Abstract
Imiquimod is a TLR7/8 agonist that has anti-cancer therapeutic efficacy in the treatment of pre-cancerous skin lesions and certain non-melanoma skin cancers. To test our hypothesis that imiquimod enhances DNA repair as a mechanism for its anticancer activity, the nucleotide excision repair genes were studied in bone marrow derived cells. Imiquimod enhanced the expression of XPA and other DNA repair genes (qPCR analysis), and resulted in an increased nuclear localization of the DNA repair enzyme XPA. This was dependent on MyD88, as bone marrow derived cells from MyD88−/− mice did not increase XPA gene expression, and did not enhance the survival of MyD88−/− derived bone marrow derived cells after UVB exposure as was observed in bone marrow derived cells from MyD88+/+ mice. Imiquimod also enhanced DNA repair of UVL irradiated gene expression constructs, and accelerated the resolution of cyclobutane pyrimidine dimers (CBPD) after UVL exposures in P388 and XS52. Lastly, topical treatment of mouse skin with 5% imiquimod cream prior to UVL irradiation resulted in a decrease in the number of cyclobutane pyridimine dimer positive, APC that were found in local lymph nodes 24 hours after UVL irradiation in both wild type and IL-12 gene targeted mice. In total, these data support the idea that TLR7 agonists such as imiquimod enhance DNA repair in bone marrow derived cells. This property is likely to be an important mechanism for its anti-cancer effects, because it protects cutaneous APC from the deleterious effects of UVL.
Introduction
Ultraviolet light (UVL) is a well-characterized carcinogen that causes genetic lesions in epidermal keratinocytes, which over time accumulate, and play a critical role in the development of skin cancers (1, 2). Equally important in the development of skin cancer is the immunosuppressive cutaneous micro-environment that develops as a result of chronic UVL exposures. Immunosuppressive cytokines such as IL-10 are induced after UVL exposure (3, 4). Additionally, there is impaired antigen presentation by skin derived dendritic cells such as Langerhans cells (LC), and immune suppressive macrophages migrate into skin after UV exposures (5,6). As a result of UVL impairment of cutaneous antigen presenting cells (APC), there is impairment in the development of Th1-immunity, and loss of sensitization to potent topically applied haptens (7,8). Instead of sensitization, there is hapten-specific immune tolerance that can be adoptively transferred to naïve hosts by Tregulatory cells (9). This loss of contact hypersensitivity is thought to be a sentinel event that correlates well with the loss of immunologic reactivity against tumor antigens that develop in parallel as a result of chronic UVL exposures. Thus, instead of preventing the development and progression of UVL induced skin tumors, there is immune tolerance and a permissive environment for skin cancer development.
The fundamental lesion for both skin cancer development as well as photo-immunosuppression is DNA damage. Within twenty four hours of UVL exposures, dendritic antigen presenting cells (APC) with cyclobutane pyrimidine dimers (CBPD) have been found in the paracortical area of draining lymph nodes of UVL irradiated mice (10). Such APC that bear DNA damage are in part responsible for the loss of protective cutaneous immunity against skin cancer development (11). A biomarker for the loss of cutaneous immunity is the loss of contact sensitization. Local exposure of the skin to UVL results in both local and systemic effects. In models systems to protect mice from cutaneous immunosuppression after UVL exposures, a variety of treatments have been applied in an attempt to enhance DNA repair by APC, potentially restoring immune competence after UVL exposures. DNA-repair promoting agents include bacterial DNA repair enzymes (T4 endonuclease encapsulated into liposomes)(12), green tea polyphenols (13) and cytokines such as IL-12 and IL-23, platelet activating factor and serotonin receptor antagonists (14, 15, 16).
In recent studies, the effect of topically applied imiquimod was studied in a mouse model of UVL induced loss of hapten sensitization. This treatment prevented the loss of contact hypersensitivity as well as the development of hapten-specific tolerance (17). Even though imiquimod preserved contact hypersensitivity in vitro, it did not protect from UVL induced depletion of LC from the epidermis of UVL irradiated skin (17). In vitro, imiquimod activation of TLR7 prior to UVL exposure induced resistant APC maturation, preserving Th1-lymphocyte derived cytokines. This is in marked contrast to UVL irradiated APC that were not activated with imiquimod. These data lead us to hypothesize that imiquimod, via TLR7 activation, renders cutaneous APC resistant to UVL induced immunosuppression because it enhances DNA repair. Herein we describe the effects of imiquimod on APC DNA repair of UVL damage. We found that imiquimod induces DNA repair gene expression that is dependent on MyD88 as well as an intact NF-kB signaling pathway, which are early and late components of TLR signaling pathway. As well, imiquimod activated APC were resistant to UVL and ionizing radiation induced loss of viability. Additionally, imiquimod activated APC exhibited enhanced functional DNA repair compared to resting APC. Lastly, topical application of imiquimod prior to UVL exposure resulted in a marked reduction of CBPD positive APC and a reduction in suppressive cytokine gene expression in local lymph nodes of such treated mice when compared to vehicle or untreated, irradiated mice. These data lead us to conclude imiquimod-mediated, TLR7 signaling enhances repair of UVL damage to genomic DNA, and may play a therapeutic role in the preservation of an intact cutaneous immune response after exposure to UVL.
Materials and Methods
Experimental Mice
C57BL/6 female mice, 8 weeks old were purchased from Jackson Laboratories (Bar Harbor, ME). These animals were chosen because they have been demonstrated to exhibit a phenotype of susceptibility to UV-induced suppression of CHS (18, 19). IL-12p40 gene targeted female mice (B6.129S1IL2btm1Jm/J, stock number 002693) in the C57BL/6 background were purchased from The Jackson Laboratory (Bar Harbor, Maine) (20). Animals were kept in standard housing conditions, fed mouse chow ad libatum, and exposed to a 12 hour light/dark cycle. To study the appearance of APC in local lymph nodes, experimental mice (either wild type or IL-12 gene targeted mice) were un-irradiated, or irradiated with a single dose of UVB at a dose of 150 mJ/cm2. Some of the UVB irradiated mice received topical applications of 5% imiquimod cream or its vehicle to the dorsal aspect of the pinna of the ear (once daily for two days); twenty four hours later, the animals were then exposed to UVB. For the UVB exposure, the animals were anesthetized with a single dose of avertin (intraperitoneal injection), then the animals' ears were taped to a restraining chamber, and the dorsum exposed to the indicated dose of UVB. Twenty four hours after this, the animals were sacrificed, and the cervical lymph nodes were dissected, and DNA extracted using standard methods. All experimental procedures were reviewed and approved by the University of Maryland Institutional Animal Care and Use Committee.
Cell lines
A20 was purchased from ATCC. P388 cell line was a generous gift from Dr. David Scott (University of Maryland Baltimore). XS52 was a generous gift from Dr. Akira Takashima (University of Toledo), and was cultured using standard conditions. Wild-type macrophages and MyD88 knockout cell lines were a generous gift from Dr. Doug Gollenbach (University of Massachusetts). XPA lymphoblasts were purchased from Coreill Institute (Camden, NJ). Control lymphoblasts were produced by our laboratory using EBV transformation of peripheral blood mononuclear cells from a healthy volunteer who had normal DNA repair (21).
