessment of the LRs in vitro is usually performed using reduction and enrichment approaches. Treatment with agents leading to cholesterol sequestration, including amphotericin, filipin or nystatin, inhibition of cholesterol synthesis using HMG-CoA reductase inhibitors, or cholesterol wash-out with mβCD, are among the well-accepted approaches to disrupt putative LRs; they are largely based on cholesterol manipulation[40,41]. Another method commonly utilized for LR destabilization is treatment with fumonisin B1, which removes sphingolipids[40]. The advantage of using mβCD over fumonisin B1 is based on the fact that the former acts rapidly, while the latter requires pretreatment of cells for about 72 h, which is longer than the time some polarized cells, including hepatocytes, can remain truly polarized in isolated cell culture[42]. Cholesterol replenishment and ceramide supplementation, which displaces cholesterol, are often employed to modulate the fluidity of the LRs and thus affect their function.
In vivo LR modulation has gained recent popularity based on findings that dietary lipids can modify lipid composition of cell membranes. In this context, multiple studies have attempted to establish how dietary factors or modulation of blood lipids, including cholesterol, affect LR-based signaling in various cell types[43,44]. Comprehensive experimental-based conclusions about the effects of dietary lipids in regulating LRs in non-liver systems and targeted evaluations of the liver in this regard are still awaited. Reliable methods of in vivo visualization of LRs also await development.
The significant difficulties in analysis of LRs in primary biological membranes have led to development of model systems. Diverse artificial membranes and models have been created over time, with different ranges of spatial and temporal orders, diverse lipid and protein compositions, protein/lipid ratio or thickness of the lipid bilayer[45,46]. While helpful to elucidate the basics of the membrane function and structure, these models lack the combination of the proximity of the membrane with the cytoskeleton and regulatory/signaling proteins that are recruited in diverse ratios and in a time-dependent manner in natural biological membranes[45]; to date there is no comprehensive artificial model of LR-containing membranes.
COMPOSITION OF LIVER LRS
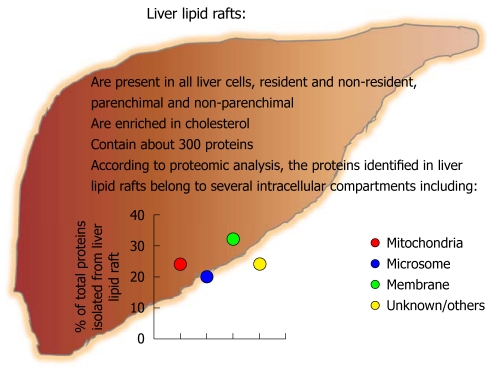
An extensive number of proteins have been identified as residing in LRs in the liver[36-39]. Depending on the method of raft isolation and protein analysis, it is currently estimated that at least 300 proteins reside in the LRs in the normal liver; these data include analysis of both human and rodent livers[36-39]. Bae et al[36] identified 196 proteins and pointed to a relatively large content of mitochondrial proteins in the rat liver membrane LRs. Zhang et al[38] reported 175 non-redundant gene products identified in mouse liver PM, isolated from mouse liver by floating in the sucrose density gradient upon ultracentrifugation, which largely resemble the DRM fraction enriched in LRs[23,34]. Zhang et al[38] also identified that about 50% of the LR-associated proteins were integral membrane proteins with one to seven transmembrane domains (TMDs), 40% represented enzymes, 12% were receptors and 9% were proteins with unknown function. He et al[39] identified 104 proteins in human liver membranes with about one third being of cytoskeletal affiliation, including proteins in fodrin-based meshworks, adhesion proteins involved in inter-cellular junctions, focal adhesions, desmosomes, hemidesmosomes and tight junctions, proteins that regulate F-actin dynamics, and motor proteins; most of these proteins usually affiliate with LRs in other cell types. Mazzone et al[37] pointed to the differential protein identity from the apical and basolateral LRs of the PM in normal rat hepatocytes. These data indicate a great diversity in the types of proteins affiliated with LRs in the liver (Figure 2) and indirectly suggest the importance of the LRs in the liver.
Figure 2.
Estimation of the protein origins identified in the liver lipid rafts. Adapted, in part, from Bae et al[36], with permission.
The analysis of the composition/function of LRs in the liver performed so far has involved whole liver and does not take into account that liver, as a whole, accommodates a wide variety of cell types. Nevertheless, fractioning of LRs from the whole liver has revealed novel information and thus spearheaded the interest in the field and targeted focused investigations towards specific liver cell populations.
LRS IN RESIDENT LIVER CELLS
LRs in hepatocytes
LRs aid polarized sorting and trafficking of apical proteins in both directed and trans-cytotic pathways in hepatocytes: Two structurally and functionally distinct PM domains, i.e. the apical and basolateral domains, determine the tri-dimensional architecture of the hepatocyte as true polarized cells; these domains are separated by the tight junctions. While the molecular signature of apical and basolateral domains is relatively well known, the maintenance of such identity requires sophisticated protein sorting and trafficking, the mechanisms of which are yet to be fully defined. Specific membrane-sorting signals have identified many involved proteins[47]. For example, GPI-membrane anchor and TMD target the proteins to the membrane[48]. Moreover, Tyr- and diLeu-based amino acid motifs, which are recognized by distinct molecular subunits of adaptor complexes, seem to direct the proteins to the basolateral membrane[49].
Two membrane-sorting pathways are known: direct and indirect. Unlike many polarized cells, hepatocytes employ both pathways to guide their proteins to the desired location. In “direct” pathway of membrane targeting, the newly synthesized proteins are primarily sorted in the trans-Golgi network (TGN) and then delivered directly to the membrane; this pathway serves both apical or basolateral membrane domains without advantaging either of them[50]. Membrane multispanning ATP-binding cassette (ABC) transporters, multidrug resistance protein 1 (MDR1), and P-glycoprotein, to name a few, employ the direct sorting mechanism in hepatocytes[51]. In “indirect” pathway, the new protein cargo travels from the TGN to the basolateral surface, from where it is endocytosed and subsequently transported to the opposite apical surface of the membrane, as reviewed by Nelson et al[52]. This laborious, energy-inefficient and very lengthy process is also called the trans-cytotic pathway and its purpose is not fully understood. The GPI-linked proteins and those with a single TMD preferentially employ the indirect pathway for apical trafficking[53].
Until recently, the factors that directed the proteins into direct vs indirect pathways of membrane-sorting were largely unknown. Nyasae et al[54] reported that cholesterol and glycosphingolipids are required for delivery from basolateral early endosomes to the subapical compartment. Slimane et al[55] identified that the protein structure and its lipophilic characteristics sort the differential apical vs basolateral targeting of the proteins in a sphingolipid/cholesterol-enriched LRs-dependent manner. These authors also reported that the liver apical proteins that contain multiple membrane-spanning domains are selectively incorporated into lipid microdomains in the TGN and are then transported directly to the apical membrane[55]. However, direct apical sorting is not solely driven by incorporation into LRs per se[55]. Conversely, proteins that have only one TMD or tether to the membrane using their GPI anchor are also sorted to the LRs in TNG; they travel first to the basolateral membrane, where LR-based mechanisms are again key in their delivery to the subapical compartment and further exposure on apical membrane. Slimane et al[55] additionally suggested that lipid composition of the LRs is also critical for protein sorting. Thus LRs play a key role in both direct and indirect membrane targeting of the proteins and act as sorting platform for directing the proteins via one pathway or another.
LRs in hepatocyte polarity: Hepatocytes are classical polarized cells; the adequate function of the liver as an organ is ensured by the spatial setting and by maintenance of hepatocyte polarity. The complex polarity of the hepatocyte is characterized by the existence of several basolateral and apical poles per cell. The complex mechanisms of establishment and maintenance of hepatocyte polarity are not fully understood; however, a role for calcium waves has been proposed. In hepatocytes the Ca2+ waves are polarized, thus occurring in an apical-to-basal fashion[56]. The polarity of the Ca2+ signal is largely due to the increased density of inositol 1,4,5-trisphosphate receptor (InsP3R) in the pericanalicular region; redistribution of InsP3R from the apical to the basolateral region is associated with concomitant slowing of the onset and speed of Ca2+ waves in hepatocytes[57]. The pericanalicular accumulation of InsP3Rs in not exclusive to hepatocytes, as it is also observed in other types of polarized cells such as pancreatic acinar cells, cholangiocytes, salivary acinar and duct cells[58]. The pericanalicular area has been named the “trigger zone,” because it defines the subcellular region that triggers the formation of Ca2+ waves[59,60]. The pericanalicular area is rich in LRs and it is also a preferred localization of InsP3Rs; most importantly, recruitment of InsP3Rs to this area is highly dependent upon the presence of intact LRs[57]. Similar to InsP3R redistribution, LR disruption by cholesterol depletion substantially slows Ca2+ waves in hepatocytes[57]. The expression of apical InsP3Rs is decreased or absent in cholangiocytes from patients with primary biliary cirrhosis, sclerosing cholangitis, common bile duct obstruction, and biliary atresia, suggesting that InsP3Rs deficit and/or misplacement may represent a final common pathway for the development of cholestatic disorders[61]. Given the key role of LRs in housing the InsP3Rs on the apical hepatocyte membrane, it is easy to envision a role for LRs and/or hepatocyte de-polarization in cholestatic disorders; this area remains open for investigation.
LRs as signaling platforms: The hepatocyte PM houses a wide variety of proteins that function as sensors, receptors, and/or transporters; these proteins allow the hepatocyte to react to a rapidly changing extracellular environment and accommodate the needs of homeostasis. Among the best researched hepatocyte receptors for which the intracellular signaling pathways are well defined and the ties to LRs are well established are hepatocyte growth factor (HGF) receptor (HGFR), epidermal growth factor (EGF) receptor (EGFR), angiotensin II type 1 (AT1R) and insulin receptor (IR) receptors.
The HGFR, also called c-Met, is activated by HGF and triggers hepatocyte proliferation, morphogenesis and survival. Defects of HGFR are a cause of hepatocellular carcinoma[62]. The HGFR is a heterodimer that exhibits tyrosine kinase activity and associates with a multiprotein complex to trigger downstream signal systems, including src, Grb2/SOS, PI3 kinase, Gab1 and focal adhesion kinase; the adequate function of these adaptors/signal transducers is largely dependent on LRs[63,64]. To date, it is not clear if the HGFR itself is localized in the LRs. However, HGF promotes HGFR association with CD44 and recruitment of this multi-protein receptor complex into caveolin-enriched LR microdomains[65]. The LR-dependent HGF/HGFR signal plays a role in several pathologic processes, including protection from lipopolysaccharide-induced vascular hyper-permeability[65]; its role in hepatocyte function remains to be clarified.
