Abstract
In this paper, potential underlying mechanisms for massage therapy effects on preterm infant weight gain are reviewed. Path analyses are presented suggesting that: 1) increased vagal activity was associated with 2) increased gastric motility, which, in turn, was related to 3) greater weight gain; and 4) increased IGF-1 was related to greater weight gain. The change in vagal activity during the massage explained 49% of the variance in the change in gastric activity. And, the change in vagal activity during the massage explained 62% of the variance in the change in insulin. That the change in gastric activity was not related to the change in insulin suggests two parallel pathways via which massage therapy leads to increased weight gain: 1) insulin release via the celiac branch of the vagus; and 2) increased gastric activity via the gastric branch of the vagus.
Preterm Infant Massage Therapy Studies
Randomized, controlled studies have consistently documented greater weight gain in preterm neonates receiving massage therapy (also known as tactile/kinesthetic stimulation) (See Field, Hernandez-Reif, Diego, Feijo, Vera, & Gil, K. 2004 for a review). Preterm neonates receiving 5 to 10 days of massage therapy exhibited a 28% to 47% greater increase in weight gain during the study period, and they were hospitalized for 3 to 6 days less (than control neonates receiving standard care) at a substantial reduction in hospital costs (Diego, Field, & Hernandez-Reif, 2005; Field, Schanberg, Scafidi, Bauer, Vega-Lahr, Garcia, Nystrom, & Kuhn ,1986; Goldstein-Ferber, 2004; Scafidi, Field, Schanberg, Bauer, Tucci et al., 1990). In addition, massaged preterm neonates showed more mature motor behavior, more stable state organization, and had fewer abnormal reflexes on the Brazelton Neonatal Behavioral Assessment Scale (Field, Diego, Hernandez-Reif, Deeds, Figuereido, Ascencio, 2006).
Calorie Consumption and Sleep
The question of how massage therapy facilitates weight gain in preterm neonates remains unanswered. One hypothesis was that massage leads to greater consumption of calories. However, preterm neonates who received massage did not consume more formula or calories than the control preterm neonates (Field et al, 1986). Another hypothesis was that the massaged neonates conserved more calories by increased sleeping time. However, the massaged neonates were more alert and spent more time in active awake states than the control neonates, suggesting that enhanced weight gain was not achieved by more time in sleep or deceased activity (Scafidi et al., 1990).
Activity Level
A third hypothesis was that preterm infant weight gain was associated with an increased activity level, as had been noted in the rat model (Mittleman & Valenstein, 1984; Mussachia, Deavers & Meininger, 1980), in malnourished children (Torun, Schutz, Viteri, et al, 1979),and as measured by activity ratings in massaged preterm infants (Lee, 2007). However, in a recent study that was focused specifically on activity recording, we documented less activity in massaged preterm infants (Field, et al, 2006). In this study, infants were randomly assigned to a moderate or light pressure massage therapy group to receive massages three times per day for 5 days. Behavior state, stress behaviors and heart rate were recorded for 15 minutes before, 15 minutes during and 15 minutes after the first and last 15 minute therapy sessions. Weight gain was recorded over the 5-day therapy period. The moderate versus light pressure massage group gained significantly more weight per day. During the behavior observations, the moderate versus light pressure massage group showed significantly lower increases from the pre-session to the session recording on: (1) active sleep; (2) fussing; (3) crying; (4) movement; and (5) stress behavior (hiccupping). They also showed a smaller decrease in deep sleep, a greater decrease in heart rate and a greater increase in vagal tone. Thus, the moderate pressure massage appeared to lead to more relaxed, less aroused and less active behavior than the light pressure massage which may have contributed to the greater weight gain of the moderate pressure massage therapy group.
The preterm infants receiving moderate pressure massage therapy also showed fewer stress behaviors and less activity over the long term from the first to the last day of the 5-day study (Hernandez-Reif, Diego, & Field, 2007). These findings suggest that massage has pacifying or stress-reducing effects on preterm infants, leading to less activity rather than greater activity.
