Abstract
Basal and forced swimming (FS) stress-induced release of noradrenaline (NA) and serotonin (5-HT) were determined by in vivo microdialysis in the ventral hippocampus of mice overexpressing galanin under the platelet-derived growth factor B promoter (GalOE/P) or under the dopamine β-hydroxylase promoter (GalOE/D) (only NA). WT mice served as controls. Intraventricular infusion of galanin significantly reduced basal extracellular NA in WT mice and in GalOE/P mice (albeit less so). Microdialysis sampling during a 10-min FS showed that NA and 5-HT release were elevated to 213% and 156%, respectively, in the GalOE/P group, whereas in the WT group the increases were only 127% and 119%, respectively. The second (repeated) 10-min FS (RFS) caused a marked enhancement of NA and 5-HT release in the GalOE/P mice to 344% and 275%, respectively. However, the RFS caused only a 192% increase of extracellular NA levels in the GalOE/D mice. Pretreatment with the putative peptidergic galanin receptor antagonist M35 almost completely blocked the elevation of NA and 5-HT levels in the GalOE/P after RFS. These results suggest that the NA and 5-HT hippocampal afferents in GalOE/P mice are hypersensitive to both conditioned and unconditioned stressful stimuli, such as FS, and that this effect is mediated by galanin receptors. The present findings support a role of galanin in the regulation of release of NA and 5-HT, two neurotransmitters involved in mood control.
Keywords: microdialysis, 5-hydroxytryptamine, transgenic mice, hippocampus, affective disorders
Galanin, a 29-aa (30 in human) neuropeptide (1), is widely distributed throughout the central nervous system (2, 3), where it coexists with several classic neurotransmitters (4). A similarly widespread distribution of galanin-like immunoreactivity (LI) in neurons and fibers was observed in the brain of the mouse (5). Three galanin receptor subtypes (GalR1–GalR3) have been cloned (see refs. 6 and 7), all belonging to the 7-transmembrane, G protein-coupled receptor superfamily. Both the noradrenaline (NA) neurons of locus coeruleus (LC) and the 5-hydroxytryptamine (5-HT) neurons of the dorsal raphe nucleus (DRN) (8) can synthesize galanin (4, 9–11). In the rat brain, galanin-LI can be observed in the terminal ramifications of the NA nerve terminals in cortical/hippocampal areas (11). However, it has been more difficult to demonstrate galanin-LI in 5-HT terminals, suggesting a higher galanin expression in the NA than in the 5-HT system.
Recently, mice with a targeted disruption of the galanin gene (12), or overexpressing galanin under the dopamine β-hydroxylase (DβH) promoter (GalOE/D) (13, ††) or the platelet-derived growth factor B promoter (GalOE/P) (14, ‡‡), have been generated and characterized with regard to several functional parameters (see refs. 15 and 16).
In vivo microdialysis studies on rats have suggested that galanin plays an important role in modulation of 5-HT (17) and NA (18) neurotransmission, supporting a possible role of galanin in mood control, anxiety, and stress responses, as proposed earlier (19–27).
A recently developed, ultra-sensitive chromatographic method allows detection of basal levels of NA (28) and 5-HT (29) in the ventral hippocampus of awake mice with microdialysis (30). The main aim of the present study, using this methodology, was to monitor extracellular hippocampal NA and 5-HT levels in GalOE and WT mice after exposure to repeated swim stress used as a model to examine the putative role of galanin in affective behavior.
Materials and Methods
Chemicals and Reagents. Chemicals and reagents were obtained from Sigma, Tokyo Kasei Kogyo, Merck, or Peninsula Laboratories. The derivatization reagent for NA and 5-HT determination was prepared daily as described (17, 28, 30). Typically, 15 μl of standard solution or 15 μl of a microdialysis sample were mixed with 15 μl of the derivatization reagent and heated. Then a 20-μl portion of the final reaction mixture was injected onto the chromatographic column. As a reagent blank, distilled water and artificial cerebrospinal fluid (aCSF) were subjected to the same procedure.
Instrumentation. Determination of NA and 5-HT by liquid chromatography was performed as described elsewhere (28–30). The chromatograms were recorded and integrated by use of a computerized data acquisition system CP-Maitre I/II (Chrompac International). A CMA/120 system for microdialysis on awake animals consisted of a round cage and a counterbalance arm with a dual-channel swivel (TSC-23, BASJ). A CMA/100 microinjection pump and a CMA/170 refrigerated fraction collector were used for constant flow delivery and automated collection of samples.
Animals. Ten-month-old male and female GalOE/P mice (birth weight, 31–45 g) were generated at the Karolinska Institute as described (14, ‡‡), and the line was back-crossed for >10 generations and bred into a C57BL genetic background. Male, 11-month-old GalOE/D mice (birth weight, 32–42 g) (13), originally generated at the University of Washington, back-crossed for more than seven generations and bred into a C57BL/6J genetic background, were used in some experiments. The microdialysis experiments were performed between 9 a.m. and 4 p.m. All animal experiments followed the general recommendations of Swedish animal protection legislation and were approved by the Animal Ethics Committee of North Stockholm, Sweden.
