Abstract
Purpose: To explore the nature of men’s experiences of osteoporosis by developing an understanding of men’s explanatory models. Design and Methods: This descriptive study invited community-residing male osteoporosis patients aged 50+ to participate in interviews about osteoporosis. Participants were recruited from a hospital-affiliated bone clinic. Men completed a questionnaire on demographic, medication, and fracture-related information, and descriptive statistics were calculated using Statistical Package for the Social Sciences. Interviews elicited the 5 domains of men’s explanatory model (Kleinman, 1987) and open-ended information regarding men’s experiences living with this disorder. Narrative data were analyzed both for content and inductively. Results: Men’s narratives demonstrate that an osteoporosis diagnosis is accompanied by negative psychosocial sequelae in this population. Men defined it as a disease of the bone that may increase the likelihood of fracture and that may cause pain. Participants reported that osteoporosis is diagnosed by bone mineral density (BMD) score and that disease progression is measured by a decrease in BMD and an increase in pain or new fractures. Men described a reluctance to take medications, dissatisfaction with side effects, and a perception that osteoporosis treatment in men had little basis in long-term medication efficacy or safety data. They viewed osteoporosis as a degenerative chronic disease with an overall stable course. Implications: Participants’ explanatory models for osteoporosis are substantively different than clinical models. These differences provide a foundation for exploring the importance of gender to osteoporosis outcomes, a context for making sense of men’s bone health behavior, and a clear case for an increase in advocacy and educational efforts for men who have or are at risk for osteoporosis.
Keywords: Masculinity, Fracture, Qualitative, Psychosocial, Risk
Understanding how older adults with chronic disease interpret and act upon health-related information is an important first step in building behavioral interventions to support improved disease-related outcomes. This kind of understanding is best achieved through qualitative methods, which allow people to use their own terms and autobiographical knowledge to elucidate the processes involved in receiving a diagnosis or treatment plan and subsequently making sense of those data in the context of their lives. These subjective views on disease can then be compared, categorized, and summarized into models with which we can identify new areas of inquiry and develop person-centered holistic research priorities (Greenhalgh & Hurwitz, 1999). Such qualitative approaches can also foster the development of standardized measures of disease-related quality of life measures or health outcomes (Hurley, 1999). The process of beginning with the patient and extending a research agenda out from the themes embedded in their experiences is especially important for subpopulations who suffer from health disparities or in cases where clinical understanding of the disorder is emergent (see Sofaer, 1999). In the case of osteoporosis, male patients may be viewed as a subpopulation with poor outcomes as compared with women and a thin literature as to the potential social causes of these disparities. This qualitative study aimed to explore how men with osteoporosis experience the disorder by collecting and analyzing men’s explanatory models. Explanatory models are historically contingent, individual patient perspectives on the diagnosis, treatment, course, cause, and nature of a particular disorder (Kleinman, 1978; 1980; 1988). An explanatory model, although structured enough to enable comparison among men, builds a narrative that situates patient beliefs within a life course perspective and in this case allows us to construct a general understanding of how men think about their osteoporosis. This improved understanding of how men’s beliefs are in part shaped by their identity as men contributes to health services research seeking to decrease gender-related health disparities in chronic care.
Osteoporosis is a metabolic bone disease responsible for disability, mortality, and reduced quality of life among many older adults. Osteoporosis prevalence increases with age, though it is certainly underdiagnosed in both women and men. In the United States, postmenopausal Caucasian women possess the greatest lifetime risk of developing osteoporosis. As a result of this sex difference, a majority of the research, prevention, and intervention resources have been focused on women. Research with older women has demonstrated that osteoporosis poses negative consequences for interpersonal relationships, gender roles, and overall quality of life (Gold, 1996; 2001; 2003). Women have difficulty performing activities, which they find meaningful, and they often experience role loss, feelings of premature aging, shame or embarrassment, stress, anxiety, and depression (Gold, 1996; Gold & Roberto, 2000; Penrod, 2000; Roberto & Gold, 1997, 2002; Roberto, Gold, & Yorgasen, 2004; Roberto & Reynolds, 2001). It is evident that much improvement can be made in the diagnosis and treatment of osteoporosis in women; however, it is also clear that men develop osteoporosis in significant numbers (Araujo et al., 2007; Scholtissen et al., 2009) and that osteoporosis in men remains substantively underdiagnosed and undertreated (Cheng et al., 2009; Ebeling, 2008).
Despite the recognition that men do develop osteoporosis, there is a considerable need to better understand clinical and psychosocial outcomes of the disease in men (Seeman et al., 2004). Lower bone mineral density (BMD) is associated with osteoporotic fracture in men as it is for women, and predictors of low BMD in men include lower body mass index, prior fracture, a family history of osteoporosis (Scholtissen et al., 2009), and increasing age (Araujo et al., 2007; Cauley et al., 2005). Predictors of osteoporosis in men include history of smoking, high alcohol consumption, hypogonadism, use of glucocorticoids, and low lifetime intake of dietary calcium and/or vitamin D (Ebeling, 2008). Fracture risk in men is increased by low BMD (Ebeling, 2008), family history of fracture, and shorter stature (Cauley et al., 2005). The growing literature on male osteoporosis shows that when compared with female patients, male osteoporosis patients have fewer treatment options and have higher postfracture morbidity, institutionalization, and mortality (Campion & Maricic, 1521; Pande & Francis, 2001; Vondracek & Hansen, 2004). Regardless of the demonstrated economic and health value of BMD screening for at-risk men, men in the United States continue to be underevaluated for this disorder (Schousboe et al., 2007).