Data from another group showing decreased energy expenditure following 5 days of moderate pressure massage also suggest reduced activity (Lahat, Mimouni, Ashbel & Dollberg, 2007). In this study, metabolic measurements were performed by indirect calorimetry. Even with only 10 infants in the sample (used as their own controls) and only after 5 days of massage, energy expenditure was significantly lower.
Vagal Activity and Gastric Motility
A fourth hypothesis was that moderate pressure massage stimulates the vagus nerve (one of the 12 cranial nerves in the brain) leading to increased vagal activity and in turn to increased gastric motility (movement of the gastrointestinal tract) and the release of insulin (a food absorption hormone) and IGF-1(a growth hormone). This hypothesized mechanism was based on studies demonstrating increased vagal activity(Diego et al, 2005; Lee,2007) and insulin levels (Field, Diego, Hernandez-Reif, Dieter, Kumar, Schanberg & Kuhn, 2008) in preterm neonates after massage therapy, on a rat model showing that moderate-pressure stroking is critical for stimulating the release of ornithine decarboxylase (an index of growth hormone), (Pauk, Kuhn, Field, & Schanberg,1986; Schanberg & Field, 1987) and on both rat and human models showing that stimulation of pressure receptors in the intraoral cavity increases vagal activity and the release of food absorption hormones (Uvnas-Moberg, Widstrom, Marchini, & Winberg, 1987).
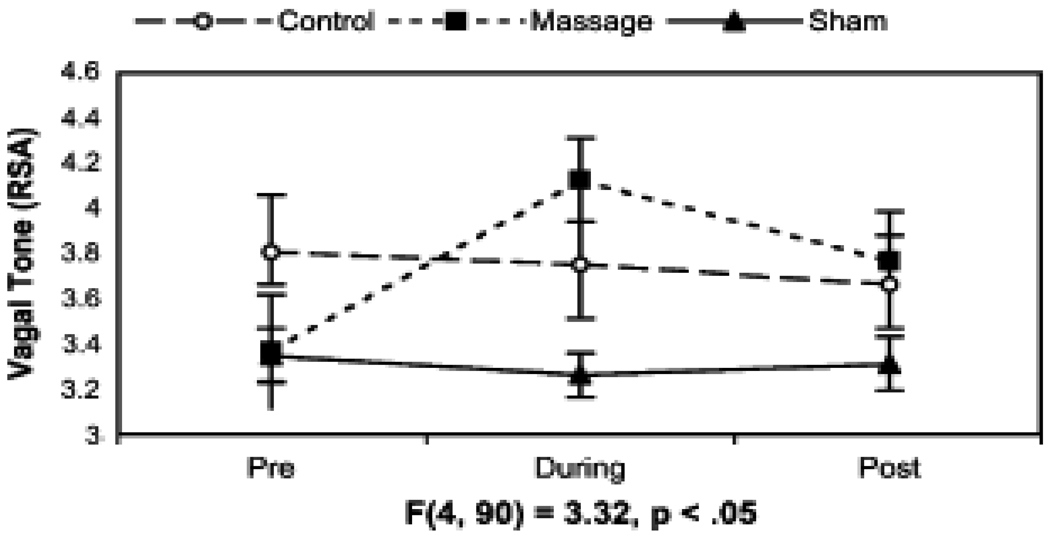
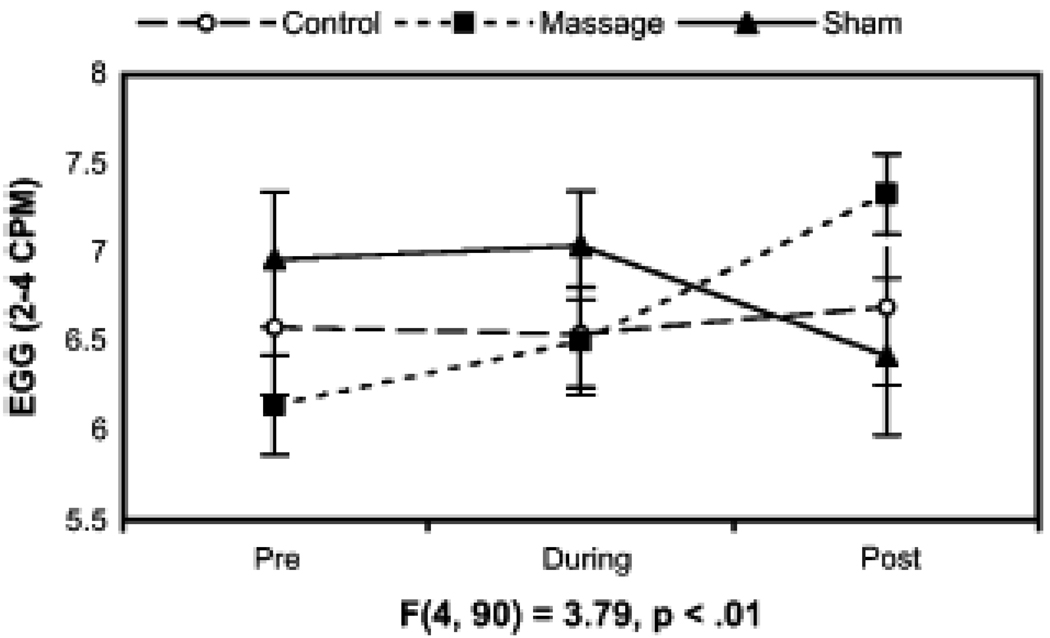
We examined this potential mechanism by assessing indices of vagal activity and gastric motility in preterm neonates receiving moderate pressure massage therapy (Diego et al, 2005). Based on previous findings, we hypothesized that preterm neonates receiving moderate pressure massage therapy would show greater weight gain and a greater increase in vagal activity and gastric motility, but not greater caloric intake than preterm neonates receiving light pressure stimulation( Sham massage) or controls. In this study, preterm neonates receiving moderate pressure massage therapy exhibited greater weight gain and increased vagal tone (see figure 1) and increased gastric motility (see figure 2) during and immediately after treatment. Gastric motility and vagal activity during massage therapy, in turn, were significantly related to weight gain (Diego et al, 2005).
