Abstract
Background
Practice pattern variations are often attributed to physician decision-making with no accounting for patient preferences.
Objective
To test whether a mass media television broadcast unrelated to health was associated with changes in the rate and characteristics of visits for acute emergency care.
Design
Time-series analysis of emergency department visits for any reason.
Subjects
Population-based sample of all patients seeking emergency care in Ontario, Canada.
Measures
The broadcast day was defined as the Olympic men’s gold medal ice hockey game final. The control days were defined as the 6 Sundays before and after the broadcast day.
Results
A total of 99 447 visits occurred over the 7 Sundays, of which 13 990 occurred on the broadcast day. Comparing the broadcast day with control days, we found no significant difference in the hourly rate of visits before the broadcast (544 vs 537, p = 0.41) or after the broadcast (647 vs 639, p = 0.55). In contrast, we observed a significant reduction in hourly rate of visits during the broadcast (647 vs 783, p < 0.001), equal to an absolute decrease of 409 patients, a relative decrease of 17% (95% confidence interval 13–21), or about 136 fewer patients per hour. The relative decrease during the broadcast was particularly large for adult men with low triage severity. The greatest reductions were for patients with abdominal, musculoskeletal or traumatic disorders.
Conclusion
Mass media television broadcasts can influence patient preferences and thereby lead to a decrease in emergency department visits.
Practice pattern variations are an interesting, enduring, and unexplained feature of modern medical care. For example, total expenditures per capita on Medicare in the United States are about 13% higher in Northeastern states than in Western states.1,2 Analyses suggest that such variations are not entirely attributable to differences in the incidence, severity, and distribution of disease.3 Instead, such variations contribute to debates concerning unnecessary health care, self-limited diseases, and the potential economic savings from reducing high outliers.4 These analyses usually do not account for patient preferences, since formal measurement of personal values is difficult to conduct on a population-wide basis and is a major gap in current science.5-7
A patient’s pattern of health care, however, reflects countless decisions shaped by personal opportunities and subjective perceptions. To take a non-medical analogy, marketing science demonstrates major differences between consumers with regard to personal choices. For example, the leading brand of spaghetti sauce outsells its nearest rival by 80% in Northeastern states (Ragu market share = 0.45, Prego market share = 0.25) yet only 24% in Western states (Ragu market share = 0.37, Prego market share = 0.30).8 These sales differences underscore the role of differing personal preferences rather than manufacturers’ intentions.9 Our theory was that health care patterns are not immune to analogous variations in individual choice.
In this study we assessed emergency department visit rates because they are frequent, objectively recorded, and primarily caused by a patient’s condition. Such visits are also an example of a practice pattern that varies across different regions.10 We chose a specific Olympic broadcast for analysis because it was a well-defined media event, received the largest television audience in Canadian history, and provided an objective measure of societal popularity.11 The broadcast also exemplifies events outside of medicine and unrelated to health policy control. Our study question was to test whether a popular broadcast might lead some patients to forgo an emergency department visit.
Methods
Setting
Canada had a population of 33 873 357 on 1 Jan. 2010, of whom 13 119 251 lived in Ontario (Canada’s most populous province).12 The Canadian health system ensures universal access to health care, including free access to emergency department care with no co-payments or user limits in Ontario. Canadian culture shares many similarities with other developed countries, although it arguably places a higher priority on hockey relative to other professional sports.13 The Olympic men’s ice hockey gold medal game, in particular, received record levels of public attention, with a total of 16.6 million Canadian television viewers (equal to about 50% of the entire population).14 For perspective, the Super Bowl broadcast had 6.0 million Canadian viewers and the World Cup Final broadcast had 5.1 million Canadian viewers.15,16
Event day
The Olympic men’s hockey gold medal game occurred on Sunday, 28 February 2010, at a venue roughly 3000 kilometers distant from Ontario. The puck dropped for the opening face-off at 1215 h Pacific Coast Time (equal to 1515 h in Ontario). Sudden death overtime ended the game with a goal at 1454 h Pacific Coast Time (equal to 1754 h in Ontario). The total broadcast exceeded 3 hours’ duration because of pre-game and post-game commentary. We defined the broadcast as the 3 hours from 1500 h to 1759 h in Ontario and maintained the same time intervals in all comparisons except where noted. We defined the 15 clock hours from 0000 h to 1459 h as the time interval before the broadcast and the 6 clock hours from 1800 h to 2359 h as the time interval after the broadcast.
