Abstract
A body of epidemiologic and clinical evidence dating back to the early 1960s establishes the relationships between sleep apnea and cardiovascular disease (CVD). Individuals with obstructive sleep apnea, the most common type of sleep-disordered breathing, are at increased risk for coronary artery disease, congestive heart failure, and stroke. Evidence that treatment of sleep apnea with continuous positive airway pressure reduces blood pressure, improves left ventricular systolic function, and diminishes platelet activation further supports linkage between obstructive sleep apnea and CVD. Notwithstanding, complex associations between these two conditions remain largely unexplained due to dearth of systematic experimental studies. Arguably, several intermediary mechanisms including sustained sympathetic activation, intrathoracic pressure changes, and oxidative stress might be involved. Other abnormalities such as dysfunctions in coagulation factors, endothelial damage, platelet activation, and increased systemic inflammation might also play a fundamental role. This review examines evidence for the associations between obstructive sleep apnea and CVD and suggested underlying anatomical and physiological mechanisms. Specific issues pertaining to definition, prevalence, diagnosis, and treatment of sleep apnea are also discussed. Consistent with rising interest in the potential role of the metabolic syndrome, this review explores the hypothesized mediating effects of each of the components of the metabolic syndrome.
Keywords: Sleep apnea, obstructive, Cardiovascular diseases, Obesity, Hypertension, Diabetes mellitus
Sleep apnea: definition and prevalence
Sleep apnea is a common medical condition that is characterized by repeated cessation of breathing during sleep, due primarily to complete or partial pharyngeal obstruction. This review focuses on obstructive sleep apnea (OSA), since it is the most prevalent sleep-disordered breathing. Sleep apnea is recognized by a combination of symptoms and laboratory results. These include repetitive apneas and hypopneas, which are accompanied by hypoxemia, sleep arousals, and hemodynamic changes.1,2 Additionally, activation of the sympathetic nervous system during respiratory events potentiates vasoconstriction and often triggers increases in blood pressure and heart rate.3
Obstructive sleep apnea causes significant sleep disturbances, leading to excessive daytime sleepiness and fatigue. These manifestations could potentially results in vehicular and industrial accidents.4 Untreated OSA may lead to a gradual decline in cognitive ability and poor performance.5 Data obtained from a chart audit of 4 million enrollees of the Veterans Health Administration have shown that psychiatric comorbid diagnoses including depression, anxiety, post-traunmatic stress disorder, psychosis, and bipolar disorders are associated with OSA.6 Obstructive sleep apnea is also associated with several cardio-respiratory problems (e.g., loud snoring, loud gasps, and daytime breathlessness) and all-cause mortality.7 Despite these alarming findings, most individuals with OSA have not been comprehensively evaluated.
It has been estimated that 82% of men and 93% of women with moderate to severe OSA remain undiagnosed.8 That the majority of patients with sleep apnea have yet to receive a diagnosis could be explained by a lack of awareness of sleep apnea among patients and/or among health professionals. It is known that patients affected by OSA are often unaware that they may wake up hundreds of times during the night. This could in part explain low complaint rates in clinical histories. According to a chart audit of a million patients, the National Commission on Sleep Disorders Research noted only 17 positive diagnoses for sleep disorders.9 Increased awareness of OSA risk factors (e.g., age, sex, ethnicity, body habitus, familial predisposition, alcohol, and chronic rhinitis) could help both the clinician and patient to decide whether a sleep evaluation is necessary. Screening rates could improve through increased awareness of co-morbid conditions (e.g., hypertension, diabetes mellitus, and cadiovascular disease [CVD]).
Epidemiologic evidence shows that 2% of middle-aged women and 4% of middle-aged men have five or more apnea/hypopnea episodes per hour (AHI) and meet criteria for obstructive sleep apnea.8 Using a respiratory disturbance index* of 10 or greater, the Wisconsin Sleep Cohort Study, an epidemiological study surveying the US adult population, showed that sleep apnea affects as much as 15% of men and 5% of women between the ages of 30 and 60 years.10 Furthermore, another study using laboratory polysomnography showed that 24% of men and 9% of Women met criteria for sleep apnea.11
Sleep apnea affects individuals of all ages, but prevalence data suggest that it is more common among middle-aged adults between 40 and 60 years old. According to one estimate, 1.6% to 10.3% of children meet criteria for sleep apnea.12 The prevalence of sleep apnea tends to be higher among older adults. In one study, it was estimated that up to 60% of community-residing older adults have significant sleep apnea, with many of them experiencing central apnea episodes.13 Specifically, 24% of adults older than 65 years old had an AHI ≥5 and 62% had an AHI ≥10.
Typical risk factors for sleep apnea listed in the public health literature are male gender, overweight/obesity, and being over the age of forty.8 New findings strongly suggest the need to include ethnicity as an important risk factor as well. Evidence suggests that hypertension and CVD (manifested as heart failure, stroke or clinically apparent coronary artery disease), perhaps the most important comorbid conditions of sleep apnea, are more prevalent among African Americans.14 In a case-control family study of sleep apnea comparing 225 African Americans and 622 Caucasians, aged 2 to 86 years, 31% of African Americans versus 10% of Caucasians had respiratory disturbance indices greater than 10.15 Despite these alarming data, the vast majority of suspected cases in minority communities remain undiagnosed and therefore untreated. A recent study ascertaining adherence rates to physician referrals for sleep apnea assessment in a community-based sample of African American patients showed that only 38% of the population adhered to doctor’s recommendations, while 91% of the subjects undergoing an assessment received a diagnosis.16
Pathophysiology of obstructive sleep apnea
In the early 1960s, it was evident that upper airway obstruction was fundamental in the pathogenesis of OSA. This notion was supported by studies showing that tracheostomy can reverse the clinical manifestations of obstructive sleep apnea.17 Patients with OSA have decreased maximal pharyngeal area and greater airway pressure compared with healthy individuals. Therefore, OSA was assumed to originate from upper-airway resistance.18 OSA could also be caused by recurrent pharyngeal occlusion, causing partial or complete cessation of airflow. During sleep, upper airway neuromuscular activity diminishes, but reduced neuromuscular activity tends to be more pronounced among patients with OSA The-reduction in ventilatory effort is the imminent event in a cascade of activity producing upper airway obstruction.
Available clinical evidence points to upper airway obstruction among most patients with sleep apnea, occurring either in the nasopharynx or the oropharynx.19 Both anatomical and physiological factors interplay in the production of pharyngeal collapse.20 Most patients have a narrow airway because of enlarged pharyngeal tissues due to obesity, with increased fat deposits producing enlarged soft palate and uvula. Other factors involved in airway obstruction include a large tongue, vascular congestion, and pulse edema of the pharyngeal mucosa.19 Edema of the pharyngeal wall associated with central venous pressure elevation can produce luminal narrowing and predispose at-risk individuals to airway collapse. A handful or patients have narrow upper airway due several anatomic predispositions including enlarged tonsils, macroglossia, micrognathia, retrognathia, and adenotonsillar hypertrophy.
During periods of wakefulness, individuals counteract the effects of upper airway narrowing by compensatory increase in the activity of upper airway dilator muscles. However, efforts to compensate for this narrowing among patients with OSA appear ineffective during sleep. This inability to provide an adequate compensatory response leads to imbalance between rival forces promoting collapse of the pharynx and those maintaining upper airway patency.19 This then results in an upper airway closure. The ensuing decrease in ventilation causes hypoxia and hypercapnia. This sets in motion a cascade of events beginning with increased ventilatory efforts leading to labored breathing. Subsequently, patients experience cortical arousals and/or abrupt awakenings as they endeavor to resume normal breathing. Upon awakening, the upper airway dilator muscles are reactivated and airway patency and ventilation are restored. With adequate ventilation, patients can return to sleep (Figure 1).
