Abstract
Background
The goal of this study was to determine if increasing strength in primary knee extensors and flexors would directly affect net knee joint moments during a common functional task in persons with knee osteoarthritis.
Methods
An exploratory single sample clinical trial with pre-post treatment measures was used to study volunteers with clinical diagnosis of mild knee OA in one knee. Subjects participated in an individually supervised training program 3 times a week for eight weeks consisting of progressive resistive exercises for knee extensors and knee flexors. Pre and post training outcome assessments included: 1. Net internal knee joint moments, 2. Electromyography of primary knee extensors and flexors, and 3. Self-report measures of knee pain and function. The distribution of lower extremity joint moments as a percent of the total support moment was also investigated.
Findings
Pain, symptoms, activities of daily life, quality of life, stiffness, and function scores showed significant improvement following strength training. Knee internal valgus and hip internal rotation moments showed increasing but non-statistically significant changes post-training. There were no significant differences in muscle co-contraction activation of the Quadriceps and Hamstrings.
Interpretations
While exercise continues to be an important element of OA management, the results of this study suggest improvements in function, pain, and other symptoms, as a result of strength training may not be causally related to specific biomechanical changes in net joint moments.
Keywords: Biomechanics, Exercise, Osteoarthritis, Knee, Rehabilitation
INTRODUCTION
Treatments for knee osteoarthritis (OA) attempt to decrease pain and stiffness, and increase function through a variety of approaches. These approaches include pharmacological, surgical, physical therapy modalities, orthotics and braces, and exercise. Exercises specifically aimed at muscle strengthening have been used as the cornerstone of most exercise rehabilitation programs (Myers 1995), and the American College of Rheumatology (ACR) recommends strengthening exercise for the management of knee OA symptoms (Hochberg, Altman et al. 1995).
Strength training is presumed to protect the joint from pathologic stress and loading. Programs to strengthen knee extension and flexion have resulted in significant strength gains and appear to reduce pain and improve function (Messier, Loeser et al. 1992; Marks 1993; Fisher, White et al. 1997; Rogind, Bibow-Nielsen et al. 1998; Maurer, Stern et al. 1999; Minor 1999; Baker and McAlindon 2000; Roddy, Zhang et al. 2005). The beneficial effects of resistive exercise for individuals with OA may be attributed to several associated factors such as: facilitation of endogenous opiates which creates an analgesic effect to improve a person’s tolerance to pain (Fraioli, Moretti et al. 1980; Carr, Bullen et al. 1981; Allen 1983), decrease in depression coupled with perceived level of disability (Minor and N.E. 1996; van Baar, Dekker et al. 1998), through associated weight loss (Jenkinson, Doherty et al. 2009), or mechanically through alteration of the biomechanics of the joint (Thorstensson, Henriksson et al. 2007). It is this latter point that this study is designed to address by investigating joint moment changes associated with a strength training intervention. While there may be physiological and psychological effects related to strengthening, it is the mechanical effects that might have the most direct influence on the knee joint itself. Since abnormal or excessive joint loading can lead to articular cartilage degradation (Pearle, Warren et al. 2005), it is clinically assumed that the positive influence of strengthening the knee musculature on OA symptoms and other knee joint problems, is due to the strengthened muscle’s ability to “stabilize” or “reduce stress” in the knee joint. In a review by Bennell et al, the author’s stated “… Improving the load-bearing capacities of lower-limb muscles—in particular, the quadriceps—through strength-training and muscle rehabilitation programs may protect against soft tissue damage resulting from excessive load”(Bennell, Hunt et al. 2009). This commonly held belief has had limited studies looking at specific causal relationships between strength and actual internal knee moment adaptations. Thorestensson et al. tested an 8 week training program for effects on knee adduction moment in early knee OA patients (Thorstensson, Henriksson et al. 2007). Although they reported a statistically significant reduction in external knee adduction moment following the training, the actual reduction was less than 1 Nm, which may not be clinically significant. In addition, the intervention program included motor control oriented training, education in alignment, and stretching exercises. Educating persons on proper technique and motor control can affect alignment (Kato, Urabe et al. 2008), and may have accounted for the observed small change in the joint moment. Mikesky et al. looked at whether muscle strength appeared to be related to OA progression (Mikesky, Mazzuca et al. 2006). In patients with established OA at baseline, the joint space narrowing was not significantly different at 30 months in the strength-trained group compared to the non-strength group. In addition, the frequency of incident loss of joint space beyond their measurement error was not different between the groups. There were also similar osteophyte scores between the groups. In a cohort of 1269 women and 1006 men aged 50–79 years-old with, or at risk for, knee OA, Segal et al reported that neither concentric quadriceps strength, nor Hamstring/Quadricep ratios predicted the development of knee symptoms during a 15- & 30-month longitudinal study.(Segal, Torner et al. 2009)