Control days
We selected 6 control days to achieve adequate statistical power17 and focused on Sundays to mitigate daily fluctuations (February 7, 14, 21 and March 7, 14, 21). The television broadcasts on the control Sundays were generally less popular but not devoid of viewers (February 7 = 6.0 million, February 14 = 7.3 million, March 14 = 2.5 million, March 21 = 2.0 million viewers).18 The previous Sunday was notable for a broadcast of a game between the same two hockey teams (February 21 = 10.6 million viewers).19 The Sunday immediately following was notable for a broadcast of the Academy Awards ceremony (March 7 = 5.9 million viewers).20 For all 6 control days, Ontario experienced no major political developments, economic crises, natural disasters, or other large potential temporal confounders.21
Emergency visits
We obtained data on emergency department visits throughout Ontario using the National Ambulatory Care Reporting System (NACRS) database.22 This database, which has been used extensively in previous studies, is the official governmental source for defining emergency department utilization and has been validated in past research.23-25 Our research was approved by the Sunnybrook Research Ethics committee and conducted using privacy safeguards of the Institute for Clinical Evaluative Sciences. The main strength of using this database was to gather population-based, individual-linked data in a manner blind to exposure status and study hypothesis. The database did not contain data on vital signs, physical findings, laboratory information, quality of life, or financial costs.
Patient characteristics
We identified all patients who made an emergency department visit during the study interval, excluding those with a missing health card number. Patient age, gender, home location, neighborhood income, and date of death were obtained through computerized linkages to the demographic database.26 Patient arrival time, hospital, and length of stay were obtained directly from the NACRS database, as were data on discharge departure (e.g., admitted, sent home, dead) and subsequent return visits. Health status variables included triage acuity (coded using the Canadian Triage and Acuity Scale), chief complaint (13 mutually exclusive groups), and main diagnosis (coded using the International Classification of Disease 10th ICD10 Canadian Revision).27,28
Statistical analysis
Our primary analysis focused on the number of patients arriving during the hours of the broadcast compared with the number arriving during the same hours on the 6 control days. The simplest model subjected these two sums to a binomial test and evaluated departures from the expected ratio of 1:6. Results from alternative statistical approaches yielded similar findings and are not reported.29,30 Secondary analysis examined the hours before and after the broadcast to test for potential spillover. Subgroup analyses explored the robustness of results with special attention to cardiac emergencies.31-33 Follow-up analyses examined subsequent visits to any emergency department within 7 days and mortality within 30 days. All p values were two-tailed and not adjusted for multiple comparisons.34
Results
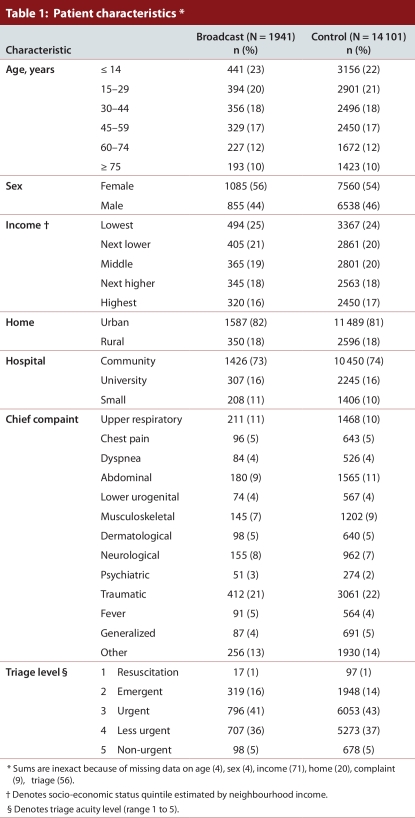
A total of 99 447 visits occurred across 170 emergency departments over the 7 Sundays, of which 16% (16 042) occurred during the hours of the broadcast, 57% (56 523) during earlier hours, and 27% (26 882) during later hours. The total was equivalent to about 14 207 patients per day, or 592 patients per hour. The most active 3-hour interval was 0900h to 1159h and averaged 916 patients per hour. The least active 3-hour interval was 0300h to 0559h and averaged 205 patients per hour. The 3 hours of the broadcast averaged 764 patients per hour (Table 1). The typical patient lived in an urban location and was given a triage severity of 3 or 4 (urgent or less urgent). The most common specific chief complaints were upper respiratory symptoms, traumatic injury, and abdominal pain.