Cytotoxicity Assay
A thiazolyl blue tetrazolium bromide (MTT assay) was used to measure cell viability twenty four hours after UVL or ionizing radiation exposures (22). Either adherent cells (P388) or non-adherent lymphoblasts (EBV immortalized cells) were used at a cell density of approximately 5,000 cells/well of a 96 well plate. For adherent P388 cells, the cells remained adherent to the microtiter wells; for the non-adherent lymphoblasts (XPA or control lymphoblasts), the microtiter plates were centrifuged (1200 RPM for 10 minutes) prior to any washes or medium changes. Using standard methods (22), MTT solution (20 μl of 5mg/ml MTT stock solution) was added to cell cultures, then incubated for 4 hours at 37°C. The culture medium was then removed, and 150 μl of MTT solvent (4mM HCL, 0.1% Nondet P-40(NP40) in isopropanol was added, and the plates were covered with tinfoil and placed on an orbital shaker for 15 minutes. The optical density (OD) was read at 590nm with a reference filter of 620nm. Background O.D. was MTT was assayed in wells that contained no cells.
Ultraviolet Light Source
Groups of mice were irradiated with a panel of 48” Q-Sun light bank (Q-Panel Laboratory products, Cleveland, OH) (equipped with a UVC WG320 filter) at a distance of 12 inches from the light source to their shaved abdominal skin. The spectral emission profile of this light source closely mimics that of natural sunlight, emitting predominantly UVA. A UVB radiometer (National Biologic Corporation, Twinsburg, OH) was used to determine UVB output, and calculate the time necessary to deliver the desired doses of UVB. Plasmid DNA, cell monolayers or experimental mice received UVL, at the doses indicated in each of the individual experiments.
Ionizing Radiation
A 137Cs radiation source was utilized to deliver ionizing radiation to either control or XPA lymphoblasts. Exposure time of the irradiated cells was adjusted to deliver the desired dose of radiation (see results), using calibration curves.
Transient transfection by electoporation and luciferase assays
For the gene reactivation assay, control (medium alone) or imiquimod treated cells (at the indicated doses for 24 hours prior to electroporation) were transfected with the following constructs: pGL3, an empty vector that contains no luciferase gene as a negative control; pGL4.1[luc2], which encodes for firefly luceriferase as a positive control; these negative and positive controls were co-transfected with pGL4.70[hRluc] (renila luciferase), which serves as a control for transfection efficiency. In parallel, control or imiquimod treated cells were transfected with UVL irradiated pGL4.10 [luc2] constructs, with UVL radiation doses ranging from 1,000 to 5,000 mJ/cm2. The UVL irradiated constructs were produced by placing a 5 μl volume of the plasmid DNA on a glass slide, and exposing to the indicated doses of UVL at a 12 inch distance from the UVL source. After UVL irradiation, these constructs were co-transfected with un-irradiated pGL4.70[hRluc], which served as a control for transfection efficiency.
The luminometry data represent a normalized ratio of firefly luciferase to renila luciferase. These normalized data were then normalized to the negative (pGL3/pGL4.7) and positive control values (pGL4.1/pGL4.7). The normalized expression of the UVL-irradiated (pGL4.1UVL/pGL4.7) was then compared to its respective positive and negative controls. Data are reported as % of control because imiquimod treatment of host cells had significant effects on transfection efficiency (expression of positive control construct, data not shown). Thus the formula for calculating gene reactivation was as follows: [(pGL4.1UVL/pGL4.7)− (pGL3/pGL4.7)/(pGL4.1/pGL4.7)− (pGL3/pGL4.7)] × 100 = % Gene reactivation compared to control. We utilized methods as previously described for the luminometry assays (23).
Cell lines (P388, XS52, macrophage cell line) used in the gene reactivation assay were transfected at approximately 70% confluence using the Amaxa nucleofector kit (Amaxa AG, Germany) according to the manufacturer's protocol. Briefly, cells were transfected with 2μg of supercoiled plasmid DNA per well in transfection of 6 well plates. A positive control plasmid pGL4.10 [luc2] which encodes a synthetic firefly luciferase gene. An internal control plasmid, pGL4.70 [hRluc], which expresses the Renilla luciferase gene was also used for correcting variations in the transfection efficiency. After 15 minutes, 1 ml of growth medium was added and incubated for 48h. Lysates were harvested and extracts were prepared using freeze-thaw lysis. Lysates were monitored for luciferase activities using a commercially available Dual Luciferase (firefly and renilla) Reagent kit (Promega) in a Turner 20/20n luminometer (Turner Biosystems, Sunnyvale, CA). Firefly luciferase activity was normalized to the renilla luciferase activity. Briefly, trypsinized 1 million cells were electroporated with 3 μg of DNA and incubated for 48h prior to harvesting the cellular lysates. All gene reporter assays were repeated at least three times.
Chemicals
Imiquimod ((1-(2-Methylpropyl)-1H-imidazo[4,5-c]quinolin-4-amine, R-837) 5% cream and its vehicle cream were used for topical applications, and were provided by Graceway Pharmaceuticals (Exton, PA). For the in vitro studies, imiquimod powder was used (also provided by Graceway Pharmaceuticals). It was prepared as a stock solution in sterile water at 1 mg/ml, and diluted to the appropriate working concentration in complete medium. BAY 11-7085 (Calbiochem) was dissolved in DMSO and was added to the culture medium of APC thirty minutes prior to exposure to imiquimod treatment at the indicated concentrations to block NF-kB (24).
Western blot
Western blotting was performed as previously described (24). Equal quantities of total protein from different samples were separated on a 10% Bis-Tris NuPage denaturing gel (Invitrogen Life Technologies, Carlsbad, CA). Gels were transferred to nitrocellulose membranes and probed with appropriate first antibodies and detected using a Western Breeze Chemiluminescent detection kit (Invitrogen Life Technologies, Carlsbad, CA). The bands were detected using Chemi-Doc densitometer and Quantity-One software (Bio-Rad, Hercules, CA). Beta-actin signals from each same sample were used for normalizing the intensity of specific bands of interest. A mouse anti-XPA antibody (clone B1) (Santa Cruz Biotechnology, Santa Cruz, CA) was used to western blot XPA in control or imiquimod treated cells. This clone was raised against human amino acids 1–123 derived from full length human XPA. This monoclonal antibody reacts with a polypeptide of approximately 38–40kD.
Cell fractionation
Nuclei from cultured cells were isolated using Active Motif Nuclear Extraction Kit (Active Motif North America, Carlsbad, CA). Nuclear extracts were prepared using the manufacturer's instructions.
RNA Extraction, cDNA synthesis and qPCR
Standard methods were utilized to extract total cellular RNA and cDNA synthesis. Detection of XPA, TNF-α and TLR7 mRNA was performed using real-time PCR according to previously published methods (26). The annealing temperature was 55°C, followed by 35 cycles of amplification using a PCR Sprint (Hybaid, Inc.). Primers to amplify mouse DNA repair genes were as follows: XPA (reference #592) and XPC (catalogue #04375e), XPG (catalogue #04636a), XPF Rpa1(catalogue #05392a), Rpa3 (catalogue #03481a), Xab2 (catalogue #05491a), Rad23b(catalogue #04360a), Ddb1 (catalogue# 04381a). Primers to amplify other genes included: TLR7 (reference# 1136), TNF-α (reference# 879) FoxP3, IL-4, IL-10 (catalogue #074) TGF-β (catalogue #035) and 18S (reference #X03205). All of these primers were purchased from Superarray biosciences (Qiagen, Valencia, CA). Real-time PCR (LightCycler, Roche, Indianapolis, IN) was used to confirm differences in the levels of expression of selected mRNA. The primers, PCR protocol, and product quantification for 18S ribosomal RNA were exactly as reported previously (SYBER green detection) (26). Amplification (40–50 cycles) of a single PCR product was confirmed by gel electrophoresis and melting curve analyses. The cDNAs were assayed in duplicate, and mean values are depicted in the graphics for the quantitative PCR.