Figure 1.
Illustration of obstructive sleep apnea event leading to oxyhemoglobin desaturation (SaO2). Adapted from the Sleep Academy Award Program sponsored by National Sleep Foundation.
Diagnosis of obstructive sleep apnea
Standard of care for sleep apnea screening typically entails a detailed sleep history, which is performed by a sleep clinician in a structured setting. Whenever possible family members are queried regarding patients’ sleep patterns, since often times patients are unaware that they are experiencing disordered sleep. Patients with positive screening results are routinely referred to a sleep clinic for a comprehensive assessment of sleep apnea using laboratory polysomnographic studies.21 In some instances, investigators rely on home recordings or oxymetry to render a sleep apnea diagnosis. This has often complicated the ability to establish head-to-head comparison of rates and/or severity of sleep apnea in published studies.
A noctumal polysomnographic study incorporates assessment of sleep architecture, airflow and ventilatory effort arterial blood saturation, electrocardiogram, body position and periodic limb movement.22 Consistent with the need to arrive at an accurate diagnosis, a sleep specialist typically interprets the results of the study. Although less common, the diagnosis of central sleep apnea, another a type sleep-disordered breathing, distinct from OSA, is rendered when a lack of airflow is observed in the absence of ventilatory effort using predetermined criteria.23 However OSA is by all accounts more prevalent and is characterized by closure of the upper airway, causing cessation of airflow despite persistent ventilatory effort.
Treatment of obstructive sleep apnea
The most effective, noninvasive treatment for sleep apnea requires the use of continuous positive airway pressure (CPAP). This therapy requires the patient to wear a sealed mask over the nose, or in certain cases both the nose and mouth while sleeping. The patient receives forced room air via the mask (that has been fitted by a technician), increasing the pressure in the oropharyngeal airway, which helps to maintain airway patency. Oral-dental devices may also be used in mild cases or for patients requiring treatment for primary snoring. These are intended to reposition the mandible, thereby maximizing the diameter of the oropharyngeal airway. In other cases, surgical procedures (e.g., uvulopalatopharyngoplasty, laser-assisted uvulopalatopharyngoplasty) remain viable options, albeit the least desired treatment because of their invasiveness and complexity. In severe cases of sleep apnea, especially among patients with significant episodes of bradyarrhythmias or tachyarrhythmias, gastric bypass surgery should be considered.
The use of CPAP as a therapeutic modality for sleep apnea is often coupled with some form of behavior modification.24 Thus, the objectives of treatment are to eradicate not only physiologic abnormalities including sleep fragmentation, apneic episodes, and oxygen desaturations but also symptoms such as snoring and daytime sleepiness and to reduce risks for comorbid conditions. Ultimately, weight loss interventions, aiming to reduce total body weight by 7% to 10%, seems to be the most effective lifestyle modification encouraged by sleep clinicians. Although it is often difficult for patients with OSA to initiate or maintain a weight management program, even modest weight loss can yield significant reduction in symptom severity.25 This constitutes the standard of care, according to published practice parameters established by the American Academy of Sleep Medicine.26
Issues pertaining to CPAP adherence should also be addressed. Evidence shows that only 50% of patients initially accept CPAP devices,27 but that 40% of patients discontinue home CPAP therapy during the first week.28 Factors that may increase CPAP adherence include satisfaction with disease management; adherence during the first week augurs greater adherence one year later, and personality characteristics. Adherence can be enhanced when CPAP management-related issues are recognized and addressed, including monitoring disease severity, depressive symptomotology, oxygen deficits, and cardiovascular sequelae. Better outcome is observed when family members are involved in the process of overcoming barriers interfering with nightly CPAP use, particularly when incorporated in educational programs. Intervention programs aiming at enhancing adherence to prescribed CPAP therapy suggested that education should endeavor to improve patients’ lifestyle through weight reduction, increasing physical activity, and tobacco avoidance, in addition to direct CPAP therapy. More importantly, intensive educational program should be instituted in the first two weeks of treatment because patients exhibiting satisfaction with CPAP treatment are likely to remain adherent a year later.
Associations of obstructive sleep apnea with cardiovascular disease
Sleep apnea is thought to be as prevalent as adult diabetes and might affect more than 18 million Americans.29 It might be as important a public health hazard as smoking is.29,30 The National Commission on Sleep Disorders Research estimated that sleep apnea is probably responsible for 38 000 cardiovascular deaths yearly, with an associated 42 million dollars spent on related hospitalizations.31 Data from the Sleep Heart Health Study, an National Heart Lung and Blood Institute (NHLBI)-sponsored project, indicate that sleep apnea increases the risk of heart failure by 140% the risk of stroke is increased by 60% and the risk of coronary heart disease is increased by 30%. Patients with severe sleep apnea may have two-four fold greater odds for complex arrhythmias than non-affected persons.32 In light of these findings, the American Heart Association/American College of Cardiology Foundation issued a scientific statement on sleep apnea and CVD, highlighting the need for systematic research to explicate important associations between these two conditions, with the desired goal to improve disease management, thereby reducing CVD morbidity and premature death.33
Clinical and epidemiologic evidence
About three decades ago, two research groups studied the relationships between obstructive sleep apnea and CVD by performing numerous observational laboratories studies. Investigators performed tracheostomy to alleviate comorbid conditions among patients with a diagnosis of sleep apnea. Subsequent to tracheostomy, they observed complete disappearance of a severe atrial flutter and a postoperative decrease in systemic blood pressure.1,2 Other investigators observed normalization of blood pressure in two hypertensive children with severe apneas within 24 hours after surgery.20 Data from another study demonstrated a 10% difference in mortality over a 10-year period, comparing patients with sleep apnea agreeing to undergo tracheostomy with those favoring conservative treatment.34
More recent experimental and clinical studies have further established the link between OSA and CVD. A study involving 400 patients with sleep apnea showed that 48% of them had cardiac arrhythmias,35 which often accompany severe nocturnal hypoxemia.36 Through follow-up studies, tracheostomy eliminated those arrhythmias in a subset of those patients. It should be noted that among patients with sleep apnea who experience episodes of prolonged ventricular asystole, invasive electrophysiologic evaluation has failed to establish any anatomic abnormalities or irreversible sinus or atrioventricular nodal disease. It is currently recommended that bradyarrhythmias be treated with oxygen therapy or CPAP in patients with sleep apnea, since it is enhanced vagal tone during the hypoxemic episodes that results in bradycardia.