As the epidemiologic and clinical understanding of osteoporosis in men develops, the need for qualitatively derived substantive exploration of men’s beliefs becomes greater. Several studies have demonstrated men’s poor knowledge of osteoporosis risk factors, suboptimal calcium consumption, and infrequent participation in weight bearing exercise (Ailinger, Braun, Lasus, & Whitt, 2005; Sedlak, Doheny, & Estok, 2000; Tung & Lee, 2006). Interventions designed to increase the incidence of BMD screening, risk factor identification and risk reduction, medication adherence, or calcium and vitamin D intake among men must be informed by knowledge of men’s osteoporosis-related beliefs and practices (Solimeo, 2008). Men participate in doctor–patient encounters from a gendered standpoint, which frames the importance and scope of health maintenance behavior in their life (O’Brien, Hunt, & Hart, 2005; Thompson, 2008). For some, masculinity is constructed through activities, which actively distance men from socially defined “healthy” behaviors, whereas for others, their sense of manliness is maintained through a performed disinterest in health. Those men who seek to maximize their health and well-being may be confronted with gender-related constraints upon the ways in which they can do this: Men whose health interests fall outside of these gender roles may run a risk of others calling their masculinity into question.
The relationship between masculinity and health behavior is especially germane to the study of osteoporosis. Often characterized as a women’s disease because of women’s greater risk for the disorder, clinicians may be primed to downplay the importance of symptoms in male patients, and men may have difficulty reconciling their gender identity with the diagnosis or its recommended treatments. This study demonstrates the variance and commonalities found among men’s experience and raises the clinical implications of patient beliefs. By attending to what men already know, feel, and believe, we can begin the task of delivering care and designing patient-centered interventions which incorporate gender differences in the experience of osteoporosis.
Methods
Participants and Recruitment
The underdiagnosis of osteoporosis and the potential stigma internalized by men make it difficult to identify potential participants from a population sample. For this study, potential participants were sought from a clinic specializing in bone health. Eligibility requirements included spoken and written English literacy; the ability to participate in an audio-recorded interview; osteoporosis diagnosis; male sex; and age 50 years or older. Diagnosis was defined as a history of osteoporotic fracture and/or a BMD t score of <2.5 in the spine or the hip. A board-certified endocrinologist (T. J. Weber) prescreened eligible men from consecutive clinic appointments occurring within a 6-month time period. Thirty-eight men gave him permission to share their contact information with the study team, who followed up by telephone. Of these 38, 14 men declined to participate. Information as to why men declined to participate was not solicited, but 2 men explicitly mentioned the burden of comorbid conditions as a factor in their decision. Twenty-four men initially enrolled in the study. One participant did not return the first mailing and dropped out of the study without comment. Twenty-three men completed all data collection procedures.
A medical anthropologist (S. Solimeo) established written informed consent with potential participants and conducted interviews. All participants were offered an honorarium and interview transcript. The Duke University Medical Center Institutional Review Board approved the study protocol (IRB#8354-06-ROER).
Study Design and Data Collection
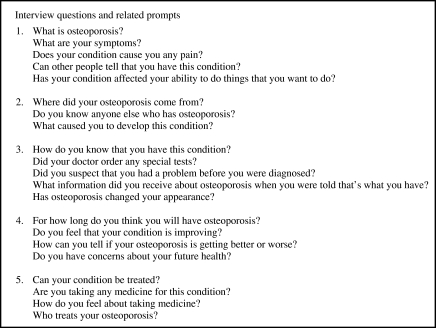
The interview schedule was semistructured to maximize the breadth of information obtained while minimizing participant burden. The interviews comprised two parts. The first portion aimed to collect men’s responses to the five constructs of an Explanatory Model—diagnosis, treatment, cause, nature, and course (Kleinman, 1988). The second portion of the interviews was open ended. The interviewer (S. Solimeo) used an iterative process, reflecting on respondent’s explanatory model and prompting men to elaborate on how osteoporosis has influenced their daily activities as well as their relationships with themselves and others. The open-ended interview provided feedback and verification of the explanatory model categories and allowed for the emergence of a participant-driven social context within which to understand the model constructs. See Figure 1 for examples of interview questions and prompts. Interview sites were selected by participants, and they included a clinic office and men’s private residences. Three men preferred phone interviews due to their travel or physical limitations. The interviews were on average 1-hr long. Audio recordings were transcribed, and transcripts were mailed to participants as a courtesy and to provide an opportunity for participants to review and clarify their content.
Figure 1.
Examples: Interview questions and related prompts.