Statistical Analyses
Graph Pad Instat and Prism software programs (Graph Pad, San Diego, CA.) were used to compare quantitative data from experimental groups for statistical significance. For comparisons between multiple groups, ANOVA was used; p < 0.05 were considered to be statistically significant.
Results
Imiquimod induces DNA repair gene expression in a variety of bone marrow derived cells
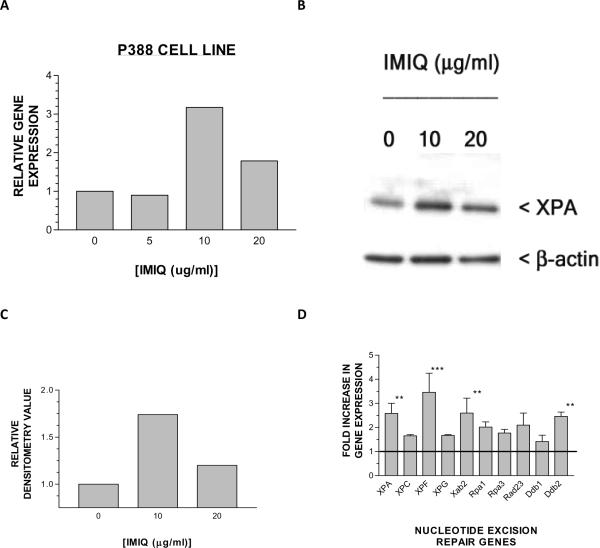
To determine whether the TLR7 agonist, imiquimod, increased DNA repair gene expression in bone marrow derived cells, we cultured a variety of cell lines with this agent, and studied DNA repair gene expression. Although there are a over 30 genes involved in the repair of DNA damage induced by ultraviolet light, we focused on XPA gene expression because it is involved in the recognition of UV damage to DNA, an early event in the DNA repair process (6). The importance of this gene in DNA repair is further confirmed by the clinical correlation that defects in this DNA repair gene can resulting in a severe xeroderma pigmentosum phenotype (27). As demonstrated in Figure 1, P388 cell line (monocyte lineage) exhibited enhanced XPA gene expression as a result of the addition of imiquimod to the cell culture medium (A). Twenty four hours after imiquimod treatment, XPA protein (as detected by western blotting, see methods) is increased in the nucleus of imiquimod-stimulated P388 compared to control (unstimulated) P388 (B); densitometry scanning of the western blot autoradiogram was then normalized (XPA/β-actin ratio), and is presented as a histogram in (C), with a close to two fold increase in nuclear XPA protein at 24 hours after 10 μg/ml imiquimod exposure, and a smaller increase induced by imiquimod at 20 μg/ml. Because DNA repair of UVL damage is a complex process that involves a family of DNA damage recognition and repair, we screened P388 cell line for changes in other repair genes at the 10 μg/ml dose of imiquimod, and found that the transcription of the entire family of genes was modestly increased (range of increase between 1.5 to 3.5 fold above control cells (D). We found that the optimal dose for the increasing XPA gene expression, as well as the amplitude of the increase, varied between these three cell lines. The optimal dose of imiquimod for increasing XPA gene expression varied between 10–30 μg/ml, which is slightly higher than the optimal dose (5–10 μg/ml) for triggering cytokine secretion by TLR7 expressing mouse antigen presenting cells (28).
Figure 1. Imiquimod enhances gene expression and nuclear localization of the DNA repair enzyme, XPA in bone marrow derived cells.
(A)The P388 cell line was incubated with medium alone, or medium containing the indicated doses of imiquimod, for 6 hours, and then gene expression was assayed using qPCR analysis (single representative experiment, see methods). (B) Western blotting of nuclear XPA (approximately 38kD) 24 hours after P388 was incubated with medium alone, or medium containing the indicated doses of imiquimod. (C) Densitometry scanning of normalized XPA/β-actin indicated that there was close to a two-fold increase in nuclear XPA protein in imiquimod treated cells. (D) Fold change expression of multiple DNA repair genes in P388 cells cultured with 10 μg/ml of imiquimod relative to cells cultured in medium alone (not shown, but depicted as horizontal line) (The data in this experiment represent the mean and standard deviation of three different gene expression experiments; **p < 0.01; ***p < 0.001, ANOVA).
Imiquimod Enhanced DNA repair gene expression and survival after UV exposure is dependent on MyD88
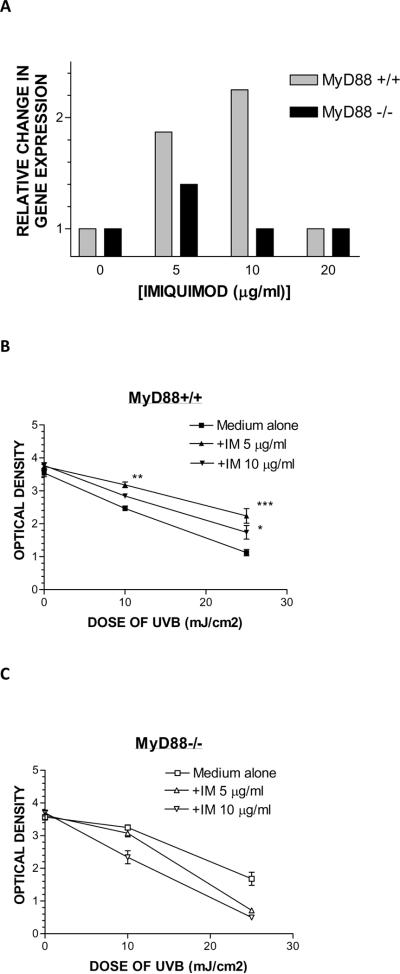
All of the TLR receptors, including TLR7 and 8, utilize MyD88 as an adaptor protein to initiate early events that eventually result in NFkB signaling in the nucleus, which reprograms cells to express inflammatory cytokine genes (29–31). Bone marrow derived cells from MyD88 gene targeted mice exhibit impaired inflammatory responses after exposure to TLR ligands (3). Thus, if imiquimod induction of the DNA repair gene XPA is indeed dependent on TLR7 signaling, then cells deficient in MyD88 would exhibit impaired ability to up-regulate XPA gene expression after stimulation by imiquimod. Macrophage cell lines from wild type mice (MyD88 +/+) and MyD88 knockout mice (MyD88−/−) were exposed to medium alone, or medium containing imiquimod, for four hours and XPA gene expression was assayed. Whereas macrophages from wild type mice (MyD88+/+) responded by increasing XPA gene expression at both 5 and 10 μg/ml, the macrophages from MyD88–/– knockout mice exhibited a blunted to respond to 5 μg/ml, and an absent response to the 10 μg/ml dose, which induced optimal gene expression in macrophages from MyD88+/+ mice (Figure 2A).