Table 1.
Patient characteristics
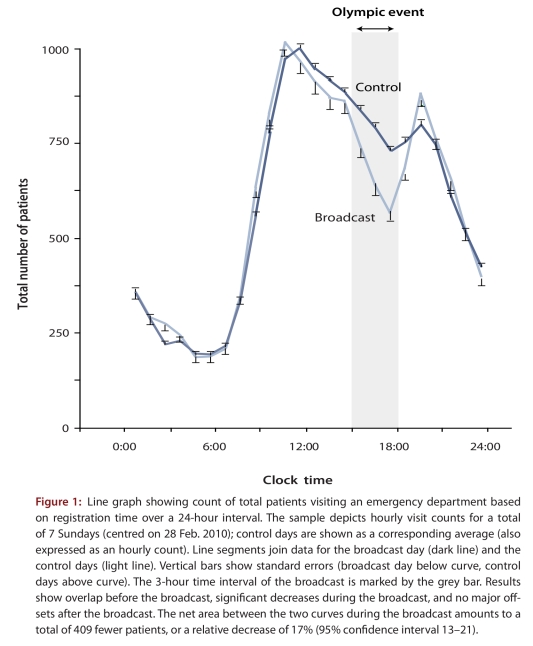
We observed no significant difference between the Olympic event day and control days in the average number of patients per hour before the broadcast (544 vs 537, p = 0.41) or after the broadcast (647 vs 639, p = 0.55). In contrast, we observed a significant decrease in the average number of patients per hour during the hours of the broadcast (647 vs 783, p < 0.001). The decrease in visit frequency during the broadcast was evident for all three of the individual hours of the broadcast and amounted to a total of 409 fewer visits at the time of the broadcast compared with the same hours on control days (Fig. 1). This was equivalent to a 17% (95% confidence interval [CI] 13–21) relative decrease in emergency department visits during the hours of the broadcast.
Figure 1.
Line graph showing count of total patients visiting an emergency department based on registration time over a 24-hour interval
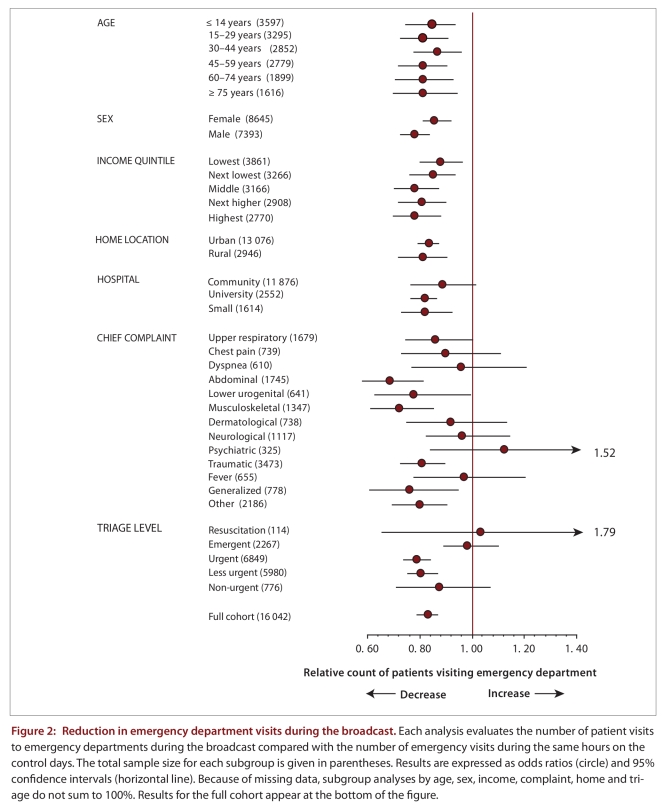
The relative decrease in emergency department visits during the broadcast varied by patient characteristics (Fig. 2). The relative decrease was somewhat more apparent among adult men living in rural locations, yet was still significant for elderly women living in urban locations. The relative decrease was evident throughout the socio-economic spectrum. The largest relative reductions were seen for patients with lower triage severity scores. We found no significant contrary pattern in any of the 13 chief complaints, except for a marginal increase among those with psychiatric disorders (p > 0.20). The most distinctly decreased chief complaints were abdominal pain, musculoskeletal disorders, and traumatic injuries.