EGF binds to the EGFR and regulates hepatocyte growth both in vivo and in primary culture. EGFR signaling activates a group of signal transducers and activators of transcription, which increase the transcription of a characteristic set of early growth response genes thus leading to hepatic DNA replication[66]. In normal adult liver, EGFR expression is low, whereas EGF is virtually nondetectable. In contrast, in advanced cirrhosis, a continuous EGFR synthesis is accompanied by EGF expression that is localized to hepatocytes and proliferative bile epithelium[67,68]. EGF treatment is followed by rapid ubiquitination of the EGFR in hepatocytes[69] and plays a key role in trafficking of the EGFR between early and late endosomal compartments[70]. Ubiquitinated EGFR is internalized almost exclusively via a non-clathrin LR-dependent route[70]. In this context, EGFRs recruited to LRs in response to EGF derive almost exclusively from endosomes[24]. EGFRs in early endosomes are more tyrosine phosphorylated than those in late endosomes, indicating that EGFR might be partially dephosphorylated in an LR-dependent manner before accessing the late compartment; however, once localized, the EGFRs in endosomal LRs are relatively resistant to dephosphorylation[24]. Some of the kinase receptors that are internalized through caveolin-containing LRs have a high probability of being directed to the degradative pathway rather than having a function in signaling[70]. To this extent, the EGFR is no exception: the EGF-engaged EGFRs that are localized in LRs are more tyrosine phosphorylated than EGFRs in whole endosomes. Endosomal LRs recruit highly Tyr-phosphorylated EGFR along with various signaling proteins, including Grb-2, Shc, and c-Src, indicating a likely role for this compartment in signal transduction[24]. According to Teis et al[25], targeting of the MP1-ERK1/2 complex to late endosomes during EGF-mediated ERK activation depends on the adaptor protein; further, p14-MP1-ERK1/2 complex formation is needed for EGF-induced ERK activation at later stages of this process. Thus, it seems plausible that intracellular LRs target the ubiquitinated PY-EGFR/Grb2/Shc complex to the cytoplasmic face of the late endosomes for specific activation of ERK1/2. If this theory holds true, the ubiquitinated EGFRs should be later sorted into the intraluminal vesicles of late endosomes before their degradation or may be recycled back to the PM. This hypothesis was in part confirmed by data from Balbis et al[24] and by Lai et al[26], thus placing the LRs among the key players in ensuring efficient EGF/EGFR function. The possibility that this LR-dependent mechanism can be exploited is valid, because some of the widely-used drugs can be employed for this purpose. For example, heparin can suppress LR-mediated signaling and ligand-independent EGF receptor activation[71]. The detailed role of LR-mediated EGF/EGFR function in liver diseases remains to be determined.
Angiotensin II (AT) engages and initiates angiotensin AT1 receptor (AT1) signaling which is involved in cell growth and mitogenesis[72]. At least in C9 liver cells, Ang II-stimulation involves LR-mediated activation of ERK1/2[73]. Furthermore, Yin et al[74] reported that in angiotensin-stimulated C9 cells the cholesterol-rich LR domains mediate the actions of early upstream signaling molecules such as Src kinases and intracellular Ca2+ and that LR resident caveolin-1 has a scaffolding role in this process. Angiotensin causes caveolin-1 phosphorylation that is in turn regulated by intracellular Ca2+ and Src, thus indicating reciprocal interactions between LRs, caveolin-1, Src kinases, and intracellular Ca2+ through the AT1[74].
Insulin is an anabolic hormone with a role in carbohydrate and lipid metabolism and cell growth. The IR is a transmembrane tyrosine kinase that binds insulin with its two extracellular α-subunits and transmits signals via its two β-subunits that contain the tyrosine kinase domain; the receptor is activated by autophosphorylations. LRs ensure the initial steps of IR activation[24,75,76]. IR β subunits require palmitoylation for proper function[75]; however, regardless of its palmitoylation status, the unoccupied IR has low affinity to LRs[76]. In adipose or muscle tissue, IR needs to partner with caveolin-1 for function. In the liver, the autophosphorylation of the insulin engaged-IR still takes place in the LRs but can occur with[24] or without[76] caveolin participation. In the latter context, glycophospholipid clustering inhibits IR phosphorylation and IR is excluded from the LRs when the latter are more rigid[76]. These results suggest that LRs offer an additional level of control over IR function in the liver and support the hope that manipulation of LRs could modulate IR activity and thus liver metabolism.
LR role in bile formation/secretion: Bile production is one of the basic functions and an organ-specific signature of the liver. ABC transporters are located in the canalicular membrane of hepatocytes and are critical players in bile formation and detoxification. ABC is a family that includes P-glycoprotein (MDR1) for organic cations; MDR2 for phosphatidylcholine translocation; P-glycoprotein-related protein acting as bile salt export pump; and MRP2 (or cMOAT) for non-bile acid organic anions[51]. ABC transporters are located in LRs of the hepatocyte cellular membrane and mediate the transport of the majority of lipids secreted into the bile[77].
The canalicular PM is constantly exposed to bile acids, which act as detergents. Once secreted into bile canaliculi, bile salts extract phosphatidylcholine from the outer leaflet of the cellular membrane and incorporate it into mixed micelles. The bile preferentially extracts phosphatidylcholine; the latter constitutes only about 35% of canalicular phospholipids in the context of a relative abundance of sphingomyelin, thus the bile threatens the well-being of healthy cells. During evolution, a protective mechanism was developed in all bile-exposed cells to prevent self-solubilization with own bile by means of expressing a combination of distinct LRs that have unique lipid composition and protein content. Ismair et al[35] reported the existence of at least two such LR entities on the canalicular side of the hepatocyte PM. One of these is rich in caveolin-1, contains the majority of canalicular cholesterol and phospholipids, portions of the marker enzymes APN and DDPIV, and a large portion of all known ABC transporters including ABCG5, BSEP, MRP2, MDR2, and MDR1; this LR is Lubrol-soluble. In contrast, Triton-soluble LRs are associated with reggie-1/2 proteins and sphingomyelin; they contain a minor fraction of canalicular cholesterol, APN, DDPIV and MDR1/2 ABC transporters[35]. The exact purpose of such differential expression of ABC transporters in distinct LRs is not fully understood; furthermore, their distribution in LRs in steady-state vs activated state is largely unknown. However, several liver diseases are linked to ABC defects; for example, recessively inherited hepatobiliary phenotype is related to mutations in ABC transporter genes; defects in ABCB11 and MDR3 lead to familial intrahepatic cholestasis types 2 and 3, respectively; Dubin Johnson syndrome is associated with defects in MRP2 produced, and sitosterolemia with defects in ABCG5 or ABCG8[51]. It is also known that an altered secretory process of biliary cholesterol is associated with elevated hepatic cholesterol levels[78], thus suggesting the possibility that low membrane fluidity due to stabilization with cholesterol could provide an additional layer of control of ABC transporter function. It remains to be investigated whether the increased rigidity of LRs, which occurs when cholesterol content in the cell increases[15,16], may supplement the impairment of bile secretion in real-life liver diseases in addition to functional impairment of ABC transporters per se.
LRs in KCs/monocytes
KCs are active immune players and participants in a wide variety of liver diseases. The role of the LR in KCs is currently unknown, in part due to the scarcity of primary KCs and difficulties with their isolation. However, taking into account that KCs are tissue macrophages (Mf), several key findings about the role of LR in other types of tissue Mf could be extrapolated to KCs.
Inflammation occurs in a diverse array of liver diseases and is highly dependent on Mf. In Mf, the key molecules involved in pathogen recognition from exogenous danger signals either reside (CD14) or are recruited [Toll-like receptor (TLR)2, TLR4] to the LRs upon ligand engagement[79,80]; the function of pathogen recognition is thus highly dependent on LRs and suggests that LR modulation may be a candidate for managing the macrophages. Indeed, exposure to acute alcohol renders Mf temporarily insensitive to TLR4/CD14 ligands in a LR-dependent manner[81,82]. Similar to alcohol, selective modulation of fat content in LRs by macrophage-specific ABC transporter A1 also dampens inflammation by reducing MyD88-dependent TLRs trafficking to LRs[83]. Furthermore, peritoneal macrophages from dyslipidemic mice are primed for more robust TLR responses, reflecting increased LRs and increased TLR4 expression[84]. In the same dyslipidemic mice, the Mf from the lung airspace, in which cholesterol is maintained as constant during dyslipidemia, have normal responses and normal composition of LRs[84]. It is important to note that LRs also drive the Mf response to endogenous danger signals, such as those coming from dead cells. In this context, necrotic but not apoptotic cells co-localize with LRs within engulfing Mf. Interestingly, necrotic cell-induced secretion of tumor necrosis factor (TNF)-α and interleukin (IL)-1β by Mf is susceptible to LR destruction, suggesting a role for LRs in the signaling of necrosis-driven inflammatory response[85].
Related to the role of liver in the iron cycle, the ability of Mf to capture/store iron is highly dependent on the LRs. Expression of the iron exporter ferroportin at the PM of Mf is enhanced by iron loading and is decreased by hepcidin[86]. Macrophage ferroportin is preferentially located in caveolin/flotillin 1-enriched LRs; iron overload strongly increases the presence of ferroportin in the LRs, while LR destruction decreases hepcidin activity on macrophage ferroportin[86]. Collectively, these data support the idea that LRs participate in several key Mf functions that are key for liver homeostasis.
LRs in SCs
The SCs store retinol and are the main cellular source of collagen and other extracellular matrix substances in normal as well as fibrotic livers. The LR composition, and their distribution and function in primary SCs are largely unknown, mainly due to limited numbers of SCs isolated from the normal liver and extreme technical difficulties of their isolation from the fibrotic liver. Andrade et al[87] employed the murine hepatic SC line GRX, which expresses the myofibroblast phenotype at baseline and can be induced in vitro to display the fat-storing phenotype (lipocytes), to show that total ganglioside content and GM2 synthase activity were lower in myofibroblasts compared to lipocytes. Both SC phenotypes presented similar content of gangliosides GM2, GM1, and GD1a, as well as their precursor GM3. Sphingomyelin and all the gangliosides were expressed as doublets; their ratio is increased in retinol-induced lipocytes due to increased content of long-chain fatty acids[87]. Taken together, these results indicated that myofibroblasts and lipocytes can use distinct ceramide pools for sphingolipid synthesis. Differential ganglioside expression and presence of long-chain saturated fatty acids suggested that these components could participate in the formation of LRs with specific functions in the two phenotypes of GRX-SCs[87].
Anandamide (AEA) is an amide of arachidonic acid and ethanolamine with endogenous endocannabinoid function that engages cannabinoid and other yet unknown receptors, and exerts a variety of physiological and pharmacological effects in chronic liver diseases[87]. Yang et al[88] employed the hepatic SC line T6 and reported that moderate AEA amounts inhibited hepatic SC proliferation and high-dose AEA caused hepatic SC death; cell death was necrotic rather than apoptotic and occurred independently of cannabinoid receptors. More importantly, AEA-mediated death in hepatic SCs was dependent on the cholesterol content of the membrane LRs, the fatty acid composition of the membrane, and the function of PI3K/protein kinase B signaling pathway[87]. These data gave support to speculations that AEA may be a potential antifibrogenic drug in the treatment of liver fibrosis in a LR-dependent manner.
Sonic hedgehog (Shh) is an embryonic morphogen that is key in cell proliferation, differentiation, and morphological patterning during embryogenesis; the Shh signaling pathway also promotes maintenance of adult stem cells and is involved in tumorigenesis[89]. In the hepatic SC line HSC8B, Shh physically interacts with caveolin-1 within the LRs in the Golgi apparatus to form large protein complexes that are packaged as large punctuate structures (transport vesicles) and transported to the PM in an LR-dependent manner[90]. Collectively these data suggest that LR manipulation can have a significant impact on liver SCs.
LRs in endothelial cells
Liver sinusoidal endothelial cells (ECs) isolate and protect the hepatocytes from passing blood and play an important role in hepatic microcirculation. Microvascular exchange in the liver is governed by fenestrations in sinusoidal ECs and is key to proper liver function. One of the basic properties of liver endothelium is the fact that there is no basal lamina, thus allowing free passage of macromolecules up to medium-sized chylomicrons[91]. The fenestrae are surrounded by a dense ring of actin, whereas the sieve plates are formed by microtubules; both number and size of fenestrae can be regulated by a variety of processes that will impact on hepatic function. For example, loss of fenestrae or sinusoidal capillarization occurs in alcoholic liver disease (ALD) and cirrhosis, respectively[91,92]. While the details in the liver are unknown, in other vascular systems the ECs are heavily governed by the functionality of their LRs. Disruption of LRs in ECs causes loss of cell viability and altered cell morphology, including loss of fenestration[93,94]. LRs govern the function of EGFR, multi-drug resistance P-glycoprotein, and adhesion molecules in ECs, and are critical to a sound EC-gated vascular barrier, at least at the blood/brain interface[95-98]. LRs also house the NADPH oxidase components gp91, p22phox, and p47phox; several pro-inflammatory cytokines, such as TNF-α, employ a LR-dependent mechanism to trigger oxidative stress and eNOS production in ECs[99].
