Abstract
Suicidal behavior is a major problem worldwide and at the same time has received relatively little empirical attention. This relative lack of empirical attention may be due in part to a relative absence of theory development regarding suicidal behavior. The current paper presents the Interpersonal Theory of Suicidal Behavior. We propose that the most dangerous form of suicidal desire is caused by the simultaneous presence of two interpersonal constructs—thwarted belongingness and perceived burdensomeness (and hopelessness about these states)—and further, that the capability to engage in suicidal behavior is separate from the desire to engage in suicidal behavior. According to the theory, the capability for suicidal behavior emerges, via habituation and opponent processes, in response to repeated exposure to physically painful and/or fear-inducing experiences. In the current paper, the theory’s hypotheses are more precisely delineated than in previous presentations (Joiner, 2005), with the aim of inviting scientific inquiry and potential falsification of the theory’s hypotheses.
Approximately one million individuals worldwide died by suicide in 2000, and estimates suggest that 10 to 20 times more individuals attempted suicide (World Health Organization, 2008). Only two interventions have been shown to prevent deaths by suicide (Fleischmann, Bertolote, Wasserman, De Leo, Bolhari, Botega, et al., 2008; Motto & Bostrom, 2001) and only one form of psychotherapy has been shown to prevent suicide attempts in more than one clinical trial (Linehan, Comtois, Murray, Brown, Gallop, Heard, et al., 2006). Why is the state of knowledge for such a devastating psychological phenomenon relatively lacking?
One answer may be that suicidal behavior is difficult to study (for a discussion of this issue, see Prinstein, 2008). First, very large samples are needed because the base rates of suicide attempts and deaths are low in the general population (Moscicki, 2001). Second, individuals with suicidal behaviors are often excluded from clinical trials due to safety concerns on the part of researchers (Rudd, Joiner, & Rajab, 2001). Finally, individuals who die by suicide are not available for psychological assessments, thus limiting methods researchers can employ.
Another explanation may lie with the status of theory in the suicide literature. Prinstein (2008) notes, “few theoretical models have been offered to help understand self-injury in the manner that other manifestations of psychopathology have been examined. In particular, few studies have considered integrative models that address interplay between dynamic systems within the individual and between individuals and their environments” (p. 2). Thus, another explanation for the relatively low number of empirical advances in understanding the causes and correlates of suicide, as well as methods for suicide prevention, may therefore be the absence of a theory that can comprehensively explain known facts about suicide, as well as reliably and precisely identify risk for future occurrences of suicidal behavior.
Here, we propose the Interpersonal Theory of Suicide to explain heretofore unexplained facts about suicide and to increase our understanding of the etiology of suicide. Briefly, according to the theory, the most dangerous form of suicidal desire is caused by the simultaneous presence of two interpersonal constructs—thwarted belongingness and perceived burdensomeness—and further, that the capability to engage in suicidal behavior is separate from the desire to engage in suicidal behavior. The model is depicted graphically in Figure 1, with the relatively small area of overlap in the Venn diagram representing the small minority of individuals who possess both desire and capability for suicide. In the current paper, the theory’s hypotheses are more precisely delineated than in previous presentations (Joiner, 2005), with the aim of inviting scientific inquiry and potential falsification of the theory’s hypotheses. We first ground our theory in the context of previous empirical research and theorizing on suicidal behavior. In reviewing and integrating the literature, we reflect on the status of theory regarding suicidal behavior and indicate areas of relative weakness. Next, we describe our Interpersonal Theory of Suicide and indicate how we address (or fail to address) areas of need delineated above. Finally, we close with future directions for theory-based research on suicidal behavior.
Figure 1.
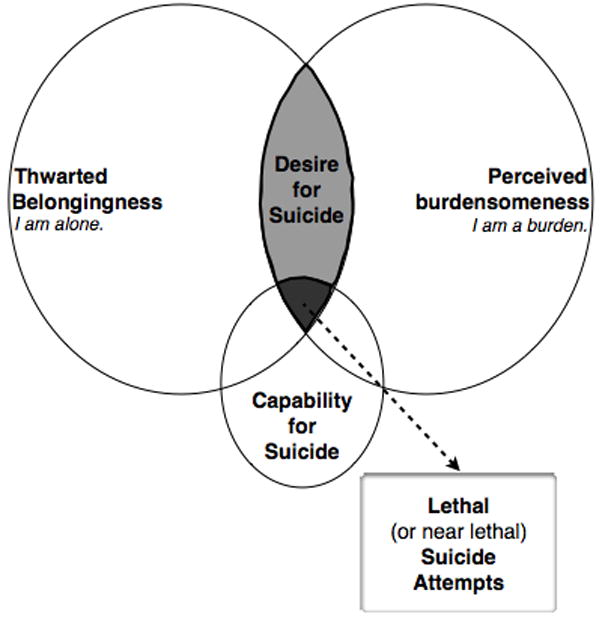
Assumptions of the Interpersonal Theory of Suicide.
Defining Suicidal Behavior
An on-going task for the field involves refining definitions of key suicide-related constructs to increase precision of measurement and standardize usage of terms across studies (Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007a). Our discussion below draws upon—and is consistent with—a recently revised nomenclature (Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007b), which posits that “suicide-related behaviors” (previously referred to as “suicidality”) can be classified as ideations (i.e., thoughts), communications, and behaviors. The authors of the nomenclature further posit that all suicide-related behaviors are self-initiated. Further, these behaviors can vary in terms of the presence or absence of intent to die and presence or absence of physical injury sustained. In the absence of intent to die, the term self-harm is used (e.g., self-cutting in the service of emotion regulation). As the current theory is concerned with ideations, communications, and behaviors that involve some degree of intent to die, we use the term “suicidal behavior” rather than “suicide-related behaviors.” Our primary focus in the current theoretical account is on near-lethal and lethal suicide attempts. The nomenclature states that suicide attempts possess the following qualities: 1) self-initiated, potentially injurious behavior; 2) presence of intent to die; 3) non-fatal outcome. The term suicide is reserved for those cases in which a suicide attempt results in death. As this distinction is potentially confusing, whenever possible we refer to non-lethal suicide attempts (i.e., suicide attempts with non-fatal outcomes) versus lethal suicide attempts (i.e., suicide attempts with fatal outcomes), with the latter term synonymous with deaths by suicide. The theory defines “serious suicidal behavior” as lethal and near-lethal attempts. Near-lethal attempts are a type of non-lethal suicide attempts (i.e., death does not result) for which the person presumably survived by chance (e.g., individuals do, on occasion, survive jumps from the Golden Gate bridge).
One could argue that a phenomenon is not yet ready to be studied empirically until all definitional issues have been addressed. We take a different stance and believe that theory-driven, empirical research can—and should—be used to inform and define the nomenclature and taxonomy of suicide-related behaviors. The definitional issues reviewed above regarding distinctions between ideations, attempts, and deaths highlight the multidimensional nature of suicide and suicide-related behaviors (Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007a).
The value of theory-driven investigations of the taxonomy of suicidal behavior becomes clear upon consideration of the prevalence of suicidal behavior. Arguably the most difficult aspect of the prediction of suicidal behavior is the finding replicated worldwide and over time that only a small subset of those who think about suicide go on to attempt, and even fewer will die by suicide (World Health Organization, 1998). Both suicidal ideation and non-lethal attempts are vastly more common than lethal attempts. As will be described in more detail below, current theories of suicidal behavior are inconsistent with this striking aspect of the phenomenon of suicidal behavior and instead address the phenomenology of suicidal behavior broadly as a unitary construct. Without clearly differentiating between thoughts about suicide, non-fatal suicidal behaviors, and fatal suicidal behaviors, current theories are inconsistent with the taxonomy of suicidal behavior. This results in a number of theories being overly sensitive in the prediction of suicidal behavior at a severe cost in specificity (see Theories section below).
In defining a phenomenon, the boundaries of the construct must also be considered – what is, and what is not, suicidal behavior? Our theory is primarily concerned with what might be termed the “prototype” of suicide-related behaviors—near-lethal and lethal suicide attempts. At the same time, our theory assumes that a core set of processes and conditions underlie near-lethal and lethal suicide attempts and that these processes are operative, to varying degrees, in other suicide-related behaviors on the periphery of the construct. The extent to which our assumption of core processes in suicidal behavior is supported may help delineate the boundaries of suicidal behavior, thus indicating a role for theory in clarifying definitions and taxonomies.
Empirical and Theoretical Foundations
Risk factors are variables that are associated with an increased probability that an outcome will occur, whereas causal processes explain an outcome. However, when a risk factor is shown to temporally precede the outcome and is shown to be non-spurious, a causal relation may be present (Wagner, 1997). In addition, risk factors can be conceptualized as indicators of underlying causal processes that lead to outcomes (Cicchetti & Cohen, 1995); in this way, examining risk factors can be viewed as a stepping-stone to the construction of etiological models. Finally, a useful theory of suicide must be consistent with—and able to account for—empirically-documented risk factors for suicide.
In the section that follows, we examine the literature on risk factors for suicidal behavior, followed by a discussion of theoretical perspectives. As practicalities limit the inclusion of all variables associated with suicidal behavior, we limit our discussion to those risk factors shown to be associated with increased risk for lethal suicidal behavior, as this is the primary outcome of the theory. Table 1 lists these risk factors, grouped by the degree of support that has been found for the association between each factor and lethal suicidal behavior (i.e., number of studies documenting such an association). The literature indicates the most consistent and robust support for the following as risk factors for suicide: mental disorder, past suicide attempts, social isolation, family conflict, unemployment, and physical illness. However, the literature also indicates the presence of other risk factors for suicide, which are also listed in Table 1. Some of these risk factors with less empirical support may in fact be robust predictors of suicide, but have not yet been studied as frequently as other risk factors (e.g., there is consensus in the field that hopelessness is an important predictor of suicide), thus we discuss these risk factors as well, but in relatively less depth.
Table 1.
Empirically Demonstrated Risk Factors for Suicide
Family Conflict
Indices of family conflict are robust risk factors for lethal suicidal behavior across the lifespan, with studies listed in Table 1 documenting associations between suicide and familial discord, domestic violence, familial stress, and perceptions that one is a burden on family.
Mental disorders
The vast majority of people who die by suicide (i.e., approximately 95%) suffer from mental disorders (Cavanagh, Carson, Sharpe, & Lawrie, 2003) – and it is quite possible that the remaining 5% suffer from subclinical variants of mental disorders or presentations of disorders not detected by methodologies such as psychological autopsies (Ernst, Lalovic, Lesage, Seguin, Tousignant, & Turecki, 2004). In addition, certain mental disorders confer higher risk for suicidal behavior than others. The studies listed in Table 1 indicate that the following disorders are associated with particularly elevated rates of suicide: major depressive disorder, with suicide rates between 2–6% (Bostwick & Pankratz, 2000); bipolar disorder, with estimates suggesting a 15-fold increased risk for suicide (Harris & Barraclough, 1997); borderline personality disorder, with suicide rates between 4–5% (Duberstein & Witte, 2008); anorexia nervosa (AN), with a suicide rate 58 times that which was expected (Herzog et al., 2000); schizophrenia, with suicide rates between 1.8%-5.6% (Palmer, Pankratz, & Bostwick, 2005); substance abuse, with a suicide rate 5.7 times that of the general population (Harris & Barraclough, 1997); and conduct disorder in youth, with a six-fold increase in risk for suicide compared to community controls.
However, the studies listed in Table 1 also indicate that the vast majority of individuals diagnosed with the above disorders do not die by suicide. For example, among depressed individuals, approximately one-quarter make a non-fatal suicide attempt during their lifetime (Verona, Sachs-Ericsson, & Joiner, 2004), and at least 25% report having experienced suicidal ideation in the past two weeks (Goldney, Dal Grande, Fisher, & Wilson, 2003). Further, although depression greatly increases risk for suicidal ideation, it does not increase risk for suicide attempts above and beyond its association with ideation (Nock, Hwang, Sampson, Kessler, Angermeyer, Beautrais, et al., 2009). Disorders with anxiety/agitation as characteristic symptoms (i.e., generalized anxiety disorder, social phobia, PTSD, bipolar disorder) or impulse-control deficits as characteristic symptoms (i.e., conduct disorder, intermittent explosive disorder, substance use disorders) are predictive of the transition from suicidal ideation to non-lethal suicide attempts (Nock, et al., 2009). These data indicate that depression is likely associated with the development of desire for suicide, while other disorders, marked by agitation or impulse control deficits, are associated with increased likelihood of acting on suicidal thoughts.
Previous suicide attempt(s)
The studies listed in Table 1 indicate that one of the most reliable and potent predictors of future suicidal ideation, attempts, and death by suicide across the lifespan is having a prior history of this type of behavior. The presence of multiple past attempts is an especially strong predictor of lethal suicidal behavior in both adolescents (Kotila & Lonnqvist, 1987) and adults (Christiansen & Jensen, 2007; Haw, Bergen, Casey, & Hawton, 2007; Suominen, Isometsa, Haukka, & Lonnqvist, 2004; Zonda, 2006), as is a previous attempt with high medical lethality (Gibb, Beautrais, & Fergusson, 2005). A 37-year longitudinal study indicated that the elevation in risk for lethal suicidal behavior conferred by a history of a previous attempt persists over the lifetime (Suominen, Isometsa, Suokas, Haukka, Achte, & Lonnqvist, 2004).
Physical Illness
A review by Whitlock (1986) demonstrated that more than one-third of people who die by suicide had a medical illness at the time of their death and numerous studies (listed in Table 1) have documented a relation between the presence of physical illness and suicide. However, the majority of medical illnesses do not appear to actually increase risk for suicide, including rheumatoid arthritis, diabetes, and hypertension (Harris & Barraclough, 1997; Stenager & Stenager, 1992). One disease with a particularly high risk for suicide is HIV/AIDS, which has been shown to confer approximately a seven-fold risk for suicide as compared to the general population (Conwell, 1994; Harris & Barraclough, 1997). Another illness that appears to confer suicide risk is brain cancer, which has a nine-fold increased risk for suicide as compared to the general population and a four-fold risk as compared to individuals with other forms of cancer (Harris & Barraclough, 1997). Finally, amyotrophic lateral sclerosis has an estimated sixfold increased risk (Fang, Valdimarsdóttir, Fürst, Hultman, Fall, Sparén, et al., 2008) and multiple sclerosis a two-fold risk (Harris & Barraclough, 1997).
The relationship between physical illness and suicide is likely indirect and accounted for by a multitude of other risk factors, including comorbid mental disorders (O’Mahony, Goulet, Kornblith, Abbatiello, Clarke, Kless-Siegel, et al., 2005; Rasic, Belik, Bolton, Chochinov, & Sareen, 2008), functional limitations (Goodwin, Marusic, & Hoven, 2003; Kaplan, McFarland, Huguet, & Newsom, 2007), and social isolation (Carrico, Johnson, Morin, Remien, Charlebois, Steward, et al., 2007; Flavin, Franklin, & Frances, 1986; Rasic, Belik, Bolton, Chochinov, & Sareen, 2008). As one example, among patients with end-stage cancer, the will to live was found to be negatively associated with patients’ apperceptions of burdensomeness on others and was positively associated with perceived social support (Chochinov, Hack, Hassard, Kristjanson, McClement, & Harlos, 2005).
Social isolation
Social isolation is arguably the strongest and most reliable predictor of suicidal ideation, attempts, and lethal suicidal behavior among samples varying in age, nationality, and clinical severity (Conwell, 1997; Dervic, Brent, & Oquendo, 2008; Joiner & Van Orden, 2008; Trout, 1980). Numerous empirical studies (listed in Table 1) have demonstrated associations between lethal suicidal behavior and various facets of social isolation, including loneliness, social withdrawal, living alone and having few social supports, living in non-intact families, losing a spouse through death or divorce, and residing in a single prison cell. In contrast, marriage, children, and greater number of friends/family are associated with decreased risk for lethal suicidal behavior.
Unemployment
Numerous studies (listed in Table 1) have demonstrated that unemployment is a common factor among individuals who have died by suicide and is associated with elevated risk for lethal suicidal behavior. However, several studies examining associations between unemployment and suicide rates at the population level have failed to find an association, while studies examining smaller, more homogeneous populations (that also tend to be higher risk samples) tend to find an association (Lester & Yang, 2003; Stack, 2000). This pattern of findings indicates that many individuals who die by suicide are unemployed, but that the vast majority of unemployed individuals do not die by suicide. Thus, it may be that unemployment is associated with elevated risk only among vulnerable individuals, or only when it results in certain negative outcomes. Similarly, economic recessions are associated with increased suicide rates, but only those recessions with marked elevations in negative outcomes such as job losses and home foreclosures (American Association of Suicidology, 2009).
Other risk factors
Several warning signs for suicide (i.e., signs of acute risk) have empirically-demonstrated associations with lethal suicidal behavior—agitation, hopelessness, and sleep disturbances including nightmares (see Table 1 for references). Consistent and robust support has been found for hopelessness and sleep disturbances. Less research has been conducted on agitation, but available data indicate that agitation is a pernicious sign of elevated risk. Several severely stressful life events are associated with elevated risk for lethal suicidal attempts: studies listed in Table 1 indicate that individuals who have experienced childhood abuse, military combat, homelessness, and incarceration are at elevated risk for lethal suicidal behavior. The studies listed in Table 1 also include several psychiatric and medical history variables that are associated with elevated risk for lethal suicidal behavior. Finally, the literature also indicates the presence of environmental factors that are associated with elevated risk for suicide, including easy access to lethal means, clustering/exposure to suicidal behavior, and seasonal variation in rates of suicidal behavior, as well as increases in connectedness through “pulling together” effects that are protective against suicide.
Theoretical Perspectives
Although much research on suicidal behavior has been conducted in an atheoretical context, theories of suicide spanning diverse perspectives—including biological, psychodynamic, cognitive-behavioral, and developmental/systems etiologies—have been proposed. Biological theories propose that suicidal behavior results from the dual presence of a biologically-based diathesis (such as dysregulation of the serotonergic system in the ventromedial prefrontal cortex) and an activating psychosocial stressor (Mann, 2003; Plutchik, Van Praag, & Conte, 1989; van Pragg, 2001). Psychodynamic theories propose that suicide is caused by unconscious drives (Menninger, 1938), intense affective states (Hendin, 1991), desire for escape from psychological pain (Baumeister, 1990; Shneidman, 1998), existential drives for meaning (Rogers, 2001), and disturbed attachment (Bowlby, 1973). Cognitive-behavioral theories posit causal roles for hopelessness (Beck, Brown, Berchick, Stewart, & et al., 1990; Beck, Steer, Kovacs, & Garrison, 1985), the suicidal cognitive mode (Beck, 1996; Rudd, Joiner, & Rajab, 2001), autobiographical memory deficits and perceptions of entrapment (Williams, 2001; Williams, Van der Does, Barnhofer, Crane, & Segal, 2008), and emotion dysregulation (Linehan, 1993). Developmental/systems theories posit causal roles for disturbed social forces (Durkheim, 1897) and family systems (Richman, 1986; Sabbath, 1969).