Stereotaxic Operations. Mice were anaesthetized with sodium pentobarbital and placed in a Kopf stereotaxic frame, and the body temperature was maintained at 37°C during the operation. Holes (0.7 mm in diameter) were drilled for the microdialysis and the intracerebroventricular (i.c.v.) injection guide cannulas and for two fixing microscrews, which were cemented to the skull. The CMA/7 guide cannula with a dummy was implanted into the right ventral hippocampus (anterior-posterior, -3.0; lateral, +3.0; ventral, -1.8 mm from bregma), and the injection cannula was implanted into the right lateral ventricle (anterior-posterior, -0.1; lateral, +0.9; ventral, -1.8 mm from bregma) (31).
Microdialysis and Behavior. After recovery (5–7 days), the animals were placed in the CMA/120 system for freely moving animals equipped with a two-channel swivel for an initial 2-h habituation period. The CMA/7 microdialysis probe (2-mm membrane length) was inserted into the guide cannula and perfused at a constant flow rate of 1 μl/min with aCSF. In the initial experiment, after a 120-min stabilization period, six microdialysis samples were collected for estimation of basal extracellular NA and 5-HT levels; thereafter, galanin (1 nmol per 0.5 μl per min) was infused i.c.v., and the additional six 20-min fractions were collected. In separate experiments, the mice were exposed to a repeated 10-min forced swimming test with concurrent collection of the microdialysis samples. After initial stabilization, the mice were infused with M35 or aCSF i.c.v., 90 min before the start of the swim trial, while the basal microdialysis samples were collected in 10-min intervals. Then, each mouse was gently transferred to a glass cylinder, which was filled with water at 24°C. During swimming, the swivel was rotated manually. An additional 10-min forced-swimming stress (RFS) was performed 120 min later in a manner similar to the first trial, and the microdialysates were collected for an additional 60-min period.
Statistical Analysis. The basal levels of NA and 5-HT in all groups were calculated as means of the three fractions collected before the drug/aCSF administration or during FS or RFS. The values (mean ± SEM) in graphs are expressed as percentage of the basal (control) levels. A repeated-measures two-way ANOVA and a Fisher's probable least-squares difference test were used to analyze statistically significant differences between the groups, and for differences within the same group, a paired t test was used. A level of P < 0.05 was regarded as a statistically significant effect.
Immunohistochemistry. The mice were deeply anaesthetized with pentobarbital and perfused through the ascending aorta with formalin-picric acid fixative (32). After postfixation, the tissues were rinsed, cut in a cryostat, and processed according to the highly sensitive tyramide signal amplification plus immunohistochemical method (33) by using a commercial kit (NEN). Briefly, sections were incubated with rabbit antiserum to rat galanin (34), rinsed, incubated with horseradish peroxidase-labeled porcine anti-rabbit IgG, rinsed, incubated with fluorophore tyramide Tris-NaCl-blocking reagent (NEN), rinsed again, and finally mounted and examined by using a Nikon Eclipse E600 microscope equipped with epifluorescence and appropriate filter combinations.
Results
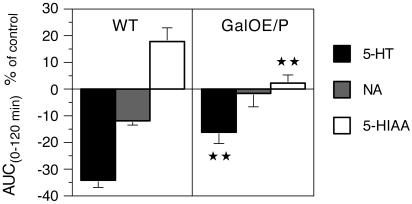
Effect of Exogenous Galanin on Hippocampal NA and 5-HT Release. In WT mice, the basal concentrations of extracellular NA, 5-HT, and 5-hydroxyindoleacetic acid (5-HIAA) were 3.02 ± 1.18, 2.68 ± 1.33, and 551.4 ± 42.4, respectively (expressed in fmol per 10 μl, mean ± SEM, n = 9). In the GalOE/P mice, the corresponding basal levels were 2.84 ± 1.14, 2.55 ± 1.36, and 532 ± 47.1 for NA, 5-HT, and 5-HIAA, respectively, and in the GalOE/D mice, the basal concentrations of NA were 5.22 ± 0.05 (all expressed in fmol per 10 μl, mean ± SEM, n = 5–9). There were no significant differences in basal NA and 5-HT levels between the WT and GalOE/P groups, and the i.c.v. infusion of aCSF failed to alter basal NA and 5-HT concentrations (data not shown). Infusion of porcine galanin (1 nmol per 0.5 μl per min, i.c.v.) caused a gradual, time-dependent reduction of basal NA and 5-HT levels in both WT and GalOE/P mice. At the end of the experiment (120 min), the NA values were reduced by 30% of the baseline levels in the WT and by 7% in the GalOE/P mice (F1,8 = 12.23, P < 0.01). The corresponding results for 5-HT were 44% and 19% (F1,8 = 11.62, P < 0.01), respectively. Fig. 1 shows the data expressed as area under the curve [AUC(0–120 min)] values, calculated from six 20-min microdialysis samples collected after galanin injection. There was a significant difference between the AUC levels for 5-HT and 5-HIAA in the WT vs. GalOE/P mice. The galanin-induced reduction of 5-HT in the WT mice (AUC value of -34%) was in the GalOE/P mice attenuated to -16% only (P < 0.01). A similar effect was observed for 5-HIAA levels, where the AUC value was attenuated from 18% to 2% in the respective groups (P < 0.01).
Fig. 1.