LRs in cholangiocytes
Cholangiocytes outline the intrahepatic bile ducts; they are of epithelial origin, share their common hepatoblast progenitor with the hepatocytes and, similar to them, are polarized cells[100]. The cholangiocytes function as regulators of ductal bile secretion; in addition, they absorb and secrete water, organic anions, organic cations, lipids, and electrolytes[101]. Cholangiocytes interact with the immune cells and are potent cytokine producers, thus playing a role in liver immune responses[100,101]. Several research groups have recently reported that polarized primary rat cholangiocytes express LRs[102,103]. McWilliams identified that Shank2E, which is an ankyrin repeat-rich multidomain scaffolder, is localized in the LRs of the apical surface of the cholangiocytes[103]. LRs not only host but are also vital for the function of Shank proteins, which involves coordination of the targeted delivery of the proteins to the apical membrane in actin-containing cytoskeleton-dependent fashion[103]. These novel findings point to the role of LRs in cholangiocyte function.
LRs in non-resident liver immune cells (dendritic cells, natural killer cells, lymphocytes)
At any given time healthy liver accommodates a wide variety of non-resident immune cells, including dendritic cells (DCs), natural killer (NK) cells and lymphocytes; selective recruitment and retention of certain immune populations occurs during diverse liver diseases and these cells play a critical role in development and resolution of liver inflammation, remodeling and injury[2]. All immune cells have LRs as components of their cellular membranes; more importantly, LRs participate in some of the key functions of the immune cells.
DCs recognize, engulf, process and present antigens to other immune cells while producing a wide array of immune-modulating factors, including cytokines, chemokines, and metabolites, to control the immune responses. LRs provide the signaling platforms for a variety of DC receptors, including TLRs, major histocompatibility complex molecules, and co-stimulatory molecules; disruption of LRs significantly impairs the functional capacity of DCs[104-106]. More recently, Wang et al[107] reported that high-density lipoprotein (HDL) promotes reverse cholesterol transport and is protective against dyslipidemia and atherosclerosis. Further, they reported that HDL and apolipoprotein A-I promoted tolerance and inhibited immune responses by inhibiting the ability of antigen presenting cells, and DCs in particular, to stimulate T cells in a cholesterol-dependent manner[107]. HDL-induced cholesterol efflux from cells alters their LR structure, which in turn activates the TNF-α converting enzyme ADAM17-dependent processing of transmembrane substrates[108]. These findings suggest that LRs may play a role in HDL-induced DC impairment and further regulate the inflammatory processes; these authors also suggested that modulation of LRs in DCs could provide a desirable approach to inducing immune tolerance[108].
NK cells link innate and adaptive immunity via the production of cytokines and have the ability to kill/lyse infected non-malignant and tumor cells. Unlike other immune cells, NKs are activated and inhibited by separate sets of receptors which ensure their rapid initiation and prompt silencing to promote immune response without autoimmune reactions. LRs are implicated in both activating and limiting steps of NK function. Upon CD2 cross-linking or target cell binding, the NK-activating receptors aggregate in the LRs, which further leads to the formation of complexes of LAT with PI3K and PLC-γ1 which are essential for the NK lytic mechanisms[109]. Moreover, NK cell cytotoxicity was found to be closely related to total plasma cholesterol concentration in humans[110]. Further, colocalization of the IL-12 receptor and FcγRIIIa to LRs leads to activation of ERK and enhanced production of interferon-γ by NKs[111]. Engagement of inhibitory receptors by HLA class I on target cells blocks phosphorylation of 2B4 receptor which is found exclusively in LRs. CD94/NKG2A is an ITIM-containing inhibitory receptor expressed by NK cells that recognizes HLA-E; the engagement of this receptor prevents NK cell activation by disruption of the actin network and exclusion of LRs from the point of contact with its ligand. The latter structure is an inhibitory NK cell immunological synapse (iNKIS) and is key to NK function. Thus, targeted LR exclusion from the iNKIS is an active process that aims to maintain LRs outside the inhibitory synapse[112,113]. These data suggest that LRs are actively engaged in dousing the NK activity. However, the DCs and NK cells work closely together; in the reverse order of events, activation of resting NK cells by mature DCs is important at the initiation phases of immune responses; more importantly, DC/NK cross-talk is dependent on CX3CL1, intact cytoskeleton and LRs[114].
Lymphocytes are classified into T and B cells, and further differentiated in diverse subpopulations depending on their abilities to produce certain cytokines or antibodies, respectively.
In T-lymphocytes, LRs are implicated in signaling from the T-cell antigen receptor (TCR) and in localization and function of proteins recruited/activated downstream from the receptor. Statins (inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase) block cholesterol biosynthesis and reduce the pathogenesis of classical T-cell-inducing damage in experimental autoimmune encephalomyelitis by interfering with leukocyte recruitment, transmigration through vascular barriers and their adhesion, and ultimately limiting T-cell activation, as reviewed by Weber et al[115]. Polyunsaturated fatty acids (PUFAs) intercalate and thus remodel LRs; treatment of TCR-stimulated T-lymphocytes with PUFAs leads to miss-localization of LR-anchored TCR adaptor LAT, reduction in LAT tyrosine phosphorylation and low IL-2 production[116]. PUFAs inhibit the formation of the immune synapse[117]; it remains to be determined if this is due to isolated effects of PUFA on LRs of T cells, on DCs, or on both. Exposure of T cells to sialidases, which are able to hydrolyze the non-reducing terminal sialic acid linkage, led to control of LR-associated glycosphingolipid content and influenced activation in T-lymphocytes. Furthermore, sialidase inhibitor oseltamivir (Tamiflu) down-regulated the expression of LR-resident GM1 on the surface of T-cells and reduced cytokine production in activated T-cells[118,119]. These results suggest that LR-dependent modulation of T cells has translational potential.
In B lymphocytes, B-cell depleting anti-CD20 antibodies, namely rituximab, induced translocation of CD20 to the membrane LR fraction and triggered cell apoptosis; this process was prevented by LR disruption[120,121]. While the detailed mechanisms of such LR-mediated cytotoxicity of malignant B cells is not well understood, it is known that in normal B cells, trafficking of internalized Ag/B-cell receptor (BCR) complexes to intracellular Ag-processing compartments is driven by ubiquitination of the cytoplasmic domain of the BCR. The ubiquitinated Ag/BCR complexes are formed via a signaling-dependent mechanism and restricted to PM LRs[122]; the signaling from BCR is initiated only when the LR localization is accomplished. At this stage, Bright, which is a B-cell-restricted factor, forms complexes with Bruton’s tyrosine kinase (Btk) and its substrate transcription initiation factor-I (TFII-I), and acts to activate immunoglobulin heavy chain gene transcription in the nucleus[123]. In resting B cells, palmitoylated pool of Bright is diverted to LRs where it associates with signalosome components. After BCR ligation, Bright transiently interacts with sumoylation enzymes, blocks calcium flux and interferes with phosphorylation of Btk and TFII-I; Bright is then excluded from LRs as a Sumo-I-modified form. The remaining LR-associated Bright contributes to the signaling threshold of B cells: the sensitivity to BCR stimulation decreases as the levels of Bright increase[123]. Thus, LRs play a key role in governing B cell function.
IMPLICATIONS OF LRS IN LIVER DISEASES
Bacterial and viral diseases
Role of LRs in bacterial infections involving liver: Listeria monocytogenes (LM) causes severe liver disease in children, pregnant women and in immunocompromised individuals. LM proteins internalin and InIB bind E-cadherin (E-CAD) and HGFR, respectively; engagement of E-CAD and HGFR are sufficient for LM invasion into the host hepatocyte[124]. More importantly, intact host LRs are needed to complete the E-CAD/HGFR-mediated entry of LM[124,125].
Elevated intestinal permeability is implicated in the pathogenesis of a wide variety of diseases, including those of liver[126,127]. While the translocation of whole bacteria across the intact intestinal wall is unusual, the inflamed gut is permissive to bacterial-derived products, including endotoxin, which acts as TLR4 ligand and is considered a 2nd hit in the pathogenesis of several liver diseases, including non-alcoholic fatty liver disease and ALD[12,13,126,127]. In this context, it has been hypothesized that gut colonization plays a key role in the pathogenesis of liver diseases. Campylobacter species represent a risk factor for the development of inflammation in the GI tract via largely unknown mechanisms. Kalischuk et al[128] reported that Campylobacter jejuni (C. jejuni) induced translocation of commensal intestinal bacteria to the liver of infected mice. In vitro Campylobacter-induced internalization and translocation of Escherichia coli (E. coli) occurred via a transcellular pathway without increasing epithelial permeability; this process was blocked by cholesterol depletion and thus LR impairment[128]. Invasion-defective mutants and Campylobacter-conditioned cell culture medium also favored E. coli translocation, indicating that C. jejuni does not directly “shuttle” other bacteria into enterocytes. In C. jejuni-treated epithelial monolayers, translocating E. coli was associated with LRs and this phenomenon was blocked by cholesterol depletion[128]. However, translocation of commensals does not require the presence of active infection with pathogens at the intestinal epithelial border. Clark et al[129] reported that interferon (IFN)-γ influences the epithelium to mediate transcellular translocation of E. coli C25; this process required intact LRs. These data suggest that intestinal LRs are key to establishing leaky gut, which in turn plays a role in the pathogenesis of liver diseases; it remains to be identified whether liver infection with translocated commensal intestinal bacteria is mediated by the LRs in hepatocytes.
Role of LRs in viral infections of liver: (1) Hepatitis C virus (HCV). The lifecycle of HCV is dependent on the integrity of LRs. Using a subgenomic HCV replicon system, Aizaki et al[130] showed that HCV RNA synthesis occurs in LRs. HCV replication complex is highly dependent on the abundance of cholesterol and it is protected within LRs; only LRs that contain both non-structural proteins and viral RNA were capable of performing HCV RNA synthesis using the endogenous HCV RNA template, while depletion of cellular cholesterol selectively reduced HCV RNA replication[130]. However, the virus has preferences for specific types of LRs. Core protein, for example, does not colocalize with classical PM LR markers, such as caveolin-1 and the B subunit of cholera toxin, suggesting that core protein is bound to cytoplasmic raft microdomains distinct from caveolin-based LRs[131]. Furthermore, while both the structural core and NS5A protein associate with membranes, they do not always colocalize in the LR. Finally, the ability of core protein to localize to the LRs does not require other elements of the HCV polyprotein[131]. These results suggest that the LR implications in HCV lifecycle are complex and require further investigation. Nevertheless, HCV takes over LR control in the host cells and leads to modification of host LR-resident proteome upon its replication[131]. Roughly 10% of proteins residing in LRs of HUH7 cells are modified by HCV presence[132]. Interestingly, the majority of the host proteins involved in HCV recognition/internalization/sensing[133] including CD81, claudins, TLR2, LDL-R, Scavenger Receptor type B, and DC-SIGN/L-SIGN reside in LRs[134-140]. It is thus plausible to foresee that LR modulation may have a place in anti-HCV therapy; the proof of this hypothesis is awaited; (2) Hepatitis B virus (HBV). Funk et al[141] identified that duck hepatitis B virus (DHBV) attaches predominantly to detergent-soluble LR domains on the PM, but that cholesterol depletion from host membranes and thus disruption of LRs does not affect DHBV infection. In contrast, depletion of cholesterol from the envelope of both DHBV and human HBV strongly reduces virus infectivity[141]. Cholesterol depletion increases the density of viral particles and leads to changes in the ultrastructural appearance of the virus envelope; the infectivity and density of viral particles were partially restored upon cholesterol replenishment. Binding and entry of cholesterol-deficient DHBV into hepatocytes were not significantly impaired, in contrast to their release from endosomes. The authors therefore concluded that viral, but not host cholesterol is required for endosomal escape of DHBV[141]. Bremer et al[142] did not confirm a role of LRs in viral binding, but identified that LRs are indispensable for the entry process of HBV and might be important for a later step in viral uptake, such as fusion in a yet-unknown compartment.