Each of these theories is able to explain part of the landscape of suicidal behavior. For example, theories on hopelessness are readily able to account for the relationship between hopelessness and later death by suicide, biological theories are able to explain the association between serotonergic functioning and suicide, and family systems theories are able to explain the association between family conflict and suicide. However, individuals who die by suicide present with numerous risk factors, rather than a single risk factor in isolation (Maris, Berman, & Maltsberger, 1992). Thus, theories of suicide should be able to account for the diverse array of factors associated with lethal suicidal behavior. Our review of risk factors indicates the most robust support for associations with suicide and mental disorders, previous suicide attempts, social isolation, family conflict, unemployment, and physical illnesses. Thus, a theory of suicide should illuminate how these diverse factors are related to suicidal behavior.
Theories must also be able to account for the imprecision of the risk factors listed above—each risk factor in isolation is limited as a predictor of suicide and each risk factor has complex relations with suicidal behavior. To take a couple of prominent examples, a history of past attempts (see references in Table 1) especially multiple past attempts (Christiansen & Jensen, 2007; Haw, Bergen, Casey, & Hawton, 2007; Kotila & Lonnqvist, 1987; Suominen, Isometsa, Haukka, & Lonnqvist, 2004; Zonda, 2006), is a robust predictor of death by suicide, yet many individuals who die by suicide do so on their first attempt (ie., up to half; Rudd, Joiner, & Rajab, 1996). The vast majority of those who die by suicide suffer from mental disorders (Cavanagh, Carson, Sharpe, & Lawrie, 2003); however, the vast majority of those with mental disorders, including disorders with the highest suicide rates, will not attempt or die by suicide, though many will think about suicide (Bostwick & Pankratz, 2000; Hawton, Sutton, Haw, Sinclair, & Harriss, 2005; Herzog, Greenwood, Dorer, Flores, Ekeblad, Richards, et al., 2000; Palmer, Pankratz, & Bostwick, 2005).
A comprehensive theory of suicidal behavior must also be able to account for other demographic differences in suicide rates, including that suicide rates vary by gender, age, and culture. One of the most consistent findings with regards to the epidemiology of suicidal behavior is its gender distribution. With the exception of China, male suicides outnumber female suicides in every nation, worldwide (World Health Organization, 2003). In the United States, the ratio of male to female deaths by suicide is four to one, whereas for non-lethal attempts, females outnumber males at a three to one ratio (American Association of Suicidology, 2006). Non-lethal suicide attempts greatly outnumber lethal attempts (at a ratio of 25 to 1), which means that every day, far more females than males are engaging in (ultimately non-lethal) suicidal behavior. These data indicate that although females die by suicide at much lower rates than do men, it is more common for females to desire, and thus, attempt suicide. Suicide rates also vary by age, with the highest suicide rate (in the U.S.) among the elderly (Gould, Shaffer, & Greenberg, 2003). However, suicidal behavior does occur in children: in 2003, 250 children between the ages of five and fourteen died by suicide (Hoyert, Heron, Murphy, & Hsiang-Ching, 2006). Suicide rates have also been found to differ by race and ethnicity. In the United States, European Americans die by suicide approximately twice as often as members of other minority groups, with the exception of Native Americans (American Association of Suicidology, 2006). Suicide rates also vary by occupation, with, for instance, female physicians having a particularly elevated rate compared to the general population (Lindeman, Laara, Hakko, & Lonnqvist, 1996).
Finally, the observation about suicidal behavior that is arguably the most difficult to grapple with theoretically is the fact that only a small subset of those who think about suicide go on to attempt, and even fewer will die by suicide (World Health Organization, 2008). Estimates from nationally-representative studies indicate that each year, 3.3 percent of Americans seriously consider suicide (i.e., active suicidal ideation), 1.0 percent develop a plan for suicide, and 0.6 percent attempt suicide (Kessler, Berglund, Borges, Nock, & Wang, 2005). Yet, each year, only .01 percent of Americans die by suicide (American Association of Suicidology, 2006). It is this observation about suicide that underlies many of the limitations of the risk factors listed above. At a minimum, theories of suicide must be able to account for these data on the epidemiology of suicidal behavior and those factors shown to be associated with elevated risk for suicide. Optimally, theories could build upon this empirical foundation by delineating putative etiological connections among risk factors and the outcome of interest, suicidal behavior.
Several comprehensive models of suicide have been presented that can account for several risk factors simultaneously, as well as the prevalence of suicidal behavior. These models are structured to describe (i.e., model) suicidal behavior, compared to theories that are structured to explain (i.e., predict) suicidal behavior. Blumenthal and Kupher (1986) propose that suicidal behavior results from the joint presence of risk across five domains: biology; psychosocial life events and chronic medical illness; personality traits; family history and genetics; and psychiatric disorder. This model can be graphically depicted as a Venn diagram with five overlapping circles and greatest risk for suicide represented by the area of overlap from all five circles. Maris (1991, 2002) proposes a comprehensive model of suicidal behavior from a developmental (or life-course) perspective that emphasizes the study of multiply-interacting factors within life histories of individuals who die by suicide, which he denotes as suicidal careers. The interaction of factors across several domains of risk (including time) allows these models to account for differential prevalence of suicide ideation, non-lethal attempts, and deaths by suicide, with the assumption that deaths by suicide occur at the intersection of numerous facets of risk, non-lethal attempts with fewer facets of risk, and ideation with even fewer.
However, while the models described above are comprehensive and thereby able to account for the prevalence of suicidal behavior, they are not structured with a degree of precision that would allow for the falsification of the model and the prediction of suicidal behavior. Thus, what is needed to improve prediction of suicidal behavior is a theory that is both precise—allowing scientific falsifiability and clinical utility—and comprehensive—allowing the theory to account for both suicidal ideation and suicide attempts. Shneidman’s psychache theory (Shneidman, 1998) involves the proposal that the simultaneous presence of three factors is necessary for lethal suicidal behavior to occur—psychache, press, and perturbation—and that the presence of these factors will create the strongest, and most lethal, level of desire for suicide. It is this assumption about suicidal behavior—that individuals who think about versus attempt suicide differ in terms of how much they desire suicide—that is challenged by the Interpersonal Theory of Suicide. It is this level of empirical precision and opposing hypotheses open to falsification that is needed to advance the scientific study of suicidal behavior.
Constructs of the Interpersonal Theory of Suicide
The foundation of the Interpersonal Theory, as discussed above, is the assumption that people die by suicide because they can and because they want to (Figure 1). Within the framework of our theory, three constructs are central to suicidal behavior, two primarily related to suicidal desire—thwarted belongingness and perceived burdensomeness—and one primarily related to capability—acquired capability for suicide. The theory also includes a specification of the relations between these constructs in the form of four hypotheses (listed in Table 2), and thereby includes a specification of a causal pathway for the development of the desire for suicide and the capability to engage in serious suicidal behavior (i.e., lethal or near-lethal attempts). Below we describe both the theory’s constructs and its hypotheses with a level of detail that opens it to possible falsification and invites tests of its hypotheses and comparisons with other theories of suicidal behavior.
Table 2.
Hypotheses of the Interpersonal Theory of Suicide
|
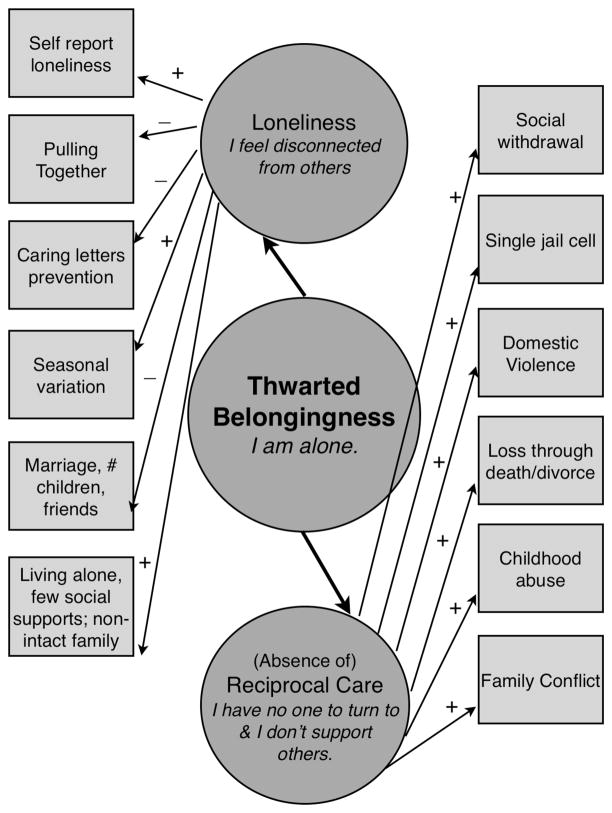
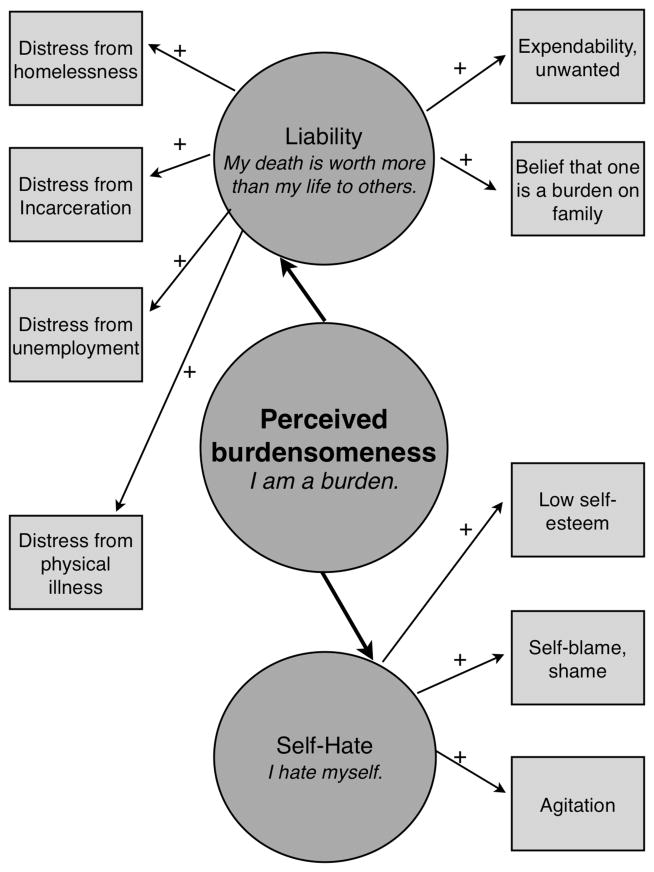
We begin by describing the constructs of thwarted belongingness, perceived burdensomeness, and acquired capability. To do so, we utilize Figures 2–4, each of which graphically depicts components of the constructs, as well as relations with the empirically-demonstrated risk factors discussed in the previous section. The figures utilize many conventions of structural equation modeling for ease of interpretation, including that latent variables are denoted by circular shapes and observable variables by rectangles; in addition, hierarchical latent variables “cause” the lower level latent variables (as well as observable variables) they are connected to, thus arrows point from the latent variable to the observable/lower level latent variable. In contrast, emergent variables (i.e., those caused by variables depicted earlier in the causal chain of the model) are depicted with causal arrows pointing towards them from other variables. To illustrate how individuals experiencing these constructs might describe their experiences, sample items from self-report measures designed to measure the constructs (i.e., the Interpersonal Needs Questionnaire for thwarted belongingness and perceived burdensomeness and the Acquired Capability for Suicide Scale for the acquired capability) are included in italics within the circles representing the constructs. The behavioral (observable) indicators of the constructs in these figures are the empirically-supported risk factors for lethal suicidal behavior (discussed above) that, according to the theory’s definitions of the constructs, represent behavioral indicators of thwarted belongingness, perceived burdensomeness, or acquired capability.
Figure 2.
Dimensions—and indicators—of Thwarted Belongingness.
Figure 4.
Dimensions—and indicators—of Acquired Capability.
Note. Dotted arrows represent habituation and strengthening of opponent processes.
Thwarted Belongingness
As noted above, social isolation is one of the strongest and most reliable predictors of suicidal ideation, attempts, and lethal suicidal behavior across the lifespan. Social isolation can be conceptualized as measuring one facet of the higher order construct of social connectedness (or social integration), which can be measured at multiple levels (Berkman, Glass, Brissette, & Seeman, 2000). Our review also indicated that other facets of social connectedness (e.g., loneliness and loss of a spouse) are also predictive of lethal suicidal behavior. We propose that these social connectedness variables are associated with suicide because they are observable indicators that a fundamental human psychological need is unmet; this need is described by Baumeister and Leary (1995) as the “need to belong” (p. 1). According to the theory, when this need is unmet—a state we refer to as thwarted belongingness—a desire for death develops (also referred to in the suicidology and clinical literature as passive suicidal ideation). Other suicide theorists have also proposed a central role for social connectedness (see below), though the proposed mechanisms for the relations between social connectedness and suicide differ across theoretical accounts.
According to Durkheim (1897), dysregulation of social forces—specifically, degrees of social integration—results in suicide. He proposes that too little social integration leads to an increase in suicide because individuals lack a connection to something that transcends themselves. When examining changes in suicide rates for a population over time, Durkheim’s theory could provide explanations for—and facilitate prediction of—patterns and shifts in suicide rates. However, Durkheim’s theory pays little attention to individual factors: if all individuals in a society are exposed to the shifts in social forces, why then do only particular individuals, and a very small subset of them at that, die by suicide?
In contrast, Shneidman articulated a theory of suicide focused on individual factors, with “psychache”—psychological and emotional pain that reaches intolerable intensity –as the primary factor causing suicide (Shneidman, 1987). Shneidman further posits that psychache is intolerable because it results from basic needs that have been thwarted (Shneidman, 1985). Shneidman (1998) proposes an extensive list of basic needs, seven of which he argues are most commonly thwarted in suicidal individuals, ranging from “affiliation” to “shame avoidance” to “order and understanding.” In contrast to Shneidman’s model, we propose that the need to belong is the need central to the development of suicidal desire, consistent with the wealth of findings linking social connectedness to suicidal behavior.
Thus, the Interpersonal Theory is consistent with past theoretical accounts of suicidal behavior through its proposal for a key role for social connectedness. However, the Interpersonal Theory diverges from previous theories in its proposal that an unmet “need to belong” (Baumeister & Leary, 1995; p. 1) is the specific interpersonal need involved in desire for suicide. The theory also differs in that we propose that thwarted belongingness is a multidimensional construct. Figure 2 depicts in greater detail the proposed definition of the construct of thwarted belongingness (analogous to a latent variable measurement model). The figure depicts a hierarchical latent variable model, with thwarted belongingness as a higher-order latent variable with two subordinate factors. Consistent with this, Baumeister and Leary (1995) propose that the need to belong is comprised of two facets: “people seem to need frequent, affectively pleasant or positive interactions with the same individuals, and they need these interactions to occur in a framework of long-term, stable caring and concern” (p. 520). We conceptualize these two dimensions of interpersonal functioning that are posited to comprise thwarted belongingness as loneliness and the absence of reciprocally-caring relationships. These constructs are depicted in Figure 3 as latent variables caused by (i.e., components of) the latent construct of thwarted belongingness.
Figure 3.
Dimensions—and indicators—of Perceived Burdensomeness.
Drawing upon Russell’s (1996) and Joiner and colleagues’ (Joiner, Lewinsohn, & Seeley, 2002) conceptualization of the construct, loneliness is conceptualized as an affectively-laden cognition that one has too few social connections, which also maps onto Baumeister and Leary’s (1995) first facet of the need to belong (i.e., frequent and positive interactions). For example, an individual experiencing the mental state of thwarted belongingness might express the loneliness component of the construct by stating, “I did not have a satisfying social interaction today” or “I feel disconnected from other people.” The second component of thwarted belongingness according to the Interpersonal Theory is the absence of reciprocally-caring relationships (i.e., ones in which individuals both feel cared about and demonstrate care of another). In order for relationships to meet the need to belong, they must be characterized by positive feelings and occur in a supportive context (Baumeister & Leary, 1995) and when they are not, relationships cease to meet the criteria as reciprocally-caring. An individual with an absence of reciprocally caring relationships might express the experience by stating, “I am not a support for others” or “There are no people I can turn to in times of need” (see Figure 3).
In addition to depicting the multidimensional nature of thwarted belongingness, Figure 3 also further clarifies the definitions of these constructs by including observable indicators of the constructs of loneliness and reciprocally caring relationships – all of which are associated with elevated risk for lethal suicide attempts (and were discussed above in the ‘Risk Factors’ section). The loneliness factor is posited to give rise to six observable risk factors for lethal suicidal behavior (citations for the elevation of risk for lethal attempts are provided in Table 1): self-report loneliness; pulling together effects; caring letters interventions (interventions designed to increase social contacts through long-term follow-ups, thereby decreasing loneliness and thus lowering risk for suicide); seasonal variation (reductions in social interactions that lead to increased feelings of loneliness have been posited as the mechanism whereby the spring peak in lethal suicidal behavior occurs); the presence of marriage and the number of children and friends; and living alone and reporting few to no social supports. The absence of reciprocally-caring relationships factor is posited to give rise to six observable risk factors for lethal suicidal behavior: social withdrawal; low openness to experience; residing in a single jail cell; domestic violence; childhood abuse; and familial discord.
The Interpersonal Theory includes the assumption that thwarted belongingness is a dynamic cognitive-affective state, rather than a stable trait, that is influenced by both interpersonal and intrapersonal factors. These include an individuals’ actual interpersonal environments (e.g., number of individuals in the social network; Hawkley, Hughes, Waite, Masi, Thisted, & Cacioppo, 2008), activated interpersonal schemas (e.g., proneness to interpret others’ behavior as indicative of rejection; Downey & Feldman, 1996), and current emotional states (e.g., depressed mood; Cacioppo, Hawkley, Ernst, Burleson, Berntson, Nouriani, et al., 2006). Thus, the theory presumes that an individual’s degree of belongingness is likely to vary over time.
The theory also includes the assumption that the need to belong is a dimensional, rather than categorical phenomenon. This is in line with Baumeister and Leary (1995) who propose that “partial deprivation” (p. 511) occurs when the need to belong is partially, but not fully met. At what point, and under what conditions, does a thwarted need to belong lead to suicidal thoughts? Research from our laboratory group demonstrated a significant linear relationship between self-reported thwarted belongingness and suicidal ideation among participants who also endorsed high levels of perceived burdensomeness (Van Orden, Witte, Gordon, Bender, & Joiner, 2008). This study indicated that even among participants with high levels of thwarted belongingness (i.e., those at the 90th percentile in the sample), elevations in suicidal ideation were not evident unless high perceptions of burdensomeness were also present. These data suggest that one condition under which thwarted belongingness may cause suicidal ideation is when it is experienced concurrently with perceptions of burdensomeness. We return to this idea in subsequent sections.
However, numerous studies have documented independent associations between indices of thwarted belongingness and suicide. To what degree must the need to belong be thwarted in order for suicidal ideation to result? Empirical studies have not directly examined this question, but data on the association between thwarted belongingness and other deleterious health outcomes speak to this question. Chronic feelings of loneliness (i.e., one facet of thwarted belongingness) are associated with elevated salivary cortisol levels, suggesting higher levels of a physiologic stress response (Cacioppo, Ernst, Burleson, McClintock, Malarkey, Hawkley, et al., 2000). Chronic feelings of loneliness are also associated with numerous negative emotional and interpersonal states, including elevations in negative emotions (i.e., anxiety and anger), pessimism, fear of negative evaluation, and shyness, as well lower levels of social support, agreeableness, and sociability (Cacioppo, et al., 2006). These data suggest that a significant parameter along which thwarted belongingness may vary with regards to psychological/health outcomes is chronicity, as chronic loneliness was the key variable in the two preceding studies. Thus, we propose that when thwarted belongingness is prolonged, suicidal ideation is more likely to result.