Figure 2. MyD88 expression is necessary for the enhanced XPA gene expression and survival after exposure to UVL in bone marrow derived cells.
(A) Macrophage cell lines derived from MyD88+/+ (wild type) mice or MyD88−/− (gene targeted) mice were incubated with medium alone, or medium containing the indicated doses of imiquimod, and XPA gene expression was assayed 6 hours later. (B) Bone marrow derived cells from MyD88+/+ (wild type) mice were incubated with the indicated doses of imiquimod for 24 hours, and then exposed to increasing doses of UVL, and survival was measured after another 24 hours using an MTT assay (see methods). (C) Bone marrow derived cells from MyD88−/− (gene targeted) mice were incubated with the indicated doses of imiquimod for 24 hours, and then exposed to increasing doses of UVL, and survival was measured after another 24 hours using an MTT assay (see methods). (data depicted represent the mean +/− SD of six replicates from a single representative experiment that was repeated three times; * p < 0.05; ** p < 0.01; ***p < 0.001, ANOVA)
After exposure to UVL, an irradiated cell will sense DNA damage, and can go on to repair the DNA damage, and survive. Alternatively, if the DNA damage is too severe, an irradiated cell will then undergo apoptosis (32, 33). We hypothesized that if DNA repair induced by TLR7 was functionally significant, there would be enhanced survival after exposures to increasing doses of UVL. As shown in Figure 2B, treatment of MyD88+/+ macrophages enhanced the survival of these cells (MTT assay) compared to control (medium alone) cells. In contrast, MyD88−/− macrophages did not respond to imiquimod with enhanced survival to UVL (MTT assay) (Figure 2C). Other cell lines such as P388 also exhibited imiquimod-induced enhanced survival after UVB exposure (data not show).
A late event in the TLR signaling pathway is translocation of the transcription factor NF-kB from the cytoplasm to the nucleus of activated cells (28–30). Under steady-state conditions, NFkB proteins are sequestered in the cytoplasm by members of the IkB family. Upon cellular stimulation by TLR agonists, activation of the IkB kinase phosphorylates IkB, which dissociates the NF-kB-IkB complexes. Free NFkB heterodimers then translocate into the nucleus, where they bind to enhancer elements of target genes (24). The chemical compound BAY 11-7085 inhibits the NF-kB signaling pathway by preventing the degradation of IkB (24), and hence prevents the translocation of NF-kB from the cytoplasm to the nucleus, thus blocking the activation of its target genes. If the induction of XPA gene expression is dependent on classical TLR signaling, we hypothesized that Bayer compound would block the up-regulation of XPA gene expression after TLR7 stimulation by imiquimod. Consistent with our hypothesis, BAY 11-7085 blocked the increase in XPA gene expression in P388 cell line (Figure 3A). Similarly, BAY 11-7085 blocked the imiquimod-induced enhanced nuclear localization of NF-kB and XPA protein (western blotting of nuclear extracts, Figure 3B). Additionally, BAY 11-7085 blocked the ability of imiquimod to enhance survival of P388 after exposure to UVL (Figure 3C). Thus, the up-regulation of XPA gene expression is dependent upon both early (MyD88 dependent, Figure 2A) and late events (nuclear activation of NFkB, Figure 3A, 3B).
Figure 3. NF-kB inhibition blocks the ability of imiquimod to enhance XPA gene expression as well as enhancement of survival after UVL exposure.
(A) P388 cells were pulse incubated with medium alone, medium containing DMSO vehicle or medium with BAY 11-7085 at the indicated dose for 30 minutes. After washing, the cells were then incubated with the indicated dose of imiquimod for 4 hours, and then gene expression was measured using qPCR. (B) The same experiment was repeated as in (A), except that the cells were incubated with imiquimod for 48 hours; then the cells were lysed, nuclei were isolated, and western blot performed (see methods). (C) Densitometry scanning of western blot depicted in (B). (D) The same experiment as in (A) except that P388 were incubated with the indicated dose of imiquimod for 24 hours, then exposed to the indicated doses of UVL, and survival was measured after another 24 hours using an MTT assay (see methods). (data depicted represent the mean +/− SD; **p < 0.01, ANOVA).
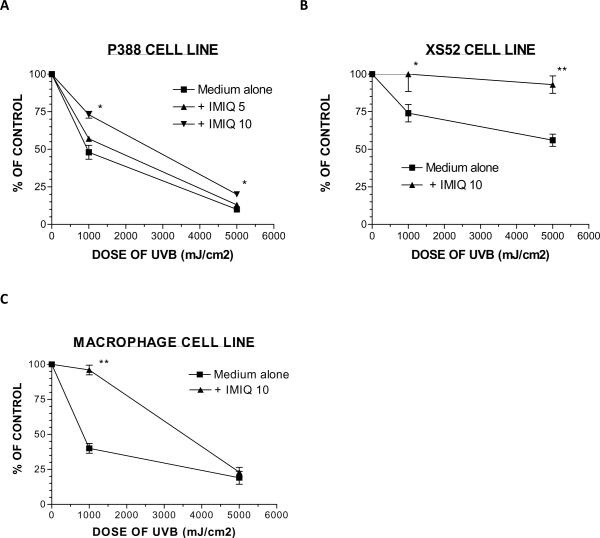
Imiquimod stimulation of bone marrow derived cells enhances functional DNA repair in a gene reactivation assay and the resolution of CBPD
Next, to determine whether imiquimod stimulation of bone marrow derived cells enhanced DNA repair, we utilized a functional assay (known as the gene reactivation assay) to study this phenomenon (34, 35). In this assay, a firefly luciferase encoding plasmid is UVL irradiated, and then co-transfected (along with an un-irradiated renila luciferase encoding plasmid to control for transfection efficiency) into a host cell. Visible light emission (luciferase functional activity) was studied over time (luminometer, see methods). The P388 cell line was pre-treated with medium alone, or medium containing imiquimod 5 or 10 μg/ml for twenty four hours, then transfected with control (un-irradiated) or UVL irradiated luciferase constructions. Forty eight hours after transfection, a lysate was prepared, and visible light was measured. As is depicted in Figure 4A, 10 μg/ml of imiquimod significantly enhanced the repair of the irradiated constructs. Higher doses of imiquimod did not further enhance repair (data not shown). Although the lower dose of imiquimod enhanced the repair relative to the untreated host cells, this was not statistically significant. We studied two other cell lines (XS52 and macrophage cell line) for responsiveness to imiquimod in the gene reactivation assay, and found that both responded similarly to 10 μg/ml of this TLR7 agonist (Figures 4B and 4C). We conclude that pre-treatment of bone marrow derived cells with imiquimod enhances the repair (and hence gene expression) above that of background levels of exogenously irradiated plasmid DNA that is introduced into three different host cells using electroporation method.
Figure 4. Imiquimod enhances functional DNA repair activity in bone marrow derived cells as measured in a gene reactivation assay.
