Abstract
OBJECTIVE:
To describe the rate of increase of the population of adults seeking care as inpatients in children's hospitals over time.
PATIENTS AND METHODS:
We analyzed data from January 1, 1999, to December 31, 2008, from patients hospitalized at 30 academic children's hospitals, including growth rates according to age group (pediatric: aged <18 years; transitional: aged 18–21 years; or adult: aged >21 years) and disease.
RESULTS:
There were 3 343 194 hospital discharges for 2 143 696 patients. Transitional patients represented 2.0%, and adults represented 0.8%, totaling 59 974 patients older than 18 years. The number of unique patients, admissions, patient-days, and charges increased in all age groups over the study period and are projected to continue to increase. Resource use was disproportionately higher in the older ages. The growth of transitional patients exceeded that of others, with 6.9% average annual increase in discharges, 7.6% in patient-days, and 15% in charges. Chronic conditions occurred in 87% of adults compared with 48% of pediatric patients. Compared with pediatric patients, the rates of increase of inpatient-days increased significantly for transitional age patients with cystic fibrosis, malignant neoplasms, and epilepsy, and for adults with cerebral palsy. Annual growth rates of charges increased for transitional and adult patients for all diagnoses except cystic fibrosis and sickle cell disease.
CONCLUSIONS:
The population of adults with diseases originating in childhood who are hospitalized at children's hospitals is increasing, with varying disease-specific changes over time. Our findings underscore the need for proactive identification of strategies to care for adult survivors of pediatric diseases.
Keywords: inpatients, hospitals, pediatric, congenital diseases, chronic conditions, adult patients, age groups
WHAT'S KNOWN ON THIS SUBJECT:
Health care innovations have improved survival in children with conditions previously fatal in childhood. Implications for specific diseases have been reported, but little information is available on disease comparisons or population increases in adult survivors of childhood illness.
WHAT THIS STUDY ADDS:
In this study of adults with chronic childhood diseases treated at 30 children's hospitals over a 10-year period, 6 conditions were compared and patient population growth was projected. The disparity between diagnoses suggests the existence of systemic barriers to the transition of these patients to adult health care providers.
Children's hospitals and pediatric providers have been instrumental in achieving improved outcomes of patients with conditions as diverse as congenital heart disease (CHD), cystic fibrosis (CF), chromosomal abnormalities, and epilepsy. Survival well into the middle decades of life is now common for many diseases that were historically fatal in childhood.1–4 However, these successes create new challenges for the patients, their families, and the health care system.5–7 Every year at least 500 000 to 750 000 young people with special health care issues become adults.8,9 As patients survive past historical age limits, they become vulnerable to acquired conditions. Pediatric providers may be ill equipped to treat the adult medical needs of these patients, whereas providers and hospitals that specialize in care of adult patients may have insufficient expertise to manage the adult manifestations of conditions that originate in childhood.5 Although patients' needs within specific disease categories have been characterized,4,10–30 few investigators have looked at this patient population in aggregate, and the utilization of inpatient treatment facilities by these patients has been poorly described.31–34 As efforts to reform health care intensify, an assessment of hospital care for adults with chronic conditions originating in childhood is needed to facilitate the optimal allocation of resources to meet the needs of this population.
To inform policy and prepare children's hospitals for this changing demographic group, we investigated hospitalizations of adults at children's hospitals to determine (1) the growth of this population, (2) differences between transitional (aged 18–21 years) and older patients, and (3) projections for future growth. We hypothesized that children's hospitals are caring for increasing numbers of adults and that changes vary according to chronic condition.
METHODS
Human Subject Protection
This study was approved by the institutional review board at Children's Memorial Hospital.
Data Sources and Quality
Data were obtained from the Pediatric Health Information System (PHIS), which contains inpatient demographic, diagnosis, procedure, and resource utilization data from 41 freestanding, tertiary care children's hospitals. PHIS-participating hospitals are affiliated with the Child Health Corporation of America (CHCA), a business alliance of children's hospitals, and account for ∼20% of all tertiary care at general (rather than subspecialty) children's hospitals. Located in 23 states and the District of Columbia, no more than 1 hospital is present in a specific region. Data quality and reliability are assured through a joint effort between CHCA and participating hospitals as previously described.35,36
Patients
We focused on hospital care for adults with conditions originating in childhood and compared 3 age groups: pediatric (<18 years old); transitional (18–21 years), and adult patients (>21 years).
Inclusion and Exclusion Criteria
We included patients who were discharged from the 30 participating hospitals that had available data for the entire 10-year period from January 1, 1999, to December 31, 2008. The other 11 freestanding tertiary care PHIS children's hospitals did not have complete data for the period of analysis.
We excluded patients who were admitted for conditions of pregnancy and their healthy newborns. Only a few of the hospitals have obstetrical services, and the majority of delivered newborns are healthy. Because healthy newborns have markedly lower resource utilization and shorter lengths of stay, the inclusion of their data would have biased the pediatric age group toward less cost and resource use at hospitals providing obstetric services.