Figure 1.
Mean sympathetic and parasympathetic activity 15 minutes before, during, and after treatment (error bars denote ± 2 standard errors). Group-by-time interaction statistics for each measurement are presented under each line plot.
Figure 2.
Mean gastric activity 15 minutes before, during, and after treatment (error bars denote ± 2 standard errors). Group-by-time interaction statistics for each measurement are presented under each line plot.
To determine whether preterm infant massage leads to consistent increases in vagal activity and gastric motility and whether these increases are associated with greater weight gain, EKG and EGG were recorded in 80 preterm infants randomly assigned to a moderate pressure massage therapy group or to a standard care control group (Diego, Field & Hernandez-Reif, 2007). Vagal activity and gastric motility were measured before, during and after massage therapy sessions on the first and fifth day of therapy. The massaged infants exhibited consistent short-term increases in vagal activity and gastric motility on both the first and the last days of the 5-day study (see figure 3). These measures were, again, significantly related to weight gain during the 5-day treatment period.
Figure 3.
Mean vagal activity and gastric motility on the first and last days of the study for preterm infants assigned to the control (closed circles) and massage group (open circles).
Data from other labs provide further support for the relationships between moderate pressure massage and increased vagal activity and weight gain. In a study using moderate pressure massage, vagal activity increased (Lee, 2007), while, in another study using light pressure stimulation, no changes were noted in vagal activity or weight gain (Harrison, Williams, Leeper, Stem & Wang, 2000). These findings highlight the critical importance of moderate pressure for attaining these effects.
