Abstract
OBJECTIVE
The study objective was to evaluate the possible role of the macrophage molecule CD14 in insulin resistance.
RESEARCH DESIGN AND METHODS
The effects of recombinant human soluble CD14 (rh-sCD14) on insulin sensitivity (clamp procedure) and adipose tissue gene expression were evaluated in wild-type (WT) mice, high fat–fed mice, ob/ob mice, and CD14 knockout (KO) mice. We also studied WT mice grafted with bone marrow stem cells from WT donor mice and CD14 KO mice. Finally, CD14 was evaluated in human adipose tissue and during differentiation of human preadipocytes.
RESULTS
rh-sCD14 led to increased insulin action in WT mice, high-fat–fed mice, and ob/ob mice, but not in CD14 KO mice, in parallel to a marked change in the expression of 3,479 genes in adipose tissue. The changes in gene families related to lipid metabolism were most remarkable. WT mice grafted with bone marrow stem cells from WT donor mice became insulin resistant after a high-fat diet. Conversely, WT mice grafted with cells from CD14 KO mice resisted the occurrence of insulin resistance in parallel to decreased mesenteric adipose tissue inflammatory gene expression. Glucose intolerance did not worsen in CD14 KO mice grafted with bone marrow stem cells from high fat–fed WT mice when compared with recipient KO mice grafted with cells from CD14 KO donor mice. CD14 gene expression was increased in whole adipose tissue and adipocytes from obese humans and further increased after tumor necrosis factor-α.
CONCLUSIONS
CD14 modulates adipose tissue inflammatory activity and insulin resistance.
Insulin resistance and chronic, low-grade inflammation are important predisposing factors for the development of type 2 diabetes and atherosclerosis. Genes and environment unequivocally induce variations in the inflammatory response that contribute to different susceptibility for developing all these processes among healthy individuals (1–4).
Adipose tissue is the main source and target for several inflammatory pathways. In obesity, both the intrinsic cells (adipocytes) and the infiltrating immune cells exhibit proinflammatory properties. Of these infiltrating cells, macrophages are of particular importance given their capacity to secrete a variety of proinflammatory molecules leading to insulin resistance. In fact, the percentage of resident macrophages in adipose tissue is higher with increased fat mass, confirming that fat tissue growth is associated with a recruitment of blood monocytes (5–7).
One of the main functions of macrophages is to continuously sense the extracellular milieu. Toll-like receptors in these cells efficiently transduce the inflammatory signals, and this process is especially important in obesity. In particular, toll-like receptor 4 (TLR4) is a key receptor highly expressed in macrophages and adipose tissue, and involved in activation of the innate/inflammatory response. Knockout of TLR4 in hematopoietic cells (including macrophages) prevented hyperinsulinemia and hyperglycemia induced by obesity and a high-fat diet (HFD) and abrogated insulin resistance in adipose tissue in contrast with diverse effects found in systemic TLR4 deletion (8). However, TLR4 does not interact directly with the most potent inflammatory signals. Upstream to TLR4 is the multifunctional receptor CD14 (9–11).
CD14 is a 55-kDa protein that is expressed in two forms: glycosylphosphatidylinositol-anchored membrane protein (mCDI4) and a soluble serum protein (sCD14) lacking the glycosylphosphatidylinositol anchor (9–12). Different tissues and cells express a different form of CD14, i.e., mCD14 is the expressed form mainly in myeloid cells and macrophages, whereas sCD14 is the expressed form in the other cells, including hepatocytes and adipocytes (13–16). Both circulating sCD14 and cellular CD14 receptor interact with the inflammatory signals; lipopolysaccharide (LPS) is one of the most potent stimuli known. An excess of circulating sCD14 is known to buffer these signals, avoiding their exposure with cell (macrophage)-anchored CD14 (9–12).
Any strategy directed at blocking macrophage CD14 (e.g., with excess sCD14) will be capable of interrupting the inflammatory signal (LPS) before it is transduced. CD14 is in close interaction with TLR4, and LPS induces physical proximity between TLR4 and CD14 before nuclear translocation of nuclear factor-κB and triggering of the inflammatory cascade (12).
Mice harboring null mutations in CD14 showed decreased body fat and increased bone mineral content. These mutant mice live long lives. Unlike many strains of caged wild-type (WT) mice, they do not become obese (17) and resist most of the features of metabolic disease triggered by CD14 ligands (18). However, it is important to elucidate whether bone marrow CD14 and adipocyte CD14 are equally responsible for these metabolic changes.
The grafting of mice with bone marrow stem cells has been used to evaluate the influence of these cells on whole-body insulin sensitivity (8). We grafted CD14 knockout (KO) mice with bone marrow stem cells from WT donor mice fed an HFD. We also grafted WT mice with cells from CD14 KO mice to test the reverse hypothesis. We then explored whether these findings can be extended to normal physiology. sCD14, apparently derived from both secretion and enzymatically cleaved glycosyl-phosphatidylinositol-anchored tissue CD14, is known to antagonize CD14 receptor signaling (11). Blocking cellular CD14 in macrophages and adipocytes by excess sCD14 should result in a decrease of the inflammatory pathways in adipose tissue and improvement of whole-body insulin action. Finally, we explored whether the observations can be extended to humans.
RESEARCH DESIGN AND METHODS
Animal studies
Effects of recombinant human soluble CD14 on insulin action.