Assignment of Primary Underlying Condition
Up to 21 diagnostic fields were permitted for each patient. Our intention was to identify the primary underlying condition for which the patient was seen at the hospital, with the acknowledgment that subsequent complicating conditions may also be present. For each patient all discharge diagnoses (principal diagnosis and secondary diagnoses) coded according to the International Classification of Diseases, Ninth Revision, were listed. We then assigned each patient to a single mutually exclusive diagnostic category by sequentially searching the list and using the hierarchy listed in the Appendix. Once assigned to a diagnosis, the patient was removed from the list and the remaining patients were then searched for the next diagnosis in the hierarchy. In this way, a patient with CF and pancreatic insufficiency would be assigned to the CF, not the diabetes, diagnostic category.
Variables
Demographic variables included age, gender, race, and primary payer. Clinical data included primary and secondary diagnoses; outcome data included mortality and discharge disposition; and utilization data included hospital lengths of stay and charges. Charges were converted to year 2008 US dollars by using the US Department of Labor Bureau of Labor Statistics consumer price index for hospital and related services (www.bls.gov/CPI).
Analytic Sequence
We examined patient demographic characteristics for the 10-year study period. This 10-year period informed projections for the subsequent 3 years. We performed more detailed analyses according to diagnosis for 2007 and 2008, the 2 most recent years from which data were available.
Statistical Analysis
We calculated the annual percent change compared with the year 1999 for the entire cohort and for patients with the 6 most common conditions. Time-trend forecasts were performed by using a stepwise autoregressive method. To determine if the growth rate was different among the age groups, we tested the interaction between year and age group with a general linear model.
We calculated the actual annual percent change in utilization and the standardized mortality rate (SMR) for the 6 common conditions from 2007 to 2008 at the hospital level and presented the median and interquartile range. The expected mortality in the PHIS database is assigned to each discharged patient on the basis of their assigned All-Patient Refined Diagnosis-Related Group (APR-DRG) and risk of mortality level. We used the expected mortality that is calculated by Thomson-Reuters on the basis of their national normative pediatric database as the proportion of mortalities in each APR-DRG and risk of mortality level combination. At the hospital level, we used a sign test to determine if the percent change values for the transitional and adult groups were different from those in the pediatric group.
All statistical analyses were performed by using SAS 9.2 (SAS Institute, Inc, Cary, NC). A P value of <.05 was considered statistically significant.
RESULTS
Characteristics of the Population
We studied 2 143 696 patients discharged 3 343 194 times. Transitional patients represented only 2.0% of patients, and adults 0.8%, with a total of 59 974 patients aged 18 years or older being discharged 119 573 times from the 30 children's hospitals (Table 1). Transitional and adult patients had more discharges per patient (2.0) than pediatric patients (1.6). Hospital mortality was significantly higher among adults (1.8%) than among transitional (1.1%) or pediatric patients (1.0%; P < .001). Seventy-five percent of adults older than 21 years were also aged 23 years or older, 25% were aged 32 years or older, and 10% were aged 41 years or older.
TABLE 1.
Demographic, Clinical, and Utilization Characteristics of Patients Seeking Care at 30 Children's Hospitals From 1999 to 2008, According to Age Group
| Pediatric (<18 y) | Transitional (18–21 y) | Adults (>21 y) | |
|---|---|---|---|
| Unique patients, n (% of all patients) | 2 083 722 (97.2) | 43 157 (2.0) | 16 817 (0.8) |
| Discharges | 3 223 621 (96.4) | 85 616 (2.6) | 33 957 (1.0) |
| Gender, n (% of age group) | |||
| Male | 1 788 663 (55.5) | 43 452 (50.8) | 17 925 (52.8) |
| Female | 1 434 840 (44.5) | 42 164 (49.2) | 16 031 (47.2) |
| Race/ethnicity, n (% of age group) | |||
| Non-Hispanic white | 1 532 643 (50.2) | 46 865 (56.6) | 24 473 (74.1) |
| Non-Hispanic black | 722 543 (23.7) | 22 042 (26.6) | 4605 (13.9) |
| Hispanic | 509 714 (16.7) | 8953 (10.8) | 2164 (6.6) |
| Asian | 58 215 (1.9) | 1280 (1.5) | 372 (1.1) |
| Other | 231 195 (7.6) | 3708 (4.5) | 1414 (4.3) |
| Payor Type, n (% of age group) | |||
| Government | 1 383 855 (43.0) | 35 053 (41.0) | 13 977 (41.2) |
| Private | 1 094 320 (34.0) | 31 154 (36.4) | 12 784 (37.7) |
| Other | 739 933 (23.0) | 19 311 (22.6) | 7158 (21.1) |
| Disposition, n (% of age group) | |||
| Home | 3 114 378 (96.8) | 82 604 (96.9) | 32 192 (95.1) |
| Died | 32 818 (1.0) | 893 (1.1) | 624 (1.8) |
| Transferred to subacute facility | 71 189 (2.2) | 1797 (2.1) | 1039 (3.1) |
| Utilization, n (% of all hospitalizations) | |||
| Inpatient-days | 18 719 220 (95.9) | 546 648 (2.8) | 255 885 (1.3) |
| Charges, 2008 US $ | 126 358 764 252 (95.3) | 4 218 967 988 (3.2) | 2 059 688 721 (1.6) |
Values reflect discharges, not patients, and may not add up to the total discharges due to missing data.
