Abstract
Objectives:
Most patients with anti-NMDA receptor (NMDAR) encephalitis have intrathecal synthesis of antibodies, which cause a decrease of cell surface and synaptic NMDAR. Antibodies are immunoglobulin G (IgG)1 and IgG3 subtypes and can potentially activate complement. We examined whether complement immunoreactivity and antibody-secreting cells (plasma cells/plasmablasts) are present in the brain of these patients.
Methods:
Cultured rat hippocampal neurons were used in an immunocytochemical assay to test whether patients' antibodies can fix complement. Using the same reagents (antibodies to C9neo, C5b-9, C3), complement immunoreactivity was determined in the brain of 5 patients, the teratoma of 21 patients, and appropriate control tissues. A set of markers for B (CD20), T (CD3, CD4, CD8) and antibody-secreting cells (plasma cells/plasmablasts, CD138) were used to examine the brain inflammatory infiltrates.
Results:
Patients' antibodies were able to bind complement in vitro, but deposits of complement were not detected in patients' brain. Parallel experiments with teratomas showed that in contrast to the brain, the neural tissue of the tumors contained complement. Analysis of the inflammatory infiltrates in brain samples from autopsy or biopsy performed 3–4 weeks after symptom presentation demonstrated numerous antibody-secreting cells (CD138+) in perivascular, interstitial, and Virchow-Robin spaces, and B and T cells predominantly located in perivascular regions.
Conclusions:
Complement-mediated mechanisms do not appear to play a substantial pathogenic role in anti-NMDAR encephalitis. In contrast, there are copious infiltrates of antibody-secreting cells (plasma cells/plasmablasts) in the CNS of these patients. The demonstration of these cells provides an explanation for the intrathecal synthesis of antibodies and has implications for treatment.
Anti-NMDA receptor (NMDAR) encephalitis is a severe but treatable disorder that results in psychiatric, memory, and stereotyped motor symptoms, and associates with teratomas depending on patient's age, gender, and ethnicity.1 In vitro and in vivo experiments demonstrate that patients' antibodies cause a selective and reversible decrease in NMDAR surface density and synaptic localization that correlates with antibody titers and is mediated by crosslinking and internalization of the receptors.2 The antibodies are IgG1 and IgG3 subtypes3,4 and while they can potentially activate complement, it is unknown if this occurs in the disease. Previous neuropathologic studies showed microglial activation, moderate inflammatory infiltrates that predominated in perivascular spaces, deposits of IgG, and absent or rare neuronal degeneration.5,6 In these studies, absence of complement and presence of plasma cells were reported but were not extensively studied.
The MRI of many patients with anti-NMDAR encephalitis is normal or shows mild to moderate abnormal findings which are often transient or reversible.7,e1,e2 Moreover, despite the severity of the disorder, 75% of patients have full or substantial neurologic recovery, suggesting that complement-mediated neuronal toxicity is unlikely to play a major pathogenic role.7 We also postulated that the high intrathecal synthesis of antibodies identified in most patients1,4,e3 indicates the presence of antibody-secreting cells in the CNS. We report here findings that support these hypotheses.
METHODS
Patients, tissue, neuronal cultures, and in vitro analysis of complement binding.
Tissues included paraffin-embedded brain biopsy or autopsy samples of 5 patients with anti-NMDAR encephalitis (table), 2 brain tissue samples from autopsies of neurologically normal individuals, 21 ovarian teratomas of patients with anti-NMDAR encephalitis, and 8 ovarian teratomas of individuals without encephalitis and without NMDAR antibodies.
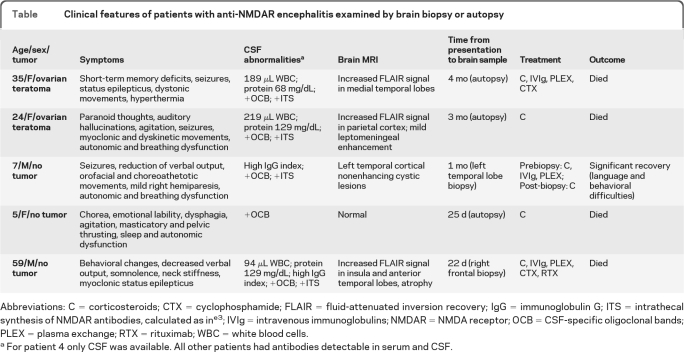
Table.
Clinical features of patients with anti-NMDAR encephalitis examined by brain biopsy or autopsy
Abbreviations: C =corticosteroids; CTX =cyclophosphamide; FLAIR =fluid-attenuated inversion recovery; IgG =immunoglobulin G; ITS=intrathecal synthesis of NMDAR antibodies, calculated as ine3; IVIg =intravenous immunoglobulins; NMDAR =NMDA receptor; OCB =CSF-specific oligoclonal bands; PLEX =plasma exchange; RTX =rituximab; WBC =white blood cells.