Cholesterol accumulation/storage diseases
Niemann-Pick type C disease (NPCD) is a lysosomal storage disorder that affects the neural system and viscera, including liver[143,144]. Defective trafficking of cholesterol, sphingolipids and fatty acids leading to endosomal cholesterol sequestration coupled to impaired cholesterol transport to PM and ER were identified as key in the pathogenesis of NPCD[145]. Sequestration of cholesterol/sphingolipid-rich LRs in the late endosomal compartment was also reported in NPCD[146,147]. Vainio et al[76] reported a significant perturbation of LR composition and LR-dependent signaling in NPCD livers. They also showed that the membrane of NPCD hepatocytes is stabilized with cholesterol, exhibits higher anisotropy and resides in a more ordered phase; i.e. it is less fluid and thus has higher ratio of raft/non-raft content, compared to normal hepatocytes. More importantly, these rigid LRs lead to increased expression and enrichment of IR in the membrane of NPCD hepatocytes. Further, IR redistribution was associated with its defective function, thus aggravating the metabolic syndrome in NPCD[76].
Alcohol-induced liver disease
Alcohol exposure is associated with a significant amount of ROS production, which leads to oxidative stress[148-156]. While the generation of alcohol-induced oxidative stress is well documented, the understanding of the effects of oxidative stress on different molecular systems is poor. Marquês et al[46] employed in situ AFM to show that low ethanol concentrations lead to a marked thinning of the fluid but not of the gel domains of the model membranes, due to water/bilayer interfacial tension variation and freezing point depression, induction of acyl chain disordering (including opening and looping), tilting, and interdigitation. These results suggested that ethanol influences the bilayer properties by altering the lateral organization of the membrane. Several groups have confirmed the pivotal role of membrane fluidity in ethanol-induced oxidative stress using both in vitro and in vivo models of alcohol exposure[150-156]; however, the role of LRs per se in this process is still under evaluated.
In primary rat hepatocytes, short-term alcohol exposure increases membrane fluidity and leads to ethanol-induced ROS generation, which interferes with mitochondria, ER, cytochrome P450, cytosolic free iron, and cytosolic enzymes such as xanthine oxidase or aldehyde oxidases[153,154,157]. More recently, it was appreciated that LRs play a pivotal role in ethanol-induced oxidative stress in hepatocytes[152]. Alcohol exposure modulates the LR composition of hepatocytes, causes spontaneous clustering of LRs due to elevation in membrane fluidity, and promotes the increase of low-molecular-weight iron intracellular content via the activation of a PI-PLC-dependent mechanism. Further, ethanol oxidizes the LR proteins, as indicated by the increased LR content of malondialdehyde-acetaldehyde (MDA) adduct, which is a secondary end product of the degradation of oxidized PUFAs that can diffuse from its production site to react with free amino groups in proteins and lipids. From the therapeutic point of view, thiourea and vitamin E pretreatment inhibited the alcohol-induced MDA adduct formation in LRs[152]. The effects of chronic alcohol exposure on LR function in hepatocytes are largely unknown.
Alcohol exposure affects the Shh signaling in an in vivo model of fetal alcohol syndrome in zebrafish[90]. Various cell function alterations due to changes in cell membrane composition in alcohol-induced fetal damage have also been described[15]. Mao et al[90] identified that alcohol does not significantly interrupt translation of Shh mRNA in ER or the trafficking of Shh from the ER to the Golgi apparatus in the SC line HSC8B. However, alcohol does prevent the entry of Shh into transport vesicles from Golgi to PM and specifically decreases the amount of caveolin-1/Shh complex found in LRs, causing cytoplasmic accumulation of Shh and leading to a deficiency of Shh ligand secretion into the extracellular matrix[90]. These data indicate that SC-mediated tissue remodeling upon alcohol exposure involves LRs.
In macrophages, and presumably KCs, acute alcohol exposure dampens the inflammatory response to pathogens via TLRs in a LR-dependent manner and involves downregulation of MAPK activity, low nuclear factor κB activity and impaired TNF-α production[81,82,158]. Such profound inhibitory effects could be envisioned as a protective measure; the effects of chronic alcohol exposure on LR function in Mf are largely unknown.
RAFTS AS THERAPEUTIC TARGETS
Development of new treatment strategies using low-toxicity high-efficiency chemotherapeutic agents is a forefront priority in research. Several novel approaches to therapeutic agents are based on LRs. In drug discovery, a viable strategy to block viral entry and its replication may incorporate the use of natural dietary and plant-derived compounds that target LRs; this strategy is based on the affinity of these products to cholesterol, as proposed in a recent review by Verma regarding HIV[159]. The nanoparticle-based drug-delivery approach for delivery of lipophilic substances to the target cell PM acts via lipid mixing and subsequent intracellular trafficking through LR-dependent processes[160]; the advantage of the latter strategy is in its ability to deliver therapeutics specifically to selected cell types, thus limiting general toxicity.
Regulation of cell death is yet another area influenced by LR modulation. Cell death occurs at low rate in normal tissue and stimulates tissue regeneration as part of normal organ lifecycle; when the tissue is malignant the cell death is deliberately desired. LRs ensure the connection between extrinsic and intrinsic apoptotic pathways[161,162], thus become an attractive therapeutic target. The Fas death receptor (CD95 or APO-1) delivers apoptotic signals through binding to its cognate ligand, FasL (CD95L). However, because of severe liver toxicity due to the high presence of Fas in hepatocytes, the putative clinical antitumor action of FasL cannot be accomplished for extra-hepatic tumors; the utility of this approach for liver tumors is yet to be defined. Recent evidence for FasL-independent activation of Fas suggests that the death receptor can also be activated intracellularly, in the absence of its ligand. According to Mollinedo et al[161], Fas-mediated apoptosis involves translocation of Fas - and downstream signaling molecules - into LRs, a process that can be pharmacologically modulated. FasL-independent clustering of Fas in membrane LRs generates high local concentrations of death receptor, providing scaffolds for coupling adaptor and effector proteins involved in Fas-mediated apoptosis. Thus, LRs act as the linchpin from which a potent death signal is launched and have become a new promising anticancer target[161-164]. The utility of this therapeutic approach has been explored in B cell malignancy[120,121,163] and seems plausible for other diseases.
Sakamoto et al[165] reported that a secondary fungal metabolite, NA255, which targets LRs, also inhibits HCV replication and suggested that the inhibition of sphingolipid metabolism and thus LR modulation may provide a new therapeutic strategy for treatment of HCV infection. Hirata showed that serine palmitoyltransferase (SerPT) inhibitor had the ability to favor the transport of HCV RNA-dependent RNA polymerase NS5B to LRs, thus facilitating binding of sphingomyelin to NS5B[166]. Further, the authors identified that the anti-HCV effect of SerPT inhibitor could be translated to in vivo systems using humanized chimeric mice: SerPT inhibitor led to a rapid decline in serum HCV-RNA of about 1-2 log within 8 d. Furthermore, combination therapy of SerPT inhibitor and PEG-IFN achieved about 3 log reduction in serum HCV-RNA[166]. Several research groups have reported that lipid metabolism could be a target in anti-HCV therapy[165-167]. Amemiya et al[167] used combination treatment with myriocin, a sphingomyelin synthesis inhibitor, and IFN, a pleiotropic cytokine, or myriocin and simvastatin, an inhibitor of cholesterol biosynthesis with pleiotropic effects owed to inhibition of prenylation, to show synergistically attenuated HCV replication. They also identified impaired replication of HCV-1b replicon and of JFH-1 strain of genotype 2a infectious HCV RNA in Huh7/Rep-Feo cells, upon treatment with either myriocin-based combination[167]. While encouraging, these data do not fully translate into human systems: O'Leary et al[168] recently reported that statins alone do not exhibit antiviral activity against HCV at conventional doses.
CONCLUSION
In conclusion, we have compiled the published evidence that LRs are present in all liver cells; more importantly, data suggest that LRs play a role in liver health and diseases. The LR area of liver physiology and pathology is understudied. In order to facilitate exploration of this area future improvements are needed, the foremost of which are listed below: (1) Better markers and better methodologies for LR research; (2) New drugs for LR modulation; and (3) Experimental data-supported evidence of the feasibility and outcomes of LR modulation in liver health and disease.
Footnotes
Supported by Grant AA016571 from NIAAA
Peer reviewer: Munechika Enjoji, MD, PhD, Department of Clinical Pharmacology, Fukuoka University, 8-17-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan
S- Editor Tian L L- Editor Logan S E- Editor Zheng XM
References
- 1.Arias IM, Alter HJ, Boyer JL, Cohen DE, Fausto N, Wolkoff AW. The Liver: Biology and Pathobiology. 5th ed. Malden, MA: Wiley-Blackwell; 2010. pp. 6–11. [Google Scholar]
- 2.Sheth K, Bankey P. The liver as an immune organ. Curr Opin Crit Care. 2001;7:99–104. doi: 10.1097/00075198-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Campbell DJ, Bouhnik J, Ménard J, Corvol P. Identity of angiotensinogen precursors of rat brain and liver. Nature. 1984;308:206–208. doi: 10.1038/308206a0. [DOI] [PubMed] [Google Scholar]
- 4.Shimada Y, Kato T, Ogami K, Horie K, Kokubo A, Kudo Y, Maeda E, Sohma Y, Akahori H, Kawamura K. Production of thrombopoietin (TPO) by rat hepatocytes and hepatoma cell lines. Exp Hematol. 1995;23:1388–1396. [PubMed] [Google Scholar]
- 5.Kjekshus H, Risoe C, Scholz T, Smiseth OA. Regulation of hepatic vascular volume: contributions from active and passive mechanisms during catecholamine and sodium nitroprusside infusion. Circulation. 1997;96:4415–4423. doi: 10.1161/01.cir.96.12.4415. [DOI] [PubMed] [Google Scholar]
- 6.Lamson PD. The part played by the liver tn the regulation of blood volume and red corpuscle concentration in acute physiological conditions. J Pharmacol Exp Ther September. 1920;16:125–134. [Google Scholar]
- 7.Kmieć Z. Cooperation of liver cells in health and disease. Adv Anat Embryol Cell Biol. 2001;161:III–XIII, 1-151. doi: 10.1007/978-3-642-56553-3. [DOI] [PubMed] [Google Scholar]
- 8.Kim WR, Brown RS, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 9. http://www.cdc.gov/nchs/fastats/liverdis.htm.