Infusion of porcine galanin (1 nmol per 0.5 μl per min i.c.v.) caused a gradual decrease of basal extracellular 5-HT and NA levels in the hippocampus of both WT and GalOE/P mice, measured over a period of 120 min. However, the 5-HT levels were reduced to a higher extent in the WT than in the GalOE/P mice, whereas the 5-HIAA concentrations were higher in the WT group. There was a significant difference between the AUC(0–120 min) values for 5-HT and 5-HIAA in the GalOE/P mice (⋆⋆, P < 0.01) compared with the WT mice. In control experiments, the i.c.v. infusion of aCSF failed to alter basal NA and 5-HT concentrations (data not shown).
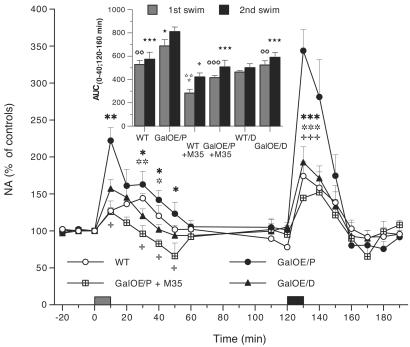
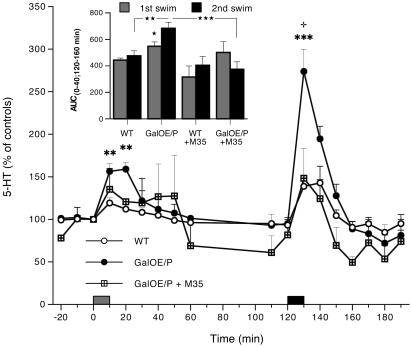
Effects of FS and RFS Stressors on NA and 5-HT Release. FS caused an immediate increase in hippocampal NA and 5-HT release in both WT and GalOE/P mice (Figs. 2 and 3). Insets in Figs. 2 and 3 show the AUC values after the first and second swim trials (FS and RFS), corresponding to the periods of 0–40 min and 120–160 min, respectively (F11,44 = 10.75, P < 0.001 for NA; F7,24 = 5.8, P < 0.001 for 5-HT groups). In GalOE/P mice (n = 5), the maximal increase of NA and 5-HT in the first swim was to 213% and 156%, respectively, and during the second swim to 344% and 275%, respectively. In the WT group (n = 5), the corresponding values for NA were 127% and 174% for the first and second swim trials, respectively, and for 5-HT the corresponding values were 119% and 139%. The differences between WT and GalOE/P mice were significant already during the first FS stress both for NA and 5-HT and highly significant during the RFS stress. Within the group, analysis (paired t test) in the GalOE/P mice revealed that the effects of the RFS at 130 min on NA and 5-HT release were significantly different from the maximal effects of the first swim trial (P < 0.05 for NA and P < 0.01 for 5-HT). In GalOE/D mice (n = 5), the effects of FS stress on hippocampal NA release were moderate (Fig. 2), with a maximal increase during the RFS trial only to 147% and 192% in the WT (data not shown) and GalOE/D mice, respectively. There were significant differences in stress-induced NA levels between the GalOE/P and GalOE/D mice (P < 0.05 to P < 0.002). In all groups, the NA and 5-HT levels returned to normal within 50–60 min after each stress period. The AUC values (Insets in Figs. 2 and 3) confirm the results from analysis of individual time points for NA and 5-HT. The AUC for NA after FS was significantly higher in the GalOE/P mice than in the WT and GalOE/D mice (P < 0.01). The RFS caused a significant increase in AUC of NA in GalOE/P as compared to FS in the same group (P < 0.05) and also compared to the AUC values after RFS in the WT and GalOE/D mice, respectively (P < 0.001). The AUC values of 5-HT in GalOE/P mice (Fig. 3 Inset) after RSF were significantly higher than in the first swim (P < 0.05) and in WT mice (P < 0.05).
Fig. 2.
The effect of repeated 10-min swim stress on NA release in the hippocampus of WT and galanin-overexpressing mice. FS and, even more profoundly, RFS caused a marked increase in NA release in GalOE/P mice, which was significantly higher than the stress-induced NA release in the WT mice (*, P < 0.05; **, P < 0.01; ***, P < 0.002, n = 5) and the GalOE/D mice ( , P < 0.05;
, P < 0.05; 
 , P < 0.01;
, P < 0.01; 

 , P < 0.002, n = 5). The galanin antagonist M35 given i.c.v. to GalOE/P mice significantly attenuated the elevation of NA levels induced by both FS and RFS stressors (
, P < 0.002, n = 5). The galanin antagonist M35 given i.c.v. to GalOE/P mice significantly attenuated the elevation of NA levels induced by both FS and RFS stressors ( , P < 0.05;
, P < 0.05; 

 , P < 0.001, n = 4–5). After FS, the AUC for NA in the GalOE/P mice was significantly higher than in the WT and GalOE/D mice (
, P < 0.001, n = 4–5). After FS, the AUC for NA in the GalOE/P mice was significantly higher than in the WT and GalOE/D mice (
 , P < 0.01, n = 5), whereas M35 completely abolished the stress effects induced by FS (
, P < 0.01, n = 5), whereas M35 completely abolished the stress effects induced by FS (

 , P < 0.001) and RFS (⋆⋆⋆, P < 0.001) in GalOE/P mice (Inset). M35 given to WT mice significantly reduced the AUC for NA (
, P < 0.001) and RFS (⋆⋆⋆, P < 0.001) in GalOE/P mice (Inset). M35 given to WT mice significantly reduced the AUC for NA (

 , P < 0.001;
, P < 0.001;  , P < 0.05; n = 5). The RFS caused a significant increase in AUC of NA in GalOE/P as compared to FS in the same group (⋆, P < 0.05) and compared to the AUC values after RFS in the WT and GalOE/D mice, respectively (⋆⋆⋆, P < 0.001).