Figure 2.
Reduction in emergency department visits during the broadcast
A comparison of the distribution of common diagnoses during the broadcast hours and the corresponding hours on the control days showed variation across a wide range (Appendix A). For example, fracture of the forearm (code S52) was the 14th most common patient diagnosis (n = 203) and showed a 52% reduction associated with the broadcast (p = 0.004). Overall, 75 of the 100 most common diagnoses showed a reduction associated with the broadcast (10 at p < 0.05). In contrast, 23 of the 100 diagnoses showed an increase (1 at p < 0.05). The largest absolute reductions were for diagnoses of abdominal and pelvic pain (code R10) and diarrhea or gastroenteritis of presumed infectious origin (code A09). The largest absolute increase was for superficial injury to the head (code S00).
We examined specific cardiac emergencies in light of earlier reports of a doubling of such risk while viewing exciting sports. To do so, we identified patients who had a diagnosis of myocardial infarction (codes I21–I22), unstable angina (codes I20), major arrhythmia (codes I47–I49), or cardiac arrest (codes I46). For this subgroup (n = 153) there was a non-significant increase in visits during the broadcast (odds ratio [OR] 1.22, 95% CI 0.78–1.93). When we narrowed the cardiac subgroup to include only those with the top triage score (n = 22) we found a significant increase in visits during the broadcast (OR 2.73, 95% CI 1.07–6.98). When we widened the cardiac subgroup to include all patients (n = 553) with any cardiac diagnosis (codes I00-I99), we found no decrease in visits (OR 1.02, 95% CI 0.79–1.32).
Median length of stay in the emergency department varied more than two-fold depending on chief complaint but was almost identical during the broadcast day and control days (Appendix B). The likelihood of being admitted varied more than five-fold depending on chief complaint and was similar during the broadcast day and control days. The probability of making a return visit to an emergency department within the following week was substantial for most chief complaints and similar for the broadcast and control days. The risk of death within 30 days was usually low and similar for the broadcast and control days. Overall, the broadcast yielded a 12% reduction in occupancy (95% CI 9–15), calculated as total patient-hours in the emergency department during the broadcast, and no significant change in total admissions, return visits, or deaths.
Discussion
We found that the rate of total emergency visits was 17% lower during the single most popular television broadcast in Canadian history than during corresponding hours for 6 control days. This effect extended throughout Canada’s largest province, amounted to a decrease of about 136 fewer patients per hour, appeared accentuated for adult men living in rural locations, and was most evident for those with milder triage severity scores presenting with abdominal pain, musculoskeletal disorders, or traumatic injuries. This lower rate of emergency visits was not associated with spillover to hours immediately before or after the broadcast, was not shared by patients with severe acute cardiac emergencies, and was not associated with major differences in return rates or deaths.
The most important limitation of our research is that we examined only one mass media event and one sector of the health care system. The Olympics, for example, contain many other sports and recur in the summer and winter on a regular basis. Other broadcasts, however, tend to have smaller audiences and arguably a smaller effect on community attention.35 The 2010 Olympic men’s hockey final was also an exceptional event in that millions of people aligned and shared the same preference for a brief time over a large region.36 Olympic broadcasts, moreover, are not the only popular entertainment event, and watching television is not the most powerful preference for the majority of people in Ontario.
Our analysis has other limitations related to the nature of universal health care databases. The available data did not indicate who was watching television; hence, changes in emergency department visits may reflect decisions by patients or by friends, family, and others around the patient. The data do not directly distinguish between an individual’s increased reluctance to seek care and an individual’s decreased need to seek care. The control days, furthermore, contained ongoing broadcasts, so that all odds ratio estimates are biased toward the null. Finally, the study could not be conducted in a manner that was randomized or double-blinded.
Data sets derived from universal health care databases have strengths compared with data gathered at single centres.37-39 Our sample, which encompasses a large and diverse patient population, avoids selection bias, supports rigorous subgroup analyses, and provides wide generalizability. The hourly time data are precise and consistent, enabling analyses of activity levels before and after an event. The clinical data include triage acuity, chief complaint, main diagnosis, ongoing care, and other details that are often missing in administrative files. In addition, the data we used track real practice patterns throughout a population and thereby revealed latent hidden preferences rather than capturing self-reported responses from voluntary surveys.