In their extensive review Bennel et all (Bennell, Hunt et al. 2009) posed the question: “Do improvements in muscle function lead to improved symptoms and joint structure in knee OA? While there is ample evidence that strengthening helps patients with OA, they concluded, “…definitive conclusions regarding the mechanistic effects of strengthening cannot be drawn…”
Sharma’s group has made significant contributions to our understanding of risk factors with knee OA. Their group has shown that varus/valgus malalignment is a significant risk factor for the progression of OA and that persons with greater knee extensor strength are actually associated with increased progression on Knee OA, at least in patients with malaligned or lax knees. (Sharma, Song et al. 2001). They concluded greater strength has not been shown to make significant changes in the course of degenerative joint disease of the knee. (Sharma 2003) and suggested that approaches beyond strengthening exercises should be developed to enhance joint-protective muscle activity.(Sharma, Dunlop et al. 2003). However these results may pertain to only to persons with significant malalignment where greater strength may be associated with greater overall activity levels in these persons and result in increased abnormal knee joint loads due to the malalgnment thus facilitating the progression of their OA. In other populations such as patients post menisectomy, normalizing lower limb muscle strength has been associated with improved joint biomechanics such as lowering frontal plane knee moments (Sturnieks, Besier et al. 2008)
In a large Framingham subset study 1,279 people had knee x-rays and activity evaluation and were followed for nine years. Those exercising even at vigorous intensities had no greater risk of developing OA than participants who did not exercise (Felson, Niu et al. 2007), and the arthritis foundation continues to recommend exercise and in particular strengthening exercises for patients with OA in any joint. (see http://www.arthritis.org/types-exercise.php.)Therefore, the objective of this study was to investigate the biomechanical response to strengthening primary knee joint musculature that may directly influence deleterious knee joint mechanical loading. The goal was to explore whether changing strength alone in primary knee extensors and flexors would cause knee joint sagittal and frontal plane moments to be altered during a common functional task. Since stair climbing is a stressful and important locomotor functional activity, we have chosen to evaluate the knee biomechanics during stair stepping. Moreover we looked at the total support moment and proportional distribution of Hip extensor, knee extensor, and ankle extensor moments to the total support moment as an indicator of kinetic motor strategy changes. Muscle activation pattern changes for six muscles supporting the knee joint were also evaluated. Understanding the mechanisms of how this intervention affects symptoms is critical to providing, optimal care for patients with joint injury and joint disease.
METHODS
Participants
Subject inclusion criteria were: 1. Adults between 40 and 60 years of age, 2. Physician’s clinical diagnosis of mild knee OA using ACR criteria(Altman, Asch et al. 1986) (The ACR criteria can be found in detail at http://www.hopkins-arthritis.org/physician-corner/education/acr). The criteria rely on physical examination, age, self-reports of pain and stiffness, and radiographic reports if available, 3. Report no higher than moderate knee pain 50% of the time in past month using a 5-point Likert scale (Bucher 1991), 4. Not participating in a regular program of physical activity at time of enrollment (defined as 30–45 minutes of moderate intensive activity 3–5 times per week) and 5. Stable on any analgesic or anti-inflammatory medications used to treat their knee OA and, if medically justifiable, agree not to alter their medications or undergo any joint injections for the duration of the trial. Potential participants were excluded if: 1. They presented radiographic evidence of misalignment greater than 5 degrees of varus or valgus angulations or severe joint space narrowing, 2. They had any knee flexion contractures, 3. They had cardiovascular, respiratory or musculoskeletal conditions other than the knee OA or any serious medical condition that precludes participation in an exercise program, 4. Were unable to walk or exercise without the use of an assistive device, or 5. Had Glucocorticoid injection to the knee joint within the past 30 days or anticipated within the next 30 days or hylauronic acid injection within the past 90 days.
Twenty-one participants were recruited from UW Medical Center and Seattle metropolitan area through fliers and word of mouth. The average age was 55.8 years (± 5.8 years), average height 1.65 m (± 0.1 m), and average mass 80.8 Kg (± 19 Kg). The sample was 76% female. The demographic data are presented in detail in Table 1. One participant failed to return for follow-up and two participants were not included in analysis due to data corruption. The drop out subject dropped for motivational reasons, the other two subject’s data could not be analyzed due to technical equipment problems. All participants completed the Informed Consent Process approved by the Institution Review Board.
Table 1.
Demographic characteristics and strengthening measures for participants (n=18).
