Abstract
Study Objective:
Continuous positive airway pressure (CPAP) titration studies are commonly performed using a nasal mask but some patients may prefer a full-face or oronasal mask. There is little evidence regarding the equivalence of different mask interfaces used to initiate treatment. We hypothesized that oronasal breathing when using an oronasal mask increases upper airway collapsibility and that a higher pressure may be required to maintain airway patency. We also assessed patient preferences for the 2 mask interfaces.
Design:
Prospective, randomized, cross-over design with 2 consecutive CPAP titration nights.
Setting:
Accredited laboratory in a university hospital.
Patients or Participants:
Twenty-four treatment-naive subjects with obstructive sleep apnea syndrome and respiratory disturbance index of greater than 15 events per hour.
Interventions:
CPAP titration was performed using an auto-titrating machine with randomization to a nasal or oronasal mask, followed by a second titration night using the alternate mask style.
Measurements and Results:
There was no significant difference in the mean pressures determined between nasal and oronasal masks, although 43% of subjects had nasal-to-oronasal mask-pressure differences of 2 cm H2O or more. Residual respiratory events, arousals, and measured leak were all greater with the oronasal mask. Seventy-nine percent of subjects preferred the nasal mask.
Conclusions:
Patients with obstructive sleep apnea syndrome can generally switch between nasal and oronasal masks without changing machine pressure, although there are individual differences that may be clinically significant. Measured leak is greater with the oronasal mask. Most patients with obstructive sleep apnea syndrome prefer a nasal mask as the interface for initiation of CPAP.
Clinical Trial Registration:
Australian New Zealand Clinical Trials Registry (ANZCTR). ACTRN: ACTRN12611000243910. URL: http://www.ANZCTR.org.au/ACTRN12611000243910.aspx
Citation:
Teo M; Amis T; Lee S; Falland K; Lambert S; Wheatley J. Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. SLEEP 2011;34(7):951-955.
Keywords: Obstructive sleep apnea, continuous positive airway pressure, nasal, oronasal, mask leak
INTRODUCTION
The most commonly prescribed therapy for symptomatic obstructive sleep apnea syndrome (OSAS) is continuous positive airway pressure (CPAP). A number of studies have now demonstrated that properly adjusted CPAP therapy is effective at preventing snoring, upper airway obstruction, and oxygen desaturation, as well as reversing symptoms of OSAS.1 Traditionally, CPAP therapy is initiated at a fixed pressure following a titration procedure that may be undertaken manually overnight in a sleep-laboratory setting or, alternatively, by an automatic-titrating CPAP machine in the home or laboratory setting.2 Two of the main variables that are key to the initiation of effective CPAP therapy are the mask interface chosen and the final determined CPAP that is prescribed.
Although there are now well-documented practice parameters developed by the American Academy of Sleep Medicine for the initiation of CPAP therapy,1 there is little evidence available regarding the equivalence of different mask interfaces that may be used to initiate treatment. Currently, there are multiple different styles of mask interfaces available for treatment, and it is likely that patient acceptance of and adherence with CPAP therapy may be optimized by choosing the mask interface that provides the most effective and acceptable therapy regimen on an individual-patient basis. Most mask interfaces fall into 2 broad categories, either a nasal-only interface, which provides CPAP exclusively via the nasal route, or an oronasal interface, which delivers CPAP to both the nasal and oral routes.
A Cochrane review of CPAP-delivery interfaces for OSAS therapy concluded that the optimal interface for CPAP delivery remained unclear due to the limited number of studies available that compare interface types.3 In particular, there were few data available to guide the clinician as to whether the pressure required for CPAP delivered by an oronasal mask is equivalent to that required with a nasal-only mask.