Insulin and IGF-1
Massage therapy may also lead to increased insulin and insulin-like growth factor-1 (IGF-1) and ultimately greater weight gain. IGF-1 is notably lower in preterm infants (Cutfield, Regan, Jackson, Jefferies, Robinson, Harris & Hoffman, 2004). And, in both full-term and preterm infants, IGF-1 is significantly correlated with birthweight, body length and Ponderal index (Lo, Tsao, Hsu, Chen,Yu & Chi, 2002). Inasmuch as a positive relationship has been observed between IGF-1 levels and subsequent weight gain (Amad, Zaldivar, Iwanaga, Koeppel, Grochow, Nemet, Waffarn, Eliakim, Leu & Cooper, 2007; Xu,1996), IGF-1 might be one of the factors mediating the greater weight gain observed in massaged preterms, and the reverse might also be true, i.e. that weight gain may stimulate insulin and IGF-1.
In a recent study, we examined the effects of massage therapy on insulin and IGF-1(Field et al, 2008). Following five days of massage therapy, preterm neonates were expected to show greater weight gain and higher concentrations of insulin and IGF-1 than neonates who were not massaged. To determine if massage therapy increased serum insulin and insulin-like growth factor 1 (IGF-1) in preterm neonates, forty-two preterm neonates ( M=29.5 weeks gestational age; M birthweight=1237 gms) were randomly assigned to massage therapy (body stroking and passive limb movements for three, 15-minute periods per day for 5 days) or a standard treatment control group. The groups did not differ on baseline variables including ethnicity, gestational age and birthweight. On days 1 and 5, the serum collected by clinical heelsticks was also assayed for insulin and insulin-like growth factor-1 (IGF-1), and weight gain and kilocalories consumed were recorded daily. Despite similar formula intake, the massaged preterm neonates showed greater increases during the 5 day period in: 1) weight gain; 2) serum levels of insulin; and 3) insulin-like growth factor-1 (IGF-1) (see table 1). Insulin and IGF-1 were, in turn, significantly related to weight gain.
Table 1.
Means for changes in growth variables (standard deviations in parentheses)
| Group | ||
|---|---|---|
| Variables | Control | Massages |
| Kcal/Kg Consumed | 115.9 | 115.1 |
| (10.8) | (9.8) | |
| Change in Weight Gain | −.47 | 13.62 |
| (24.1) | (16.0) | |
| Change in Insulin | .42 | .953 |
| (.11) | (.24) | |
| Change in IGF-1 | .33 | .721 |
| (.49) | (.74) | |
p<.05,
p<.02
p<.001
The data from this study suggested for the first time that weight gain was also related to increased serum insulin and IGF levels following massage therapy. As already mentioned, in an earlier study we had documented increased vagal activity and gastric motility following massage therapy, and these two variables were, in turn, related to weight gain (Diego et al, 2005). Inasmuch as moderate pressure massage led to those effects, while light pressure massage did not, we concluded that stimulation of pressure receptors may lead to enhanced vagal activity and, in turn, increased gastric motility. The increased insulin and IGF-1 levels and associated weight gain in massaged preterm infants might also be mediated by increased vagal activity. Enhanced vagal activity has been associated with increased production of food absorption hormones including gastrin, as reported by at least one group (Uvnas-Moberg, Widstrom, Marchini, Winberg, 1997), suggesting vagal activity as a potential mediating mechanism.
Path Analyses Models
Based on these data, we used path analysis as the recommended statistical model for assessing the relationships between massage therapy and the potential mediating variables of vagal activity, gastric motility, insulin, and IGF-1 for preterm newborn weight gain. In this hypothesized model we tested the following three paths independently for the massage and for the control group (See figure 4): 1) increased calorie intake leading to greater weight gain; 2) increased physical activity leading to greater weight gain; and 3) increased vagal activity leading to increased gastric activity and IGF-1 levels, in turn, leading to increased weight gain.