| Demographic Characteristics | Pre-Intervention | Post-Intervention | P-Value* |
|---|---|---|---|
| Age (years), Mean (s.d.) | 55.8 (5.8) | NA | NA |
| Height (m), Mean (s.d.) | 1.65 (0.1) | NA | NA |
| Mass (kg), Mean (s.d.) | 80.8 (19.0) | NA | NA |
| Body Mass Index(kg/m2), Mean (s.d.) | 30.4 (8.5) | NA | NA |
|
| |||
| MVIC Ipsilateral Leg | |||
| Knee Extension (Nm), Mean (s.d.) | 252.7 (91.7) | 304.5 (101.0) | |
| Median (Range) | 255.1 (149.7–530.7) | 273.4 (180.3–597.8) | 0.002 |
| Knee Flexion (Nm), Mean (s.d.) | 145.4 (40.2) | 149.4 (39.8) | |
| Median (Range) | 138.8 (86.7–232.0) | 149.3 (85.5–222.8) | 0.065 |
|
| |||
| Ten-Repetition Maximum Tests** | |||
| Knee Extension (Kg), Mean (s.d.) | 20.0 (7.6) | 30.8 (11.4) | |
| Median (Range) | 19.4 (9.7–45.2) | 29.1 (16.1–64.6) | <.001 |
| Knee Flexion (Kg), Mean (s.d.) | 20.5 (6.4) | 29.0 (7.2) | |
| Median Range | 21.0 (8.1–38.8) | 28.1 (14.2–48.5) | <.001 |
| Leg Press (Kg, Mean (s.d.) | 46.7.0 (14.3) | 62.6 (18.5) | |
| Median (Range) | 42.0 (18.1–64.6) | 64.6 (34.2–97.0) | <.001 |
P-value from Wilcoxon Signed Ranks Test
Outcome measures
The measures obtained in this study included: surface electromyography, knee joint biomechanics; (net joint moments, net knee internal forces) and self-report measures of knee pain and function. Maximum voluntary isometric strength as well as the ten-repetition maximum test (10RM) was used to set up the initial exercise intensity and monitor progress.
Electromyography
Surface electromyography (EMG) data were obtained using a Delsys system (DelSys Inc Boston, MA 02215.), single differential Ag/AgCl surface electrodes with a diameter of 0.8mm and inter-electrode distance of 1.0cm. The EMG signals were sampled at 1200 Hz and differentially amplified (input impedance 1015Ω//0.2pF, common mode rejection ratio (CMRR) 92dB @ 60 Hz, adjustable gain from 500–10,000)b. Electrode placement for the medial & lateral hamstrings, vastus lateralis, rectus femoris, and vastus medialis was used as described by Cram and Kasman (Cram and Kasman 1998). RMS values from three anterior thigh muscles were averaged to represent quadriceps EMG data, while the two posterior thigh muscles activity averaged represented collectively the hamstrings EMG data (Hakkinen, Kallinen et al. 1991; Babault, Pousson et al. 2002; Pereira and Goncalves 2010).
Knee Biomechanics
Six infrared cameras(Qualisys ProReflex MCU 240, Packhusgatan 6, S-411 13 Gothenburg, Sweden) were used to record position of marker clusters fixed to rigid plastic bodies attached to the pelvis, thighs, shanks, and feet of each subject bilaterally (Figure 1). Additional anatomical landmarks were digitized directly using a 3D digitizer. The digitized anatomical landmarks were used to scale segment anthropometry and to define local reference frames for each segment. The hip joint center was determined using pelvis offsets as described by Bell et.al (Bell, Pedersen et al. 1990). The knee and ankle joint centers were defined as the midpoint of medial and lateral knee joint and ankle joint markers respectively.
Figure 1.
Subject Set up with reflective markers and Instrumented step
Two forceplates (Bertec Corporation, Columbus, OH,), one embedded in the floor and one mounted on a 20 cm high step, were used to record external stance forces and as event indicators for normalization of the step task. Net joint moments were determined using standard inverse dynamics methods (Riener and Straube 1997) utilizing the segment kinematics and ground reaction forces from the two force platforms.
Strength measures
Lower extremity quadriceps and hamstring strength was assessed using maximum voluntary isometric contraction (MVIC) effort tests with the knee flexed at an angle of 45 degrees. Based on clinical experience, 45 degrees is a position well tolerated by most patients with knee problems where then can exert maximal efforts with little or no pain. Forty-five to sixty degrees is also the range of peak torque for knee extensors. A custom-designed torque transducer was mounted to an examination table with an adjustable arm to allow for isolated knee flexion and extension testing. After familiarization, the best of three trials was used as the maximum isometric torque. The MVIC tests were also used to obtain EMG amplitudes to normalize the EMG allowing for inter-subject comparisons. To set up subjects Training loads, 10RM testing (Ferguson and Mayhew 2004) was also performed for knee extensors and knee flexors.
Knee pain and function
The Knee injury and Osteoarthritis Outcome Score (KOOS)(Roos, Roos et al. 1998) was used to provide a self-reported joint-specific measures. KOOS consists of five subscales or sub-domains: Pain, Symptoms, ADL Function, Sport and Recreation Function, and knee related Quality of Life. Standardized answer options are given (5 Likert boxes) and each question is scored from 0–4. Normalized scores (100 indicating no symptoms or best health state and 0 indicating extreme symptoms or worst health state) were calculated for each subscale.
Intervention protocol
The strengthening program was based on the well-established principles of progressive resistive exercises consistent with American college of Sports Medicine guidelines (ACSM 2009) The training program duration was 8-wks. Participants were required to complete three exercise sessions per week, each lasting a maximum of one half-hour, making 24 total sessions. Each exercise session began with a 5-minute warm-up on a stationary bicycle. Exercise sessions consisted of isotonic knee extension and flexion and leg-press exercises on weight training machines. All exercises were performed bilaterally. Participants were evaluated for ten repetitions maximum (10RM) for each exercise weekly. Exercise resistances were targeted at 60%–85% of patient’s 10RM. Participants completed three sets of 10 repetitions at each session. Using the progressive resistive loading principle, the first set was at an effort level of 60–65% 10RM, the second set at 70–75% 10RM, and the third set at 80–85% 10RM effort. There was a 2-minute rest between sets. The exercise sessions were completed within 30 minutes. A Physical Therapist directly supervised all exercise sessions.
