Abstract
An ongoing loss of cardiomyocytes to apoptotic and necrotic cell death pathways contributes to the progressive nature of heart failure. The pathophysiological origins of necrotic cell loss relate to the neurohormonal activation that accompanies acute and chronic stressor states and which includes effector hormones of the adrenergic nervous system. Fifty years ago, Albrecht Fleckenstein and coworkers hypothesized the hyperadrenergic state, which accompanies such stressors, causes cardiomyocyte necrosis based on catecholamine-initiated excessive intracellular Ca2+ accumulation (EICA), and mitochondrial Ca2+ overloading in particular, in which the ensuing dysfunction and structural degeneration of these organelles leads to necrosis. In recent years, two downstream factors have been identified which, together with EICA, constitute a signal–transducer–effector pathway: (i) mitochondria-based induction of oxidative stress, in which the rate of reactive oxygen metabolite generation exceeds their rate of detoxification by endogenous antioxidant defences; and (ii) the opening of the mitochondrial inner membrane permeability transition pore (mPTP) followed by organellar swelling and degeneration. The pathogenesis of stress-related cardiomyopathy syndromes is likely related to this pathway. Other factors which can account for cytotoxicity in stressor states include: hypokalaemia; ionized hypocalcaemia and hypomagnesaemia with resultant elevations in parathyroid hormone serving as a potent mediator of EICA; and hypozincaemia with hyposelenaemia, which compromise antioxidant defences. Herein, we revisit the Fleckenstein hypothesis of EICA in leading to cardiomyocyte necrosis and the central role played by mitochondria.
Keywords: Potassium, Magnesium, Calcium, Zinc, Selenium, Acute stressor states, Congestive heart failure, Neurohormonal activation
Introduction
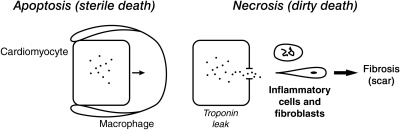
An ongoing loss of cardiomyocytes via apoptotic and necrotic cell death pathways contributes to the progressive nature of heart failure. As depicted in Figure 1, apoptotic cells are rapidly scavenged by macrophages; they neither disintegrate nor lose their contents to stimulate the immune system. As a result, serum troponin levels are not elevated and a wound healing response is not invoked.1–3 Dying necrotic cells, on the other hand, release troponins and other intracellular contents, which serve as danger signals to the immune system and chemoattractants that promote invasion of inflammatory cells to the site of injury. These cells, together with myofibroblasts, account for subsequent tissue repair. Foci of microscopic scarring are the final outcome. Hence, elevations in serum troponins and cardiac fibrosis are each footprints of cardiomyocyte necrosis. Scattered foci of fibrosis are found throughout both ventricles of the explanted failing human heart and are considered the major component of the pathological structural remodelling of myocardium.4 This would not only implicate the importance of cardiomyocyte necrosis, but would also suggest it to be an ongoing process. The loss of cardiomyocytes and their replacement with stiff fibrillar collagen each contribute to the progressive failure of this muscular pump. Elevations in serum troponins are found in patients hospitalized because of their congestive heart failure (CHF) and are associated with an increased risk of morbidity and mortality from cardiovascular events.5–14 In ambulatory asymptomatic elderly men, followed for 11 years in a community in Sweden, the appearance of elevated serum troponin predicted an increased risk of heart failure.15 Factors other than overt ischaemia with a segment of infarcted myocardium can account for cardiomyocyte necrosis (vide infra). An understanding of pathophysiological mechanisms involved becomes essential to the optimal evaluation and management of these patients. Towards this end, the origins of the CHF syndrome provide crucial insights.
Figure 1.
Heart failure involves an ongoing loss of cardiomyocytes to apoptosis and necrosis. See text.
Congestive heart failure has its origins rooted in inappropriate neurohormonal activation. This includes the hypothalamic–pituitary–adrenal axis (HPA), the adrenergic nervous (ANS), and renin–angiotensin–aldosterone (RAAS) systems. Their effector hormones are cytotoxic to cardiomyocytes.16–18 Some 50 years ago, Albrecht Fleckenstein and coworkers at the University of Freiburg im Breisgau hypothesized that hyperadrenergic state which accompanies stressor states, such as CHF, would lead to catecholamine-mediated excessive intracellular Ca2+ accumulation (EICA), particularly involving cardiac mitochondria. The ensuing dysfunction of Ca2+ overloaded mitochondria, coupled with the diminished synthesis of high-energy phosphate and structural degeneration of these organelles, would lead to cardiomyocyte necrosis. They validated their hypothesis using isoproterenol-induced cardiac injury in rodents in which cotreatment with a calcium-channel blocker, verapamil, proved cardioprotective.19,20 Later, others confirmed this paradigm and provided further insights into the adverse consequences of elevated plasma epinephrine levels (5000 pg/mL) comparable with those found in man during acute and chronic stressor states.18,21–24 Today, the importance of catecholamine excess that accompanies marked emotional stress or acute stressor states, such as head trauma or subarachnoid haemorrhage, is now recognized as leading to stress-related cardiomyopathy syndromes (e.g. apical ballooning or Takotsubo cardiomyopathy).25
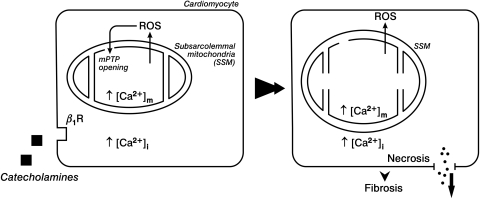
In recent years, two other factors, together with EICA, were identified to be major participants in a signal–transducer–effector pathway to cardiomyocyte necrosis during acute or chronic hyperadrenergic states (see Figure 2). This includes the genesis of oxidative stress, where the rate of reactive oxygen and nitrogen species generation overwhelms their rate of elimination by endogenous antioxidant defences, invoked in response to EICA. Second, the role of the mitochondrial inner membrane permeability transition pore (mPTP) opening which leads to organellar dysfunction, osmotic swelling, and ultimate structural degeneration of these organelles. Other pathophysiological responses that accompany catecholamine excess and which extend beyond the importance of Ca2+ overloading can also be cytotoxic. They cannot be overlooked and include a dyshomeostasis of essential cations which are manifested as hypokalaemia, ionized hypomagnesaemia and hypocalcaemia, hypozincaemia, and hyposelenaemia. Herein, we introduce and highlight this broader perspective of cation dyshomeostasis in revisiting the Fleckenstein hypothesis and cardiomyocyte necrosis.
Figure 2.
Catecholamine-mediated cellular and subcellular Ca2+ overloading with induction of oxidative stress and reactive oxygen species generation and opening of the mitochondrial inner membrane permeability transition pore that leads to solute entry, osmotic swelling and structural degeneration of these organelles. Cell death follows with a leak of intracellular troponins, which raise serum troponin levels, and ultimate appearance of replacement fibrosis, or scarring.
Acute stressor states and cation dyshomeostasis
Neurohormonal activation
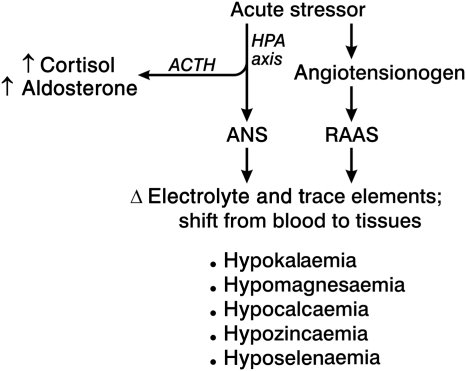
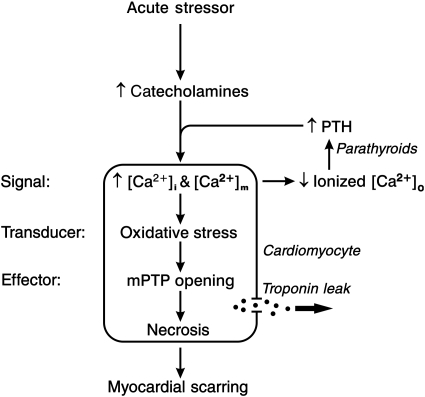
Acute stressor states are broadly referred to as representing acute bodily injury in one form or another. For example, they include: acute myocardial infarction; major cardiac or noncardiac surgery; thermal or electrical burns; head or musculoskeletal trauma; and subarachnoid haemorrhage or intracerebral bleed. An acute systemic inflammatory response invoked by sepsis or diabetic ketoacidosis is another example. Acute stressor states are inextricably linked to neurohormonal activation involving the HPA axis as well as the ANS and RAAS, and whose effector hormones are integral to acute stressor state-mediated homeostatic responses. Catecholamines, parathyroid hormone (PTH), angiotensin II, and endothelin-1 account for homeostasis gone awry to beget dyshomeostasis at cellular and molecular levels involving the heart and systemic organs. This includes a dyshomeostasis of mono- and divalent cations. At the time of or shortly after hospital admission, a dyshomeostasis of a whole host of electrolytes and trace elements are manifested contemporaneously in critically ill patients (Figure 3). These effector hormones orchestrate the concordant appearance of hypokalaemia, ionized hypocalcaemia and hypomagnesaemia, hypozincaemia and hyposelenaemia. The shift in electrolytes from blood to soft tissues accounts for ionized hypocalcaemia and hypomagnesaemia which will invoke secondary hyperparathyroidism (SHPT) with the parathyroid glands’ elaboration of the calcitropic PTH (Figure 4) seeking to restore the homeostasis of these circulating divalent cations through bone mineral resorption. Intracellular cation shifts, particularly catecholamine- and PTH-mediated EICA, converge on mitochondria to induce oxidative stress and raise the opening potential of their inner membrane mPTP (Figure 2). The ensuing loss of intracellular cationic homeostasis and diminished ATP synthesis, together with osmotic swelling of mitochondria, lead to organellar degeneration. Cardiomyocyte necrosis follows with the leakage of troponins ultimately appearing in the circulation as biomarkers confirmatory of necrosis.
Figure 3.
An acute stressor state, such as bodily injury, activates the hypothalamic–pituitary–adrenal axis with resultant release of adrenocorticotropin hormone, which promotes the adrenals’ release of cortisol and aldosterone, and catecholamines from the adrenal medulla. The acute phase reactant, angiotensinogen, is released by the liver during stressor states and is accompanied by activation of the renin–angiotensin–aldosterone system . In turn, elevated plasma catecholamines, norepinephrine, and epinephrine, promote a coordinated cation translocation from the vascular space to tissue compartment accounting for a concordant fall in their serum concentrations and presenting as hypokalaemia, ionized hypocalcaemia and hypomagnesaemia, hypozincaemia and hyposelenaemia.
Figure 4.
An acute stressor state with elevated circulating catecholamines is responsible for intracellular Ca2+ overloading with a subsequent fall in plasma ionized [Ca2+]o, which in turn provokes the parathyroid glands to release parathyroid hormone, a calcitropic hormone, also contributing to intracellular Ca2+ overloading. In cardiomyocytes this is accompanied by the induction of oxidative stress, which leads to the opening of the mitochondrial permeability transition pore and osmotic injury of these organelles. The necrosis of cardiomyocytes follows accompanied by the leak of intracellular troponins into the interstitial space accounting for the ultimate rise in plasma troponins. Cardiac myocytes lost to necrosis are replaced by fibrous tissue, or scarring, which preserves the structural integrity of the myocardium. Adapted from Whitted AD et al. Am J Med Sci. 2010;340:48–53.