Addressing confounding factors
Several epidemiologic and clinical studies have explored the associations between OSA and CVD. Some of the early studies showing those associations were questioned, since samples were too small to account for the influence of confounding factors. Some argued that sleep apnea and CVD have common risk factors including, age, gender, race/ethnicity and obesity,37 which could confound the observed associations. Studies also needed to take into account the fact that patients with OSA generally are unhealthy. It has been shown that the 10-year-risk of coronary heart disease and stroke, for instance, approximately is. 30% among patients with sleep apnea.38
More recent attempts have been made through large-scale epidemiologic studies to explain associations between OSA and CVD, with adequate statistical control for known confounding factors. In one of those studies, OSA significantly increased the risk for stroke independently of other risk factors (i.e., age, sex, race, smoking, alcohol-consumption, body-mass index, and the presence or absence of diabetes mellitus, dyslipidemia, atrial fibrillation, and hypertension).39 With adequate adjustment for confounding factors, a cross-sectional study showed that patients with an AHI ≥20 have significantly greater odds for stroke (odds ratio=4.33) relative to individuals without sleep apnea (AHI<5).40
The independent association of OSA with cardiovascular morbidity was further supported using evidence from animal studies. Investigators have induced sleep apnea in dogs by orchestrating intermittent airway occlusion.41 This line of experiments led to the observation of sustained daytime hypertension. Other researchers have studied patients with sleep apnea presenting without other known medical conditions in order to rule out the influence of confounding factors. Those studies have indicated that patients with sleep apnea are characterized by higher levels of sympathetic nervous system activity during wakefulness as well during sleep, relative to healthy controls.42 During apnea events, oxygen levels decreased and carbon dioxide levels increased commensurately, which activated the sympathetic nervous system. Higher level of sympathetic nervous system activity induced blood vessel constriction, with blood pressure rising up to 250/150 mmHg. Those patients also exhibited faster heart rates during wakefulness, although heart rates are often less variable. Indeed, heart rate, itself, is directly associated with survival in unselected populations and among patients with evidence of coronary artery disease and/or hypertension. Thus, upward alteration by sleep apnea may add to the detrimental effect of this condition.43
An important epidemiologic study, the Sleep Heart Health Study, sampling 6 424 free-living individuals who underwent home polysomnography, evidenced increased risk of coronary artery disease, congestive heart failure, and stroke among patients with severe sleep apnea.44 Analysis also showed that patients with OSA had four times the odds for atrial fibrillation (adjusted OR=4.02).32 This is in tandem with findings from a prospective study of consecutive patients undergoing electrocardioversion for atrial fibrillation, which showed that the adjusted odds ratio for atrial fibrillation among patients with OSA was 2.19.45 Data from the Sleep Heart Health Study also revealed that odds for coronary heart disease (OR=4.02) and tachycardia (OR=3.40) were also significantly greater among individuals with OSA.32
Linking obstructive sleep apnea to cardiovascular disease
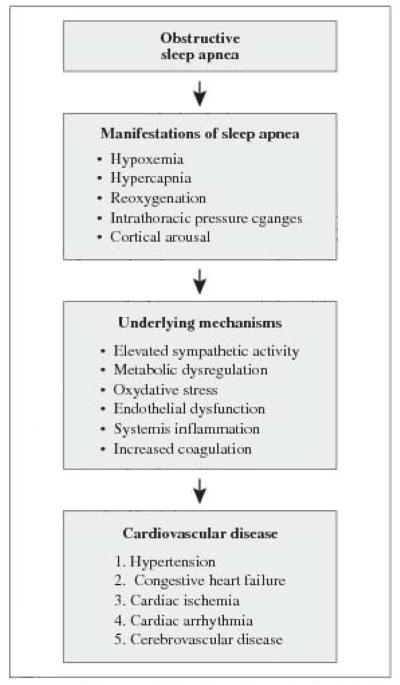
The intermediary pathophysiology underlying the associations between OSA and CVD are not fully established, but several mechanisms have been observed as potential targets for systematic empirical analyses. These mechanisms are changes in intrathoracic pressure, elevated sympathetic drive, and oxidative stress and vascular inflammation resulting from the nocturnal hypoxia and reoxygenation cycles.33 Regarding the significance of elevated sympathetic drive, it is believed that repetitive apneic/hypopneic events along with ensuing arterial desaturation and hypercapnia cause activation of the sympathetic nervous system (Figure 2). This then results in frequent increases in systolic blood pressure that might ultimately lead to hypertension or exacerbation of this condition. Among individuals with moderate to severe OSA, systolic and diastolic pressure can rise up to 25% of baseline.46 Some have advanced that the Similar mechanism might explain the link between sleep apnea and arrhythmias one hand.45
Figure 2.
Pathway linking obstructive sleep apnea to cardiovascular disease. Data suggest that underlying mechanisms may interact with each other to increase risk of developing cardiovascular disease or worsen cardiovascular outcomes.
Patients With OSA are characterized by other abnormalities that might also be involved in the pathogenesis of CVD. These include disorders in coagulation factors, endothelial damage, platelet activation, and increased inflammatory mediators.47 Typically, patients with OSA have greater levels of endothelin and lower levels of nitric oxide than healthy sleepers, which may explain why they often experience greater blood vessel constriction. Some patients may have levels of endothelin rising up to 50%. Elevated endothelin can also impair blood pressure regulation. With CPAP treatment, however, levels of endothelin and circulating nitric oxide invariably return to normal.48
The relative contribution of oxidative stress in explaining the associations between OSA and CVD has been examined.49,50 Studies suggest that hypoxia, which is commonly observed in sleep apnea, promotes the formation of reactive oxygen species, particularly during the reoxygenation period. With increased production of reactive oxygen species, a consequential increase in circulating levels of adenosine and urinary uric acid is observed. Reactive oxygen species, however, regulate the activation of critical transcription factors that are redox sensitive, resulting in increased expression of genes, which encode proteins that promote adaptation to hypoxia. It has also been suggested that redox-sensitive transcription factors that elicit inflammatory pathways are also activated, thereby affecting inflammatory and immune responses by promoting activation of endothelial cells, leukocytes, and platelets.49 Once activated, those cells express adhesion molecules and proinflammatory cytokines that may led to endothelial injury and dysfunction; this series of events inevitably leads to cardiovascular morbidity.
Examination of these physiologic findings has led investigators to conclude that that atherogenesis apparently starts soon after the onset of sleep apnea. Conceivably, significant atherosclerotic damage is experienced by the time OSA is detected, since symptoms become apparent often around the age of 45 years.51 Of note, among African Americans the onset of sleep apnea is much earlier, and they do not always show the typical body habitus suggestive of sleep apnea. It is believed that diagnosis at this age may be too late for some patients, given that some of these insults are irreversible. Although such atherogenic damages cannot be reversed, treatment can retard their progress.52 Utilization of CPAP therapy has been shown to reduce levels of C-reactive protein and interleukin-6 53 and to regress atherogenic plaque among patients with dyslipidemia.54 This explains in part why many patients with OSA present with cardiovascular morbidity in the clinic.
Evidence from clinical studies with CPAP
Intervention studies aiming to treat OSA with nasal continuous positive airway pressure has further confirmed the link between OSA and CVD. Results of those studies have included reduced diurnal and nocturnal blood pressure.55 Among patients with congestive heart failure, treatment of coexisting sleep apnea with continuous positive airway pressure reduces systolic blood pressure and improves left ventricular systolic function.56 CPAP therapy has been shown to eliminate apneic episodes and associated hemodynamic changes occurring during sleep.57 A more recent controlled study examined the effects of sleep apnea treatment on nonfatal (myocardial infarction, stroke, and acute coronary syndrome requiring revascularization procedures) and fatal (death from myocardial infarction or stroke) cardiovascular events.58 Investigators demonstrated that subsequent to adjustment for age, gender, cardiovascular risk factors, and baseline, comorbidities, sleep apnea treatment was associated with a cardiovascular risk reduction of 64%.
Does the metabolic syndrome play a mediating role?
No conclusive evidence supports a cause-and-effect relationship between OSA and CVD, although various physiologic factors produced by obstructive sleep apnea may play a significant role in the pathogenesis of CVD. Sleep apnea is widely recognized for its adverse vascular sequelae: acute myocardial infarction and/or nocturnal angina caused by arterial vasospasm.59 The relationships between sleep apnea and CVD are rather complex, and several systematic studies are necessary to explain fully the nature of those associations. There is also a concern regarding the design of randomized controlled trials, which might not incorporate methodologies to ensure that all participants receive full benefits of proposed treatment regimens. These complexities are further compounded by findings suggesting that conditions comprising the metabolic syndrome might mediate effects of sleep apnea on CVD.
