Single incision laparoscopic inguinal hernia repair appears to be a safe and efficient alternative to multiport laparoscopic inguinal hernia repair.
Keywords: Inguinal hernia, Total extraperitoneal, Laparoscopy, SILS™
Abstract
Almost 20 years after the first laparoscopic inguinal hernia repair was performed, single incision laparoscopic surgery (SILS™) is set to revolutionize minimally invasive surgery. However, the loss of triangulation must be overcome before the technique can be popularized. This study reports the first 100 laparoscopic total extraperitoneal hernia repairs using a single incision. The study cohort comprised 68 patients with a mean age of 44 (range, 18 to 83): 36 unilateral and 32 bilateral hernias. Twelve patients also underwent umbilical hernia repair with the Ventralex patch requiring no additional incisions. A 2.5-cm to 3-cm crescentic incision within the confines of the umbilicus was performed. Standard dissecting instruments and 52-cm/5.5-mm/300 laparoscope were used. Operation times were 50 minutes for unilateral and 80 minutes for bilateral. There was one conversion to conventional 3-port laparoscopic repair and none to open surgery. Outpatient surgery was achieved in all (except one). Analgesic requirements were minimal: 8 Dextropropoxyphene tablets (range, 0 to 20). There were no intraoperative or postoperative complications with a high patient satisfaction score. Single-incision laparoscopic hernia repair is safe and efficient simply by modifying dissection techniques (so-called “inline” and “vertical”). Comparable success can be obtained while negating the risks of bowel and vascular injuries from sharp trocars and achieving improved cosmetic results.
INTRODUCTION
Medicare Australia provides accurate figures on all types of operations performed (www.medicareasutralia.gov.au). In 2009, there were 26 407 inguinal hernia repairs. In 1994, only 9.7% of all inguinal hernias were performed laparoscopically compared to 40% in 2009. Indeed in certain states, such as New South Wales and Queensland, this figure now approaches 50%. Therefore, at least in these states in 2009, laparoscopic repair of inguinal hernias has become the gold standard in terms of percentages, having overtaken all other methods of open inguinal hernia repair, including Bassini1,2,3 (1889), Shouldice4 (1945), Lichenstein5 (1987), and Stoppa6 (1989). This is quite remarkable given that the laparoscopic repair was only first introduced by Ger et al7,8 in 1990.
The fact that laparoscopic inguinal hernia repair has become popular worldwide can be attributed to 2 main reasons. First, laparoscopy has allowed placement of a large piece of mesh behind the defect where, according to Laplace's Law, the same forces that cause the hernia are used to reinforce the repair. Second, the associated benefits of minimally invasive surgery, such as improved cosmesis, less pain, faster recovery, and improved success rates, have been shown not just in hernia surgery but also in other general surgical procedures like cholecystectomy, gastric banding and appendectomy, as well as in other surgical disciplines like gynecology and urology.
However, despite its apparent popularity, laparoscopic hernia repair is a relatively difficult procedure to learn compared with open hernia repair. In addition, unlike open inguinal hernia surgery, laparoscopic hernia surgery is associated with rare and dangerous complications, such as bladder, bowel, and vascular injuries. Some of these injuries have been caused by the sharp introducers used for traditional 3-port laparoscopic inguinal hernia repair. These injuries are often under reported.
Single incision laparoscopic surgery represents the first major advance in laparoscopic hernia repair since the latter was first introduced 20 years ago. The SILS port introduced via a single incision allows the deployment of 3 ports with blunt introducers, hence negating the risks of potential catastrophic bowel or vascular punctures. The first case report by Filipovic-Cugura et al9 in 2009 paved the way for its application in laparoscopic surgical procedures. However, single port laparoscopic surgery has its unique challenges, mainly the relative loss of triangulation, which must be overcome before it can be popularized. This study aims to assess the safety and efficacy of the single incision laparoscopic inguinal hernia repair and to identify solutions to the challenges of SILS.
MATERIALS AND METHODS
This prospective nonrandomized study was approved by the Holroyd Private Hospital Medical Advisory Committee. Our unit began performing SILS TEP repair in October 2009. Patients with inguinal hernias are placed on routine hernia operating lists on a first-come-first-serve basis, unless they have medical conditions like diabetes, in which case they are placed first on the list. In the first 2 months, an average of 1 to 3 cases were selected from a routine list of some 5 to 10 hernias on an operating day, including laparoscopic ventral hernia repairs. Patients for SILS TEP repair were the first on the list. We anticipated that the initial learning curve would not permit smooth and timely running of our lists. However, since December 2009, all patients undergoing laparoscopic inguinal hernia repair have been enrolled in the study. This coincided with availability of the 52-cm/5.5-mm/30° angle laparoscope (Karl Storz, Hamburg, Germany).