Figure 4.
Hypothesized path analyses models for mediating variables contributing to weight gain in massage and control groups.
Inspection of the hypothesized model for the massage group revealed the following: 1) increased calorie intake and increased physical activity did not play a role in weight gain; 2) increased vagal activity was associated with increased gastric motility, which was ,in turn, related to greater weight gain; and 3) even though increased IGF-1 was related to greater weight gain, it was not related to increased vagal activity, suggesting that increased IGF-1 represents an independent pathway for weight gain. Inspection of the hypothesized model for the control group revealed that greater calorie consumption was the only pathway related to greater weight gain.
A subsequent reevaluation of these models (See figure 5) revealed that the change in vagal activity during massage therapy explained 53% of the variance in the change in gastric motility, consistent with our hypothesized model. Further, the change in gastric motility and the change in IGF-1 predicted 45% of the variance in weight gain during the study period. The strongest path involved the change in gastric motility. However, the direct paths between the change in IGF-1 and weight gain explained at least an additional 7% of the variance in weight gain during the study period, independent of the effects of gastric motility on weight gain. Surprisingly, the change in vagal activity was not related to the change in IGF-1, suggesting that massage may have resulted in increased IGF-1 levels via mechanisms not involving parasympathetic nervous system activity (vagal activity). One potential pathway may involve direct release of IGF-1 from muscle tissue following massage. Path analyses conducted on data for the control group revealed that the change in calorie consumption explained 27% of the variance in weight gain.
Figure 5.
Corrected path analyses models for mediating variables contributing to weight gain in massage and control groups
Taken together, these findings suggest that massage therapy may lead to increased weight gain via at least two potential mechanisms: 1) increased vagal activity leading to increased gastric motility, and, perhaps, the release of food absorption hormones (insulin) leading to greater weight gain; and 2) release of IGF-1 directly leading to greater weight gain, perhaps by fomenting muscle and bone development. That calorie intake was the only variable related to weight gain in the control group, further supports the role of vagal activity, gastric motility and IGF-1 as potential mediators for the effects of massage on preterm infant weight gain.
Adding insulin in still another path analysis conducted on data for the massage group revealed that the change in vagal activity during the massage explained 49% of the variance in the change in gastric motility, consistent with our hypothesized model (See figure 6). Similarly, the change in vagal activity during the massage explained 62% of the variance in the change in insulin, consistent with our hypothesized model. That the change in gastric activity was not related to the change in insulin suggests two parallel pathways via which massage therapy leads to increased weight gain: 1) insulin release via the celiac branch of the vagus; and 2) increased gastric motility via the gastric branch of the vagus. Significant paths further revealed that the changes in gastric motility, insulin and IGF- I predicted 62% of the variance in weight gain during the study period. Surprisingly, neither the change in vagal activity nor the change in insulin were related to the change in IGF-1, suggesting that massage may have resulted in increased IGF-1 levels via a mechanism not involving parasympathetic nervous system activity (vagal activity) or insulin release. One potential pathway may involve direct release of IGF-1 from muscle tissue following massage. Taken together these findings suggest that massage therapy may lead to increased weight gain via at least two potential mechanisms 1) increased vagal activity leading to increased gastric motility and the release of insulin leading, in turn, to greater weight gain; and 2) the release of IGF-1 via unknown mechanisms leading to greater weight gain, perhaps by fomenting muscle and bone development.
Figure 6.
Path analysis conducted for the massage (N=14) group for infants with Insulin data
There are, of course other potential mediating variables that were not entered into these analyses including other sources of stimulation on the neonatal intensive care unit such as breastfeeding and kangaroo care (parent carrying the infant inside of the parent’s clothing), although these were standard practices for all of the infants in the studies. Nonetheless, the data provide further support for massage therapy effects on the growth of preterm infants.