Utilization
Patients aged 18 years and older and accumulated >80 000 hospital days and $627 million in charges on average annually, and resource utilization was disproportionately higher in the older age groups. Compared with pediatric patients, transitional and adult patients consumed an average of 41% and 69% more hospital days per patient, respectively (Table 1). In addition, per patient charges averaged 61% (transitional) and 102% (adult) higher than those for pediatric patients.
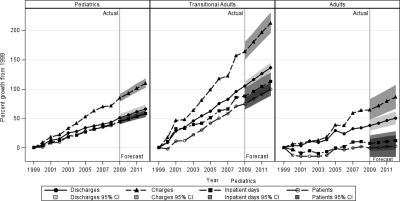
The number of unique patients, discharges, patient-days, and charges increased among all age groups over the study period (Fig 1). The largest increases were among transitional patients, with average annual increases of 6.9% in discharges, 7.6% in patient-days, and 15% in charges, all significantly greater than increases among pediatric patients (all P < .001). In contrast, growth rates were significantly lower for adult patients compared with pediatric patients (inpatient-days: P = .009; charges: P = .03). Overall, there were 4303 more discharges of transitional patients and 280 more discharges of adults in 2008 than in 1999. If this growth continues, we forecast that 12 693 transitional and 3784 adult discharges will occur in these 30 children's hospitals in 2012.
FIGURE 1.
Increase in adults treated at children's hospitals, 1999–2012, according to age group. Shown are the aggregated actual 10-year and forecasted 3-year percentage growth from 1999 in discharges, charges, and patient-days of patients hospitalized at children's hospitals, according to age group. In aggregate, patients in the transitional age group had dramatic increase in discharges, charges, and patient-days. CI indicates confidence interval.
Chronic Conditions
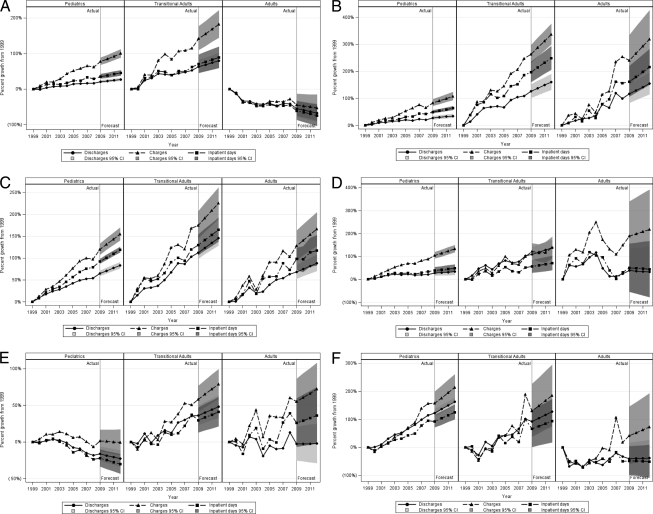
The percentage of patients with an identifiable chronic condition increased with age, from 47.9% of pediatric patients to 80.9% of transitional and 86.5% of adult patients. Figure 2 displays the change in utilization over the 10-year study period, with projections to 2012 for each of the 6 major chronic disease diagnoses, according to age group. We compared the rate of change for each of the older 2 age groups with that of the pediatric age group. For CF (Fig 2A), transitional patients had a greater rate of increase in charges (P = .006) and discharges (P = .003) and a trend toward more inpatient-days (P = .05). In contrast, charges, discharges, and inpatient-days decreased significantly among adults with CF (P < .001). Transitional and adult patients with malignant neoplasms (Fig 2B) had more discharges, charges, and inpatient-days (P < .001). For CHD patients (Fig 2C), transitional patients had a greater increase in charges (P < .001) and discharges (P = .01), but no statistical difference in the rate of increase in inpatient-days. No significant differences were found among patients with CHD in the adult age group. For patients with sickle cell disease (Fig 2D) no comparisons were statistically significant. Pediatric patients with cerebral palsy (Fig 2E) had a significant reduction over time in discharges, patient-days, and charges (P < .001), whereas utilization increased among transitional and adult patients (P < .001; except, P = .05 for charges for adults). For epilepsy patients (Fig 2F), the rate of increases in discharges, patient-days, and charges for adult patients was significantly slower than that of pediatric patients (P < .001), and adults had decreasing inpatient-days over time (P = .002).
FIGURE 2.
Increase in adults treated at children's hospitals, 1999–2012, according to age group and disease. The aggregated actual 10-year and forecasted 3-year percentage growth from 1999 in discharges, charges, and patient-days of patients hospitalized at children's hospitals, according to age group and disease: A, CF; B, malignant neoplasms; C, CHD; D, sickle cell disease; E, cerebral palsy; and F, epilepsy. CI indicates confidence interval.