Patients are informed of our practice of using a single incision under the umbilicus and that there would be a small possibility that additional incisions in the midline may need to be used as per traditional TEP repair. All our patients are catheterized after induction of anesthesia and receive 1g of Cephazolin. Patients are prepped with Betadine from the mid thighs to the epigastrium but are draped to expose only a 2-cm window of skin just above the umbilicus to symphysis pubis to minimize skin exposure.
Having infiltrated the infraumbilical skin with 20mL of 0.5% Marcaine with 1:200 000 Adrenaline, a 2.5-cm transverse skin crease incision is made. The subcutaneous tissue is dissected down to the anterior rectus sheath on the side of the hernia for a unilateral hernia or the side of the larger hernia with the aid of S-shaped retractors. The anterior rectus sheath is then incised transversely from midline to laterally with care being taken to avoid going through the intersection. The fleshy part of the rectus muscle can usually be seen through the anterior rectus sheath. The S-shaped retractors are then used to retract the rectus muscle laterally and anteriorly. At this stage, we place the patient 10° to 15° head down.
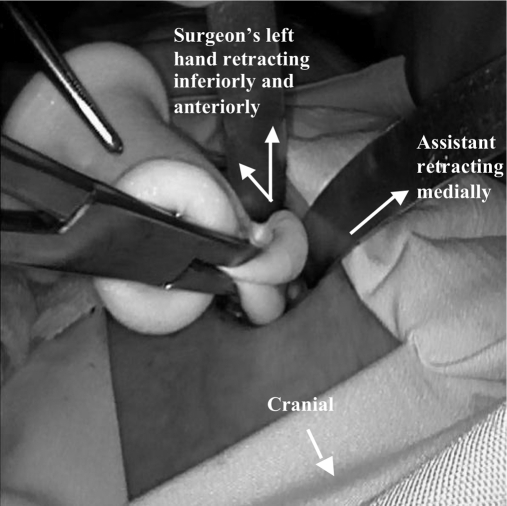
We routinely create the extraperitoneal space with a distension balloon (Covidien, Norwalk, Connecticut, USA) under direct vision. The surgeon then grasps the SILS port with a pair of Kochers at the inferior edge with the gas insufflator hose being distal (Figure 1). With the assistant retracting the rectus laterally and upward, the surgeon's left hand retracts the rectus upward, and the SILS port is introduced in the direction under the rectus muscle in one smooth but firm motion. It is usually obvious that the port is in the correct location when the retractors are removed, because the port seems to be “sucked” down against the skin. Difficulties can arise when the skin or anterior rectus sheath incisions are not big enough, in which case an extension by a further 2mm or so will be sufficient. Once the port is in place, it is rotated by using 2 Kocher forceps (7”, curved, Biomedical Research Instruments, Inc. Silversprings, MD, USA) applied to the outside flange of the port until the insufflator hose is in the inferior position. The three 5-mm ports are then inserted with the anterior-most port being used for the 52-cm/5.5-mm/30°angle laparoscope (Karl Storz, Hamburg, Germany). From October to November 2009, only conventional 30-cm (5-mm or 10-mm), 30° angle laparoscopes were used.
Figure 1.
Insertion of SILSport in infraumbilical incision for TEP inguinal hernia repair.
Once we are satisfied that the port is in the correct position, the extraperitoneal space is insufflated with CO2 to 12 mm Hg. Unlike the triangular balloon in the structural port used for the traditional TEP repair, which pushes the posterior rectus sheath down, the SILS port does not have this, and hence care must be taken in introducing the dissecting instruments to avoid puncturing the posterior rectus sheath, as this would create a pneumoperitoneum, and make the operation more difficult. With each entry of the dissecting instrument, the laparoscope is withdrawn back close to the port, and the instrument is introduced with the hand being pushed down so that it travels deep to the rectus muscle. This is also important in taking some of the leveraging pressure off the scope, as due to its relatively small size, it is prone to being damaged if excessive bending pressure is exerted.