Select quantitative items were collected to contextualize the interview data. Related data derived from a brief questionnaire and materials to test the validity and reliability of the male version of the Osteoporosis Assessment Questionnaire (Male OPAQ) are reported elsewhere. The questionnaire invited participants to report on their use of medications to treat osteoporosis, insurance coverage, the specialty of the diagnosing physician, whether they had had a BMD test, and the location of fractures with the year sustained. Information on participants’ race, marital status, educational attainment, employment status, household income, and whether they reside alone or with a friend or family member was also requested.
Analysis
The interview texts were imported into an NVivo project for coding to facilitate analysis (QSR International, 2002). The coding process provides a live index within the text, allowing investigators to retrieve pertinent passages quickly and providing a means for comparison among participants. The first portion of the interviews was coded by explanatory model construct, whereas the open-ended portion was coded for content. The resultant codebook was then reviewed for redundancy, and the entire code set was reorganized into a set of hierarchically organized themes relating to the explanatory model construct and a set of loosely related themes relating to men’s social worlds and risk management (reported elsewhere). The explanatory model construct code sets were then further coded topically and thematically, with subcodes organized hierarchically within the constructs. In other words, the initial coding was a rough sort of passages into the preestablished constructs of the explanatory model plus a content analysis of open-ended sections. The coded passages were then recoded for finer detail and many of the open-ended passages recoded into subcategories of the original explanatory model codes. This process was designed to achieve a balance between the final comparability of narratives across explanatory model components and the maximization of individual variance among men’s experiences. Coded excerpts for each theme were compiled, read, and compared with the extant literature on osteoporosis to evaluate the contributions of this study’s data to clinical practice and research.
Questionnaire responses were entered into a spreadsheet and descriptive statistics calculated using SPSS (SPSS, 2003).
Results
Table 1 summarizes participant characteristics. Participants’ age ranged from 53 to 86 years (mean = 70.36 years). All but one were Caucasian. These men were well educated and financially secure, and a majority were retired and residing with their spouse. Almost all men suffered from comorbid conditions. Men were employed in a variety of occupations and settings, including customer relations, accounting, higher education, law, electrical engineering, and emergency response. Slightly more than half of participants reported a fracture, and a majority of those fractures were vertebral. Almost all men were taking a prescription medication to treat osteoporosis.
Table 1.
Participant Characteristics
| n = 23 | Number of participants reporting |
| Mean age in years | 70.36 (range = 33, SD = 9.438) |
| Marital status | |
| Married | 19 |
| Widowed | 1 |
| Divorced | 2 |
| Single | 1 |
| Educational attainment | |
| High school diploma | 1 |
| Vocational or trade school or some college | 4 |
| College degree or more | 18 |
| Employment status | |
| Retired from paid employment | 16 |
| Working in paid position | 5 |
| Retired due to disability | 2 |
| Entire household income for prior year | |
| Less than $25,000 | 2 |
| Between $25,000 and $75,000 | 11 |
| More than $75,000 | 10 |
| History of fracture | |
| At any site | 13 |
| At hip | 2 |
| Vertebral | 9 |
| Wrist | 2 |
| Pelvis | 1 |
| Other (e.g., rib, finger, and leg) | 3 |
| Mean number of fractures | 0.739 (range = 2, SD = 0.751) |
| Use prescription medication for osteoporosis | 17 |
Explanatory Model: Variability
Overall, men’s explanatory models illustrate their belief that osteoporosis is a disease that causes bone structure to weaken. According to men, this can be painful and can increase the possibility of fracture. Men cited the importance of pharmacotherapy in strengthening the bone and noted that medications are likely to stop or slow progression but will rarely improve bone density. In contrast to the emphasis on pharmacotherapy, men’s narratives stressed the limitations of treatment options and an overall reluctant to take medications. For these men, despite clear association between BMD screening and diagnosis, they expressed uncertainty as to which provider was responsible for their osteoporosis care as well as the long-term efficacy of pharmacological treatment. Presented later is a brief accounting of the variation within each construct, followed by a generalized model of osteoporosis in men.
Definition.—
Men defined osteoporosis as a disease of the bones, primarily affecting the spine but with the potential to damage the entire skeleton. A majority of men (15) describe osteoporosis as a weakening of the bone tissue and an enlargement of the “Swiss cheese” holes in the bone structure. Men viewed osteoporosis as both a “silent” disease and a disease whose symptoms include back pain, shortened stature, and fatigue. All participants associated osteoporosis with fractures whether or not they themselves had suffered one, yet men’s use of the qualifiers potential and possible reveals a belief that although osteoporosis increased their chances of sustaining fracture, fracture was considered neither an inevitable nor a likely outcome.
Diagnosis.—
Men came to receive an osteoporosis diagnosis through four initiating factors: fracture (9), unusual back or hip pain (6), self-initiated action (6), and chance encounter with diagnostic screening (2). Men who experienced painful fractures and sought immediate attention were x-rayed and then later referred for BMD screening. Men who suffered from back or hip pain did not realize initially that they had experienced compression fractures and often spent weeks treating their back pain with over the counter analgesics, heating pads, chiropractic adjustments, or rest. When such remedies were no longer effective or the pain became too severe, these men sought the care of their family doctors. Some men were familiar with osteoporosis symptoms from their wives’ experiences or from patient education materials posted in clinic offices. These men correctly self-diagnosed and sought clinical confirmation. For a small number of men, the diagnostic process was initiated by BMD screenings at local health fairs. Such men subsequently confirmed diagnosis from their physicians. Regardless of clinical path, all men considered BMD testing to be essential for diagnosis.