When an oronasal mask is used as a CPAP interface, the CPAP is applied to the nasal route and can also be applied to the oral route, simply by opening the mouth. It has previously been demonstrated that mouth opening increases upper airway collapsibility.4,5 Therefore, we hypothesized that, because the upper airway may be more collapsible when breathing via the oronasal route, use of an oronasal mask would require a higher pressure to maintain upper airway patency, as compared with the nasal-only mask. To test this hypothesis, we randomly assigned patients to 2 separate CPAP-titration nights, which were identical apart from using an oronasal mask or a nasal mask, to clarify whether the CPAP interface type can influence the final determined CPAP.
METHODS
We studied 24 subjects who were referred to a sleep laboratory in a university hospital for CPAP titration. Patients had OSAS of at least moderate severity (respiratory disturbance index > 15 events/h) on a baseline polysomnogram and had no previous experience with CPAP. Subjects were excluded for previous oronasal operations, history of clinically severe nasal or sinus disease, complex sleep disordered breathing, significant comorbid respiratory or cardiac disease, and orofacial problems precluding the use of a nasal or oronasal mask. Informed consent was obtained, and the protocol was approved by the Sydney West Area Health Service Human Research Ethics Committee.
Protocol
Baseline data collection included measurement of anthropometric data and the Epworth Sleepiness Scale. Nasal resistance was measured using posterior rhinomanometry while the subjects were awake in the seated posture.6 Each subject underwent 2 consecutive, attended, full-polysomnography, CPAP-titration studies, with randomization (computer-generated first-night mask choice) to either a nasal (Resmed Micro Mirage, Sydney, Australia) or an oronasal (Resmed Quattro Mirage) mask on the first night, with the alternate mask style used on the second night. A chinstrap (Seatec, Sydney, Australia) was always used in conjunction with the nasal mask to reduce the occurrence of mouth leak. Heated humidification was used on both study nights. Sleep technicians fitted and adjusted the interface as per the manufacturer's recommendations and provided patient support during the night as required.
Subjects were monitored with standard polysomnography,7 including direct measurement of pressure in the mask, together with the pressure, flow, and leak output signals from the CPAP device, with all signals recorded on a computerized monitoring system (Compumedics Profusion 3, Abbotsford, Australia). CPAP was automatically titrated with the same Autoset S8 II Spirit CPAP device (Resmed) on both nights, and sleep technicians did not manually titrate pressure.
On the morning following each CPAP study, the patient's subjective perception of sleep quality, mask comfort and fit, mouth dryness, and overall satisfaction with each mask style was assessed using a 10-point visual analogue scale (0 = poorest, 10 = best). At the conclusion of both studies, they were asked to nominate their preferred mask style.
Data Analysis
Studies were scored according to standard guidelines8,9 for sleep staging, arousals, and respiratory events. All polysomnograms were scored by 1 sleep technician who was blinded to the interface used, with calculation of the respiratory disturbance index, arousal index, sleep efficiency, total sleep time, wake after sleep onset time, and time spent in each sleep stage. The summary data from the CPAP device were also downloaded to obtain the 95th percentile pressure level and 95th percentile leak, as computed by the device. Because both mask interfaces and the CPAP device were compatible Resmed products, the leak data downloaded from the device only reflected the unintentional leak (mask cushion seal leak or mouth leak [nasal mask]) over and above the intentional mask leak (related to individual mask dead-space washout).
All scored polysomnograms were also reviewed by a single sleep physician who was blinded to the interface used and the summary data from the CPAP device. Concealment of interface style was maintained by de-identifying each subject's study data prior to scoring and reporting, with only 1 researcher (MT) aware of which study interface was used. The physician-determined pressure (PDP) was the final prescribed CPAP level for each study based on the minimum pressure required to abolish all obstructive events, oxygen desaturations, and snoring, with pressures above this level assessed for improvement in the nasal pressure flow profile, and the PDP that minimized flow limitation prescribed, provided that mask leak was not increased.
Group data were expressed as mean values (± SD). Variables were compared between nasal and oronasal mask nights using paired t-test analysis. A P value of < 0.05 was regarded as statistically significant.