, P < 0.05; n = 5). The RFS caused a significant increase in AUC of NA in GalOE/P as compared to FS in the same group (⋆, P < 0.05) and compared to the AUC values after RFS in the WT and GalOE/D mice, respectively (⋆⋆⋆, P < 0.001).
Fig. 3.
The effect of repeated 10-min swim stress on 5-HT release in the hippocampus of WT and GalOE/P mice. FS and, even more profoundly, RFS caused significantly higher increase in 5-HT release in GalOE/P mice than in the WT mice (**, P < 0.01; ***, P < 0.002, n = 5), as also was confirmed by the AUC values (⋆⋆, P < 0.01) (Inset). The effect of RFS stress on 5-HT levels was almost completely blocked by the galanin antagonist M35 (+, P < 0.05, n = 3–5) at 130 min [★★★, P < 0.001 for the AUC(120–160 min) values].
Effect of M35 on Swim Stress-Induced Increase in NA and 5-HT Release. In GalOE/P mice pretreated with the galanin antagonist M35 (1 nmol per 0.5 μl per min i.c.v.) 90 min before the first 10-min FS stress, the elevation of NA was significantly attenuated at the peak effects of both swims (FS: F1,6 = 18.964, P < 0.01; RFS: F1,6 = 47.114, P < 0.001). The AUC values for NA in WT mice were significantly attenuated by M35 at both FS (P < 0.001) and RFS (P < 0.05) and in the GalOE/P mice after RFS (P < 0.001) (Fig. 2 Inset). Similarly, increased 5-HT release after RFS in GalOE/P mice was attenuated by pretreatment with M35 as shown in Fig. 3 at the peak effect (F1,6 = 8.485, P < 0.05), as well as for the AUC levels (P < 0.001) (Fig. 3 Inset).
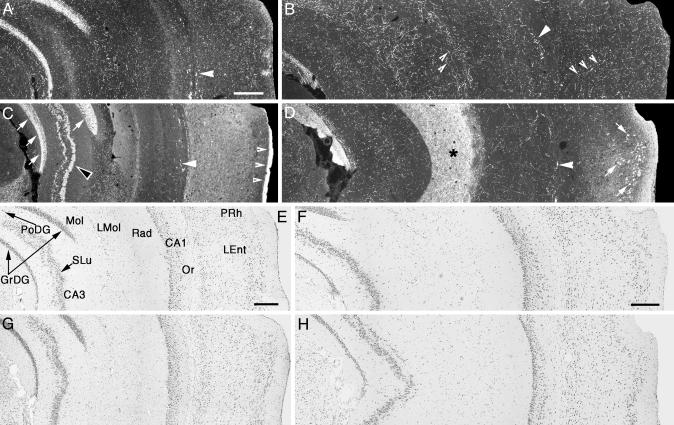
Immunohistochemical Analysis. In both types of WT mice (Figs. 4 A and B and 5 A and B) and in the GalOE/D mouse (Figs. 4D and 5D), a moderately dense galanin-positive fiber plexus was observed in all hippocampal layers and cortical regions with a similar density in both strains. A low number of strongly fluorescent fibers in the ventral CA1 stratum oriens of all mice (Figs. 4 A–D and 5). There was a galanin-immunoreactive band of varying intensity in the supragranular layer of the dentate gyrus (Fig. 4A), with some cell bodies in the polymorph layer of both WT mice. The GalOE/D mouse, in addition, expressed a strong diffuse galanin-LI in strata moleculare and lacunosum and in many strongly fluorescent cell bodies in laminae II/III of the entorhinal cortex (Fig. 4D). In the GalOE/P mouse, a distinctly different pattern was observed with a strongly immunoreactive granular cell layer, mossy fibers, and cells in the polymorph layer (Fig. 4C). However, the moderately dense, widely distributed galanin plexus was almost absent (compare Fig. 5C with A, B, and D), whereas the strongly fluorescent fibers in stratum oriens remained. Galanin-LI could not be seen in LC or DRN cell bodies of untreated WT, GalOE/P, or GalOE/D mice (not shown). However, in the LC, but not in the DRN, strong galanin-LI was seen in the cell bodies after colchicine (not shown). None of the fluorescent structures described above was observed after incubation with control serum (not shown).
Fig. 4.