Thwarted belongingness can also vary in terms of its magnitude. A robust association has been documented between social isolation—a relatively severe manifestation of thwarted belongingness as it involves few to no social relationships—and suicide (as reviewed above). Thwarted belongingness has also been experimentally induced in the laboratory by randomly assigning participants to receive feedback that they are likely to end up alone later in their lives. This experimental manipulation has been shown to cause numerous deleterious effects on cognition and behavior, including self-regulatory impairments (Baumeister, DeWall, Ciarocco, & Twenge, 2005), executive functioning impairments (Baumeister, Twenge, & Nuss, 2002; Campbell, Krusemark, Dyckman, Brunell, McDowell, Twenge, et al., 2006), reduced prosocial behaviors (Twenge, Baumeister, DeWall, Ciarocco, & Bartels, 2007), aggressive behaviors (Twenge, Baumeister, Tice, & Stucke, 2001), a hostile social-cognitive processing biases (DeWall, Twenge, Gitter, & Baumeister, 2009), unintentional self-defeating behaviors, including risky behaviors (Twenge, Catanese, & Baumeister, 2002), and a state of “inner numbness” (Twenge, Catanese, & Baumeister, 2003). However, the same experimental manipulation of thwarted belongingness has also been shown to cause increased attention to stimuli relevant to belongingness (Dewall, Maner, & Rouby, 2009) as well as increased motivation to connect with others (Maner, DeWall, Baumeister, & Schaller, 2007). This raises the question: What conditions tend to elicit positive versus negative behavioral outcomes? To answer this question, the latter study (Maner, DeWall, Baumeister, & Schaller, 2007) also investigated “boundary conditions” (p. 52) for the increases in affiliative behaviors. The authors found that those with thwarted needs to belong did not tend to engage in affilitative behaviors under two conditions: 1) if the person with whom affiliation could be increased was the person who caused the lowered belongingness (i.e., someone who rejected the participant) or 2) if the persons with whom affiliation could be increased would not be available for in-person interactions. It follows then, that individuals who perceive others in their social networks as individuals who rejected them or as unavailable for in-person interactions would be less likely to engage in affiliative behaviors, but just as likely (or more likely) to engage in the self-defeating behaviors that accompany thwarted belongingness. The data from the cited studies suggest that this more extreme form of thwarted belongingness may result in a more extreme form of self-defeating behavior, of which suicidal behaviors are an example. The theory is concerned with this most severe form of thwarted belongingness that involves perceptions that meaningful and mutually supportive connections are completely absent, with chronicity likely increasing these perceptions.
Perceived Burdensomeness
Family conflict, unemployment, and physical illness were three of the risk factors for suicide (discussed above) with the most robust support for their association with suicide. These three factors are all types of negative life events; why might these three types of negative life events be particularly associated with suicide? Recall that one form of family conflict that has been shown to be associated with lethal suicidal behavior is perceptions that one is a burden on family members. We propose that the elevated likelihood of developing perceptions of burdensomeness on others is the common thread between family conflict, unemployment, and physical illness that can account for the associations with suicide.
Perceptions of burdensomeness on family are also the key factor in Sabbath’s (1969) family systems theory of adolescent suicidal behavior. The theory emphasizes adolescents’ perceptions that they are expendable members of the family. The causal factors leading to adolescent suicidal behavior, according to the theory, are pathogenic parental attitudes toward the adolescent that are interpreted by the adolescent that he/she is not needed in the family, and in fact, that the family would be better off if the adolescent were dead. In a direct test of Sabbath’s theory, perceptions of expendability in the family were found to be positively correlated with suicidal behavior in adolescents (Woznica & Shapiro, 1990). Converging results were found in a sample of preschoolers: suicidal children were significantly more likely to be the product of “unwanted” pregnancies (Rosenthal & Rosenthal, 1984). However, Sabbath’s theory does not account for the fact that the majority of youth who perceive that their families would be better of without them do not die by suicide.
The Interpersonal Theory is consistent with past conceptual work (e.g., Sabbath (1969) as we posit a key role for perceptions of burdensomeness in the etiology of suicide. However, the Interpersonal Theory differs in that the construct is broader and involves perceptions of burdensomeness on close others, including, but not limited to family members, are associated with desire for suicide. Further, according to the theory, perceived burdensomeness comprises two dimensions of interpersonal functioning – beliefs that the self is so flawed as to be a liability on others, and affectively-laden cognitions of self-hatred. These two dimensions are depicted as subordinate latent variables in Figure 3. An individual experiencing the mental state of perceived burdensomeness might express the liability component of the construct by stating, “I make things worse for the people in my life,” while someone expressing self-hatred might directly state, “I hate myself” or “I am useless” (also depicted in Figure 3).
As was done for thwarted belongingness, observable indicators of the dimensions of perceived burdensomeness are depicted in Figure 3. The liability factor is posited to give rise to six observable risk factors for lethal suicidal behavior (citations for the elevation of risk for lethal attempts are provided in Table 1): distress caused by unemployment (the theory is able to account for mixed findings regarding the relation between unemployment and suicide: unemployment should elevate risk for suicide, according to the Interpersonal Theory, only when the stress of unemployment results in perceptions that one is a liability to oneself and others); distress from incarceration (in this way, the theory is consistent with the fact that markedly elevated rates of suicide are found in incarcerated (and recently incarcerated) populations); homelessness; serious physical illnesses; and direct statements in suicide notes or verbal communications that individuals perceive that they are expendable, unwanted, or burdens on others. It should be noted that we posit that in the vast majority of cases (if not all), these perceptions of liability are misperceptions amenable to therapeutic modification. The other dimension of perceived burdensomeness is the affectively-laden construct of self-hate, with three corresponding observable indicators with empirically-demonstrated associations with lethal suicidal behavior: low self-esteem; self-blame and shame; and the mental state of agitation (in part, because it indicates that an individual may be experiencing a degree of self-hatred and anguish that is so elevated as to manifest physiologically).
As with thwarted belongingness, perceived burdensomeness is presumed to be a dynamic cognitive affect state, as well as a dimensional phenomenon. Thus, individuals’ levels of perceived burdensomeness are likely to vary over time, over relationships, and along a continuum of severity. Thus, it is necessary to define the point at which perceptions of burdensomeness are relevant to suicidal behaviors. What does previous research on the construct suggest with regards to the critical level?
A psychological autopsy study of terminal cancer patients who died by suicide indicated that self-perceptions of being a burden on others was a key characteristic likely contributing to desire for suicide (Filiberti, Ripamonti, Totis, Ventafridda, De Conno, Contiero, et al., 2001). In a comparison of suicide notes of individuals who made lethal versus non-lethal attempts, the presence of perceptions of burdensomeness on others differentiated between those who attempted and survived and those who attempted and died – with perceptions of burdensomeness characterizing the notes of those who died (Joiner, Pettit, Walker, Voelz, Cruz, Rudd, et al., 2002). In addition, in the same study, greater perceptions of burdensomeness in the notes predicted the use of more lethal means among the sample of notes from individuals who died. A prospective study following psychiatric patients at high risk for suicide found that statements about feeling like a burden on others significantly elevated risk for suicide during a 60-day follow-up period after an evaluation (Motto & Bostrom, 1990).
Self-perceptions that one is a burden on others also differentiate between individuals with histories of suicide attempts versus no attempts (Brown, Dahlen, Mills, Rick, & Biblarz, 1999; Van Orden, Lynam, Hollar, & Joiner, 2006) and are also associated with suicidal ideation (Brown, Brown, Johnson, Olsen, Melver, & Sullivan, 2009; de Catanzaro, 1995; Van Orden, Lynam, Hollar, & Joiner, 2006). Similar to perceiving that one is a burden, the desire to “make others better off” was shown to be a more common reason given for suicide attempts versus episodes of self-harm without suicidal intent (Brown, Comtois, & Linehan, 2002) and the belief that someone wishes one dead was shown to differentiate between suicidal and non-suicidal individuals (Rosenbaum & Richman, 1970). Recall also that perceptions of expendability have been shown to characterize suicidal adolescents (Woznica & Shapiro, 1990). Similarly, suicidal preschoolers (compared to preschoolers with behavior problems) have been shown to be more likely to be unwanted by their parents (Rosenthal & Rosenthal, 1984).
These studies indicate that it may be that perceptions of burdensomeness on multiple others, rather than on a single individual, that may be particularly deleterious. It may also be that extreme perceptions of burdensomeness within a single relationship are most strongly related to suicidal ideation. We take the former stance (while acknowledging that this is ultimately an empirical question) and propose that when an individual holds perceptions of burdensomeness for all significant others in his/her life and the person endorses some degree of self-hate regarding those perceptions, a critical threshold is crossed – and it is this severe level of perceptions of burdensomeness that is relevant to the theory.
Relations Between Thwarted Belonging and Perceived Burdensomeness
The theory involves the proposal that other more distal risk factors exert their influence on desire for suicide by increasing levels of thwarted belongingness, perceived burdensomeness, or some combination of the two. Childhood maltreatment and mental disorders are not conceptualized as indicators that an individual is currently experiencing thwarted belongingness or perceived burdensomeness (and are not caused by either construct); thus they are not included in Figures 2 or 3. However, these risk factors are relevant to the development of both constructs. For example, both are life experiences that may increase an individual’s risk for developing social isolation and/or feelings of loneliness. Indeed, social alienation (cf., thwarted belongingness) has been proposed as the mechanism whereby the experience of childhood abuse increases risk for suicidal behavior (Twomey, Kaslow, & Croft, 2000). Insofar as childhood maltreatment and mental disorders predispose individuals to perceive that they are unwanted or expendable, these experiences may also elevate risk for perceptions of burdensomeness. Thus, we posit that these risk factors increase risk for suicide through their relationship with both thwarted belongingness and perceived burdensomeness.
Thwarted belongingness and perceived burdensomeness are presumed to be distinct, but related constructs. This assumption raises important issues with regards to the definitions of the constructs. One could argue, for example, that if an individual’s need to belong is completely thwarted, perceptions of burdensomeness are not possible because human connections are a prerequisite for the development of perceived burdensomeness. We suggest that this is not the case because the presence of perceptions of connections to others does not equate with meeting the need to belong. In other words, the construct of thwarted belongingness is not synonymous with a lack of human connections and conversely, the need to belong is not fulfilled by the mere presence of perceptions of connections to others.
Another question arises concerning relationships that are characterized by perceptions of burdensomeness – can those relationships satisfy the need to belong? Does the presence of perceptions of burdensomeness preclude the satisfaction of the need to belong? Imagine a prison inmate whose wife and children come to visit each month. This individual might feel cared about by his family and experience positive interactions during these visits. However, imagine also that this individual believes that the stress of his incarceration on his family is too much for them and that they would be better off if he were gone. In this instance, a degree of belongingness is evident in the presence of strong perceptions of burdensomeness.
But what about the prison inmate who has no family or friends – what about individuals for whom meaningful connections are absent? Does this condition preclude the development of perceptions of burdensomeness – as raised above, is some degree of belonging necessary for the development of perceptions of burdensomeness? Again, we suggest that this is not the case because the presence of human connections does not in itself satisfy the need to belong; thus, even the most isolated individuals typically possess some degree of connection to others (e.g., estranged family members, health care providers, neighbors) and those connections could be characterized by perceptions of burdensomeness. Second, those individuals who perceive total isolation from others are most likely alienated to the point that they perceive themselves as completely inconsequential and/or unwanted– a state akin to perceptions of expendability posited to function as behavioral indicators of perceived burdensomeness. Thus, according to the theory, thwarted belongingness and perceived burdensomeness are related, but distinct constructs. Empirical findings are supportive, with prior studies indicating a significant correlation of moderate magnitude between the two constructs (e.g., zero order correlation coefficient of .58; Van Orden, Witte, Gordon, Bender, & Joiner, 2008).
Acquired Capability for Suicide
The models of suicide described above assume that suicide is multifactorially caused such that suicidal ideation results from the fewest number of co-occurring risk factors, suicide attempts from a greater number, and death by suicide from the co-occurrence of the greatest number. These models also assume that risk for suicide is elevated due to greater risk for suicidal desire, and perhaps, increasingly severe forms of suicidal desire. These assumptions remain unchallenged by current theories and models of suicide. In contrast, according to the Interpersonal Theory, desire to die by suicide is not sufficient for lethal suicidal behavior to result because, simply put, dying by suicide is not an easy thing to do. Consider the following case example of a woman who died by suicide (Holm-Denoma, Witte, Gordon, Herzog, Franko, Fichter, et al., 2008): “Case #7 was described as being socially isolated when she attempted suicide with an unknown quantity and type of pain medication and also opened her wrist arteries. This action led to some degree of unconsciousness, from which she awoke… She then threw herself in front of a train, which was the ultimate cause of her death” (p. 233). In this case, initial behaviors were not lethal, and to bring about death, the individual engaged in another method of suicide. These are frightening and painful behaviors.
According to the theory, in order to die by suicide, individuals must lose some of the fear associated with suicidal behaviors, and that it would be very uncommon (if not impossible) to find someone born with a level of fear low enough to engage in suicide. Why might this be the case? Ohman and Mineka (2001) propose an evolutionary-based model of fear grounded in the hypothesis that natural selection processes have shaped the human fear system so that it functions as a signal for the presence of “potentially life-threatening situations in the ecology of our distant forefathers” (p. 484). Thus, these authors posit that the adaptive value of fear (i.e., why humans who possess the fear system are more likely to survive and thus reproduce) lies in its potential to aid humans in the identification of stimuli associated with threats to survival. The Interpersonal Theory draws upon—and extends—evolutionary models of fear and anxiety by proposing that humans are biologically prepared to fear suicide because suicidal behavior involves exposure to stimuli and cues that have long been associated with threats to survival.
And yet, some individuals die by suicide. According to the theory, it is possible to acquire the capability for suicide, which is composed of both increased physical pain tolerance and reduced fear of death, through habituation and activation of opponent processes, in response to repeated exposure to physically painful and/or fear-inducing experiences. In other words, through repeated practice and exposure, an individual can habituate to the physically painful and fearful aspects of self-harm, making it possible for him or her to engage in increasingly painful, physically damaging, and lethal forms of self-harm. Further, acquired capability is presumed to be a multidimensional emergent latent variable that involves the dimensions of lowered fear of death and increased physical pain tolerance, as depicted in the top of Figure 4.
Lowered fear of death
Fear of suicide is one category of reasons that individuals give when asked why they do not engage in suicidal behavior (Linehan, Goodstein, Nielsen, & Chiles, 1983). Further, an investigation of reasons for living, including fear of suicide, found that individuals who reported a history of “past serious ideation” about suicide (p. 280) but had not attempted suicide reported higher levels of fear of suicide compared to individuals with serious ideation who had acted on this ideation through suicidal behaviors (Linehan, Goodstein, Nielsen, & Chiles, 1983). These data suggest that suicidal ideation (cf., suicidal desire) is not sufficient for suicide attempts to result; rather, suicidal desire must occur in the context of reduced fear of suicide. Fear of suicide is presumed to be a dimensional construct varying from very high levels to negligible levels of fear, and further, in order for active suicidal desire to progress towards more severe manifestations of suicide risk (i.e., intent for suicide), fear must be reduced to the point that individuals endorse a non-zero degree of fearlessness regarding suicidal actions. To operationalize this construct, and thus potentially falsify the theory, fearlessness about suicide can be measured using the Beck Suicide Scale (Beck & Streer, 1991) item number 14, with responses two and three indicating reduced fear: response one: “I do not have the courage or the ability to commit suicide”; response two: “I am unsure that I have the courage or the ability to commit suicide”; response three: “I have the courage and the ability to commit suicide.” In support of this threshold for fear reduction, this item is strongly associated (i.e., r = .79) with a self-report measure of acquired capability (Van Orden, Witte, Gordon, Bender, & Joiner, 2008).
Elevated physical pain tolerance
Dying by suicide is not only frightening, but physically painful. Consider the following case example of a woman who died by suicide (Holm-Denoma, et al., 2008): “Case #1 ingested an unknown quantity of chloral hydrate and 354.9 mL of Lysol Toilet Bowl Cleaner [which contains hydrochloric acid (HCL)]… and died 4 hours after being transported to the emergency room due to gastric hemorrhaging” (p. 233). Swallowing hydrochloric acid requires a tolerance for physical pain that most do not possess. The empirical literature concurs with this case example: individuals with recent suicidal behavior demonstrate elevated physical pain tolerance (as measured by electric shock and thermal pain) compared to non-suicidal psychiatric patients and individuals in the community (Orbach, Mikulincer, King, Cohen, & Stein, 1997; Orbach, Palgi, Stein, HarEven, LotemPeleg, Asherov, et al., 1996) and compared to individuals admitted to the emergency room due to accident injuries (Orbach, Stein, Palgi, Asherov, HarEven, & Elizur, 1996). The latter finding indicates that elevated pain tolerance is likely specific to suicidal behavior, rather than physical injury more generally. In addition, more serious levels of suicidal ideation have been shown to predict higher levels of self-administered shock (Berman & Walley, 2003).
Pain tolerance is conceptualized as a dimensional phenomenon. What level of pain tolerance is necessary to allow lethal (or near lethal) suicidal behavior to occur? First, this construct is likely highly method-specific, thus someone gaining the requisite pain tolerance to engage in cutting behaviors will not necessarily have gained the same tolerance for other methods, such as jumping. In this way, we are able to provide an explanation for data indicating that method substitution does not typically occur. In addition, the type of actions involved must also be considered. For example, cutting one’s wrists requires sustained behavior on the part of the suicidal individual, and this individual must continue cutting his/her wrist in spite of the physical pain endured. An individual swallowing pills must continue to do so in spite of feelings of nausea or dizziness. In contrast, pulling the trigger on a gun or jumping off a building typically require a single action. We propose that both expectations about pain-to-be-experienced (e.g., “I won’t feel anything once I pull the trigger”), physiological habituation to physical pain sensations, and cognitive appraisals of the tolerability of expected/experienced pain are key factors in determining individuals’ tolerance for the pain involved in a specific suicide method. According to the theory, the common and proximate factor among all methods that serves as either a barrier or facilitator of lethal (or near lethal) suicidal behavior is the presence of a cognitive appraisal that the pain involved in the chosen method of suicide is tolerable. In order for lethal (or near lethal) suicide attempts to result, this cognitive appraisal must be non-ambivalent and held with a strength of conviction of 100% (with duration of non-ambivalence varying by method).
Habituation and Opponent Processes
The theory also includes a description of mechanisms whereby individuals acquire the capability for suicide; it is for this reason that the acquired capability latent variable is depicted in Figure 4 as an emergent variable (i.e., one that is caused by other variables in the model). How does the acquired capability develop? We propose that the mechanisms whereby individuals acquire the capability for lethal self-injury are habituation (to fear and pain involved in self-injury) and the strengthening of opponent processes (in response to fear and pain); both processes are described by Opponent Process Theory (Solomon & Corbit, 1974). Opponent process theory states that observed emotional responses are a function of the summation of two underlying oppositely valenced processes (i.e., opponent processes). Further, with repeated exposure, the emotional effects of the opposite process become amplified (while the primary emotional effects of a stimulus remain stable). This results in a net change in the observed response to be more similar to the valence of the opponent process, which behaviorally manifests as habituation. For example, an individual’s initial, primary response to a stimulus such as bungee jumping will likely be fear. However with repeated exposure to bungee jumping, the effect of the primary process (e.g., fear) will remain stable while the effect of the opponent process (e.g., exhilaration) will become amplified, yielding a net observed emotional response of decreased fear. If the process is continued long enough, eventually the strength of the opponent process will be such that the valence of the observed emotional experience shifts from negative to less negative to positive.