A firefly luciferase pGL4.1[luc2] containing construct was either unirradiated (positive control), or irradiated with the indicated doses of UVL, and electroporated into either (A) P388 cells; (B) XS52 cells; (C) Bone marrow derived cells from MyD88+/+ mice. These host cells had been incubated with medium alone, or medium containing the indicated doses of imiquimod. Forty eight hours after transfection, a lysate was prepared, and luciferase activity was measured using luminometry and a reference luciferase to normalize for transfection efficiency (pGL4.70[hRluc], renila luciferase). Data are expressed as a % of control (% of expression of the irradiated luciferase to that of the unirradiated luciferase construct). See methods for the formula utilized to calculate percent gene reactivation. (data depicted represent mean +/− SD; * p < 0.05; ** p < 0.01, ANOVA).
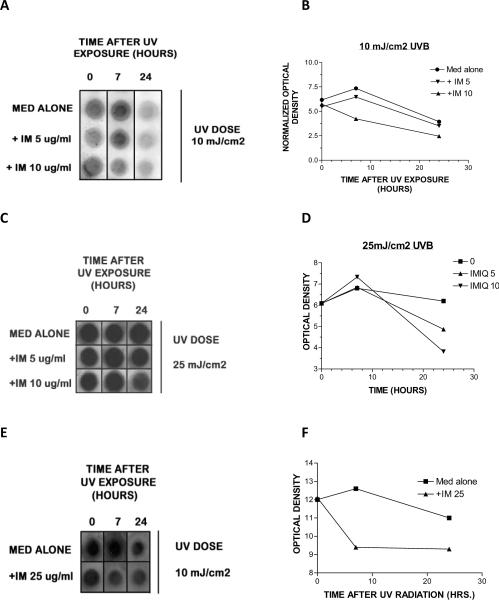
In another functional assay of DNA repair that is more relevant to in vivo exposures, we first treated bone marrow derived cells with medium alone, or medium containing imiquimod at the indicated doses, and then exposed the bone marrow-derived cells to UVL at doses of 10 or 25 mJ/cm2. The resolution of DNA damage was followed over time utilizing a DNA dot blot, in which genomic DNA was extracted from cells, blotted onto nylon membranes, and then probed with a monoclonal antibody that reacts with CBPD (14). P388 cells stimulated with 10μg/ml of imiquimod had noticeably less DNA damage seven hours after a single exposure to 10mJ/cm2 of UVB compared to P388 treated with medium alone or lower doses of imiquimod (Figures 5A and B). With higher doses of UVB (25mJ/cm2), there was a delay in the accelerated resolution of damage to 24 hours that occurred in P388 cells stimulated with imiquimod 10 μg/ml when compared to either the control P388 cells, or P388 cells stimulated with lower doses of imiquimod (5μg/ml) (Figures 5C and D). XS52 cells were also treated with imiquimod prior to 10mJ/cm2 of UVB, and then studied for the resolution of CBPD over time. Similar to P388, XS52 more rapidly resolved CBPD (by seven hours) compared to control cells (Figures 5E and F).
Figure 5. Imiquimod enhances functional DNA repair activity in bone marrow derived cells as measured in a DNA dot-blot assay.
P388 cells (A–D) or XS52 cells (E–F) were pre-treated with medium, or medium containing the indicated dose of imiquimod for twenty-four hours, and then irradiated with the 10 mJ/cm2 (A–B, E,F) or 25 mJ/cm2 (C,D) of UVB. After another twenty-four hours, DNA was extracted, denatured, and crosslinked onto a nylon membrane, and probed with a cyclobutane pyrimidine dimer specific monoclonal antibody. Antibody binding to the DNA was detected using a secondary antibody and chemiluminescence (See methods). DNA dot blots (A,C,E); densitometry scanning of DNA dot blots depicted as a line point graph (B,D,F).
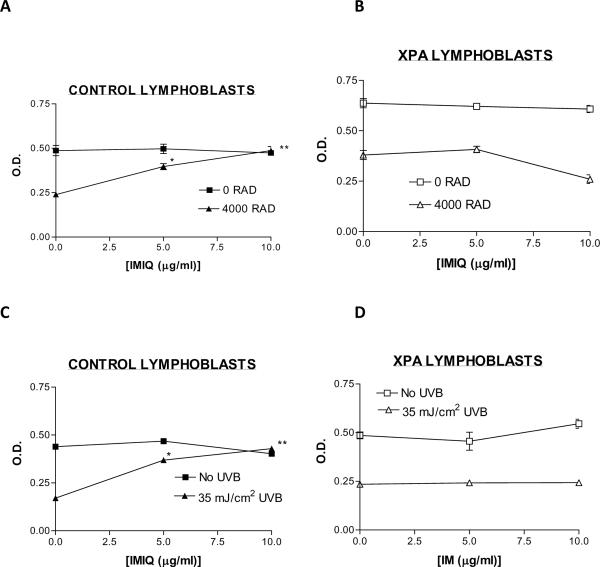
Imiquimod induced resistance to ionizing or UV radiation is dependent on intact DNA repair activity
To determine whether TLR7 activation by imiquimod enhanced the survival of human cells after ionizing radiation, we exposed EBV immortalized lymphoblasts (from a healthy individual or from a xeroderma pigmentosum patient [XPA gene defect]) to 4000 RAD from a 137Cs irradiator. Treatment of control EBV lymphoblasts with imiquimod (5 or 10 μg/ml) prior to exposure to ionizing radiation significantly (p <0.05, ANOVA) enhanced cell survival 24 hours later (MTT assay, see methods) (Figure 6A). In contrast, exposure of XP lymphoblasts to imiquimod did not enhance cell survival 24 hours after exposure to the same amount of ionizing radiation (4000 RAD) (Figure 6B). Identical results were obtained with these two cell lines after exposure to a single dose of 35 mJ/cm2 of UVB. Whereas exposure of control lymphoblasts to either 5 or 10 μg/ml of imiquimod enhanced survival twenty-four hours after UVB (Figure 6C), XPA lymphoblasts did not respond to these same doses of imiquimod (Figure 6D). These data suggest that enhanced survival after ionizing or UVB irradiation induced by TLR7 signaling is dependent on intact DNA repair mechanisms. This is consistent with our hypothesis that TLR7 signaling enhances DNA repair.
Figure 6. Intact DNA repair is necessary for imiquimod enhancement of survival of immortalized lymphoblasts after exposure to ionizing or UV irradiation.
EBV immortalized lymphoblasts derived from a healthy individual with normal DNA repair (A,C), or a from a patient with XPA (B,D) were cultured with medium alone, or medium containing the indicated doses of imiquimod and then exposed to 4000RAD ionizing radiation (137Cs source)(A, B) or 35mJ/cm2 of UVB radiation (C,D). After 24 hours, cell survival was measured using an MTT assay (see methods) (data depicted represent mean +/− SD; **p<0.01, highly significant, ANOVA).