RESULTS
The study-group characteristics and baseline diagnostic polysomnography data are presented in Table 1. The subjects were generally middle-aged obese men and had severe obstructive sleep apnea syndrome. Two patients had awake nasal resistances that were elevated above the upper limit of the reference range (3.3 cm H2O·L−1·sec−1) at 6.5 and 8.9 cm H2O·L−1·sec−1. Eleven subjects used a nasal mask on the first night, whereas the remaining 13 subjects used an oronasal mask on the first night.
Table 1.
Characteristics of the 24 study participants
| Parameter | Results |
|---|---|
| Age, y | 51.3 ± 13.3 |
| Male sex, no. | 18 |
| BMI, kg/m2 | 33.8 ± 9.4 |
| Neck circumference, cm | 41.7 ± 4.8 |
| RDI, events/h | 47.0 ± 15.2 |
| AI, events/h | 35.9 ± 15.8 |
| Min O2 sat, % | 79.3 ± 14.2 |
Data are presented as mean ± SD. BMI, body mass index; RDI, respiratory disturbance index; AI, arousal index; Min O2 sat, minimum oxygen saturation.
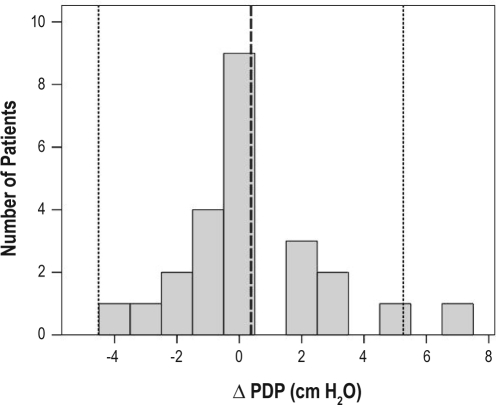
The PDP when using the nasal mask was 11.4 ± 1.9 cm H2O, which was not different from that determined when using the oronasal mask (11.8 ± 2.4 cm H2O; P = 0.46). The 95th percentile pressure (determined by the CPAP device) when using the nasal mask was 12.2 ± 2.2 cm H2O, which also did not differ from that determined when using the oronasal mask (11.9 ± 1.4 cm H2O; P = 0.48). When PDP values were compared with device-determined pressures, there was no difference in group mean pressure for the oronasal mask (P = 0.73). However, for the nasal mask, the device-determined pressure (12.2 ± 2.2 cm H2O) was significantly higher than the PDP (11.4 ± 1.9 cm H2O; P = 0.01), with a mean difference of 0.8 cm H2O. For the PDP measurements, we calculated the difference between the nasal and oronasal mask values for each individual subject (Figure 1). When the distribution of pressure differences was examined, only 1 patient's pressure difference was more than 2 standard deviations from the mean. The majority of patients had pressure differences of less than 2 cm H2O. However, 11 subjects (or 46%) had differences of 2 cm H2O or greater. The 2 subjects with elevated awake nasal resistances both had pressure differences of less than 2 cm H2O.
Figure 1.
A frequency histogram for the PDP (physician-determined pressure) for patients when they used the oronasal (ON) mask minus the PDP using the nasal (N) mask (Δ PDP). Note that 11 of 24 subjects had a Δ PDP of ≥ ± 2 cm H2O, and 1 subject had a difference of +7 cm H2O. (The dashed line refers to the mean Δ PDP = 0.4 cm H2O; dotted lines, ± 2 SD)
We compared the polysomnography titration outcomes by mask style for the 2 nights (Table 2). The residual respiratory disturbance index and the arousal index were higher when using the oronasal mask. In addition, the 95th percentile leak doubled with the oronasal mask. There was also a trend toward a lower sleep efficiency when using an oronasal mask; however, this difference did not reach statistical significance.
Table 2.
Titration outcomes by mask style
| Nasal Mask | Oronasal Mask | P Value | |
|---|---|---|---|
| RDI, events/h | 5.3 ± 3.4 | 11.0 ± 10.4 | 0.01 |
| Sleep efficiency (%) | 82.3 ± 13.6 | 75.7 ± 15.8 | 0.11 |
| AI, events/h | 13.3 ± 7.3 | 17.6 ± 9.6 | 0.02 |
| 95th percentile leak, L/min | 11.2 ± 8.1 | 22.1 ± 9.9 | < 0.001 |
Data are presented as mean ± SD. RDI, respiratory disturbance index; AI, arousal index.