Treatment.—
The interviews chronicled men’s dissatisfaction with medication side effects, high costs, and their perception that long-term medication safety or efficacy data for men were limited. Men identified the following treatments for osteoporosis: prescription medications, calcium supplements, and exercise. A few men sought adjunctive therapies, such as chiropractic manipulation, massage, or physical therapy for pain relief or to restore function after an injury.
Men’s discussion of treatment focused largely upon pharmacotherapy, though it is unclear whether this focus is due to patient preference or to limited understanding of dietary supplements. Within pharmacotherapy, discussion focused primarily upon bisphosphonates, which were described by men as a kind of bone vitamin that can help forestall disease progression but which does not halt or reverse bone loss. Development of adverse gastrointestinal effects with bisphosphonates led some men to discontinue or seek alternative medication delivery systems. Calcium was described as an important vitamin (sic), which most men reported taking, but few described making any dietary changes to increase calcium intake. Consistent with literature citing low intake among men (Ma, Johns, & Stafford, 2007), vitamin D supplementation was not discussed. Despite their not linking exercise to osteoporosis, almost all men reported engaging in some exercise, including walking, jogging, swimming, and stretches, to maintain their range of motion and flexibility. The nonexercisers had severe kyphosis and were very impaired by current fractures or pain.
For men with vertebral fractures, pain management was a key concern. Some men acknowledged a reluctance to take pain medication for fear of dependency or cognitive side effects, whereas others complained that the available medications were ineffective in restoring them to normal function. For men with chronic pain, managing osteoporosis meant limiting their use of pain medication in order to forestall the likelihood of developing medication tolerance and potentially running out of pain treatment options.
Etiology.—
Men believed that osteoporosis is caused by circumstances more or less beyond their individual control. When asked what might have caused their osteoporosis, men cited a variety of mechanisms, including cancer treatments, muscular dystrophy, gastrointestinal disorders, parathyroid imbalance, kidney stones, childhood aversion to milk, genetics, normal aging, a change in activity level, and stress. Seven men reported having received treatment for prostate, lung, esophageal, and brain cancers, but only two of them felt that osteoporosis was a direct result of such therapy. Comorbidities causing calcium depletion, such as celiac, were discussed. Tobacco use was not cited by men as a cause of osteoporosis nor was its use uniformly documented in this study; however, some men were smokers. Genetics and aging also informed men’s beliefs about causation. Men who cited genetics as a potential cause believed that it could be passed down from parent to child, including men who lead self-described healthy lifestyles. Aging was implicated similarly, and although no one equated normal aging with osteoporosis, several cited older age as a potential cause.
Course.—
All men reported that osteoporosis is a lifelong condition, but they differed in their assessment of whether it might improve or inevitably advance over the life course. Men measured their disease progress by fracture incidence, pain, and BMD scores. Six men reported that their osteoporosis had improved, citing reduced fracture incidence, better pain management, or higher BMD scores as evidence. BMD improvement also figured prominently in men’s sense of hope regarding their prognosis, often more so than their own experience. The majority of men were dismayed by their lack of improvement in BMD scores over time. Men with poorly managed pain were less optimistic and more guarded about disease progression. Participants explained that their unease regarding prognosis was a result of the limitation of medical knowledge about osteoporosis in men.
Explanatory Model: Commonality
Although men’s individual models of osteoporosis are unique, in aggregate, they highlight the current limitations of diagnosis, treatment, and care coordination for men with this disorder. Explanatory models can illustrate participants’ health care preferences and dislikes and make clear which aspects of the health care system are dysfunctional from the patient’s experience. However, as Kleinman (1980) writes, “To analyze popular [explanatory models] into the five categories enumerated above is to attribute more formal organization and specificity to them than they usually possess. Vagueness, multiplicity of meanings, frequent changes, and lack of sharp boundaries between ideas and experiences are characteristics of lay [explanatory models]” (p. 107). In light of this nuanced view and of the study’s aims in providing a balanced contextualized examination of men’s experience with osteoporosis, we opt to present the model not as a series of narrative vignettes linked to individual constructs but as a longer composite narrative. Traditionally, these data are reported in a series of short quotations interspersed throughout the results presentation. In contrast, this narrative combines passages from multiple voices, which together represent an overall majority view within the study sample. In addition to providing a deeper and more contextualized explanatory model, our approach, although unconventional, stems from a desire to present qualitative data in a way that recognizes between-person differences while contributing results which can be used as a foundation for intervention work.