Our study replicates earlier research on cardiac events related to championship football matches. One explanation for the agreement may be that populations in high-income countries share a similar diet, activity, lifestyle, and other cardiac risk factors.40 An alternative reason may relate to similarities in pre-hospital service and access to care when a popular event occurs at a remote venue with no disruption in local services.41-43 An added factor might be that clinical evaluation and diagnostic accuracy have some consistent standards.44 Another possibility is that the agreement is coincidental, since our research was based on a single hockey broadcast, and prior research was based on a short series of football games.45-48
Patients seek care for diverse reasons, and thoughtful clinicians generally want to know why. A classic interaction entails the physician asking for a chief complaint and eliciting a symptom, such as “headaches.” Some clinicians probe further for elaboration, such as “because the pain was worse today than yesterday.” Our study suggests, however, that a full response might sometimes include patient preferences, such as “because no major broadcast was on television today.” The failure of clinical encounters to always capture these nuances may help explain both the failure of medical economics to account for patient preferences and why practice pattern uniformity might sometimes be a quixotic goal.
Experienced clinicians are aware of fluctuating demands for care and make schedules that adapt to such changes.49-51 Our study serves to remind others that clinicians are not necessarily the source of such practice pattern variations. At face value, the data suggest that perhaps 1 in 6 emergency department visits reflects decisions by patients. A sustained decrease of this magnitude, in theory, might translate to savings in the range of $100 million annually in Ontario.52 Together, the data highlight the contribution of patient decisions and a role for more behavioural science in medical economics.53,54 The Olympics may reveal something about both world champions and everyday patients.
Acknowledgments
We thank the following for their helpful comments: Maya Bar-Hillel, William Chan, Victoria Dickinson, Daniel Hackam, David Juurlink, Joel Ray, Lee Ross, Damon Scales, Michael Schull, Steven Shumak, Arthur Slutsky, and Jack Williams.
Biographies
Donald A. Redelmeier is a Professor of Medicine at the University of Toronto, the Director of Clinical Epidemiology at the Sunnybrook Research Institute, a Staff Physician at Sunnybrook Health Sciences Center, a Senior Scientist at the Institute for Clinical Evaluative Sciences, and the Research Director of the Sunnybrook Injury Control Unit, Toronto, Ontario, Canada.
Marian J. Vermeulen is an Epidemiologist at the Institute for Clinical Evaluative Sciences and a Lecturer in the Department of Health Policy Managment & Evaluation at the University of Toronto, Toronto, Ontario, Canada.
Appendix
Appendix A.
Top 100 most common main diagnoses
Appendix B.
Overview of process and outcomes by patient chief complaint
Footnotes
Competing interests: None declared.
Contributors: Both DAR and MJV take responsibility for the work; contributed to the conception and design of the analysis; drafted and revised the article for important intellectual content; and approved the published version. The lead author (DAR) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
Funding source: This project was supported by the Canada Research Chair in Medical Decision Sciences and the University of Toronto Comprehensive Research Experience for Medical Students program. The views expressed in this paper are those of the authors and do not necessarily reflect the Ontario Ministry of Health. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
- 1.Zhang Y, Baicker K, Newhouse JP. Geographic variation in Medicare drug spending. N Engl J Med. 2010 Jun 09;363(5):405–409. doi: 10.1056/NEJMp1004872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Dartmouth Atlas Working Group. The Dartmouth Atlas of Health Care. Downloads: Selected Medicare reimbursement measures, state level, 2007 [data file] 2010. [accessed 2010 July 16]. http://www.dartmouthatlas.org/tools/downloads.aspx.