The Interpersonal Theory involves an application of Solomon and Corbit’s (1974) ideas to self-harm behaviors such that that the primary effect of painful and provocative stimuli (e.g., self harm) is fear and pain and that the opponent processes are relief and analgesia. However, the Interpersonal Theory differs in that it includes a proposal that the primary process also weakens. Thus, through repeated practice, what was originally a painful and/or fear-inducing experience (i.e., self-injury) may become less frightening as well as a source of emotional relief, thereby rendering individuals capable of engaging in what were previously painful and frightening behaviors. While it has been observed that increases in positive affect may occur subsequent to self-harm without suicidal intent (Brain, Haines, & Williams, 1998; Muehlenkamp, Engel, Wadeson, Crosby, Wonderlich, Simonich, et al., 2009), data are not available that examine changes in positive affect during or after suicidal behaviors.
Painful and Provocative Experiences
The risk factors depicted in Figure 4—childhood maltreatment, clustering, combat exposure, impulsivity, and previous suicide attempts—are posited to increase risk for lethal suicidal behavior because they are physically painful and/or sufficiently frightening to engage habituation and opponent processes with regards to the pain and fear involved in self-harm. In addition, factors such as limiting access to lethal means may serve to block acquired capability, thus reducing rates of suicide.
Our review of risk factors for suicide indicates that a history of a past suicide attempt is another of the strongest and most reliable predictors of suicidal behavior; however, the literature also indicates that the majority of individuals who attempt suicide will not eventually die by suicide and that many individuals (i.e., up to half) who die by suicide do so on their first attempt (Rudd, Joiner, & Rajab, 1996). The construct of acquired capability provides a framework for understanding the complex relations between a history of past attempts and risk for future suicidal behavior. According to the theory, the most direct route (but not the only route) to acquiring the capability for suicide (i.e., the most potent painful and provocative experience) is by engaging in suicidal behavior, either through suicide attempts, aborted suicide attempts (preparing for the attempt and nearly carrying it out), or practicing/preparing for suicidal behavior (e.g., tying a noose; buying a gun with intent to engage in suicidal behavior; imagining one’s death by suicide). Suicide attempts are the most potent of these behaviors with regards to acquiring the capability for suicide; thus, a potential way to falsify the theory would be to show that individuals with histories of past attempts have equivalent levels of acquired capability to those without past attempts.
Initial tests conducted by our laboratory group on acquired capability opened the theory to falsification by examining the association between number of past suicide attempts and self-reported level of acquired capability, as measured by a self-report measure, the Acquired Capability for Suicide Scale (ACSS) (Van Orden, Witte, Gordon, Bender, & Joiner, 2008). The ACSS assesses fearlessness about lethal self-injury as well as self-perceived ability to tolerate the pain involved in self-injury (e.g., “I can tolerate more pain than most people” and “The pain involved in dying frightens me” [reversed]). Results indicated that number of past attempts positively correlated with levels of acquired capability, with highest levels of acquired capability reported by individuals with multiple past attempts. Further, a study on military personnel found that the branch of service (e.g., Army vs. Navy) was associated with a specific method of suicide (i.e., guns for Army; hanging/knots for Navy; falling/heights for Air Force). These data suggest that habituation to the pain and fear in suicide may be method specific and is acquired through exposure.
However, the capability for self-harm can be acquired through behaviors other than suicide attempts; thus, the theory would not generate the prediction that all individuals who die by suicide would necessarily have histories of prior attempts. This aspect of the theory is depicted graphically by the presence of other painful and provocative experiences in Figure 4 that are posited to activate habituation/opponent processes, thereby giving rise to acquired capability. In addition to previous suicidal behavior, other less potent pathways may also exist through the experience of other fear-inducing, risky behaviors. This aspect of the theory organizes a great deal of the literature on risk factors (described above) that otherwise appears disparate. Childhood maltreatment that involves physical and sexual abuse may activate habituation with regards to fear of self-injury as well as increased pain tolerance. Exposure to others who have engaged in suicidal behavior may activate habituation to the fear of suicidal behavior, thus accounting for clustering of suicidal behavior as a by-product of elevated acquired capability. Combat exposure, which involves exposure to the fear of one’s own possible death, as well as killing others, represents a relatively direct pathway, according to the theory.
In support of a less direct route to acquired capability, one study found that individuals who reported engaging in more painful and provocative experiences (e.g., shoplifting, promiscuous sex, played contact sports, got a piercing, shot a gun, intentionally hurt animals, physical fights, jumped from high places) also reported higher acquired capability scores (Van Orden, Witte, Gordon, Bender, & Joiner, 2008). These results persisted after controlling for potentially confounding variables, including current level of suicidal ideation, age, gender, and depressive symptoms. Suicidal ideation was controlled for in this particular analysis because, according to the theory, it is possible to be capable of suicidal behavior without desiring suicide.
Veterans are at increased risk for lethal suicidal behavior and are more likely to use firearms as the suicide method (Kaplan, Huguet, McFarland, & Newsom, 2007); the increased risk for use of firearms is notable given that this population has extensive exposure to firearms, thus providing ample opportunities to habituate to the fearsome aspects of the use of firearms. A psychological autopsy study found that retrospectively assessed levels of acquired capability—sample items included the prior engagement in suicide-preparatory behaviors, past suicide attempts, and problems with impulsivity—discriminated between living controls and those who died by suicide in a military sample (Nademin, Jobes, Pflanz, Jacoby, Ghahramanlou-Holloway, Campise, et al., 2008).
The theory does not preclude more complex relations between risk factors. Studies document a relationship between the trait of impulsivity and suicidal behavior: impulsive people do not necessarily make impulsive suicide attempts; in fact, people who have engaged in more impulsive behaviors have been shown to engage in more prior planning for suicide attempts and use more medically serious methods. The construct of acquired capability provides a parsimonious explanation for this array of facts: impulsive and/or aggressive individuals are more likely to engage in behaviors that are painful and provocative (e.g., physical fights, injecting drugs). Because of this, we propose that impulsive individuals have higher levels of acquired capability for suicide and it is this consequence of impulsivity that elevates risk for suicidal behavior. Regarding the relationship between the planfulness of suicide attempts and their lethality, we propose that this is also related to habituation to painful and provocative experiences. Specifically, an individual who spends a great deal of time planning an attempt is not only making pragmatic arrangements for his or her death, but is also habituating to the fear associated with making a suicide attempt (i.e., is engaging in mental practice). Thus, while the capability for suicide is conceptualized as a capability that is gained over time, we also propose that through genetic and/or temperamental predispositions to fearlessness, impulsivity, or greater physical pain tolerance, some individuals are more susceptible to acquiring the capability for suicide given exposure to painful and provocative events, or even more likely to seek such events out.
The proposal that mental practice is an element of acquiring the capability for suicide provides one possible explanation for the fact that method substitution—when access to a means for suicide is blocked—does not occur. Working up to the act of suicide is quite difficult to do; habituating to one means does not necessarily result in habituation to another. Theoretical accounts of suicide that focus only on suicidal desire struggle to account for these data on method substitution (and for many other findings too).
The Proximal Causal Pathway to Suicide
Hypothesis 1: Passive Suicidal Ideation
The theory involves four hypotheses that are listed in Table 2. These hypotheses are depicted graphically in Figure 5, which illustrates the etiology of suicide according to the Interpersonal Theory. The causal process is depicted from left to right beginning with thwarted belongingness and perceived burdensomeness and ending with lethal (or near lethal) suicidal behavior at the far right. The model also contains latent variable interactions, moderating effects, and emergent variables, each of which will be discussed in detail. The Interpersonal Theory is concerned with proximal risk factors – the mental states and behavioral capacities that will be evident in an individual at varying degrees of non-zero risk for lethal suicidal behavior, ranging from individuals evidencing passive suicidal ideation up to those demonstrating imminent risk for lethal suicidal behavior. The causal process depicted in Figure 5 also illustrates those factors that are present at varying degrees of risk, with the lowest level of risk for suicide toward the left of the figure, with risk incrementally increasing toward the right end of the figure.
Figure 5.
Causal pathway to lethal suicidal behavior.
Note. H1 = Hypothesis 1, H2 = Hypothesis 2, H3 = Hypothesis 3, H4 = Hypothesis 4. For text of hypotheses, see Table 1
The theory’s first hypothesis is that thwarted belongingness and perceived burdensomeness are proximal and sufficient causes of passive suicidal ideation. Individuals who possess either complete thwarted belongingness or complete perceived burdensomeness will experience passive (versus active) suicidal ideation, which may manifest as cognitions such as, “I wish I was dead” or “I would be better off dead.” In contrast, active suicidal ideation is marked by an active desire to engage in behaviors to take one’s life (e.g., “I want to kill myself”). This hypothesis is depicted in the far left of Figure 2, which also illustrates independent causal paths between thwarted belongingness and passive suicidal ideation and perceived burdensomeness and passive suicidal ideation. Note however, that these causal paths do not continue beyond passive suicidal ideation, a point addressed by the next hypothesis.
The theory could be falsified if studies do not document independent associations for both thwarted belongingness and perceived burdensomeness with suicidal ideation or behaviors. Two studies have opened the theory to falsification by examining the hypothesized relation between perceived burdensomeness and indices of suicidal behavior. First, perceived burdensomeness measured by self-report in a clinical sample was shown to cross-sectionally predict greater severity of suicidal ideation and greater numbers of past suicide attempts, while controlling for age, gender, personality disorder status, depressive symptoms, and hopelessness (Van Orden, Lynam, Hollar, & Joiner, 2006). Second, an examination of the content of suicide notes found higher levels of perceived burdensomeness in notes from individuals who died by suicide compared to notes from individuals who attempted but survived (Joiner et al., 2002). Results of these studies indicate an association between perceptions of burdensomeness and suicidal ideation (though thwarted belongingness was not measured in either study thus precluding conclusions regarding the effects of the presence of both constructs).
Several studies have examined the relation between thwarted belongingness and indices of suicidal behavior. One study examined the relation between thwarted belongingness measured by self-report and likelihood of having a past suicide attempt (Conner, Britton, Sworts, & Joiner, 2007) among methadone maintenance patients at an urban university hospital. Results indicated that a one-point increase on the belongingness subscale (indicating greater belongingness) decreased odds of having a past suicide attempt by six percent; the same association did not hold for accidental overdoses, supporting the specificity of thwarted belongingness to suicidal behavior. The relationship between thwarted belongingness and suicidal desire was also supported by a series of studies investigating the phenomenon of “pulling together” after positive collective experiences, in this case, sporting events (Joiner, Hollar, & Van Orden, 2006). These studies indicated that lower suicide rates were associated with sports team successes, which is consistent with the hypothesis that sporting events may foster increased belongingness and thereby buffer suicide rates.
Regarding thwarted belongingness, this hypothesis could be falsified if studies do not demonstrate the presence of passive suicidal ideation among all individuals with a completely thwarted need to belong (i.e., those holding perceptions that all meaningful and reciprocally-caring relationships are absent). Regarding perceptions of burdensomeness, this hypothesis could be falsified if studies do not demonstrate the presence of passive suicidal ideation among all individuals with global perceived burdensomeness (i.e., those who perceive themselves as a burden on all significant others and who experience a non-zero degree of self-hate secondary to these perceptions). Note, however, that this hypothesis does not posit that these factors are necessary, but instead, allows for situations in which passive suicidal ideation may result from other causes. The degree to which the theory’s constructs are necessary for suicidal behavior remains an empirical question and is addressed in later sections.
Hypothesis 2: Suicidal Desire
The literature on suicide indicates that among those who have passive thoughts of suicide (e.g., “I would be better off dead”), most will not experience active suicidal ideation involving thoughts of killing themselves (Thomas, Crawford, Meltzer, & Lewis, 2002). Consistent with this fact, the theory includes the hypothesis that in order for a passive desire for suicide to intensify into an active desire for suicide, a completely thwarted need to belong must be accompanied by global perceived burdensomeness, as well as hopelessness regarding these two painful states. Thus, the theory’s second hypothesis states that a mental state characterized by the simultaneous presence of thwarted belongingness, perceived burdensomeness, and hopelessness about one’s interpersonal connections is a proximal and sufficient cause of suicidal desire. This hypothesis is graphically depicted in the middle of Figure 5 with the intersection of thwarted belongingness, perceived burdensomeness, and hopelessness regarding these states causing desire for suicide (e.g., thoughts such as “I want to kill myself”).
According to the theory, the absence of either thwarted belongingness (perceived as unchanging) or perceived burdensomeness (also perceived as unchanging) is likely to be lifesaving, as active suicidal desire develops only in the confluence of both factors. Thus, this hypothesis could be falsified if individuals who are elevated on only thwarted belongingness or perceived burdensomeness demonstrate more severe (or equivalent) suicidal ideation compared to individuals who are elevated on both. Two studies have opened the theory to falsification by examining this prediction. In the first study (Van Orden, Witte, Gordon, Bender, & Joiner, 2008), the most severe levels of suicidal desire (operationalized as suicidal ideation on the Beck Suicide Scale) were reported by undergraduates at the most severe levels (in the sample) on both thwarted belongingness and perceived burdensomeness, relative to individuals with severe levels of only thwarted belongingness or perceived burdensomeness. This result was observed above and beyond age, gender, and level of depression. In the second study (Joiner, Van Orden, Witte, Selby, Ribeiro, & Lewis, in press), using an ethnically diverse community sample, young adults with low levels of both family support (cf. low belongingness) and mattering to others (cf. perceived burdensomeness) demonstrated the most severe levels of suicidal ideation, while including both six-month and lifetime histories of depression as covariates, indicating that the theory’s variables predicted suicidal desire above and beyond the contribution of depression. Findings from these studies suggest that when people hold two psychological states in their minds simultaneously—low belongingness and perceived burdensomeness—risk for the development of suicidal desire is elevated (and this occurs beyond the effects of depression).
However, in order for active suicidal desire to develop, individuals must perceive their levels of belongingness and burdensomeness to be stable and permanent – in other words, they must be hopeless about their perceived interpersonal status. This hypothesis builds upon the empirical and theoretical literature on the association between hopelessness and lethal suicidal behavior (see Table 1). A meta-analytic review showed that the Beck Hopelessness Scale (BHS; (Beck, Weissman, Lester, & Trexler, 1974), using a cut-off score of 9, is predictive of both lethal and non-lethal suicide attempts (McMillan, Gilbody, Beresford, & Neilly, 2007). The sensitivity (i.e. the probability of a positive test result among individuals who went on to die by suicide) of the BHS was .80 for predicting death by suicide and .78 for non-fatal suicide attempts. This indicates that approximately 80% of people who engaged in serious suicidal behavior score above this cut-off point on the BHS. This finding is certainly supportive of the notion that hopelessness is associated with suicidal behavior. Nevertheless, the specificity of the BHS (i.e., the probability of a negative test result among those who did not engage in suicidal behavior) was 0.42 for both fatal and non-fatal suicide attempts. This indicates that nearly 60% of those who did not make a suicide attempt had a cut-off score above 9 on the BHS. Taken together, these data indicate that hopelessness is sensitive in the prediction of suicidal behavior, but it performs less well regarding specificity: most hopeless individuals will not die by suicide.
We propose that one explanation for this well-replicated finding is that the content of hopeless beliefs—what individuals are hopeless about—is relevant in the prediction of suicidal behavior. We propose that it is only hopelessness regarding complete and pervasive thwarted belongingness and perceived burdensomeness that will cause active suicidal desire because it is only at this juncture of mental states that individuals see no possibility of positive change. This hypothesis could be falsified if individuals demonstrating hopelessness about thwarted belongingness and perceived burdensomeness are more likely to report passive, rather than active suicidal ideation; for example, a counter hypothesis could propose that hopelessness causes individuals to shut down so that active behavior and ideation, including suicide-related, are suppressed.
Hypothesis 3: Suicidal Intent
Intent to engage in suicidal behavior has been found to be part of a pernicious group of suicidal symptoms termed “resolved plans and preparation” (Joiner, Rudd, & Rajab, 1997; Witte, Joiner, Brown, Beck, Beckman, Duberstein, et al., 2006) and has been shown to predict death by suicide in adults (Conner, Duberstein, & Conwell, 1999; Harriss, Hawton, & Zahl, 2005; Obafunwa & Busuttil, 1994). Current intent for suicide is a key component of suicide risk assessment protocols (Brent, 2001; Jobes, 2006; Joiner, Walker, Rudd, & Jobes, 1999; Linehan, Comtois, & Murray, 2000; Reynolds, 1991; Shea, 1999; Simon, 2006) and is conceptualized as a necessary component of serious, imminent risk for suicide. Thus, the presence of intent can also be conceptualized as the level of suicidal desire that is most likely to translate into behavior. However, we posit that in order to possess suicidal intent, individuals must have habituated to the fear involved in suicide to an extent that they are able to imagine, plan, or decide to engage in suicidal actions. Thus, it is hypothesized (as depicted in Figure 5) that the simultaneous presence of suicidal desire and the first component of acquired capability—lowered fear of death—serves as the condition under which suicidal desire will transform into suicidal intent.
This hypothesis would be falsified if, among those with suicidal desire, studies documented a lack of an association between fear of suicide and suicidal intent. Stronger tests could examine the sensitivity and specificity of decreased fear of suicide (e.g., a non zero response on a measure of confidence regarding suicide) in the identification of suicidal intent among individuals with suicidal desire. The strongest test would involve examining the prediction that among individuals with suicidal intent, all would demonstrate fearlessness of suicide.
Hypothesis Four: Lethal (and near lethal) Suicide Attempts
The theory’s final hypothesis directly addresses the relative rarity of lethal suicidal behavior compared to non-lethal attempts and suicidal ideation. As depicted in Figure 1, the theory involves the assumption that there are relatively large numbers of people who desire suicide and moderate numbers of those who have developed the capacity for suicidal behavior, but the presence of both should be comparatively rare. Crucially, however, the theory’s fourth hypothesis is that the outcome of serious suicidal behavior (i.e., lethal or near lethal suicide attempts) is most likely to occur in the context of suicidal intent (which results from thwarted belongingness, perceived burdensomeness, and hopelessness regarding both), reduced fear of suicide, and elevated physical pain tolerance. This hypothesis is depicted in Figure 5 as the final causal arrow from suicidal intent to lethal (or near lethal) suicide attempts. Notice that this causal path is moderated by the presence of increased pain tolerance: suicidal intent does not result in lethal (or near lethal) suicide attempts unless increased pain tolerance is present that allows an individuals to endure the pain involved in dying by suicide.
To examine the theory’s prediction regarding the role of physical pain tolerance as a final barrier to the outcome of lethal suicidal behavior, longitudinal studies could examine physical pain tolerance and follow individuals over time to see if physical pain tolerance is elevated among individuals who die by suicide. Another approach could compare individuals who survived attempts that are almost always lethal (e.g., jumping from the Golden Gate Bridge) to survivors who called for help after engaging (or beginning to engage) in suicidal behavior. Although this approach would necessarily involve retrospective reports (thereby introducing recall biases), cognitive appraisals of the degree to which pain associated with the chosen suicide method was tolerable at the time of the intent could be compared between the groups. The theory’s hypothesis would be falsified if individuals who called for help reported greater appraisals of tolerability compared to the individuals whose survival could be attributed to chance.