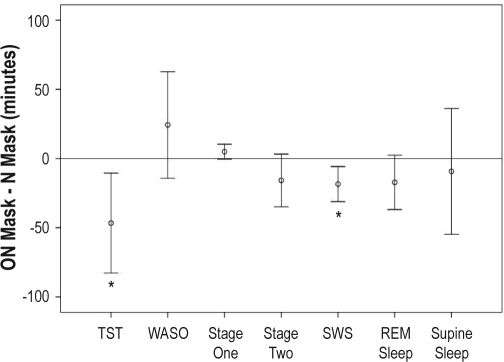
Differences in sleep architecture were measured between the 2 titration nights (Figure 2). When patients used the oronasal mask, there was a significantly reduced amount of total sleep time (oronasal = 319 ± 76 min, nasal = 366 ± 65 min; P = 0.01) and time spent in slow wave sleep (oronasal = 76 ± 39 min, nasal = 94 ± 36 min; P < 0.01). There were no significant differences between the 2 mask styles for the quantities of stages 1 and 2 non-rapid eye movement sleep, rapid eye movement sleep, and supine sleep.
Figure 2.
Durations of sleep variables, based on the results of 2 nights of polysomnography. Data represent the durations on the nights with continuous positive airway pressure titration using an oronasal (ON) mask minus the durations of these same variables from the nights on which a nasal (N) mask was used. TST refers to total sleep time; WASO, wake after sleep onset; SWS, slow wave sleep; REM, rapid eye movement. Open circles refer to the mean difference; bars, ± 1 SD; *P < 0.05.
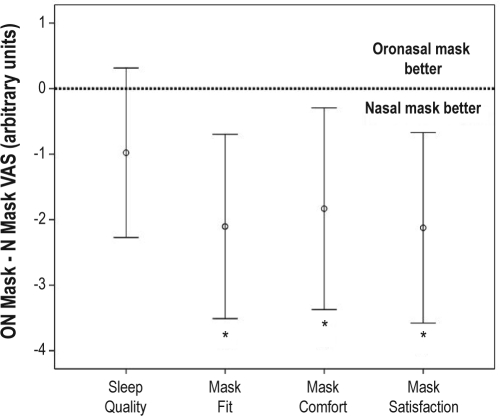
Patients rated nasal masks as better fitting (nasal = 7.5 ± 1.9 arbitrary units [au], oronasal = 5.4 ± 2.6 au; P < 0.01), and more comfortable (nasal = 6.3 ± 2.1 au, oronasal = 4.4 ± 2.6 au; P = 0.02). Overall satisfaction was also greater with the nasal mask (6.7 ± 2.1 au), compared with the oronasal mask (4.5 ± 2.6 au; P < 0.01). Perceived sleep quality was not different when using a nasal mask (6.2 ± 2.2 au), compared with an oronasal mask (5.2 ± 2.2 au; P = 0.13). Figure 3 shows the differences in visual analogue scale scores between the 2 nights. Seven patients reported dry mouth when using a nasal mask, compared with 16 subjects when using an oronasal mask. Overall, 19 patients nominated the nasal mask as their preferred interface, 4 patients chose the oronasal mask, and 1 patient was undecided.
Figure 3.
Scores from the visual analogue scales (VAS) for patients undergoing continuous positive airway pressure titration with an oronasal (ON) mask minus their scores from the night they used a nasal (N) mask. Open circles represent mean differences; bars, ± 1 SD; *P < 0.05.