Three additional notes underlie the rationale for this approach. First, the constructed narrative serves to protect the identity of individual respondents in a study with a modest sample size (Rhodes, 2002, p. 461, note 421). Second, the narrative combines passages from multiple participants in order to overcome the bias presented by a particularly eloquent speaker who can fulfill the investigator’s expectation of self-reflection and insight. Third, the constructed narrative allows readers to immerse themselves into men’s experiences, without the sometimes jarring effect of interspersing narrative passages with explanatory comments. Such a rationale is shared in part by other ethnographers working in rather different circumstances, who explicitly discuss the importance of carefully editing narrative to produce reporting that is more balanced and contextualized (Bourgois, 2003; Bourgois & Schonberg, 2009). Narrative data collected over the course of months or even within the scope of a single interview can be disjointed and self-referential. Rearranging and editing these documents to maximize contextual meaning and reserve the beauty of narrative flow must be done with caution but can be done with integrity. In our case, we have taken passages from multiple interviews to create a narrative that reflects the middle ground within our data and illustrates common themes concerning uncertainty, frustration, and gender identity found in men’s narratives.
As I understand it, it’s as you grow older the bone density just kind of deteriorates like everything else, [laughs] and so it’s not surprising as you advance in years. [Osteoporosis is] a degeneration of the bone system. The entire bone system I would say, not just the back. It is the thinning and the decomposing of the bones, a weakening in the back, stooping over and shrinking maybe a little bit, too. It’s when the interior of the bone turns Swiss cheese, really old Swiss cheese and they break real easily. I don’t think there are symptoms of it unless you have a fracture. [Osteoporosis is] certainly not like cancer: “Oh you’re going to die tomorrow.” I guess it’s something that has a potential of being damaging. You know if you fall you’re going to be bad [off]. If you don’t fall, it’s okay. Although there are some people with very weak bones where anything is debilitating.
I’ve had occasions where I’ve hurt my back and, you know, I’m out for 2 or 3 days with a lower back problem. … I came back from [a trip] with a back problem and it was lingering for 2 or 3 weeks. I went to my general doctor. He said, “Look why don’t you let me do a bone density scan?” [The BMD test] shows your bone structure—the pictures of it they make—and it shows you how much percentage of the bone that you have left in there. And he had a machine in his office and I said, “Sure. Why not?” I was [in my fifties] then. And he looked at the results and he said, “Look I don’t know what to tell you but according to what I’m seeing here you’ve got severe osteoporosis.”
I was mad at the doctors for not telling me [about the risk for osteoporosis] right away, because I felt that if I had known that that was a side effect of this androgen deprivation thing … . I would have asked: “What should I be doing to prevent calcium loss?” But I wasn’t told. And so there were I know 4 or 5 years of the problem before it got to the point of severe osteoporosis.
I have been very embarrassed with men because of it, you know … because I’m so bent over and I look so terrible. It’s not a manly kind of thing. Because you look so weak and so bent over and you know, like this [stands to show his kyphosis] … . They all think of it as a woman’s thing. Not a man’s thing, you know. “What’s wrong with you that you have that? Only women get that.” It is embarrassing.
I haven’t seen [osteoporosis literature] other than describing what [osteoporosis] is and that [bisphosphonates] can help it. I think [bisphosphonates] may actually help it in the sense, in the term of the sense of that it strengthens your bones. But it doesn’t help with the pain!… It may help me in the future from a future fracture or something. But it doesn’t help the pain here and now. I think it’s a little misleading to people. [laughs] It’s a preventive type of thing, you know. You see it on TV all the time. You know “once a month pills” or “once a week pill” to help prevent a fracture, but, you know, “What do you do once you”ve got it?” I don’t want to manage the pain. I want it eliminated. I want to be able to do normal activities instead of saying “Well, manage it so that you compromise your living by not doing these things that cause the pain.” Well that’s a way of managing it but that doesn’t correct it.
[My BMD is] staying pretty stable, which is a little disappointing to me. I hoped that with the [bisphosphonate] I’ve been taking, and with the calcium supplement and all that my bone density might increase. And that has not been the case, but I guess it’s a small triumph just to maintain it at my age. I know that I will never get over it. I am hoping that it can be controlled. I seem to be running downhill with it. I hope that I can better control the pain part of it—control to a point—to forestall severe injury. I am hoping that I’m not going to die with it further in that it is.
As I said there’s so little knowledge about osteopenia and osteoporosis and then I don’t know that anyone feels a level of comfort about, you know, what the numbers mean in men. In women we have all sorts of things so [my doctor] could diagnose it 18 ways from Sunday. But with men you just don’t know. The level of knowledge is just not there so that we can say what it should be, you know.
Discussion
The men in this study had osteoporosis, an asymptomatic disease that in men becomes clinically apparent only after a low-trauma fracture and related impairments are incurred. Like many others with asymptomatic conditions, these men found it difficult to consider osteoporosis as an immediate and serious threat to their current health. Contributing to this lack of concern was their perception that so little is known about osteoporosis in men and their experience that, despite taking medications, their BMD remained relatively unchanged.