Testing procedures
One week prior to initiating the training program, participants were assessed in the Human Motion Analysis laboratory. Participants were instrumented with motion capture markers and EMG and described above. Isometric strength values were obtained. Following a five-minute rest, participants were asked to perform five step-ups onto a 20 cm high step at a self-selected pace. They were instructed to step as smoothly as possible and not jump up. The beginning of the step was defined by initial heel contact on the ground force plate with the contralateral (uninvolved) leg and the step was completed when the subject was standing straight with both legs on the top step Subjects were asked to step up leading with one leg five times and then with the other leg five times. The order of which leg went first was randomized.
Data analysis
The tasks were temporally normalized to 100% of the step cycle based on initial contact with the ground force plate and to complete standing bilaterally on the top of the step. The average of five step-ups was used to create a representative step-up. The total support moment (TSM) was calculated as the sum of the extensor moments of the hip, knee, and ankle. Each joint contributed some percentage of the TSM and changes in the distribution of the joint moments that contributed to the TSM were considered indicators of motor pattern changes associated with the strength-training program. A negative number for percentage TSM change means that the percentage of the maximal moment coming from knee joint, for example, decreased from pre- to post-intervention.
The raw EMG was RMS processed using a 55ms time constant window and normalized to the subject’s MVIC for knee flexion and extension with the knee at a 45-degree angle. EMG was evaluated by determining the total muscle activity work during stepping up (area under the RMS EMG curve during the task). Mean Hamstring/mean Quadriceps EMG ratios of total work were calculated as an index of co-contraction of thigh muscles (Pereira and Goncalves 2010).
Mean, median and standard deviations were calculated for joint moments, and normalized EMG. Normalized median and range scores were calculated from KOOS subscales as representatives of knee pain and function.
Because of the limited sample size and uncertainty associated with normality assumptions, the Wilcoxon Signed Rank Test was used to assess the pre- to post-training differences in joint kinetics and kinematics, and EMG. The data were analyzed using SPSS 17.0 and the significance level was set at alpha<0.05.
Results
Effect of training program
The intensive strength training program was tolerated well by all participants. There were no complaints of knee pain exacerbations because of the exercises. The knee extensors showed greater strength gains compared to the knee flexors. Participants’ strength changes ranged from >30% for the pre-post training MVIC of the involved knee extensors to about 2% for the uninvolved knee flexors. In addition to the Pre-Post MVIC values the participants showed even greater changes in their dynamic training 10RM loads.
Self-report measures of knee pain and function – KOOS
Table 2 shows the results for the functional and psychosocial measures collected through the KOOS scores. Except for the median scores related to Sports/Recreation sub domain, all subscales of the KOOS were statistically significant. Scores in these scales were higher at the post-intervention time, reflecting an improvement in pain, symptoms, activities of daily life, quality of life, stiffness, and function.
Table 2.
