The main aim of treatment in glaucoma is to reduce intraocular pressure. Good evidence from multiple large randomised trials shows that reducing intraocular pressure is effective in preventing disease progression in ocular hypertension, primary open angle glaucoma, and even in so called normal tension glaucoma. Target pressures in the low teens are associated with the lowest progression rates.
Medical treatment
β blockers
The β blockers—for example, timolol, carteolol, betaxolol levobunolol, and metipranolol—reduce the secretion of aqueous and are the most commonly prescribed topical treatment. Contraindications to their use include a history of lung or heart disease, as the drops may cause systemic β blockade. Topical β blockers can unmask latent and previously undiagnosed chronic obstructive pulmonary disease in elderly people.
Systemic effects from eye drops can be reduced by occlusion of the punctum (finger pressed on the caruncle, which is felt as a lump at the inner canthus of the eye) or shutting the eyes for several minutes after putting in the drops. This reduces the lacrimal pumping mechanism and stops the drops running down the lacrimal passages and being absorbed systemically through the nasal mucosa or by inhalation directly into the lungs. It may also enhance ocular absorption of the drugs. Drops are usually given twice a day, but long acting forms can be given once a day, either alone or in combination with other drops.
Figure 1.

Eye closure to reduce systemic side effects after instilling drops
Prostaglandin analogues
Prostaglandin analogues (such as, latanoprost, travoprost, and bimatoprost) reduce the intraocular pressure by increasing aqueous outflow from the eye through the uveoscleral pathway. These drugs can reduce intraocular pressure by 30-35%.
Systemic side effects are minimal, but a few patients with light irides experience a gradual, permanent darkening of the iris. Eyelashes may also increase in length and darken. For optimum effect, these drops are used once daily (at night).
Parasympathomimetic drugs
Parasympathomimetic drugs such as pilocarpine constrict the pupil and “pull” on the trabecular meshwork, increasing the flow of aqueous out of the eye. The small pupil may, however, cause visual problems if central lens opacities are present. Constriction of the ciliary body causes accommodation and blurred vision in young patients.
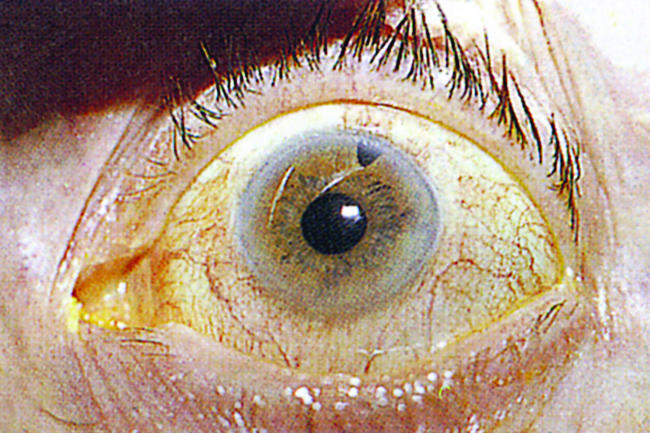
Figure 2.
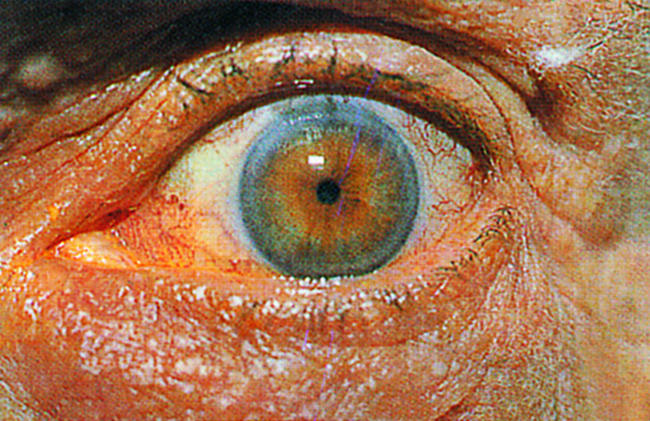
Small pupil after instillation of pilocarpine
Pilocarpine should not be used if there is inflammation in the eye because the pupil may stick to the lens close to the visual axis (posterior synechiae) and affect vision. Pilocarpine is usually given four times a day but can be used twice daily in a combined form with a β blocker or once at night in a gel preparation, which reduces side effects.