DISCUSSION
In a group of patients with newly diagnosed OSAS commencing CPAP therapy, there was no significant difference in either the PDP or machine-determined pressures for the prescribed therapeutic CPAP levels, as measured via CPAP titration using a nasal versus an oronasal mask. However, CPAP titration with an oronasal mask, as compared with a nasal mask, was characterized by increased mask leak, increased residual respiratory disturbance and arousal indexes, decreased amount of slow wave sleep, and decreased amount of total sleep time on the titration night. From a subjective viewpoint, patients expressed a preference for the nasal mask, particularly in relation to mask fit and mask comfort.
This study is the first to directly compare the pressures determined using different mask interfaces on separate CPAP-titration nights in a group of patients who did not have any prior CPAP experience. In contrast, the 5 patients studied by Prosise et al.10 had previously used nasal CPAP for periods ranging from 6 months to 3 years and did not have a separate CPAP titration performed using an oronasal mask. They concluded that an effective level of CPAP applied with a nasal mask was similarly effective, compared with an oronasal mask, but were unable to conclude that the optimal level of CPAP had been delivered by the oronasal mask. In our group, the level of CPAP titrated differed between the 2 interfaces by 2 cm H2O or more in 11 subjects, suggesting that there are interindividual differences that may be clinically significant. We did not study night-to-night variability in titrated pressure using the same interface, but there is some evidence from home-based automatic CPAP titration that the determined pressure does not demonstrate significant variance over a 1-week period.11 Our data suggested that differences in body position or elevated nasal resistances were unlikely to account for any differences in the titrated pressure between the 2 test nights. Interestingly, there are no American Academy of Sleep Medicine practice parameter1 recommendations that provide guidance as to what would be the minimum difference in titrated pressure that is likely to be of clinical significance. Meurice et al.12 studied the effect of treatment pressure set with 2 different titration methods, either to eliminate flow limitation (mean pressure 10.4 ± 2.6 cm H2O) or to eliminate apnea, hypopnea, and snoring (mean pressure 8.9 ± 2.6 cm H2O), with a resultant mean treatment pressure difference of 1.5 cm H2O. They reported a longer nightly duration of CPAP use in the group treated for flow limitation (7.3 h vs 6.0 h), which, if maintained over a longer period, could potentially translate into meaningful clinical outcomes.
In the present study, there was only 1 patient whose determined pressure difference was more than 2 standard deviations above the mean (7 cm H2O higher) when using an oronasal mask, compared with a nasal mask. This particular patient also had a much higher 95th percentile leak when using the oronasal mask (44 L/min) compared with the nasal mask (18L/min). The higher oronasal mask-determined pressure in this patient may therefore reflect titration difficulties encountered by the automatic CPAP device in the presence of a large leak. It has also been demonstrated that automatic CPAP devices may have a tendency to pressure overshoot if there are increased arousals and fragmented sleep,13 which was the case with the oronasal mask. An alternative explanation for the high pressure difference may relate to a bimodal distribution of pressure differences, with a small group of patients always requiring higher pressures with an oronasal mask.
The role of the mask style was studied by Mortimore et al.14 in 20 patients with newly diagnosed OSAS following a 1-night nasal-mask CPAP-titration study. Patients were then randomly assigned to CPAP with a nasal or oronasal mask at the same fixed pressure for 4 weeks each. This study demonstrated that compliance was greater with the nasal mask CPAP, with a corresponding larger reduction in the Epworth Sleepiness Scale score, and the authors attributed this finding to improved overall mask comfort. However, the possible impact of suboptimal pressure titration for the oronasal mask, leading to less effective therapy and reduced compliance, was not able to be addressed by this study. There are data to suggest that both mask style and CPAP pressure are important determinants of ongoing CPAP compliance.12,14
In our study, use of an oronasal mask for CPAP titration was associated with less consolidated sleep, with decreased total sleep time and reduced slow wave sleep. Similarly, Prosise et al.10 found significantly less stage 2 non-rapid eye movement sleep when using an oronasal mask, as well as a trend toward a decreased total sleep time, increased wakefulness, and increased amount of stage 1 non-rapid eye movement sleep. These differences in sleep architecture seen with use of an oronasal mask during initial titration may not necessarily be the case following a period of acclimatization and treatment at a fixed pressure of CPAP with this interface. However, a study by Drake et al.15 found that improvement in sleep efficiency from the diagnostic night to the titration night was the best predictor of subsequent CPAP compliance. Thus, it is plausible that a better first-night effect (as occurred with the nasal mask night in our study) will carry over to better patient acceptance and adherence to long-term therapy.