For patient 4 only CSF was available. All other patients had antibodies detectable in serum and CSF.
Cultures of rat hippocampal neurons were established as reported.e4 In vitro analysis of complement binding by patients' antibodies is described in appendix e-1 on the Neurology® Web site at www.neurology.org.
Immunohistochemistry.
Paraffin-embedded brain and tumor sections were deparaffinized and the antigen retrieved as reported.e5 Tissue sections were serially incubated with 0.3% H2O2 for 15 minutes, 5% goat serum for 30 minutes, and primary antibodies (C3, C9neo, MAP2, CD3, CD4, CD8, CD20, or CD138) overnight at 4°C, followed by the appropriate biotinylated secondary antibodies (1:2,000) for 2 hours. Reactivity was developed with the avidin-biotin-peroxidase method (see appendix e-1 for further information).
Standard protocol approvals, registrations, and patient consents.
Studies were approved by the Institutional Review Board of the University of Pennsylvania. In all instances, written consent for studies was provided by guardians of patients.
RESULTS
Complement immunoreactivity in the tumor but not in the brain of patients with anti-NMDAR encephalitis.
Using cultures of rat hippocampal neurons, we confirmed that patients' antibodies were able to fix complement (figure e-1). Next, we examined the presence of complement in patients' brain and tumor, comparing these tissues side by side. Deposits of IgG in patients' brain were reported in previous studies5 and are not described here. No complement immunostaining was detected in any of the brain regions from autopsies of 3 patients (frontal, temporal lateral, temporal medial/hippocampus, and parietal) and biopsies of 2 patients with anti-NMDAR encephalitis (figure 1, A and B), or in the control brain samples (figure 1C).
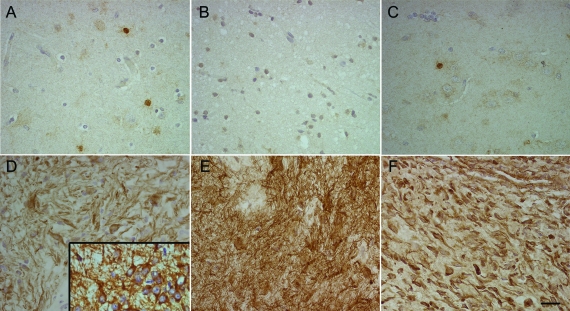
Figure 1. Comparative analysis of complement immunostaining in brain and tumor.
Paraffin-embedded sections of brain of 2 patients with anti-NMDA receptor (NMDAR) encephalitis (A, B), control brain (C), and teratomas of patients with anti-NMDAR encephalitis (D–F), all immunostained with anti-C9neo. While patients' tumors show intense complement immunoreactivity on the cell surface of neurons and neuronal processes, the brain of patients and a control individual show lack of complement (the nuclear staining is not specific). Inset in D shows staining of neurons contained in the tumor with MAP2, a specific dendritic marker. Scale =20 μm.
Patient 3 was atypical because the brain MRI showed cortical cystic lesions suggesting necrosis (figure 2). Biopsy of one of the lesions showed necrosis, dystrophic calcification, chronic inflammation, and microglial activation. Studies for an infectious process were negative and the etiology of these cystic lesions remains unknown. Complement immunostaining was only detected in the necrotic tissue (figure 2D).
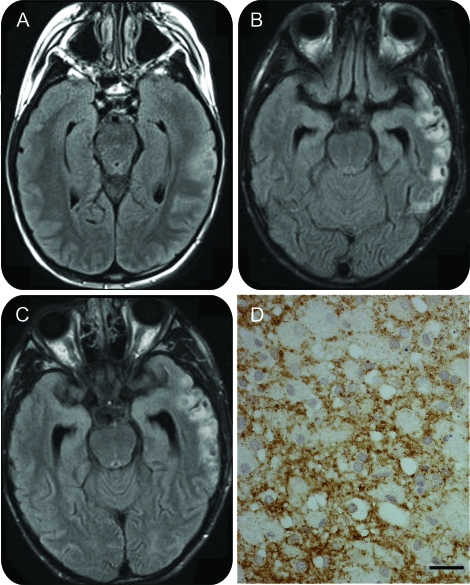
Figure 2. Brain MRI and biopsy of a patient with anti-NMDA receptor (NMDAR) encephalitis and cortical cystic lesions.
Fluid-attenuated inversion recovery MRI obtained at 2 (A), 8 (B), and 16 (C) weeks after symptom presentation. There is progressive development of abnormal areas with cystic changes. Biopsy of one of these lesions showed prominent necrosis, and complement immunostaining in the necrotic tissue without recognizable neurons (D, immunostained with anti-C9neo). No complement immunoreactivity was noted outside the necrotic tissue (not shown). Scale =20 μm.