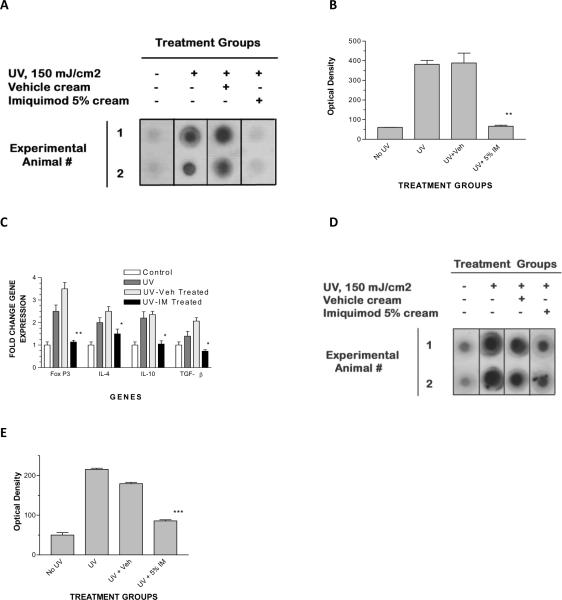
Imiquimod decreases UVL induced DNA damage in an in vivo model
After UVB irradiation of mouse skin, class II MHC positive, APC that bear CBPD can be detected within the local lymph nodes within hours after UVB exposure, and persist for days after a single UVB exposure (36, 37). These damaged APC are thought to be responsible for systemic immune suppression that occurs after UVB irradiation (11). Topical applications of imiquimod decreased the amount of CBPD bearing APC in local lymph nodes 24 hours after UVB exposure, as seen in a DNA dot blot derived from draining lymph nodes of UVB irradiated mice (Figure 7A), as well as reversed the presence of immunosuppressive cytokines (IL-10, TGF-β) as well as Tregulatory cell associated transcription factor, Fox P3 (9) (Figure 7C).
Figure 7. Topical applications of imiquimod cream decrease the amount of DNA damage found in local lymph nodes and immune suppressive cytokines after a single cutaneous UVL exposure.
Experimental animals were un-irradiated, or irradiated with a single dose of 150mJ/cm2 of UVB on the dorsal surface of the pinna of the ear. The UVL irradiated mice were either untreated, treated with topical applications of vehicle (placebo) cream or 5% imiquimod cream for two consecutive days prior to the UVL exposure. Twenty four hours after the single UVL exposure, the cervical lymph nodes were dissected from all four groups of animals and DNA was extracted as described in the methods. (A) DNA dot blot, showing decreased CBPD only in imiquimod treated mice compared to the UV irradiated, untreated or the vehicle treated groups of mice, but similar to the mice not exposed to UV. (B) Summary of densitometry scanning (data represent mean +/− SD of the two depicted animals; **p < 0.01, ANOVA). (C) qPCR analysis of immune suppressive gene expression (IL-4, IL-10, TGF-β and FoxP3) in local lymph nodes, using experimental protocol as described above. These data represent data from two animals from each experimental group (data depicted represent mean +/− SD; ** p<0.01, highly significant; * p <0.05 compared to vehicle control, significant, ANOVA); this experiment was repeated three times, and found to be reproducible. (D) DNA dot blot depicting CBPD from lymph nodes derived from IL-12 knockout mice (same protocol used for wild type mice as described above). (E) Summary of densitometry scanning (data represent mean +/− SD of the two depicted animals; ***p < 0.001, ANOVA).
Discussion
TLR are a major class of innate immune signaling receptors (38). These receptors, after sensing certain microbial products or damage-associated molecular patterns trigger an inflammatory response that is orchestrated by a family of cytokines such as IL-1, TNF-α and IL-6. In total, these inflammatory cytokines are pleiotropic and recruit inflammatory cells, enhance vascular permeability, regulate cell death, and induce the production of acute phase reactants (39, 40).
TLR 7, 8 and 9 are distinct members of the larger TLR family, and are clustered in a group of intracellular receptors that recognize intracellular viral and bacterial infections (41). Imiquimod is a small, synthetic adenosine analog that activates TLR 7 in mice and TLR7/8 in humans (42). It has been used therapeutically in the treatment of actinic keratosis, superficial basal cell carincoma, external genital warts and a variety of other skin conditions (43). As a topically applied anti-cancer compound, imiquimod is thought to have a number of mechanisms that are responsible for its ability to cause the clearance of pre-cancerous skin lesions (actinic keratoses) or fully developed non-melanoma skin cancer (superficial basal cell carcinoma). First, because of its adjuvant effects on TLR7/8 antigen presenting cells, this agent induces the maturation of such APC and the production of a number of cytokines that favor the development of Th1 lymphocytes during antigen presentation (17), which play an important role in anti-tumor responses. This has been confirmed at the tissue level, as histologic analysis of imiquimod treated non-melanoma skin cancers develop lymphocyte-rich (CD4, CD8-T-lymphocytes and NK-cells) infiltrates which are thought to be anti-tumor effector cells (44). Second, imiquimod induces a strong local inflammatory response in treated cancerous tissue (45), and cytokine production (such as TNF-α) which may be cytotoxic to tumor cells. Third, imiquimod has been demonstrated to promote the development of cytotoxic “killer” dendritic cells, which may also attack tumors (46). Lastly, imiquimod can induce mitochondrial-mediated cell apoptosis of proliferating tumor cells (i.e., transformed epithelial cells) directly through its interaction with nucleoside transition molecules (47).
The dominant focus of research on TLR signaling is related to its properties of generating “Danger signals” to the immune system (i.e., an inflammatory response), (38–41) as well as the ability of TLR-mediated signaling to shape adaptive immunity (i.e., T-lymphocyte memory). However, there is evidence that TLR signaling can play a role in tissue repair. MyD88 deficient mice were found to be more susceptible to radiation and dextran suflate sodium induced intestinal and colonic epithelial injury (48). Additionally, TLR 9 agonists enhance T-lymphocyte survival after exposure to ionizing radiation, which was dependent on MyD88 expression, involved ATM/ATR kinases, and the phosphorylation of the DNA repair enzymes, Chk1/2 (49). There was also evidence of enhanced DNA repair of ionizing radiation induced DNA damage, as detected by a comet assay. Thus, there is precedent that other TLR agonists enhance DNA repair.
Our previous studies with topical imiquimod in a mouse model of UVL-induced immune cutaneous immune suppression indicated that this TLR7 agonist protected mice from the loss of contact hypersensitivity, as well as the associated hapten-specific immune tolerance induced by UVL exposures (17). Our studies using the XS52 cell line (a LC-like APC line), suggested the TLR7 agonist imiquimod induced “UVL-resistant” XS52 maturation during T-cell interactions, as measured by the ability of this cell line to stimulate interferon-gamma secretion during antigen presentation, even after UVL exposure.
One possible explanation for this resistance to UVL immune suppression is the enhanced repair of UVL induced DNA damage, subsequent survival and preservation of immune competence. We demonstrate that imiquimod has direct effects on APC on XPA gene expression, as well as nuclear localization of XPA protein (Figure 1). This effect occurred rapidly (within 4–6 hours after exposure to imiquimod) suggesting that it is a primary effect, rather than a late secondary effect of cytokines triggered by imiquimod such as IL-12 (42). Our studies of important components of the TLR signaling pathway indicated that MyD88 was necessary for both the enhancement of the expression of the DNA repair gene, XPA (and possibly other DNA repair genes as well) (Figure 2A) as well as the enhanced cell survival after UVL exposure (Figure 2B).