WT and CD14 KO mice in a C57Bl/6 J background were anesthetized with isoflurane-oxygen (1.5–2.5%) (Abbott Laboratories, Abbott Park, IL), and an intrafemoral catheter was indwelled as previously described by Riant et al. (19). All mice were allowed to recover until they fully reached their presurgery body weight.
Oral glucose tolerance test.
Overnight fasted mice were given glucose (2 g/kg) orally. Whole blood was collected from the tail vein at 0, 15, 30, 60, 120, and 180 min. To assess whether insulin sensitivity could be controlled by sCD14, a 4-h intravenous infusion of the recombinant human soluble CD14 (rh-sCD14) protein was performed at a rate of 5 μg/kg/h.
Euglycemic hyperinsulinemic clamp and isotope measurements and calculations were performed as previously described (19). Briefly, 6-h fasted mice were infused with insulin at a rate of 4 mU/kg/min for 3 h, and D-(3H)3-glucose (Perkin Elmer Inc., Waltham, MA) was simultaneously infused at rate of 30 μCi/kg/min. Euglycemia was maintained by periodically adjusting a variable infusion of a 16.5% (w/v) glucose solution. Plasma glucose concentrations and D-(3H)3-glucose specific activity were determined in 5 μL of blood sampled from the tip of the tail vein every 10 min during the last hour of the infusion.
Effects of rh-sCD14 on insulin resistance in mice fed HFD.
Forty C57BL/6 J male mice (8 weeks old) were purchased from Harlan Iberica (Barcelona, Spain). Thirty mice were fed a high-fat Western-type diet (Harlan Teklad No. 88137, Madison, WI) that contained 21% (wt/wt) fat (42% of calories), 49.2% (wt/wt) carbohydrate, and 19.8% (wt/wt) protein for 26–28 weeks (mice were 34–36 weeks old at the experimental procedure). Ten mice were fed a standard rodent chow diet. Mice were maintained on 12-h light/12-h dark cycles. Water and food were available ad libitum. Twenty mice fed an HFD received 1 μg/g/day of rh-sCD14, or vehicle, for 12 days. rh-sCD14 was administered in two subcutaneous injections (0.5 μg/g each one) every 12 h. This interval was calculated after observing that a single subcutaneous injection of rh-sCD14 resulted in serum concentration of this protein between 0.6 and 1.2 ng/mL. rh-sCD14 was easily measured using a human sCD14 enzyme-linked immunosorbent assay after rh-sCD14 administration and was preferred over murine-sCD14. Intraperitoneal glucose tolerance test (IPGTT), mice exsanguination, and tissue harvest were then performed. The Animal Ethics Committee at Parc Científic de Barcelona approved the protocols.
Effects of rh-sCD14 on insulin resistance in ob/ob mice.
Male C57BL/6 J ob/ob mice (10 weeks old) were purchased from The Jackson Laboratory (Bar Harbor, ME). Mice were maintained on 12-h light/12-h dark cycles and fed a standard chow diet and water ad libitum. rh-sCD14 (1 μg/g/day) was continuously delivered by Alzet pumps (pump 1002, 100 μL; Cupertino, CA) to five mice for 12 days. The mini pumps were implanted on the back, slightly posterior to the scapulae. The control group (n = 5) received vehicle alone.
HFD effects on insulin resistance in WT mice grafted with CD14 bone marrow stem cells.
Six-week-old C57Bl6/J male mice were subjected to 9.5-Gy lethal total body γ-irradiation to eliminate endogenous bone marrow stem cells and bone marrow–derived cells as described. Twelve hours later, they were intravenously reconstituted with bone marrow cells (5 × 106) extracted from the femur and tibia of CD14 KO mice. Mice were then allowed to recover for 4 weeks under a chow diet. Then, mice were fed an HFD for 4 weeks. CD14 bone marrow cell deficiency was systematically assessed in peripheral blood mononuclear cells and resident peritoneal macrophages by PCR (data not shown). We performed fluorescence-active cell sorter analyses on total blood and showed that the grafting efficiency was >85%. Any mouse showing a grafting efficiency below this cutoff was discarded. The mice then underwent clamp experiments to assess insulin sensitivity.
Human studies
Study of circulating sCD14.
Consecutive nondiabetic healthy subjects (n = 146 [93 men], aged 38.7 ± 9.8 years, with a BMI of 25.7 ± 3.1 [men] and 24.6 ± 4.3 kg/m2 [women]) were recruited prospectively in the Hospital of Girona. None of these healthy subjects were taking any medication or showed any evidence of metabolic disease other than obesity. All subjects were of Caucasian origin and reported that their body weight had been stable for at least 3 months before the study. Inclusion criteria were 1) BMI (weight in kilograms divided by the square of height in meters) <40 kg/m2, 2) absence of any systemic disease, and 3) absence of any infections in the previous month. Fat mass and fat-free mass were measured through bioelectric impedance (Holtain BC Analyzer, Holtain, Cambridge, U.K.), which provides both absolute and percent fat mass.
Circulating sCD14 was measured by the sCD-14 EASIA (Biosource Europe S.A., Zoning Industriel B-6220, Fleunes, Belgium), a solid-phase Enzyme Amplified Sensitivity Immunoassay performed on microliter plate. The minimum detectable concentration is estimated to be 1 ng/mL. The intra- and interassay coefficients of variation were <5.2 and 7.8%, respectively.
Study of CD14 expression in human adipose tissue.