Hypokalaemia
Catecholamines promote hypokalaemia. Struthers et al.26–28 administered intravenous epinephrine to normal human volunteers and demonstrated a prompt and marked fall in serum K+ of 0.8 ± 0.19 mEq/L (from 4.0 to 3.2 mEq/L) which was prevented by a β2-adrenergic receptor blocker. A simultaneous fall in serum Mg2+ and Ca2+ also occurred. In patients with acute bodily injury accompanied by haemorrhagic shock, endogenous plasma catecholamines are markedly elevated to promote arteriolar vasoconstriction and in so doing raise fallen arterial pressure. When these levels are further elevated by pharmacological doses of exogenous norepinephrine, epinephrine, or dopamine, given to further raise blood pressure from shock levels, the reductions in serum K+ (<3.0 mEq/dL) and Mg2+ (<1.5 mg/dL) can be more profound and lead to serious atrial and malignant ventricular arrhythmias.29
The underlying K+ balance prior to bodily injury determines the severity of the ensuing hypokalaemia during an acute stressor state. Pretreatment of normal volunteers with a thiazide diuretic predisposed them to marked hypokalaemia in response to epinephrine infusion.30 Spironolactone (Spiro), an aldosterone antagonist, was protective against hypokalaemia in this setting.31 Patients with arterial hypertension or CHF who are receiving long-term thiazide or loop diuretic treatment, respectively, may have marginal K+ and Mg2+ reservoirs, which are then further compromised by a hyperadrenergic state that accompanies bodily injury or acute myocardial infarction leading quickly to marked hypokalaemia and hypomagnesaemia with consequent QTc prolongation and a greater propensity for arrhythmias. Inhaled albuterol can likewise predispose to hypokalaemia and hypomagnesaemia in normal volunteers and those receiving diuretics.27 Chronic excessive use of β2 receptor agonists also lead to marked hypokalaemia and arrhythmias and injury to the heart and skeletal muscle.32 Drug-induced prolongation of myocardial repolarization, as reflected in the lengthening of the QTc interval of the electrocardiogram, usually accompany certain antibiotics, antidepressants, and antipsychotics.33,34 Prolongation of the QTc interval enhances the risk of polymorphic ventricular tachycardia, also known as torsades de pointes. Risk factors for drug-related QTc prolongation include hypokalaemia, sympathomimetics, and the concomitant administration of several of these agents.35 Furthermore, hypokalaemia has been associated with cardiomyocyte necrosis and resultant cardiac pathology.36
Hypomagnesaemia
Dietary Mg2+ deficiency can cause cardiovascular lesions that eventuate in heart failure.37,38 Elevations in plasma catecholamines associated with an acute stressor state are accompanied by hypomagnesaemia which is related to a cyclic AMP-mediated rise in intracellular Mg2+, together with increased lipolysis and Mg2+ binding to free fatty acids.39 Hypomagnesaemia is common in critically ill children and adults with such predisposing risk factors as hypokalaemia, hypocalcaemia, thiazide and loop diuretics, and sepsis. The hypomagnesaemia prevalent on admission in critically ill patients may worsen during prolonged hospital stay due to ongoing excretory losses and reduced Mg2+ intake.40–42 Moreover, atrial and ventricular arrhythmias appear when hypomagnesaemia is of moderate to marked severity (<1.70 mg/dL).43–45
Concurrent hypokalaemia and hypomagnesaemia
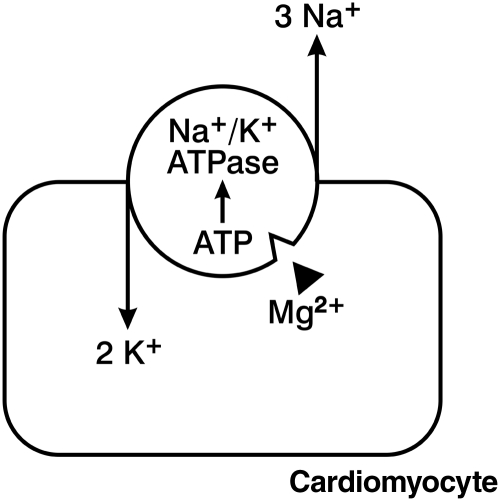
Contemporaneous hypokalaemia and hypomagnesaemia are common in critically ill patients. The interactions of K+ and Mg2+ are multifactorial and complex, including the importance of Mg2+ deficiency that interferes with K+ retention.46 The ability to successfully correct hypokalaemia mandates the simultaneous reversal of hypomagnesaemia.47–49 The cell membrane's Na+/K+-ATPase pump maintains the crucial electrochemical K+ gradient between high-intracellular K+ concentration with lower K+ concentration of the extracellular compartment (see Figure 5). Activated by Mg2+ this pump requires ATP as its energy source and hence Mg2+ participates in maintaining intracellular K+, which falters during Mg2+ deficiency with suboptimal amounts of K+ pumped into cells. As a result, Mg2+ deficiency contemporaneously begets K+ deficiency. Digoxin, a Na+/K+ ATPase inhibitor, can worsen this dyshomeostasis by limiting renal tubular reabsorption of Mg2+ and thereby raising urinary Mg2+ excretion which exacerbates hypomagnesaemia and further predisposes to arrhythmias in this setting.50 In order to resolve hypokalaemia, the Mg2+ deficiency must first or simultaneously be restored. In the absence of gastrointestinal losses or diuretic and digoxin usage, hypomagnesaemia and hypokalaemia due to impaired renal tubular reabsorption, in the form of urinary K+ and Mg2+ wasting, must be considered. Inheritable renal tubular disorders, such as the Gitelman syndrome in adults and Bartter syndrome in children, should be addressed when prompt resolution of these cations using oral Mg2+ and K+ supplements proves difficult to achieve.51 Regular serum electrolyte measurements should be augmented with serial ECG monitoring of the QTc interval, a useful biomarker of intracellular K+ and Mg2+ levels. QTc prolongation (>460 ms) demonstrates their deficiency while its normalization serves to address the adequacy of their cellular replacement. The attainment of QTc of <460 ms with these supplements may require several additional days compared with the relatively rapid return of their normal serum levels.
Figure 5.
The sodium pump of the cardiomyocyte is an energy consuming, Mg2+-dependent Na+/K+ ATPase which is responsible for the extrusion of three Na+ ions and entry of two K+ ions. Pump activity falters with Mg2+ deficiency accompanied by reduced intracellular K+ and prolongation of the QTc interval of the electrocardiogram. In the presence of hypokalaemia and hypomagnesaemia, digoxin, a Na+/K+ ATPase inhibitor, would further reduce intracellular K+ to raise the potential for arrhythmias.
Hypocalcaemia and intracellular Ca2+ overloading
Reductions in plasma ionized [Ca2+]o are commonly found in the emergency department and intensive care units in patients having an acute stressor state with elevated plasma catecholamines (Figure 4). The fall in [Ca2+]o correlates with the severity of the hyperadrenergic state and, in turn, the severity of illness. Ionized hypocalcaemia serves as an in-hospital predictor of survival.52–61 Hypoalbuminaemia can contribute to reduced total Ca2+ concentration. In response to hypocalcaemia, the Ca2+-sensing receptor of the parathyroid glands provokes stimulated secretion of PTH. The ensuing SHPT seeks to restore extracellular Ca2+ homeostasis by promoting the resorption of bone Ca2+ and increased Ca2+ absorption from the gut and kidneys. When hypocalcaemia is associated with hypomagnesaemia, PTH secretion may be impaired but can be rapidly resolved by reversing hypomagnesaemia.
The appearance of acute ionized hypocalcaemia in critically ill patients is caused by a shift in Ca2+ from the circulating pool to the intracellular compartment of various tissues, including the heart and skeletal muscle. This cation shift occurs in response to catecholamine-induced intracellular Ca2+ overloading followed by PTH-mediated excessive Ca2+ entry (Figure 4). Thus, catecholamine- and PTH-facilitated intracellular Ca2+ overloading of cardiomyocytes, in keeping with the Fleckenstein hypothesis, converge into mitochondrial Ca2+ overloading and is coupled to the induction of oxidative stress. The ensuing necrotic death of cardiomyocytes is followed by tissue repair and a consequent replacement fibrosis. Such scarring preserves the structural integrity of the myocardium. However, this structural remodelling has adverse consequences. These include compromised myocardial stiffness and ventricular function which collectively serve as substrate for reentrant arrhythmia.
The catecholamine-induced disintegration of necrotic cardiomyocytes is accompanied by the release of troponins, an intracellular enzyme that plays a crucial role in revealing myocardial injury (Figure 2). Catecholamine-induced cardiomyocyte necrosis with increased plasma troponin levels occur in critically ill patients, including those having sepsis, haemorrhagic shock, subarachnoid haemorrhage, trauma, gastrointestinal bleeding, or pulmonary embolus.62–65 The levels to which plasma troponins rise in such patients, however, do not reach the more marked elevations seen with the segmental loss of infarcted myocardium that accompanies an acute reductions in coronary blood flow due to a thrombosed coronary artery.
Hypozincaemia
Hypozincaemia appears in critically ill patients, including those having an acute myocardial infarction66–73 where it persists during much of the first week and then slowly recovers.74,75 It also appears during week 1 following major trauma and is related to excessive urinary excretion and fluid losses, reduced Zn2+ intake and preferential redistribution of Zn2+ to injured tissues.76 Tissue Zn2+ contributes to antioxidant defences, and are integral to wound healing.77–79 Hypozincaemia is frequently associated with hyposelenaemia.77,80,81
Hyposelenaemia
Hyposelenaemia has been identified on admission in patients with an acute myocardial infarction, where it correlates with the rise in serum troponin levels.82 In critically ill patients having the systemic inflammatory response syndrome, hyposelenaemia is accompanied by reduced plasma Se-glutathione peroxidase (GSHPx) activity.83 Since thyroid hormone is a selenoprotein, thyroid function can be compromised with hyposelenaemia.
Summary
The complex dyshomeostasis of electrolytes and trace elements that occurs with acute stressor states has broad and diverse pathophysiological sequelae, including cardiomyocyte necrosis. To minimize adverse cardiovascular consequences during hyperadrenergic states, systematic and serial surveillance of serum K+, Mg2+, and Ca2+ is warranted. Complementary protective measures should include QTc interval monitoring with serial ECG, a biomarker of myocardial repolarization. Prolonged QTc, due to reduced intracellular K+ and Mg2+ or to drug therapy, raises the vulnerability of the heart to atrial and/or ventricular arrhythmias. The maintenance of serum K+ and Mg2+ within the strictly defined narrow physiological threshold (i.e. K+ ≥4.0 mEq/L and Mg2+ ≥2.0 mg/dL) will inevitably prove most effective in preventing arrhythmias. An awareness of hypozincaemia and hyposelenaemia also broadens our clinical perspective on the acute stressor state paradigm to include their deleterious impacts on the compromised efficiency of metalloenzyme-based antioxidant defences to combat oxidative stress.