Median and range values calculated from KOOS used to compare the pre- and post-intervention effects. n=18
| KOOS Measures | Pre-Intervention Median (Range) | Post-Intervention Median (Range) | P-Value* |
|---|---|---|---|
| Pain | 66.7 (41.7–100.0) | 80.6 (52.8–100.0) | 0.008* |
| Symptoms | 64.3 (28.6–96.4) | 75 (25.0–100.0) | 0.01* |
| Activities of Daily Life | 76.5 (45.6–100.0) | 91.2 (67.6–100.0) | 0.02* |
| Sports/Recreation | 40 (0.0–100.0) | 40 (0.0–100.0) | 0.28 |
| Quality of Life | 43.7 (25.0–100.0) | 56.3 (18.7–100.0) | 0.01* |
P-value from Wilcoxon Signed Ranks Test
Net internal Knee joint moments
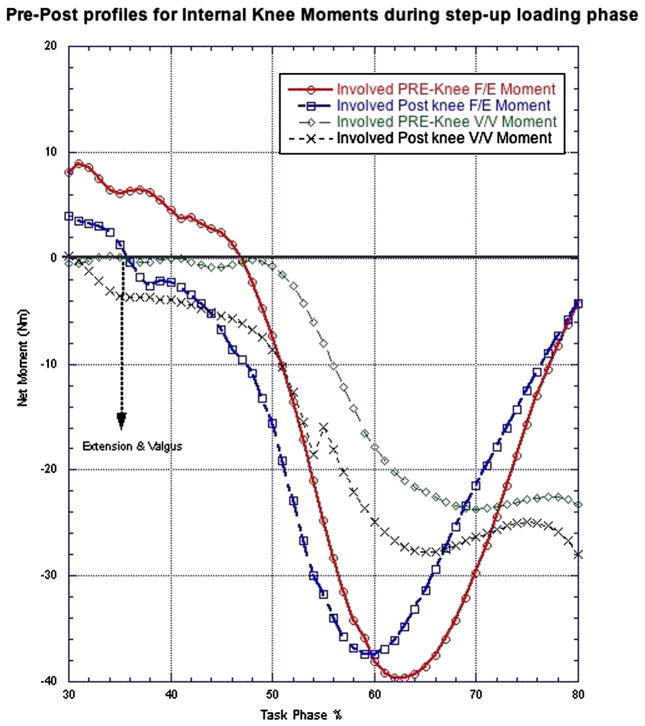
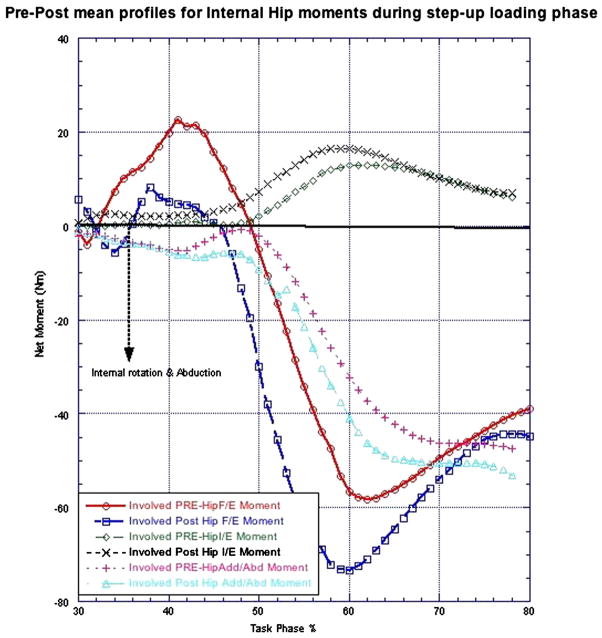
In general, there were little changes in the net moments (P=0.05–0.65) as determined by the inverse dynamics analysis, associated with the strength-training program (Table 3). The peak loading during the step up occurred between 30–80% of the step up. During this time, tendency for greater knee internal valgus moments (Figure 2), but this did not reach a level of statistical significance (P=0.08). Hip internal rotation as well as abduction moments similarly shifted post-training to be marginally increased (P=0.05) (Figure 3).
Table 3.
Median and range values calculated from Knee contact forces, Peak Moments and normalized EMG used to compare the pre- and post-intervention effects on biomechanical outcomes. n=18
| Outcome Measures | Pre-Intervention | Post-Intervention | P-Value* |
|---|---|---|---|
| Peak Step-up Moments for Involved Limb | |||
| Hip Flex/Extension (Nm) | 90.8 (36.2–126.8) | 90.7 (42.0–169.2) | 0.2 |
| Hip I/E Rotation (Nm) | 18.7 (6.7–35.0) | 21.1 (8.7–34.4) | 0.05 |
| Hip Add/Abduction (Nm) | 51.7 (33.8–95.6) | 58.7 (36.1–90.0) | 0.09 |
| Knee Flex/Extension (Nm) | 15.5 (17.2–71.3) | 18.2 (19.8–80.6) | 0.65 |
| Knee Varus/Valgus (Nm) | 33.3 (16.9–47.5) | 37.9 (15.3–55.2) | 0.08 |
| Ankle Flex/Extension (Nm) | 19.3 (12.0–82.5) | 31.2 (13.7–54.5) | 0.35 |
|
| |||
| Electromyography Measures# | |||
| Hamstring (NetArea) | 0.12 (0.066–291) | 0.11 (0.074–262) | 0.51 |
| Quadriceps (NetArea) | 0.17 (0.104–314) | 0.15 (0.103–305) | 0.73 |
| H/Q Ratio | 0.71 (0.207–1.73) | 0.62 (0.335–1.88) | 0.59 |
Hip I/E Rotation – Hip Internal/External Rotation
Hamstrings was represented by the mean profile for both Biceps Femoris + Semitendinosis. The Quadriceps activity was represented by the mean activity of the Rectus Femoris + Vastus lateralis + Vastus Medialis
P-value from Wilcoxon Signed Ranks Test
Figure 2.
Average net internal knee joint moments pre = before strength training program and post = after strength training program for involved side F/E= knee flexion/extension, V/V = knee Varus/Valgus (n=18).
Figure 3.
Average net internal hip joint moments pre = before strength training program and post = after strength training program for involved side (n=18). F/E= flexion extension, I/E = internal/external hip rotation, Add/Abd = hip adduction/abduction
Table 4 shows the mean distribution of net moments as a percent of the total support moment revealing very little strategic change in the way moments were distributed before and after training. There was high variability of the total support moment distribution attributable to the knee extensor, hip extensor, and ankle extensor net joint moments during step-up. Taken collectively there was a small trend for subjects to rely on more hip extension to power the step up by generating greater hip extension moments compared to knee extension moments after training. However, the strategy used to generate the total lower limb moment varied considerably from subject to subject.
Table 4.