All TLR receptors activate NF-kB through a canonical pathway involving MyD88, TRAF6, TAK1 and Ikk complex (37–40). Our studies using the pharmacologic compound BAY 11-7085 (inhibitor of the degradation of Ikk) indicates that this late component of the TLR pathway also directly regulates both XPA gene expression, as well as the enhanced survival of UVL-irradiated cells (Figures 3A–C). NF-kB is a central regulator of immune responses and inflammation, but it also targets genes related to cell survival and proliferation, such as cyclin D1, cyclin D2, c-Myc, c Myb, cycloxygenase 2 (COX2), BcL-2 and BcL-XL (50, 51, 52). Thus, the observation that imiquimod enhanced cell survival after exposure to either UVB or ionizing radiation (Figures 2, 3, 6) may in part be secondary to its broader effects of NF-kB signaling on cell survival gene expression. However, against this idea is the observation that imiquimod does not enhance the survival of lymphoblasts derived from an XPA patient after exposures to ionizing radiation or UVB. These data indicate that intact DNA repair mechanisms are necessary for imiquimod's effects on survival to agents that damage genomic DNA (in this case, ionizing radiation or UVB) (Figure 6).
Our data indicate that TLR7 signaling can enhance the XPA gene expression, and nuclear localization. XPA is involved in recognition of UVB damage, and is thought to be an important early component of nucleotide excision repair of UV-induced CBPD (27). Although nucleotide excision repair genes are constitutively expressed, there is evidence that they are inducible (52). Cytokines such as IL-12 and IL-18, natural products such as green tea polyphenols and DNA oligonucleotides all enhance nucleotide excision repair of UV damaged DNA (12–15, 54– 57). Imiquimod also induces the nucleotide excision repair gene XPA (and presumably other nucleotide excision repair genes) as well as promoting functional DNA repair (gene reactivation and DNA dot blot assays, Figures 4 and 5).
Our studies of the local (cervical) lymph nodes after UVB irradiation of the dorsal surface of the pinna of the ear demonstrate that imiquimod treatment prevents the appearance of APC bearing CBPD (Figure 7A and B), and prevents the expression of immunosuppressive genes (IL-4, IL-10, TGF-β and FoxP3) (Figure 7C) in the skin associated lymphoid tissue, preventing systemic immune suppression, and the loss of contact sensitization, as we had previously demonstrated (16). Although imiquimod induced less efficient resolution of UV-induced CBPD in the local lymph nodes of IL-12 knockout mice (Figures 7D and 7E) when compared to wild type mice (Figures 7A and 7B), there remained significant DNA repair in these gene targeted mice. These data indicate that there is TLR7 inducible DNA repair even in the absence of IL-12, suggesting that TLR7 signaling has direct effects on DNA repair.
In summary, the TLR7 agonist imiquimod enhances DNA excision repair of UVB induced CBPD. Thus, in addition to triggering inflammation and acting as an adjuvant, this topically applied anti-cancer agent also serves to protect the immune system against the deleterious effects of UVB by promoting the repair and subsequent survival of UVB damage by APC. These data also imply that imiquimod and its related analogues can be utilized as a therapy to prevent skin cancer by accelerating the repair of UV-induced DNA damage in cutaneous antigen presenting cells, thus preserving immune competence.
Acknowledgements
None
Grant Support: This study was supported by an unrestricted grant from Graceway Pharmaceuticals, Exton, PA
Abbreviations
- APC
antigen presenting cells
- CBPD
cyclobutane pyrimidine dimers
- qPCR
quantitative real time polymerase chain reaction
- UVL
ultraviolet light
- XP
Xeroderma pigmentosum
References
- 1).Beissert S, Schwarz T. Ultraviolet-induced immunosuppression: implications for photocarcinogenesis. Cancer Treatment & Research. 2009;146:109–21. doi: 10.1007/978-0-387-78574-5_10. [DOI] [PubMed] [Google Scholar]
- 2).Murphy GM. Ultraviolet light and immunosuppression. British Journal of Dermatology. 2009;161(Suppl. 3):90–95. doi: 10.1111/j.1365-2133.2009.09455.x. [DOI] [PubMed] [Google Scholar]
- 3).Ghoreishi M, Dutz JP. Tolerance induction by transcutaneous immunization through ultraviolet-irradiated skin is transferable through CD4+CD25+ T regulatory cells and is dependent on host derived IL-10. J Immunol 2006. 2006;176:2635–44. doi: 10.4049/jimmunol.176.4.2635. [DOI] [PubMed] [Google Scholar]
- 4).Rivas JM, SE Ullrich SE. Systemic suppression of delayed-type hypersensitivity by supernatants from UV-irradiated keratinocytes. An essential role for keratinocyte-derived IL-10. J Immunol. 1992;149:3865–71. [PubMed] [Google Scholar]
- 5).Schwarz A, Noordegraff M, Maeda A, Torii K, Clausen BE, Schwarz T. Langerhans cells are required for UVR-induced immunosuppression. J. Investig. Dermatol. 2010;130(5):1419–27. doi: 10.1038/jid.2009.429. [DOI] [PubMed] [Google Scholar]
- 6).Toichi E, McCormick TS, Cooper KD. Cell surface and cytokine phenotypes of skin immunocompetent cells involved in ultraviolet-induced immunosuppression. Methods. 2002;28(1):104–10. doi: 10.1016/s1046-2023(02)00202-5. [DOI] [PubMed] [Google Scholar]
- 7).Simon JC, Mosmann T, Edelbaum D, Schopf E, Bergstresser PR, PD Cruz PD., Jr. In vivo evidence that ultraviolet B-induced suppression of allergic contact sensitivity is associated with functional inactivation of Th1 cells. Photodermatology, Photoimmunology & Photomedicine. 1994;10(5):206–11. [PubMed] [Google Scholar]
- 8).Saijo S, Kodari E, Kripke ML, Strickland FM. UVB irradiation decreases the magnitude of the Th1 response to hapten but does not increase the Th2 response. Photodermatology, Photoimmunology & Photomedicine. 1996;12(4):145–53. doi: 10.1111/j.1600-0781.1996.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 9).Maeda A, Beissert S, Schwarz T, Schwarz A. Phenotypic and functional characterization of ultraviolet radiation-induced regulatory T cells. Journal of Immunology. 2008;180(5):3065–71. doi: 10.4049/jimmunol.180.5.3065. [DOI] [PubMed] [Google Scholar]
- 10).Sontag Y, Cees LH, Guikers AA. Cells with UV-specific DNA damage are present in murine lymph nodes after in vivo UV irradiation. J. Investig. Dermatol. 1995;104:734–8. doi: 10.1111/1523-1747.ep12606971. [DOI] [PubMed] [Google Scholar]