Osteoporosis is frequently described as both a “women’s disease” and a “silent disease,” and men’s beliefs about the cause, nature, treatment, course, and diagnosis of osteoporosis reveal the gendered interpretation of these characterizations. Prior to diagnosis, men rarely considered osteoporosis as a potential cause of back pain or a possible consequence of cancer treatment, and they were virtually uniformly surprised to learn of their disease status. This surprise contributed to a frustration they expressed with conflicting information on prognosis, risk factors, and treatment options. Men demonstrated limited clinical knowledge of osteoporosis and fracture risk factors, but their knowledge was interpreted through a gendered lens. Masculinity is commonly constructed around men’s ability to withstand or ignore pain (Courtenay, 2000). Pain itself may be interpreted by men as a positive but private side effect of the physical expression of their masculinity, that is, men who physically exert themselves may experience pain as a side effect, but that pain is interpreted as positive feedback for identity management. Thus, even though it appears as if there is a logical inconsistency in men’s simultaneously labeling osteoporosis a “silent disease” and identifying back pain as a symptom, men may interpret pain as a positive or even normal response to masculine performance. Accordingly, though as health service researchers we may be inclined to blame men for fractures when they admittedly ignore their provider’s recommendations to limit the amount of weight they handle, men’s ability to moderate their behavior may be constrained by social pressures to perform their masculinity somatically. These pressures notwithstanding, men with severe osteoporosis who incur fractures while sneezing or bending over to pick something up off of the floor may certainly act upon fracture risk reduction recommendations, but even their experience underscores the logic of men’s belief that fracture incidence is beyond individual control.
Attention to the gendered interpretation of health information does not negate the importance of pursuing an agenda of improved patient education. Educational interventions must be both patient and clinician focused. Albeit uncommon, men’s correct self-diagnosis suggests a need for improvement in practitioner’s ability to recognize symptoms. Once diagnosed, men feel that they are provided inadequate information concerning risk management, treatment options, and prognosis. This information issue derives from two factors: overall limited of knowledge concerning osteoporosis in men and the preponderance of literature dedicated to postmenopausal women. No data on treatment adherence were collected in this study, but men’s self-reported reluctance to take medication and their inadequate vitamin D and calcium intake imply that adherence may be an important issue. Men assess their bone health through BMD scores, but they expressed confusion concerning the appropriate frequency of these tests. In addition, they seemed unsure of which physician should be coordinating care: their primary care physician? An oncologist? An endocrinologist?
The cause of osteoporosis in men is incompletely defined, and attention to men’s belief that osteoporosis is a concern only for women should be incorporated into clinical efforts. Men who had healthy lifestyles or who viewed osteoporosis as a consequence of normal aging may be less likely to engage in further preventative health practices because they believe osteoporosis progression is inevitable and beyond their control. Others who cited cancer treatments and lack of physician oversight as potential causes may be disinclined to adhere to medical advice due to a lack of confidence in their medical care. Finally, due to limited disease outcome information, men’s confidence in care management, their willingness to comply with treatment, and their risk aversion practices may be weakened.
Explanatory models are a tool with which we can identify sites for improvement in the health care system. When the distance between patient and provider models is great, as it is for osteoporosis in men, the potential for poor health outcomes is increased (Kleinman, 1980). It is important to recall that the health care system is a cultural system in which individual actors are socialized to perform certain roles (Kleinman, 1980). The traditional expectation of the receptive compliant patient is changing with patients’ increased access to sophisticated medical information (2009), but this does not mean that in becoming more empowered, patients automatically stop performing other important social roles. Qualitative research is well suited to investigating such roles because narratives are at once event centered, experience derived, and experience creating (Mattingly, 1998). In this study, men draw upon their life experience to create for us a picture of how men with osteoporosis think about the disorder. In doing so, they highlight limitations to the current health care approach to osteoporosis in men as well as indicate the ways in which masculinity influences their health-related behavior. “ … [M] any older people try to become what culture signals as desirable without always recognizing where the pressures originate and even if those efforts are ultimately self-defeating” (Holstein & Minkler, 2003, p. 787). For older men, clinical focus on postmenopausal osteoporosis may engender a sense of invulnerability, obscuring men’s risk and couching osteoporosis risk prevention behaviors as feminine and outside the masculine social rubric.
These data present a limited view of men’s experience with osteoporosis due to the small sample size, uniform racial background, and participants’ relatively advantaged position with regards to socioeconomic status and health care utilization. Men who were approached but did not enroll may differ in some important ways from those who decided to participate, and limited anecdotal information collected from nonenrollees suggests that they may have had poorer health. Although this study improves our knowledge of the relationship between masculinity and osteoporosis, men perform masculinity in various ways (Calasanti, 2004). Considering participants’ demographic profiles, we should not expect that all older men experience osteoporosis similarly but acknowledge that other men with fewer economic, medical, and social privileges may have a far worse experience with this disorder if they have even been diagnosed. Additionally, given the relationship of cancer and cancer treatments with osteoporosis incidence and treatment, it may be important to examine the explanatory models of cancer patients separately or differently than those of cancer-free men. Regardless of such limitations, however, this descriptive study demonstrates the importance of exploring patient-held models of disease and establishes a framework with which intervention and practice models can be developed.
Funding
Dr. S. Solimeo received support for this research from the National Institute on Aging (grant number 5T32 AG00029-31).