The principles of TEP repairs are the same and must be followed to avoid injuries to bladder, vessels, nerves, and vas deferens. Briefly, the symphysis pubis is identified and dissected free of areolar tissues and the bladder. The inferior epigastric vessels are then identified, and the lateral space is then dissected and continued medially until the cord structures are identified. An indirect sac and its accompanying lipoma of the cord are reduced with sufficient proximal dissection of the peritoneal reflection to allow the inferior edge of the mesh to lie well clear of it. This dissection then continues medially and any direct sac is reduced and stapled onto the pubic bone with Protack staples (Covendien, Norwalk, Connecticut, USA).
Loss of Triangulation
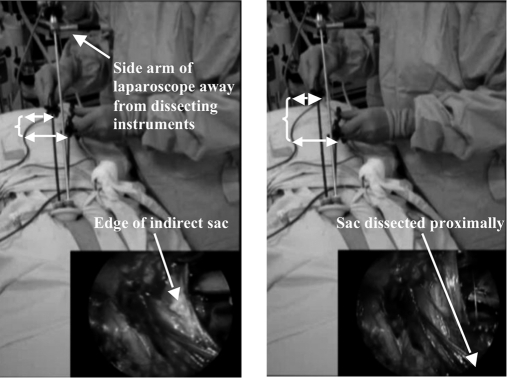
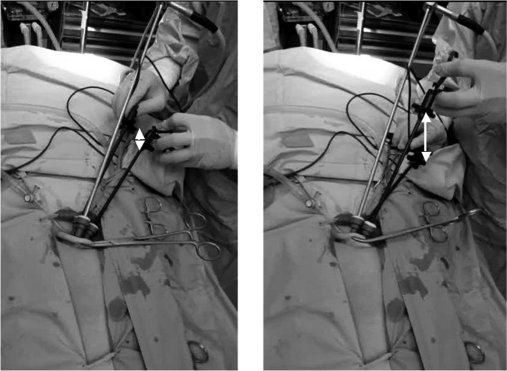
Dissection techniques must be modified to accomplish safe and efficient TEP repair with SILS. Because all 3 instruments are in the same port, severe and disheartening clashing of these will occur, especially if a normal 10-mm scope is used. Two of the most important maneuvers are first the “inline” dissection (Figure 2), ie, with one dissecting instrument pushing away and the other pulling the instrument out. This maneuver is especially useful for reducing an indirect sac or lipoma of the cord. The second important maneuver is the “vertical” dissection technique whereby dissecting instruments go vertically in opposite directions on either side of the laparoscope (Figure 3). This is especially useful for dissecting the lateral space. The normal “horizontal” dissection technique can still be used, but this is limited, because of the clashing of instruments, to achieving dissection of delicate structures in millimeters at a time.
Figure 2.
Inline dissection showing right hand pulling backward and left hand pushing forward shown by increased distance between the 2 graspers from left to right (see arrows).
Figure 3.
“Vertical” dissection with graspers on either side of scope as seen by increase in vertical separation of graspers shown by arrows.
Once the dissection is complete, the camera port is then removed and a 10-mm, nondisposable port is introduced. The mesh is then inserted with a pair of “dolphin” graspers in the direction of the symphysis pubis. To ensure that the mesh is out of the port, a 10-mm laparoscope is introduced and if necessary the mesh is pushed inside before the 10-mm port is replaced with a 5-mm port. The mesh (VyproII, Ethicon GmbH, Hamburg, Germany) is fixed in a standard way. In our unit, we use 2 Protack staples to fix the mesh in the midline and one laterally. If a large direct sac is present, we also fix the mesh to the pubic bone with 1 or 2 staples. The inferior edge of the mesh is then sprayed with 2mL of fibrin sealant (Tisseel, Baxter AG, Vienna, Austria). If a bilateral inguinal hernia is present, then the dissection now occurs on the opposite side. Once the mesh is in place, deflation occurs under direct vision with the patient being placed at 15° head up. The rectus sheath is now closed with interrupted and continuous 1 Nylon sutures. The subcutaneous layer is closed with 2.0 Vicryl, and the skin is closed with 4.0 Monocryl subcuticularly. One point of caution is that if the skin incision is slightly too small or the procedure is excessively long then the skin edges, usually the inferior edge, tend to become ischemic, and this must then be excised to prevent poor wound healing and potential infection. The wound is then dressed with Steristrips and Opsite. Our patients are cared for in the normal way, being able to eat and mobilize after 4 hours, and are discharged in the normal time frame.