Immunofluorescence (A–D) and brightfield (E–H) micrographs of the hippocampal formation and cortex of WT/P (A and E), WT/D (B and F), GalOE/P (C and G), and GalOE/D (D and H) mice after incubation with galanin antiserum (A–D) or staining with cresyl violet (E–H). E–H show adjacent or semiadjacent sections to A–D, respectively. The various layers in the hippocampal formation and cortex are indicated in E.(A and B) A moderately dense galanin fiber network is seen in most layers in the WT mice (small arrowheads). Big arrowheads show strongly fluorescent fibers in stratum oriens. Note fluorescence in supragranular layer in A.(C) In the GalOE/P mouse, a strong galanin-LI can be seen in the granule cell layer (arrows) and in the mossy fibers (black arrowhead). Big arrowheads indicate strong fibers in stratum oriens, and small arrowheads indicate strong fluorescence in the superficial layer of the entorhinal cortex. Note that the moderately dense fiber network cannot be seen any longer. (D) Strong fluorescence is seen in the molecular layer and stratum lacunosum-moleculare (asterisk). Also note cell bodies in laminae II/III of the entorhinal cortex (arrows). Arrowheads show strongly fluorescent terminals in stratum oriens. CA1 and CA3, CA1 and CA3 pyramidal cell layers, respectively; GrDG, granule cell layer; LEnt, lateral entorhinal cortex; LMol, stratum lacunosum moleculare; Mol, molecular layer; Or, stratum oriens; PoDG, polymorph cell layer; PRh, perirhinal cortex; Rad, stratum radiatum; SLu, stratum lucidum. [Each bar indicates 200 μm (A for B–D; E for G; F for H).]
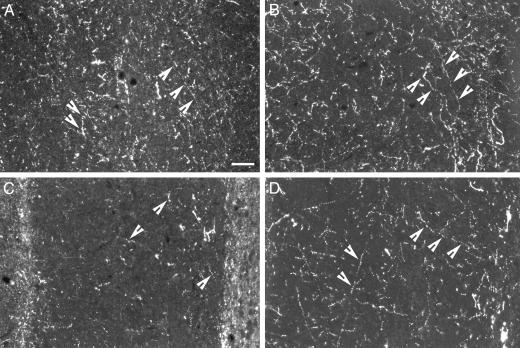
Fig. 5.
Immunofluorescence micrographs of the ventral hippocampal formation of WT/P (A), WT/D (B), GalOE/P (C), and GalOE/D (D) mice after incubation with galanin antiserum. Arrowheads indicate galanin-positive, presumably noradrenergic fibers forming a plexus of medium density (A, B, and D). Note that this immunoreactivity is almost absent in the GalOE/P mouse (C). (Bar = 100 μm for all micrographs.)
Discussion
Our microdialysis data collected from mice during FS stress, used as a model of learned helplessness, confirm previous observations in rats and especially in mice that sensory stimulation or a mild stressor increases hippocampal NA and 5-HT release (35–38). Moreover, our study indicates that the GalOE/P mice, but much less so the GalOE/D mice, respond more strongly to swim stress than the corresponding WT mice, as suggested by markedly higher levels of extracellular NA and 5-HT, especially during the second swim stress session. This effect was blocked by the putative galanin antagonist M35 (see ref. 39). The reason for the distinct difference in stress-induced NA release between GalOE/P and WT and even GalOE/D mice is not easily explained, but it may be due to a differential expression of galanin in the two groups of mice. Based on present histochemical analysis, a major difference between the two groups tested was the observation of low galanin immunoreactivity in the diffuse, likely noradrenergic fiber network in the GalOE/P mouse, whereas WT and GalOE/D mice had a strong network. This suggests that either galanin synthesis in the LC neurons is compromised/attenuated in the GalOE/P mice or that there is increased galanin release. The latter seems less likely, as galanin mRNA levels in LC are not increased in these mice (unpublished results). It may be speculated that high galanin levels in cortex/hippocampal formation of the GalOE/P mice, via a feedback mechanism, reduce galanin synthesis in the LC cell bodies. A second difference was the widespread ectopic expression of galanin in hippocampus and cortex of the GalOE/P mouse, whereas in the GalOE/D mouse this was confined to the entorhinal cortex/stratum lacunosum-moleculare/molecular layer. Another issue is to what extent galanin receptor expression is changed and different between the WT, GalOE/P, and GalOE/D mice. It has been reported that GalR1 mRNA levels are higher in some brain areas of the GalOE/D mouse as compared to the corresponding regions of the WT mouse (40). Thus, it will be important to monitor galanin receptor levels in the mice strains under the same conditions as studied here. Finally, to be considered for future studies is the differential expression of galanin in the GalOE/P and GalOE/P in the amygdala, another brain region that mediates stress responses.
In the rat, galanin has been shown to exert an inhibitory effect on LC neurons (41), presumably mainly via GalR1 receptors (42). Because in the rat galanin-injected i.c.v., but not directly into hippocampus, inhibits NA release in the hippocampus (43), it seems likely that the inhibition of NA release by exogenous galanin shown in the present experiments is via an effect at NA neurons in the LC. If then galanin expression is compromised in the GalOE/P mouse, this may lead to a deficient inhibition of LC neurons by endogenous galanin, resulting in a more pronounced NA release after swim stress in the GalOE/P mouse as compared to the WT and GalOE/D mouse.
Presynaptic effects of galanin should also be considered. Galanin has been shown to, presynaptically, inhibit potassium-induced NA release from slices from the hypothalamus and medulla oblongata (44, 45), an effect perhaps mediated via GalR1. Therefore, endogenous galanin concomitantly released with NA from hippocampal terminals in the WT mouse could presumably also attenuate NA release. However, this inhibition will not occur at these terminals of the GalOE/P mouse because of low galanin levels, resulting in a strong NA release. This and the previous hypothesis of an inhibitory effect of galanin on the NA cell bodies are consistent with the comparatively small FRS-induced release of NA in the GalOE/D mouse, which has high galanin levels in the LC system due to the overexpression under the DβH promoter (see ref. 16). This is also in agreement with increased galanin expression after stress (20, 46, 47). The concept (see ref. 48) that a coexisting peptide like galanin is preferentially released, when neurons are firing at a high rate or during burst firing, may likely be valid also for the LC neurons during FS and especially RFS stress.