A causal link between the metabolic syndrome and sleep apnea has not been established, in part because previous research has considered linkage analysis primarily for individual components of the metabolic syndrome. However, preliminary data suggest an important role for the metabolic syndrome itself. Indeed, data from the Mayo Clinic demonstrate higher prevalence of metabolic syndrome among patients with sleep apnea (60% in the Mayo study) than among those without (40%).60 In addition, among patients with co-existing sleep apnea and metabolic syndrome, a recent controlled trial showed that CPAP treatment improved insulin sensitivity, reduced systemic inflammation and oxidative stress, and reduced global CVD risk.61 More specifically, patients using CPAP for at least four hours a night showed reduced, 10-year risk of cardiovascular events using Framingham scores (from 18.8% to 13.9%).
Definition of the metabolic syndrome
The metabolic syndrome has become a public health concern,62 It represents a collection of interrelated risk factors of metabolic origin that increase chances of developing heart disease, stroke, and diabetes. It increases the risk for coronary heart disease at any LDL-C level, and it is associated with prothrombotic and proinflammatory states, two common risk factors for coronary heart disease and diabetes mellitus.50 The metabolic syndrome is an important contributor to the development of atherosclerosis and CVD. Individuals presenting with characteristics of the metabolic syndrome are at increased risk of developing type 2 diabetes,63 and those with diabetes are at increased risk of developing CVD.64
Data from the third National Health and Nutrition Examination Survey (1988–1994) of 8814 adults (aged ≥20 years) indicated that the age-adjusted prevalence of the metabolic syndrome was 23.7%.65 Analysis of data from the National Health and Nutrition Examination Survey (1999–2002; N=3601), using a new definition from the National Cholesterol Education Program, demonstrated unadjusted prevalence of the metabolic syndrome among men and women (aged 814 adults (aged 20 years) of 33.7% and 35.4%, respectively.66
Since the observation of the first cluster of metabolic diseases in the 1920s, many definitions have been offered by different research groups. Given that the metabolic syndrome has become a worldwide health concern, formal definitions have been proposed by several health organizations to allow consensus agreement in recognizing the components of the metabolic syndrome as well as in identifying high-risk individuals.67 Criteria proposed by the World Health Organization and the National Cholesterol Education Program are compared in Table I. Other criteria have been proposed by the American Heart Association/National Heart, Lung, and Blood Institute and the European Group for Study of Insulin Resistance (AHA/NHLBI Scientific Statement).68 Thus far, available definitions share similar criteria, although they differ somewhat regarding etiology of the metabolic syndrome and degree of importance assigned to each of its components.
Table I.
Information in the table was obtained from guidelines provided by the World Health Organization (WHO) and the National Cholesterol Education Program (NCEP).
| WHO and NCEP ATP III Definition of the Metabolic Syndrome
| ||
|---|---|---|
| Characteristics | WHO | NCEP ATP III |
| Hypertension | Current antihypertensive therapy and/or BP >140/90 | Blood pressure medication or BP>130/85 |
| Dyslipidemia | Plasma triglycerides >1.7 mmol/L (150 mg/dL) and/or HDL <0.9 mmol/L (35 mg/dL) in men and <1.0 mmol/L (<40 mg/dL) in women | Plasma triglycerides >150 mg/dL, HDL cholesterol <40 mg/dL in men and <50 mg/dL in women |
| Obesity | BMI>30 and/or waist/hip ratio >0.90 in men and >0.85 in women | Waist circumference >40 cm in men and >50 cm in women |
| Diabetes | Type 2 diabetes or IGT | |
| Other | Microalbuminuria=overnight urinary albumin excretion rate >20 mcg/min (30 mg/g Cr) | Fasting blood sugar>110 mg/dL* |
| Requirements for diagnosis | Type 2 diabetes or IGT and any 2 of the above criteria. If normal glucose tolerance is found, three other disorders must be present | Any three of the above disorders |
BMI: body mass index; BP blood pressure; HDL high-density lipoprotein; IGT: impaired glucose tolerance.
Fasting plasma glucose has been updated to 100 mg/dL by the American Diabetes Association.
Besides considering the impact of metabolic diseases (including OSA) on CVD risks, interest is emerging in ascertaining the relative contribution of circadian rhythms to cardiovascular events. Sleep researches believe that risks may be greater if there is synergistic interplay among sleep cycles, arousal mechanisms, and acute thrombosis.69 Evidence suggests that peripheral cells, including those of the cardiovascular system, contain a circadian clock functioning in a manner similar to the one found in the suprachiasmatic nuclei.70 It is known that several factors in cardiovascular physiology are subject to diurnal variation.69 In effect, cardiovascular events including stroke, myocardial infarction and sudden cardiac death tend to occur during specific phases of the circadian cycle.69 Blood pressure patterns also have a Circadian component, which is used to differentiate dippers from non-dippers,71 with non-dippers showing no difference in blood pressure at night compared with their daytime values. Evidence suggests that the temporal distribution of blood pressure is an important marker for vascular events.71 Accordingly, abnormal patterns of blood pressure variation correlate with advanced target organ damage and poor cardiovascular prognosis.71 Work is underway to elucidate the contribution of circadian patterns of tumor necrosis factor-α (TNFα) and interleukin-6 (IL-6) in blood pressure variations among sleep apnea patients.
AHA Scientific Statement
Obstructive sleep apnea and obesity
According to the National Institutes of Diabetes and Digestive and Kidney Diseases, approximately two-thirds of American adults are either overweight (BMI>25; 33%) or obese (BMI>30; 31%) These findings are consistent with CDC data from the National Health and Nutrition Examination Survey, suggesting that 20.9% of Americans are obese. It is well established that obesity plays an important role in the development of OSA; it is the most significant predictor of sleep apnea. A recent study of obese men (BMI=30 kg/m2) without major medical illnesses indicated that 60% of them met criteria for sleep-disordered breathing and 27% had obstructive sleep apnea.72 It is estimated that 60–90% of patients with sleep apnea are obese (defined as BMI>28 kg/m2), and that a BMI of 28 kg/m2 has a sensitivity of 93% and a specificity of 74% for sleep apnea.73 The risk of having moderate to severe sleep apnea over a four-year period increases six-fold among persons gaining 10% excess weight.74 Thus, the high incidence of cardiovascular morbidity among patients with OSA is explained in part by the presence of obesity.75
Initial reports on associations between sleep apnea with cardiovascular morbidity were thought to be confounded by obesity since both OSA and CVD are linked to obesity. It is believed that both conditions are caused by a defect in a common pathway potentially resulting from central (visceral) obesity. With the onset of OSA, patients develop leptin resistance, which in turn contributes to further weight gain.76 Leptin is an adipocyte-derived hormone that regulates weight by controlling appetite and energy expenditure. Plausibly, inflammatory cytokines TNFα and IL-6, which are associated with daytime sleepiness, might also be involved in the causal pathway as they are elevated among obese patients with OSA.76 New empirical evidence leads to the notion that the comorbid associations between OSA and CVD may be explained by the presence of the metabolic syndrome, particularly common among obese persons.