Chronic stressor states and cation dyshomeostasis
Chronic stressor states include: a failure of the heart, kidneys, lungs, or liver, irrespective of aetiological origins; and chronic inflammatory diseases, such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. We now focus on the chronic neurohormonal activation involving the HPA axis, ANS, and RAAS which are integral pathophysiological features of CHF, and which occurs irrespective of its aetiological origins or patient age. Elevated plasma levels of cortisol, renin activity, angiotensin II, aldosterone, epinephrine, norepinephrine, and endothelin–1 are each found in CHF.84–88
Hypokalaemia and hypomagnesaemia
Renin–angiotensin–aldosterone system activation in patients with systolic or diastolic heart failure leads to a salt-avid state with Na+ and water retention that eventuates in the appearance of symptoms and signs of the CHF syndrome. Urinary and faecal excretion of K+ and Mg2+ are increased during CHF based on the endocrine-mediated actions of circulating aldosterone acting at these sites, where high-density aldosterone receptor binding occurs. The loss of these cations is accentuated by loop diuretics commonly used in the management of CHF.47,89 Chronic hypomagnesaemia is frequently associated with hypokalaemia and hypocalcaemia and portends an adverse prognosis.90 Loop as well as thiazide diuretics promote excessive urinary loss of K+ and Mg2+ that can lead to both hypokalaemia and hypomagnesaemia. Combining either of these diuretics with Spiro preserves K+ and Mg2+ homeostasis,30 provided renal function is not markedly impaired (serum creatinine <2.0 mg/dL) and K+ supplements are discontinued.
The importance of hypokalaemia on patient mortality has been well documented. The Digitalis Investigative Group (DIG) trial database involving more than 7700 patients revealed that in ambulatory patients having either systolic or diastolic heart failure, serum K+ <4.0 mEq/L and Mg2+ <2.0 mg/dL were associated with increased mortality.91,92 The same was true in patients with heart failure having associated chronic kidney disease.93 This database also revealed the adverse impact of loop diuretics on death, cardiovascular mortality, and heart failure-related hospitalization in ambulatory patients, including the elderly.94,95 This raises the prospect that prolonged routine use of a potent loop diuretic, in the absence of symptoms and signs of salt avidity, can be quite deleterious and should be discontinued and milder diuretics implemented, if necessary, in salt-sensitive patients.96 However, the loop diuretic can be reinstituted, if and when the patient is again avidly and persistently retaining Na+ and water.
In the Study of Left Ventricular Dysfunction (SOLVD) trial with a cohort of more than 6700 patients, such adverse events were not seen with potassium-sparing diuretics, such as Spiro, amiloride, or triamterene. Indeed, these agents may be associated with reduced risk of all-cause mortality or death from or hospitalization for progressive heart failure.97–99 Spiro, an aldosterone receptor antagonist, conserves both K+ and Mg2+. In the Randomized Aldactone Evaluation (RALES) trial the efficacy and safety of Spiro, when combined with an ACE-Inhibitor or angiotensin receptor blocker and a loop diuretic, was demonstrated and included a 30% risk reduction for all-cause and cardiovascular-related mortality and sudden cardiac death and cardiovascular morbidities.99
Ionized hypocalcaemia and intracellular Ca2+ overloading
The secondary aldosteronism of CHF in man leads to increased faecal and urinary Ca2+ excretion and consequent ionized hypocalcaemia and, in turn, SHPT with elevated plasma PTH levels.80,100–103 As noted earlier, dyshomeostasis of divalent cations frequently occurs in patients hospitalized with decompensated biventricular failure having a dilated cardiomyopathy. Elevated plasma PTH levels and SHPT are also found in patients with pulmonary hypertension or obstructive airway disease,104,105 in which RAAS activation with secondary aldosteronism is expected due to reduced systemic blood flow that includes renal perfusion. This hormonal profile is found in patients with primary aldosteronism,106–109 where aberrations in serum ionized and total Ca2+, together with elevated PTH, are normalized by either Spiro or adrenal surgery.108,109 Furthermore, elevated PTH is a known stimulus to adrenal aldosterone production and can further account for elevated plasma aldosterone levels. In patients with primary hyperparathyroidism, preoperative PTH levels in excess of 100 ng/mL are independent predictors of abnormally elevated plasma aldosterone levels.110 The impact of chronic aldosteronism on the increased incidence of adverse cardiovascular outcomes in patients with primary hyperparathyroidism remains uncertain.111 However, experimental findings congruently point towards the importance of PTH-mediated intracellular Ca2+ overloading and induction of oxidative stress as major pathogenic events accounting for adverse myocardial remodelling, as contrasted to elevations in circulating aldosterone, per se.112–114
Abnormal elevations in serum PTH (>65 pg/mL), a calcitropic hormone and mediator of EICA in cardiomyocytes and mitochondria,112,115,116 are found in patients hospitalized with decompensated heart failure and those awaiting cardiac transplantation.100,103,117,118 In outpatients having heart failure, elevated serum PTH levels are also identified and serve as an independent predictor of CHF and the need for hospitalization.119–121 Plasma PTH levels were shown to be an independent risk factor for mortality and cardiovascular events in patients undergoing coronary angiography in Austria,122 and increased risk for cardiovascular mortality and the risk of heart failure were predicted in a community-based cohort of elderly men followed longitudinally for 8 years or more in Sweden.123,124 We found SHPT to be especially prevalent in African-Americans (AA) with protracted decompensated biventricular failure, where chronic elevations in plasma aldosterone account for symptoms and signs of CHF.103 Secondary hyperparathyroidism is also related to the prevalence of hypovitaminosis D in AA with CHF.103 The increased melanin content of darker skin in AA serves as a natural sunscreen. Accordingly, the prevalence of hypovitaminosis D, often of marked severity (<10 ng/mL), compromises Ca2+ homeostasis predisposing AA to hypocalcaemia and consequent SHPT.103,125,126 Vitamin D deficiency is also common in Caucasians and Asians with heart failure.119,127–129
Other factors which may be associated with compromised Ca2+ stores and contribute to the appearance of SHPT, especially in AA with CHF, include: reduced dietary Ca2+ intake because of lactose intolerance and an active avoidance of dairy products rich in Ca2+130; and a preference for a high-Na+ diet that enhances urinary Ca2+ excretion. A high-salt diet and consequential hypercalciuria is well known for predisposing patients to ionized hypocalcaemia and SHPT with resorption of bone which is invoked to restore extracellular Ca2+ homeostasis. Over time, osteopenia and osteoporosis appear as an adverse outcome to SHPT invoked by the hypercalciuria of long-term dietary Na+ excess further predisposing to atraumatic bone fractures.131,132 Patients with heart failure have reduced bone density, which is related to SHPT and vitamin D deficiency coupled with reduced physical activity that may be a cofactor of their effort intolerance due to symptomatic failure.100,117,133–137 The risk of such fractures is increased in elderly patients with heart failure,138 where SHPT may be contributory, and which appears to be preventable when Spiro is combined with today's standard of care.139
Elevations in serum troponins, biomarkers of cardiomyocyte necrosis, but not due to acute MI or renal failure, are found in patients hospitalized because of their decompensated heart failure and are associated with increased in-hospital and overall cardiac mortality.5–14 The role of intracellular Ca2+ overloading and oxidative stress, induced by neurohormonal activation that includes calcitropic hormones, catecholamines and PTH, in promoting myocardial cell loss in these patients is not absolutely clear, but must be explored. An ongoing loss of cardiomyocytes contributes to the progressive nature of heart failure.
Zn2+ and Se2+ dyshomeostasis
In addition to hypokalaemia, ionized hypocalcaemia and hypomagnesaemia that accompany increased urinary and faecal losses of these divalent cations with the aldosteronism of CHF, there also is a concomitant dyshomeostasis of Zn2+ with hypozincaemia.81,140 Furthermore, urinary Zn2+ excretion is increased in response to angiotensin-converting enzyme inhibitor or angiotensin receptor antagonist, commonly prescribed agents in the management of patients with CHF and where hypozincaemia is associated with abnormalities in taste (or dysgeusia).141,142 Serum Zn2+ and Se2+ levels are reduced in AA patients.80,102 This includes those with decompensated failure and compensated failure, as well as with heart disease but without heart failure. Interactions between Zn2+ and Se2+ have been reported.143 Underlying causes for the simultaneous deficiencies of these divalent cations in AA, including inadequate dietary intake, are presently uncertain.
The prooxidant effect representing intracellular Ca2+ overloading that accompanies elevations in either plasma catecholamines or PTH is intrinsically coupled to Zn2+ entry acting as an antioxidant.115,116,144,145 Although less robust, Zn2+ entry is known to occur via L-type Ca2+ channels whereas more substantive amounts ingress by Zn2+ transporters activated by oxidative stress. The release of inactive Zn2+ bound to metallothionein-1 contributes to increased cytosolic-free levels of Zn2+, which can also be achieved by a ZnSO4 supplement or Zn2+ ionophore.145,146 These cumulative salutary observations raise the therapeutic prospect that cation-containing nutriceuticals capable of favourably influencing extra- and intracellular Ca2+ and Zn2+ equilibrium, which is pivotal to combating oxidative injury and promoting repair, could attenuate or even prevent cardiomyocyte necrosis and myocardial scarring.
Selenium is a cofactor of antioxidant selenoenzymes, such as GSH-Px and thioredoxin reductase, that promote optimal antioxidant/oxidant balance.147 Monitoring serum Se levels, Se-dependent enzymatic activities, and Se-GSH-Px mRNA expression are clinically useful in addressing optimal Se supplementation.148,149 Appearance of a dilated cardiomyopathy in greater abundance has been reported in general populations, in which dietary Se2+ deficiencies are found, such as in the Se-poor soil of the Keysan Province of China, or when parenteral nutrition was inadvertently deficient in Zn and/or Se.150–152 The selenium-deficiency-induced cardiomyopathy is often reversible with Se2+ replacement.153
Summary
Thus, neurohormonal activation that accompanies CHF is comparable with acute stressor states (Table 1). Together with the adverse impact of loop diuretics, there is a concerted and contemporaneous complex dyshomeostasis of K+, Mg2+, and Ca2+ associated with adverse pathophysiological consequences. Compromised Ca2+ stores related to excretory losses and/or altered dietary intake, together with vitamin D deficiency, predispose to SHPT with compromised cardiomyocyte survival and impaired skeletal health.
Table 1.