Mean and standard deviation of the percent distribution of net joint extensor moments to the total support moment (TSM) before and after training as an indicator of motor strategy changes. n=18
| Ankle % TSM | Knee % TSM | Hip % TSM | TSM =Sum | |
|---|---|---|---|---|
| Pre-Training | ||||
| Mean (s.d.) | 11.37 (8.1) | 35.67 (14.6) | 52.95 (11.8) | = 100% |
| Post-Training | ||||
| Mean (s.d.) | 8.94 (6.0) | 34.23 (15.2) | 56.81 (12.7) | =100% |
Electromyography
Neither the mean nor median total Hamstrings nor Quadriceps EMG activation levels changed significantly (P=0.51–0.73) pre to post (Table 3). As an indication of co-contraction, we analyzed the H/Q ratios. There was a small trend for this ratio to increase after training suggesting some motor recruitment pattern adaptation but this was not statistically significant (P=0.59).
Discussion
The results of this study suggest that while patients self-report functional and psychosocial improvements associated with strength training, these improvements may not be causally linked to any direct biomechanical adaptations. Therefore, it questions the presumption that strength training directly effect knee joint mechanics in patients with mild OA and no significant pre-training weakness. Based on the studied sample, the peak knee extensor moments during the step-ups averaged about 25% of the participant’s maximal isometric knee extensor moment, suggesting that the step-up was a relatively low demand task. In other words, even though a patient can maximally lift more weight due to strength training, it may not change functional activities such as walking and even stair climbing if these are already a low percentage of person’s maximum strength capacity. It is possible that higher demand tasks would have shown more adaptive responses.
In a recent eight week training study with OA patients grade III or lower on the Kellegren/Lawrence classification, Jan et al (Jan, Lin et al. 2008) reported no significant difference in any measures of pain, function, walking time, and muscle moment between groups randomly assigned to high-resistance strength exercise group, low-resistance exercise group, or no exercise. This supports the question raised in this study of how much increase in strength is enough to be considered clinically necessary. These data are currently unavailable, but warrant study to determine minimum capacities based on age, gender, and perhaps BMI, for a variety of functional activities similar to the way in which physical capacity requirements are determined for many occupational groups (Sothmann, Gebhardt et al. 2004).
In this study, we used the percent of the total support moment (TSM) (Table 4) as an indicator of the motor strategy used by individuals in distributing extensor moment across the ankle, knee and hip joints when performing a step up. Our data suggest that there is potential redistribution in that patients tended to drive more of the step up using hip extensors after training. This was unexpected because we would speculate that if the knee extensors were strengthened this would allow patients to shift their stepping strategy more toward using the knee extensors. This shift toward the hip extensors only occurred in the patient’s involved limb. It may be possible that such a strategy may unburden the knee and reduces knee OA symptoms.
Table 4 suggests that different combinations of extensor moments in the Hip, knee, and ankle, can be adopted to accomplish the step-up task. This is analogous to the description of ankle, hip, and trunk strategies that can be adopted to maintain balance (Deniskina, Levik et al. 2001). This way of looking at stepping may prove useful in the future to delineate different internal moment strategies to accomplish the same task.
A crucial kinetic issue for osteoarthritis is the varus-valgus moment on the knee. The medial compartment of the tibiofemoral joint is predominately affected by OA and this is related to greater tendency of external varus alignment of the knee causing increased compression forces on the medial compartment. If the vertical ground reaction force is medial to the knee joint center and/or the shear ground reaction force is medially directed, this creates a external varus moment that must be balanced by increased internal valgus moments for dynamic equilibrium. An increased internal valgus moment may help to “unload” the medial tibiofemoral compartment. In the present study, moment patterns showed a non-significant trend to increase in the internal valgus knee moment during the step up task. This may be considered a positive effect because it is a response to an external varus (adduction) moment, which has been shown to be increased in OA patients (Sharma, Hurwitz et al. 1998; Baliunas, Hurwitz et al. 2002). In addition, while not statistically significant, the increasing trend in net hip moments may have implications for the knee as well (Souza and Powers 2009; Souza and Powers 2009). For example, hip muscles may stabilize the pelvis during gait in ways to maintain the center of mass in alignment, which may have an effect on frontal plane knee moments as suggested by Bennell (Bennell, Hunt et al. 2007). However, this has not been shown experimentally.
While the small sample size and variability are limiting factors, the findings of this pilot study offer perspectives to the link between presumed and real effects of strength training on a select patient group and the mechanisms underlying some of the observed therapeutic benefits. The minimal impairments and pre-training strength of subjects may have also minimized potential changes. Including weaker or more advanced OA patients might have magnified potential changes. The greater changes in the actual dynamic training loads reached after strength training compared to the MVIC tests are most likely related to the closeness of the test to the actual exercise training and reflects the principle of specificity of training.