Furthermore, the possible presence of GalR2 receptors on nerve terminals should be considered. In the rat, GalR2 receptors are expressed in LC neurons (42), but local application of a selective GalR2 agonist has no membrane effects on LC neurons (49), suggesting that the GalR2 is presynaptic. GalR2 is known to activate phospholipase C (50), increasing Ca2+ influx and possibly enhancing transmitter release. In the GalOE/P mouse, galanin is synthesized in many local hippocampal neurons, and FS and RFS may activate these neurons to release galanin, which via presynaptic GalR2 could heterosynaptically enhance NA release. It is possible that the blockade of the FRS-induced NA release from hippocampal terminals by M35 is mediated via an effect on such presynaptic GalR2.
Galanin and 5-HT represents an even more complicated situation. Thus, DRN 5-HT neurons seem to lack galanin, as well as the GalR1 receptor (51), a clear species difference when compared to the rat. Here, we confirm that DRN neurons also in GalOE mouse transgenes and our WTs lack galanin expression. At present, we have no simple explanation for the enhanced 5-HT release in the GalOE/P vs. WT mouse after FRS. Should the DRN in the GalOE/P mouse neurons express GalR2, then a similar mechanism may exist as hypothesized for LC neurons: a locally released, overexpressed galanin could enhance 5-HT release via presynaptic GalR2 receptors.
Concluding Remarks
The present and earlier results suggest that galanin, a neuropeptide that coexists with NA in most LC neurons, is an important modulator of NA release under stressful conditions. The behavioral consequences of such a modulation are still an open question. It has been proposed that i.c.v. galanin has an anxiolytic effect (19), whereas galanin given into the amygdala has an “anxiogenic-like action” (25). The present GalOE/P mice show increased floating behavior in the forced swim test compared to WT mice,§§ suggesting low stress tolerance and increased “depressive behavior.” Is this behavior related to the apparently deficient galanin expression in the LC NA neurons or to the increased expression in many other neuronal systems of the GalOE/P mice? Furthermore, the GalOE/D showed normal anxiolytic-like behaviors and responses to chlordiazepoxide on anxiety-related tasks, but less pro-anxiety-like response to yohimbine, as compared to WT littermate controls (52). Because galanin is localized in many brain areas, coexisting with different types of classic transmitters in multiple systems, it is at present difficult to ascribe a single function for galanin in relation to mood control. Further neurochemical and behavioral analysis of the GalOE/P mouse are clearly needed to understand the possible role of galanin in mood control.
Acknowledgments
This work was supported by grants from the Karolinska Institutet, Swedish Research Council, and the Marianne and Marcus Wallenberg Foundation. T.Y. was supported by the Swedish Foundation for International Cooperation in Research and Higher Education, STINT. J.N.C. was supported by the National Institute of Mental Health Intramural Research Program.
Abbreviations: aCSF, artificial cerebrospinal fluid; AUC, area under the curve; DRN, dorsal raphe nucleus; FS, forced swimming; GalOE/D, overexpressing galanin under the dopamine β-hydroxylase promoter; GalOE/P, overexpressing galanin under the platelet-derived growth factor B promoter; 5-HIAA, 5-hydroxyindoleacetic acid; 5-HT, 5-hydroxytryptamine or serotonin; i.c.v., intracerebroventricular(ly); LC, locus coeruleus; LI, like immunoreactivity; NA, noradrenaline; RFS, repeated FS.
Footnotes
Hohmann, J. G., Cadd, G. C., Teal, T. H., Clifton, D. K. & Steiner, R. A. (1997) Soc. Neurosci. Abstr. 23, 1878 (abstr.).
Holmberg, K., Kahl, U., Lendahl, U., Kokaia, Z., Nanobashvili, A., Lindvall, O., Ekström, P., Bartfai, T. & Hökfelt, T. (2000) Soc. Neurosci. Abstr. 26, 27 (abstr.).
Kuteeva, E., Kehr, J., Yoshitake, T., Wang, F. H., Holmberg, K., Calzà, L., Ögren, S.-O. & Hökfelt, T. (2003) Sixth IBRO World Congress of Neuroscience, July 10–15, Prague, 94 (abstr.).