Table 2 shows the most common chronic conditions in 2007 and 2008. CHD and malignant neoplasms were the 2 most common chronic conditions in all age groups, with CHD being the most common among pediatric and adult patients, and malignant neoplasms the most common among transitional patients. There were no significant differences between 2007 and 2008.
TABLE 2.
Chronic Conditions Among Patients Hospitalized at Children's Hospitals in 2007 and 2008
| Pediatrics (<18 y), n (%) | Transitional (18–21 y), n (%) | Adults (>21 y), n (%) | |
|---|---|---|---|
| CF | 7003 (1.0) | 1426 (6.9) | 1055 (14.4) |
| Malignant neoplasms | 69 773 (10.1) | 4283 (20.6) | 1451 (19.8) |
| Sickle cell disease, median (interquartile range), % | 18 706 (2.7) | 1825 (8.8) | 136 (1.9) |
| CHD | 113 684 (16.4) | 4275 (20.5) | 2121 (28.9) |
| Cerebral palsy, median (interquartile range), % | 15 924 (2.3) | 1300 (6.2) | 647 (8.8) |
| Epilepsy and recurrent seizures, median (interquartile range), % | 10 815 (1.6) | 239 (1.1) | 59 (0.8) |
| Other chronic condition | 95 440 (13.8) | 3491 (16.8) | 888 (12.1) |
| No identified chronic condition | 360 614 (52.1) | 3976 (19.1) | 988 (13.5) |
Values are the sum of 2007 and 2008 discharges.
Table 3 focuses on data from 2007–2008. For each variable, the hospital level experience was examined and the percentage change in utilization and SMR for each hospital for the 6 common conditions was determined. We present the median and interquartile range for these variables, which illustrate the marked heterogeneity according to condition and age group and the extent to which individual hospital experiences vary. Transitional and adult patients are compared with pediatric-aged patients as the reference. The transitional age range had an increase in inpatient-days for those with CF, and for those with malignant neoplasms, discharges, inpatient-days, and total charges increased, whereas SMR decreased. Transitional-aged patients with CHD and epilepsy had an increase in charges, and those with epilepsy also had an increase in inpatient-days. For adult patients, charges increased only for those with malignant neoplasms and cerebral palsy and the only diagnosis with an increase in either discharges or inpatient-days was cerebral palsy. Patients with epilepsy had a significant decrease in discharges. Changes were similar according to age for diagnoses of mental retardation, muscular dystrophy, central nervous system degeneration, and brain and spinal cord malformations (data not shown). The principal diagnosis, or primary reason for admission, was similar between age groups for each of the common conditions (data not shown).
TABLE 3.
Annual Percent Change in Utilization and SMR According to Chronic Condition From 2007 to 2008 in 30 Hospitals
| Pediatric (<18 y) | Transitional (18–21 y) | Adult (>21 y) | |
|---|---|---|---|
| CF, median (interquartile range), % | |||
| Discharges | 0.4 (−10.8 to 14.4) | 0 (−22.5 to 50) | −3.3 (−25.4 to 45) |
| Inpatient-days | −0.6 (−15.3 to 10.6) | 10.1 (−18.3 to 89.8)a | 9.9 (−35.3 to 69.2) |
| Total charges | 7.3 (−9 to 27) | 28 (−18.4 to 95.9) | 67 (−20.3 to 97.1) |
| SMR | 0 (−100 to 0) | 0 (0 to 0) | 0 (0 to 0) |
| Malignant neoplasms, median (interquartile range), % | |||
| Discharges | −1.2 (−4.7 to 4) | 10.2 (−13.3 to 33.3)a | −12.6 (−36.1 to 26.2) |
| Inpatient-days | −2.8 (−10 to 6.8) | 12.7 (−16.3 to 73.3)a | 27.1 (−41.6 to 116.1) |
| Total charges | 4 (−9.6 to 19.2) | 24.5 (−18.1 to 87.7)a | 56.7 (−20 to 161.3)a |
| SMR | 12 (−25.8 to 42.1) | −1.2 (−51.3 to 0)a | 0 (−38.4 to 0) |
| Sickle cell disease, median (interquartile range), % | |||
| Discharges | 0.6 (−7 to 14.6) | 0 (−26.4 to 42.9) | −33.3 (−100 to 0) |
| Inpatient-days | 4.6 (−14.6 to 26.2) | 3.4 (−17.7 to 62.4) | −29 (−46.7 to 68.2) |
| Total charges | 9.7 (−9.2 to 48.9) | 5.8 (−17.8 to 111.1) | 47.2 (−66.7 to 136) |
| SMR | 0 (−6.9 to 0) | 0 (0 to 0) | 0 (0 to 0) |
| CHD, median (interquartile range), % | |||
| Discharges | 2.3 (−3.8 to 5.4) | 11.4 (−10.7 to 24.6) | 5.4 (−16.9 to 34) |
| Inpatient-days | 2.6 (−3.4 to 13.2) | 10.1 (−11.2 to 54.1) | −3.9 (−50 to 37.2) |
| Total charges | 8.9 (−2.4 to 17.9) | 25.9 (−1.4 to 76.8)a | 9.5 (−11.4 to 47.4) |
| SMR | −2.2 (−11 to 3.6) | 0 (0 to 13.8) | 0 (−18.4 to 0) |
| Cerebral palsy, median (interquartile range), % | |||
| Discharges | −2.1 (−12.4 to 7.4) | 0 (−16.7 to 33.3) | 0 (−19.4 to 80) |
| Inpatient-days | −10.4 (−24.5 to 11.9) | −10.9 (−37.1 to 29.9) | 83.9 (−21.6 to 228.8)a |
| Total charges | −2.1 (−14.3 to 13.8) | −7 (−29.6 to 29.7) | 111.1 (−13.1 to 200.7)a |
| SMR | −38.4 (−100 to 0) | 0 (0 to 0) | 0 (0 to 0) |
| Epilepsy and recurrent seizures, median (interquartile range), % | |||
| Discharges | 9.4 (−6.6 to 20.2) | 0 (−50 to 100) | −66.7 (−100 to 40)a |
| Inpatient-days | 7 (−3.8 to 32.2) | 121.9 (0 to 250)a | 15.6 (−80 to 100) |