- 3.Fisher Elliott S, Bynum Julie P, Skinner Jonathan S. Slowing the growth of health care costs--lessons from regional variation. N Engl J Med. 2009;360(9):849–852. doi: 10.1056/NEJMp0809794. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/19246356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein Arnold M. Geographic variation in Medicare spending. N Engl J Med. 2010 May 12;363(1):85–86. doi: 10.1056/NEJMe1005212. http://www.nlm.nih.gov/medlineplus/medicare.html. [DOI] [PubMed] [Google Scholar]
- 5.Diehr P, Yanez D, Ash A, Hornbrook M, Lin D Y. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. http://www.scholaruniverse.com/ncbi-linkout?id=10352853. [DOI] [PubMed] [Google Scholar]
- 6.Fuchs VR. Floridian exceptionalism. Health Aff (Millwood) 2003. W3–357–362 http://content.healthaffairs.org/cgi/pmidlookup?view=long&pmid=15506138. [DOI] [PubMed]
- 7.Anthony Denise L, Herndon M Brooke, Gallagher Patricia M, Barnato Amber E, Bynum Julie P W, Gottlieb Daniel J, Fisher Elliott S, Skinner Jonathan S. How much do patients' preferences contribute to resource use? Health Aff (Millwood) 2009;28(3):864–873. doi: 10.1377/hlthaff.28.3.864. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/19414899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo SC, Capps O. Regional variability of price and expenditure elasticities: the case of spaghetti sauces. Agribusiness. 1998;13(6):659–672. [Google Scholar]
- 9.Thaler RH. Quasi rational economics. New York: Russell Sage Foundation; 1994. [Google Scholar]
- 10.Chan BT, Schull MJ, Schultz SE. Emergency department services in Ontario. Toronto: Institute for Clinical Evaluative Sciences; 2001. [Google Scholar]
- 11.CTV Media Release. Oh Canada!! 16.6 million watch Team Canada ignite a nation. 2010. Mar 1, [accesssed 2011 Mar 16]. http://www.ctvmedia.ca/olympics/releases/release.asp?id=12312&yyyy=2010.
- 12.Statistics Canada. Quarterly demographic estimates. [accessed 2011 Mar 16]. http://www.statcan.gc.ca/daily-quotidien/091223/t091223b2-eng.htm.
- 13.Canadian Encyclopedia. Hockey (Ice) [accessed 2010 Mar 16]. http://www.thecanadianencyclopedia.com/index.cfm?PgNm=TCE&Params=A1ARTA0003794.
- 14.BBM. Top programs—Total Canada (English) February 22 – February 28, 2010. [accessed 2011 Mar 16]. http://www.bbm.ca/_documents/top_30_tv_programs_english/2010/nat02222010.pdf.
- 15.BBM. Top programs—Total Canada (English) February 1 – February 7, 2010. [accessed 2011 Mar 16]. http://www.bbm.ca/_documents/top_30_tv_programs_english/2010/nat02012010.pdf.
- 16.BBM. Top programs—Total Canada (English) July 5 -– July 11, 2010. [accessed 2011 Mar 16]. http://www.bbm.ca/_documents/top_30_tv_programs_english/2010/nat07052010.pdf.
- 17.Hulley SB, Cummings SR. Designing clinical research. Baltimore: William & Wilkins; 1988. p. 148. [Google Scholar]
- 18.BBM. 2009–10 National top program reports archive. [accessed 2011 Mar 16]. http://www.bbm.ca/index.php?option=com_content&task=view&id=108&Itemid=108.
- 19.BBM. Top programs—Total Canada (English) February 15 – February 21, 2010. [accessed from 2011 Mar 16]. http://www.bbm.ca/_documents/top_30_tv_programs_english/2010/nat02152010.pdf.
- 20.BBM. Top programs—Total Canada (English) March 1 – March 7, 2010. [accessed 2011 Mar 16]. http://www.bbm.ca/_documents/top_30_tv_programs_english/2010/nat03012010.pdf.
- 21.Macleans. Archives. [accessed 2011 Mar 16]. http://www2.macleans.ca/archive.