RESULTS
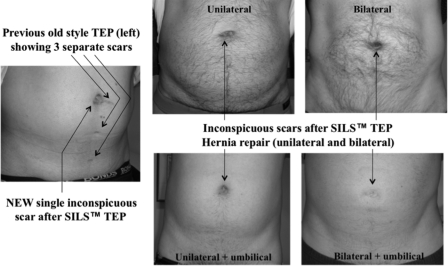
Between October 2009 and June 2010, we performed 100 hernias in 68 patients: 32 bilateral (22 indirect, 2 combined indirect and femoral, 8 direct) and 36 unilateral (20 indirect, 15 direct, and 1 pantaloon) inguinal hernias with no scrotal hernias. The mean body mass index was 29.5 ± 6.4 kg/m2. The median age was 44 (range, 18 to 83). All except 2 were males. The operation time was 50 minutes for unilateral (range, 35 to 90) and 80 minutes for bilateral (range, 60 to 125) for the entire cohort. However, of the 12 patients who underwent SILS TEP inguinal hernia repair in the first 2 months, the median operation time was 65 minutes for unilateral (9 patients) and 110 minutes for bilateral (3 patients). There was one conversion to traditional 3-port TEP repair in a patient who had previously had a laparoscopic repair on the opposite side, and the scar tissues inferior to the umbilicus prevented the safe deployment of the SILS port. There was no conversion to an open operation. All except one were outpatient cases. One patient was in the hospital overnight, because he lived 6 hours away in a rural area. The analgesic requirement was 8 tablets of Dextropropoxyphene hydrochloride with paracetamol (range, 0 to 20) with most patients ceasing analgesia 2 days after surgery. Umbilical hernia repair was also performed in 12 patients with a Ventralex hernia patch (Composix, Davol, Inc., Cranston, RI) with no additional incision (Figure 4). There was no recurrence with a follow-up of 1 month to 10 months. All patients returned to normal physical activities in 1 week to 2 weeks. There were no wound complications. The mean satisfaction score was 2.8 (range, 2 to 3) with no patient being dissatisfied with the procedure.
Figure 4.
Single-incision laparoscopic inguinal hernia repair with or without umbilical hernia repair results in inconspicuous scars (3 months postoperation).
DISCUSSION
Since the first successful laparoscopic cholecystectomy by Mühe10 in 1986, many previously open surgical procedures have become virtually obsolete or performed only as a last resort. In many industrialized nations, laparoscopic inguinal hernia repair is becoming the gold standard. Since its introduction in 1990, most of the efforts of laparoscopic hernia surgeons have concentrated on optimizing the repair with identifying the optimal mesh size or defect overlap, methods of mesh fixation and the type of mesh used for a particular hernia. With respect to mesh development, enormous efforts have been made by the industry to produce an amazing array of mesh prostheses. Therefore, the average hernia surgeon is left bewildered as to which mesh to use. Therein lies the real cost of surgical innovations in that in the field of laparoscopic inguinal hernia repair there have not been any real new technical advances. Single incision laparoscopic surgery represents the first major advance in laparoscopic surgery in 20 years in that new surgical techniques need to be learned. After all, surgery is an art and advances in instrumentation should merely compliment such artistry.
Like the prolific mesh prosthetic development, surgical instrumentation for single-port surgery and its associated instruments such as angulated graspers is rapidly expanding. However, common to all these single port devices is the relative loss of triangulation, which must be overcome for safe and efficient surgery. In our hernia practice, the routine use of SILS compared to the traditional 3 ports has meant an equivalent increase of about US $150 per patient. This is on the basis that existing instruments, including graspers and scissors that are also used for other surgical procedures, such as laparoscopic cholecystectomy, are used. While it is possible and indeed expected that the costs of these single ports will come down with increasing popularity and competition, further added costs of specialized angulated instruments, which are currently disposable, would add massively to the overall cost per procedure. Even if grasping instruments can be made to be reusable, there is still the initial capital outlay that must be made. Therefore, it is our intention to keep the single incision laparoscopic hernia repair cost effective by developing specific techniques to overcome the relative loss of triangulation, which can be applied to other general surgical procedures.