A sample of 32 subjects (13 lean [BMI <25 kg/m2] and 19 obese) were selected at the Endocrinology Service among patients who were scheduled for abdominal elective surgical procedures (gastric bypass operation, cholecystectomy, and surgery of abdominal hernia) at the Hospital Universitari Joan XXIII and Hospital Sant Pau i Santa Tecla (Tarragona, Spain). An independent replication study in a sample of 40 subjects was performed at the Hospital of Girona (Girona, Spain).
All subjects were of Caucasian origin and reported that their body weight had been stable for at least 3 months before the study. Systemic inflammatory disease and recent infections (in the previous month) were considered as exclusion criteria. Liver and renal diseases were specifically excluded by biochemical workup. All subjects gave informed written consent. The ethics committees of the participant institutions approved the study.
CD14 real-time PCR.
Real-time quantitative PCR analyses were performed with 2 μL of cDNA, corresponding to 100 ng of total RNA on LightCycler Instrument (Roche Diagnostics, Basel, Switzerland), using the SYBR Green (Molecular Probes, Inc., Eugene, OR) fluorescence method. Primers are available on request. Adipose tissue and adipocyte expression levels of CD14 were normalized by β-actin and cyclophilin A (CypA) gene. CypA gene expression was highly homogeneous comparing lean versus obese subjects (23.48 ± 1.2 vs. 23.4 ± 1.03, P = 0.6), and preadipocytes and stromovascular cells versus adipocytes (23.66 ± 0.24 and 23.3 ± 0.7 vs. 23.86 ± 0.6, P = 0.8 and P = 0.5). β-Actin gene expression (with a variation coefficient of 3%) was more heterogeneous than CypA (with a variation coefficient of 1.2%) comparing preadipocytes with adipocytes.
CD14 expression during differentiation of human preadipocytes.
Isolated preadipocytes from adipose tissue of lean and obese subjects (SP-F1 and SP-F3; Zen-Bio, Inc., Research Triangle Park, NC) were plated on T-75 cell culture flasks and cultured at 37°C and 5% CO2 in Dulbecco’s modified Eagle’s medium/Nutrient Mix F-12 medium (1:1, v/v). Further details of the differentiation process are available on request. The experiment was performed in triplicate for each sample. The differentiation was monitored with the fatty acid synthase and adiponectin expression (Hs00188012_m1 and Hs00605917_m1; Applied Biosystems, Inc., Madrid, Spain).
Effects of TNF-α on CD14 gene expression in human adipocytes.
Adipocytes were incubated with fresh media (control) and fresh media containing TNF-α (100 ng/mL; Santa Cruz Biotechnology, Santa Cruz, CA). After 48 h, the supernatants were centrifuged at 400g for 5 min. The cells were then harvested, and pellets and supernatants were stored at −80°C for RNA and protein analysis.
Statistical methods.
Descriptive results of continuous variables are expressed as mean ± SD. Before statistical analysis, normal distribution and homogeneity of the variances were evaluated using Levene test, and then variables were given a log-transformation if necessary. Relation between variables was tested using Pearson test and stepwise multiple linear regression analysis. Unpaired t tests were used to compare CD14 mRNA expression in subcutaneous adipose tissue. The analyses were performed using the program SPSS version 12.0 (SPSS, Inc., Chicago, IL).
RESULTS
Effects of bone marrow grafting on HFD-induced insulin resistance and adipose tissue inflammation.
After irradiation, the time required for the mice to become frankly diabetic increased from 1 to 3 months in response to a high-fat carbohydrate-free diet (Supplementary Fig. 1A). Furthermore, the extent of glucose intolerance obtained is lower compared with nonirradiated and nongrafted WT mice (Supplementary Fig. 1B–D). Figure 1B–C compares oral glucose tolerance tests performed at 1 and 3 months in HFD-fed mice grafted and not grafted with bone marrow stem cells. Body weight gain and fat mass in response to an HFD was unchanged in irradiated grafted mice with either WT or CD14−/− bone marrow (data not shown). This effect was most likely attributed to the destruction of precursor cells from the adipose tissue during irradiation, which hampers the development of the tissue. Circulating levels of sCD14 in the different models used are shown in Supplementary Fig. 2A.
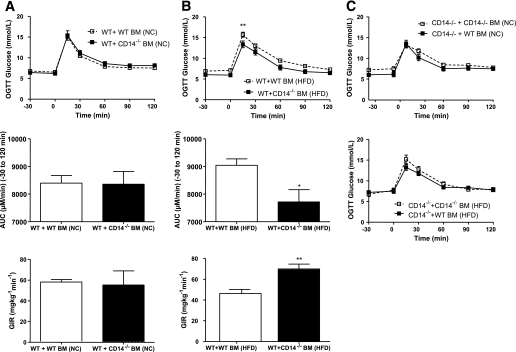
FIG. 1.
Glucose tolerance time course in WT mice. A and B: Glucose tolerance test (top) and the corresponding area under the curve (μmol/L/min, middle) and glucose infusion rates (bottom) in WT mice grafted with cells from CD14 KO mice (CD14−/−) and fed normal chow or HFD. Data are from 6–8 mice per group. *P < 0.05 and **P < 0.01 for WT mice grafted with cells from CD14 KO mice vs. WT mice grafted with cells from WT donor using Student t test. Glucose infusion rate calculations were made during the last 60 min of the 180-min clamp in steady-state condition. C: Glucose tolerance test in CD14 KO mice (CD14−/−) grafted with cells from CD14 KO or WT mice and fed normal chow or HFD (n = 6–8 mice per group). AUC, area under the curve; BM, bone marrow; GIR, glucose infusion rate; NC, normal chow; OGTT, oral glucose tolerance test.