A common signal–transducer–effector pathway to cardiomyocyte necrosis in acute and chronic stressor states
| Stressor state |
||
|---|---|---|
| Acute | Chronic | |
| Neurohormonal activation | ||
| HPA axis | + | + |
| ANS | + | + |
| RAAS | + | + |
| Cation dyshomeostasis | ||
| ↑ [Ca2+]i & [Ca2+]m | + | + |
| ↑ [Zn2+]i & [Zn2+]m | ± | + |
| Oxidative stress > antioxidant defences | + | + |
| mPTP opening | + | + |
Taken together, the multitude of evidence gathered to date congruently supports the Fleckenstein hypothesis which invokes catecholamine- and PTH-mediated intracellular Ca2+ overloading as the most tenable mechanism leading to the induction of oxidative stress, where ROS and RNS, primarily derived from mitochondria in cardiomyocytes and membrane-bound NADPH oxidase in vascular tissue, overwhelm cellular antioxidant defences. This scenario anticipates the question whether ensuing adverse consequences are the result of an excessive generation of prooxidants or due to compromised endogenous antioxidant defences, or both. Zn2+ supplementation, serving as antioxidant, has shown promise in enhancing antioxidant defences in experimental animals receiving aldosterone/salt treatment or having streptozocin-induced diabetes.115,145,146,154 A polynutrient supplement, however, which includes these cations and vitamin D, at a minimum, will likely be necessary. Promising results with a polynutrient supplement have been reported in critically ill patients, including those with heart failure.155–159
Summary and conclusions
Acute and chronic stressor states are each accompanied by neurohormonal activation that includes the ANS. As Fleckenstein and coworkers originally envisaged, the hyperadrenergic state is accompanied by cardiomyocyte Ca2+ overloading, particularly involving their mitochondria, with resultant dysfunction and disintegration of the organelles and ensuing necrotic cell death. More recent studies have identified subsarcolemmal mitochondria-based induction of oxidative stress and opening of their inner membrane mPTP as other major components of the pathophysiological signal–transducer–effector pathway to cardiomyocyte necrosis which eventuates in the release of troponins causing elevated serum troponins and a consequent wound healing response leading to scattered foci of microscopic scarring. Fibrosis is a major component to the adverse structural remodelling of failing myocardium and whose ongoing appearance accounts for the progressive failure of this normally efficient muscular pump.
Furthermore, neurohormonal activation, including HPA axis, ANS and RAAS, and their effector hormones, orchestrate the concordant appearance of hypokalaemia, ionized hypocalcaemia and hypomagnesaemia, hypozincaemia and hyposelenaemia, and is based on the coordinated translocation of cations to injured tissues. Intracellular cation shifts adaptively regulate the equilibrium between prooxidants and antioxidants, a critical determinant of cardiomyocyte survival. The intrinsically coupled dyshomeostasis of Ca2+ and Zn2+, representing prooxidant and antioxidant, respectively, can be uncoupled in favour of increased intracellular-free Zn2+ and antioxidant defences. In so doing, cardiomyocytes that are on the brink of necrotic death can be rescued. The use of nutriceuticals to achieve these lofty goals ought to be considered as complementary to today's standard of care using pharmaceuticals alone.
Funding
This work was supported, in part, by National Institutes of Health grants [R01-HL73043 and R01–HL90867] to KTW. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Authors have no conflicts of interest to disclose.
Conflict of interest: none declared.
References
- 1.Matzinger P. The danger model: a renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. doi:10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 2.Gallucci S, Matzinger P. Danger signals: SOS to the immune system. Curr Opin Immunol. 2001;13:114–119. doi: 10.1016/s0952-7915(00)00191-6. doi:10.1016/S0952-7915(00)00191-6. [DOI] [PubMed] [Google Scholar]
- 3.Todryk SM, Melcher AA, Dalgleish AG, Vile RG. Heat shock proteins refine the danger theory. Immunology. 2000;99:334–337. doi: 10.1046/j.1365-2567.2000.00002.x. doi:10.1046/j.1365-2567.2000.00002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beltrami CA, Finato N, Rocco M, Feruglio GA, Puricelli C, Cigola E, Quaini F, Sonnenblick EH, Olivetti G, Anversa P. Structural basis of end-stage failure in ischemic cardiomyopathy in humans. Circulation. 1994;89:151–163. doi: 10.1161/01.cir.89.1.151. [DOI] [PubMed] [Google Scholar]
- 5.Ishii J, Nomura M, Nakamura Y, Naruse H, Mori Y, Ishikawa T, Ando T, Kurokawa H, Kondo T, Nagamura Y, Ezaki K, Hishida H. Risk stratification using a combination of cardiac troponin T and brain natriuretic peptide in patients hospitalized for worsening chronic heart failure. Am J Cardiol. 2002;89:691–695. doi: 10.1016/s0002-9149(01)02341-4. doi:10.1016/S0002-9149(01)02341-4. [DOI] [PubMed] [Google Scholar]
- 6.Kuwabara Y, Sato Y, Miyamoto T, Taniguchi R, Matsuoka T, Isoda K, Yamane K, Nishi K, Fujiwara H, Takatsu Y. Persistently increased serum concentrations of cardiac troponin in patients with acutely decompensated heart failure are predictive of adverse outcomes. Circ J. 2007;71:1047–1051. doi: 10.1253/circj.71.1047. doi:10.1253/circj.71.1047. [DOI] [PubMed] [Google Scholar]
- 7.Peacock WF, IV, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AH. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008;358:2117–2126. doi: 10.1056/NEJMoa0706824. doi:10.1056/NEJMoa0706824. [DOI] [PubMed] [Google Scholar]
- 8.Zairis MN, Tsiaousis GZ, Georgilas AT, Makrygiannis SS, Adamopoulou EN, Handanis SM, Batika PC, Prekates AA, Velissaris D, Kouris NT, Mytas DZ, Babalis DK, Karidis KS, Foussas SG. Multimarker strategy for the prediction of 31 days cardiac death in patients with acutely decompensated chronic heart failure. Int J Cardiol. 2009;141:284–290. doi: 10.1016/j.ijcard.2008.12.017. doi:10.1016/j.ijcard.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Löwbeer C, Gustafsson SA, Seeberger A, Bouvier F, Hulting J. Serum cardiac troponin T in patients hospitalized with heart failure is associated with left ventricular hypertrophy and systolic dysfunction. Scand J Clin Lab Invest. 2004;64:667–676. doi: 10.1080/00365510410003002. doi:10.1080/00365510410003002. [DOI] [PubMed] [Google Scholar]
- 10.Horwich TB, Patel J, MacLellan WR, Fonarow GC. Cardiac troponin I is associated with impaired hemodynamics, progressive left ventricular dysfunction, and increased mortality rates in advanced heart failure. Circulation. 2003;108:833–838. doi: 10.1161/01.CIR.0000084543.79097.34. doi:10.1161/01.CIR.0000084543.79097.34. [DOI] [PubMed] [Google Scholar]
- 11.Sukova J, Ostadal P, Widimsky P. Profile of patients with acute heart failure and elevated troponin I levels. Exp Clin Cardiol. 2007;12:153–156. [PMC free article] [PubMed] [Google Scholar]
- 12.Ilva T, Lassus J, Siirilä-Waris K, Melin J, Peuhkurinen K, Pulkki K, Nieminen MS, Mustonen H, Porela P, Harjola VP. Clinical significance of cardiac troponins I and T in acute heart failure. Eur J Heart Fail. 2008;10:772–779. doi: 10.1016/j.ejheart.2008.06.009. doi:10.1016/j.ejheart.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Sato Y, Nishi K, Taniguchi R, Miyamoto T, Fukuhara R, Yamane K, Saijyo S, Tanada Y, Yamamoto E, Goto T, Takahashi N, Fujiwara H, Takatsu Y. In patients with heart failure and non-ischemic heart disease, cardiac troponin T is a reliable predictor of long-term echocardiographic changes and adverse cardiac events. J Cardiol. 2009;54:221–230. doi: 10.1016/j.jjcc.2009.05.007. doi:10.1016/j.jjcc.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Miller WL, Hartman KA, Burritt MF, Grill DE, Jaffe AS. Profiles of serial changes in cardiac troponin T concentrations and outcome in ambulatory patients with chronic heart failure. J Am Coll Cardiol. 2009;54:1715–1721. doi: 10.1016/j.jacc.2009.07.025. doi:10.1016/j.jacc.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 15.Sundström J, Ingelsson E, Berglund L, Zethelius B, Lind L, Venge P, Arnlöv J. Cardiac troponin-I and risk of heart failure: a community-based cohort study. Eur Heart J. 2009;30:773–781. doi: 10.1093/eurheartj/ehp047. doi:10.1093/eurheartj/ehp047. [DOI] [PubMed] [Google Scholar]
- 16.Tan LB, Burniston JG, Clark WA, Ng Y, Goldspink DF. Characterization of adrenoceptor involvement in skeletal and cardiac myotoxicity induced by sympathomimetic agents: toward a new bioassay for beta-blockers. J Cardiovasc Pharmacol. 2003;41:518–525. doi: 10.1097/00005344-200304000-00003. doi:10.1097/00005344-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Goldspink DF, Burniston JG, Ellison GM, Clark WA, Tan LB. Catecholamine-induced apoptosis and necrosis in cardiac and skeletal myocytes of the rat in vivo: the same or separate death pathways? Exp Physiol. 2004;89:407–416. doi: 10.1113/expphysiol.2004.027482. doi:10.1113/expphysiol.2004.027482. [DOI] [PubMed] [Google Scholar]
- 18.Benjamin IJ, Jalil JE, Tan LB, Cho K, Weber KT, Clark WA. Isoproterenol-induced myocardial fibrosis in relation to myocyte necrosis. Circ Res. 1989;65:657–670. doi: 10.1161/01.res.65.3.657. [DOI] [PubMed] [Google Scholar]
- 19.Fleckenstein A, Kanke J, Döring HJ, Leder O. Key role of Ca in the production of noncoronarogenic myocardial necroses. Recent Adv Stud Cardiac Struct Metab. 1975;6:21–32. [PubMed] [Google Scholar]
- 20.Lossnitzer K, Janke J, Hein B, Stauch M, Fleckenstein A. Disturbed myocardial calcium metabolism: a possible pathogenetic factor in the hereditary cardiomyopathy of the Syrian hamster. Recent Adv Stud Cardiac Struct Metab. 1975;6:207–217. [PubMed] [Google Scholar]