Obstructive sleep apnea and hypertension
One of the challenges limiting understanding of associations between OSA and CVD relates to the fact that both conditions are potentially characterized by similar pathogenetic mechanisms.77 Both sleep apnea and CVD are linked to hypertension.10 Multivariate analytical models have indicated that sleep apnea represents an independent risk factor for hypertension,10,78 and hypertension constitutes a significant predictor of cardiopulmonary deaths among patients with sleep apnea.78
Regarding the link between sleep apnea and hypertension, data suggests that approximately 40% of patients with sleep apnea suffer from hypertension, whereas 30% of hypertensive patients have occult sleep apnea.79 Data from the Wisconsin Sleep Cohort Study, sampling 1 060 women and men ages 30 to 60 years, showed that for individuals with a BMI of 30 kg/m2 an AHI of 15 was associated with blood pressure increases of 3.6 mmHg for systolic and 1.8 mmHg for diastolic. Further analyses indicated a dose-response relationship between sleep apnea and blood pressure, independent of confounding factors.10
Data from the same study exploring the relationship between sleep apnea and hypertension indicated that severity of sleep apnea based on initial sleep studies could predict newly diagnosed hypertension during the subsequent four year. Even with control for known confounders, analyses suggested the odds ratios for the presence of hypertension at follow-up were 1.42 with an AHI of 0.1 to 4.9 at baseline relative to none, 2.03 with an AHI of 5.0 to 14.9, and 2.89 with an AHI of 15.0 or more.80 These data are consistent with findings of the Sleep Heart Health Study, a community-based multicenter study involving 6 132 patients.81 Investigators found that mean systolic and diastolic blood pressure and prevalence of hypertension increased significantly with greater severity of OSA Notably, this observation held even at relatively low AHI levels (AHI=10). Furthermore, clinical evidence suggests that treatment of sleep apnea results in a diminution of daytime systemic blood pressure,82 although it has not been Conclusively demonstrated that CPAP treatment lowers blood pressure on a long-term basis.
Obstructive sleep apnea and diabetes
The obesity pandemic over the last decade has accompanied a rise the prevalence of type 2 diabetes mellitus. One of the characteristic features of diabetes mellitus is the inability to regulate serum glucose levels, resulting in impaired glucose tolerance affecting 11% to 15.6% of the US population.83 Research conducted to define the biochemistry of the insulin-response pathway has shown that both type 1 and type 2 diabetes are associated with insulin deficiency, but type 2 diabetes is further complicated by cellular resistance to insulin action. According to data from the Third National Health and Nutrition Examination Survey, 5.1%. of US adults have an existing diagnosis for diabetes; an additional 2.7% met criteria for the diagnosis, but have yet to receive one.83 Analysis from the same research group indicated that 15.6% of American adults exhibit glucose intolerance (140 mg/dL) and 6.9% showed impaired fasting glucose levels (≥110 mg/dL).83 According to the NIH, diabetes mellitus is the sixth leading cause of disease-related deaths in the US.
On a parallel tract, there is a growing body of evidence suggesting that OSA is involved in the pathogenesis of altered glucose metabolism A number of epidemiologic and experimental studies have shown that patients with OSA have increased glucose levels and increased insulin resistance,84 which might predispose afflicted individuals to developing type 2 diabetes mellitus. Cross-sectional data suggest that associations of sleep apnea with greater glucose levels and increased insulin resistance might be independent of the presence of obesity.76 It is known that both obese and non-obese patients with sleep apnea are insulin resistant, whereas not all apnea patients are obese. More specifically, investigators have proposed the following likely scenario. Sleep apnea causes an increase in sympathetic activity,57 and increased sympathetic activity impairs glucose homeostasis by enhancing glycogen breakdown and gluconeogenesis.85 Hence, recurrent hypoxemia along with abnormal sympathetic activity, commonly observed among patients with sleep apnea, might mediate the relationships between insulin resistance and sleep apnea.
Data from the Sleep Heart Health Study, which enrolled 2 000 patients, indicated that the prevalence of two-hour glucose tolerance values increased from 9.3% among patients with an AHI<5 to 15% among those with an AHI>15.86
The odds ratio for having an abnormal glucose tolerance was 1.44 among patients with an AHI ≥15. Results of that study also indicated that insulin resistance was also greatest among the latter group. This study provided evidence that apnea-induced hypoxemia is associated with glucose intolerance and insulin resistance.86 Moreover, data from the Nurse’s Health Study suggest that curtailed sleep duration resulting from sleep fragmentation induced by sleep apnea may also lead to the development or exacerbation of type 2 diabetes mellitus.87 This is corroborated by analysis of data from the Sleep Heart Health Study.88
Compared with individuals sleeping 7 to 8 hours per night, individuals sleeping ≤5 hours or <6 hour per night had adjusted odds ratios for diabetes of 2.51 and 1.66, respectively. Indeed, data suggests that the associations between sleep apnea and diabetes might be mediated through obesity, a common risk factor,89 although the prevalence of periodic breathing itself remained significantly higher among diabetic individuals, even after control for covariates. Thus, more definitive explanation of these relations awaits further empirical studies.
Given the potential effects of reduced sleep on glucose metabolism, one wonders about the overall, long-term health impact of curtailed sleep time on American adults. Converging data indicate that the US population has been sleeping less and less.90 Interestingly, although sleep duration is a strong predictor of morbidity and mortality, among American adults we found that the quality of one’s well-being hinged on the quality, rather than on the quantity of one’s sleep.91 Based on the most recent report by investigators from the University of California, San Diego who studied over one million men and women ages 30 to 102 years, the greatest longevity was observed among individuals sleeping seven hours per night. Those who slept eight hours or more experienced significantly increased mortality risks, as did participants who reported sleeping-six hours or less.92
If an independent association between sleep apnea and impaired glucose metabolism can be shown, this might offer another mechanism to explain increased cardiovascular morbidity. Evidently, this will require better delineation of the contribution of cytokines and leptin. In support of such hypotheses, investigators have pointed out that CPAP studies produced significant improvement in insulin sensitivity and left ventricular function with a corresponding decrease in blood pressure.84 CPAP therapy can also normalize leptin levels, thereby reducing central obesity. We note, however, that some studies have not shown significant improvement in metabolic disorders subsequent to CPAP treatment, but those clinical studies had several limitations. These include limited treatment compliance, inadequate duration of treatment, and some may have been underpowered to detect statistical effects. In light of such evidence, therapeutic approaches might integrate methods to increase sleep time both via reduction of sleep apnea severity as well as through lifestyle modifications. Synergystically, these would confer significant benefits in the management of cardiovascular complications, resulting from uncontrolled diabetes and/or untreated sleep apnea.
Obstructive sleep apnea and dyslipidemia
Dyslipidemia is another condition in the metabolic syndrome constellation. It is primarily a disorder of lipoprotein metabolism, usually caused by excessively high cholesterol levels. It is a known risk factor in the development of coronary artery disease,93 and it is highly prevalent among hypertensive adults. Data from the Multi-Ethnic Study of Atherosclerosis, a multicenter study of 6 814 persons ages 45 to 84 years, indicated that 29.3% met criteria for dyslipidemia.94 In that study, the prevalence of dyslipidemia was similar among ethnic groups, although a disproportionate number of African Americans and Hispanics, relative to Caucasians, did not receive treatment to control their dyslipidemia.94 These findings were inconsistent with data obtained from the GENOA study, indicating that the prevalence of dyslipidemia was significantly greater among Caucasians than among African Americans. Among women, rates were 64.7% and 49.5% respectively; whereas for men, rates were 78.4% and 56.7%, respectively.95 Patterns of treatment were nonetheless similar, favoring better treatment for Caucasians.