We hypothesized that CD14 expression in bone marrow stem cells was responsible for HFD-induced insulin resistance. To this end, WT mice were grafted with bone marrow stem cells from CD14 KO mice and then clamped at hyperinsulinemia. The data showed that, as expected, WT mice grafted with bone marrow stem cells from WT donor mice became insulin resistant and glucose intolerant when fed an HFD when compared with mice fed normal chow (Fig. 1A and B, Supplementary Fig. 2B). Fasting glycemia values were 5.6 ± 0.2 mmol/L in the WT mice grafted with bone marrow stem cells from WT donor mice and 7.2 ± 0.4 mmol/L in the WT mice grafted with bone marrow stem cells from CD14−/− mice. Free fatty acids and fasting triglycerides are shown in Supplementary Fig. 2C.
Conversely, WT mice grafted with cells from CD14 KO mice resisted the occurrence of glucose intolerance and insulin resistance when fed an HFD.
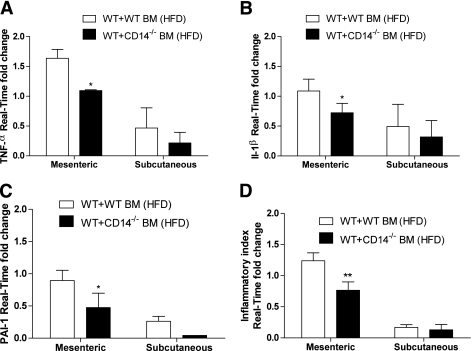
These observations were associated with decreased mesenteric adipose tissue mRNA expression of genes coding for common cytokines (Fig. 2). It is noteworthy that these differences primarily affected the mesenteric rather than the subcutaneous adipose depot.
FIG. 2.
Gene expression in fat from CD14−/− mice and HFD effect. mRNA concentration coding for TNF-α (A), IL1-β (B), plasminogen activator inhibitor-1 (C), and inflammatory index (D) in the mesenteric and subcutaneous adipose depots from WT mice grafted with cells from WT or CD14 KO mice (CD14−/−) fed HFD. The inflammatory index was calculated as follows. The relative mRNA concentration was quantified as fold change over an internal control gene (RPL19) for all individuals and for all cytokines considered. Then all relative quantifications were pooled (including plasminogen activator inhibitor-1, IL1-β, and TNF-α). Data are from 6–8 mice per group. *P < 0.05 and **P < 0.01 for WT mice grafted with cells from CD14 KO mice vs. WT mice grafted with cells from WT donor using Student t test. BM, bone marrow; PAI, plasminogen activator inhibitor.
Both macrophages and adipocytes could be responsible for these effects because glucose intolerance did not worsen in CD14 KO mice grafted with bone marrow stem cells from WT mice fed an HFD, when compared with recipient KO mice grafted with cells from CD14 KO donor mice also fed an HFD (Fig. 1C).
Effects of sCD14 on insulin action.
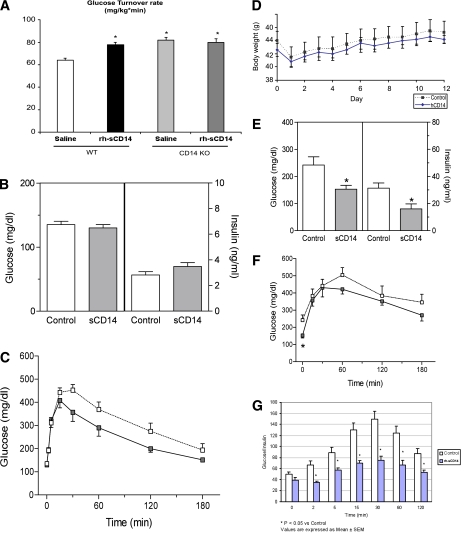
We then explored whether these observations can be extended to normal physiology. If cellular CD14 in macrophages and adipocytes plays a role in inflammation-induced systemic insulin resistance, a strategy known to block cellular CD14 should result in improved inflammatory activity in adipose tissue and increased insulin action. It is known that an excess of sCD14 buffers the inflammatory signals, avoiding their exposure with cell-anchored CD14. To analyze this hypothesis, we clamped mice at a low physiologic insulin infusion rate ensuring a total inhibition of hepatic glucose production and submaximal peripheral insulin known to stimulate glucose utilization. After a 4-h infusion with rh-sCD14, insulin sensitivity was increased in WT mice (Fig. 3A) to a level similar to what was observed in CD14 KO mice not infused with the recombinant protein (18). The insulin-sensitizing action of sCD14 was totally absent in CD14 KO mice, showing the specificity of the effect (Fig. 3A).
FIG. 3.
Effects of rh-sCD14 on insulin action and glucose turnover. A: Glucose turnover rates (mg/kg/min) of WT and CD14 KO mice infused with rh-sCD14 or saline during a hyperinsulinemic glucose clamp (n = 6–8 mice per group). *P < 0.05 for sCD14 vs. saline treatment, using Student t test. Effects of rh-sCD14 (n = 9) or vehicle (n = 9) in high fat–fed mice on (B) fasting glucose and insulin concentrations and (C) glucose after IPGTTs. Glucose (2 g/kg) was injected intraperitoneally after an overnight fast. Effects of treatment with rh-sCD14 or vehicle in ob/ob mice on body weight (D), fasting glucose and insulin concentrations (n = 4–5) (E), and IPGTT (F). Dashed line, mice treated with vehicle; continuous line, mice treated with rh-sCD14. G: Glucose/insulin ratio. Two-way ANOVA test indicated a significant difference between the glucose (P = 0.002) and insulin (P < 0.0001) curves of sCD14- and vehicle-treated mice. *P < 0.05 for sCD14 vs. vehicle treatment, using Student t test. (A high-quality color representation of this figure is available in the online issue.)