- 22.Li Guohua, Lau Jonathan T, McCarthy Melissa L, Schull Michael J, Vermeulen Marian, Kelen Gabor D. Emergency department utilization in the United States and Ontario, Canada. Acad Emerg Med. 2007 Apr 30;14(6):582–584. doi: 10.1197/j.aem.2007.02.030. http://www.scholaruniverse.com/ncbi-linkout?id=17470903. [DOI] [PubMed] [Google Scholar]
- 23.Canadian Institute for Health Information. CIHI Data quality study of emergency department visits for 2004-2005. Vol. 2: Main study findings. Ottawa: CIHI; 2008. [Google Scholar]
- 24.Vermeulen Marian J, Ray Joel G, Bell Chaim, Cayen Barry, Stukel Therese A, Schull Michael J. Disequilibrium between admitted and discharged hospitalized patients affects emergency department length of stay. Ann Emerg Med. 2009 Jun 25;54(6):794–804. doi: 10.1016/j.annemergmed.2009.04.017. http://www.scholaruniverse.com/ncbi-linkout?id=19556025. [DOI] [PubMed] [Google Scholar]
- 25.Schull MJ, Hatcher CM, Guttmann A, Leaver CA, Vermeulen M, Rowe BH, Anderson GM, Zwarenstein M. Development of a consensus on evidence-based quality of care indicators for Canadian emergency departments. Toronto: Institute for Clinical Evaluative Sciences; 2010. http://www.ices.on.ca/file/National%20ED%20Quality%20Indicators%20March%2010%202010.pdf. [Google Scholar]
- 26.Iron K, Zagorski BM, Sykora K, Manuel DG. Living and dying in Ontario: an opportunity for improved health information. Toronto: Institute for Clinical Evaluative Sciences; 2008. http://www.ices.on.ca/file/Living_and_dying_in_Ontario_March19-08.pdf. [Google Scholar]
- 27.Bullard Michael J, Unger Bernard, Spence Julie, Grafstein Eric CTAS National Working Group. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) adult guidelines. CJEM. 2008;10(2):136–151. doi: 10.1017/s1481803500009854. http://www.cjem-online.ca/v10/n2/p136. [DOI] [PubMed] [Google Scholar]
- 28.Warren David W, Jarvis Anna, LeBlanc Louise, Gravel Jocelyn CTAS National Working Group; Canadian Association of Emergency Physicians; National Emergency Nurses Affiliation; Association des Médecins d'Urgence du Québec; Canadian Paediatric Society; Society of Rural Physicians of Canada. Revisions to the Canadian Triage and Acuity Scale paediatric guidelines (PaedCTAS) CJEM. 2008;10(3):224–243. http://www.cjem-online.ca/v10/n3/p224. [PubMed] [Google Scholar]
- 29.Redelmeier DA, Stewart CL. The fatal consequences of the Superbowl telecast. Chance. 2005;17:19–24. [Google Scholar]
- 30.Redelmeier DA, Tibshirani RJ. Road crashes and the next U.S. presidential election. Chance. 2010;23(3):20–24. [Google Scholar]
- 31.World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th rev. Geneva: The Organization; 2004. [Google Scholar]
- 32.Wilbert-Lampen Ute, Leistner David, Greven Sonja, Pohl Tilmann, Sper Sebastian, Völker Christoph, Güthlin Denise, Plasse Andrea, Knez Andreas, Küchenhoff Helmut, Steinbeck Gerhard. Cardiovascular events during World Cup soccer. N Engl J Med. 2008;358(5):475–483. doi: 10.1056/NEJMoa0707427. [DOI] [PubMed] [Google Scholar]
- 33.Leeka Justin, Schwartz Bryan G, Kloner Robert A. Sporting events affect spectators' cardiovascular mortality: it is not just a game. Am J Med. 2010;123(11):972–977. doi: 10.1016/j.amjmed.2010.03.026. http://www.scholaruniverse.com/ncbi-linkout?id=21035586. [DOI] [PubMed] [Google Scholar]
- 34.Redelmeier Donald A. Multiple attacks from multiple perspectives. J Clin Epidemiol. 2006 Jun 19;59(9):871–872. doi: 10.1016/j.jclinepi.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 35.Spa MM, Rivenburgh NK, Larson JF. Television in the Olympics. London: John Libbey; 1995. [Google Scholar]
- 36.Linden J. Obama, Canada’s Harper bet beer on ice hockey. 2010. Feb 28, accessed 2010 Mar 16 http://ca.reuters.com/article/sportsNews/idCATRE61R2VN20100228.