| Total charges | 16.6 (1.8 to 56.6) | 82.8 (−11.2 to 322.9)a | −2.8 (−72.2 to 134.5) |
| SMR | 0 (−100 to 0) | 0 (0 to 0) | 0 (0 to 0) |
P < .05 compared to the pediatric change, according to results of the sign test.
DISCUSSION
Children's hospitals are caring for increasing numbers of patients outside of the traditional pediatric age range. Although these individuals make up only a small fraction of inpatients, thousands of adults receive care at these 30 children's hospitals annually. Adults are more frequently readmitted than patients in the pediatric age group, and their inpatient-days and charges are disproportionately higher. The increase of patients aged 18 to 21 years exceeds that for pediatric patients, and our projections suggest that both transitional and adult inpatient populations will continue to grow. Although children's hospitals may see a disproportionate number of these patients compared with general hospitals because of their clinical focus, our observations demonstrate that the growth of transitional-aged patients is out of proportion to general increases in pediatric patient numbers.
Determination of the best location for the care of adults with chronic conditions that originate in childhood is a topic that is addressed in a growing body of literature 4,16–18,23,29,37 but remains unclear. A key question is the role of children's hospitals and whether they provide care for children only or for all patients with childhood diseases. Balancing subspecialty care against age-appropriate care is difficult. Care for young adults with CF is an example of a situation in which adult and pediatric providers work together to successfully transfer care provided in children's hospitals to adult care settings.4,23,29 Young adults with CHD, on the other hand, have high health care utilization, which increases with age.38 However, CHD is much more heterogeneous, and encompasses >100 separate conditions that require specialized medical, surgical, and imaging equipment and personnel.12 Recent studies of the prevalence of CHD have shown that the numbers of children and adults with complex CHD is roughly equal.39,40 This emerging population will require lifelong proactive management to reduce secondary disability and might be expected to consume considerable health care resources. Cerebral palsy is among the most challenging of conditions, because it is even more heterogeneous, often with complex comorbidities and developmental disabilities not typically treated in adult-oriented environments.10,34
Children's hospitals rarely have the comprehensive resources and expertise necessary for care of conditions acquired in adulthood. Their physical facilities and supplies are not designed for adults, personnel tend to be less well-trained in adult care, and ancillary services that support adults, such as for job placement, are often lacking. Nonetheless, pediatric hospitals and providers may be uniquely able to provide specialized care for sequelae from conditions originating in childhood. For example, children's hospitals have providers and equipment needed to perform complex invasive procedures to treat CHD,16–18,22,37 and standardized, multiinstitutional protocols used by pediatric oncologists lead to better outcomes among young adults with leukemia compared with patients of the same age treated by providers trained to provide care to adult patients.25
When specific disease categories are compared, a complex landscape emerges. The CF community has an explicit program to facilitate the transition of patients to adult providers.23,29 The increase in patients among the transitional age group likely reflects improved survival, and the decrease of adult patients treated at pediatric hospitals may be attributable to successful transitions to adult providers. In contrast, growth rates are high for adult patients with malignancy, CHD, and cerebral palsy treated at pediatric hospitals, conditions that lack widespread transition programs. Although these patients may continue to require the specialized resources of pediatric centers, they may also be encountering barriers to transition to adult providers.
Barriers to transitioning patients to adult providers include concerns regarding patient maturity, psychosocial and family needs, and systemic issues of transfer coordination and reimbursement.1,5,6,11 The identification of adult providers able to care for these patients is a challenging task that requires unique attributes of training and access,41,42 especially for patients with unique needs, such as those with severe neurodevelopmental compromise. Coordination among multiple providers (eg, pediatric, adult, and primary and specialty care) and the preparation for transfer of care are all essential. The markedly increasing number of inpatient-days and charges for adults with cerebral palsy may serve as an example that illustrates these systemic issues.