All teratomas from patients with anti-NMDAR encephalitis and control teratomas showed the presence of nervous tissue, including neuronal-like cells and networks of neuronal processes expressing MAP2 (inset in figure 1D). Complement immunoreactivity was found in 17 of 21 teratomas of patients with anti-NMDAR encephalitis (figure 1, D–F) and in 5 of 8 control teratomas (not shown); the cell surface complement immunoreactivity was highly confined to neuronal tissue.
Antibody-secreting cells in perivascular, interstitial, and Virchow-Robin spaces.
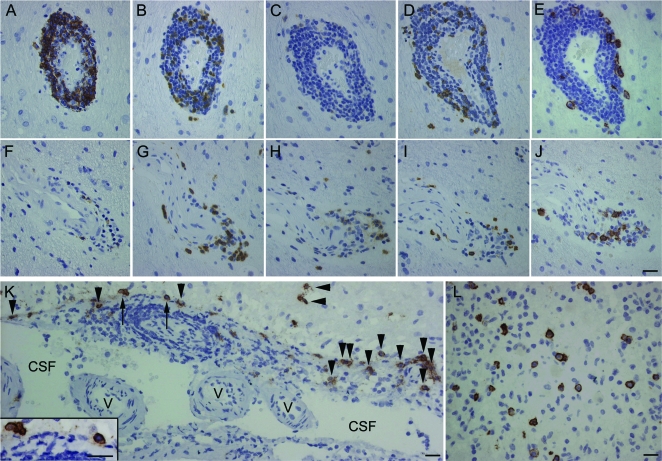
Brain tissue samples from patients 3–5 were available for these studies. In all 3 patients, abundant CD138+ cells (plasma cells/plasmablasts) were noted in perivascular regions and interstitial space (figures 3 and e-2). In perivascular regions, the CD138+ cells were part of B- and T-cell lymphocytic cuffing surrounding blood vessels. In Virchow-Robin spaces, CD138+ cells were found along with other inflammatory infiltrates lining the meningeal-brain surface in proximity to the CSF (figure 3K).
Figure 3. CD138+ cells in brain of patients with anti-NMDA receptor (NMDAR) encephalitis.
Paraffin-embedded sections of brain biopsy of 2 patients with anti-NMDAR encephalitis (patient 5, top and middle rows; patient 3, lower row) immunostained with anti-CD20 (A, F), anti-CD3 (B, G), anti-CD4 (C, H), anti-CD8 (D, I), and anti-CD138 (E, J–L). CD138+ cells (plasma cells/plasmablasts) are present in perivascular (E, J), Virchow-Robin (K), and interstitial spaces (L). In Virchow-Robin spaces (K), the CD138+ cells are in perivascular regions (arrows) and along the tissue surface (arrowheads) that delineates spaces containing CSF and small vessels (v). The plasma cells/plasmablasts indicated with arrows are amplified in the inset in K. Scales =20 μm.
DISCUSSION
The 2 main findings of this study are the absence of deposits of complement and the presence of abundant CD138+ cells (plasma cells/plasmablasts) in the brain of patients with anti-NMDAR encephalitis. The absence of complement was emphasized in studies comparing in parallel brain and tumor tissue, showing that in contrast to brain, the neural tissue contained in tumors frequently had complement immunoreactivity. Whether the cystic lesions in the brain of patient 3 were caused by complement-mediated toxicity is unclear; we have not identified similar lesions in 400 patients with anti-NMDAR encephalitis.1
Complement immunoreactivity was identified in 81% of teratomas from patients with anti-NMDAR encephalitis and 62.5% of teratomas from control individuals, suggesting the presence of antibody-dependent and independent mechanisms of complement binding. Indeed, studies using human fetal neurons have shown spontaneous complement activation through the classic pathway in immunoglobulin-deficient serum.8 Similar to these experiments, we found linear deposits of complement in 5% of cultured rodent neurons treated with human complement regardless of the presence of neuronal antibody binding (data not shown).
CD138 is a highly specific marker of plasma cells and plasmablasts, which are precursors of plasma cells. Our studies do not clarify whether the brain-infiltrating CD138+ cells were plasma cells or plasmablasts, but both types of cells are known to secrete high amounts of antibodies.e6 These cells were found in perivascular, interstitial, and Virchow-Robin spaces, providing an explanation for the intrathecal synthesis of antibodies frequently noted in anti-NMDAR encephalitis.1,4
We postulate that after systemic immune activation by an NMDAR-expressing tumor or unknown mechanisms, antibodies synthesized systemically may cross the blood–brain barrier (BBB) through leaky regions, but activated B cells that are able to cross an intact BBB reach the brain and differentiate into plasmablasts/plasma cells, producing most of the antibodies detected in patients' CNS. These antibodies cause a decrease of cell surface and synaptic NMDAR, as reported.2 The lack of complement immunoreactivity in patients' brain is likely due to the low levels of complement in the CNS (estimated 440 times lower than serum levels9).