There was a clear patient preference for use of a nasal mask following a 1-night trial of each interface in our study. Similarly, Mortimore et al.14 reported that, in a group of 20 patients commencing CPAP, 19 patients preferred a nasal mask over an oronasal mask, following a 4-week trial of each mask interface. The patients in our study reported increased mouth dryness when using an oronasal mask, as compared with a nasal mask, most likely due to the minimization of mouth leak by use of a chin-strap with the nasal mask, whereas significant mouth breathing may have persisted with an oronasal mask. Overall, our data clearly demonstrated that the leak is doubled by the use of an oronasal mask, suggesting that it is inherently more difficult to achieve a good seal with these interfaces, which may complicate the delivery of therapy in some cases.
Strengths of this study include the use of an automatic titrating CPAP device to objectively provide an algorithm-based titration and minimize pressure-titration variability between the 2 nights, such as may have occurred with a manual titration. Adequacy of determined pressure was reviewed in a blinded fashion by an experienced sleep physician, and all CPAP titrations were judged to have provided an adequate level of CPAP using the automatic device. Another strength of the study was the quantitative measure of leak provided by the automatic CPAP machine, which has not been assessed in previous studies comparing interfaces, all of which have relied on subjective assessment of leak.14,16,17
Limitations of this study include the relatively small sample size, which may have hampered our ability to detect either small differences in mean determined pressure or any bimodal distribution of pressure differences. However, it remains unclear whether a small significant pressure difference of less than 1 cm H2O, if demonstrated in a much larger sample size, would have any clinically significant meaning. In addition, we have only used 1 brand of automatic-titrating CPAP machine with the correctly sized manufacturer's mask, which may limit the generalizability of results to other mask styles and CPAP machines. Finally, our results may not be applicable to a situation in which a nasal mask is used without a properly fitted chin strap.
We were unable to assess the degree of mouth opening or the separate contributions of oral and nasal airflows when patients used an oronasal mask. This would have been of particular interest, as the degree of mouth opening may have altered upper airway anatomy and collapsibility,4,5 which may have explained some of the variability in determined pressure between nasal and oronasal masks. It has previously been demonstrated that mouth opening increases collapsibility of the upper airway,4 possibly by posterior-inferior mandibular displacement, resulting in narrowing of the oropharyngeal cross-sectional area. This mandibular displacement may also adversely impact the length-tension relationships of the upper airway dilator muscles, thereby reducing their contractile force.5 In addition, soft-palate apposition with the tongue may be lost with the use of an oronasal mask, further reducing the patency of the oropharynx. Thus, the degree of mouth opening and associated posterior displacement of the tongue base may substantially increase the CPAP required to maintain airway patency, and it is possible that the individual configuration of upper airway anatomy when using the oronasal mask may explain some of the variability in pressure between the different interface styles.
In conclusion, for the initial titration of CPAP in patients with OSAS, nasal and oronasal masks are interchangeable in terms of the final determined pressure, although there are individual differences that may be clinically significant. In addition, patients prefer the use of nasal masks, which fit better, are more comfortable, leak less, result in longer and better quality sleep, and are generally cheaper. Thus, our study supports the use of a nasal mask as the initial interface of choice in titrating CPAP for patients with OSAS, and we speculate that this may translate into improved longer-term adherence to CPAP treatment with better clinical outcomes. However, this would require confirmation by future studies comparing outcomes for the use of oronasal versus nasal masks in longer-term CPAP therapy.