- 21.Bier CB, Rona G. Mineralocorticoid potentiation of isoproterenol-induced myocardial injury: Ultrastructural equivalent. J Mol Cell Cardiol. 1979;11:961–966. doi: 10.1016/0022-2828(79)90387-0. doi:10.1016/0022-2828(79)90387-0. [DOI] [PubMed] [Google Scholar]
- 22.Rona G, Boutet M, Huttner I. Reperfusion injury. A possible link between catecholamine-induced and ischemic myocardial alterations. Adv Myocardiol. 1983;4:427–439. [PubMed] [Google Scholar]
- 23.Yates JC, Taam GM, Singal PK, Beamish RE, Dhalla NS. Modification of adrenochrome-induced cardiac contractile failure and cell damage by changes in cation concentrations. Lab Invest. 1980;43:316–326. [PubMed] [Google Scholar]
- 24.Singal PK, Forbes MS, Sperelakis N. Occurrence of intramitochondrial Ca2+ granules in a hypertrophied heart exposed to adriamycin. Can J Physiol Pharmacol. 1984;62:1239–1244. doi: 10.1139/y84-207. [DOI] [PubMed] [Google Scholar]
- 25.Bybee KA, Prasad A. Stress-related cardiomyopathy syndromes. Circulation. 2008;118:397–409. doi: 10.1161/CIRCULATIONAHA.106.677625. doi:10.1161/CIRCULATIONAHA.106.677625. [DOI] [PubMed] [Google Scholar]
- 26.Brown MJ, Brown DC, Murphy MB. Hypokalemia from beta2-receptor stimulation by circulating epinephrine. N Engl J Med. 1983;309:1414–1419. doi: 10.1056/NEJM198312083092303. doi:10.1056/NEJM198312083092303. [DOI] [PubMed] [Google Scholar]
- 27.Reid JL, Whyte KF, Struthers AD. Epinephrine-induced hypokalemia: the role of beta adrenoceptors. Am J Cardiol. 1986;57:23F–27F. doi: 10.1016/0002-9149(86)90884-2. doi:10.1016/0002-9149(86)90884-2. [DOI] [PubMed] [Google Scholar]
- 28.Hansen O, Johansson BW, Nilsson-Ehle P. Metabolic, electrocardiographic, and hemodynamic responses to increased circulating adrenaline: effects of selective and nonselective beta adrenoceptor blockade. Angiology. 1990;41:175–188. doi: 10.1177/000331979004100302. doi:10.1177/000331979004100302. [DOI] [PubMed] [Google Scholar]
- 29.Tarditi DJ, Hollenberg SM. Cardiac arrhythmias in the intensive care unit. Semin Respir Crit Care Med. 2006;27:221–229. doi: 10.1055/s-2006-945525. doi:10.1055/s-2006-945525. [DOI] [PubMed] [Google Scholar]
- 30.Struthers AD, Whitesmith R, Reid JL. Prior thiazide diuretic treatment increases adrenaline-induced hypokalaemia. Lancet. 1983;1:1358–1361. doi: 10.1016/s0140-6736(83)92140-2. doi:10.1016/S0140-6736(83)92140-2. [DOI] [PubMed] [Google Scholar]
- 31.Lipworth BJ, McDevitt DG, Struthers AD. Hypokalemic and ECG sequelae of combined beta-agonist/diuretic therapy. Protection by conventional doses of spironolactone but not triamterene. Chest. 1990;98:811–815. doi: 10.1378/chest.98.4.811. doi:10.1378/chest.98.4.811. [DOI] [PubMed] [Google Scholar]
- 32.Burniston JG, Clark WA, Tan LB, Goldspink DF. Dose-dependent separation of the hypertrophic and myotoxic effects of the beta(2)-adrenergic receptor agonist clenbuterol in rat striated muscles. Muscle Nerve. 2006;33:655–663. doi: 10.1002/mus.20504. doi:10.1002/mus.20504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta A, Lawrence AT, Krishnan K, Kavinsky CJ, Trohman RG. Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes. Am Heart J. 2007;153:891–899. doi: 10.1016/j.ahj.2007.01.040. doi:10.1016/j.ahj.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 34.Buckley MS, Leblanc JM, Cawley MJ. Electrolyte disturbances associated with commonly prescribed medications in the intensive care unit. Crit Care Med. 2010;38:S253–S264. doi: 10.1097/CCM.0b013e3181dda0be. doi:10.1097/CCM.0b013e3181dda0be. [DOI] [PubMed] [Google Scholar]
- 35.Curtis LH, Østbye T, Sendersky V, Hutchison S, Allen LaPointe NM, Al-Khatib SM, Usdin Yasuda S, Dans PE, Wright A, Califf RM, Woosley RL, Schulman KA. Prescription of QT-prolonging drugs in a cohort of about 5 million outpatients. Am J Med. 2003;114:135–141. doi: 10.1016/s0002-9343(02)01455-9. doi:10.1016/S0002-9343(02)01455-9. [DOI] [PubMed] [Google Scholar]
- 36.Darrow DC, Miller HC. The production of cardiac lesions by repeated injections of desoxycorticosterone acetate. J Clin Invest. 1942;21:601–611. doi: 10.1172/JCI101338. doi:10.1172/JCI101338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weglicki WB, Mak IT, Stafford RE, Dickens BF, Cassidy MM, Phillips TM. Neurogenic peptides and the cardiomyopathy of magnesium-deficiency: effects of substance P-receptor inhibition. Mol Cell Biochem. 1994;130:103–109. doi: 10.1007/BF01457391. doi:10.1007/BF01457391. [DOI] [PubMed] [Google Scholar]
- 38.Kramer JH, Spurney C, Iantorno M, Tziros C, Mak IT, Tejero-Taldo MI, Chmielinska JJ, Komarov A, Weglicki WB. Neurogenic inflammation and cardiac dysfunction due to hypomagnesemia. Am J Med Sci. 2009;338:22–27. doi: 10.1097/MAJ.0b013e3181aaee4d. doi:10.1097/MAJ.0b013e3181aaee4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rayssiguier Y. Hypomagnesemia resulting from adrenaline infusion in ewes: its relation to lipolysis. Horm Metab Res. 1977;9:309–314. doi: 10.1055/s-0028-1093519. doi:10.1055/s-0028-1093519. [DOI] [PubMed] [Google Scholar]
- 40.Escuela MP, Guerra M, Añon JM, Martínez-Vizcaino V, Zapatero MD, Garcia-Jalón A, Celaya S. Total and ionized serum magnesium in critically ill patients. Intensive Care Med. 2005;31:151–156. doi: 10.1007/s00134-004-2508-x. doi:10.1007/s00134-004-2508-x. [DOI] [PubMed] [Google Scholar]
- 41.Ryzen E. Magnesium homeostasis in critically ill patients. Magnesium. 1989;8:201–212. [PubMed] [Google Scholar]
- 42.Ueshima K, Tachibana H, Suzuki T, Hiramori K. Factors affecting the blood concentration of ionized magnesium in patients in the acute phase of myocardial infarction. Heart Vessels. 2004;19:267–270. doi: 10.1007/s00380-004-0782-8. doi:10.1007/s00380-004-0782-8. [DOI] [PubMed] [Google Scholar]
- 43.Ceremuzynski L, Van Hao N. Ventricular arrhythmias late after myocardial infarction are related to hypomagnesemia and magnesium loss: preliminary trial of corrective therapy. Clin Cardiol. 1993;16:493–496. doi: 10.1002/clc.4960160607. doi:10.1002/clc.4960160607. [DOI] [PubMed] [Google Scholar]
- 44.Saleem AF, Haque A. On admission hypomagnesemia in critically ill children: Risk factors and outcome. Indian J Pediatr. 2009;76:1227–1230. doi: 10.1007/s12098-009-0258-z. doi:10.1007/s12098-009-0258-z. [DOI] [PubMed] [Google Scholar]
- 45.Safavi M, Honarmand A. Admission hypomagnesemia–impact on mortality or morbidity in critically ill patients. Middle East J Anesthesiol. 2007;19:645–660. [PubMed] [Google Scholar]
- 46.Sheehan JP, Seelig MS. Interactions of magnesium and potassium in the pathogenesis of cardiovascular disease. Magnesium. 1984;3:301–314. [PubMed] [Google Scholar]
- 47.Leier CV, Dei Cas L, Metra M. Clinical relevance and management of the major electrolyte abnormalities in congestive heart failure: hyponatremia, hypokalemia, and hypomagnesemia. Am Heart J. 1994;128:564–574. doi: 10.1016/0002-8703(94)90633-5. doi:10.1016/0002-8703(94)90633-5. [DOI] [PubMed] [Google Scholar]
- 48.Milionis HJ, Alexandrides GE, Liberopoulos EN, Bairaktari ET, Goudevenos J, Elisaf MS. Hypomagnesemia and concurrent acid-base and electrolyte abnormalities in patients with congestive heart failure. Eur J Heart Fail. 2002;4:167–173. doi: 10.1016/s1388-9842(01)00234-3. doi:10.1016/S1388-9842(01)00234-3. [DOI] [PubMed] [Google Scholar]
- 49.Kraft MD, Btaiche IF, Sacks GS, Kudsk KA. Treatment of electrolyte disorders in adult patients in the intensive care unit. Am J Health Syst Pharm. 2005;62:1663–1682. doi: 10.2146/ajhp040300. doi:10.2146/ajhp040300. [DOI] [PubMed] [Google Scholar]
- 50.Schwinger RH, Erdmann E. Heart failure and electrolyte disturbances. Methods Find Exp Clin Pharmacol. 1992;14:315–325. [PubMed] [Google Scholar]
- 51.Adeboye AA, Borkowski BJ, Weber KT. Atrial and ventricular arrhythmias in a woman with prolonged QTc, hypokalemia, hypomagnesemia and a metabolic alkalosis [abstr] J Investig Med. 2010;58:365. [Google Scholar]
- 52.Carlstedt F, Lind L, Joachimsson PO, Rastad J, Wide L, Ljunghall S. Circulating ionized calcium and parathyroid hormone levels following coronary artery by-pass surgery. Scand J Clin Lab Invest. 1999;59:47–53. doi: 10.1080/00365519950185995. doi:10.1080/00365519950185995. [DOI] [PubMed] [Google Scholar]
- 53.Carlstedt F, Lind L, Rastad J, Stjernstrom H, Wide L, Ljunghall S. Parathyroid hormone and ionized calcium levels are related to the severity of illness and survival in critically ill patients. Eur J Clin Invest. 1998;28:898–903. doi: 10.1046/j.1365-2362.1998.00391.x. doi:10.1046/j.1365-2362.1998.00391.x. [DOI] [PubMed] [Google Scholar]
- 54.Carlstedt F, Lind L, Wide L, Lindahl B, Hänni A, Rastad J, Ljunghall S. Serum levels of parathyroid hormone are related to the mortality and severity of illness in patients in the emergency department. Eur J Clin Invest. 1997;27:977–981. doi: 10.1046/j.1365-2362.1997.2310778.x. doi:10.1046/j.1365-2362.1997.2310778.x. [DOI] [PubMed] [Google Scholar]
- 55.Hästbacka J, Pettilä V. Prevalence and predictive value of ionized hypocalcemia among critically ill patients. Acta Anaesthesiol Scand. 2003;47:1264–1269. doi: 10.1046/j.1399-6576.2003.00236.x. doi:10.1046/j.1399-6576.2003.00236.x. [DOI] [PubMed] [Google Scholar]
- 56.Choi YC, Hwang SY. The value of initial ionized calcium as a predictor of mortality and triage tool in adult trauma patients. J Korean Med Sci. 2008;23:700–705. doi: 10.3346/jkms.2008.23.4.700. doi:10.3346/jkms.2008.23.4.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cherry RA, Bradburn E, Carney DE, Shaffer ML, Gabbay RA, Cooney RN. Do early ionized calcium levels really matter in trauma patients? J Trauma. 2006;61:774–779. doi: 10.1097/01.ta.0000239516.49799.63. doi:10.1097/01.ta.0000239516.49799.63. [DOI] [PubMed] [Google Scholar]