The theory’s final hypothesis can also be empirically examined with regards to the prediction that the greatest risk for suicide is conferred by the simultaneous presence of thwarted belongingness, perceived burdensomeness, hopelessness in relation to both, and acquired capability for lethal self-injury. Psychological autopsy methods, whereby the characteristics of individuals who died by suicide are assessed, could be used to examine the proportion who evidenced all of the theory’s constructs. This proportion could be compared to the proportion from a sample of non-lethal suicide attempters. The theory’s hypothesis would be falsified if a greater proportion of non-lethal attempters evidenced all of the theory’s constructs compared to lethal attempters.
This hypothesis would also be falsified if greater risk for suicide was not found among those demonstrating more severe levels of the theory’s constructs. Using a sample of clinical outpatients, one study used self-reports of perceptions of burdensomeness and acquired capability as (partial) indices of suicidal desire and capability for suicide respectively, and measured risk for suicidal behavior, as rated by clinicians, using a standardized risk assessment framework (Joiner, Walker, Rudd, & Jobes, 1999; Van Orden, Witte, Gordon, Bender, & Joiner, 2008, Study 3). Consistent with Hypothesis Four, results indicated a significant interaction between perceived burdensomeness and acquired capability in the prediction of clinician-rated risk for suicide, above and beyond the effects of other risk factors (i.e., depression scores, gender, and age). In line with predictions, the form of the interaction indicated that individuals high on both perceived burdensomeness and acquired capability were rated at highest risk for suicide by clinicians. The limitation of this finding, of course, is that desire was only partially measured – belongingness was not included.
To remedy this, members of our research group studied a sample of young adults experiencing a suicidal crisis (Joiner et al., 2009, Study 2). Some participants’ crises involved a suicide attempt, while others experienced serious suicidal desire in the absence of attempts. Results were consistent with the theory and indicated that the three-way interaction of thwarted belongingness, perceived burdensomeness, and acquired capability (measured by number of past suicide attempts) predicted whether or not participants’ current suicidal crises involved suicide attempts. Results indicated that the combination of high levels of both thwarted belongingness and perceived burdensomeness was most likely to translate into suicide attempts in the presence of higher levels of acquired capability (i.e., greater numbers of past attempts). Results were obtained above and beyond the contribution of numerous documented risk factors for suicidality, including depression, hopelessness, and borderline personality disorder features.
If empirically supported with lethal suicidal behavior, the final hypothesis of the theory could provide an explanation for the imprecision of the individual risk factors: unless a risk factor causes both desire and capability for suicide, its specificity in the prediction of lethal suicidal behavior will be low. The Interpersonal Theory’s final hypothesis provides a parsimonious account for mechanisms whereby risk factors for suicide confer risk: risk factors—such as mental disorders and childhood abuse—confer risk for suicidal behavior indirectly by increasing—or indicating the presence of—experiences of thwarted belongingness, perceived burdensomeness, and pain/provocation.
Consider the role of mental disorders: individuals who suffer from mental disorders are at elevated risk for suicide (with some disorders conferring greater risk than others), but the vast majority of these individuals will not demonstrate suicidal behaviors. As one example, consider borderline personality disorder. A hallmark feature of BPD is repeated non-lethal, self-injurious behavior, which according to the theory represents a relatively direct pathway to the acquired capability to lethal self-injury. This hypothesis that individuals with BPD may be more likely to have acquired the capability for lethal self-injury is consistent with the fact that approximately 60–70% of people with BPD have made at least one severe suicide attempt (Gunderson, 2001). Another hallmark feature of BPD is extreme fear of abandonment (American Psychiatric Association, 2000), a symptom that likely relates to thwarted belongingness. In fact, it is often during threatened or real abandonment episodes when individuals with BPD engage in self-injurious behavior (American Psychiatric Association, 2000). Research also suggests that individuals with BPD may be more prone to perceptions of burdensomeness: self-hate, self-blame, and strong feelings of shame are common among individuals with BPD (Linehan, 1993; Rizvi & Linehan, 2005), and it is likely that feelings of shame accompany perceptions that one is a burden on others. Thus, according to the Interpersonal Theory, high rates of suicidal behavior among individuals with BPD may be due to the fact that these individuals are more susceptible to thwarted belongingness and perceived burdensomeness and more likely to engage in painful and provocative events that lead to an acquired capability.
Consider also that Anorexia Nervosa is associated with a high suicide rate (Keel, Dorer, Eddy, Franko, Charatan, & Herzog, 2003). Members of our research group examined methods of suicide among a sample of nine women with AN who died by suicide in order to investigate competing hypotheses about the relation between AN and suicidal behavior (Holm-Denoma, et al., 2008). One possibility is that these women were physically fragile due to AN, and died using methods that would be relatively less lethal among physically healthy adults (i.e., those without compromised body weight). Another possibility is that these women died using methods that would be highly lethal among physically healthy adults because they had acquired the capability for suicidal behavior through the painful experience of self-starvation. Results were consistent with the latter hypothesis: out of nine women with AN who died by suicide, all used methods that would be lethal for physically healthy individuals (e.g., jumping in front of a train) and seven were unlikely to be rescued following their attempts. This study suggests that the high rate of suicidal behavior among individuals with AN may be accounted for, in part, by experiences of pain and provocation that are a central component of the disorder (e.g., self-starvation) and that may foster acquired capability for suicidal behavior.
Conclusions and Future Directions
In the current paper, we examined the literature on empirically demonstrated risk factors for suicidal behavior and demonstrated how the Interpersonal Theory is able to account for these facts about suicidal behavior. The theory involves the assumption that, to a large extent, the same mental processes underlie all forms of suicidal behavior. Thus, when looking to the literature on suicidal behavior, available data should be consistent with the role of all constructs in the development of suicidal desire. Figures 2–4 depict the hypothesis that empirically-supported risk factors for suicide elevate risk because they are indicators of thwarted belongingness, perceived burdensomeness, or the acquired capability. Our discussion illustrated mechanisms whereby risk factors influence the constructs of the theory. This description of mechanisms underlying proximal risk for suicidal behavior provides a parsimonious account for why the majority of individuals who possess a given risk factor will not attempt or die by suicide – few risk factors increase all components of the Interpersonal Theory. The theory also provides explanations for heretofore difficult to explain epidemiological facts about suicide – including the gender distribution and prevalence of different forms of suicidal behavior – facts that available theories are unable to explain fully.
One of the most consistent findings with regards to the epidemiology of suicidal behavior is its gender distribution. Male suicides outnumber female suicides worldwide, yet far more females than males are engaging in ultimately non-lethal suicidal behavior. Studies suggest that women may be more likely to experience many risk factors that increase—or indicate the presence of—thwarted belongingness and perceived burdensomeness, including major depression (i.e., females are approximately twice as likely as males to suffer from Major Depression; Nolen-Hoeksema, Larson, & Grayson, 1999). In addition, data indicate that women rank helping others, having a close family, and being loved by loved ones significantly higher than do men as sources of happiness (Crossley & Langdridge, 2005), suggesting that when these potential sources of happiness are absent, women are particularly likely to perceive thwarted belongingness and high burdensomeness, and thus suffer greater emotional pain than men in the same situations. However, because females on the whole have fewer experiences that inure them to fear of self-injury (e.g., exposure to guns, physical fights, violent sports, etc.), and because they have lower pain and fear tolerance than males (Berkley, 1997), they may be less able to develop the acquired capability for suicidal behavior than are males. Therefore, although women may be more likely than males to desire suicide, they are less likely to die by suicide.
The Interpersonal Theory is also able to explain the prevalence of suicidal behavior. The theory involves three conditions that, when present simultaneously, are sufficient to result in lethal (or near lethal) suicide attempts. As each of these conditions is relatively rare, and their confluence more so, the theory is consistent with the rarity of suicidal behavior itself.
Available theories are unable to explain these aspects of suicidal behavior as these theories assume that risk for suicide is elevated solely through increasingly severe levels of desire for suicide. This assumption is exemplified in several descriptive models that account for the prevalence of suicidal behavior by positing the necessary presence of numerous risk factors for suicidal desire. These models, however, are unable to explain facts about suicide such as the gender distribution and seasonal variation, and lack the level of precision needed to prospectively predict suicidal behavior. In addition, as noted by Prinstein (2008), available theories do not, for the most part, address both intra-individual and inter-individual factors. The Interpersonal Theory emphasizes the role of acquired capability—a primarily intra-individual factor—as well as the role of thwarted belongingness and perceived burdensomeness—intrapersonal factors (i.e., emphasizing perceptions) that transact with the interpersonal environment.
Thus far, we have posited that the simultaneous presence of the theory’s constructs is sufficient, but not necessary, for suicidal behavior to occur. Thus, other pathways to suicidal behaviors are possible. However, a testable alternative is that the theory’s constructs represent the etiological mechanisms that underlie all forms of suicidal behavior. This alternative contrasts with many existing theoretical accounts. Consider, Baechler’s (1979) taxonomy of suicide that proposes all suicidal behavior seeks to solve a problem, but that the problem “solved” by suicide varies and results in types of suicide, each with different etiological origins, including escapist suicides (i.e., escape from grief or punishment), aggressive suicides (i.e., vengeance or blackmail), oblative suicides (i.e., sacrifice), and ludic suicides (i.e., proving onself; Shneidman, 2001). A recent review of the theoretical literature on suicide (Maris, Berman, & Silverman, 2000) addresses this assumption by asking, “Is suicide one thing or many things?” and answers, “it seems clear that the answer is ‘many’” (p. 50). We suggest that this assumption has been accepted because of the relative inability of previous theories to comprehensively explain and predict suicidal behavior. We also acknowledge that the question proposed by Maris and colleagues (2000) – “Is suicide one thing or many things?” – is an empirical one and is in need of scientific scrutiny. Further, the assumption that the same mechanisms underlie all suicidal behaviors—if it were supported—would greatly enhance the clinical utility of the theory. It is this application of the theory—clinical applications—to which we now turn.
One of the primary tasks facing clinicians working with suicidal patients is the assessment of the degree of risk faced by individual patients. Suicide risk assessment frameworks are formalized procedures for clinicians that synthesize the research on the many documented predictors of suicide and provide structured ways to assess both current and more long-standing risk. Applying the Interpersonal Theory to risk assessment suggests that risk assessment frameworks should explicitly address the degree to which patients are currently experiencing thwarted belongingness and perceived burdensomeness, as well as the degree to which they have acquired the capability for lethal self-harm. Risk assessment grounded in the Interpersonal Theory, if supported empirically, will allow for a more parsimonious and clinically useful conceptualization of the etiology of suicide because this conceptualization does not presume that to assess individuals’ degree of risk for suicide requires measurement (or estimation of) a vast number of risk factors. For more specific recommendations on using the Interpersonal Theory in suicide risk assessment (as well as treatment and prevention), readers are referred to Joiner, Van Orden, Witte, and Rudd (2009).
Clinical care for suicidal patients also involves treatment (i.e., psychotherapy and pharmacotherapy) aimed to reduce risk for engaging in suicidal behavior. Public health campaigns also aim to prevent suicidal behavior by targeting all individuals or those at elevated risk for developing thoughts about suicide or engaging in suicidal behavior. We propose that thwarted belongingness and perceived burdensomeness (as well as hopelessness concerning these states) are dynamic (i.e., frequently-changing) factors, while acquired capability, once acquired, is relatively stable and unchanging. These aspects of the theory are relevant for treatment. The theory includes a clearly delineated danger zone at the intersection of perceived burdensomeness, thwarted belongingness, and the acquired capability, and thus yields a clear prediction about what components of suicide interventions will be most effective at treating suicidal symptoms. According to the theory, interventions that directly or indirectly address perceived burdensomeness and thwarted belongingness should produce the best outcomes among suicidal individuals. The acquired capability would be relatively difficult to effectively address in treatment since a therapist is not able to modify a patient’s history, but this aspect of the theory does provide a clear prediction regarding who may benefit most from suicide focused preventive interventions: specifically, those who have a history fraught with painful and provocative experiences. The theory also suggests that prevention efforts targeting thwarted belongingness and perceived burdensomeness may be effective. For example, public health campaigns promoting the importance of maintaining social connections and social contributions could impact suicide rates. Using the Interpersonal Theory to improve clinical care for suicidal patients and as a basis for suicide prevention efforts would, we suggest, support Lewin’s (1951) claim that “there is nothing so practical as a good theory” (p. 169).
Acknowledgments
This research was supported, in part, by a grant from the National Institute of Mental Health to Tracy K. Witte and Thomas Joiner (1 F31 MH077386-01), a grant from the National Institute of Mental Health to Edward A. Selby and Thomas Joiner (1 F31MH081396) and a grant from the National Institute of Mental Health to Yeates Conwell (5T32MH020061-09).
Contributor Information
Kimberly A. Van Orden, University of Rochester Medical Center
Tracy K. Witte, Florida State University
Kelly C. Cukrowicz, Texas Tech University
Scott Braithwaite, Florida State University.
Edward A. Selby, Florida State University
Thomas E. Joiner, Jr., Florida State University
References
- Abe R, Shioiri T, Nishimura A, Nushida H, Ueno Y, Kojima M, et al. Economic slump and suicide method: preliminary study in Kobe. Psychiatry Clin Neurosci. 2004;58:213–216. doi: 10.1111/j.1440-1819.2003.01219.x. [DOI] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Adams DP, Barton C, Mitchell GL, Moore AL, Einagel V. Hearts and minds: suicide among United States combat troops in Vietnam, 1957–1973. Social Science and Medicine. 1998;47:1687–1694. doi: 10.1016/s0277-9536(98)00253-6. [DOI] [PubMed] [Google Scholar]
- Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. British Medical Journal. 2002;325:74. doi: 10.1136/bmj.325.7355.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajdacic-Gross V, Wang J, Bopp M, Eich D, Rossler W, Gutzwiller F. Are seasonalities in suicide dependent on suicide methods? A reappraisal. Social Science and Medicine. 2003;57:1173–1181. doi: 10.1016/s0277-9536(02)00493-8. [DOI] [PubMed] [Google Scholar]
- American Association of Suicidology. USA Suicide: 2003 Final Data. 2006 Retrieved May 30, 2006, from http://www.suicidology.org/associations/1045/files/2003datapgb.pdf.