DISCLOSURE STATEMENT
Automatic titrating CPAP machine, nasal and oronasal masks were provided courtesy of ResMed Australia. Dr. Wheatley has participated in clinical trial research projects funded by Actelion, Apnex Medical, Boehringer Ingelheim, and GlaxoSmithKline The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Resmed, Sydney, NSW, Australia, for supplying nasal and oronasal masks for this study, as well as the automatic titrating continuous positive airway pressure machine. All work was performed at Westmead Hospital.
REFERENCES
- 1.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 2.Littner M, Hirshkowitz M, Davila D, et al. Practice parameters for the use of auto-titrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome. Sleep. 2002;25:143–7. doi: 10.1093/sleep/25.2.143. [DOI] [PubMed] [Google Scholar]
- 3.Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;4:CD005308. doi: 10.1002/14651858.CD005308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meurice JC, Marc I, Carrier G, Series F. Effects of mouth opening on upper airway collapsibility in normal sleeping subjects. Am J Respir Crit Care Med. 1996;153:255–9. doi: 10.1164/ajrccm.153.1.8542125. [DOI] [PubMed] [Google Scholar]
- 5.Kuna ST, Remmers JE. Neural and anatomic factors related to upper airway occlusion during sleep. Med Clin North Am. 1985;69:1221–42. doi: 10.1016/s0025-7125(16)30984-1. [DOI] [PubMed] [Google Scholar]
- 6.Wheatley JR, Amis TC, Engel LA. Nasal and oral airway pressure-flow relationships. J Appl Physiol. 1991;71:2317–24. doi: 10.1152/jappl.1991.71.6.2317. [DOI] [PubMed] [Google Scholar]
- 7.Kushida CA, Littner MR, Morgenthaler T, et al. Parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 8.The Report of an American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 9.Rechtschaffen A, Kales A, editors. A Manual of Standardized Terminology, Techniques, and Scoring System for Sleep Stages of Human Subjects. US Department of Health, Education, and Welfare Public Health Service—NIH/NIND; 1968. [Google Scholar]
- 10.Prosise GL, Berry RB. Oral-nasal continuous positive airway pressure as a treatment for obstructive sleep apnea. Chest. 1994;106:180–6. doi: 10.1378/chest.106.1.180. [DOI] [PubMed] [Google Scholar]
- 11.Series F, Plante J, Lacasse Y. Reliability of home CPAP titration with different automatic CPAP devices. Resp Res. 2008;9:56. doi: 10.1186/1465-9921-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meurice JC, Paquereau J, Denjean A, Patte F, Series F. Influence of correction of flow limitation on continuous positive airway pressure efficiency in sleep apnoea/hypopnoea syndrome. Eur Respir J. 1998;11:1121–7. doi: 10.1183/09031936.98.11051121. [DOI] [PubMed] [Google Scholar]
- 13.Marrone O, Insalaco G, Bonsignore MR, Romano S, Salvaggio A, Bonsignore G. Sleep structure correlates of continuous positive airway pressure variations during application of an autotitrating continuous positive airway pressure machine in patients with obstructive sleep apnea syndrome. Chest. 2002;121:759–67. doi: 10.1378/chest.121.3.759. [DOI] [PubMed] [Google Scholar]
- 14.Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53:290–2. doi: 10.1136/thx.53.4.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drake CL, Day R, Hudgel D, Stefadu Y, Parks M, Syron ML, Roth T. Sleep during titration predicts continuous positive airway pressure compliance. Sleep. 2003;26:308–11. doi: 10.1093/sleep/26.3.308. [DOI] [PubMed] [Google Scholar]
- 16.Wilson GN, Piper AJ, Norman M, et al. Nasal versus full face mask for non-invasive ventilation in chronic respiratory failure. Eur Respir J. 2004;23:605–9. doi: 10.1183/09031936.04.00051604. [DOI] [PubMed] [Google Scholar]
- 17.Criner GJ, Travaline JM, Brennan KJ, Kreimer DT. Efficacy of a new full face mask for non-invasive positive pressure ventilation. Chest. 1994;106:1109–15. doi: 10.1378/chest.106.4.1109. [DOI] [PubMed] [Google Scholar]