Conclusions
The results of this study suggest that patients with mild OA of the knee report improvements in function, pain, and other symptoms, as a result of a supervised eight-week strength training program. The participants tolerated the intensive progressive resistance exercise program well, and showed significant strength gains with no exacerbations of symptoms reported. While there were some small trends toward some adaptive changes in motor strategies for stepping, there were no significant changes in net joint moments, or specific muscle activation patterns such as the level of co-contraction of the Quadriceps and Hamstring muscles. Given the general acceptance of the importance of strengthening exercises for OA, even with specific subset limitations, and suggested by Sharma. It is important to continue to investigate direct mechanistic relationships between the improvement of strength and potential biomechanical adaptations. Our study suggests that while improving strength results in improvements in self-report measures of pain and function these improvements may not be related to strong specific biomechanical adaptations such as changes in joint moments, distribution of the total support moment or Muscle activation levels during a step-up activity
Acknowledgments
Source of support: Supported by: NIH-NICHD R03 project #04-3978-E/A 04
The Authors would like to thank Marcia Ciol, PhD, for statistical consultation and support and Robert Price, MSME, for data reduction software design and support.
Footnotes
Disclaimers: None. We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (e.g., NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
The study was performed at the University of Washington.
Contributor Information
Kevin James McQuade, Department of Rehabilitation Medicine, Physical Therapy Program, University of Washington, Seattle, WA, USA.
Anamaria Siriani de Oliveira, Department of Biomechanics, Medicine and Rehabilitation of Locomotor Apparatus, Physical Therapy Program, University of São Paulo, Ribeirão Preto, SP, Brazil.
References
- ACSM. Progression Models in Resistance Training for Healthy Adults. Medicine & Science in Sports & Exercise. 2009;41(3):687–708. doi: 10.1249/MSS.0b013e3181915670. 610.1249/MSS.1240b1013e3181915670. [DOI] [PubMed] [Google Scholar]
- Allen M. Activity-generated endorphins: a review of their role in sports science. Can J Appl Sport Sci. 1983;8(3):115–133. [PubMed] [Google Scholar]
- Altman R, Asch E, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- Babault N, Pousson M, et al. EMG activity and voluntary activation during knee-extensor concentric torque generation. Eur J Appl Physiol. 2002;86(6):541–547. doi: 10.1007/s00421-002-0579-3. [DOI] [PubMed] [Google Scholar]
- Baker K, McAlindon T. Exercise for knee osteoarthritis. Curr Opin Rheumatol. 2000;12(5):456–463. doi: 10.1097/00002281-200009000-00020. [DOI] [PubMed] [Google Scholar]
- Baliunas AJ, Hurwitz DE, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10(7):573–579. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- Bell AL, Pedersen DR, et al. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23(6):617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- Bennell KL, Hunt MA, et al. The effects of hip muscle strengthening on knee load, pain, and function in people with knee osteoarthritis: a protocol for a randomised, single-blind controlled trial. BMC Musculoskelet Disord. 2007;8:121. doi: 10.1186/1471-2474-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennell KL, Hunt MA, et al. Muscle and exercise in the prevention and management of knee osteoarthritis: an internal medicine specialist’s guide. Med Clin North Am. 2009;93(1):161–177. xii. doi: 10.1016/j.mcna.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Bucher L. Evaluating the affective domain. Consider a Likert scale. J Nurs Staff Dev. 1991;7(5):234–238. [PubMed] [Google Scholar]
- Carr DB, Bullen BA, et al. Physical conditioning facilitates the exercise-induced secretion of beta-endorphin and beta-lipotropin in women. N Engl J Med. 1981;305(10):560–563. doi: 10.1056/NEJM198109033051006. [DOI] [PubMed] [Google Scholar]
- Cram JR, Kasman CS. Introduction to surfac electromyography. Gaithersburg: Aspen; 1998. [Google Scholar]
- Deniskina IV, Levik YS, et al. Relative Roles of the Ankle and Hip Muscles in Human Postural Control in the Frontal Plane during Standing. Human Physiology. 2001;27(3):317–321. [Google Scholar]
- Felson DT, Niu J, et al. Effect of recreational physical activities on the development of knee osteoarthritis in older adults of different weights: the Framingham Study. Arthritis Rheum. 2007;57(1):6–12. doi: 10.1002/art.22464. [DOI] [PubMed] [Google Scholar]
- Ferguson RH, Mayhew JL. Validation of a 7–10-RM Bench Press Test to Predict Maximum Bench Press Strength. Medicine & Science in Sports & Exercise. 2004;36(5):S353. [Google Scholar]
- Fisher NM, White SC, et al. Muscle function and gait in patients with knee osteoarthritis before and after muscle rehabilitation. Disabil Rehabil. 1997;19(2):47–55. doi: 10.3109/09638289709166827. [DOI] [PubMed] [Google Scholar]
- Fraioli F, Moretti C, et al. Physical exercise stimulates marked concomitant release of beta-endorphin and adrenocorticotropic hormone (ACTH) in peripheral blood in man. Experientia. 1980;36(8):987–989. doi: 10.1007/BF01953837. [DOI] [PubMed] [Google Scholar]