- 10.Brunt EM. Pathology of fatty liver disease. Mod Pathol. 2007;20 Suppl 1:S40–S48. doi: 10.1038/modpathol.3800680. [DOI] [PubMed] [Google Scholar]
- 11.Tsukamoto H, She H, Hazra S, Cheng J, Wang J. Fat paradox of steatohepatitis. J Gastroenterol Hepatol. 2008;23 Suppl 1:S104–S107. doi: 10.1111/j.1440-1746.2007.05294.x. [DOI] [PubMed] [Google Scholar]
- 12.Syn WK, Teaberry V, Choi SS, Diehl AM. Similarities and differences in the pathogenesis of alcoholic and nonalcoholic steatohepatitis. Semin Liver Dis. 2009;29:200–210. doi: 10.1055/s-0029-1214375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jou J, Choi SS, Diehl AM. Mechanisms of disease progression in nonalcoholic fatty liver disease. Semin Liver Dis. 2008;28:370–379. doi: 10.1055/s-0028-1091981. [DOI] [PubMed] [Google Scholar]
- 14.Bartosch B, Thimme R, Blum HE, Zoulim F. Hepatitis C virus-induced hepatocarcinogenesis. J Hepatol. 2009;51:810–820. doi: 10.1016/j.jhep.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Escribá PV, González-Ros JM, Goñi FM, Kinnunen PK, Vigh L, Sánchez-Magraner L, Fernández AM, Busquets X, Horváth I, Barceló-Coblijn G. Membranes: a meeting point for lipids, proteins and therapies. J Cell Mol Med. 2008;12:829–875. doi: 10.1111/j.1582-4934.2008.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singer SJ, Nicolson GL. The fluid mosaic model of the structure of cell membranes. Science. 1972;175:720–731. doi: 10.1126/science.175.4023.720. [DOI] [PubMed] [Google Scholar]
- 17.van Meer G, Voelker DR, Feigenson GW. Membrane lipids: where they are and how they behave. Nat Rev Mol Cell Biol. 2008;9:112–124. doi: 10.1038/nrm2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Engel A, Gaub HE. Structure and mechanics of membrane proteins. Annu Rev Biochem. 2008;77:127–148. doi: 10.1146/annurev.biochem.77.062706.154450. [DOI] [PubMed] [Google Scholar]
- 19.Simons K, Ikonen E. Functional rafts in cell membranes. Nature. 1997;387:569–572. doi: 10.1038/42408. [DOI] [PubMed] [Google Scholar]
- 20.Brown DA, London E. Structure and origin of ordered lipid domains in biological membranes. J Membr Biol. 1998;164:103–114. doi: 10.1007/s002329900397. [DOI] [PubMed] [Google Scholar]
- 21.Pike LJ. Rafts defined: a report on the Keystone Symposium on Lipid Rafts and Cell Function. J Lipid Res. 2006;47:1597–1598. doi: 10.1194/jlr.E600002-JLR200. [DOI] [PubMed] [Google Scholar]
- 22.Woudenberg J, Rembacz KP, Hoekstra M, Pellicoro A, van den Heuvel FA, Heegsma J, van Ijzendoorn SC, Holzinger A, Imanaka T, Moshage H, et al. Lipid rafts are essential for peroxisome biogenesis in HepG2 cells. Hepatology. 2010;52:623–633. doi: 10.1002/hep.23684. [DOI] [PubMed] [Google Scholar]
- 23.Kim KB, Lee JW, Lee CS, Kim BW, Choo HJ, Jung SY, Chi SG, Yoon YS, Yoon G, Ko YG. Oxidation-reduction respiratory chains and ATP synthase complex are localized in detergent-resistant lipid rafts. Proteomics. 2006;6:2444–2453. doi: 10.1002/pmic.200500574. [DOI] [PubMed] [Google Scholar]
- 24.Balbis A, Parmar A, Wang Y, Baquiran G, Posner BI. Compartmentalization of signaling-competent epidermal growth factor receptors in endosomes. Endocrinology. 2007;148:2944–2954. doi: 10.1210/en.2006-1674. [DOI] [PubMed] [Google Scholar]
- 25.Teis D, Wunderlich W, Huber LA. Localization of the MP1-MAPK scaffold complex to endosomes is mediated by p14 and required for signal transduction. Dev Cell. 2002;3:803–814. doi: 10.1016/s1534-5807(02)00364-7. [DOI] [PubMed] [Google Scholar]
- 26.Lai WH, Cameron PH, Wada I, Doherty JJ, Kay DG, Posner BI, Bergeron JJ. Ligand-mediated internalization, recycling, and downregulation of the epidermal growth factor receptor in vivo. J Cell Biol. 1989;109:2741–2749. doi: 10.1083/jcb.109.6.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.López D, Kolter R. Functional microdomains in bacterial membranes. Genes Dev. 2010;24:1893–1902. doi: 10.1101/gad.1945010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderton CR, Lou K, Weber PK, Hutcheon ID, Kraft ML. Correlated AFM and NanoSIMS imaging to probe cholesterol-induced changes in phase behavior and non-ideal mixing in ternary lipid membranes. Biochim Biophys Acta. 2011;1808:307–315. doi: 10.1016/j.bbamem.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 29.de Almeida RF, Loura LM, Prieto M. Membrane lipid domains and rafts: current applications of fluorescence lifetime spectroscopy and imaging. Chem Phys Lipids. 2009;157:61–77. doi: 10.1016/j.chemphyslip.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 30.Kiss E, Nagy P, Balogh A, Szöllosi J, Matkó J. Cytometry of raft and caveola membrane microdomains: from flow and imaging techniques to high throughput screening assays. Cytometry A. 2008;73:599–614. doi: 10.1002/cyto.a.20572. [DOI] [PubMed] [Google Scholar]
- 31.Sankaran J, Manna M, Guo L, Kraut R, Wohland T. Diffusion, transport, and cell membrane organization investigated by imaging fluorescence cross-correlation spectroscopy. Biophys J. 2009;97:2630–2639. doi: 10.1016/j.bpj.2009.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moertelmaier M, Brameshuber M, Linimeier M, Schütz GJ, Stockinger H. Thinning out clusters while conserving stoichiometry of labeling. Appl Phys Lett. 2005;87:263903. [Google Scholar]
- 33.Gaus K, Gratton E, Kable EP, Jones AS, Gelissen I, Kritharides L, Jessup W. Visualizing lipid structure and raft domains in living cells with two-photon microscopy. Proc Natl Acad Sci USA. 2003;100:15554–15559. doi: 10.1073/pnas.2534386100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown DA. Lipid rafts, detergent-resistant membranes, and raft targeting signals. Physiology (Bethesda) 2006;21:430–439. doi: 10.1152/physiol.00032.2006. [DOI] [PubMed] [Google Scholar]
- 35.Ismair MG, Häusler S, Stuermer CA, Guyot C, Meier PJ, Roth J, Stieger B. ABC-transporters are localized in caveolin-1-positive and reggie-1-negative and reggie-2-negative microdomains of the canalicular membrane in rat hepatocytes. Hepatology. 2009;49:1673–1682. doi: 10.1002/hep.22807. [DOI] [PubMed] [Google Scholar]
- 36.Bae TJ, Kim MS, Kim JW, Kim BW, Choo HJ, Lee JW, Kim KB, Lee CS, Kim JH, Chang SY, et al. Lipid raft proteome reveals ATP synthase complex in the cell surface. Proteomics. 2004;4:3536–3548. doi: 10.1002/pmic.200400952. [DOI] [PubMed] [Google Scholar]
- 37.Mazzone A, Tietz P, Jefferson J, Pagano R, LaRusso NF. Isolation and characterization of lipid microdomains from apical and basolateral plasma membranes of rat hepatocytes. Hepatology. 2006;43:287–296. doi: 10.1002/hep.21039. [DOI] [PubMed] [Google Scholar]
- 38.Zhang L, Xie J, Wang X, Liu X, Tang X, Cao R, Hu W, Nie S, Fan C, Liang S. Proteomic analysis of mouse liver plasma membrane: use of differential extraction to enrich hydrophobic membrane proteins. Proteomics. 2005;5:4510–4524. doi: 10.1002/pmic.200401318. [DOI] [PubMed] [Google Scholar]
- 39.He J, Liu Y, He S, Wang Q, Pu H, Ji J. Proteomic analysis of a membrane skeleton fraction from human liver. J Proteome Res. 2007;6:3509–3518. doi: 10.1021/pr070197v. [DOI] [PubMed] [Google Scholar]
- 40.Sarnataro D, Campana V, Paladino S, Stornaiuolo M, Nitsch L, Zurzolo C. PrP(C) association with lipid rafts in the early secretory pathway stabilizes its cellular conformation. Mol Biol Cell. 2004;15:4031–4042. doi: 10.1091/mbc.E03-05-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li C, Duan W, Yang F, Zhang X. Caveolin-3-anchored microdomains at the rabbit sarcoplasmic reticulum membranes. Biochem Biophys Res Commun. 2006;344:1135–1140. doi: 10.1016/j.bbrc.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 42.Gautam A, Ng OC, Boyer JL. Isolated rat hepatocyte couplets in short-term culture: structural characteristics and plasma membrane reorganization. Hepatology. 1987;7:216–223. doi: 10.1002/hep.1840070203. [DOI] [PubMed] [Google Scholar]
- 43.Mattson MP. Dietary modulation of lipid rafts implications for disease prevention and treatment. In: Mattson MP, editor. Membrane microdomain signaling. Totowa, NJ: Humana Press Inc; 2005. pp. 191–201. [Google Scholar]
- 44.Chansrichavala P, Chantharaksri U, Sritara P, Ngaosuwankul N, Chaiyaroj SC. Atorvastatin affects TLR4 clustering via lipid raft modulation. Int Immunopharmacol. 2010;10:892–899. doi: 10.1016/j.intimp.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 45.Jacobson K, Mouritsen OG, Anderson RG. Lipid rafts: at a crossroad between cell biology and physics. Nat Cell Biol. 2007;9:7–14. doi: 10.1038/ncb0107-7. [DOI] [PubMed] [Google Scholar]
- 46.Marquês JT, Viana AS, De Almeida RF. Ethanol effects on binary and ternary supported lipid bilayers with gel/fluid domains and lipid rafts. Biochim Biophys Acta. 2011;1808:405–414. doi: 10.1016/j.bbamem.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 47.Zegers MM, Hoekstra D. Mechanisms and functional features of polarized membrane traffic in epithelial and hepatic cells. Biochem J. 1998;336(Pt 2):257–269. doi: 10.1042/bj3360257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brown DA, Crise B, Rose JK. Mechanism of membrane anchoring affects polarized expression of two proteins in MDCK cells. Science. 1989;245:1499–1501. doi: 10.1126/science.2571189. [DOI] [PubMed] [Google Scholar]
- 49.Matter K, Mellman I. Mechanisms of cell polarity: sorting and transport in epithelial cells. Curr Opin Cell Biol. 1994;6:545–554. doi: 10.1016/0955-0674(94)90075-2. [DOI] [PubMed] [Google Scholar]
- 50.Rodriguez-Boulan E, Powell SK. Polarity of epithelial and neuronal cells. Annu Rev Cell Biol. 1992;8:395–427. doi: 10.1146/annurev.cb.08.110192.002143. [DOI] [PubMed] [Google Scholar]
- 51.Kipp H, Arias IM. Intracellular trafficking and regulation of canalicular ATP-binding cassette transporters. Semin Liver Dis. 2000;20:339–351. doi: 10.1055/s-2000-9388. [DOI] [PubMed] [Google Scholar]
- 52.Nelson WJ, Yeaman C. Protein trafficking in the exocytic pathway of polarized epithelial cells. Trends Cell Biol. 2001;11:483–486. doi: 10.1016/s0962-8924(01)02145-6. [DOI] [PubMed] [Google Scholar]
- 53.Hoekstra D, Maier O, van der Wouden JM, Slimane TA, van IJzendoorn SC. Membrane dynamics and cell polarity: the role of sphingolipids. J Lipid Res. 2003;44:869–877. doi: 10.1194/jlr.R300003-JLR200. [DOI] [PubMed] [Google Scholar]