Health care reform will undoubtedly have an impact on the transition experience and quality of life of adults who are survivors of pediatric chronic diseases. Currently, these patients are at risk of losing health insurance when their age makes them unqualified for assistance programs for children but they are ineligible for conventional insurance owing to preexisting conditions.43–45 In addition to bringing about the expansion of insurance coverage, reform efforts could improve care for this population by incorporating reimbursement of time-intensive tasks such as counseling and transition planning. Our data suggest that transition planning is an ongoing need, with a substantial percentage of our patients being older than 23 years and one-quarter of them being 32 years old or older.
This study has important limitations, many of which are related to its focus on inpatient care at 30 children's hospitals, which represents only a fraction of the health care that this population receives nationally. Although one could assert that the focus on this group of patients imposes a selection bias, this subset reveals important trends. The disparate observations according to diagnostic group suggest that underlying systemic issues explain our findings that some conditions predispose patients to continue to seek care from pediatricians, whereas others do not. The hospitals that participated in this study care for 7.6% of pediatric inpatients and 20% of inpatients at tertiary general children's hospitals in the United States. Because one-third of health care costs are for inpatient care,46 the $627 million annual inpatient charges for our sample of transitional age and adult patients may actually be indicative of billions of dollars across the health care continuum per year. In addition, we were unable to explore differences between pediatric and adult providers or to compare care rendered at general hospitals versus children's hospitals. Finally, for the situations in which adult use of children's hospitals is decreasing, we cannot determine if the change is attributable to successful transition to adult care, decreased survival, or geographic relocation. In addition, there are inherent limitations to use of administrative data for health services research, including those of diagnostic coding and data entry.
Adults with chronic conditions of childhood require the expertise of both pediatric- and adult-trained providers and are familiar with the pediatric and adult manifestations of the conditions. Patients with complex lesions who require a highly resourced system of care to support surgical and other procedural interventions may benefit from unique services available in a pediatric hospital. For these patients, comanagement by a provider trained in adult medicine may be optimal. Ultimately, each institution, on a condition-by-condition basis, must determine the best way to organize their local health care system and community to care for these patients.
CONCLUSIONS
We believe we have provided important new information. We have described disparate experiences based on diagnosis, most notably the contrast between an entity with a well-established template for transition (CF) and other conditions. Moreover, we established growth rates and projections for future growth according to age group, and found that the most rapid rate of growth was among patients aged 18 to 21 years. We also found that substantial numbers of patients in their 30's and 40's continue to be seen at children's hospitals. These patients may be the population most likely to benefit from a concerted effort to develop transition strategies and identify long-term medical homes. As practitioners define the scope of practice, whether according to age or subspecialty focus, the unique needs of these patients must be incorporated into training programs and clinical pathways. With the data presented here we hope to inform the debate on health care reform and the environment of care for patients who survive diseases that were previously fatal in childhood.
ACKNOWLEDGMENTS
Dr Watson received support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant K23 HD046489). Dr Shah received support from the National Institute of Allergy and Infectious Diseases (grant K01 AI73729) and the Robert Wood Johnson Foundation under its Physician Faculty Scholar Program. Dr Hall had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
APPENDIX: HIERARCHY OF CHRONIC CONDITIONS
CF
Malignant neoplasms
Sickle cell disease
CHD
Infantile cerebral palsy
Brain and spinal cord malformations
Muscular dystrophies and myopathies
Central nervous system degeneration and disease
Epilepsy and recurrent seizures
Mental retardation
Chronic respiratory disease
Congenital anomalies: gastrointestinal
Inflammatory bowel disease
Respiratory malformations
Congenital anomalies: renal
Chronic renal failure
Chronic liver disease and cirrhosis
Storage disorders
Acquired immunodeficiency
Hereditary anemias
Amino acid metabolism
Carbohydrate metabolism
Lipid metabolism
Hereditary immunodeficiency
Diaphragm and abdominal wall
Bone and joint anomalies
Other congenital anomalies
Chromosomal anomalies
Other metabolic disorders
Diabetes
Technology dependant
No chronic condition
Dr Goodman participated in the conception and design of the study, analysis and interpretation of data, and drafting and critical revision of the manuscript; Dr Hall participated in the conception and design of the study, acquisition of data, analysis and interpretation of data, and statistical analysis; Dr Levin participated in the analysis and interpretation of data and critical revision of the manuscript; Dr Watson participated in the analysis and interpretation of data and critical revision of the manuscript; Dr Williams participated in the analysis and interpretation of data and critical revision of the manuscript; Dr Shah participated in the analysis and interpretation of data and critical revision of the manuscript; and Dr Slonim participated in the conception and design of the study, analysis and interpretation of data, and drafting and critical revision of the manuscript.