Two factors that commonly define dyslipidemia (i.e., high triglyceride levels and low high-density lipoprotein concentrations) are affected by obesity, a common predictor of OSA and cardiovascular morbidity. With increased adiposity, a commensurate increase in triglyceride levels is observed, whereas high-density lipoprotein levels decrease.96 Given that most of the available evidence comes from cross-sectional data, it remains a daunting task to establish direct causality. In that regard, it cannot be said that dyslipidemia causes OSA or that OSA causes dyslipidemia, although the two conditions tend to aggregate among patient with increased adiposity. It would certainly help to view these association in the context of data pointing to a direct correlation between lipid profile and cortical arousals, as often observed among patients with sleep apnea. Patients with OSA exhibit greater HDL dysfunction and oxidized LDL levels compared with matched control persons.97 Of note, AHI explained 30% of the variance in HDL dysfunction in sleep apnea.
Moreover, clinical evidence indicates that patients with abnormal serum lipid/lipoprotein levels improved significantly with CPAP or BiPAP therapy.98 In that follow-up (six months) study of 127 patients, investigators observed that the mean HDL-C serum level increased significantly by 5.8% This finding is in line with evidence that CPAP improved insulin secretion capacity and reduced leptin, total cholesterol, and low-density lipoprotein levels among patients with moderate-to-severe OSA.99 Such therapeutic interventions are consistent with the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III), recommending that reduction of dyslipidemia is a potential secondary target risk-reduction therapy.100
Conclusions
Vital statistics indicate that CVD is the leading cause of death among adults in developed countries. It has long been recognized that obesity, hypertension and diabetes are among the most important CVD risk factors. Based on data collected in the field of sleep medicine over the last four decades, there is abundant epidemiologic and clinical evidence pointing to obstructive sleep apnea as an important CVD risk factor as well. Plausibly, relationships among disorders forming the metabolic syndrome constellation point to a maladaptive autonomic response of chemoreceptor, reacting to hypoxia, hypercapnia, and acidosis commonly found in sleep apnea. Observational findings are plentiful, but experimental data explaining causal pathways between OSA and CVD are lacking. Available data suggest that activation of the sympathetic nervous system through hypoxemia and hypercapnia seems to provoke an inflammatory response engendering several downstream activities including hypertension, diabetes, and dyslipidemia.
While awaiting results of important clinical trials to elucidate complex associations between OSA and CVD, it may be a prudent practice to screen comprehensively for OSA among patients with known CVD and a suspicion of OSA There is ample evidence (Figure 3) that CPAP/BiPAP therapy is very effective in improving left ventricular ejection fraction and quality of life; it lowers blood pressure and sympathetic activity; it reduces mortality among patients with congestive heart failure; it lowers lipid levels; it improves insulin sensitivity; and it improves, mood. Evidence indicates that CPAP treatment reduces risks of cardiovascular death and likelihood of hospitalization for heart failure.
Figure 3.

Demonstrated positive benefits of treating OSA with CPAP or bi-level positive airway pressure therapy.
Acknowledgments
This research was Supported by funding from the NIH/NCMHD (R01MD004113).
Footnotes
The apnea-hypopnea index (AHI) or respiratory disturbance index (RDI) refers to the total number of apneas (complete cessation of breathing lasting ≥10 s) and hypopneas (≥30% reduction in airflow associated with either a cortical arousal or SaO2 desaturations) divided by the patient’s total sleep time. The AHI or RDI provides a measure of the severity of sleep apnea. AHI <5 is considered normal; AHI values ≥5 and <15 are viewed as mild; AHI values ≥15 and ≤30 are moderate; and AHI values >30 indicate severe sleep apnea.
References
- 1.Coccagna G, Mantovani M, Brignani F, Parchi C, Lugaresi E. Tracheostomy in hypersomnia with periodic breathing. Bull Physiopathol Respir. 1972;8:1217–27. [PubMed] [Google Scholar]
- 2.Coccagna G, Mantovani M, Brignani F, Parchi C, Lugaresi E. Continuous recording of the pulmonary and systemic arterial pressure during sleep in syndromes of hypersomnia with periodic breathing. Bull Physiopathol Respir. 1972;8:1159–72. [PubMed] [Google Scholar]
- 3.Hedner J, Ejnell H, Sellgren J, Hedner T, Wallin G. Is high and fluctuating muscle nerve sympathetic activity in the sleep apnoea syndrome of pathogenetic importance for the development of hypertension? J Hypertens Suppl. 1988;6:SS29–S31. doi: 10.1097/00004872-198812040-00166. [DOI] [PubMed] [Google Scholar]
- 4.Stoohs RA, Guilleminault C, Itoi A, Dement WC. Traffic accidents in commercial long-haul truck drivers: the influence of sleep-disordered breathing and obesity. Sleep. 1994;17:619–23. [PubMed] [Google Scholar]
- 5.El Ad B, Lavie P. Effect of sleep apnea on cognition and mood. Int Rev Psychiatry. 2005;17:277–82. doi: 10.1080/09540260500104508. [DOI] [PubMed] [Google Scholar]
- 6.Starafkhaneh A, Giray N, Richardson P, Young T, Hirshkowit M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28:1405–11. doi: 10.1093/sleep/28.11.1405. [DOI] [PubMed] [Google Scholar]
- 7.Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young T, Finn L. Epidemiological insights into the public health burden of sleep disordered breathing: sex differences in survival among sleep clinic patients. Thorax. 1998;53(Suppl 3):S16–S9. doi: 10.1136/thx.53.2008.s16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. [Accessed on 2002 August 8];The National Commission on Sleep Disorders Research. cited 2009 November 5. Available at http://www-stanford.edu/-dement/overview-ncsdr.html.
- 10.Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, et al. Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med. 1997;157:1746–52. [PubMed] [Google Scholar]
- 11.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults [see comments] N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 12.Schechter MS. Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109:e69. doi: 10.1542/peds.109.4.e69. [DOI] [PubMed] [Google Scholar]
- 13.Ancoli-lsrael S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Sleep-disordered breathing in community-dwelling elderly. Sleep. 1991;14:496–500. doi: 10.1093/sleep/14.6.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meetze K, Gillespie MB, Lee FS. Obstructive sleep apnea: a comparison of black and white subjects. Laryngoscope. 2002;112:1271–4. doi: 10.1097/00005537-200207000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Redline S, Tishler P, Hans M, Tosteson T, Strohl K, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997;155:186–92. doi: 10.1164/ajrccm.155.1.9001310. [DOI] [PubMed] [Google Scholar]
- 16.Jean-Louis G, Zizi F, von Gizycki H, Dharawat A, Lazar J, Brown C. Evaluation of Sleep Apnea in a Sample of Black Patients. J Clin Sleep Med. 2008;15:421–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Jung R. Physiology and pathophysiology of sleep. Med Welt. 1965;24:1358–9. [PubMed] [Google Scholar]
- 18.Badr MS, Kawak A, Skatrud JB, Morrell MJ, Zahn BR, Babcock MA. Effect of induced hypocapnic hypopnea on upper airway patency in humans during NREM sleep. Respir Physiol. 1997;110:33–45. doi: 10.1016/s0034-5687(97)00072-8. [DOI] [PubMed] [Google Scholar]
- 19.Remmers JE, Launois S, Feroah T, Whitelaw WA. Mechanics of the pharynx in patients with obstructive sleep apnea. Prog Clin Biol Res. 1990;345:261–8. [PubMed] [Google Scholar]
- 20.Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:484. doi: 10.1146/annurev.me.27.020176.002341. [DOI] [PubMed] [Google Scholar]
- 21.Rechtshaffen A, Kales A. A manual of standardized terminoly, techniques, and scoring systems of sleep stages of human subjects. Los Angeles: UCLA Brain Information Service/Brain Research Institute; 1968. p. 10. [Google Scholar]
- 22.Chesson AL, Jr, Ferber RA, Fry JM, Grigg-Damberger M, Hartse KM, Hurwiry TD, et al. The indication for polysomnography and related procedures. Sleep. 1997;20:423–87. doi: 10.1093/sleep/20.6.423. [DOI] [PubMed] [Google Scholar]
- 23.Kryger MH, Roth T, Dement WC. MD Principles and, Practice of Sleep Medicine. 3. New York, NY: W B Saunders Co; 2002. [Google Scholar]
- 24.Stepnowsky CJ, Palau JJ, Gifford AL, Ancoli-Israel S. A self-management approach to improving continuous positive airway pressure adherence and outcomes. Behav Sleep Med. 2007;5:131–46. doi: 10.1080/15402000701190622. [DOI] [PubMed] [Google Scholar]
- 25.Strobel RJ, Rosen RC. Obesity and weight loss in obstructive sleep: apnea a critical review. Sleep. 1996;19:104–15. doi: 10.1093/sleep/19.2.104. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed 2008 August 24];The American Academy of Sleep Medicine (Practice Parameters) cited 2009 November 5. Available at: http://www.aasmnet.org/PracticeParameters.aspx.