- 58.Dickerson RN, Henry NY, Miller PL, Minard G, Brown RO. Low serum total calcium concentration as a marker of low serum ionized calcium concentration in critically ill patients receiving specialized nutrition support. Nutr Clin Pract. 2007;22:323–328. doi: 10.1177/0115426507022003323. doi:10.1177/0115426507022003323. [DOI] [PubMed] [Google Scholar]
- 59.Burchard KW, Simms HH, Robinson A, DiAmico R, Gann DS. Hypocalcemia during sepsis. Relationship to resuscitation and hemodynamics. Arch Surg. 1992;127:265–272. doi: 10.1001/archsurg.1992.01420030027005. [DOI] [PubMed] [Google Scholar]
- 60.Joborn H, Hjemdahl P, Larsson PT, Lithell H, Lundin L, Wide L, Ljunghall S. Platelet and plasma catecholamines in relation to plasma minerals and parathyroid hormone following acute myocardial infarction. Chest. 1990;97:1098–1105. doi: 10.1378/chest.97.5.1098. doi:10.1378/chest.97.5.1098. [DOI] [PubMed] [Google Scholar]
- 61.Karlsberg RP, Cryer PE, Roberts R. Serial plasma catecholamine response early in the course of clinical acute myocardial infarction: relationship to infarct extent and mortality. Am Heart J. 1981;102:24–29. doi: 10.1016/0002-8703(81)90408-7. doi:10.1016/0002-8703(81)90408-7. [DOI] [PubMed] [Google Scholar]
- 62.Gunnewiek JM, Van Der Hoeven JG. Cardiac troponin elevations among critically ill patients. Curr Opin Crit Care. 2004;10:342–346. doi: 10.1097/01.ccx.0000135514.20538.44. doi:10.1097/01.ccx.0000135514.20538.44. [DOI] [PubMed] [Google Scholar]
- 63.Jeremias A, Gibson CM. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med. 2005;142:786–791. doi: 10.7326/0003-4819-142-9-200505030-00015. [DOI] [PubMed] [Google Scholar]
- 64.Maeder M, Fehr T, Rickli H, Ammann P. Sepsis-associated myocardial dysfunction: diagnostic and prognostic impact of cardiac troponins and natriuretic peptides. Chest. 2006;129:1349–1366. doi: 10.1378/chest.129.5.1349. doi:10.1378/chest.129.5.1349. [DOI] [PubMed] [Google Scholar]
- 65.Vasile VC, Babuin L, Rio Perez JA, Alegria JR, Song LM, Chai HS, Afessa B, Jaffe AS. Long-term prognostic significance of elevated cardiac troponin levels in critically ill patients with acute gastrointestinal bleeding. Crit Care Med. 2009;37:140–147. doi: 10.1097/CCM.0b013e318192faa3. doi:10.1097/CCM.0b013e318192faa3. [DOI] [PubMed] [Google Scholar]
- 66.Tan IK, Chua KS, Toh AK. Serum magnesium, copper, and zinc concentrations in acute myocardial infarction. J Clin Lab Anal. 1992;6:324–328. doi: 10.1002/jcla.1860060513. doi:10.1002/jcla.1860060513. [DOI] [PubMed] [Google Scholar]
- 67.Versieck J, Barbier F, Speecke A, Hoste J. Influence of myocardial infarction on serum manganese, copper, and zinc concentrations. Clin Chem. 1975;21:578–581. [PubMed] [Google Scholar]
- 68.Jain VK, Mohan G. Serum zinc and copper in myocardial infarction with particular reference to prognosis. Biol Trace Elem Res. 1991;31:317–322. doi: 10.1007/BF02990200. doi:10.1007/BF02990200. [DOI] [PubMed] [Google Scholar]
- 69.Arnaud J, Faure H, Bourlard P, Denis B, Favier AE. Longitudinal changes in serum zinc concentration and distribution after acute myocardial infarction. Clin Chim Acta. 1994;230:147–156. doi: 10.1016/0009-8981(94)90267-4. doi:10.1016/0009-8981(94)90267-4. [DOI] [PubMed] [Google Scholar]
- 70.Lekakis J, Kalofoutis A. Zinc concentrations in serum as related to myocardial infarction. Clin Chem. 1980;26:1660–1661. [PubMed] [Google Scholar]
- 71.Berger MM, Cavadini C, Chiolero R, Dirren H. Copper, selenium, and zinc status and balances after major trauma. J Trauma. 1996;40:103–109. doi: 10.1097/00005373-199601000-00019. doi:10.1097/00005373-199601000-00019. [DOI] [PubMed] [Google Scholar]
- 72.Berger MM, Shenkin A. Update on clinical micronutrient supplementation studies in the critically ill. Curr Opin Clin Nutr Metab Care. 2006;9:711–716. doi: 10.1097/01.mco.0000247466.41661.ba. doi:10.1097/01.mco.0000247466.41661.ba. [DOI] [PubMed] [Google Scholar]
- 73.Berger MM, Shenkin A, Revelly JP, Roberts E, Cayeux MC, Baines M, Chioléro RL. Copper, selenium, zinc, and thiamine balances during continuous venovenous hemodiafiltration in critically ill patients. Am J Clin Nutr. 2004;80:410–416. doi: 10.1093/ajcn/80.2.410. [DOI] [PubMed] [Google Scholar]
- 74.Lindeman RD, Bottomley RG, Cornelison RL, Jr, Jacobs LA. Influence of acute tissue injury on zinc metabolism in man. J Lab Clin Med. 1972;79:452–460. [PubMed] [Google Scholar]
- 75.Low WI, Ikram H. Plasma zinc in acute myocardial infarction. Diagnostic and prognostic implications. Br Heart J. 1976;38:1339–1342. doi: 10.1136/hrt.38.12.1339. doi:10.1136/hrt.38.12.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Selmanpakoğlu AN, Cetin C, Sayal A, Işimer A. Trace element (Al, Se, Zn, Cu) levels in serum, urine and tissues of burn patients. Burns. 1994;20:99–103. doi: 10.1016/s0305-4179(06)80002-1. doi:10.1016/S0305-4179(06)80002-1. [DOI] [PubMed] [Google Scholar]
- 77.Agay D, Anderson RA, Sandre C, Bryden NA, Alonso A, Roussel AM, Chancerelle Y. Alterations of antioxidant trace elements (Zn, Se, Cu) and related metallo-enzymes in plasma and tissues following burn injury in rats. Burns. 2005;31:366–371. doi: 10.1016/j.burns.2004.11.010. doi:10.1016/j.burns.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 78.Berger MM. Antioxidant micronutrients in major trauma and burns: evidence and practice. Nutr Clin Pract. 2006;21:438–449. doi: 10.1177/0115426506021005438. doi:10.1177/0115426506021005438. [DOI] [PubMed] [Google Scholar]
- 79.Berger MM, Baines M, Raffoul W, Benathan M, Chiolero RL, Reeves C, Revelly JP, Cayeux MC, Senechaud I, Shenkin A. Trace element supplementation after major burns modulates antioxidant status and clinical course by way of increased tissue trace element concentrations. Am J Clin Nutr. 2007;85:1293–1300. doi: 10.1093/ajcn/85.5.1293. [DOI] [PubMed] [Google Scholar]
- 80.Arroyo M, LaGuardia SP, Bhattacharya SK, Nelson MD, Johnson PL, Carbone LD, Newman KP, Weber KT. Micronutrients in African-Americans with decompensated and compensated heart failure. Transl Res. 2006;148:301–308. doi: 10.1016/j.trsl.2006.08.003. doi:10.1016/j.trsl.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 81.Tubek S. Zinc content in lymphocytes and the activity of zinc ion efflux from lymphocytes in primary arterial hypertension. Biol Trace Elem Res. 2005;107:89–99. doi: 10.1385/BTER:107:2:089. doi:10.1385/BTER:107:2:089. [DOI] [PubMed] [Google Scholar]
- 82.Oster O, Drexler M, Schenk J, Meinertz T, Kasper W, Schuster CJ, Prellwitz W. The serum selenium concentration of patients with acute myocardial infarction. Ann Clin Res. 1986;18:36–42. [PubMed] [Google Scholar]
- 83.Bor MV, Cevík C, Uslu I, Güneral F, Düzgün E. Selenium levels and glutathione peroxidase activities in patients with acute myocardial infarction. Acta Cardiol. 1999;54:271–276. [PubMed] [Google Scholar]
- 84.Anker SD, Chua TP, Ponikowski P, Harrington D, Swan JW, Kox WJ, Poole-Wilson PA, Coats AJS. Hormonal changes and catabolic/anabolic imbalance in chronic heart failure and their importance for cardiac cachexia. Circulation. 1997;96:526–534. doi: 10.1161/01.cir.96.2.526. [DOI] [PubMed] [Google Scholar]
- 85.Dutka DP, Olivotto I, Ward S, Nihoyannopoulos P, al-Subaili M, Oakley CM, Impallomeni M, Cleland JG. Plasma neuro-endocrine activity in very elderly subjects and patients with and without heart failure. Eur Heart J. 1995;16:1223–1230. doi: 10.1093/oxfordjournals.eurheartj.a061079. [DOI] [PubMed] [Google Scholar]
- 86.Bolger AP, Sharma R, Li W, Leenarts M, Kalra PR, Kemp M, Coats AJ, Anker SD, Gatzoulis MA. Neurohormonal activation and the chronic heart failure syndrome in adults with congenital heart disease. Circulation. 2002;106:92–99. doi: 10.1161/01.cir.0000020009.30736.3f. doi:10.1161/01.CIR.0000020009.30736.3F. [DOI] [PubMed] [Google Scholar]
- 87.Emdin M, Passino C, Prontera C, Iervasi A, Ripoli A, Masini S, Zucchelli GC, Clerico A. Cardiac natriuretic hormones, neuro-hormones, thyroid hormones and cytokines in normal subjects and patients with heart failure. Clin Chem Lab Med. 2004;42:627–636. doi: 10.1515/CCLM.2004.108. doi:10.1515/CCLM.2004.108. [DOI] [PubMed] [Google Scholar]
- 88.Buchhorn R, Hammersen A, Bartmus D, Bürsch J. The pathogenesis of heart failure in infants with congenital heart disease. Cardiol Young. 2001;11:498–504. doi: 10.1017/s1047951101000725. doi:10.1017/S1047951101000725. [DOI] [PubMed] [Google Scholar]
- 89.Law PH, Sun Y, Bhattacharya SK, Chhokar VS, Weber KT. Diuretics and bone loss in rats with aldosteronism. J Am Coll Cardiol. 2005;46:142–146. doi: 10.1016/j.jacc.2005.03.055. doi:10.1016/j.jacc.2005.03.055. [DOI] [PubMed] [Google Scholar]
- 90.Soliman HM, Mercan D, Lobo SS, Melot C, Vincent JL. Development of ionized hypomagnesemia is associated with higher mortality rates. Crit Care Med. 2003;31:1082–1087. doi: 10.1097/01.CCM.0000060867.17556.A0. doi:10.1097/01.CCM.0000060867.17556.A0. [DOI] [PubMed] [Google Scholar]