Effects of rh-sCD14 in mice fed HFD.
To further test the effects of rh-sCD14 on insulin sensitivity, we also tested this recombinant protein in C57BL/6 J mice previously fed a Western-type diet containing 21% fat for up to 28 weeks (high fat–fed mice). Fasting blood glucose levels were similar in rh-sCD14–treated versus vehicle-treated mice (Fig. 3B). However, glucose tolerance significantly improved after treatment with rh-sCD14. The area under the curve of blood glucose after IPGTT was 38% lower in rh-sCD14–treated mice compared with vehicle (P = 0.002, by two-way ANOVA, Fig. 3C).
Body weight and daily food intake were not significantly different after rh-sCD14 or vehicle treatment in high fat–fed mice for 12 days. Likewise, rh-sCD14 treatment did not change the weight of epididymal adipose tissue or soleus muscle.
Effects of rh-sCD14 on adipose tissue gene expression in mice fed HFD.
We found 3,479 genes whose expression in adipose tissue was significantly different in rh-sCD14–treated mice versus vehicle. Of all these genes, only those with a P value < 0.01 and a fold change of at least 1.5 were considered differentially expressed, giving a total of 82 genes.
Supplementary Table 1 shows the list of genes that were most changed (fold change of at least 1.75) with respect to all genes (3,479) analyzed. Some gene families—such as the APOA, APOB, and APOC genes—whose functions are clearly related to lipid metabolism appeared repeatedly in the full list of 82 genes. The microarray analysis of the expression of key genes involved in lipid metabolism and inflammation was confirmed by quantitative PCR (Supplementary Fig. 3). Supplementary Figs. 4 and 5 show the two top significant networks derived by the Ingenuity software. Of note, the two top selected networks dealt with inflammatory pathways and metabolism. No gene was considered to be differentially expressed in muscle of CD14-treated versus untreated mice.
Effects of rh-sCD14 in ob/ob mice.
Fasting blood glucose decreased significantly after rh-sCD14 treatment (242 ± 30 vs. 153 ± 14 mg/dL, for vehicle- and rh-sCD14–treated mice, respectively; P = 0.02) (Fig. 3E). In addition, glucose tolerance during an IPGTT improved significantly after treatment with rh-sCD14 (P = 0.02, by two-way ANOVA, Fig. 3F) in parallel with a decrease in the area under the curve for serum insulin (P = 0.0001) and glucose/insulin ratio (Fig. 3G). Body weight and daily food intake did not differ significantly after treatment with rh-sCD14 or vehicle for 12 days (Fig. 3D and data not shown). Likewise, rh-sCD14 treatment did not change the weight of epididymal adipose tissue or soleus muscle (data not shown).
Studies in humans.
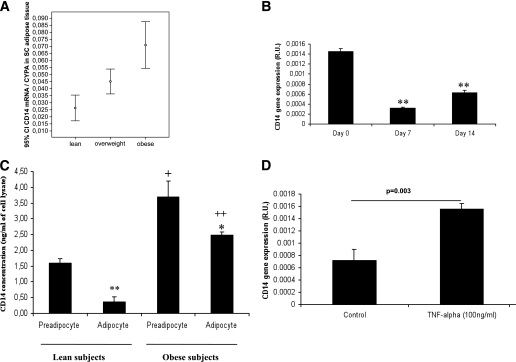
CD14 mRNA expression was evaluated in human subcutaneous adipose tissue in two independent studies. In the first study, the expression of CD14 was increased in 19 obese subjects (10 men and 9 women, BMI 30.7 ± 5 kg/m2) compared with 13 lean subjects (8 men and 5 women, BMI 22.9 ± 1.4 kg/m2) (0.054 ± 0.029 vs. 0.032 ± 0.015 relative units, P = 0.02). CD14 mRNA expression was linearly associated with BMI (r = 0.40, P = 0.02). In the replication study, we evaluated 40 subjects: 4 lean (BMI 22.3 ± 1.7 kg/m2, 1 man), 12 overweight (BMI 26.9 ± 1.8 kg/m2, 3 men), and 24 obese (BMI 45.9 ± 4.1 kg/m2, 4 men). The three groups of subjects were similar in age (43.5 ± 13.7 vs. 47.8 ± 12.2 vs. 45.3 ± 12.4 years, P = 0.8) and sex. CD14 mRNA expression increased with obesity status (Fig. 4A). Systemic inflammation contributed to this association to some extent, given the linear association between CD14 mRNA expression and peripheral white blood cell count (r = 0.37, P = 0.02).
FIG. 4.
CD14 gene expression in obese subjects and during adipogenesis. A: The 95% CI for the mean of CD14 mRNA expression according to obesity status. B: Study of CD14 mRNA expression during in vitro differentiation of human adipocytes. **P < 0.005 in comparison with day 0. C: Study of CD14 mRNA in isolated preadipocytes and adipocytes from lean and obese subjects. *P < 0.05 in comparison with preadipocyte. **P < 0.005 in comparison with preadipocyte. +P < 0.05 in comparison with lean cells. ++P < 0.005 in comparison with lean cells. D: TNF-α (100 ng/mL) administration during 48 h significantly increased CD14 gene expression in human adipocytes (P = 0.003). SC, subcutaneous.