Table 1.
Sympathomimetic drugs
| • A newer generation of drugs that stimulate the α receptors of the sympathetic system is now used—for example, brimonidine (used twice a day) or apraclonidine |
| • Contraindications include cardiovascular disease because of the potential systemic sympathomimetic effects |
| • Topical adrenaline is now rarely used because it is less effective than β blockers and has adverse effects on the conjunctiva |
Carbonic anhydrase inhibitors
These are available as topical (for example, dorzolamide, brinzolamide) or oral (for example, acetazolamide) drugs. They reduce the secretion of aqueous, and the systemic form, administered orally, is the most powerful drug for reducing intraocular pressure, although it may have side effects, including nausea, lassitude, paraesthesiae, electrolyte disturbances, and renal stones. The topical form has minimal systemic side effects. Carbonic anhydrase inhibitors should not be used in patients with sulphonamide allergy.
This article is adapted from the 4th edition of the ABC of Eyes, which will be published by BMJ Books in February 2004 (www.bmjbooks.com).
Drops used to treat glaucoma contain powerful drugs that can have serious systemic effects despite the low topical doses used.
The ability of prostaglandin analogues to achieve larger reductions in intraocular pressure with fewer side effects has been a big therapeutic advance.
When patients first instil pilocarpine they often experience a brow ache, which tends to reduce with longer term use of the drug. Pilocarpine can increase the risk of retinal detachment.
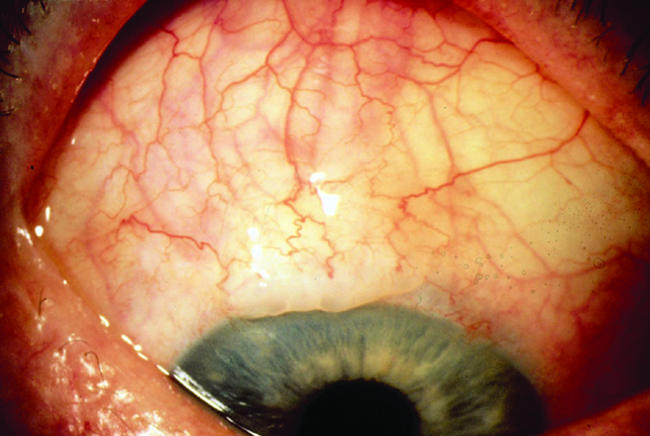
Figure 3.

Mild allergy to the active drug component of a glaucoma drug
Neuroprotective drugs
Experimental evidence suggests that some neuroprotective drugs reduce intraocular pressure induced glaucomatous damage. However, at present no conclusive evidence exists that these drugs are helpful in glaucoma, but large scale clinical trials are currently being carried out.
Allergy to glaucoma drops
The main symptoms of drop allergy are intense itching and irritation of the eyes and eyelids, which is exacerbated by instillation of the drops. The characteristic signs of drop hypersensitivity include red injected eyes, red swollen eyelids, and ezcema like excoriation of the eyelids and periocular skin.
Figure 4.
Severe allergy: bilateral allergic dermatitis secondary to the preservative component in a glaucoma drop
The patient may be hypersensitive to the active glaucoma drug or one of the preservative agents used to stabilise the preparation (usually benzalkonium chloride). The diagnostic test for drop hypersensitivity is controlled cessation of therapy. Symptoms and signs should rapidly improve on withdrawal of the topical therapy. When patients are receiving multiple topical drugs it can be difficult to isolate the agent responsible for the allergic reaction. For patients who are allergic to the preservative agent, some topical drugs are available in preservative free form.