- 91.Ahmed A, Zannad F, Love TE, Tallaj J, Gheorghiade M, Ekundayo OJ, Pitt B. A propensity-matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J. 2007;28:1334–1343. doi: 10.1093/eurheartj/ehm091. doi:10.1093/eurheartj/ehm091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Adamopoulos C, Pitt B, Sui X, Love TE, Zannad F, Ahmed A. Low serum magnesium and cardiovascular mortality in chronic heart failure: a propensity-matched study. Int J Cardiol. 2009;136:270–277. doi: 10.1016/j.ijcard.2008.05.006. doi:10.1016/j.ijcard.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bowling CB, Pitt B, Ahmed MI, Aban IB, Sanders PW, Mujib M, Campbell RC, Love TE, Aronow WS, Allman RM, Bakris GL, Ahmed A. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail. 2010;3:253–260. doi: 10.1161/CIRCHEARTFAILURE.109.899526. doi:10.1161/CIRCHEARTFAILURE.109.899526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Domanski M, Tian X, Haigney M, Pitt B. Diuretic use, progressive heart failure, and death in patients in the DIG study. J Card Fail. 2006;12:327–332. doi: 10.1016/j.cardfail.2006.03.006. doi:10.1016/j.cardfail.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 95.Ahmed A, Husain A, Love TE, Gambassi G, Dell'Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. doi:10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Weber KT. Furosemide in the long-term management of heart failure. The good, the bad and the uncertain. J Am Coll Cardiol. 2004;44:1308–1310. doi: 10.1016/j.jacc.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 97.Cooper HA, Dries DL, Davis CE, Shen YL, Domanski MJ. Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation. 1999;100:1311–1315. doi: 10.1161/01.cir.100.12.1311. [DOI] [PubMed] [Google Scholar]
- 98.Domanski M, Norman J, Pitt B, Haigney M, Hanlon S, Peyster E. Diuretic use, progressive heart failure, and death in patients in the Studies Of Left Ventricular Dysfunction (SOLVD) J Am Coll Cardiol. 2003;42:705–708. doi: 10.1016/s0735-1097(03)00765-4. doi:10.1016/S0735-1097(03)00765-4. [DOI] [PubMed] [Google Scholar]
- 99.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes W. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. doi:10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 100.Shane E, Mancini D, Aaronson K, Silverberg SJ, Seibel MJ, Addesso V, McMahon DJ. Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am J Med. 1997;103:197–207. doi: 10.1016/s0002-9343(97)00142-3. doi:10.1016/S0002-9343(97)00142-3. [DOI] [PubMed] [Google Scholar]
- 101.Khouzam RN, Dishmon DA, Farah V, Flax SD, Carbone LD, Weber KT. Secondary hyperparathyroidism in patients with untreated and treated congestive heart failure. Am J Med Sci. 2006;331:30–34. doi: 10.1097/00000441-200601000-00009. doi:10.1097/00000441-200601000-00009. [DOI] [PubMed] [Google Scholar]
- 102.LaGuardia SP, Dockery BK, Bhattacharya SK, Nelson MD, Carbone LD, Weber KT. Secondary hyperparathyroidism and hypovitaminosis D in African-Americans with decompensated heart failure. Am J Med Sci. 2006;332:112–118. doi: 10.1097/00000441-200609000-00003. doi:10.1097/00000441-200609000-00003. [DOI] [PubMed] [Google Scholar]
- 103.Alsafwah S, LaGuardia SP, Nelson MD, Battin DL, Newman KP, Carbone LD, Weber KT. Hypovitaminosis D in African Americans residing in Memphis, Tennessee with and without heart failure. Am J Med Sci. 2008;335:292–297. doi: 10.1097/MAJ.0b013e318167b0bd. doi:10.1097/MAJ.0b013e318167b0bd. [DOI] [PubMed] [Google Scholar]
- 104.Ulrich S, Hersberger M, Fischler M, Huber LC, Senn O, Treder U, Speich R, Schmid C. Bone mineral density and secondary hyperparathyroidism in pulmonary hypertension. Open Respir Med J. 2009;3:53–60. doi: 10.2174/1874306400903010053. doi:10.2174/1874306400903010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Franco CB, Paz-Filho G, Gomes PE, Nascimento VB, Kulak CA, Boguszewski CL, Borba VZ. Chronic obstructive pulmonary disease is associated with osteoporosis and low levels of vitamin D. Osteoporos Int. 2009;20:1881–1887. doi: 10.1007/s00198-009-0890-5. doi:10.1007/s00198-009-0890-5. [DOI] [PubMed] [Google Scholar]
- 106.Fertig A, Webley M, Lynn JA. Primary hyperparathyroidism in a patient with Conn's syndrome. Postgrad Med J. 1980;56:45–47. doi: 10.1136/pgmj.56.651.45. doi:10.1136/pgmj.56.651.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hellman DE, Kartchner M, Komar N, Mayes D, Pitt M. Hyperaldosteronism, hyperparathyroidism, medullary sponge kidneys, and hypertension. JAMA. 1980;244:1351–1353. doi:10.1001/jama.244.12.1351. [PubMed] [Google Scholar]
- 108.Resnick LM, Laragh JH. Calcium metabolism and parathyroid function in primary aldosteronism. Am J Med. 1985;78:385–390. doi: 10.1016/0002-9343(85)90328-6. doi:10.1016/0002-9343(85)90328-6. [DOI] [PubMed] [Google Scholar]
- 109.Rossi E, Sani C, Perazzoli F, Casoli MC, Negro A, Dotti C. Alterations of calcium metabolism and of parathyroid function in primary aldosteronism, and their reversal by spironolactone or by surgical removal of aldosterone-producing adenomas. Am J Hypertens. 1995;8:884–893. doi: 10.1016/0895-7061(95)00182-O. doi:10.1016/0895-7061(95)00182-O. [DOI] [PubMed] [Google Scholar]
- 110.Brunaud L, Germain A, Zarnegar R, Rancier M, Alrasheedi S, Caillard C, Ayav A, Weryha G, Mirallie E, Bresler L. Serum aldosterone is correlated positively to parathyroid hormone (PTH) levels in patients with primary hyperparathyroidism. Surgery. 2009;146:1035–1041. doi: 10.1016/j.surg.2009.09.041. doi:10.1016/j.surg.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 111.Andersson P, Rydberg E, Willenheimer R. Primary hyperparathyroidism and heart disease—a review. Eur Heart J. 2004;25:1776–1787. doi: 10.1016/j.ehj.2004.07.010. doi:10.1016/j.ehj.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 112.Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, Smith RA, Gerling IC, Weber KT. Hyperparathyroidism and the calcium paradox of aldosteronism. Circulation. 2005;111:871–878. doi: 10.1161/01.CIR.0000155621.10213.06. doi:10.1161/01.CIR.0000155621.10213.06. [DOI] [PubMed] [Google Scholar]
- 113.Vidal A, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC, Weber KT. Calcium paradox of aldosteronism and the role of the parathyroid glands. Am J Physiol Heart Circ Physiol. 2006;290:H286–H294. doi: 10.1152/ajpheart.00535.2005. doi:10.1152/ajpheart.00535.2005. [DOI] [PubMed] [Google Scholar]
- 114.Selektor Y, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT. Cinacalcet and the prevention of secondary hyperparathyroidism in rats with aldosteronism. Am J Med Sci. 2008;335:105–110. doi: 10.1097/MAJ.0b013e318134f013. doi:10.1097/MAJ.0b013e318134f013. [DOI] [PubMed] [Google Scholar]
- 115.Gandhi MS, Deshmukh PA, Kamalov G, Zhao T, Zhao W, Whaley JT, Tichy JR, Bhattacharya SK, Ahokas RA, Sun Y, Gerling IC, Weber KT. Causes and consequences of zinc dyshomeostasis in rats with chronic aldosteronism. J Cardiovasc Pharmacol. 2008;52:245–252. doi: 10.1097/FJC.0b013e3181833eb8. doi:10.1097/FJC.0b013e3181833eb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kamalov G, Deshmukh PA, Baburyan NY, Gandhi MS, Johnson PL, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT. Coupled calcium and zinc dyshomeostasis and oxidative stress in cardiac myocytes and mitochondria of rats with chronic aldosteronism. J Cardiovasc Pharmacol. 2009;53:414–423. doi: 10.1097/FJC.0b013e3181a15e77. doi:10.1097/FJC.0b013e3181a15e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lee AH, Mull RL, Keenan GF, Callegari PE, Dalinka MK, Eisen HJ, Mancini DM, DiSesa VJ, Attie MF. Osteoporosis and bone morbidity in cardiac transplant recipients. Am J Med. 1994;96:35–41. doi: 10.1016/0002-9343(94)90113-9. doi:10.1016/0002-9343(94)90113-9. [DOI] [PubMed] [Google Scholar]
- 118.Schmid C, Kiowski W. Hyperparathyroidism in congestive heart failure. Am J Med. 1998;104:508–509. [PubMed] [Google Scholar]
- 119.Ogino K, Ogura K, Kinugasa Y, Furuse Y, Uchida K, Shimoyama M, Kinugawa T, Osaki S, Kato M, Tomikura Y, Igawa O, Hisatome I, Bilezikian JP, Shigemasa C. Parathyroid hormone-related protein is produced in the myocardium and increased in patients with congestive heart failure. J Clin Endocrinol Metab. 2002;87:4722–4727. doi: 10.1210/jc.2002-020314. doi:10.1210/jc.2002-020314. [DOI] [PubMed] [Google Scholar]
- 120.Zittermann A, Schleithoff SS, Tenderich G, Berthold HK, Korfer R, Stehle P. Low vitamin D status: a contributing factor in the pathogenesis of congestive heart failure? J Am Coll Cardiol. 2003;41:105–112. doi: 10.1016/s0735-1097(02)02624-4. doi:10.1016/S0735-1097(02)02624-4. [DOI] [PubMed] [Google Scholar]
- 121.Sugimoto T, Tanigawa T, Onishi K, Fujimoto N, Matsuda A, Nakamori S, Matsuoka K, Nakamura T, Koji T, Ito M. Serum intact parathyroid hormone levels predict hospitalisation for heart failure. Heart. 2009;95:395–398. doi: 10.1136/hrt.2008.147652. doi:10.1136/hrt.2008.147652. [DOI] [PubMed] [Google Scholar]
- 122.Pilz S, Tomaschitz A, Drechsler C, Ritz E, Boehm BO, Grammer TB, März W. Parathyroid hormone level is associated with mortality and cardiovascular events in patients undergoing coronary angiography. Eur Heart J. 2010;31:1591–1598. doi: 10.1093/eurheartj/ehq109. doi:10.1093/eurheartj/ehq109. [DOI] [PubMed] [Google Scholar]
- 123.Hagström E, Hellman P, Larsson TE, Ingelsson E, Berglund L, Sundström J, Melhus H, Held C, Lind L, Michaëlsson K, Arnlöv J. Plasma parathyroid hormone and the risk of cardiovascular mortality in the community. Circulation. 2009;119:2765–2771. doi: 10.1161/CIRCULATIONAHA.108.808733. doi:10.1161/CIRCULATIONAHA.108.808733. [DOI] [PubMed] [Google Scholar]
- 124.Hagström E, Ingelsson E, Sundström J, Hellman P, Larsson TE, Berglund L, Melhus H, Held C, Michaëlsson K, Lind L, Ärnlöv J. Plasma parathyroid hormone and risk of congestive heart failure in the community. Eur J Heart Fail. 2010;12:1186–1192. doi: 10.1093/eurjhf/hfq134. [DOI] [PubMed] [Google Scholar]