- American Association of Suicidology. AAS statement on the economy and suicide. 2009 Retrieved August 18, 2009, from http://www.suicidology.org/web/guest/current-research.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision ed. [Google Scholar]
- Anisman H, Du L, Palkovits M, Faludi G, Kovacs GG, Szontagh-Kishazi P, et al. Serotonin receptor subtype and p11 mRNA expression in stress-relevant brain regions of suicide and control subjects. Journal of Psychiatry and Neuroscience. 2008;33:131–141. [PMC free article] [PubMed] [Google Scholar]
- Appleby L, Cooper J, Amos T, Faragher B. Psychological autopsy study of suicides by people aged under 35. The British journal of psychiatry: the journal of mental science. 1999;175:168–174. doi: 10.1192/bjp.175.2.168. [DOI] [PubMed] [Google Scholar]
- Arango V, Underwood MD, Gubbi AV, Mann JJ. Localized alterations in pre- and postsynaptic serotonin binding sites in the ventrolateral prefrontal cortex of suicide victims. Brain Research. 1995;688:121–133. doi: 10.1016/0006-8993(95)00523-s. [DOI] [PubMed] [Google Scholar]
- Arranz B, Eriksson A, Mellerup E, Plenge P, Marcusson J. Brain 5-HT1A, 5-HT1D, and 5-HT2 receptors in suicide victims. Biological Psychiatry. 1994;35:457–463. doi: 10.1016/0006-3223(94)90044-2. [DOI] [PubMed] [Google Scholar]
- Babidge NC, Buhrich N, Butler T. Mortality among homeless people with schizophrenia in Sydney, Australia: a 10-year follow-up. Acta Psychiatr Scand. 2001;103:105–110. doi: 10.1034/j.1600-0447.2001.00192.x. [DOI] [PubMed] [Google Scholar]
- Bach-Mizrachi H, Underwood MD, Tin A, Ellis SP, Mann JJ, Arango V. Elevated expression of tryptophan hydroxylase-2 mRNA at the neuronal level in the dorsal and median raphe nuclei of depressed suicides. Molecular Psychiatry. 2008;13:507–513. 465. doi: 10.1038/sj.mp.4002143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baechler J. Suicides. New York: Basic Books; 1979. [Google Scholar]
- Bagley C, Jacobson S, Rehin A. Completed suicide: a taxonomic analysis of clinical and social data. Psychological Medicine. 1976;6:429–438. doi: 10.1017/s0033291700015877. [DOI] [PubMed] [Google Scholar]
- Barak Y, Cohen A, Aizenberg D. Suicide among the homeless: a 9-year case-series analysis. Crisis. 2004;25:51–53. doi: 10.1027/0227-5910.25.2.51. [DOI] [PubMed] [Google Scholar]
- Barraclough BM, Pallis DJ. Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychological Medicine. 1975;5:55–61. doi: 10.1017/s0033291700007212. [DOI] [PubMed] [Google Scholar]
- Bastia BK, Kar N. A psychological autopsy study of suicidal hanging from Cuttack, India: focus on stressful life situations. Archives of Suicide Research. 2009;13:100–104. doi: 10.1080/13811110802572221. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychological Review. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, DeWall CN, Ciarocco NJ, Twenge JM. Social exclusion impairs self-regulation. Journal of Personality and Social Psychology. 2005;88:589–604. doi: 10.1037/0022-3514.88.4.589. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117:497–529. [PubMed] [Google Scholar]
- Baumeister RF, Twenge JM, Nuss CK. Effects of social exclusion on cognitive processes: anticipated aloneness reduces intelligent thought. Journal of Personality and Social Psychology. 2002;83:817–827. doi: 10.1037//0022-3514.83.4.817. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Child and young adolescent suicide in New Zealand. Australian and New Zealand Journal of Psychiatry. 2001;35:647–653. doi: 10.1080/0004867010060514. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide & Life Threatening Behavior. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- Beck AT. Beyond belief: A theory of modes, personality, and psychopathology. Salkovskis: Paul M; 1996. [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, et al. Relationship between hopelessness and ultimate suicide: A replication with psychiatric outpatients. American Journal of Psychiatry. 1990;147:190–195. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of Consulting and Clinical Psychology. 1989;57:309–310. doi: 10.1037//0022-006x.57.2.309. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: A 10-year prospective study of patients hospitalized with suicidal ideation. American Journal of Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Trexler LD. Alcohol abuse and eventual suicide: a 5- to 10-year prospective study of alcohol-abusing suicide attempters. Journal of Studies on Alcohol. 1989;50:202–209. doi: 10.15288/jsa.1989.50.202. [DOI] [PubMed] [Google Scholar]
- Beck AT, Streer RA. Manual for the Beck Scale for Suicide Ideation. San Antonio, TX: Psychological Corporation; 1991. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Berkley KJ. Sex differences in pain. Behavioral and Brain Sciences. 1997;20:371–380. doi: 10.1017/s0140525x97221485. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Berman ME, Walley JC. Imitation of self-aggressive behavior: An experimental test of the contagion hypothesis. Journal of Applied Social Psychology. 2003;33:1036–1057. [Google Scholar]
- Bickley H, Kapur N, Hunt IM, Robinson J, Meehan J, Parsons R, et al. Suicide in the homeless within 12 months of contact with mental health services: a national clinical survey in the UK. Soc Psychiatry Psychiatr Epidemiol. 2006;41:686–691. doi: 10.1007/s00127-006-0087-6. [DOI] [PubMed] [Google Scholar]
- Biller OA. Suicide related to the assassination of President John F. Kennedy. Suicide & Life Threatening Behavior. 1977;7:40–44. [PubMed] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackmore ER, Munce S, Weller I, Zagorski B, Stansfeld SA, Stewart DE, et al. Psychosocial and clinical correlates of suicidal acts: results from a national population survey. British Journal of Psychiatry. 2008;192:279–284. doi: 10.1192/bjp.bp.107.037382. [DOI] [PubMed] [Google Scholar]
- Blumenthal SJ, Kupfer DJ. Generalizable Treatment Strategies for Suicidal Behavior. Annals of the New York Academy of Sciences. 1986;487:327–340. doi: 10.1111/j.1749-6632.1986.tb27911.x. [DOI] [PubMed] [Google Scholar]
- Bostwick JM, Pankratz VS. Affective disorders and suicide risk: A reexamination. American Journal of Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Separation. 2. New York: Basic Books; 1973. Attachment and Loss. [Google Scholar]
- Brain KL, Haines J, Williams CL. The psychophysiology of repetitive self-mutilation. [Meeting Abstract] International Journal of Psychophysiology. 1998;30:218. [Google Scholar]
- Breault KD. Suicide in America: A Test of Durkheim’s Theory of Religious and Family Integration, 1933–1980. The American Journal of Sociology. 1986;92:628–656. [PubMed] [Google Scholar]
- Brent DA. Assessment and treatment of the youthful suicidal patient. Hendin: Herbert; 2001. p. 932. [DOI] [PubMed] [Google Scholar]
- Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1994a;33:1080–1086. doi: 10.1097/00004583-199410000-00003. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. Psychiatric risk factors for adolescent suicide: a case-control study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Balach L, et al. Familial risk factors for adolescent suicide: a case-control study. Acta Psychiatrica Scandinavica. 1994b;89:52–58. doi: 10.1111/j.1600-0447.1994.tb01485.x. [DOI] [PubMed] [Google Scholar]
- Brevard A, Lester D, Yang B. A comparison of suicide notes written by suicide completers and suicide attempters. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 1990;11:7–11. [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of abnormal psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Brown R, Brown S, Johnson A, Olsen B, Melver K, Sullivan M. Empirical Support for an Evolutionary Model of Self-Destructive Motivation. Suicide & Life Threatening Behavior. 2009;39:1–12. doi: 10.1521/suli.2009.39.1.1. [DOI] [PubMed] [Google Scholar]
- Brown RM, Dahlen E, Mills C, Rick J, Biblarz A. Evaluation of an evolutionary model of self-preservation and self-destruction. Suicide and Life-Threatening Behavior. 1999;29:58–71. [PubMed] [Google Scholar]
- Bullman TA, Kang HK. The risk of suicide among wounded Vietnam veterans. American Journal of Public Health. 1996;86:662–667. doi: 10.2105/ajph.86.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Ernst JM, Burleson MH, McClintock MK, Malarkey WB, Hawkley LC, et al. Lonely traits and concomitant physiological processes: the MacArthur social neuroscience studies. International Journal of Psychophysiology. 2000;35:143–154. doi: 10.1016/s0167-8760(99)00049-5. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst C, Burleson MH, Berntson GG, Nouriani B, et al. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. [Google Scholar]
- Campbell WK, Krusemark EA, Dyckman KA, Brunell AB, McDowell JE, Twenge JM, et al. A magnetoencephalography investigation of neural correlates for social exclusion and self-control. Social Neuroscience. 2006;1:124–134. doi: 10.1080/17470910601035160. [DOI] [PubMed] [Google Scholar]
- Cantor CH, Slater PJ. Marital Breakdown, Parenthood, and Suicide. Journal of Family Studies. 1995;1:91–102. [Google Scholar]
- Carrico AW, Johnson MO, Morin SF, Remien RH, Charlebois ED, Steward WT, et al. Correlates of suicidal ideation among HIV-positive persons. Aids. 2007;21:1199–1203. doi: 10.1097/QAD.0b013e3281532c96. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Chatard A, Selimbegovi L, Konan PND. Self-esteem and suicide rates in 55 nations. European Journal of Personality. 2009;23:19–32. [Google Scholar]
- Cheetham SC, Crompton MR, Czudek C, Horton RW, Katona CL, Reynolds GP. Serotonin concentrations and turnover in brains of depressed suicides. Brain Research. 1989;502:332–340. doi: 10.1016/0006-8993(89)90629-x. [DOI] [PubMed] [Google Scholar]
- Chew KS, McCleary R. The spring peak in suicides: a cross-national analysis. Social Science and Medicine. 1995;40:223–230. doi: 10.1016/0277-9536(94)e0070-9. [DOI] [PubMed] [Google Scholar]
- Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the Will to Live in Patients Nearing Death. Psychosomatics: Journal of Consultation Liaison Psychiatry. 2005;46:7–10. doi: 10.1176/appi.psy.46.1.7. [DOI] [PubMed] [Google Scholar]
- Christiansen E, Jensen BF. Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. The Australian and New Zealand Journal of Psychiatry. 2007;41:257–265. doi: 10.1080/00048670601172749. [DOI] [PubMed] [Google Scholar]
- Christodoulou C, Papadopoulos IN, Douzenis A, Kanakaris N, Leukidis C, Gournellis R, et al. Seasonality of violent suicides in the athens greater area. Suicide Life Threat Behav. 2009;39:321–331. doi: 10.1521/suli.2009.39.3.321. [DOI] [PubMed] [Google Scholar]
- Chynoweth R, Tonge JI, Armstrong J. Suicide in Brisbane--a retrospective psychosocial study. Australian and New Zealand Journal of Psychiatry. 1980;14:37–45. doi: 10.3109/00048678009159352. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Cohen DJ. Developmental. John Wiley & Sons; Oxford: 1995. Perspectives on developmental psychopathology; p. 20. [Google Scholar]
- Conner KR, Britton PC, Sworts LM, Joiner TE. Suicide attempts among individuals with opiate dependence: the critical role of belonging. Addictive behaviors. 2007;32:1395–1404. doi: 10.1016/j.addbeh.2006.09.012. [DOI] [PubMed] [Google Scholar]
- Conner KR, Duberstein PR, Conwell Y. Age-related patterns of factors associated with completed suicide in men with alcohol dependence. The American Journal on Addictions. 1999;8:312–318. doi: 10.1080/105504999305712. [DOI] [PubMed] [Google Scholar]
- Conwell Y. Suicide and terminal illness: Lessons from the HIV pandemic. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 1994;15:57–58. 64. [PubMed] [Google Scholar]
- Conwell Y. Management of suicidal behavior in the elderly. Psychiatric Clinics of North America. 1997;20:667–683. doi: 10.1016/s0193-953x(05)70336-1. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practices: a controlled study. Journal of the American Geriatrics Society. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Rotenberg M, Caine ED. Completed suicide at age 50 and over. Journal of the American Geriatric Society. 1990;38:640–644. doi: 10.1111/j.1532-5415.1990.tb01422.x. [DOI] [PubMed] [Google Scholar]
- Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. The Journal of Clinical Psychiatry. 2005;66:412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- Crossley A, Langdridge D. Perceived Sources of Happiness: A Network Analysis. Journal of Happiness Studies. 2005;6:107–135. [Google Scholar]
- Cui H, Nishiguchi N, Ivleva E, Yanagi M, Fukutake M, Nushida H, et al. Association of RGS2 gene polymorphisms with suicide and increased RGS2 immunoreactivity in the postmortem brain of suicide victims. Neuropsychopharmacology. 2008;33:1537–1544. doi: 10.1038/sj.npp.1301557. [DOI] [PubMed] [Google Scholar]
- de Catanzaro D. Reproductive status, family interactions, and suicidal ideation: Surveys of the general public and high-risk groups. Ethology & Sociobiology. 1995;16:385–394. [Google Scholar]
- Dervic K, Brent DA, Oquendo MA. Completed suicide in childhood. Psychiatric Clinics of North America. 2008;31:271–291. doi: 10.1016/j.psc.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Dewall CN, Maner JK, Rouby DA. Social exclusion and early-stage interpersonal perception: selective attention to signs of acceptance. Journal of Personality and Social Psychology. 2009;96:729–741. doi: 10.1037/a0014634. [DOI] [PubMed] [Google Scholar]
- DeWall CN, Twenge JM, Gitter SA, Baumeister RF. It’s the thought that counts: The role of hostile cognition in shaping aggressive responses to social exclusion. Journal of Personality and Social Psychology. 2009;96:45–59. doi: 10.1037/a0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley E. Prison suicide in England and Wales, 1972–87. Br J Psychiatry. 1990;156:40–45. doi: 10.1192/bjp.156.1.40. [DOI] [PubMed] [Google Scholar]
- Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology. 1996;70:1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- Duberstein P, Witte TK. A public health perspective on personality disorders and suicide. In: Kleespies PM, editor. Evaluating and Managing Behavioral Emergencies: An Evidence-Based Resource for Mental Health Practitioners. Washington, DC: American Psychological Association; 2008. [Google Scholar]
- Duberstein PR. Are closed-minded people more open to the idea of killing themselves? Suicide and Life-Threatening Behavior. 2001;31:9–14. doi: 10.1521/suli.31.1.9.21309. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Caine ED. Age differences in the personality characteristics of suicide completers: Preliminary findings from a psychological autopsy study. Psychiatry: Interpersonal and Biological Processes. 1994;57:213–224. [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Caine ED. Suicide at 50 years of age and older: perceived physical illness, family discord and financial strain. Psychological Medicine. 2004;34:137–146. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk Factors for Suicide Completion in Major Depression: A Case-Control Study of Impulsive and Aggressive Behaviors in Men. American Journal of Psychiatry. 2005;162:2116–2124. doi: 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- DuRand CJ, Burtka GJ, Federman EJ, Haycox JA, Smith JW. A quarter century of suicide in a major urban jail: implications for community psychiatry. Am J Psychiatry. 1995;152:1077–1080. doi: 10.1176/ajp.152.7.1077. [DOI] [PubMed] [Google Scholar]
- Durkheim E. Le Suicide: Etude de socologie. Paris: F. Alcan; 1897. [Google Scholar]
- Ernst C, Lalovic A, Lesage A, Seguin M, Tousignant M, Turecki G. Suicide and no axis I psychopathology. BMC Psychiatry. 2004;4:7. doi: 10.1186/1471-244X-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exeter DJ, Boyle PJ. Does young adult suicide cluster geographically in Scotland? Journal of Epidemiology & Community Health. 2007;61:731–736. doi: 10.1136/jech.2006.052365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang F, Valdimarsdóttir U, Fürst CJ, Hultman C, Fall K, Sparén P, et al. Suicide among patients with amyotrophic lateral sclerosis. Brain: a journal of neurology. 2008;131:2729–2733. doi: 10.1093/brain/awn161. [DOI] [PubMed] [Google Scholar]
- Farberow NL, MacKinnon D. A suicide prediction schedule for neuropsychiatric hospital patients. Journal of Nervous and Mental Disorders. 1974;158:408–419. doi: 10.1097/00005053-197406000-00003. [DOI] [PubMed] [Google Scholar]
- Faupel CE, Kowalski GS, Starr PD. Sociology’s one law: religion and suicide in the urban context. Journal for the Scientific Study of Religion. 1987;26:523–534. [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, et al. Time-related predictors of suicide in major affective disorder. American Journal of Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Fazel S, Cartwright J, Norman-Nott A, Hawton K. Suicide in prisoners: A systematic review of risk factors. Journal of Clinical Psychiatry. 2008;69:1721–1731. [PubMed] [Google Scholar]
- Filiberti A, Ripamonti C, Totis A, Ventafridda V, De Conno F, Contiero P, et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. Journal of Pain and Symptom Management. 2001;22:544–553. doi: 10.1016/s0885-3924(01)00295-0. [DOI] [PubMed] [Google Scholar]
- Flavin DK, Franklin JE, Frances RJ. The acquired immune deficiency syndrome (AIDS) and suicidal behavior in alcohol-dependent homosexual men. American Journal of Psychiatry. 1986;143:1440–1442. doi: 10.1176/ajp.143.11.1440. [DOI] [PubMed] [Google Scholar]
- Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bulletin of the World Health Organization. 2008;86:703–709. doi: 10.2471/BLT.07.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossey E, Shapiro CM. Seasonality in psychiatry--a review. Canadian Journal of Psychiatry. 1992;37:299–308. doi: 10.1177/070674379203700503. [DOI] [PubMed] [Google Scholar]
- Foster T. Suicide note themes and suicide prevention. International Journal of Psychiatry in Medicine. 2003;33:323–331. doi: 10.2190/T210-E2V5-A5M0-QLJU. [DOI] [PubMed] [Google Scholar]
- Fruehwald S, Frottier P, Eher R, Ritter K, Aigner M. Fifty years of prison suicide in Austria: does legislation have an impact? Suicide and Life Threatening Behavior. 2000;30:272–281. [PubMed] [Google Scholar]
- Fudalej S, Fudalej M, Kostrzewa G, Kuzniar P, Franaszczyk M, Wojnar M, et al. Angiotensin-converting enzyme polymorphism and completed suicide: an association in Caucasians and evidence for a link with a method of self-injury. Neuropsychobiology. 2009;59:151–158. doi: 10.1159/000218077. [DOI] [PubMed] [Google Scholar]
- Gibb BE, McGeary JE, Beevers CG, Miller IW. Serotonin Transporter (5-HTTLPR) Genotype, Childhood Abuse, and Suicide Attempts in Adult Psychiatric Inpatients. Suicide and Life-Threatening Behavior. 2006;36:687–693. doi: 10.1521/suli.2006.36.6.687. [DOI] [PubMed] [Google Scholar]
- Gibb SJ, Beautrais AL, Fergusson DM. Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. The Australian and New Zealand Journal of Psychiatry. 2005;39:95–100. doi: 10.1080/j.1440-1614.2005.01514.x. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Dal Grande E, Fisher LJ, Wilson D. Population attributable risk of major depression for suicidal ideation in a random and representative community sample. Journal of Affective Disorders. 2003;74:267–272. doi: 10.1016/s0165-0327(02)00017-4. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. [Peer Reviewed] Journal of Consulting and Clinical Psychology. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Sergent DS, Alaattin E, ARB, Andrew M, HFP, et al. Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: Developmental changes. Journal of Consulting and Clinical Psychology. 2009;77:281–290. doi: 10.1037/a0014732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Manic-depressive illness: Bipolar disorders and recurrent depression. 2. New York: Oxford University Press; 2007. [Google Scholar]
- Goodwin RD, Marusic A, Hoven CW. Suicide attempts in the United States: The role of physical illness. Social Science & Medicine. 2003;56:1783–1788. doi: 10.1016/s0277-9536(02)00174-0. [DOI] [PubMed] [Google Scholar]
- Gould MS, Fisher P, Parides M, Flory M, Shaffer D. Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry. 1996;53:1155–1162. doi: 10.1001/archpsyc.1996.01830120095016. [DOI] [PubMed] [Google Scholar]
- Gould MS, Shaffer D, Greenberg T. The epidemiology of youth suicide. King, Robert A; 2003. [Google Scholar]