Summary
In this paper, potential underlying mechanisms for massage therapy effects on preterm infant weight gain are reviewed including a model for increased vagal activity, gastric motility, IGF-1 and insulin. Path analyses are presented suggesting that increased calorie intake and physical activity did not play a role in weight gain. However, 1) increased vagal activity was associated with 2) increased gastric motility, which, in turn, was related to 3) greater weight gain; and 4) increased IGF-1 was related to greater weight gain. IGF-1 was not related to increased vagal activity, suggesting that increased IGF-1 represents an independent pathway for weight gain. For the control group, greater calorie consumption was the only pathway related to greater weight gain. Adding insulin in another path analysis conducted on data for the massage group revealed that the change in vagal activity during the massage explained 49% of the variance in the change in gastric activity. Similarly, the change in vagal activity during the massage explained 62% of the variance in the change in insulin. That the change in gastric activity was not related to the change in insulin suggests two parallel pathways via which massage therapy leads to increased weight gain: 1) insulin release via the celiac branch of the vagus; and 2) increased gastric activity via the gastric branch of the vagus.
Further studies might evaluate other aspects of the IGF system such as various IGF-binding proteins. In the interim, these data highlight the clinical significance of preterm neonates receiving massage therapy. Although massage therapy is not widely practiced on neonatal intensive care units, these data on potential underlying mechanisms for its effects on preterm infant growth will hopefully facilitate wider acceptance by the neonatal medical community.
Research Highlights.
Potential underlying mechanisms for massage therapy effects on preterm infant weight gain are reviewed.
Change in vagal activity during the massage explained the variance in the change in gastric activity and insulin.
Two parallel pathways are suggested in which massage therapy leads to increased weight gain.
Acknowledgements
We would like to thank the mothers and infants who participated in these studies. This research was supported by a merit Award (MH # 46586), an NIH grant ( AT#00370) and Senior Research Scientist Awards ( MH#0033 1 and AT#0011585) and a March of Dimes Grant (#12-FY03-48) to Tiffany Field and funding from Johnson and Johnson Pediatric Institute to the Touch Research Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmad I, Zaldivar F, Iwanaga K, Koeppel R, Grochow D, Nemet D, Waffarn F, Eliakim A, Leu S, Cooper D. Inflammatory and growth mediators in growing preterm infants. Journal of Pediatric Endocrinology and Metabolism. 2007;20:387–396. doi: 10.1515/jpem.2007.20.3.387. [DOI] [PubMed] [Google Scholar]
- Cutfield W, Regan F, Jackson W, Jefferies C, Robinson E, Harris R, Hoffman P. The endocrine consequences for very low birthweight premature infants. Growth Hormone and IGF Research. 2004;14:130–135. doi: 10.1016/j.ghir.2004.03.028. [DOI] [PubMed] [Google Scholar]
- Diego MA, Field T, Hernandez-Reif M. Vagal activity, gastric motility and weight gain in massaged preterm neonates. Journal of Pediatrics. 2005;147:50–55. doi: 10.1016/j.jpeds.2005.02.023. [DOI] [PubMed] [Google Scholar]
- Diego MA, Field T, Hernandez-Reif M, Deeds O, Ascencio A, Begert G. Preterm infant massage elicits consistent increases in vagal activity and gastric motility and those are associated with greater weight gain. Acta Paediatrica. 2007;96:1588–1591. doi: 10.1111/j.1651-2227.2007.00476.x. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M, Dieter J, Kumar A, Schanberg S, Kuhn C. Insulin and insulin-like growth factor 1 (IGF-1) increase in preterm infants following massage therapy. Journal of Developmental and Behavioral Pediatrics. 2008;29:463–466. doi: 10.1097/DBP.0b013e3181856d3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Hernandez-Reif M, Diego M. Massage therapy for pediatric problems. In: Field T, editor. Touch and Massage in Early Child Development. Johnson & Johnson Pediatric Institute; 2004. pp. 99–111. [Google Scholar]