- 54.Nyasae LK, Hubbard AL, Tuma PL. Transcytotic efflux from early endosomes is dependent on cholesterol and glycosphingolipids in polarized hepatic cells. Mol Biol Cell. 2003;14:2689–2705. doi: 10.1091/mbc.E02-12-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slimane TA, Trugnan G, Van IJzendoorn SC, Hoekstra D. Raft-mediated trafficking of apical resident proteins occurs in both direct and transcytotic pathways in polarized hepatic cells: role of distinct lipid microdomains. Mol Biol Cell. 2003;14:611–624. doi: 10.1091/mbc.E02-08-0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hirata K, Pusl T, O’Neill AF, Dranoff JA, Nathanson MH. The type II inositol 1,4,5-trisphosphate receptor can trigger Ca2+ waves in rat hepatocytes. Gastroenterology. 2002;122:1088–1100. doi: 10.1053/gast.2002.32363. [DOI] [PubMed] [Google Scholar]
- 57.Nagata J, Guerra MT, Shugrue CA, Gomes DA, Nagata N, Nathanson MH. Lipid rafts establish calcium waves in hepatocytes. Gastroenterology. 2007;133:256–267. doi: 10.1053/j.gastro.2007.03.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hirata K, Dufour JF, Shibao K, Knickelbein R, O’Neill AF, Bode HP, Cassio D, St-Pierre MV, Larusso NF, Leite MF, et al. Regulation of Ca(2+) signaling in rat bile duct epithelia by inositol 1,4,5-trisphosphate receptor isoforms. Hepatology. 2002;36:284–296. doi: 10.1053/jhep.2002.34432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nathanson MH, Fallon MB, Padfield PJ, Maranto AR. Localization of the type 3 inositol 1,4,5-trisphosphate receptor in the Ca2+ wave trigger zone of pancreatic acinar cells. J Biol Chem. 1994;269:4693–4696. [PubMed] [Google Scholar]
- 60.Kasai H, Li YX, Miyashita Y. Subcellular distribution of Ca2+ release channels underlying Ca2+ waves and oscillations in exocrine pancreas. Cell. 1993;74:669–677. doi: 10.1016/0092-8674(93)90514-q. [DOI] [PubMed] [Google Scholar]
- 61.Shibao K, Hirata K, Robert ME, Nathanson MH. Loss of inositol 1,4,5-trisphosphate receptors from bile duct epithelia is a common event in cholestasis. Gastroenterology. 2003;125:1175–1187. doi: 10.1016/s0016-5085(03)01201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kanda H, Tajima H, Lee GH, Nomura K, Ohtake K, Matsumoto K, Nakamura T, Kitagawa T. Hepatocyte growth factor transforms immortalized mouse liver epithelial cells. Oncogene. 1993;8:3047–3053. [PubMed] [Google Scholar]
- 63.Baillat G, Siret C, Delamarre E, Luis J. Early adhesion induces interaction of FAK and Fyn in lipid domains and activates raft-dependent Akt signaling in SW480 colon cancer cells. Biochim Biophys Acta. 2008;1783:2323–2331. doi: 10.1016/j.bbamcr.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 64.Biedi C, Panetta D, Segat D, Cordera R, Maggi D. Specificity of insulin-like growth factor I and insulin on Shc phosphorylation and Grb2 recruitment in caveolae. Endocrinology. 2003;144:5497–5503. doi: 10.1210/en.2003-0417. [DOI] [PubMed] [Google Scholar]
- 65.Singleton PA, Salgia R, Moreno-Vinasco L, Moitra J, Sammani S, Mirzapoiazova T, Garcia JG. CD44 regulates hepatocyte growth factor-mediated vascular integrity. Role of c-Met, Tiam1/Rac1, dynamin 2, and cortactin. J Biol Chem. 2007;282:30643–30657. doi: 10.1074/jbc.M702573200. [DOI] [PubMed] [Google Scholar]
- 66.Ruff-Jamison S, Zhong Z, Wen Z, Chen K, Darnell JE, Cohen S. Epidermal growth factor and lipopolysaccharide activate Stat3 transcription factor in mouse liver. J Biol Chem. 1994;269:21933–21935. [PubMed] [Google Scholar]
- 67.Kömüves LG, Feren A, Jones AL, Fodor E. Expression of epidermal growth factor and its receptor in cirrhotic liver disease. J Histochem Cytochem. 2000;48:821–830. doi: 10.1177/002215540004800610. [DOI] [PubMed] [Google Scholar]
- 68.Mullhaupt B, Feren A, Fodor E, Jones A. Liver expression of epidermal growth factor RNA. Rapid increases in immediate-early phase of liver regeneration. J Biol Chem. 1994;269:19667–19670. [PubMed] [Google Scholar]
- 69.Marmor MD, Yarden Y. Role of protein ubiquitylation in regulating endocytosis of receptor tyrosine kinases. Oncogene. 2004;23:2057–2070. doi: 10.1038/sj.onc.1207390. [DOI] [PubMed] [Google Scholar]
- 70.Sigismund S, Woelk T, Puri C, Maspero E, Tacchetti C, Transidico P, Di Fiore PP, Polo S. Clathrin-independent endocytosis of ubiquitinated cargos. Proc Natl Acad Sci U S A. 2005;102:2760–2765. doi: 10.1073/pnas.0409817102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu YT, Song L, Templeton DM. Heparin suppresses lipid raft-mediated signaling and ligand-independent EGF receptor activation. J Cell Physiol. 2007;211:205–212. doi: 10.1002/jcp.20924. [DOI] [PubMed] [Google Scholar]
- 72.de Gasparo M, Catt KJ, Inagami T, Wright JW, Unger T. International union of pharmacology. XXIII. The angiotensin II receptors. Pharmacol Rev. 2000;52:415–472. [PubMed] [Google Scholar]
- 73.Olivares-Reyes JA, Shah BH, Hernández-Aranda J, García-Caballero A, Farshori MP, García-Sáinz JA, Catt KJ. Agonist-induced interactions between angiotensin AT1 and epidermal growth factor receptors. Mol Pharmacol. 2005;68:356–364. doi: 10.1124/mol.104.010637. [DOI] [PubMed] [Google Scholar]
- 74.Yin X, Li B, Chen H, Catt KJ. Differential signaling pathways in angiotensin II- and epidermal growth factor-stimulated hepatic C9 cells. Mol Pharmacol. 2008;74:1223–1233. doi: 10.1124/mol.108.048504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hedo JA, Collier E, Watkinson A. Myristyl and palmityl acylation of the insulin receptor. J Biol Chem. 1987;262:954–957. [PubMed] [Google Scholar]
- 76.Vainio S, Heino S, Mansson JE, Fredman P, Kuismanen E, Vaarala O, Ikonen E. Dynamic association of human insulin receptor with lipid rafts in cells lacking caveolae. EMBO Rep. 2002;3:95–100. doi: 10.1093/embo-reports/kvf010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tietz P, Jefferson J, Pagano R, Larusso NF. Membrane microdomains in hepatocytes: potential target areas for proteins involved in canalicular bile secretion. J Lipid Res. 2005;46:1426–1432. doi: 10.1194/jlr.M400412-JLR200. [DOI] [PubMed] [Google Scholar]
- 78.Voshol PJ, Koopen NR, de Vree JM, Havinga R, Princen HM, Elferink RP, Groen AK, Kuipers F. Dietary cholesterol does not normalize low plasma cholesterol levels but induces hyperbilirubinemia and hypercholanemia in Mdr2 P-glycoprotein-deficient mice. J Hepatol. 2001;34:202–209. doi: 10.1016/s0168-8278(00)00021-0. [DOI] [PubMed] [Google Scholar]
- 79.Schmitz G, Grandl M. Role of redox regulation and lipid rafts in macrophages during Ox-LDL-mediated foam cell formation. Antioxid Redox Signal. 2007;9:1499–1518. doi: 10.1089/ars.2007.1663. [DOI] [PubMed] [Google Scholar]
- 80.Schmitz G, Orsó E. CD14 signalling in lipid rafts: new ligands and co-receptors. Curr Opin Lipidol. 2002;13:513–521. doi: 10.1097/00041433-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 81.Dolganiuc A, Bakis G, Kodys K, Mandrekar P, Szabo G. Acute ethanol treatment modulates Toll-like receptor-4 association with lipid rafts. Alcohol Clin Exp Res. 2006;30:76–85. doi: 10.1111/j.1530-0277.2006.00003.x. [DOI] [PubMed] [Google Scholar]
- 82.Dai Q, Zhang J, Pruett SB. Ethanol alters cellular activation and CD14 partitioning in lipid rafts. Biochem Biophys Res Commun. 2005;332:37–42. doi: 10.1016/j.bbrc.2005.04.088. [DOI] [PubMed] [Google Scholar]
- 83.Zhu X, Owen JS, Wilson MD, Li H, Griffiths GL, Thomas MJ, Hiltbold EM, Fessler MB, Parks JS. Macrophage ABCA1 reduces MyD88-dependent Toll-like receptor trafficking to lipid rafts by reduction of lipid raft cholesterol. J Lipid Res. 2010;51:3196–3206. doi: 10.1194/jlr.M006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Madenspacher JH, Draper DW, Smoak KA, Li H, Griffiths GL, Suratt BT, Wilson MD, Rudel LL, Fessler MB. Dyslipidemia induces opposing effects on intrapulmonary and extrapulmonary host defense through divergent TLR response phenotypes. J Immunol. 2010;185:1660–1669. doi: 10.4049/jimmunol.0903501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Acosta-Pérez G, Maximina Bertha Moreno-Altamirano M, Rodríguez-Luna G, Javier Sánchez-Garcia F. Differential dependence of the ingestion of necrotic cells and TNF-alpha / IL-1beta production by murine macrophages on lipid rafts. Scand J Immunol. 2008;68:423–429. doi: 10.1111/j.1365-3083.2008.02155.x. [DOI] [PubMed] [Google Scholar]
- 86.Auriac A, Willemetz A, Canonne-Hergaux F. Lipid raft-dependent endocytosis: a new route for hepcidin-mediated regulation of ferroportin in macrophages. Haematologica. 2010;95:1269–1277. doi: 10.3324/haematol.2009.019992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Andrade CM, Trindade VM, Cardoso CC, Ziulkoski AL, Trugo LC, Guaragna RM, Borojevic R, Guma FC. Changes of sphingolipid species in the phenotype conversion from myofibroblasts to lipocytes in hepatic stellate cells. J Cell Biochem. 2003;88:533–544. doi: 10.1002/jcb.10373. [DOI] [PubMed] [Google Scholar]
- 88.Yang Q, Liu HY, Zhang YW, Wu WJ, Tang WX. Anandamide induces cell death through lipid rafts in hepatic stellate cells. J Gastroenterol Hepatol. 2010;25:991–1001. doi: 10.1111/j.1440-1746.2009.06122.x. [DOI] [PubMed] [Google Scholar]
- 89.Huang S, He J, Zhang X, Bian Y, Yang L, Xie G, Zhang K, Tang W, Stelter AA, Wang Q, et al. Activation of the hedgehog pathway in human hepatocellular carcinomas. Carcinogenesis. 2006;27:1334–1340. doi: 10.1093/carcin/bgi378. [DOI] [PubMed] [Google Scholar]
- 90.Mao H, Diehl AM, Li YX. Sonic hedgehog ligand partners with caveolin-1 for intracellular transport. Lab Invest. 2009;89:290–300. doi: 10.1038/labinvest.2008.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reichen J. The Role of the Sinusoidal Endothelium in Liver Function. News Physiol Sci. 1999;14:117–121. doi: 10.1152/physiologyonline.1999.14.3.117. [DOI] [PubMed] [Google Scholar]
- 92.Tsukamoto H, Lu SC. Current concepts in the pathogenesis of alcoholic liver injury. FASEB J. 2001;15:1335–1349. doi: 10.1096/fj.00-0650rev. [DOI] [PubMed] [Google Scholar]
- 93.Kline MA, O'Connor Butler ES, Hinzey A, Sliman S, Kotha SR, Marsh CB, Uppu RM, Parinandi NL. A simple method for effective and safe removal of membrane cholesterol from lipid rafts in vascular endothelial cells: implications in oxidant-mediated lipid signaling. Methods Mol Biol. 2010;610:201–211. doi: 10.1007/978-1-60327-029-8_12. [DOI] [PubMed] [Google Scholar]