The views in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
Abbreviations:
- CHD
- congenital heart disease
- CF
- cystic fibrosis
- PHIS
- Pediatric Health Information System
- SMR
- standardized mortality rate
REFERENCES
- 1. Callahan ST, Winitzer RF, Keenan P. Transition from pediatric to adult-oriented health care: a challenge for patients with chronic disease. Curr Opin Pediatr. 2001;13(4):310–316 [DOI] [PubMed] [Google Scholar]
- 2. Scal P, Evans T, Blozis S, Okinow N, Blum R. Trends in transition from pediatric to adult health care services for young adults with chronic conditions. J Adolesc Health. 1999;24(4):259–264 [DOI] [PubMed] [Google Scholar]
- 3. Viner RM. Transition of care from paediatric to adult services: one part of improved health services for adolescents. Arch Dis Child. 2008;93(2):160–163 [DOI] [PubMed] [Google Scholar]
- 4. Zack J, Jacobs CP, Keenan PM, et al. Perspectives of patients with cystic fibrosis on preventive counseling and transition to adult care. Pediatr Pulmonol. 2003;36(5):376–383 [DOI] [PubMed] [Google Scholar]
- 5. Peter NG, Forke CM, Ginsburg KR, Schwarz DF. Transition from pediatric to adult care: internists' perspectives. Pediatrics. 2009;123(2):417–423 [DOI] [PubMed] [Google Scholar]
- 6. Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115(1):112–120 [DOI] [PubMed] [Google Scholar]
- 7. Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck? Arch Dis Child. 1999;81(3):271–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lotstein DS, McPherson M, Strickland B, Newacheck PW. Transition planning for youth with special health care needs: results from the National Survey of Children With Special Health Care Needs. Pediatrics. 2005;115(6):1562–1568 [DOI] [PubMed] [Google Scholar]
- 9. Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics. 2005;115(6):1607–1612 [DOI] [PubMed] [Google Scholar]
- 10. Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51(8):670–678 [DOI] [PubMed] [Google Scholar]
- 11. Bell LE, Bartosh SM, Davis CL, et al. Adolescent Transition to Adult Care in Solid Organ Transplantation: a consensus conference report. Am J Transplant. 2008;8(11):2230–2242 [DOI] [PubMed] [Google Scholar]
- 12. Bhat AH, Sahn DJ. Congenital heart disease never goes away, even when it has been “treated”: the adult with congenital heart disease. Curr Opin Pediatr. 2004;16(5):500–507 [DOI] [PubMed] [Google Scholar]
- 13. Davis M, Sondheimer DL. State child mental health efforts to support youth in transition to adulthood. J Behav Health Serv Res. 2005;32(1):27–42 [DOI] [PubMed] [Google Scholar]
- 14. Garson A, Jr, Allen HD, Gersony WM, et al. The cost of congenital heart disease in children and adults. A model for multicenter assessment of price and practice variation. Arch Pediatr Adolesc Med. 1994;148(10):1039–1045 [DOI] [PubMed] [Google Scholar]
- 15. Gurvitz MZ, Inkelas M, Lee M, Stout K, Escarce J, Chang RK. Changes in hospitalization patterns among patients with congenital heart disease during the transition from adolescence to adulthood. J Am Coll Cardiol. 2007;49(8):875–882 [DOI] [PubMed] [Google Scholar]
- 16. Karamlou T, Diggs BS, Person T, Ungerleider RM, Welke KF. National practice patterns for management of adult congenital heart disease: operation by pediatric heart surgeons decreases in-hospital death. Circulation. 2008;118(23):2345–2352 [DOI] [PubMed] [Google Scholar]
- 17. Kogon BE, Plattner C, Leong T, et al. Adult congenital heart surgery: adult or pediatric facility? Adult or pediatric surgeon? Ann Thorac Surg. 2009;87(3):833–840 [DOI] [PubMed] [Google Scholar]
- 18. Mahle WT, Kirshbom PM, Kanter KR, Kogon BM. Cardiac surgery in adults performed at children's hospitals: trends and outcomes. J Thorac Cardiovasc Surg. 2008;136(2):307–311 [DOI] [PubMed] [Google Scholar]
- 19. Opotowsky AR, Siddiqi OK, Webb GD. Trends in hospitalizations for adults with congenital heart disease in the U.S. J Am Coll Cardiol. 2009;54(5):460–467 [DOI] [PubMed] [Google Scholar]
- 20. Simon TD, Lamb S, Murphy NA, Hom B, Walker ML, Clark EB. Who will care for me next? Transitioning to adulthood with hydrocephalus. Pediatrics. 2009;124(5):1431–1437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sood MR, Rudolph CD. Gastrointestinal motility disorders in adolescent patients: transitioning to adult care. Gastroenterol Clin North Am. 2007;36(3):749–763, xi [DOI] [PubMed] [Google Scholar]
- 22. Webb GD, Williams RG. Care of the adult with congenital heart disease: introduction. J Am Coll Cardiol. 2001;37(5):1166. [DOI] [PubMed] [Google Scholar]