Acknowledgments
The authors thank the men who participated in this study. Dr. S. Solimeo is a health research scientist specialist in the Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Medical Center, which is funded through the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government. The Center for the Study of Aging and Human Development at Duke University provided facility support for Drs. S. Solimeo and D. T. Gold. Related presentations: S. Solimeo, T. J. Weber, and D. T. Gold, “A women’s disease? Report on men’s experiences of osteoporosis.” Poster presented at the 60th Annual Scientific Meeting of the Gerontological Society of America.” November 16–20, 2007, San Francisco, CA.
References
- Ailinger RL, Braun MA, Lasus H, Whitt K. Factors influencing osteoporosis knowledge: A community study. Journal of Community Health Nursing. 2005;22:135–142. doi: 10.1207/s15327655jchn2203_1. doi:10.1207/s15327655jchn2203_1. [DOI] [PubMed] [Google Scholar]
- Araujo AB, Travison TG, Harris SS, Holick MF, Turner AK, McKinlay JB. Race/ethnic differences in bone mineral density in men. Osteoporosis International. 2007;18:943–953. doi: 10.1007/s00198-006-0321-9. doi:10.1007/s00198-006-0321-9. [DOI] [PubMed] [Google Scholar]
- Bourgois P. Search of respect: Selling crack in El Barrio. 2nd ed. New York: Cambridge Univerisity Press; 2003. doi:10.2277/0521017114. [Google Scholar]
- Bourgois P, Schonberg J. Righteous dopefiend. Berkeley, CA: University of California Press; 2009. [Google Scholar]
- Calasanti TM. Feminist gerontology and old men. Journal of Gerontology: Social Sciences. 2004;59B:S305–S314. doi: 10.1093/geronb/59.6.s305. doi:10.1093/geronb/59.6.S305. [DOI] [PubMed] [Google Scholar]
- Campion JM, Maricic MJ. osteoporosis in men. American Family Physician. 1521;67:1521–1526. [PubMed] [Google Scholar]
- Cauley JA, Fullman RL, Stone KL, Zmuda JM, Bauer DC, Barrett-Connor E, et al. Factors associated with the lumbar spine and proximal femur bone mineral density in older men. Osteoporosis International. 2005;16:1525–1537. doi: 10.1007/s00198-005-1866-8. doi:10.1007/s00198-005-1866-8. [DOI] [PubMed] [Google Scholar]
- Cheng H, Gary LC, Curtis JR, Saag KG, Kilgore ML, Morrisey MA, et al. Estimated prevalence and patterns of presumed osteoporosis among older Americans based on Medicare data. Osteoporosis International. 2009;20:1507–1515. doi: 10.1007/s00198-009-0835-z. doi:10.1007/s00198-009-0835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay WH. Constructions of masculinity and their impact on Men’s well-being: A theory of gender and health. Social Science & Medicine. 2000;50:1385–1401. doi: 10.1016/s0277-9536(99)00390-1. doi:10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- Ebeling PR. Osteoporosis in men. New England Journal of Medicine. 2008;358:1474–1482. doi: 10.1056/NEJMcp0707217. doi:10.1056/NEJMcp0707217. [DOI] [PubMed] [Google Scholar]
- Gold DT. The clinical impact of vertebral fractures: Quality of life in women with osteoporosis. Bone. 1996;18(3 Suppl.):s189–s194. doi: 10.1016/8756-3282(95)00500-5. doi:10.1016/8756-3282(95)00500-5. [DOI] [PubMed] [Google Scholar]
- Gold DT. The nonskeletal consequences of osteoporotic fractures: Psychologic and social outcomes. Rheumatic Disease Clinics of North America. 2001;27:255–262. doi: 10.1016/s0889-857x(05)70197-6. doi:10.1016/S0889-857X%2805%2970197-6. [DOI] [PubMed] [Google Scholar]
- Gold DT. Osteoporosis and quality of life psychosocial outcomes and interventions for individual patients. Clinics in Geriatric Medicine. 2003;19:271–280. doi: 10.1016/s0749-0690(02)00077-0. doi:10.1016/S0749-0690%2802%2900077-0. [DOI] [PubMed] [Google Scholar]
- Gold DT, Roberto KA. Correlates and consequences of chronic pain in older adults. Geriatric Nursing. 2000;21:270–273. doi: 10.1067/mgn.2000.110838. doi:10.1067/mgn.2000.110838. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T, Hurwitz B. Narrative based medicine—Why study narrative? British Medical Journal. 1999;318:48–50. doi: 10.1136/bmj.318.7175.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holstein MB, Minkler M. Self, society, and the ‘‘new gerontology’’. The Gerontologist. 2003;43:787–796. doi: 10.1093/geront/43.6.787. doi:10.1093/geront/43.6.787. [DOI] [PubMed] [Google Scholar]