- 125.Bell NH, Greene A, Epstein S, Oexmann MJ, Shaw S, Shary J. Evidence for alteration of the vitamin D-endocrine system in blacks. J Clin Invest. 1985;76:470–473. doi: 10.1172/JCI111995. doi:10.1172/JCI111995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sawaya BP, Monier-Faugere MC, Ratanapanichkich P, Butros R, Wedlund PJ, Fanti P. Racial differences in parathyroid hormone levels in patients with secondary hyperparathyroidism. Clin Nephrol. 2002;57:51–55. doi: 10.5414/cnp57051. [DOI] [PubMed] [Google Scholar]
- 127.Zittermann A, Fischer J, Schleithoff SS, Tenderich G, Fuchs U, Koerfer R. Patients with congestive heart failure and healthy controls differ in vitamin D-associated lifestyle factors. Int J Vitam Nutr Res. 2007;77:280–288. doi: 10.1024/0300-9831.77.4.280. doi:10.1024/0300-9831.77.4.280. [DOI] [PubMed] [Google Scholar]
- 128.Zittermann A, Schleithoff SS, Gotting C, Dronow O, Fuchs U, Kuhn J, Kleesiek K, Tenderich G, Koerfer R. Poor outcome in end-stage heart failure patients with low circulating calcitriol levels. Eur J Heart Fail. 2008;10:321–327. doi: 10.1016/j.ejheart.2008.01.013. doi:10.1016/j.ejheart.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 129.Zittermann A, Schleithoff SS, Koerfer R. Vitamin D and vascular calcification. Curr Opin Lipidol. 2007;18:41–46. doi: 10.1097/MOL.0b013e328011c6fc. doi:10.1097/MOL.0b013e328011c6fc. [DOI] [PubMed] [Google Scholar]
- 130.Jarvis JK, Miller GD. Overcoming the barrier of lactose intolerance to reduce health disparities. J Natl Med Assoc. 2002;94:55–66. [PMC free article] [PubMed] [Google Scholar]
- 131.Cohen AJ, Roe FJ. Review of risk factors for osteoporosis with particular reference to a possible aetiological role of dietary salt. Food Chem Toxicol. 2000;38:237–253. doi: 10.1016/s0278-6915(99)00145-3. doi:10.1016/S0278-6915(99)00145-3. [DOI] [PubMed] [Google Scholar]
- 132.Teucher B, Dainty JR, Spinks CA, Majsak-Newman G, Berry DJ, Hoogewerff JA, Foxall RJ, Jakobsen J, Cashman KD, Flynn A, Fairweather-Tait SJ. Sodium and bone health: impact of moderately high and low salt intakes on calcium metabolism in postmenopausal women. J Bone Miner Res. 2008;23:1477–1485. doi: 10.1359/jbmr.080408. doi:10.1359/jbmr.080408. [DOI] [PubMed] [Google Scholar]
- 133.Kerschan-Schindl K, Strametz-Juranek J, Heinze G, Grampp S, Bieglmayer C, Pacher R, Maurer G, Fialka-Moser V, Pietschmann P. Pathogenesis of bone loss in heart transplant candidates and recipients. J Heart Lung Transplant. 2003;22:843–850. doi: 10.1016/s1053-2498(02)00806-9. doi:10.1016/S1053-2498(02)00806-9. [DOI] [PubMed] [Google Scholar]
- 134.Nishio K, Mukae S, Aoki S, Itoh S, Konno N, Ozawa K, Satoh R, Katagiri T. Congestive heart failure is associated with the rate of bone loss. J Intern Med. 2003;253:439–446. doi: 10.1046/j.1365-2796.2003.01130.x. doi:10.1046/j.1365-2796.2003.01130.x. [DOI] [PubMed] [Google Scholar]
- 135.Kenny AM, Boxer R, Walsh S, Hager WD, Raisz LG. Femoral bone mineral density in patients with heart failure. Osteoporos Int. 2006;17:1420–1427. doi: 10.1007/s00198-006-0148-4. doi:10.1007/s00198-006-0148-4. [DOI] [PubMed] [Google Scholar]
- 136.Frost RJ, Sonne C, Wehr U, Stempfle HU. Effects of calcium supplementation on bone loss and fractures in congestive heart failure. Eur J Endocrinol. 2007;156:309–314. doi: 10.1530/EJE-06-0614. doi:10.1530/EJE-06-0614. [DOI] [PubMed] [Google Scholar]
- 137.Abou-Raya S, Abou-Raya A. Osteoporosis and congestive heart failure (CHF) in the elderly patient: double disease burden. Arch Gerontol Geriatr. 2009;49:250–254. doi: 10.1016/j.archger.2008.09.004. doi:10.1016/j.archger.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 138.van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation. 2008;118:1946–1952. doi: 10.1161/CIRCULATIONAHA.108.784009. doi:10.1161/CIRCULATIONAHA.108.784009. [DOI] [PubMed] [Google Scholar]
- 139.Carbone LD, Cross JD, Raza SH, Bush AJ, Sepanski RJ, Dhawan S, Khan BQ, Gupta M, Ahmad K, Khouzam RN, Dishmon DA, Nesheiwat JP, Hajjar MA, Chishti WA, Nasser W, Khan M, Womack CR, Cho T, Haskin AR, Weber KT. Fracture risk in men with congestive heart failure. Risk reduction with spironolactone. J Am Coll Cardiol. 2008;52:135–138. doi: 10.1016/j.jacc.2008.03.039. doi:10.1016/j.jacc.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 140.Garcia Zozaya JL, Padilla Viloria M. [Alterations of calcium, magnesium, and zinc in essential hypertension: their relation to the renin-angiotensin-aldosterone system] [Spanish] Invest Clin. 1997;38(Suppl. 2):27–40. [PubMed] [Google Scholar]
- 141.Golik A, Modai D, Averbukh Z, Sheffy M, Shamis A, Cohen N, Shaked U, Dolev E. Zinc metabolism in patients treated with captopril versus enalapril. Metabolism. 1990;39:665–667. doi: 10.1016/0026-0495(90)90098-w. doi:10.1016/0026-0495(90)90098-W. [DOI] [PubMed] [Google Scholar]
- 142.Golik A, Zaidenstein R, Dishi V, Blatt A, Cohen N, Cotter G, Berman S, Weissgarten J. Effects of captopril and enalapril on zinc metabolism in hypertensive patients. J Am Coll Nutr. 1998;17:75–78. doi: 10.1080/07315724.1998.10720459. [DOI] [PubMed] [Google Scholar]
- 143.Chmielnicka J, Zareba G, Witasik M, Brzeźnicka E. Zinc-selenium interaction in the rat. Biol Trace Elem Res. 1988;15:267–276. doi: 10.1007/BF02990143. doi:10.1007/BF02990143. [DOI] [PubMed] [Google Scholar]
- 144.Kamalov G, Ahokas RA, Zhao W, Johnson PL, Shahbaz AU, Bhattacharya SK, Sun Y, Gerling IC, Weber KT. Temporal responses to intrinsically coupled calcium and zinc dyshomeostasis in cardiac myocytes and mitochondria during aldosteronism. Am J Physiol Heart Circ Physiol. 2010;298:H385–H394. doi: 10.1152/ajpheart.00593.2009. doi:10.1152/ajpheart.00593.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kamalov G, Ahokas RA, Zhao W, Zhao T, Shahbaz AU, Johnson PL, Bhattacharya SK, Sun Y, Gerling IC, Weber KT. Uncoupling the coupled calcium and zinc dyshomeostasis in cardiac myocytes and mitochondria seen in aldosteronism. J Cardiovasc Pharmacol. 2010;55:248–254. doi: 10.1097/FJC.0b013e3181cf0090. doi:10.1097/FJC.0b013e3181cf0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wang J, Song Y, Elsherif L, Song Z, Zhou G, Prabhu SD, Saari JT, Cai L. Cardiac metallothionein induction plays the major role in the prevention of diabetic cardiomyopathy by zinc supplementation. Circulation. 2006;113:544–554. doi: 10.1161/CIRCULATIONAHA.105.537894. doi:10.1161/CIRCULATIONAHA.105.537894. [DOI] [PubMed] [Google Scholar]
- 147.Prabhu KS, Zamamiri-Davis F, Stewart JB, Thompson JT, Sordillo LM, Reddy CC. Selenium deficiency increases the expression of inducible nitric oxide synthase in RAW 264.7 macrophages: role of nuclear factor-κB in up-regulation. Biochem J. 2002;366(Pt 1):203–209. doi: 10.1042/BJ20020256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hatanaka N, Nakaden H, Yamamoto Y, Matsuo S, Fujikawa T, Matsusue S. Selenium kinetics and changes in glutathione peroxidase activities in patients receiving long-term parenteral nutrition and effects of supplementation with selenite. Nutrition. 2000;16:22–26. doi: 10.1016/s0899-9007(99)00183-5. doi:10.1016/S0899-9007(99)00183-5. [DOI] [PubMed] [Google Scholar]
- 149.Weiss SL, Evenson JK, Thompson KM, Sunde RA. The selenium requirement for glutathione peroxidase mRNA level is half of the selenium requirement for glutathione peroxidase activity in female rats. J Nutr. 1996;126:2260–2267. doi: 10.1093/jn/126.9.2260. [DOI] [PubMed] [Google Scholar]
- 150.Xia YM, Hill KE, Burk RF. Biochemical studies of a selenium-deficient population in China: measurement of selenium, glutathione peroxidase and other oxidant defense indices in blood. J Nutr. 1989;119:1318–1326. doi: 10.1093/jn/119.9.1318. [DOI] [PubMed] [Google Scholar]
- 151.van Rij AM, Thomson CD, McKenzie JM, Robinson MF. Selenium deficiency in total parenteral nutrition. Am J Clin Nutr. 1979;32:2076–2085. doi: 10.1093/ajcn/32.10.2076. [DOI] [PubMed] [Google Scholar]
- 152.Reeves WC, Marcuard SP, Willis SE, Movahed A. Reversible cardiomyopathy due to selenium deficiency. JPEN J Parenter Enteral Nutr. 1989;13:663–665. doi: 10.1177/0148607189013006663. doi:10.1177/0148607189013006663. [DOI] [PubMed] [Google Scholar]
- 153.Boldery R, Fielding G, Rafter T, Pascoe AL, Scalia GM. Nutritional deficiency of selenium secondary to weight loss (bariatric) surgery associated with life-threatening cardiomyopathy. Heart Lung Circ. 2007;16:123–126. doi: 10.1016/j.hlc.2006.07.013. doi:10.1016/j.hlc.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 154.Song Y, Wang J, Li XK, Cai L. Zinc and the diabetic heart. Biometals. 2005;18:325–332. doi: 10.1007/s10534-005-3689-7. doi:10.1007/s10534-005-3689-7. [DOI] [PubMed] [Google Scholar]
- 155.Demling RH, DeBiasse MA. Micronutrients in critical illness. Crit Care Clin. 1995;11:651–673. [PubMed] [Google Scholar]
- 156.Sriram K, Lonchyna VA. Micronutrient supplementation in adult nutrition therapy: practical considerations. JPEN J Parenter Enteral Nutr. 2009;33:548–562. doi: 10.1177/0148607108328470. doi:10.1177/0148607108328470. [DOI] [PubMed] [Google Scholar]
- 157.Witte KK, Clark AL, Cleland JG. Chronic heart failure and micronutrients. J Am Coll Cardiol. 2001;37:1765–1774. doi: 10.1016/s0735-1097(01)01227-x. doi:10.1016/S0735-1097(01)01227-X. [DOI] [PubMed] [Google Scholar]
- 158.Soukoulis V, Dihu JB, Sole M, Anker SD, Cleland J, Fonarow GC, Metra M, Pasini E, Strzelczyk T, Taegtmeyer H, Gheorghiade M. Micronutrient deficiencies an unmet need in heart failure. J Am Coll Cardiol. 2009;54:1660–1673. doi: 10.1016/j.jacc.2009.08.012. doi:10.1016/j.jacc.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 159.Bhattacharya SK, Ahokas RA, Carbone LD, Newman KP, Gerling IC, Sun Y, Weber KT. Macro- and micronutrients in African-Americans with heart failure. Heart Fail Rev. 2006;11:45–55. doi: 10.1007/s10741-006-9192-6. doi:10.1007/s10741-006-9192-6. [DOI] [PubMed] [Google Scholar]