The brain infiltrates of plasma cells/plasmablasts provide a plausible explanation for the prolonged clinical course of anti-NMDAR encephalitis,1,4 and for the limited response to plasma exchange or IVIg once the peripheral immune response has expanded in the CNS. Accordingly, patients with protracted symptoms usually have persistent levels of antibodies in the CSF.e7 The half-life of human plasmablasts is believed to be several days, but plasma cells may live many months in an inflammatory environment, such as that provided by B and T cells.e6,e8,e9 Moreover, plasma cells and most plasmablasts do not express CD20, the target of rituximab. This is important because in current practice, patients who do not improve with IV immunoglobulin, plasma exchange, or corticosteroids are frequently treated with rituximab or cyclophosphamide. These drugs have limited BBB penetration but result in improvement in approximately 70% of those cases.1 While rituximab causes a decrease of B cells and prevents maturation into antibody-secreting cells,10 cyclophosphamide reduces all types of inflammatory infiltrates. The distribution of plasma cells/plasmablasts noted in this study suggests that treatment strategies that facilitate BBB penetration, such as high-dose methotrexate, may be useful in patients with refractory symptoms and persistently elevated CSF antibody titers.
Future studies should focus on the analysis of a possibly CNS compartmentalized B cell immune response in patients with anti-NMDAR encephalitis, and how an expansion or retraction of this response may explain maintenance, improvement, or relapse of symptoms.
Supplementary Material
GLOSSARY
- BBB
blood–brain barrier
- IgG
immunoglobulin G
- NMDAR
NMDA receptor
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Dr. Martinez-Hernandez: drafting/revising the manuscript, analysis or interpretation of data, acquisition of data, study supervision. Dr. Horvath: drafting/revising the manuscript, acquisition of data. Dr. Shiloh-Malawsky: drafting/revising the manuscript, contribution of vital reagents/tools/patients. Dr. Sangha: drafting/revising the manuscript. Dr. Martinez-Lage: drafting/revising the manuscript, analysis or interpretation of data, acquisition of data. Dr. Dalmau: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, contribution of vital reagents/tools/patients, statistical analysis, study supervision, obtaining funding.
ACKNOWLEDGMENT
The authors thank the physicians who provided clinical information and tissue samples.
DISCLOSURE
Dr. Martinez-Hernandez receives research support from the Fondo de Investigaciones Sanitarias, FIS, Spain. Dr. Horvath has received funding for travel from UCB and research support from the Parkinson Swiss Foundation. Dr. Shiloh-Malawsky and Dr. Sangha report no disclosures. Dr. Martinez-Lage holds a patent re: Compositions and methods for the treatment of frontotemporal lobar degeneration with TDP-43 inclusions. Dr. Dalmau serves on the editorial board of Neurology®; receives royalties from the editorial board of Up-To-Date; has filed a patent application for the use of LGI1 as a diagnostic test; has received royalties from Athena Diagnostics, Inc. for a patent re: Ma2 autoantibody test and has patents pending re: NMDA and GABAB receptor autoantibody tests (license fee payments received from EUROIMMUN AG); and receives research support from EUROIMMUN AG, the NIH/NCI, and a McKnight Neuroscience of Brain Disorders award. Dr. Dalmau is ICREA (Institució Catalana de Recerca i Estudis Avançats) Research Professor at IDIBAPS, Hospital Clínic, Barcelona, Spain.
REFERENCES
- 1. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 2011;10:63–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hughes EG, Peng X, Gleichman AJ, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci 2010;30:5866–5875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tuzun E, Zhou L, Baehring JM, Bannykh S, Rosenfeld MR, Dalmau J. Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol Epub 2009 Aug 14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Irani SR, Bera K, Waters P, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 2010;133:1655–1667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007;61:25–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Camdessanche JP, Streichenberger N, Cavillon G, et al. Brain immunohistopathological study in a patient with anti-NMDAR encephalitis. Eur J Neurol Epub 2010 Aug 16 [DOI] [PubMed] [Google Scholar]
- 7. Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singhrao SK, Neal JW, Rushmere NK, Morgan BP, Gasque P. Spontaneous classical pathway activation and deficiency of membrane regulators render human neurons susceptible to complement lysis. Am J Pathol 2000;157:905–918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kossmann T, Stahel PF, Morganti-Kossmann MC, Jones JL, Barnum SR. Elevated levels of the complement components C3 and factor B in ventricular cerebrospinal fluid of patients with traumatic brain injury. J Neuroimmunol 1997;73:63–69 [DOI] [PubMed] [Google Scholar]
- 10. Hauser SL, Waubant E, Arnold DL, et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med 2008;358:676–688 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.