- Hurley RE. Qualitative research and the profound grasp of the obvious. Health Services Research. 1999;34:1119–1136. [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine. 1978;12:85–93. doi: 10.1016/0160-7987(78)90014-5. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine and psychiatry. Berkeley, CA: University of California Press; 1980. [Google Scholar]
- Kleinman A. The Illness Narratives. New York: Basic Books; 1988. [Google Scholar]
- Ma J, Johns RA, Stafford RS. Americans are not meeting current calcium recommendations. American Journal of Clinical Nutrition. 2007;85:1361–1366. doi: 10.1093/ajcn/85.5.1361. [DOI] [PubMed] [Google Scholar]
- Mattingly C. Healing dramas and clinical plots. New York: Cambridge University Press; 1998. [Google Scholar]
- O’Brien R, Hunt K, Hart G. ‘It’s cavemen stuff, but that is to a certain extent how guys still operate’: Men’s accounts of masculinity and help seeking. Social Science & Medicine. 2005;61:503–516. doi: 10.1016/j.socscimed.2004.12.008. doi:10.1016/j.socscimed.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Pande I, Francis RM. Osteoporosis in men. Best Practice & Research Clinical Rheumatology. 2001;15:415–427. doi: 10.1053/berh.2001.0158. doi:10.1053/berh.2001.0158. [DOI] [PubMed] [Google Scholar]
- Penrod J. Living with osteoporosis: The personal experience. In: Smiciklas-Wright H, editor. Preventing and managing osteoporosis. New York: Springer; 2000. pp. 17–24. [Google Scholar]
- QSR International. NVivo (Version 2.0) Cambridge, MA: QSR International (Americas) Inc; 2002. [Google Scholar]
- Rhodes LA. Psychopathy and the face of control in supermax. Ethnography. 2002;3:442–466. doi:10.1177/1466138102003004016. [Google Scholar]
- Roberto KA, Gold DT. Spousal support of older women with osteoporotic pain: Congruity of perceptions. Journal of Women and Aging. 1997;9:17–31. doi:10.1300/J074v09n01_03. [Google Scholar]
- Roberto KA, Gold DT. Chronic pain in later life women: Issues and challenges from the research literature. Journal of the American Medical Women’s Association. 2002;57:97–99. [PubMed] [Google Scholar]
- Roberto KA, Gold DT, Yorgasen JB. The Influence of osteoporosis on the marital relationship of older couples. Journal of Applied Gerontology. 2004;23:443–456. doi:10.1177/0733464804270856. [Google Scholar]
- Roberto KA, Reynolds SG. The meaning of osteoporosis in the lives of rural older women. Health Care for Women International. 2001;22:599–611. doi: 10.1080/07399330127198. doi:10.1080/07399330127198. [DOI] [PubMed] [Google Scholar]
- Scholtissen S, Guillemin F, Bruyere O, Collette J, Dousset B, Kemmer C, et al. Assessment of determinants for osteoporosis in elderly men. Osteoporosis International. 2009;20:1157–1166. doi: 10.1007/s00198-008-0789-6. doi:10.1007/s00198-008-0789-6. [DOI] [PubMed] [Google Scholar]
- Schousboe JT, Taylor BC, Fink HA, Kane RL, Cummings SR, Orwoll ES, et al. Cost-effectiveness of bone densitometry followed by treatment of osteoporosis in older men. Journal of the American Medical Association. 2007;298:629–637. doi: 10.1001/jama.298.6.629. doi:10.1001/jama.298.6.629. [DOI] [PubMed] [Google Scholar]
- Sedlak CA, Doheny MO, Estok PJ. Osteoporosis in older men: Knowledge and health beliefs. Orthopaedic Nursing. 2000;19:38–46. doi: 10.1097/00006416-200019030-00006. doi:10.1097/00006416-200019030-00006. [DOI] [PubMed] [Google Scholar]
- Seeman E, Bianchi G, Adami S, Kanis J, Khosla S, Orwoll E. Osteoporosis in men: Consensus is premature. Calcified Tissue International. 2004;75:120–122. doi: 10.1007/s00223-004-4002-4. doi:10.1007/s00223-004-4002-4. [DOI] [PubMed] [Google Scholar]
- Sofaer S. Qualitative methods: What are they and why use them? Health Services Research. 1999;34:1101–1117. [PMC free article] [PubMed] [Google Scholar]
- Solimeo S. Osteoporosis in older men: Feelings of masculinity and a women’s disease’. Generations-Journal of the American Society on Aging. 2008;32:73–77. [Google Scholar]
- SPSS. Statistical Package for the Social Sciences (Version 11.0) Somers, NY: IBM; 2003. [Google Scholar]
- Thompson E. Gender matters: Aging men’s health. Generations. 2008;XXXII:5–8. [Google Scholar]
- Tung WC, Lee IFK. Effects of an osteoporosis educational programme for men. Journal of Advanced Nursing. 2006;56:26–34. doi: 10.1111/j.1365-2648.2006.03976.x. doi:10.1111/j.1365-2648.2006.03976.x. [DOI] [PubMed] [Google Scholar]
- Vondracek S, Hansen LB. Current approaches to the management of osteoporosis in men. American Journal of Health System Pharmacists. 2004;61:1801–1811. doi: 10.1093/ajhp/61.17.1801. [DOI] [PubMed] [Google Scholar]