- 94.Bao JX, Jin S, Zhang F, Wang ZC, Li N, Li PL. Activation of membrane NADPH oxidase associated with lysosome-targeted acid sphingomyelinase in coronary endothelial cells. Antioxid Redox Signal. 2010;12:703–712. doi: 10.1089/ars.2009.2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhong Y, Hennig B, Toborek M. Intact lipid rafts regulate HIV-1 Tat protein-induced activation of the Rho signaling and upregulation of P-glycoprotein in brain endothelial cells. J Cereb Blood Flow Metab. 2010;30:522–533. doi: 10.1038/jcbfm.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Barreiro O, Zamai M, Yáñez-Mó M, Tejera E, López-Romero P, Monk PN, Gratton E, Caiolfa VR, Sánchez-Madrid F. Endothelial adhesion receptors are recruited to adherent leukocytes by inclusion in preformed tetraspanin nanoplatforms. J Cell Biol. 2008;183:527–542. doi: 10.1083/jcb.200805076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhao J, Singleton PA, Brown ME, Dudek SM, Garcia JG. Phosphotyrosine protein dynamics in cell membrane rafts of sphingosine-1-phosphate-stimulated human endothelium: role in barrier enhancement. Cell Signal. 2009;21:1945–1960. doi: 10.1016/j.cellsig.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dodelet-Devillers A, Cayrol R, van Horssen J, Haqqani AS, de Vries HE, Engelhardt B, Greenwood J, Prat A. Functions of lipid raft membrane microdomains at the blood-brain barrier. J Mol Med. 2009;87:765–774. doi: 10.1007/s00109-009-0488-6. [DOI] [PubMed] [Google Scholar]
- 99.Yang B, Rizzo V. TNF-alpha potentiates protein-tyrosine nitration through activation of NADPH oxidase and eNOS localized in membrane rafts and caveolae of bovine aortic endothelial cells. Am J Physiol Heart Circ Physiol. 2007;292:H954–H962. doi: 10.1152/ajpheart.00758.2006. [DOI] [PubMed] [Google Scholar]
- 100.Choi SS, Diehl AM. Epithelial-to-mesenchymal transitions in the liver. Hepatology. 2009;50:2007–2013. doi: 10.1002/hep.23196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Strazzabosco M, Fabris L, Spirli C. Pathophysiology of cholangiopathies. J Clin Gastroenterol. 2005;39:S90–S102. doi: 10.1097/01.mcg.0000155549.29643.ad. [DOI] [PubMed] [Google Scholar]
- 102.Kiselyov K, Wang X, Shin DM, Zang W, Muallem S. Calcium signaling complexes in microdomains of polarized secretory cells. Cell Calcium. 2006;40:451–459. doi: 10.1016/j.ceca.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 103.McWilliams RR, Gidey E, Fouassier L, Weed SA, Doctor RB. Characterization of an ankyrin repeat-containing Shank2 isoform (Shank2E) in liver epithelial cells. Biochem J. 2004;380:181–191. doi: 10.1042/BJ20031577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Eren E, Yates J, Cwynarski K, Preston S, Dong R, Germain C, Lechler R, Huby R, Ritter M, Lombardi G. Location of major histocompatibility complex class II molecules in rafts on dendritic cells enhances the efficiency of T-cell activation and proliferation. Scand J Immunol. 2006;63:7–16. doi: 10.1111/j.1365-3083.2006.01700.x. [DOI] [PubMed] [Google Scholar]
- 105.Xu S, Huo J, Gunawan M, Su IH, Lam KP. Activated dectin-1 localizes to lipid raft microdomains for signaling and activation of phagocytosis and cytokine production in dendritic cells. J Biol Chem. 2009;284:22005–22011. doi: 10.1074/jbc.M109.009076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Khandelwal S, Roche PA. Distinct MHC class II molecules are associated on the dendritic cell surface in cholesterol-dependent membrane microdomains. J Biol Chem. 2010;285:35303–35310. doi: 10.1074/jbc.M110.147793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang SH, Yuan SG, Peng DQ, Zhao SP. High-density lipoprotein affects antigen presentation by interfering with lipid raft: a promising anti-atherogenic strategy. Clin Exp Immunol. 2010;160:137–142. doi: 10.1111/j.1365-2249.2009.04068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tellier E, Canault M, Poggi M, Bonardo B, Nicolay A, Alessi MC, Nalbone G, Peiretti F. HDLs activate ADAM17-dependent shedding. J Cell Physiol. 2008;214:687–693. doi: 10.1002/jcp.21265. [DOI] [PubMed] [Google Scholar]
- 109.Inoue H, Miyaji M, Kosugi A, Nagafuku M, Okazaki T, Mimori T, Amakawa R, Fukuhara S, Domae N, Bloom ET, et al. Lipid rafts as the signaling scaffold for NK cell activation: tyrosine phosphorylation and association of LAT with phosphatidylinositol 3-kinase and phospholipase C-gamma following CD2 stimulation. Eur J Immunol. 2002;32:2188–2198. doi: 10.1002/1521-4141(200208)32:8<2188::AID-IMMU2188>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 110.Hillyard DZ, Nutt CD, Thomson J, McDonald KJ, Wan RK, Cameron AJ, Mark PB, Jardine AG. Statins inhibit NK cell cytotoxicity by membrane raft depletion rather than inhibition of isoprenylation. Atherosclerosis. 2007;191:319–325. doi: 10.1016/j.atherosclerosis.2006.05.037. [DOI] [PubMed] [Google Scholar]
- 111.Kondadasula SV, Roda JM, Parihar R, Yu J, Lehman A, Caligiuri MA, Tridandapani S, Burry RW, Carson WE. Colocalization of the IL-12 receptor and FcgammaRIIIa to natural killer cell lipid rafts leads to activation of ERK and enhanced production of interferon-gamma. Blood. 2008;111:4173–4183. doi: 10.1182/blood-2007-01-068908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Masilamani M, Nguyen C, Kabat J, Borrego F, Coligan JE. CD94/NKG2A inhibits NK cell activation by disrupting the actin network at the immunological synapse. J Immunol. 2006;177:3590–3596. doi: 10.4049/jimmunol.177.6.3590. [DOI] [PubMed] [Google Scholar]
- 113.Sanni TB, Masilamani M, Kabat J, Coligan JE, Borrego F. Exclusion of lipid rafts and decreased mobility of CD94/NKG2A receptors at the inhibitory NK cell synapse. Mol Biol Cell. 2004;15:3210–3223. doi: 10.1091/mbc.E03-11-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pallandre JR, Krzewski K, Bedel R, Ryffel B, Caignard A, Rohrlich PS, Pivot X, Tiberghien P, Zitvogel L, Strominger JL, et al. Dendritic cell and natural killer cell cross-talk: a pivotal role of CX3CL1 in NK cytoskeleton organization and activation. Blood. 2008;112:4420–4424. doi: 10.1182/blood-2007-12-126888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Weber MS, Steinman L, Zamvil SS. Statins--treatment option for central nervous system autoimmune disease? Neurotherapeutics. 2007;4:693–700. doi: 10.1016/j.nurt.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zeyda M, Szekeres AB, Säemann MD, Geyeregger R, Stockinger H, Zlabinger GJ, Waldhäusl W, Stulnig TM. Suppression of T cell signaling by polyunsaturated fatty acids: selectivity in inhibition of mitogen-activated protein kinase and nuclear factor activation. J Immunol. 2003;170:6033–6039. doi: 10.4049/jimmunol.170.12.6033. [DOI] [PubMed] [Google Scholar]
- 117.Geyeregger R, Zeyda M, Zlabinger GJ, Waldhäusl W, Stulnig TM. Polyunsaturated fatty acids interfere with formation of the immunological synapse. J Leukoc Biol. 2005;77:680–688. doi: 10.1189/jlb.1104687. [DOI] [PubMed] [Google Scholar]
- 118.Nan X, Carubelli I, Stamatos NM. Sialidase expression in activated human T lymphocytes influences production of IFN-gamma. J Leukoc Biol. 2007;81:284–296. doi: 10.1189/jlb.1105692. [DOI] [PubMed] [Google Scholar]
- 119.Moore ML, Chi MH, Zhou W, Goleniewska K, O’Neal JF, Higginbotham JN, Peebles RS. Cutting Edge: Oseltamivir decreases T cell GM1 expression and inhibits clearance of respiratory syncytial virus: potential role of endogenous sialidase in antiviral immunity. J Immunol. 2007;178:2651–2654. doi: 10.4049/jimmunol.178.5.2651. [DOI] [PubMed] [Google Scholar]
- 120.Unruh TL, Li H, Mutch CM, Shariat N, Grigoriou L, Sanyal R, Brown CB, Deans JP. Cholesterol depletion inhibits src family kinase-dependent calcium mobilization and apoptosis induced by rituximab crosslinking. Immunology. 2005;116:223–232. doi: 10.1111/j.1365-2567.2005.02213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Janas E, Priest R, Wilde JI, White JH, Malhotra R. Rituxan (anti-CD20 antibody)-induced translocation of CD20 into lipid rafts is crucial for calcium influx and apoptosis. Clin Exp Immunol. 2005;139:439–446. doi: 10.1111/j.1365-2249.2005.02720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Katkere B, Rosa S, Caballero A, Repasky EA, Drake JR. Physiological-range temperature changes modulate cognate antigen processing and presentation mediated by lipid raft-restricted ubiquitinated B cell receptor molecules. J Immunol. 2010;185:5032–5039. doi: 10.4049/jimmunol.1001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schmidt C, Kim D, Ippolito GC, Naqvi HR, Probst L, Mathur S, Rosas-Acosta G, Wilson VG, Oldham AL, Poenie M, et al. Signalling of the BCR is regulated by a lipid rafts-localised transcription factor, Bright. EMBO J. 2009;28:711–724. doi: 10.1038/emboj.2009.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Seveau S, Bierne H, Giroux S, Prévost MC, Cossart P. Role of lipid rafts in E-cadherin-- and HGF-R/Met--mediated entry of Listeria monocytogenes into host cells. J Cell Biol. 2004;166:743–753. doi: 10.1083/jcb.200406078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gekara NO, Jacobs T, Chakraborty T, Weiss S. The cholesterol-dependent cytolysin listeriolysin O aggregates rafts via oligomerization. Cell Microbiol. 2005;7:1345–1356. doi: 10.1111/j.1462-5822.2005.00561.x. [DOI] [PubMed] [Google Scholar]
- 126.Mathurin P, Deng QG, Keshavarzian A, Choudhary S, Holmes EW, Tsukamoto H. Exacerbation of alcoholic liver injury by enteral endotoxin in rats. Hepatology. 2000;32:1008–1017. doi: 10.1053/jhep.2000.19621. [DOI] [PubMed] [Google Scholar]