- Gove WR, Hughes M. Reexamining the ecological fallacy: A study in which aggregate data are critical in investigating the pathological effects of living alone. Social Forces. 1980;58:1157–1177. [Google Scholar]
- Groholt B, Ekeberg O, Wichstrom L, Haldorsen T. Suicide among children and younger and older adolescents in Norway: a comparative study. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:473–481. doi: 10.1097/00004583-199805000-00008. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Ponicki WR, Mitchell PR. Suicide rates and alcohol consumption in the United States, 1970–89. Addiction. 1995;90:1063–1075. doi: 10.1046/j.1360-0443.1995.90810635.x. [DOI] [PubMed] [Google Scholar]
- Gunderson JG. Borderline Personality Disorder: A Clinical Guide. Washington, D.C: American Psychiatric Press; 2001. [Google Scholar]
- Gururaj G, Isaac MK, Subbakrishna DK, Ranjani R. Risk factors for completed suicides: a case-control study from Bangalore, India. International Journal of Injury Control and Safety Promotion. 2004;11:183–191. doi: 10.1080/156609704/233/289706. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Harriss L, Hawton K, Zahl D. Value of measuring suicidal intent in the assessment of people attending hospital following self-poisoning or self-injury. British Journal of Psychiatry. 2005;186:60–66. doi: 10.1192/bjp.186.1.60. [DOI] [PubMed] [Google Scholar]
- Harwood DM, Hawton K, Hope T, Harriss L, Jacoby R. Life problems and physical illness as risk factors for suicide in older people: a descriptive and case-control study. Psychological Medicine. 2006;36:1265–1274. doi: 10.1017/S0033291706007872. [DOI] [PubMed] [Google Scholar]
- Haste F, Charlton J, Jenkins R. Potential for suicide prevention in primary care? An analysis of factors associated with suicide. The British Journal of General Practice. 1998;48:1759–1763. [PMC free article] [PubMed] [Google Scholar]
- Haw C, Bergen H, Casey D, Hawton K. Repetition of deliberate self-harm: a study of the characteristics and subsequent deaths in patients presenting to a general hospital according to extent of repetition. Suicide and Life Threatening Behavior. 2007;37:379–396. doi: 10.1521/suli.2007.37.4.379. [DOI] [PubMed] [Google Scholar]
- Haw C, Hawton K, Casey D. Deliberate self-harm patients of no fixed abode: a study of characteristics and subsequent deaths in patients presenting to a general hospital. Social Psychiatry and Psychiatric Epidemiology. 2006;41:918–925. doi: 10.1007/s00127-006-0106-7. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. J Gerontol B Psychol Sci Soc Sci. 2008;63:S375–384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Fagg J, Simkin S. Deliberate self-poisoning and self-injury in children and adolescents under 16 years of age in Oxford, 1976–1993. British Journal of Psychiatry. 1996;169:202–208. doi: 10.1192/bjp.169.2.202. [DOI] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, Sinclair J, Harriss L. Suicide and attempted suicide in bipolar disorder: a systematic review of risk factors. Journal of Clinical Psychiatry. 2005;66:693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- Hayes LM. National study of jail suicides: seven years later. The Psychiatric Quarterly. 1989;60:7–29. doi: 10.1007/BF01064362. [DOI] [PubMed] [Google Scholar]
- Heikkinen M, Aro H, Lönnqvist J. Recent life events, social support and suicide. Acta psychiatrica Scandinavica Supplementum. 1994;377:65–72. doi: 10.1111/j.1600-0447.1994.tb05805.x. [DOI] [PubMed] [Google Scholar]
- Heikkinen ME, Lonnqvist JK. Recent life events in elderly suicide: A nationwide study in Finland. 1995. [DOI] [PubMed] [Google Scholar]
- Hem E, Loge JH, Haldorsen T, Ekeberg O. Suicide risk in cancer patients from 1960 to 1999. Journal of Clinical Oncology. 2004;22:4209–4216. doi: 10.1200/JCO.2004.02.052. [DOI] [PubMed] [Google Scholar]
- Hendin H. Psychodynamics of suicide, with particular reference to the young. [Peer Reviewed] American Journal of Psychiatry. 1991;148:1150–1158. doi: 10.1176/ajp.148.9.1150. [DOI] [PubMed] [Google Scholar]
- Herzog DB, Greenwood DN, Dorer DJ, Flores AT, Ekeblad ER, Richards A, et al. Mortality in eating disorders: A descriptive study. International Journal of Eating Disorders. 2000;28:20–26. doi: 10.1002/(sici)1098-108x(200007)28:1<20::aid-eat3>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Hoffmann H, Modestin J. Completed suicide in discharged psychiatric inpatients. Soc Psychiatry. 1987;22:93–98. doi: 10.1007/BF00584011. [DOI] [PubMed] [Google Scholar]
- Holm-Denoma JM, Witte TK, Gordon KH, Herzog DB, Franko DL, Fichter M, et al. Deaths by suicide among individuals with anorexia as arbiters between competing explanations of the anorexia-suicide link. Journal of Affective Disorders. 2008;107:231–236. doi: 10.1016/j.jad.2007.07.029. [DOI] [PubMed] [Google Scholar]
- Hoyer G, Lund E. Suicide among women related to number of children in marriage. Archives of General Psychiatry. 1993;50:134–137. doi: 10.1001/archpsyc.1993.01820140060006. [DOI] [PubMed] [Google Scholar]
- Hoyert DL, Heron MP, Murphy SL, Hsiang-Ching K. Deaths: Final Data for 2003. National Vital Statistics Reports. 2006;54:1–120. [PubMed] [Google Scholar]
- Hrdina PD, Demeter E, Vu TB, Sotonyi P, Palkovits M. 5-HT uptake sites and 5-HT2 receptors in brain of antidepressant-free suicide victims/depressives: increase in 5-HT2 sites in cortex and amygdala. Brain Research. 1993;614:37–44. doi: 10.1016/0006-8993(93)91015-k. [DOI] [PubMed] [Google Scholar]
- Hunt IM, Kapur N, Webb R, Robinson J, Burns J, Shaw J, et al. Suicide in recently discharged psychiatric patients: a case-control study. Psychol Med. 2009;39:443–449. doi: 10.1017/S0033291708003644. [DOI] [PubMed] [Google Scholar]
- Hutchinson GA, Simeon DT. Suicide in Trinidad and Tobago: associations with measures of social distress. Int J Soc Psychiatry. 1997;43:269–275. doi: 10.1177/002076409704300404. [DOI] [PubMed] [Google Scholar]
- Huth-Bocks AC, Kerr DCR, Ivey AZ, Kramer AC, King CA. Assessment of Psychiatrically Hospitalized Suicidal Adolescents: Self-Report Instruments as Predictors of Suicidal Thoughts and Behavior. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:387–395. doi: 10.1097/chi.0b013e31802b9535. [DOI] [PubMed] [Google Scholar]
- Inoue K, Tanii H, Kaiya H, Abe S, Nishimura Y, Masaki M, et al. The correlation between unemployment and suicide rates in Japan between 1978 and 2004. Leg Med (Tokyo) 2007;9:139–142. doi: 10.1016/j.legalmed.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Insel BJ, Gould MS. Impact of modeling on adolescent suicidal behavior. Psychiatric Clinics of North America. 2008;31:293–316. doi: 10.1016/j.psc.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Jobes DA. Managing suicidal risk: A collaborative approach. New York, NY, US: Guilford Press; 2006. p. 222. [Google Scholar]
- Joiner T. Why people die by suicide. Cambridge, MA, US: Harvard University Press; 2005. [Google Scholar]
- Joiner T, Pettit JW, Walker RL, Voelz ZR, Cruz J, Rudd MD, et al. Perceived burdensomeness and suicidality: Two studies on the suicide notes of those attempting and those completing suicide. Journal of Social & Clinical Psychology. 2002;21:531–545. [Google Scholar]
- Joiner TE, Jr, Hollar D, Van Orden K. On Buckeyes, Gators, Super Bowl Sunday, and the Miracle on Ice: “Pulling together” is associated with lower suicide rates. Journal of Social & Clinical Psychology. 2006;25:179–195. [Google Scholar]
- Joiner TE, Jr, Rudd MD, Rajab MH. The Modified Scale for Suicidal Ideation: Factors of suicidality and their relation to clinical and diagnostic variables. Journal of abnormal psychology. 1997;106:260–265. doi: 10.1037//0021-843x.106.2.260. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Walker RL, Rudd MD, Jobes DA. Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice. 1999;30:447–453. [Google Scholar]
- Joiner TE, Lewinsohn PM, Seeley JR. The core of loneliness: lack of pleasurable engagement--more so than painful disconnection--predicts social impairment, depression onset, and recovery from depressive disorders among adolescents. Journal of Personality Assessment. 2002;79:472–491. doi: 10.1207/S15327752JPA7903_05. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Van Orden KA. The Interpersonal Psychological Theory of Suicidal Behavior Indicates Specific and Crucial Psychotherapeutic Targets. International Journal of Cognitive Therapy. 2008;1:80–89. [Google Scholar]
- Joiner TE, Van Orden KA, Witte TK, Rudd MD. The Interpersonal Theory of Suicide: Guidance for Working with Suicidal Clients. Washington, D.C: American Psychological Association; 2009. [Google Scholar]
- Joiner TE, Van Orden KA, Witte TK, Selby EA, Ribeiro J, Lewis R. Main Predictions of the Interpersonal-Psychological Theory of Suicidal Behavior: Empirical Tests in Two Samples of Young Adults. Journal of Abnormal Psychology. doi: 10.1037/a0016500. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokinen J, Carlborg A, Martensson B, Forslund K, Nordstrom AL, Nordstrom P. DST non-suppression predicts suicide after attempted suicide. Psychiatry Research. 2007;150:297–303. doi: 10.1016/j.psychres.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: A prospective population-based study. Journal of Epidemiology & Community Health. 2007;61:619–624. doi: 10.1136/jech.2006.054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: a population-based study. American Journal of Orthopsychiatry. 2007;77:56–60. doi: 10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- Kariminia A, Butler TG, Corben SP, Levy MH, Grant L, Kaldor JM, et al. Extreme cause-specific mortality in a cohort of adult prisoners--1988 to 2002: a data-linkage study. International Journal of Epidemiology. 2007;36:310–316. doi: 10.1093/ije/dyl225. [DOI] [PubMed] [Google Scholar]
- Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DL, Herzog DB. Predictors of mortality in eating disorders. Archives of General Psychiatry. 2003;60:179–183. doi: 10.1001/archpsyc.60.2.179. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kim CD, Seguin M, Therrien N, Riopel G, Chawky N, Lesage AD, et al. Familial aggregation of suicidal behavior: a family study of male suicide completers from the general population. American Journal of Psychiatry. 2005;162:1017–1019. doi: 10.1176/appi.ajp.162.5.1017. [DOI] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Life satisfaction and suicide: a 20-year follow-up study. The American journal of psychiatry. 2001;158:433–439. doi: 10.1176/appi.ajp.158.3.433. [DOI] [PubMed] [Google Scholar]
- Kotila L, Lonnqvist J. Adolescents who make suicide attempts repeatedly. Acta Psychiatrica Scandinavica. 1987;76:386–393. doi: 10.1111/j.1600-0447.1987.tb05623.x. [DOI] [PubMed] [Google Scholar]
- Kposowa AJ. Marital status and suicide in the National Longitudinal Mortality Study. Journal of epidemiology and community health. 2000;54:254–261. doi: 10.1136/jech.54.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreitman N, Platt S. Suicide, unemployment, and domestic gas detoxification in Britain. Journal of Epidemiology & Community Health. 1984;38:1–6. doi: 10.1136/jech.38.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kullgren G. Factors associated with completed suicide in borderline personality disorder. The Journal of Nervous and Mental Disease. 1988;176:40–44. doi: 10.1097/00005053-198801000-00005. [DOI] [PubMed] [Google Scholar]
- Leighton AH, Hughes CC. Notes on Eskimo Patterns of Suicide. Southwestern Journal of Anthropology. 1955;11:327–338. [Google Scholar]
- Lester D, Yang B. Unemployment and suicidal behaviour. J Epidemiol Community Health. 2003;57:558–559. doi: 10.1136/jech.57.8.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin K. Field Theory in Social Science. New York: Harper & Brothers Publishers; 1951. [Google Scholar]
- Li XY, Phillips MR, Zhang YP, Xu D, Yang GH. Risk factors for suicide in China’s youth: a case-control study. Psychological Medicine. 2008;38:397–406. doi: 10.1017/S0033291707001407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limosin F, Loze JY, Philippe A, Casadebaig F, Rouillon F. Ten-year prospective follow-up study of the mortality by suicide in schizophrenic patients. Schizophrenia Research. 2007;94:23–28. doi: 10.1016/j.schres.2007.04.031. [DOI] [PubMed] [Google Scholar]
- Lindeman S, Laara E, Hakko H, Lonnqvist J. A systematic review on gender-specific suicide mortality in medical doctors. British Journal of Psychiatry. 1996;168:274–279. doi: 10.1192/bjp.168.3.274. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- Linehan MM, Comtois KA, Murray A. The University of Washington Risk Assessment Protocol (UWRAP) University of Washington; 2000. [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-Year Randomized Controlled Trial and Follow-up of Dialectical Behavior Therapy vs Therapy by Experts for Suicidal Behaviors and Borderline Personality Disorder. Archives of General Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing youself: the Reasons for Living Inventory. [Article] Journal of Consulting and Clinical Psychology. 1983;51:276–286. doi: 10.1037//0022-006x.51.2.276. [DOI] [PubMed] [Google Scholar]
- Llorente MD, Burke M, Gregory GR, Bosworth HB, Grambow SC, Horner RD, et al. Prostate cancer: a significant risk factor for late-life suicide. American Journal of Geriatric Psychiatry. 2005;13:195–201. doi: 10.1176/appi.ajgp.13.3.195. [DOI] [PubMed] [Google Scholar]
- Lopez de Lara C, Dumais A, Rouleau G, Lesage A, Dumont M, Chawky N, et al. STin2 variant and family history of suicide as significant predictors of suicide completion in major depression. Biological Psychiatry. 2006;59:114–120. doi: 10.1016/j.biopsych.2005.06.021. [DOI] [PubMed] [Google Scholar]
- Maner JK, DeWall CN, Baumeister RF, Schaller M. Does social exclusion motivate interpersonal reconnection? Resolving the “porcupine problem”. Journal of Personality and Social Psychology. 2007;92:42–55. doi: 10.1037/0022-3514.92.1.42. [DOI] [PubMed] [Google Scholar]
- Mann JJ. Neurobiology of Suicidal Behaviour. Nature Reviews Neuroscience. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Huang YY, Underwood MD, Kassir SA, Oppenheim S, Kelly TM, et al. A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Archives of General Psychiatry. 2000;57:729–738. doi: 10.1001/archpsyc.57.8.729. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Stanley M, McBride PA, McEwen BS. Increased serotonin2 and beta-adrenergic receptor binding in the frontal cortices of suicide victims. Archives of General Psychiatry. 1986;43:954–959. doi: 10.1001/archpsyc.1986.01800100048007. [DOI] [PubMed] [Google Scholar]
- Maris RW. Social forces in urban suicide. Homewood, IL: Dorsey Press; 1969. [Google Scholar]
- Maris RW. A developmental perspective of suicide. Leenaars, Antoon A; 1991. [Google Scholar]
- Maris RW. Suicide. Lancet. 2002;360:319–326. doi: 10.1016/S0140-6736(02)09556-9. [DOI] [PubMed] [Google Scholar]
- Maris RW, Berman AL, Maltsberger JT. Summary and conclusions: What have we learned about suicide assessment and prediction? In: Maris RW, Berman AL, Maltsberger JT, Yufit RI, editors. Assessment and Prediction of Suicide. New York: Guilford Press; 1992. pp. 640–672. [Google Scholar]
- Maris RW, Berman AL, Silverman MM. Comprehensive textbook of suicidology. New York: Guilford Press; 2000. [Google Scholar]
- Marshall JR, Burnett W, Brasure J. On precipitating factors: cancer as a cause of suicide. Suicide Life Threat Behav. 1983;13:15–27. doi: 10.1111/j.1943-278x.1983.tb00002.x. [DOI] [PubMed] [Google Scholar]
- Maser JD, Akiskal HS, Schettler P, Scheftner W, Mueller T, Endicott J, et al. Can temperament identify affectively ill patients who engage in lethal or near-lethal suicidal behavior? A 14-year prospective study. Suicide and Life-Threatening Behavior. 2002;32:10–32. doi: 10.1521/suli.32.1.10.22183. [DOI] [PubMed] [Google Scholar]
- McGirr A, Paris J, Lesage A, Renaud J, Turecki G. Risk factors for suicide completion in borderline personality disorder: a case-control study of cluster B comorbidity and impulsive aggression. Journal of Clinical Psychiatry. 2007;68:721–729. doi: 10.4088/jcp.v68n0509. [DOI] [PubMed] [Google Scholar]
- McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychological Medicine. 2008;38:407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- McGirr A, Tousignant M, Routhier D, Pouliot L, Chawky N, Margolese HC, et al. Risk factors for completed suicide in schizophrenia and other chronic psychotic disorders: a case-control study. Schizophrenia Research. 2006;84:132–143. doi: 10.1016/j.schres.2006.02.025. [DOI] [PubMed] [Google Scholar]
- McKenzie N, Landau S, Kapur N, Meehan J, Robinson J, Bickley H, et al. Clustering of suicides among people with mental illness. British Journal of Psychiatry. 2005;187:476–480. doi: 10.1192/bjp.187.5.476. [DOI] [PubMed] [Google Scholar]
- McMillan D, Gilbody S, Beresford E, Neilly L. Can we predict suicide and non-fatal self-harm with the Beck Hopelessness Scale? A meta-analysis. Psychological Medicine. 2007;37:769–778. doi: 10.1017/S0033291706009664. [DOI] [PubMed] [Google Scholar]
- Menninger KA. Man Against Himself. New York: Harcourt, Brace and Company; 1938. [Google Scholar]
- Miller M. Geriatric suicide: The Arizona study. The Gerontologist. 1978;18:488–495. doi: 10.1093/geront/18.5_part_1.488. [DOI] [PubMed] [Google Scholar]
- Miller M, Mogun H, Azrael D, Hempstead K, Solomon DH. Cancer and the risk of suicide in older Americans. Journal of Clinical Oncology. 2008;26:4720–4724. doi: 10.1200/JCO.2007.14.3990. [DOI] [PubMed] [Google Scholar]
- Moscicki EK. Epidemiology of completed and attempted suicide: toward a framework for prevention. Clinical Neuroscience Research. 2001;1:310–323. [Google Scholar]
- Moskos M, Olson L, Halbern S, Keller T, Gray D. Utah Youth Suicide Study: Psychological autopsy. Suicide and Life-Threatening Behavior. 2005;35:536–546. doi: 10.1521/suli.2005.35.5.536. [DOI] [PubMed] [Google Scholar]
- Motto JA, Bostrom A. Empirical indicators of near-term suicide risk. Crisis. 1990;11:52–59. [PubMed] [Google Scholar]
- Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatric services. 2001;52:828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Engel SG, Wadeson A, Crosby RD, Wonderlich SA, Simonich H, et al. Emotional states preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. [Article] Behaviour Research and Therapy. 2009;47:83–87. doi: 10.1016/j.brat.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy GE, Wetzel RD, Robins E, McEvoy L. Multiple risk factors predict suicide in alcoholism. Archives of General Psychiatry. 1992;49:459–463. doi: 10.1001/archpsyc.1992.01820060039006. [DOI] [PubMed] [Google Scholar]
- Nademin E, Jobes DA, Pflanz SE, Jacoby AM, Ghahramanlou-Holloway M, Campise R, et al. An Investigation of Interpersonal-Psychological Variables in Air Force Suicides: A Controlled-Comparison Study. Archives of Suicide Research. 2008;12:309–326. doi: 10.1080/13811110802324847. [DOI] [PubMed] [Google Scholar]
- Nickel C, Simek M, Moleda A, Muehlbacher M, Buschmann W, Fartacek R, et al. Suicide attempts versus suicidal ideation in bulimic female adolescents. Pediatrics international: official journal of the Japan Pediatric Society. 2006;48:374–381. doi: 10.1111/j.1442-200X.2006.02224.x. [DOI] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2009 doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE. Examination of affective, cognitive, and behavioral factors and suicide-related outcomes in children and young adolescents. Journal of Clinical Child and Adolescent Psychology. 2002;31:48–58. doi: 10.1207/S15374424JCCP3101_07. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Nordstrom P, Asberg M, Aberg-Wistedt A, Nordin C. Attempted suicide predicts suicide risk in mood disorders. Acta Psychiatrica Scandinavica. 1995;92:345–350. doi: 10.1111/j.1600-0447.1995.tb09595.x. [DOI] [PubMed] [Google Scholar]