Since the report of the first case of SILS TEP repair by Filipovic-Cugura et al,9 there have only been a few other reports in the literature. Argawal,11 using the Tri-port system, reported a study over a 6-month period with 19 TEP repairs in 16 patients. The median operation time was 40 minutes for unilateral and 70 minutes for bilateral. Although there were no intraoperative complications, 2 patients developed minor wound complications and one patient reported transient pain in his testicle. Surgit12 reported 27 cases of SILS TEP inguinal hernia repairs in 23 patients using both standard and articulating instruments. There was one conversion to standard laparoscopic TEP repair. Mean operative times were 48 minutes for unilateral and 97 minutes for bilateral hernias. He found the articulating instruments useful. Our study of 100 SILS TEP repairs in 68 patients represents the largest series to date. Our results compare favorably with the early studies showing comparable operating times of 50 minutes for unilateral and 80 minutes for bilateral hernia repair with only one conversion to traditional 3-port laparoscopic TEP repair. The relative loss of triangulation can be overcome by modifying the dissection techniques; in particular, the so-called “inline” and vertical” dissection techniques are crucial for safe and efficient dissection. Once these have been learned, the hernia repair did not take any longer than the standard 3-port TEP repair. We found that the extra-long laparoscope (52-cm, 5.5-mm, and 300 angle laparoscope) was crucial in keeping the surgeon's hands holding the dissecting instruments well away from the side arm of the laparoscope. Furthermore, the relatively small size of the laparoscope used increased the mobility of the other 2 ports hosting the dissecting instruments. There were no wound complications in our study, which we attributed to judicious use of electrocautery during the initial infraumbilical dissection for deployment of the SILS port, as well as excising any skin edge that looked ischemic until it bled. The vast majority of our patients were highly satisfied with the procedure, especially with the almost invisible infraumbilical scar. We advocate a crescentic incision within the confines of the umbilicus, because this will produce the best cosmetic result.
CONCLUSION
SILS TEP repair is a safe and efficient technique for inguinal hernia repair in all patients who are fit for a general anesthetic. The main advantages include the abolition of bowel and vascular injury related to the use of sharp trocars, 1 incision as supposed to 3, which will reduce the risk of trocar hernias as well as potentially reducing the risk of port-site infection/pain and improving cosmetic results. In addition, single incision laparoscopic surgery can be applied across many general surgical procedures, such as laparoscopic ventral hernia repair, gastric banding, cholecystectomy, as well as many surgical disciplines including gynecology and urology. It should therefore be considered as part of the armamentarium of laparoscopic surgery. It should be noted that these excellent results were obtained in a specialized hernia center by the principal author who has performed nearly 2000 TEP repairs over the past 10 years. New surgeons contemplating SILS TEP repair are well advised to defer this attempt until they have mastered traditional TEP repair.
References:
- 1. Bassini E. Nuovo metodo operativo per la cura dell'ernia inguinale. Padua, 1889 [Google Scholar]
- 2. Wantz G. The operation of Bassini as described by Attilio Catterina. Surg Gynecol Obstet. 1989;168(1):67–80 [PubMed] [Google Scholar]
- 3. Sachs M, Damm M, Encke A. Historical evolution of inguinal hernia repair. World J Surg. 1997;21(2):218–23 [DOI] [PubMed] [Google Scholar]
- 4. Shouldice E. Surgical treatment of hernia. Ontario Med Rev. 1945 [Google Scholar]
- 5. Lichenstein IL. Herniorrhaphy. A personal experience with 6,321 cases. Am J Surg. 1987;153(6):553–559 [DOI] [PubMed] [Google Scholar]
- 6. Stoppa R. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545–554 [DOI] [PubMed] [Google Scholar]
- 7. Ger R, Monroe K, Duvivier R, Mishrick A. Management of indirect inguinal hernias by laparosopic closure of the neck of the sac. Am J Surg. 1990;159(4):370–373 [DOI] [PubMed] [Google Scholar]
- 8. Ger R, Mishrick A, Hurwitz J, Romero C, Oddsen R. Management of groin hernias by laparoscopy. World J Surg. 1993;17(1):46–50 [DOI] [PubMed] [Google Scholar]
- 9. Filipovic-Cugura J, Kirac I, Kulis T, Jankovic J, Benkavac-Beslin M. Single incision laparoscopic surgery (SILS) for totally extraperitoneal (TEP) inguinal hernia repair: First Case. Surg Endosc. 2009;23:920–921 [DOI] [PubMed] [Google Scholar]
- 10. Reynolds W. The first laparoscopic cholecystectomy. JSLS. 2001;5(1):89–94 [PMC free article] [PubMed] [Google Scholar]
- 11. Agrawal S, Shaw A, Soon Y. Single-port laparoscopic totally extraperitoneal inguinal hernia repair with Triport system: Initial Experience (16 patients). Surg Endosc. 2010;24(4):952–956 [DOI] [PubMed] [Google Scholar]
- 12. Surgit O. Single-incision laparoscopic surgery for total extraperitoneal repair of inguinal hernias in 23 patients. Surg Laparosc Endosc Percutan Tech. 2010;20(2):114–118 [DOI] [PubMed] [Google Scholar]