CD14 mRNA expression decreased significantly during in vitro differentiation of human preadipocytes into adipocytes when CypA was used as an internal control (P < 0.005, Fig. 4B). CD14 protein concentrations, which were concordant with CD14 mRNA levels, were significantly increased in both isolated preadipocytes and adipocytes from obese subjects when compared with lean subjects (Fig. 4C). Further supporting the role of inflammation on increased CD14 gene expression, TNF-α (100 ng/mL) administration during 48 h led to significantly increased CD14 gene expression in human adipocytes (P = 0.003) (Fig. 4D).
Finally, we evaluated circulating sCD14 concentrations. Women showed significantly higher circulating sCD14 concentrations than men in parallel to their physiologically increased percent fat mass (4.81 ± 1.8 vs. 4.13 ± 1.76 μg/mL). Circulating sCD14 was significantly associated with both absolute fat mass (r = 0.19, P = 0.02) and percent fat mass (r = 0.20, P = 0.01), and this relationship was stronger in women (r = 0.31 and r = 0.32, for absolute and percent fat mass, P = 0.023 and P = 0.018, respectively).
DISCUSSION
The inflammatory signals leading to metabolic derangement are known to be sensed by TLR4, among others (8,20,21). However, TLR4 does not interact directly. Upstream to TLR4 is the multifunctional receptor CD14. Both circulating sCD14 and cellular CD14 receptors interact with the inflammatory signals in close relationship with TLR4. Any strategy directed at blocking cellular CD14 will be capable of interrupting the inflammatory signal before it is transduced.
Mice harboring a null mutation in the CD14 gene showed decreased mesenteric fat, among other phenotypic characteristics of type 2 diabetes (17). However, genetic deletion provides little information about the relative contribution of the different cells expressing CD14 leading to this phenotype. According to current findings, both bone marrow–derived macrophages and tissue macrophages expressing CD14 seem important targets in systemic inflammation and insulin action.
As expected, WT mice grafted with bone marrow stem cells from WT donor mice became insulin resistant and glucose intolerant when fed an HFD when compared with mice fed normal chow. In confirmation that bone marrow–derived macrophages were responsible for these effects, WT mice grafted with cells from CD14 KO mice resisted the occurrence of glucose intolerance, insulin resistance, and adipose tissue inflammation when fed an HFD. The reduced cytokine mRNA concentration in mesenteric adipose depot but not the subcutaneous fat depot suggests that the former was targeted by CD14 activation. This difference was probably related to the well-known dissimilar biochemical and metabolic properties of the visceral fat versus the subcutaneous fat (22). This dataset fits with what has been described using TLR4 KO mice (8,20,21).
However, CD14 expression in adipocytes could also be responsible for these effects because glucose intolerance did not worsen in CD14 KO mice grafted with bone marrow stem cells from WT mice fed an HFD, when compared with recipient KO mice grafted with cells from CD14 KO donor mice also fed an HFD (Fig. 3A).
Given the difficulty of producing effective “diet-induced obesity” after bone marrow transplantation, tissue-specific CD14 KOs will be needed to more fully characterize the importance of the different tissue sources of CD14 in the obese state.
For all these reasons, we explored whether these findings could be extended to normal physiology. One way to decrease CD14 signaling is to deliver rh-sCD14 that competes with endogenous CD14 receptor in the membrane of macrophages and other myeloid cells. Blocking cellular CD14 in macrophages and adipocytes by excess sCD14 resulted in a decrease of the inflammatory pathways (interleukin [IL]-1α and IL-1β among them, Supplementary Fig. 3C) specifically in adipose tissue (and not in muscle) and improved insulin action. This was found not only at the individual gene but also at multiple levels, as suggested by the microarray results in adipose tissue, confirmed by quantitative PCR (Supplementary Fig. 3). Expression profiles of genes listed in Supplementary Table 1 were analyzed using the Ingenuity Pathway Analysis methodology to compose a set of interactive networks, taking into consideration canonical pathways and the relevant biological interactions.
A number of canonical pathways were revealed to play an important role, especially those related with glycolysis and gluconeogenesis and IL-4 signaling. Next, two significant biological networks were identified by the Ingenuity Pathway Analysis. Further analysis of the highest scored network (score 24, 14 focus genes) identified inflammatory response (P < 0.028), genetic disorder (P < 0.048), and inflammatory disease (P < 0.0375) as the most significant biological functions linked to these networks (Supplementary Figs. 3–5).
Treatment with rh-sCD14 was associated with improved glucose tolerance in three animal models. In WT mice, rh-sCD14 led to increased insulin action. This improvement consistently was not observed in CD14 KO mice. In obese high-fat mice, rh-sCD14 also led to improvement of glucose tolerance. In ob/ob mice, a model with established diabetes and prominent insulin resistance, treatment with rh-sCD14 resulted in lowering of plasma glucose and insulin concentrations. It is therefore conceivable that treatment with sCD14 in individuals with decreased serum sCD14 concentrations may increase their levels above a certain threshold of functional deficiency.