References
- 1.Tatemoto, K., Rökaeus, Å., Jörnvall, H., McDonald, T. J. & Mutt, V. (1983) FEBS Lett. 164, 124-128. [DOI] [PubMed] [Google Scholar]
- 2.Skofitsch, G. & Jacobowitz, D. M. (1985) Peptides 6, 509-546. [DOI] [PubMed] [Google Scholar]
- 3.Melander, T., Hökfelt, T. & Rökaeus, Å. (1986) J. Comp. Neurol. 248, 475-517. [DOI] [PubMed] [Google Scholar]
- 4.Melander, T., Hökfelt, T., Rökaeus, Å., Cuello, A. C., Oertel, W. H., Verhofstad, A. & Goldstein, M. (1986) J. Neurosci. 6, 3640-3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perez, S. E., Wynick, D., Steiner, R. A. & Mufson, E. J. (2001) J. Comp. Neurol. 434, 158-185. [DOI] [PubMed] [Google Scholar]
- 6.Branchek, T. A., Smith, K. E., Gerald, C. & Walker, M. W. (2000) Trends Pharmacol. Sci. 21, 109-117. [DOI] [PubMed] [Google Scholar]
- 7.Iismaa, T. P. & Shine, J. (1999) Results Probl. Cell Differ. 26, 257-291. [DOI] [PubMed] [Google Scholar]
- 8.Dahlström, A. & Fuxe, K. (1964) Acta Physiol. Scand. 62, Suppl. 232, 1-55. [PubMed] [Google Scholar]
- 9.Holets, V. R., Hökfelt, T., Rökaeus, Å., Terenius, L. & Goldstein, M. (1988) Neuroscience 24, 893-906. [DOI] [PubMed] [Google Scholar]
- 10.Jacobowitz, D. M. & Skofitsch, G. (1990) in Galanin: A New Multifunctional Peptide in the Neuro-Endocrine System, eds. Hökfelt, T., Bartfai, T., Jacobowitz, D. & Ottoson, D. (Macmillan, New York), Vol. 58, pp. 69-92. [Google Scholar]
- 11.Xu, Z. Q., Shi, T. J. & Hökfelt, T. (1998) J. Comp. Neurol. 392, 227-251. [DOI] [PubMed] [Google Scholar]
- 12.Wynick, D., Small, C. J., Bacon, A., Holmes, F. E., Norman, M., Ormandy, C. J., Kilic, E., Kerr, N. C., Ghatei, M., Talamantes, F., et al. (1998) Proc. Natl. Acad. Sci. USA 95, 12671-12676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steiner, R. A., Hohmann, J. G., Holmes, A., Wrenn, C. C., Cadd, G., Jureus, A., Clifton, D. K., Luo, M., Gutshall, M., Ma, S. Y., et al. (2001) Proc. Natl. Acad. Sci. USA 98, 4184-4189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kokaia, M., Holmberg, K., Nanobashvili, A., Xu, Z. Q., Kokaia, Z., Lendahl, U., Hilke, S., Theodorsson, E., Kahl, U., Bartfai, T., et al. (2001) Proc. Natl. Acad. Sci. USA 98, 14006-14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wynick, D. & Bacon, A. (2002) Neuropeptides 36, 132-144. [DOI] [PubMed] [Google Scholar]
- 16.Crawley, J. N., Mufson, E. J., Hohmann, J. G., Teklemichael, D., Steiner, R. A., Holmberg, K., Xu, Z. Q., Blakeman, K. H., Xu, X. J., Wiesenfeld-Hallin, Z., et al. (2002) Neuropeptides 36, 145-156. [DOI] [PubMed] [Google Scholar]
- 17.Kehr, J., Yoshitake, T., Wang, F. H., Razani, H., Gimenez-Llort, L., Jansson, A., Yamaguchi, M. & Ögren, S. O. (2002) Neuropsychopharmacology 27, 341-356. [DOI] [PubMed] [Google Scholar]
- 18.Khoshbouei, H., Cecchi, M., Dove, S., Javors, M. & Morilak, D. A. (2002) Pharmacol. Biochem. Behav. 71, 407-417. [DOI] [PubMed] [Google Scholar]
- 19.Bing, O., Moller, C., Engel, J. A., Soderpalm, B. & Heilig, M. (1993) Neurosci. Lett. 164, 17-20. [DOI] [PubMed] [Google Scholar]
- 20.Holmes, P. V., Blanchard, D. C., Blanchard, R. J., Brady, L. S. & Crawley, J. N. (1995) Pharmacol. Biochem. Behav. 50, 655-660. [DOI] [PubMed] [Google Scholar]
- 21.Milot, M. & Trudeau, F. (1997) Physiol. Behav. 62, 697-700. [DOI] [PubMed] [Google Scholar]
- 22.Fuxe, K., Jansson, A., Diaz-Cabiale, Z., Andersson, A., Tinner, B., Finnman, U. B., Misane, I., Razani, H., Wang, F. H., Agnati, L. F. & Ögren, S. O. (1998) Ann. N.Y. Acad. Sci. 863, 274-290. [DOI] [PubMed] [Google Scholar]
- 23.Ögren, S. O., Schott, P. A., Kehr, J., Yoshitake, T., Misane, I., Mannstrom, P. & Sandin, J. (1998) Ann. N.Y. Acad. Sci. 863, 342-363. [DOI] [PubMed] [Google Scholar]
- 24.Weiss, J. M., Bonsall, R. W., Demetrikopoulos, M. K., Emery, M. S. & West, C. H. (1998) Ann. N.Y. Acad. Sci. 863, 364-382. [DOI] [PubMed] [Google Scholar]
- 25.Möller, C., Sommer, W., Thorsell, A. & Heilig, M. (1999) Neuropsychopharmacology 21, 507-512. [DOI] [PubMed] [Google Scholar]
- 26.Sweerts, B. W., Jarrott, B. & Lawrence, A. J. (2000) Brain Res. 873, 318-329. [DOI] [PubMed] [Google Scholar]
- 27.Harro, J. & Oreland, L. (2001) Brain Res. Rev. 38, 79-128. [DOI] [PubMed] [Google Scholar]
- 28.Yamaguchi, M., Yoshitake, T., Fujino, K., Kawano, K., Kehr, J. & Ishida, J. (1999) Anal. Biochem. 270, 296-302. [DOI] [PubMed] [Google Scholar]
- 29.Ishida, J., Yoshitake, T., Fujino, K., Kawano, K., Kehr, J. & Yamaguchi, M. (1998) Anal. Chim. Acta 365, 227-232. [Google Scholar]
- 30.Kehr, J., Yoshitake, T., Wang, F. H., Wynick, D., Holmberg, K., Lendahl, U., Bartfai, T., Yamaguchi, M., Hökfelt, T. & Ögren, S. O. (2001) J. Neurosci. Methods 109, 71-80. [DOI] [PubMed] [Google Scholar]
- 31.Franklin, B. J. & Paxinos, G. (1997) The Mouse Brain in Stereotaxic Coordinates (Academic, San Diego).