- Hakkinen K, Kallinen M, et al. Neuromuscular adaptations during short-term “normal” and reduced training periods in strength athletes. Electromyogr Clin Neurophysiol. 1991;31(1):35–42. [PubMed] [Google Scholar]
- Hochberg MC, Altman RD, et al. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum. 1995;38(11):1541–1546. doi: 10.1002/art.1780381104. [DOI] [PubMed] [Google Scholar]
- Jan MH, Lin JJ, et al. Investigation of clinical effects of high- and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial. Phys Ther. 2008;88(4):427–436. doi: 10.2522/ptj.20060300. [DOI] [PubMed] [Google Scholar]
- Jenkinson CM, Doherty M, et al. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ. 2009;339:b3170. doi: 10.1136/bmj.b3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato S, Urabe Y, et al. Alignment control exercise changes lower extremity movement during stop movements in female basketball players. The Knee. 2008;15(4):299–304. doi: 10.1016/j.knee.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Marks R. The effect of isometric quadriceps strength training in mid-range for osteoarthritis of the knee. Arthritis Care Res. 1993;6(1):52–56. doi: 10.1002/art.1790060110. [DOI] [PubMed] [Google Scholar]
- Maurer BT, Stern AG, et al. Osteoarthritis of the knee: isokinetic quadriceps exercise versus an educational intervention. Arch Phys Med Rehabil. 1999;80(10):1293–1299. doi: 10.1016/s0003-9993(99)90032-1. [DOI] [PubMed] [Google Scholar]
- Messier SP, Loeser RF, et al. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992;73:29–35. [PubMed] [Google Scholar]
- Mikesky AE, Mazzuca SA, et al. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55(5):690–699. doi: 10.1002/art.22245. [DOI] [PubMed] [Google Scholar]
- Minor MA. Exercise in the treatment of osteoarthritis. Rheumatic Disease Clinics of North America. 1999;25:397–414. doi: 10.1016/s0889-857x(05)70075-2. [DOI] [PubMed] [Google Scholar]
- Minor MA, LNE . Recreational exercise in arthritis. Philadelphia: W.B. Saunders; 1996. [DOI] [PubMed] [Google Scholar]
- Myers RS. Saunders Manual of Physical Therapy Practice. Philadelphia, PA: WB Saunders Co; 1995. [Google Scholar]
- Pearle AD, Warren RF, et al. Basic science of articular cartilage and osteoarthritis. Clin Sports Med. 2005;24(1):1–12. doi: 10.1016/j.csm.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Pereira MP, Goncalves M. Muscular coactivation (CA) around the knee reduces power production in elderly women. Arch Gerontol Geriatr. 2010 doi: 10.1016/j.archger.2010.04.024. [DOI] [PubMed] [Google Scholar]
- Riener R, Straube A. Inverse dynamics as a tool for motion analysis: arm tracking movements in cerebellar patients. J Neurosci Methods. 1997;72(1):87–96. doi: 10.1016/s0165-0270(96)02168-1. [DOI] [PubMed] [Google Scholar]
- Roddy E, Zhang W, et al. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis. 2005;64(4):544–548. doi: 10.1136/ard.2004.028746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogind H, Bibow-Nielsen B, et al. The effects of a physical training program on patients with osteoarthritis of the knees. Arch Phys Med Rehabil. 1998;79(11):1421–1427. doi: 10.1016/s0003-9993(98)90238-6. [DOI] [PubMed] [Google Scholar]
- Roos EM, Roos HP, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- Segal NA, Torner JC, et al. Knee Extensor Strength Does Not Protect Against Incident Knee Symptoms at 30 Months in the Multicenter Knee Osteoarthritis (MOST) Cohort. PM&R. 2009;1(5):459–465. doi: 10.1016/j.pmrj.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma L. Examination of exercise effects on knee osteoarthritis outcomes: why should the local mechanical environment be considered? Arthritis Rheum. 2003;49(2):255–260. doi: 10.1002/art.11006. [DOI] [PubMed] [Google Scholar]
- Sharma L, Dunlop DD, et al. Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med. 2003;138(8):613–619. doi: 10.7326/0003-4819-138-8-200304150-00006. [DOI] [PubMed] [Google Scholar]
- Sharma L, Hurwitz DE, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41(7):1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Sharma L, Song J, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- Sothmann MS, Gebhardt DL, et al. Performance requirements of physically strenuous occupations: validating minimum standards for muscular strength and endurance. Ergonomics. 2004;47(8):864–875. doi: 10.1080/00140130410001670372. [DOI] [PubMed] [Google Scholar]
- Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37(3):579–587. doi: 10.1177/0363546508326711. [DOI] [PubMed] [Google Scholar]
- Sturnieks DL, Besier TF, et al. Knee strength and knee adduction moments following arthroscopic partial meniscectomy. Med Sci Sports Exerc. 2008;40(6):991–997. doi: 10.1249/MSS.0b013e318167812a. [DOI] [PubMed] [Google Scholar]
- Thorstensson CA, Henriksson M, et al. The effect of eight weeks of exercise on knee adduction moment in early knee osteoarthritis--a pilot study. Osteoarthritis Cartilage. 2007;15(10):1163–1170. doi: 10.1016/j.joca.2007.03.012. [DOI] [PubMed] [Google Scholar]
- van Baar ME, Dekker J, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol. 1998;25(12):2432–2439. [PubMed] [Google Scholar]