LPS, an abundant component of the outer membrane of gram-negative bacteria, is one of the most potent inflammatory stimuli in animal host cells. Whereas LPS recognition benefits the host by sensing the presence of bacteria and mobilizing defense mechanisms, an exaggerated response to LPS may contribute to the harmful sequelae of severe inflammation (23). The buffering of LPS is crucial not only during acute inflammatory and infectious processes. In normal humans, triglyceride-rich lipoproteins contain detectable levels of endogenous LPS that are presumably scavenged in vivo (24). LPS is extraordinarily ubiquitous in nature, being present in food and water and in normal indoor environments as a constituent of house dust (25). In the mice studied, plasma LPS concentration ranged between 6 and 15 EU/mL with a mean of 7.5 EU/mL. Of note, an HFD led to increased circulating LPS concentrations even in humans (26). Endogenous LPS is also continually produced within the gut by the death of gram-negative bacteria and absorbed into intestinal capillaries. Therefore, low-grade portal venous LPS is the status quo in humans (27). LPS is increasingly recognized as a strong stimulatory factor involved in the release of several cytokines that are key inducers of insulin resistance and other metabolic disturbances. A two- to threefold increased plasma concentration of LPS has been demonstrated to constitute a sufficient molecular mechanism for triggering insulin resistance, obesity, and type 2 diabetes (18,28). This process was named “metabolic endotoxemia,” in which day-to-day circulating endotoxin (LPS) for 1 month affects inflammation, but not enough to produce acute endotoxemia (18,28).
The host has numerous mechanisms that downregulate responses to LPS and remove it from the circulation and tissues. sCD14 can both potentiate and downregulate responses to LPS. sCD14 was originally described as an LPS inhibitor, and other studies have described inhibitory effects of high concentrations of sCD14 under various conditions (23). Other works have shown that in plasma, sCD14 decreases monocyte responses to LPS by transferring cell-bound LPS to plasma lipoproteins (23). Moderate to high concentrations of sCD14 that are found in human blood may help to prevent LPS-induced systemic inflammation, whereas lower concentrations of sCD14 may promote inflammation (23).
It remains to be determined which cells are directly sensitive to metabolic endotoxemia-induced inflammation in human obesity. At first glance, the increased CD14 mRNA and protein levels in adipocytes of obese subjects make these cells more sensitive to the effects of metabolic endotoxemia. A proinflammatory environment was possibly behind this observation because TNF-α administration led to increased CD14 mRNA in adipocytes. In fact, CD14 mRNA decreased with preadipocyte conversion into adipocytes in parallel to the downregulation of inflammatory genes during adipocyte differentiation (Fig. 4B).
The scenario seems more complex. We also found that circulating sCD14 was proportional to fat mass. This association may be envisioned as an attempt to buffer metabolic endotoxemia with increased fat mass. However, increased metabolic endotoxemia possibly results in increased turnover of sCD14 because weight loss results in both decreased LPS (J.M.M.-N. and J.M.F.-R. unpublished results) and increased sCD14 levels (29).
Finally, our results are consistent with studies reporting lower levels of proinflammatory cytokines and apparent protection from atherosclerosis in subjects with gene TLR4 mutations (30).
In summary, systemic CD14 expression might play a role in obesity and inflammation-induced insulin resistance. The administration of sCD14 could be a therapeutic strategy to ameliorate these phenotypes.
Supplementary Material
ACKNOWLEDGMENTS
This work was partially supported by research grants from the Instituto de Salud Carlos III (CIBERobn and CIBERDEM), by a grant from the Société Francophone du Diabetes (SFD) and GlaxoSmithKline, by a grant from the Société Francaise de Diabetologie (R.B.), and by Grant MTM2008-00642 (A.S.-P.). This work was partially supported by FLORINASH (7th FP). No other potential conflicts of interest relevant to this article were reported.
All authors of this article directly participated in the execution and analysis of the study. J.M.F.-R. carried out the conception, design, and coordination of the study; performed the statistical analysis; and wrote the manuscript. S.P.P. carried out the animal studies, analyzed the biochemical variables, and performed the statistical analysis. E.L. carried out the animal studies, analyzed the biochemical variables, performed the statistical analysis, and was responsible for the experiment with LPS. J.M.M.-N. and A.W. carried out the animal studies, analyzed the biochemical variables, and performed the statistical analysis. M.S. carried out the animal studies, analyzed the biochemical variables, performed the statistical analysis, and performed the HFD-based obese and diabetic mouse models. E.S. carried out the animal studies, analyzed the biochemical variables, and performed the statistical analysis. A.S.-P. and F.C.P. analyzed the microarray data. J.V. participated in the conception and coordination of the study. M.R.C. carried out the animal studies, analyzed the biochemical variables, and performed the statistical analysis. W.R., R.B., and A.Z. participated in the conception and coordination of the study.
The authors thank P. Cani, INSERM, and M. Iglesias, INSERM, for technical expertise and Roser Rodriguez, CIBERobn, for administrative help.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db10-1210/-/DC1.