- 32.Zamboni, I. & De Martino, C. (1967) J. Cell Biol. 35, 148. [Google Scholar]
- 33.Adams, J. C. (1992) J. Histochem. Cytochem. 40, 1457-1463. [DOI] [PubMed] [Google Scholar]
- 34.Theodorsson, E. & Rugarn, O. (2000) Scand. J. Clin. Lab. Invest. 60, 411-418. [DOI] [PubMed] [Google Scholar]
- 35.Abercrombie, E. D., Keller, R. W., Jr., & Zigmond, M. J. (1988) Neuroscience 27, 897-904. [DOI] [PubMed] [Google Scholar]
- 36.Vahabzadeh, A. & Fillenz, M. (1994) Eur. J. Neurosci. 6, 1205-1212. [DOI] [PubMed] [Google Scholar]
- 37.Jordan, S., Kramer, G. L., Zukas, P. K. & Petty, F. (1994) Neurochem. Res. 19, 1521-1525. [DOI] [PubMed] [Google Scholar]
- 38.Ihalainen, J. A., Riekkinen, P., Jr., & Feenstra, M. G. (1999) Neurosci. Lett. 277, 71-74. [DOI] [PubMed] [Google Scholar]
- 39.Bartfai, T., Fisone, G. & Langel, Ü. (1992) Trends Pharmacol. Sci. 13, 312-317. [DOI] [PubMed] [Google Scholar]
- 40.Hohmann, J. G., Jureus, A., Teklemichael, D. N., Matsumoto, A. M., Clifton, D. K. & Steiner, R. A. (2003) Neuroscience 117, 105-117. [DOI] [PubMed] [Google Scholar]
- 41.Pieribone, V., Xu, Z.-Q., Zhang, X., Grillner, S., Bartfai, T. & Hökfelt, T. (1995) Neuroscience 64, 861-874. [DOI] [PubMed] [Google Scholar]
- 42.O'Donnell, D., Ahmad, S., Wahlestedt, C. & Walker, P. (1999) J. Comp. Neurol. 409, 469-481. [PubMed] [Google Scholar]
- 43.Yoshitake, T., Reenila, I., Ögren, S. O., Hökfelt, T. & Kehr, J. (2003) Neurosci. Lett. 339, 239-242. [DOI] [PubMed] [Google Scholar]
- 44.Tsuda, K., Yokoo, H. & Goldstein, M. (1989) Hypertension 14, 81-86. [DOI] [PubMed] [Google Scholar]
- 45.Tsuda, K., Goldstein, M. & Masuyama, Y. (1990) Am. J. Hypertens. 3, 800-802. [DOI] [PubMed] [Google Scholar]
- 46.Sweerts, B. W., Jarrott, B. & Lawrence, A. J. (1999) Brain Res. Mol. Brain Res. 69, 113-123. [DOI] [PubMed] [Google Scholar]
- 47.O'Neal, H. A., Van Hoomissen, J. D., Holmes, P. V. & Dishman, R. K. (2001) Neurosci. Lett. 299, 69-72. [DOI] [PubMed] [Google Scholar]
- 48.Lundberg, J. M. & Hökfelt, T. (1983) Trends Neurosci. 6, 325-333. [Google Scholar]
- 49.Ma, X., Tong, Y. G., Schmidt, R., Brown, W., Payza, K., Hodzic, L., Pou, C., Godbout, C., Hökfelt, T. & Xu, Z. Q. (2001) Brain Res. 919, 169-174. [DOI] [PubMed] [Google Scholar]
- 50.Fathi, Z., Cunningham, A. M., Iben, L. G., Battaglino, P. B., Ward, S. A., Nichol, K. A., Pine, K. A., Wang, J., Goldstein, M. E., Iismaa, T. P. & Zimanyi, I. A. (1997) Brain Res. Mol. Brain. Res. 51, 49-59. [DOI] [PubMed] [Google Scholar]
- 51.Larm, J. A., Shen, P. J. & Gundlach, A. L. (2003) Eur. J. Neurosci. 17, 481-493. [DOI] [PubMed] [Google Scholar]
- 52.Holmes, A., Yang, R. J. & Crawley, J. (2002) J. Mol. Neurosci. 18, 151-165. [DOI] [PubMed] [Google Scholar]