- 23. Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D. Cystic fibrosis adult care: consensus conference report. Chest. 2004;125(1 Suppl):1S–39S [DOI] [PubMed] [Google Scholar]
- 24. Mackie AS, Pilote L, Ionescu-Ittu R, Rahme E, Marelli AJ. Health care resource utilization in adults with congenital heart disease. Am J Cardiol. 2007;99(6):839–843 [DOI] [PubMed] [Google Scholar]
- 25. Howell DL, Ward KC, Austin HD, Young JL, Woods WG. Access to pediatric cancer care by age, race, and diagnosis, and outcomes of cancer treatment in pediatric and adolescent patients in the state of Georgia. J Clin Oncol. 2007;25(29):4610–4615 [DOI] [PubMed] [Google Scholar]
- 26. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008;118(23):e714–e833 [DOI] [PubMed] [Google Scholar]
- 27. Webb GD. Care of adults with congenital heart disease: a challenge for the new millennium. Thorac Cardiovasc Surg. 2001;49(1):30–34 [DOI] [PubMed] [Google Scholar]
- 28. Williams RG, Pearson GD, Barst RJ, et al. Report of the National Heart, Lung, and Blood Institute Working Group on research in adult congenital heart disease. J Am Coll Cardiol. 2006;47(4):701–707 [DOI] [PubMed] [Google Scholar]
- 29. Tuchman LK, Schwartz LA, Sawicki GS, Britto MT. Cystic fibrosis and transition to adult medical care. Pediatrics. 2010;125(3):566–573 [DOI] [PubMed] [Google Scholar]
- 30. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the management of adults with congenital heart disease, executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008;118(23):2395–2451 [DOI] [PubMed] [Google Scholar]
- 31. Okumura MJ, Campbell AD, Nasr SZ, Davis MM. Inpatient health care use among adult survivors of chronic childhood illnesses in the United States. Arch Pediatr Adolesc Med. 2006;160(10):1054–1060 [DOI] [PubMed] [Google Scholar]
- 32. Tan J, Cox R, Shannon P, Payne D. Adolescent and young adult health in a children's hospital: everybody's business. J Paediatr Child Health. 2009;45(12):715–719 [DOI] [PubMed] [Google Scholar]
- 33. Goodman DM, Mendez E, Throop C, Ogata ES. Adult survivors of pediatric illness: the impact on pediatric hospitals. Pediatrics. 2002;110(3):583–589 [DOI] [PubMed] [Google Scholar]
- 34. American Academy of Pediatrics, Committee on Children With Disabilities The role of the pediatrician in transitioning children and adolescents with developmental disabilities and chronic illnesses from school to work or college. American Academy of Pediatrics. Committee on Children With Disabilities. Pediatrics. 2000;106(4):854–856 [DOI] [PubMed] [Google Scholar]
- 35. Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299(17):2048–2055 [DOI] [PubMed] [Google Scholar]
- 36. Shah SS, Hall M, Srivastava R, Subramony A, Levin JE. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49(9):1369–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mavroudis C. Invited commentary. Ann Thorac Surg. 2009;87(3):840. [DOI] [PubMed] [Google Scholar]
- 38. Verheugt CL, Uiterwaal CS, van der Velde ET, et al. The emerging burden of hospital admissions of adults with congenital heart disease. Heart. 2010;96(11):872–878 [DOI] [PubMed] [Google Scholar]
- 39. Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115(2):163–172 [DOI] [PubMed] [Google Scholar]
- 40. Hoffman JI, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J. 2004;147(3):425–439 [DOI] [PubMed] [Google Scholar]
- 41. Child JS, Collins-Nakai RL, Alpert JS, et al. Task force 3: workforce description and educational requirements for the care of adults with congenital heart disease. J Am Coll Cardiol. 2001;37(5):1183–1187 [DOI] [PubMed] [Google Scholar]
- 42. Skorton DJ, Garson A, Jr, Allen HD, et al. Task force 5: adults with congenital heart disease: access to care. J Am Coll Cardiol. 2001;37(5):1193–1198 [DOI] [PubMed] [Google Scholar]
- 43. Callahan ST, Cooper WO. Access to health care for young adults with disabling chronic conditions. Arch Pediatr Adolesc Med. 2006;160(2):178–182 [DOI] [PubMed] [Google Scholar]
- 44. Collins SR, Schoen C, Kriss JL, Doty MM, Mahato B. Rite of passage? Why young adults become uninsured and how new policies can help. Issue Brief (Commonw Fund). 2007;26:1–16 [PubMed] [Google Scholar]
- 45. Fox HB, Limb SJ, McManus MA. The Public Health Insurance Cliff for Older Adolescents. Washington, DC: National Alliance to Advance Adolescent Health; 2007. Available at: www.thenationalalliance.org/jan07/factsheet4.pdf Accessed April 13, 2011 [Google Scholar]
- 46. Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group The Nation's Health Dollar, Calendar Year 2007: Where It Went. Available at: www.lawrence.edu/fast/finklerm/PieChartSourcesExpenditures2007 Accessed April 13, 2011