Laser treatment
Laser trabeculoplasty
Argon or diode laser “burns” are applied to the trabecular meshwork. How this treatment works is uncertain. It was thought to contract one part of the meshwork, so stretching and opening up adjacent areas, but a more recent hypothesis is that it rejuvenates the cells in the trabecular meshwork. This treatment is used only in the types of glaucoma where the drainage angle is open. Its effect is relatively short term, so this treatment is mainly used for more elderly patients.
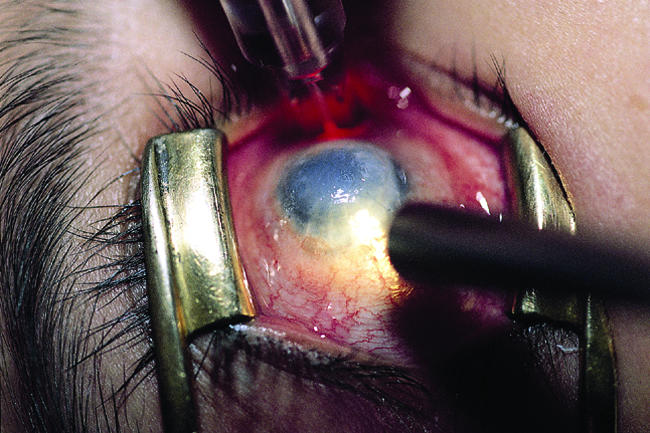
Figure 5.
Holes made in the iris (iridotomy) without having to cut into the eyeball by using neodymium: yttrium-aluminium-garnet laser
Laser iridotomy
Peripheral laser iridotomy can be performed in cases of angle closure glaucoma. A neodymium: yttrium-aluminium-garnet (Nd:YAG) laser is used, which (unlike argon or diode lasers) cuts holes in tissue rather than just burning. This procedure can be performed without incising the eye.
Laser iridoplasty
Argon laser iridoplasty is a useful procedure in some forms of angle closure glaucoma. A ring of laser burns is applied to the peripheral iris, causing contraction of tissue. This pulls the peripheral iris away from the drainage angle and helps to reduce angle occlusion.
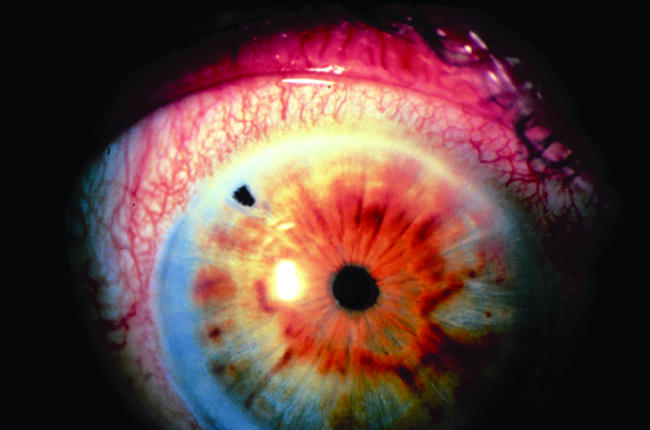
Laser ciliary body ablation
Lasers can be used to burn the circular ciliary body that produces the aqueous humour. At the correct wavelength the laser radiation passes through the white sclera and is only absorbed by the pigmented ciliary body (transcleral ciliary body cycloablation). This treatment is now commonly done with a diode laser and usually has to be repeated to maintain a lowered intraocular pressure. Most patients having laser ciliary body ablation need to continue drug treatment.
Figure 6.
Ciliary body ablation with diode laser
Laser destruction of the ciliary body usually is used only in advanced refractory glaucomas or where other surgical options are limited.
Surgical treatment
Surgery was traditionally used only when treatment had failed to halt the progress of glaucoma, but there is some evidence that earlier surgical intervention is beneficial for selected patients.