- Field T, Diego M, Hernandez-Reif M. Preterm infant massage therapy research: A review. Infant Behavior and Development. 2010;33:115–124. doi: 10.1016/j.infbeh.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego MA, Hernandez-Reif M, Deeds O, Figuereido B, Ascencio A. Moderate versus light pressure massage therapy leads to greater weight gain in preterm infants. Infant Behavior & Development. 2006;29:574–578. doi: 10.1016/j.infbeh.2006.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Schanberg S, Scafidi F, Bauer C, Vega-Lahr N. Tactile/kinesthetic stimulation effects on preterm neonates. Journal of the American Academy of Pediatrics. 1986;77:654–658. [PubMed] [Google Scholar]
- Harrison LL, Williams AK, Leeper J, Stem JT, Wang L. Factors associated with vagal tone responses in preterm infants. Western Journal of Nursing Research. 2000;22:776–792. doi: 10.1177/01939450022044755. [DOI] [PubMed] [Google Scholar]
- Hernandez-Reif M, Diego M, Field T. Preterm infants show reduced stress behaviors and activity after 5 days of massage therapy. Infant Behavior & Development. 2007;4:557–561. doi: 10.1016/j.infbeh.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahat S, Mimouni FB, Ashbel G, Dollberg S. Energy expenditure in growing preterm infants receiving massage therapy. Journal of the American College of Nutrition. 2007;26:356–359. doi: 10.1080/07315724.2007.10719623. [DOI] [PubMed] [Google Scholar]
- Lee HK. The effect of infant massage on weight gain, physiological and behavioral responses in premature infants. Taehan Kanho Hakhoe Chi. 2005;35:1451–1460. doi: 10.4040/jkan.2005.35.8.1451. [DOI] [PubMed] [Google Scholar]
- Lo H, Tsao I, Hsu W, Chen H, Yu W, Chi C. Relation of cord serum levels of growth hormone, insulin-like growth factor, insulin-like growth factor binding proteins, leptin, and interleukin-6 with birthweight, birth length, and head circumference in term and preterm neonates. Nutrition. 2002;18:604–608. doi: 10.1016/s0899-9007(01)00811-5. [DOI] [PubMed] [Google Scholar]
- Mittleman G, Valenstein ES. Ingestive behavior evoked by hypothalamic stimulation and schedule-induced polydipsia are related. Science. 1984;27:415. doi: 10.1126/science.6710151. [DOI] [PubMed] [Google Scholar]
- Mussachua XJ, Deavers DR, Meininger GA, et al. A model for hypokinesia: Effects on muscle atrophy in rat. Journal Applied Physiology. 1980;48:479–485. doi: 10.1152/jappl.1980.48.3.479. [DOI] [PubMed] [Google Scholar]
- Pauk J, Kuhn C, Field T, Schanberg S. Positive effects of tactile versus kinesthetic or vestibular stimulation on neuroendocrine and ODC activity in maternally-deprived rat pups. Life Sciences. 1986;39:2081–2087. doi: 10.1016/0024-3205(86)90359-0. [DOI] [PubMed] [Google Scholar]
- Torun B, Schutz Y, Viteri F, et al. Growth body composition and heart rate/ VO2 during the nutritional recovery of children with two different physical activity levels. Bibliotheca Nutritio et Dieta. 1979;27:55–56. doi: 10.1159/000402370. [DOI] [PubMed] [Google Scholar]
- Uvnas-Moberg K, Widstrom AM, Marchini G, Winberg J. Release of GI hormones in mother and infant by sensory stimulation. Acta Physiology Scandinavian Supplement. 1997;76:851–860. doi: 10.1111/j.1651-2227.1987.tb17254.x. [DOI] [PubMed] [Google Scholar]
- Xu R. Development of the newborn GI tract and its relation to colostrum/milk intake: A review. Reproduction, Fertility and Development. 1996;8:35–48. doi: 10.1071/rd9960035. [DOI] [PubMed] [Google Scholar]