- 27.Wright J, Johns R, Watt I, Melville A, Sheldon T. Health effects of obstructive sleep apnea and the effectiveness of continuous positive airways pressure: a systematic review of research evidence. BMJ. 1997;314:851–60. doi: 10.1136/bmj.314.7084.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenthal L, Gerhardstein R, Lumley A, Guido P, Day R, Syron ML, et al. CPAP therapy in patients with mild OSA implementation and treatment outcome. Sleep Med. 2000;1:215–20. doi: 10.1016/s1389-9457(00)00012-5. [DOI] [PubMed] [Google Scholar]
- 29.Phillipson EA. Sleep apnea — a major public health problem. N Engl J Med. 1993;328:1271–3. doi: 10.1056/NEJM199304293281712. [DOI] [PubMed] [Google Scholar]
- 30. [Accessed 2008 August 5];Report of the Scientific Committee on tobacco and health. citied 2009 November 5. Available at: http://www.dh.gov.uk/en/FreedomOfInformation/Freedomofinformationpublicationschemefeedback/FOIreleases/DH_4131889.
- 31.The National Commission on Sleep Disorders Research. Wake up America: a national sleep alert. Washington, DC: US Government Printing office; 2002. [Google Scholar]
- 32.Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, et al. Association of Nocturnal Arrhythmias with Sleep-Disordered Breathing. The Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173:910–6. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Partinen M, Guilleminault C. Evolution of obstructive sleep apnea syndrome. In: Partinen M, Guilleminault C, editors. Obstructive sleep apnea syndrome. New York, NY: Raven Press; 1990. pp. 15–23. [Google Scholar]
- 35.Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol. 1983;52:490–4. doi: 10.1016/0002-9149(83)90013-9. [DOI] [PubMed] [Google Scholar]
- 36.Hoffstein V, Mateika S. Cardiac arrhythmias, snoring, and sleep apnea. Chest. 1994;106:466–71. doi: 10.1378/chest.106.2.466. [DOI] [PubMed] [Google Scholar]
- 37.Strading J. Sleep Apnea Does Not Cause Cardiovascular Disease. Am J Respir Crit Care Med. 2004;169:148–9. doi: 10.1164/rccm.2310012. [DOI] [PubMed] [Google Scholar]
- 38.Kiely JL, McNicholas WT, Zgierska A, Gorecka D, Radzikowska M, Baranowska B, et al. Cardiovascular risk factors in patients with obstructive sleep apnea syndrome. Eur Respir J. 2000;16:128–33. doi: 10.1034/j.1399-3003.2000.16a23.x. [DOI] [PubMed] [Google Scholar]
- 39.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass TM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med J. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 40.Aartz M, Young T, Finn L, Skatrud JB, Bradley D. Association of stroke. Am J Respir Crit Care Med. 2005;172:1447–51. doi: 10.1164/rccm.200505-702OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brooks D, Homer RL, Render-Teixeira CL, Phillipson EA. Obstructive sleep apnea as a cause of systemic hypertension: evidence from a canine model. J Clin Invest. 1997;99:109. doi: 10.1172/JCI119120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Somers VK, Gami AS, Olsoi LJ. Treating sleep apnea in heart failure patients: promises but still no prizes. J Am Coll Cardiol. 2005;45:2012–4. doi: 10.1016/j.jacc.2005.02.081. [DOI] [PubMed] [Google Scholar]
- 43.Borer J. Heart rate: from risk marker to risk factor. Eur Heart J. 2008;10:F2–F6. [Google Scholar]
- 44.Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier NF, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 45.Gami AS, Pressman G, Caples SM. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;27:367. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 46.Shepard JW, Jr, Garrison MW, Grither DA, Evans R, Schweitzer PK. Relationship of ventricular ectopy to nocturnal oxygen desaturation in patients with chronic obstructive pulmonary disease. Am J Med. 1985;78:28–34. doi: 10.1016/0002-9343(85)90457-7. [DOI] [PubMed] [Google Scholar]
- 47.Dyken ME, Somers VK, Yamada T, Ren ZY, Zimmerman MB. Investigating the relationship between stroke and obstructive sleep apnea. Stroke. 1996;27:401–7. doi: 10.1161/01.str.27.3.401. [DOI] [PubMed] [Google Scholar]
- 48.Ip MS, Lam B, Chan LY, Zheng I, Tsang KW, Fung PC, et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med. 2000;162:2166–71. doi: 10.1164/ajrccm.162.6.2002126. [DOI] [PubMed] [Google Scholar]
- 49.Lavie L. Obstructive sleep apnea syndrome–an oxidative stress disorder. Sleep Med Rev. 2003;7:35–51. doi: 10.1053/smrv.2002.0261. [DOI] [PubMed] [Google Scholar]
- 50.Kasasbeh E, Chi DS, Krishnaswamy G. Inflammatory aspects of sleep apnea and their cardiovascular consequences. South Med J. 2006;99:58–67. doi: 10.1097/01.smj.0000197705.99639.50. [DOI] [PubMed] [Google Scholar]
- 51.Lavie L. Sleep-disordered breathing and cerebrovascular disease: a mechanistic approach. Neurol Clin. 2005;23:1059–75. doi: 10.1016/j.ncl.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 52.Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. 2003;107:1129–34. doi: 10.1161/01.cir.0000052627.99976.18. [DOI] [PubMed] [Google Scholar]
- 53.Ishida K, Kato M, Kato Y, Yanagihara K, Kinugasa Y, Kotani K, et al. Appropriate use of nasal continuous positive airway pressure decreases elevated C reactive protein in patients with obstructive sleep apnea. Chest. 2009;136:125–9. doi: 10.1378/chest.08-1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown G, Albers JJ, Fisher LD, Schafer SM, Lin JT, Kaplan C, et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N Engl J Med. 1990;323:1289–98. doi: 10.1056/NEJM199011083231901. [DOI] [PubMed] [Google Scholar]
- 55.Kaneko Y, Floras JS, Usui K, Plante J, Tkacova R, Kubo T, et al. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Engl J Med. 2003;348:1233–41. doi: 10.1056/NEJMoa022479. [DOI] [PubMed] [Google Scholar]
- 56.Malone S, Liu PP, Holloway R, Rutherford R, Xie A, Bradley TD. Obstructive sleep apnoea in patients with dilated cardiomyopathy: effects of continuous positive airway pressure. Lancet. 1991;338:1480–4. doi: 10.1016/0140-6736(91)92299-h. [DOI] [PubMed] [Google Scholar]
- 57.Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96:1897–904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buchner NJ, Sanner BM, Borgel J, Rump LC. Continuous positive airway pressure treatment of mild moderate obstructive sleep apnea reduces cardiovascular risk. Am J Respir Crit Care Med. 2007;176:1274–80. doi: 10.1164/rccm.200611-1588OC. [DOI] [PubMed] [Google Scholar]
- 59.Fletcher EC. Cardiovascular effects of continuously positive airway pressure in obstructive sleep apnea. Sleep. 2000;23(Suppl 4):S154–S7. [PubMed] [Google Scholar]
- 60.Parish JM, Adam T, Facchiano L. Relational of matabolic syndrome and obstructive sleep apnea. J Clin Sleep Med. 2007;3:467–72. [PMC free article] [PubMed] [Google Scholar]