Iridectomy
Peripheral iridectomy is performed in cases of angle closure glaucoma, both in the affected eye and prophylactically in the other eye. Most of these cases can be treated with the Nd:YAG laser. Surgery is reserved for difficult or refractory cases.
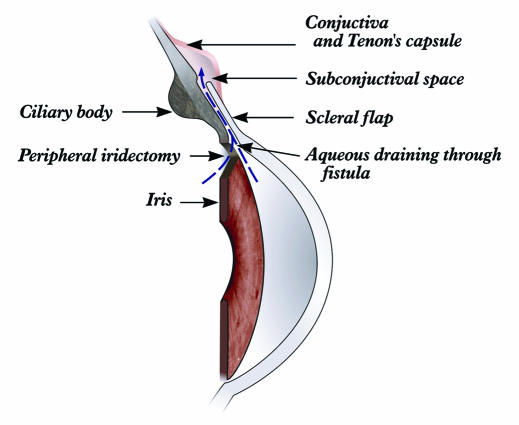
Figure 7.
Surgical peripheral iridectomy
Drainage surgery
When it is not possible to achieve the target intraocular pressure with medical (or laser) therapy in glaucoma, then the next line of management is surgical. The most effective glaucoma filtration procedure is trabeculectomy. In this procedure a guarded channel is created, which allows aqueous to flow from the anterior chamber inside the eye into the sub-Tenon's and subconjunctival space (bypassing the blocked trabecular meshwork). A drainage bleb (aqueous under the conjunctiva and Tenon's capsule) can often be seen under the upper lid. Conjunctivitis in a patient with a drainage bleb should always be treated promptly, as it increases the risk of infection entering the eye (endophthalmitis).
Figure 8.
Trabeculectomy
Possible complications
The main cause of surgical failure is postoperative scarring of the drainage channel and drainage bleb. Scarring can be reduced by using adjuvant antiscarring therapy. Various antiscarring agents are used, including drugs used in anticancer therapy. These are delivered by short applications during surgery to the drainage bed on a sponge or by postoperative injections. The most commonly used drugs are 5-fluorouracil and mitomycin-c.
Glaucoma filtration procedures carry some risk, and the patient should be advised of the risk of postoperative cataract and hypotony (low pressure) and the possibility of a reduction in postoperative best corrected visual acuity. Although trabeculectomy remains the gold standard glaucoma filtration procedure, several alternative filtration operations also exist. Non-penetrating deep sclerectomy and viscocanalostomy have good safety profiles but have tended to produce smaller reductions in intraocular pressure in all published trials.
Figure 9.
Bleb
For certain patients with refractory glaucoma, a tube drainage device may be considered. A drainage tube is inserted, connecting the anterior chamber of the eye with a reservoir in the posterior orbit. This has a good chance of controlling intraocular pressure but also has moderately high risk of serious complications.
Table 2.
Support group
| The International Glaucoma Association is the major support group for patients with glaucoma in the United Kingdom. This organisation provides information pamphlets and support for people with different forms of glaucoma. |
| International Glaucoma Association |
| King's College Hospital |
| Denmark Hill, London SE5 9RS |
| Tel/fax: 020 7737 3265 |
| Email: iga@kcl.ac.uk |
Guidelines for managing glaucoma are available from the European Glaucoma Society (www.eugs.org) and the American Academy of Ophthalmology (www.aao.org/news/eyenet/)
The ABC of Eyes is by P T Khaw, professor of ophthalmology at Moorfields Eye Hospital, London (p.khaw@ucl.ac.uk), P Shah, consultant ophthalmic surgeon at Birmingham and Midland Eye Centre, Birmingham (p.f.shah@talk21.com), and A R Elkington, emeritus professor of ophthalmology, University of Southampton.
The photographs were provided by PTK and Moorfields Eye Hospital and the line drawings were prepared by Alan Lacey, Moorfields Eye Hospital.
Competing interests: PS and PTK have received educational and research grants from pharmaceutical companies.