- 37.Reich N T, Moscati R, Jehle D, Ciotoli M. The impact of a major televised sporting event on emergency department census. J Emerg Med. 1994;12(1):15–17. doi: 10.1016/0736-4679(94)90005-1. http://www.scholaruniverse.com/ncbi-linkout?id=8163798. [DOI] [PubMed] [Google Scholar]
- 38.Farrell Stephen, Doherty Gary M, McCallion William A, Shields Michael D. Do major televised events affect pediatric emergency department attendances or delay presentation of surgical conditions? Pediatr Emerg Care. 2005;21(5):306–308. doi: 10.1097/01.pec.0000168987.61127.69. [DOI] [PubMed] [Google Scholar]
- 39.Jerrard David A. Male patient visits to the emergency department decline during the play of major sporting events. West J Emerg Med. 2009;10(2):101–103. doi: 10.1111/j.1442-2026.1998.tb00665.x. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/19561829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yusuf Salim, Hawken Steven, Ounpuu Stephanie, Dans Tony, Avezum Alvaro, Lanas Fernando, McQueen Matthew, Budaj Andrzej, Pais Prem, Varigos John, Lisheng Liu INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 41.Green G B, Burnham G. Health care at mass gatherings. JAMA. 1998;279(18):1485–1486. doi: 10.1001/jama.279.18.1485. [DOI] [PubMed] [Google Scholar]
- 42.Pitts S R, Kolla I S. The "Sherman effect": decreased ambulatory care volumes in Atlanta during the 1996 Summer Olympic Games. Med J Aust. 2000;173(6):309–311. doi: 10.5694/j.1326-5377.2000.tb125663.x. [DOI] [PubMed] [Google Scholar]
- 43.Redelmeier Donald A, Stewart Craig L. Driving fatalities on Super Bowl Sunday. N Engl J Med. 2003;348(4):368–369. doi: 10.1056/NEJM200301233480423. http://dx.doi.org/10.1056/NEJM200301233480423. [DOI] [PubMed] [Google Scholar]
- 44.Hiltunen Tuomas, Kuisma Markku, Määttä Teuvo, Tennilä Arto, Hari Tuomo, Bäckman Riitta, Väyrynen Taneli. Prehospital emergency care and medical preparedness for the 2005 World Championship Games in Athletics in Helsinki. Prehosp Disaster Med. 2007;22(4):304–311. doi: 10.1017/s1049023x0000491x. [DOI] [PubMed] [Google Scholar]
- 45.Cooke M W, Allan T F, Wilson S. A major sporting event does not necessarily mean an increased workload for accident and emergency departments. Euro96 Group of Accident and Emergency Departments. Br J Sports Med. 1999;33(5):333–335. doi: 10.1136/bjsm.33.5.333. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/10522636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berthier F, Boulay F. Lower myocardial infarction mortality in French men the day France won the 1998 World Cup of football. Heart. 2003;89(5):555–556. doi: 10.1136/heart.89.5.555. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/12695467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kloner Robert A, McDonald Scott, Leeka Justin, Poole W Kenneth. Comparison of total and cardiovascular death rates in the same city during a losing versus winning super bowl championship. Am J Cardiol. 2009 Apr 22;103(12):1647–1650. doi: 10.1016/j.amjcard.2009.02.012. http://www.scholaruniverse.com/ncbi-linkout?id=19539070. [DOI] [PubMed] [Google Scholar]
- 48.Kloner Robert A, McDonald Scott A, Leeka Justin, Poole W Kenneth. Role of age, sex, and race on cardiac and total mortality associated with Super Bowl wins and losses. Clin Cardiol. 2011 Jan 31;34(2):102–107. doi: 10.1002/clc.20876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reis BY, Brownstein JS, Mandi KD. Running outside the baselines: impact of the 2004 Major League Baseball postseason on emergency department use correspondence. Ann Emerg Med. 2005;46(4):386–387. doi: 10.1016/j.annemergmed.2005.04.031. [DOI] [PubMed] [Google Scholar]
- 50.Moody William E, Hendry Ross G, Muscatello David. Were attendances to accident and emergency departments in England and Australia influenced by the Rugby World Cup Final 2003. Eur J Emerg Med. 2007;14(2):68–71. doi: 10.1097/01.mej.0000228450.37974.a8. [DOI] [PubMed] [Google Scholar]
- 51.Redelmeier Donald A, Bell Chaim M. Weekend worriers. N Engl J Med. 2007;356(11):1164–1165. doi: 10.1056/NEJMe068310. http://www.nlm.nih.gov/medlineplus/heartattack.html. [DOI] [PubMed] [Google Scholar]
- 52.Dawson Heather, Zinck Greg. CIHI Survey: ED spending in Canada: a focus on the cost of patients waiting for access to an in-patient bed in Ontario. Healthc Q. 2009;12(1):25–28. doi: 10.12927/hcq.2009.20411. http://www.longwoods.com/product.php?productid=20411. [DOI] [PubMed] [Google Scholar]
- 53.Redelmeier Donald A, Cialdini Robert B. Problems for clinical judgement: 5. Principles of influence in medical practice. CMAJ. 2002;166(13):1680–1684. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/12126325. [PMC free article] [PubMed] [Google Scholar]
- 54.Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth, and happiness. Yale (CT): Yale University Press; 2008. [Google Scholar]