- 61.Dorkova Z, Petrasova D, Molcanyiova A, Popovnakova M, Tkacova R. Effects continuous positive airway pressure on cardiovascular risk profile in patients with severe obstructive sleep apnea and metabolic syndrome. Chest. 2008;134:686–92. doi: 10.1378/chest.08-0556. [DOI] [PubMed] [Google Scholar]
- 62.Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome a global public health problem and a new definition. J Atheroscler Thromb. 2005;12:295–300. doi: 10.5551/jat.12.295. [DOI] [PubMed] [Google Scholar]
- 63.Grundy SM. A constellation of complications: the metabolic syndrome. Clin Cornerstone. 2005;7:36–45. doi: 10.1016/s1098-3597(05)80066-3. [DOI] [PubMed] [Google Scholar]
- 64.Alexander CM. The coming of age of the metabolic syndrome. Diabetes Care. 2003;26:3180–1. doi: 10.2337/diacare.26.11.3180. [DOI] [PubMed] [Google Scholar]
- 65.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 66.Ford ES. Prevalence of the metabolic, syndrome defined by the International Diabetes Federation among adult in the U. S. Diabetes Care. 2005;28:2745–9. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 67.Grundy SM. Metabolic syndrome scientific statement by the American Heart Association and the National Heart, Lung, and Blood Institute. Arterioscler Thromb Vasc Biol. 2005;25:2243–4. doi: 10.1161/01.ATV.0000189155.75833.c7. [DOI] [PubMed] [Google Scholar]
- 68.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 69.Reilly DF, Westgate EJ, FitzGerald GA. Peripheral circadian clocks in the vasculature. Arterioscler Thromb Vasc Biol. 2007;27:1694–705. doi: 10.1161/ATVBAHA.107.144923. [DOI] [PubMed] [Google Scholar]
- 70.Ivanov PC, Hu K, Hilton MF, Shea SA, Stanley HE. Endogenous circadian rhythm in human motor activity uncoupled from circardian influences on cardiac dynamics. Proc Natl Acad Sci U S A. 2007;104:20702–7. doi: 10.1073/pnas.0709957104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7. doi: 10.1161/hy1001.092640. [DOI] [PubMed] [Google Scholar]
- 72.Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–82. doi: 10.1164/ajrccm.165.5.2104087. [DOI] [PubMed] [Google Scholar]
- 73.Kushida CA, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med. 1997;127:581–7. doi: 10.7326/0003-4819-127-8_part_1-199710150-00001. [DOI] [PubMed] [Google Scholar]
- 74.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284:3015–21. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 75.Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP. Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J. 2004;25:735–41. doi: 10.1016/j.ehj.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 76.Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, et al. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–8. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 77.Marcus DM, Lynn J, Miller JJ, Chaundhary O, Thomas D, Chaudhary B. Sleep disorders: a risk factor for pseudotumor cerebri? J Neuroophthalmol. 2001;21:121–3. doi: 10.1097/00041327-200106000-00014. [DOI] [PubMed] [Google Scholar]
- 78.Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ. 2000;320:479–82. doi: 10.1136/bmj.320.7233.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fletcher EC. The relationship between systemic hypertension and obstructive sleep apnea: facts and theory. Am J Med. 1995;98:118–28. doi: 10.1016/S0002-9343(99)80395-7. [DOI] [PubMed] [Google Scholar]
- 80.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 81.Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283:1829–36. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- 82.Mayer J, Becker H, Brandenburg U, Penzel T, Peter JH, von Wichert P. Blood pressure apnea: results of long-term nasal continuous positive airway pressure therapy. Cardiology. 1991;79:84–92. doi: 10.1159/000174864. [DOI] [PubMed] [Google Scholar]
- 83.Harris MI. Diabetes in America: epidemiology and scope of the problem. Diabetes Care. 1998;21(Suppl 3):C11–C4. doi: 10.2337/diacare.21.3.c11. [DOI] [PubMed] [Google Scholar]
- 84.Punjabi NM, Polotsky VY. Disorders of glucose metabolism in sleep apnea. J Appl Physiol. 2005;99:1998–2007. doi: 10.1152/japplphysiol.00695.2005. [DOI] [PubMed] [Google Scholar]
- 85.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol. 2003;136:167–78. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 86.Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160:521–30. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 87.Ayas NT, White DP, Al Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 88.Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 89.Sanders MH, Givelber R. Sleep disordered breathing may not be an independent risk factor for diabetes, but diabetes may contribute to the occurrence of periodic breathing in sleep. Sleep Med. 2003;4:349–50. doi: 10.1016/s1389-9457(03)00118-7. [DOI] [PubMed] [Google Scholar]
- 90.Jean-Louis G, Kripke DF, Ancoli-Israel S, Klauber M, Sepulveda RS. Sleep duration, illumination, and activity patterns in a population sample: Effects of gender and ethnicity. Biol Psychiatry. 2000;47:921–7. doi: 10.1016/s0006-3223(99)00169-9. [DOI] [PubMed] [Google Scholar]
- 91.Jean-Louis G, Kripke DF, Ancoli-Israel S. Sleep and quality of well-being. Sleep. 2000;23:1115–21. [PubMed] [Google Scholar]
- 92.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 93.Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screens of the Multiple Risk Factor Intervention Trial (MRFLT) JAMA. 1986;256:2823–8. [PubMed] [Google Scholar]
- 94.Goff DC, Jr, D’Agostino RB, Jr, Haffner SM, Otvos JD. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metabolism. 2005;54:264–70. doi: 10.1016/j.metabol.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 95.O’Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–8. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- 96.Zgierska A, Gorecka D, Radzikowska M, Baranowska B, Plywaczewski R, Bednarek M, et al. Obstructive sleep apnea and risk factors for coronary artery disease. Pneumonol Alergol Pol. 2000;68:238–46. [PubMed] [Google Scholar]
- 97.Tan KC, Chow WS, Lam JC, Lam B, Wong WK, Tam S, et al. HDL dyslunction in obstructive sleep apnea. Atherosclerosis. 2006;184:377–82. doi: 10.1016/j.atherosclerosis.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 98.Borgel J, Sanner BM, Bittlinsky A, Keskin F, Bartels NK, Buechner N, et al. Obstructive sleep apnoea and its therapy influence high-density lipoprotein cholesterol serum levels. Eur Respir J. 2006;27:121–7. doi: 10.1183/09031936.06.00131304. [DOI] [PubMed] [Google Scholar]
- 99.Cuhadaroglu C, Utkusavas A, Ozturk L, Salman S, Ece I. Effects of nasal CPAP treatment on insulin resistance, lipid profile, and plasma leptin in sleep apnea. Lung. 2009;187:75–81. doi: 10.1007/s00408-008-9131-5. [DOI] [PubMed] [Google Scholar]
- 100.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]