- 127.Mutlu E, Keshavarzian A, Engen P, Forsyth CB, Sikaroodi M, Gillevet P. Intestinal dysbiosis: a possible mechanism of alcohol-induced endotoxemia and alcoholic steatohepatitis in rats. Alcohol Clin Exp Res. 2009;33:1836–1846. doi: 10.1111/j.1530-0277.2009.01022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kalischuk LD, Inglis GD, Buret AG. Campylobacter jejuni induces transcellular translocation of commensal bacteria via lipid rafts. Gut Pathog. 2009;1:2. doi: 10.1186/1757-4749-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Clark E, Hoare C, Tanianis-Hughes J, Carlson GL, Warhurst G. Interferon gamma induces translocation of commensal Escherichia coli across gut epithelial cells via a lipid raft-mediated process. Gastroenterology. 2005;128:1258–1267. doi: 10.1053/j.gastro.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 130.Aizaki H, Lee KJ, Sung VM, Ishiko H, Lai MM. Characterization of the hepatitis C virus RNA replication complex associated with lipid rafts. Virology. 2004;324:450–461. doi: 10.1016/j.virol.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 131.Matto M, Rice CM, Aroeti B, Glenn JS. Hepatitis C virus core protein associates with detergent-resistant membranes distinct from classical plasma membrane rafts. J Virol. 2004;78:12047–12053. doi: 10.1128/JVI.78.21.12047-12053.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mannová P, Fang R, Wang H, Deng B, McIntosh MW, Hanash SM, Beretta L. Modification of host lipid raft proteome upon hepatitis C virus replication. Mol Cell Proteomics. 2006;5:2319–2325. doi: 10.1074/mcp.M600121-MCP200. [DOI] [PubMed] [Google Scholar]
- 133.Sabahi A. Hepatitis C Virus entry: the early steps in the viral replication cycle. Virol J. 2009;6:117. doi: 10.1186/1743-422X-6-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cherukuri A, Shoham T, Sohn HW, Levy S, Brooks S, Carter R, Pierce SK. The tetraspanin CD81 is necessary for partitioning of coligated CD19/CD21-B cell antigen receptor complexes into signaling-active lipid rafts. J Immunol. 2004;172:370–380. doi: 10.4049/jimmunol.172.1.370. [DOI] [PubMed] [Google Scholar]
- 135.Lambert D, O’Neill CA, Padfield PJ. Methyl-beta-cyclodextrin increases permeability of Caco-2 cell monolayers by displacing specific claudins from cholesterol rich domains associated with tight junctions. Cell Physiol Biochem. 2007;20:495–506. doi: 10.1159/000107533. [DOI] [PubMed] [Google Scholar]
- 136.Dolganiuc A, Oak S, Kodys K, Golenbock DT, Finberg RW, Kurt-Jones E, Szabo G. Hepatitis C core and nonstructural 3 proteins trigger toll-like receptor 2-mediated pathways and inflammatory activation. Gastroenterology. 2004;127:1513–1524. doi: 10.1053/j.gastro.2004.08.067. [DOI] [PubMed] [Google Scholar]
- 137.Triantafilou M, Gamper FG, Lepper PM, Mouratis MA, Schumann C, Harokopakis E, Schifferle RE, Hajishengallis G, Triantafilou K. Lipopolysaccharides from atherosclerosis-associated bacteria antagonize TLR4, induce formation of TLR2/1/CD36 complexes in lipid rafts and trigger TLR2-induced inflammatory responses in human vascular endothelial cells. Cell Microbiol. 2007;9:2030–2039. doi: 10.1111/j.1462-5822.2007.00935.x. [DOI] [PubMed] [Google Scholar]
- 138.Makoveichuk E, Castel S, Vilaró S, Olivecrona G. Lipoprotein lipase-dependent binding and uptake of low density lipoproteins by THP-1 monocytes and macrophages: possible involvement of lipid rafts. Biochim Biophys Acta. 2004;1686:37–49. doi: 10.1016/j.bbalip.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 139.Peng Y, Akmentin W, Connelly MA, Lund-Katz S, Phillips MC, Williams DL. Scavenger receptor BI (SR-BI) clustered on microvillar extensions suggests that this plasma membrane domain is a way station for cholesterol trafficking between cells and high-density lipoprotein. Mol Biol Cell. 2004;15:384–396. doi: 10.1091/mbc.E03-06-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gummuluru S, Rogel M, Stamatatos L, Emerman M. Binding of human immunodeficiency virus type 1 to immature dendritic cells can occur independently of DC-SIGN and mannose binding C-type lectin receptors via a cholesterol-dependent pathway. J Virol. 2003;77:12865–12874. doi: 10.1128/JVI.77.23.12865-12874.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Funk A, Mhamdi M, Hohenberg H, Heeren J, Reimer R, Lambert C, Prange R, Sirma H. Duck hepatitis B virus requires cholesterol for endosomal escape during virus entry. J Virol. 2008;82:10532–10542. doi: 10.1128/JVI.00422-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Bremer CM, Bung C, Kott N, Hardt M, Glebe D. Hepatitis B virus infection is dependent on cholesterol in the viral envelope. Cell Microbiol. 2009;11:249–260. doi: 10.1111/j.1462-5822.2008.01250.x. [DOI] [PubMed] [Google Scholar]
- 143.Sayre NL, Rimkunas VM, Graham MJ, Crooke RM, Liscum L. Recovery from liver disease in a Niemann-Pick type C mouse model. J Lipid Res. 2010;51:2372–2383. doi: 10.1194/jlr.M007211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rimkunas VM, Graham MJ, Crooke RM, Liscum L. TNF-{alpha} plays a role in hepatocyte apoptosis in Niemann-Pick type C liver disease. J Lipid Res. 2009;50:327–333. doi: 10.1194/jlr.M800415-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ikonen E, Hölttä-Vuori M. Cellular pathology of Niemann-Pick type C disease. Semin Cell Dev Biol. 2004;15:445–454. doi: 10.1016/j.semcdb.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 146.Blom TS, Koivusalo M, Kuismanen E, Kostiainen R, Somerharju P, Ikonen E. Mass spectrometric analysis reveals an increase in plasma membrane polyunsaturated phospholipid species upon cellular cholesterol loading. Biochemistry. 2001;40:14635–14644. doi: 10.1021/bi0156714. [DOI] [PubMed] [Google Scholar]
- 147.Lusa S, Blom TS, Eskelinen EL, Kuismanen E, Månsson JE, Simons K, Ikonen E. Depletion of rafts in late endocytic membranes is controlled by NPC1-dependent recycling of cholesterol to the plasma membrane. J Cell Sci. 2001;114:1893–1900. doi: 10.1242/jcs.114.10.1893. [DOI] [PubMed] [Google Scholar]
- 148.Koken T, Gursoy F, Kahraman A. Long-term alcohol consumption increases pro-matrix metalloproteinase-9 levels via oxidative stress. J Med Toxicol. 2010;6:126–130. doi: 10.1007/s13181-010-0081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kukiełka E, Cederbaum AI. The effect of chronic ethanol consumption on NADH- and NADPH-dependent generation of reactive oxygen intermediates by isolated rat liver nuclei. Alcohol Alcohol. 1992;27:233–239. [PubMed] [Google Scholar]
- 150.Sergent O, Morel I, Chevanne M, Cillard P, Cillard J. Oxidative stress induced by ethanol in rat hepatocyte cultures. Biochem Mol Biol Int. 1995;35:575–583. [PubMed] [Google Scholar]
- 151.Cuschieri J, Maier RV. Oxidative stress, lipid rafts, and macrophage reprogramming. Antioxid Redox Signal. 2007;9:1485–1497. doi: 10.1089/ars.2007.1670. [DOI] [PubMed] [Google Scholar]
- 152.Nourissat P, Travert M, Chevanne M, Tekpli X, Rebillard A, Le Moigne-Müller G, Rissel M, Cillard J, Dimanche-Boitrel MT, Lagadic-Gossmann D, et al. Ethanol induces oxidative stress in primary rat hepatocytes through the early involvement of lipid raft clustering. Hepatology. 2008;47:59–70. doi: 10.1002/hep.21958. [DOI] [PubMed] [Google Scholar]
- 153.Nordmann R, Ribière C, Rouach H. Implication of free radical mechanisms in ethanol-induced cellular injury. Free Radic Biol Med. 1992;12:219–240. doi: 10.1016/0891-5849(92)90030-k. [DOI] [PubMed] [Google Scholar]
- 154.Dey A, Cederbaum AI. Alcohol and oxidative liver injury. Hepatology. 2006;43:S63–S74. doi: 10.1002/hep.20957. [DOI] [PubMed] [Google Scholar]
- 155.Sergent O, Pereira M, Belhomme C, Chevanne M, Huc L, Lagadic-Gossmann D. Role for membrane fluidity in ethanol-induced oxidative stress of primary rat hepatocytes. J Pharmacol Exp Ther. 2005;313:104–111. doi: 10.1124/jpet.104.078634. [DOI] [PubMed] [Google Scholar]
- 156.Hoek JB, Thomas AP, Rooney TA, Higashi K, Rubin E. Ethanol and signal transduction in the liver. FASEB J. 1992;6:2386–2396. [PubMed] [Google Scholar]
- 157.Das SK, Vasudevan DM. Alcohol-induced oxidative stress. Life Sci. 2007;81:177–187. doi: 10.1016/j.lfs.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 158.Szabo G, Dolganiuc A, Dai Q, Pruett SB. TLR4, ethanol, and lipid rafts: a new mechanism of ethanol action with implications for other receptor-mediated effects. J Immunol. 2007;178:1243–1249. doi: 10.4049/jimmunol.178.3.1243. [DOI] [PubMed] [Google Scholar]
- 159.Verma SP. HIV: a raft-targeting approach for prevention and therapy using plant-derived compounds (review) Curr Drug Targets. 2009;10:51–59. doi: 10.2174/138945009787122851. [DOI] [PubMed] [Google Scholar]
- 160.Partlow KC, Lanza GM, Wickline SA. Exploiting lipid raft transport with membrane targeted nanoparticles: a strategy for cytosolic drug delivery. Biomaterials. 2008;29:3367–3375. doi: 10.1016/j.biomaterials.2008.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mollinedo F, Gajate C. Fas/CD95 death receptor and lipid rafts: new targets for apoptosis-directed cancer therapy. Drug Resist Updat. 2006;9:51–73. doi: 10.1016/j.drup.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 162.Gajate C, Gonzalez-Camacho F, Mollinedo F. Lipid raft connection between extrinsic and intrinsic apoptotic pathways. Biochem Biophys Res Commun. 2009;380:780–784. doi: 10.1016/j.bbrc.2009.01.147. [DOI] [PubMed] [Google Scholar]
- 163.Mollinedo F, de la Iglesia-Vicente J, Gajate C, Estella-Hermoso de Mendoza A, Villa-Pulgarin JA, Campanero MA, Blanco-Prieto MJ. Lipid raft-targeted therapy in multiple myeloma. Oncogene. 2010;29:3748–3757. doi: 10.1038/onc.2010.131. [DOI] [PubMed] [Google Scholar]
- 164.Mollinedo F, Gajate C. Lipid rafts and clusters of apoptotic signaling molecule-enriched rafts in cancer therapy. Future Oncol. 2010;6:811–821. doi: 10.2217/fon.10.34. [DOI] [PubMed] [Google Scholar]
- 165.Sakamoto H, Okamoto K, Aoki M, Kato H, Katsume A, Ohta A, Tsukuda T, Shimma N, Aoki Y, Arisawa M, et al. Host sphingolipid biosynthesis as a target for hepatitis C virus therapy. Nat Chem Biol. 2005;1:333–337. doi: 10.1038/nchembio742. [DOI] [PubMed] [Google Scholar]
- 166.Hirata Y, Sudoh M, Kohara M. [Suppression of hepatitis C virus (HCV) replication with serine palmitoyltransferase inhibitor] Yakugaku Zasshi. 2010;130:157–161. doi: 10.1248/yakushi.130.157. [DOI] [PubMed] [Google Scholar]
- 167.Amemiya F, Maekawa S, Itakura Y, Kanayama A, Matsui A, Takano S, Yamaguchi T, Itakura J, Kitamura T, Inoue T, et al. Targeting lipid metabolism in the treatment of hepatitis C virus infection. J Infect Dis. 2008;197:361–370. doi: 10.1086/525287. [DOI] [PubMed] [Google Scholar]
- 168.O'Leary JG, Chan JL, McMahon CM, Chung RT. Atorvastatin does not exhibit antiviral activity against HCV at conventional doses: a pilot clinical trial. Hepatology. 2007;45:895–898. doi: 10.1002/hep.21554. [DOI] [PubMed] [Google Scholar]