Description
73-year-old female presented with foul smelling discharge from the perianal area. Examination revealed cutaneous fistula, discharging faeculent material. CT showed a large rectal tumour with gross evasion of the perianal tissues, with extension into vagina and subcutaneous tissue bilaterally and a large volume of air in tissues (figure 1). Laparotomy demonstrated rectal tumour, Fournier’s grangrene with abscess cavities on both sides, disruption of the lower end of the rectum and a fistulating tract into the vagina (figure 2). Colostomy and extensive debridement of necrotic material was performed. Further, debridement and delayed primary closure were carried out, after which she commenced radiotherapy.
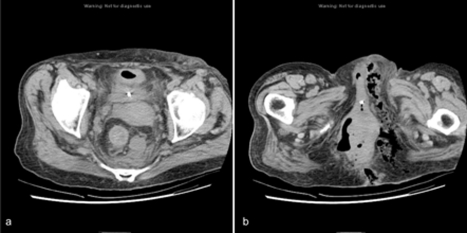
Figure 1.
CT demonstrating a large rectal tumour (A) with gross evasion of the perianal tissues, extension into the vagina and subcutaneous tissue bilaterally and a large volume of air in the tissues (B).
Figure 2.
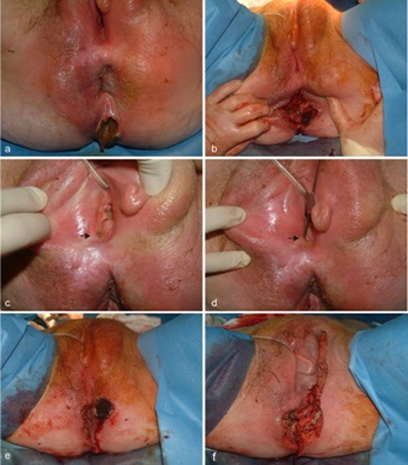
Rectocutaneous fistula (A), rectal tumour (B) with disruption of lower end of rectum. Fistulating tract into the vagina (arrow, C), explored with fistula probe (arrow, D). Fournier’s gangrene (E), requiring extensive debridement of necrotic tissue (F).
Colocutaneous fistulae can result from diverticulitis, Crohn’disease, appendicitis, pancreatitis, radiation therapy and malignancy, while the surgical treatment of these conditions account for the majority of cases.1 Fistulae from malignancy are rarely seen today because most colon cancers are diagnosed and treated at an earlier stage. Investigations include enema studies or CT. Management involves proximal diversion and treatment of pathology. Fournier’s gangrene is a necrotising fasciitis, involving the perineum and genital organs.2 It was described by Baurienne in 1764 and formally named by Fournier in 1883. The infection is usually polymicrobial and synergistic. Risk factors include diabetes, alcohol abuse and immunosuppression. Diagnosis is clinical, but radiological investigations may be helpful. CT outlines the extent and source of infection. Treatment consists of antibiotics and aggressive surgical debridement of all necrotic tissue.2 3 Urinary or faecal diversion might be required to prevent contamination or to treat an underlying condition.
Acknowledgments
Female Surgical ward and theatre, South Infirmary Victoria Hospital
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Lavery IC. Colonic fistulas. Surg Clin North Am 1996;76:1183–90 [DOI] [PubMed] [Google Scholar]
- 2.Eke N. Fournier’s gangrene: a review of 1726 cases. Br J Surg 2000;87:718–28 [DOI] [PubMed] [Google Scholar]
- 3.Endorf FW, Supple KG, Gamelli RL. The evolving characteristics and care of necrotizing soft-tissue infections. Burns 2005;31:269–73 [DOI] [PubMed] [Google Scholar]