- O’Mahony S, Goulet J, Kornblith A, Abbatiello G, Clarke B, Kless-Siegel S, et al. Desire for Hastened Death, Cancer Pain and Depression: Report of a Longitudinal Observational Study. Journal of Pain and Symptom Management. 2005;29:446–457. doi: 10.1016/j.jpainsymman.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Obafunwa JO, Busuttil A. Clinical contact preceding suicide. Postgraduate Medical Journal. 1994;70:428–432. doi: 10.1136/pgmj.70.824.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohman A, Mineka S. Fears, phobias, and preparedness: Toward an evolved module of fear and fear learning. Psychological Review. 2001;108:483–522. doi: 10.1037/0033-295x.108.3.483. [DOI] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M, King R, Cohen D, Stein D. Thresholds and tolerance of physical pain in suicidal and nonsuicidal adolescents. Journal of Consulting and Clinical Psychology. 1997;65:646–652. doi: 10.1037//0022-006x.65.4.646. [DOI] [PubMed] [Google Scholar]
- Orbach I, Palgi Y, Stein D, HarEven D, LotemPeleg M, Asherov J, et al. Tolerance for physical pain in suicidal subjects. Death studies. 1996;20:327–341. doi: 10.1080/07481189608252786. [DOI] [PubMed] [Google Scholar]
- Orbach I, Stein D, Palgi Y, Asherov J, HarEven D, Elizur A. Perception of physical pain in accident and suicide attempt patients: Self-preservation vs self-destruction. Journal of Psychiatric Research. 1996;30:307–320. doi: 10.1016/0022-3956(96)00008-8. [DOI] [PubMed] [Google Scholar]
- Owens C, Booth N, Briscoe M, Lawrence C, Lloyd K. Suicide outside the care of mental health services: a case-controlled psychological autopsy study. Crisis. 2003;24:113–121. doi: 10.1027//0227-5910.24.3.113. [DOI] [PubMed] [Google Scholar]
- Palmer BA, Pankratz S, Bostwick JM. The lifetime risk of suicide in schizophrenia: a re-examination. Archives of General Psychiatry. 2005;62:247–253. doi: 10.1001/archpsyc.62.3.247. [DOI] [PubMed] [Google Scholar]
- Pandey GN, Dwivedi Y, Rizavi HS, Ren X, Pandey SC, Pesold C, et al. Higher expression of serotonin 5-HT(2A) receptors in the postmortem brains of teenage suicide victims. American Journal of Psychiatry. 2002;159:419–429. doi: 10.1176/appi.ajp.159.3.419. [DOI] [PubMed] [Google Scholar]
- Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. 2002;360:1728–1736. doi: 10.1016/S0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- Platt S. Suicide and unemployment in Italy. Social Science & Medicine. 1992;34:1191–1201. doi: 10.1016/0277-9536(92)90312-e. [DOI] [PubMed] [Google Scholar]
- Plunkett A, O’Toole B, Swanston H, Oates RK, Shrimpton S, Parkinson P. Suicide risk following child sexual abuse. Ambulatory Pediatrics. 2001;1:262–266. doi: 10.1367/1539-4409(2001)001<0262:srfcsa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Plutchik R, Van Praag HM, Conte HR. Correlates of suicide and violence risk: III. A two-stage model of countervailing forces. Psychiatry Research. 1989;28:215–225. doi: 10.1016/0165-1781(89)90048-6. [DOI] [PubMed] [Google Scholar]
- Pokorny AD. Prediction of suicide in psychiatric patients. Report of a prospective study. [Research Support, U.S. Gov’t, Non-P.H.S. Research Support, U.S. Gov’t, P.H.S.] Archives of General Psychiatry. 1983;40:249–257. doi: 10.1001/archpsyc.1983.01790030019002. [DOI] [PubMed] [Google Scholar]
- Pompili M, Lester D, Grispini A, Innamorati M, Calandro F, Iliceto P, et al. Completed suicide in schizophrenia: evidence from a case-control study. Psychiatry Research. 2009;167:251–257. doi: 10.1016/j.psychres.2008.03.018. [DOI] [PubMed] [Google Scholar]
- Preti A, Miotto P. Suicide and unemployment in Italy, 1982–1994. J Epidemiol Community Health. 1999;53:694–701. doi: 10.1136/jech.53.11.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti A, Miotto P. Diurnal variations in suicide by age and gender in Italy. Journal of Affective Disorders. 2001;65:253–261. doi: 10.1016/s0165-0327(00)00232-9. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ. Introduction to the special section on suicide and nonsuicidal self-injury: A review of unique challenges and important directions for self-injury science. Journal of Consulting and Clinical Psychology. 2008;76:1–8. doi: 10.1037/0022-006X.76.1.1. [DOI] [PubMed] [Google Scholar]
- Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002;360:1126–1130. doi: 10.1016/S0140-6736(02)11197-4. [DOI] [PubMed] [Google Scholar]
- Qin P, Nordentoft M. Suicide Risk in Relation to Psychiatric Hospitalization. Archives of General Psychiatry. 2005;62:427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- Quan H, Arboleda-Florez J. Elderly suicide in Alberta: difference by gender. Canadian Journal of Psychiatry. 1999;44:762–768. doi: 10.1177/070674379904400801. [DOI] [PubMed] [Google Scholar]
- Rasic DT, Belik SL, Bolton JM, Chochinov HM, Sareen J. Cancer, mental disorders, suicidal ideation and attempts in a large community sample. Psycho-Oncology. 2008;17:660–667. doi: 10.1002/pon.1292. [DOI] [PubMed] [Google Scholar]
- Renaud J, Berlim MT, McGirr A, Tousignant M, Turecki G. Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: A case-control study. Journal of Affective Disorders. 2008;105:221–228. doi: 10.1016/j.jad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Renaud J, Brent DA, Birmaher B, Chiappetta L, Bridge J. Suicide in adolescents with disruptive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:846–851. doi: 10.1097/00004583-199907000-00014. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. A school-based procedure for the identification of adolescents as risk for suicidal behaviors. Family and Community Health. 1991;14:64–75. [Google Scholar]
- Richman J. Family therapy for suicidal people. New York: Springer; 1986. [Google Scholar]
- Rizvi SL, Linehan MM. The treatment of maladaptive shame in borderline personality disorder: A pilot study of “opposite action”. Cognitive and Behavioral Practice. 2005;12:437–447. [Google Scholar]
- Rocchi MB, Perlini C. Is the time of suicide a random choice? A new statistical perspective. Crisis. 2002;23:161–166. doi: 10.1027//0227-5910.23.4.161. [DOI] [PubMed] [Google Scholar]
- Rogers JR. Theoretical grounding: The “missing link” in suicide research. Journal of Counseling & Development. 2001;79:16–25. [Google Scholar]
- Rosel P, Arranz B, San L, Vallejo J, Crespo JM, Urretavizcaya M, et al. Altered 5-HT(2A) binding sites and second messenger inositol trisphosphate (IP(3)) levels in hippocampus but not in frontal cortex from depressed suicide victims. Psychiatry Research. 2000;99:173–181. doi: 10.1016/s0925-4927(00)00076-7. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M, Richman J. Suicide: The role of hostility and death wishes from the family and significant others. American Journal of Psychiatry. 1970;126:1652–1655. doi: 10.1176/ajp.126.11.1652. [DOI] [PubMed] [Google Scholar]
- Rosenthal PA, Rosenthal S. Suicidal behavior by preschool children. American Journal of Psychiatry. 1984;141:520–525. doi: 10.1176/ajp.141.4.520. [DOI] [PubMed] [Google Scholar]
- Roy A, Segal NL. Suicidal behavior in twins: a replication. Journal of Affective Disorders. 2001;66:71–74. doi: 10.1016/s0165-0327(00)00275-5. [DOI] [PubMed] [Google Scholar]
- Roy A, Segal NL, Centerwall BS, Robinette CD. Suicide in twins. Archives of General Psychiatry. 1991;48:29–32. doi: 10.1001/archpsyc.1991.01810250031003. [DOI] [PubMed] [Google Scholar]
- Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides--A case-control study. Psychological Medicine. 2001;31:1193–1202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Joiner T, Rajab MH. Relationships among suicide ideators, attempters, and multiple attempters in young-adult sample. Journal of Abnormal Psychology. 1996;105:541–550. doi: 10.1037//0021-843x.105.4.541. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Joiner T, Rajab MH. Treatment manuals for practitioners. New York, NY, US: Guilford Press; 2001. Treating suicidal behavior: An effective, time-limited approach; p. 274. [Google Scholar]
- Runeson B, Asberg M. Family history of suicide among suicide victims. American Journal of Psychiatry. 2003;160:1525–1526. doi: 10.1176/appi.ajp.160.8.1525. [DOI] [PubMed] [Google Scholar]
- Russell DW. UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. Journal of Personality Assessment. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Sabbath JC. The suicidal adolescent: The expendable child. Journal of the American Academy of Child Psychiatry. 1969;8:272–285. doi: 10.1016/s0002-7138(09)61906-3. [DOI] [PubMed] [Google Scholar]
- Sainsbury P. Suicide in London. London: Chapman & Hall; 1955. [Google Scholar]
- Salib E. Effect of 11 September 2001 on suicide and homicide in England and Wales. Br J Psychiatry. 2003;183:207–212. doi: 10.1192/bjp.183.3.207. [DOI] [PubMed] [Google Scholar]
- Samaraweera S, Sumathipala A, Siribaddana S, Sivayogan S, Bhugra D. Completed suicide among Sinhalese in Sri Lanka: A psychological autopsy study. Suicide and Life-Threatening Behavior. 2008;38:221–228. doi: 10.1521/suli.2008.38.2.221. [DOI] [PubMed] [Google Scholar]
- Schony W, Grausgruber A. Epidemiological data on suicide in upper australia. Crisis. 1987;8:49–52. [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry. 1996;53:339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- Shafii M, Carrigan S, Whittinghill JR, Derrick A. Psychological autopsy of completed suicide in children and adolescents. American Journal of Psychiatry. 1985;142:1061–1064. doi: 10.1176/ajp.142.9.1061. [DOI] [PubMed] [Google Scholar]
- Shea SC. The practical art of suicide assessment: A guide for mental health professionals and substance abuse counselors. Hoboken, NJ, US: John Wiley & Sons Inc; 1999. p. 254. [Google Scholar]
- Shneidman ES. Definition of Suicide. New York: Wiley; 1985. [Google Scholar]
- Shneidman ES. A psychological approach to suicide. VandenBos, Gary R; 1987. [Google Scholar]
- Shneidman ES. Perspectives on suicidology: Further reflections on suicide and psychache. Suicide and Life-Threatening Behavior. 1998;28:245–250. [PubMed] [Google Scholar]
- Shneidman ES. Comprehending suicide: Landmarks in 20th-century suicidology. Washington, DC, US: American Psychological Association; 2001. p. 215. [Google Scholar]
- Sholders MA. Suicide in Indianapolis. Sociological Focus. 1981;14:221–231. [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the Tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors: Part 1: Background, rationale, and methodology. Suicide and Life-Threatening Behavior. 2007a;37:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the Tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors: Part II: Suicide-related ideations, communications and behaviors. Suicide and Life-Threatening Behavior. 2007b;37:264–277. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- Simon RI. Clinically based risk management of the suicidal patient: Avoiding malpractice litigation. Simon, Robert I; 2006. [Google Scholar]
- Smith JM, Alloy LB, Abramson LY. Cognitive vulnerability to depression, rumination, hopelessness, and suicidal ideation: multiple pathways to self-injurious thinking. Suicide & Life Threatening Behavior. 2006;36:443–454. doi: 10.1521/suli.2006.36.4.443. [DOI] [PubMed] [Google Scholar]
- Solomon RL, Corbit JD. An opponent-process theory of motivation: I. Temporal dynamics of affect. Psychological Review. 1974;81:119–145. doi: 10.1037/h0036128. [DOI] [PubMed] [Google Scholar]
- Sourander A, Klomek AB, Niemela S, Haavisto A, Gyllenberg D, Helenius H, et al. Childhood Predictors of Completed and Severe Suicide Attempts: Findings From the Finnish 1981 Birth Cohort Study. Archives of General Psychiatry. 2009;66:398–406. doi: 10.1001/archgenpsychiatry.2009.21. [DOI] [PubMed] [Google Scholar]
- Stack S. New Micro-Level Data on the Impact of Divorce on Suicide, 1959–1980: A Test of Two Theories. Journal of Marriage and Family. 1990;52:119–127. [Google Scholar]
- Stack S. Suicide: a 15-year review of the sociological literature. Part I: cultural and economic factors. Suicide & life threatening behavior. 2000;30:145–162. [PubMed] [Google Scholar]
- Stenager EN, Stenager E. Suicide and patients with neurologic diseases: Methodologic problems. Archives of Neurology. 1992;49:1296–1303. doi: 10.1001/archneur.1992.00530360098025. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Haukka J, Lonnqvist J. Substance use and male gender as risk factors for deaths and suicide--a 5-year follow-up study after deliberate self-harm. Social Psychiatry and Psychiatric Epidemiology. 2004;39:720–724. doi: 10.1007/s00127-004-0796-7. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Ostamo A, Lonnqvist J. Level of suicidal intent predicts overall mortality and suicide after attempted suicide: a 12-year follow-up study. BioMed Central Psychiatry. 2004;4:11. doi: 10.1186/1471-244X-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. American Journal of Psychiatry. 2004;161:562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- Thomas HV, Crawford M, Meltzer H, Lewis G. Thinking life is not worth living - A population survey of Great Britain. [Article] Social Psychiatry and Psychiatric Epidemiology. 2002;37:351–356. doi: 10.1007/s00127-002-0556-5. [DOI] [PubMed] [Google Scholar]
- Thoresen S, Mehlum L, Roysamb E, Tonnessen A. Risk factors for completed suicide in veterans of peacekeeping: repatriation, negative life events, and marital status. Archives of Suicide Research. 2006;10:353–363. doi: 10.1080/13811110600791106. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Elofsson S, Stefansson CG, Waern M, Runeson B. Predictors of suicide in a community-based cohort of individuals with severe mental disorder. Social Psychiatry and Psychiatric Epidemiology. 2005;40:595–600. doi: 10.1007/s00127-005-0941-y. [DOI] [PubMed] [Google Scholar]
- Timonen M, Viilo K, Vaisanen E, Rasanen P, Hakko H, Sarkioja T. Burden of illness and suicide in elderly people. Physical disease and depression are prevalent in elderly Finnish suicide victims. British Medical Journal. 2002;325:441. doi: 10.1136/bmj.325.7361.441/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trout DL. The role of social isolation in suicide. Suicide and Life-Threatening Behavior. 1980;10:10–23. doi: 10.1111/j.1943-278x.1980.tb00693.x. [DOI] [PubMed] [Google Scholar]
- Tsai SY, Kuo CJ, Chen CC, Lee HC. Risk factors for completed suicide in bipolar disorder. Journal of Clinical Psychiatry. 2002;63:469–476. doi: 10.4088/jcp.v63n0602. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, et al. Risk factors for late-life suicide: A prospective community-based study. American Journal of Geriatric Psychiatry Special Issue: Suicidal behaviors in older adults. 2002;10:398–406. [PubMed] [Google Scholar]
- Twenge JM, Baumeister RF, DeWall CN, Ciarocco NJ, Bartels JM. Social exclusion decreases prosocial behavior. Journal of Personality and Social Psychology. 2007;92:56–66. doi: 10.1037/0022-3514.92.1.56. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Baumeister RF, Tice DM, Stucke TS. If you can’t join them, beat them: effects of social exclusion on aggressive behavior. Journal of Personality and Social Psychology. 2001;81:1058–1069. doi: 10.1037//0022-3514.81.6.1058. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Catanese KR, Baumeister RF. Social exclusion causes self-defeating behavior. Journal of Personality and Social Psychology. 2002;83:606–615. doi: 10.1037//0022-3514.83.3.606. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Catanese KR, Baumeister RF. Social exclusion and the deconstructed state: time perception, meaninglessness, lethargy, lack of emotion, and self-awareness. Journal of Personality and Social Psychology. 2003;85:409–423. doi: 10.1037/0022-3514.85.3.409. [DOI] [PubMed] [Google Scholar]
- Twomey HB, Kaslow NJ, Croft S. Childhood maltreatment, object relations, and suicidal behavior in women. Psychoanalytic Psychology. 2000;17:313–335. [Google Scholar]
- Van Orden KA, Lynam ME, Hollar D, Joiner TE., Jr Perceived Burdensomeness as an Indicator of Suicidal Symptoms. Cognitive Therapy and Research. 2006;30:457–467. [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE., Jr Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- van Pragg HM. Suicide and aggression: Are they biologically two sides of the same coin. In: Lester D, editor. Suicide Prevention: Resources for the New Millennium. Philadelphia: Brunner-Routledge; 2001. pp. 45–64. [Google Scholar]
- Verona E, Sachs-Ericsson N, Joiner TE. Suicide Attempts Associated With Externalizing Psychopathology in an Epidemiological Sample. American Journal of Psychiatry. 2004;161:444–451. doi: 10.1176/appi.ajp.161.3.444. [DOI] [PubMed] [Google Scholar]
- Waern M, Rubenowitz E, Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. 2003;49:328–334. doi: 10.1159/000071715. [DOI] [PubMed] [Google Scholar]
- Wagner BM. Family risk factors for child and adolescent suicidal behavior. Psychological Bulletin. 1997;121:246–298. doi: 10.1037/0033-2909.121.2.246. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Rouleau M, Joiner T. Cognitive factors related to suicidal ideation and resolution in psychiatrically hospitalized children and adolescents. Am J Psychiatry. 2000;157:2017–2021. doi: 10.1176/appi.ajp.157.12.2017. [DOI] [PubMed] [Google Scholar]
- Walker J, Waters RA, Murray G, Swanson H, Hibberd CJ, Rush RW, et al. Better off dead: suicidal thoughts in cancer patients. J Clin Oncol. 2008;26:4725–4730. doi: 10.1200/JCO.2007.11.8844. [DOI] [PubMed] [Google Scholar]
- Wen-Hung K, Gallo JJ, Eaton WW. Hopelessness, depression, substance disorder, and suicidality: A 13-year community-based study. Social Psychiatry and Psychiatric Epidemiology. 2004;39:497–501. doi: 10.1007/s00127-004-0775-z. [DOI] [PubMed] [Google Scholar]
- Whitlock F. Suicide and physical illness. In: Roy A, editor. Suicide. Baltimore: Williams and Wilkins; 1986. pp. 151–170. [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: An empirical review of cohort studies. Drug and Alcohol Dependence Special Issue: Drug Abuse and Suicidal Behavior. 2004;76:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Williams JMG. Suicide & Attempted Suicide: Understanding the Cry of Pain. 2001. [Google Scholar]
- Williams JMG, Van der Does AJW, Barnhofer T, Crane C, Segal ZS. Cognitive reactivity, suicidal ideation and future fluency: Preliminary investigation of a differential activation theory of hopelessness/suicidality. Cognitive Therapy and Research. 2008;32:83–104. [Google Scholar]
- Witte TK, Joiner TE, Brown GK, Beck AT, Beckman A, Duberstein P, et al. Factors of suicide ideation and their relation to clinical and other indicators in older adults. Journal of Affective Disorders. 2006;94:165–172. doi: 10.1016/j.jad.2006.04.005. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Primary prevention of mental, neurological and psychosocial disorders. 1998. [Google Scholar]
- World Health Organization. Suicide rates (per 100,000), by country, year, and gender. 2003 Retrieved February 14, 2006, from http://www.who.int/mental_health/prevention/suicide/suiciderates/en/
- World Health Organization. Suicide Statistics: Introduction. 2008 Retrieved January 2, 2008, from http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/print.html.
- Woznica JG, Shapiro JR. An analysis of adolescent suicide attempts: The expendable child. Journal of Pediatric Psychology. 1990;15:789–796. doi: 10.1093/jpepsy/15.6.789. [DOI] [PubMed] [Google Scholar]
- Wyder M, Ward P, De Leo D. Separation as a suicide risk factor. Journal of Affective Disorders. 2009;116:208–213. doi: 10.1016/j.jad.2008.11.007. [DOI] [PubMed] [Google Scholar]
- Yim PH, Yip PS, Li RH, Dunn EL, Yeung WS, Miao YK. Suicide after discharge from psychiatric inpatient care: a case-control study in Hong Kong. The Australian and New Zealand Journal of Psychiatry. 2004;38:65–72. doi: 10.1177/000486740403800103. [DOI] [PubMed] [Google Scholar]
- Yip PS, Chao A, Chiu CW. Seasonal variation in suicides: diminished or vanished. Experience from England and Wales, 1982–1996. British Journal of Psychiatry. 2000;177:366–369. doi: 10.1192/bjp.177.4.366. [DOI] [PubMed] [Google Scholar]
- Zill P, Buttner A, Eisenmenger W, Moller HJ, Bondy B, Ackenheil M. Single nucleotide polymorphism and haplotype analysis of a novel tryptophan hydroxylase isoform (TPH2) gene in suicide victims. Biological Psychiatry. 2004;56:581–586. doi: 10.1016/j.biopsych.2004.07.015. [DOI] [PubMed] [Google Scholar]
- Zonda T. One-hundred cases of suicide in Budapest: a case-controlled psychological autopsy study. Crisis. 2006;27:125–129. doi: 10.1027/0227-5910.27.3.125. [DOI] [PubMed] [Google Scholar]
- Zouk H, Tousignant M, Seguin M, Lesage A, Turecki G. Characterization of impulsivity in suicide completers: clinical, behavioral and psychosocial dimensions. Journal of Affective Disorders. 2006;92:195–204. doi: 10.1016/j.jad.2006.01.016. [DOI] [PubMed] [Google Scholar]