REFERENCES
- 1.Pickup JC, Crook MA. Is type II diabetes mellitus a disease of the innate immune system? Diabetologia 1998;41:1241–1248 [DOI] [PubMed] [Google Scholar]
- 2.Fernández-Real JM, Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev 2003;24:278–301 [DOI] [PubMed] [Google Scholar]
- 3.Fernández-Real JM, Broch M, Richart C, Vendrell J, López-Bermejo A, Ricart W. CD14 monocyte receptor, involved in the inflammatory cascade, and insulin sensitivity. J Clin Endocrinol Metab 2003;88:1780–1784 [DOI] [PubMed] [Google Scholar]
- 4.Fernández-Real JM, Pickup JC. Innate immunity, insulin resistance and type 2 diabetes. Trends Endocrinol Metab 2008;19:10–16 [DOI] [PubMed] [Google Scholar]
- 5.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW., Jr Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003;112:1796–1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003;112:1821–1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsou CL, Peters W, Si Y, et al. Critical roles for CCR2 and MCP-3 in monocyte mobilization from bone marrow and recruitment to inflammatory sites. J Clin Invest 2007;117:902–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saberi M, Woods NB, de Luca C, et al. Hematopoietic cell-specific deletion of toll-like receptor 4 ameliorates hepatic and adipose tissue insulin resistance in high-fat-fed mice. Cell Metab 2009;10:419–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC. CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science 1990;249:1431–1433 [DOI] [PubMed] [Google Scholar]
- 10.Pugin J, Heumann ID, Tomasz A, et al. CD14 is a pattern recognition receptor. Immunity 1994;1:509–516 [DOI] [PubMed] [Google Scholar]
- 11.Ulevitch RJ, Tobias PS. Receptor-dependent mechanisms of cell stimulation by bacterial endotoxin. Annu Rev Immunol 1995;13:437–457 [DOI] [PubMed] [Google Scholar]
- 12.Jiang Q, Akashi S, Miyake K, Petty HR. Lipopolysaccharide induces physical proximity between CD14 and toll-like receptor 4 (TLR4) prior to nuclear translocation of NF-kappa B. J Immunol 2000;165:3541–3544 [DOI] [PubMed] [Google Scholar]
- 13.Pan Z, Zhou L, Hetherington CJ, Zhang DE. Hepatocytes contribute to soluble CD14 production, and CD14 expression is differentially regulated in hepatocytes and monocytes. J Biol Chem 2000;275:36430–36435 [DOI] [PubMed] [Google Scholar]
- 14.Fearns C, Kravchenko VV, Ulevitch RJ, Loskutoff DJ. Murine CD14 gene expression in vivo: extramyeloid synthesis and regulation by lipopolysaccharide. J Exp Med 1995;181:857–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sewter CP, Digby JE, Blows F, Prins J, O’Rahilly S. Regulation of tumour necrosis factor-alpha release from human adipose tissue in vitro. J Endocrinol 1999;163:33–38 [DOI] [PubMed] [Google Scholar]
- 16.Daniel JA, Elsasser TH, Morrison CD, et al. Leptin, tumor necrosis factor-alpha (TNF), and CD14 in ovine adipose tissue and changes in circulating TNF in lean and fat sheep. J Anim Sci 2003;81:2590–2599 [DOI] [PubMed] [Google Scholar]
- 17.Johnson GB, Riggs BL, Platt JL. A genetic basis for the “Adonis” phenotype of low adiposity and strong bones. FASEB J 2004;18:1282–1284 [DOI] [PubMed] [Google Scholar]
- 18.Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007;56:1761–1772 [DOI] [PubMed] [Google Scholar]
- 19.Riant E, Waget A, Cogo H, Arnal JF, Burcelin R, Gourdy P. Estrogens protect against high-fat diet-induced insulin resistance and glucose intolerance in mice. Endocrinology 2009;150:2109–2117 [DOI] [PubMed] [Google Scholar]
- 20.Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 2006;116:3015–3025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poggi M, Bastelica D, Gual P, et al. C3H/HeJ mice carrying a toll-like receptor 4 mutation are protected against the development of insulin resistance in white adipose tissue in response to a high-fat diet. Diabetologia 2007;50:1267–1276 [DOI] [PubMed] [Google Scholar]
- 22.Pérez-Pérez R, Ortega-Delgado FJ, García-Santos E, et al. Differential proteomics of omental and subcutaneous adipose tissue reflects their unalike biochemical and metabolic properties. J Proteome Res 2009;8:1682–1693 [DOI] [PubMed] [Google Scholar]
- 23.Thompson PA, Tobias PS, Viriyakosol S, Kirkland TN, Kitchens RL. Lipopolysaccharide (LPS)-binding protein inhibits responses to cell-bound LPS. J Biol Chem 2003;278:28367–28371 [DOI] [PubMed] [Google Scholar]
- 24.Harris HW, Grunfeld C, Feingold KR, Rapp JH. Human very low density lipoproteins and chylomicrons can protect against endotoxin-induced death in mice. J Clin Invest 1990;86:696–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michel OJ, Kips J, Duchateau J, et al. Severity of asthma is related to endotoxin in house dust. Am J Respir Crit Care Med 1996;154:1641–1646 [DOI] [PubMed] [Google Scholar]
- 26.Amar J, Burcelin R, Ruidavets JB, et al. Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr 2008;87:1219–1223 [DOI] [PubMed] [Google Scholar]
- 27.Jacob AI, Goldberg PK, Bloom N, Degenshein GA, Kozinn PJ. Endotoxin and bacteria in portal blood. Gastroenterology 1977;72:1268–1270 [PubMed] [Google Scholar]
- 28.Cani PD, Bibiloni R, Knauf C, et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 2008;57:1470–1481 [DOI] [PubMed] [Google Scholar]
- 29.Manco M, Fernandez-Real JM, Vecchio FM, et al. The decrease of serum levels of human neutrophil alpha-defensins parallels with the surgery-induced amelioration of NASH in obesity. Obes Surg 2010;20:1682–1689 [DOI] [PubMed] [Google Scholar]
- 30.Kiechl S, Lorenz E, Reindl M, et al. Toll-like receptor 4 polymorphisms and atherogenesis. N Engl J Med 2002;347:185–192 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.