- 11).Fisher MS, Kripke ML. Systemic alteration induced in mice by ultraviolet light irradiation and its relationship to ultraviolet carcinogenesis. Proc Natl Acad Sci USA. 1977;74:1688–92. doi: 10.1073/pnas.74.4.1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Yarosh D, Klein J, A O'Connor A. Effect of topically applied T4 endonuclease V in liposomes on skin cancer in xeroderma pigmentosum: a randomised study. Xeroderma Pigmentosum Study Group. Lancet 2001. 2001;357:926–9. doi: 10.1016/s0140-6736(00)04214-8. [DOI] [PubMed] [Google Scholar]
- 13).Schwarz A, Maeda A, Ganz D, Mammone T, Matsui MS, Schwarz T. Green Tea Phenol Extracts Reduce UVB-induced DNA Damage in Human Cells via Interleukin-12. Photochemistry and Photobiology. 2008;84:350–355. doi: 10.1111/j.1751-1097.2007.00265.x. [DOI] [PubMed] [Google Scholar]
- 14).Schwarz A, Ständer S, Berneburg M. Interleukin-12 suppresses ultraviolet radiation-induced apoptosis by inducing DNA repair. Nature Cell Biol. 2002;4:26–31. doi: 10.1038/ncb717. [DOI] [PubMed] [Google Scholar]
- 15).Majewski S, Jantschitsch C, Maeda A, Schwarz T, Schwarz A. IL-23 antagonizes UVR-induced immunosuppression through two mechanisms: Reduction of UVR-induced DNA damage and Inhibition of UVR-Induced Regulatory T-cells. J. Investig. Dermatol. 2010;130:554–62. doi: 10.1038/jid.2009.274. [DOI] [PubMed] [Google Scholar]
- 16).Sreevidya CS, Fukunaga A, Khaskhely NM, Masaki T, Ono R, Nishigori C, Ullrich SE. Agents that reverse UV-induced immune suppression and photocarcinogenesis affect DNA repair. J. Investig. Dermatol. 2010;130:1428–37. doi: 10.1038/jid.2009.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Thatcher TH, Luzina I, Fishelevich R, Gaspari AA. Topical Imiquimod Treatment Prevents Ultraviolet-light induced loss of Contact Hypersensitivity and Immune Tolerance. J. Investig. Dermatol. 2006;126:821–31. doi: 10.1038/sj.jid.5700167. 2006. [DOI] [PubMed] [Google Scholar]
- 18).Toews GB, Bergstresser PR, Streilein JW. Epidermal Langerhans cell density determines whether contact hypersensitivity or unresponsiveness follows skin painting with DNFB. J. Immunol. 1980;124:445–453. [PubMed] [Google Scholar]
- 19).Elmets CA, Bergstresser PR, Tigelaar RE, Wood PJ, Streilein JW. Analysis of the mechanism of unresponsiveness produced by haptens painted on skin exposed to low dose ultraviolet-radiation. J. Exp. Med. 1983;158:781–94. doi: 10.1084/jem.158.3.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Magram J, Connaughton SE, Warrier RR, Carvajal DM, Wu CY, Ferrante J, Stewart C, Sarmiento U, Faherty DA, Gately MK. IL-12-deficient mice are defective in IFN gamma production and type 1 cytokine responses. Immunity. 1996;4(5):471–81. doi: 10.1016/s1074-7613(00)80413-6. [DOI] [PubMed] [Google Scholar]
- 21).Elliott J, Coulter-Mackie EJ, Jung MB, Rodenhiser DI, Singh SM. A method for transforming lymphocytes from very small blood volumes suitable for pediatric samples. Human Genetics. 1991;86(6):615–6. doi: 10.1007/BF00201551. [DOI] [PubMed] [Google Scholar]
- 22).Heo DS, Park J-G, Hata K, Day R, Herberman RB, TL Whiteside TL. Evaluation of Tetrazolium-based Semiautomatic Colorimetrie Assay for Measurement of Human Antitumor Cytotoxicity. Cancer Res. 1990;50:3681–3690. [PubMed] [Google Scholar]
- 23).Sikder H, Zhao Y, Balato A, Chapoval A, Fishelevich R, Gade P, Singh IS, Kalvakolanu DV, Johnson PF, Gaspari AA. A central role for transcription factor C/EBP-β in regulating CD1d gene expression in human keratinocytes. J. Immunol. 2009;183:1657–1666. doi: 10.4049/jimmunol.0900057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Ade N, Antonios D, Kerdine-Romer S, Boisleve F, Rousset F, M Pallardy M. NF-kB Plays a Major Role in the Maturation of Human Dendritic Cells Induced by NiSO4 but not by DNCB. Tox. Sci. 2007;99(2):488–501. doi: 10.1093/toxsci/kfm178. [DOI] [PubMed] [Google Scholar]
- 25).Zhao Y, Fishelevich R, Petrali JP, Zheng L, Anatolievna MA, Deng A, Eckert RL, Gaspari AA. Activation of keratinocyte protein kinase c-zeta in psoriasis plaques. J.Investig. Dermatol. 2008;128:2190–7. doi: 10.1038/jid.2008.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Fishelevich R, Malanina A, Luzina I, Atamas S, Smyth MJ, SA Porcelli SA, Gaspari AA. Ceramide-Dependent Regulation of Human Epidermal Keratinocyte CD1d Expression During Terminal Differentiation. J. Immunol. 2006;176:2590–99. doi: 10.4049/jimmunol.176.4.2590. 2006. [DOI] [PubMed] [Google Scholar]
- 27).Moriwaki S-I, KH Kraemer KH. Xeroderma pigmentosum – bridging a gap between clinic and laboratory. Photodermatol Photoimmunol Photomed. 2001;17:47–54. doi: 10.1034/j.1600-0781.2001.017002047.x. [DOI] [PubMed] [Google Scholar]
- 28).Gordon KB, Gorski KS, Gibson SJ. Synthetic TLR agonists reveal functional differences between human TLR 7 and TLR 8. J. Immunol. 2005;174:1259–1268. doi: 10.4049/jimmunol.174.3.1259. [DOI] [PubMed] [Google Scholar]
- 29).Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–81. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 30).Kawai T, S Akira S. The role of pattern recognition receptors in innate immunity: update on TLR. Nat. Immunol. 2010;11(5):373–84. doi: 10.1038/ni.1863. [DOI] [PubMed] [Google Scholar]
- 31).Blasius AL, Beutler B. Intracellular TLR. Immunity. 2010;32:305–15. doi: 10.1016/j.immuni.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 32).Ziegler A. Sunburn and p53 in the onset of skin cancer. Nature. 1994;372:773–76. doi: 10.1038/372773a0. [DOI] [PubMed] [Google Scholar]
- 33).Brash DE, Ziegler A, AS Jonason AS. Sunlight and sunburn in human skin cancer: p53, apoptosis, and tumor promotion. J. Investig. Dermatol. Symp. Proc. 1996;1:136–42. [PubMed] [Google Scholar]
- 34).Carreau M, Eveno E, Quilliet X. Development of a new easy complementation assay for DNA repair deficient human syndromes using cloned repair genes. Carcinogenesis. 1995;16:1003–1009. doi: 10.1093/carcin/16.5.1003. [DOI] [PubMed] [Google Scholar]
- 35).Khan SG, Levy HL, R Legerski R. Xeroderma pigmentosum group C splice mutation associated with autism and hypoglycemia. J Invest Dermatol. 1998;111:791–796. doi: 10.1046/j.1523-1747.1998.00391.x. [DOI] [PubMed] [Google Scholar]
- 36).Kripke ML, Cox PA, Alas LG. Pyrimidine dimers in DNA initiate systemic immunosuppression in UV-irradiated mice. Proc. Natl. Acad. Sci. USA. 1992;89:7516–20. doi: 10.1073/pnas.89.16.7516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37).Sontag Y, Guikers CLH, Vink AA. Cells with UV-specific DNA damage are present in murine lymph nodes after in vivo UV irradiation. J. Investig Dermatol. 1995;104:734–8. doi: 10.1111/1523-1747.ep12606971. [DOI] [PubMed] [Google Scholar]
- 38).Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–20. doi: 10.1016/j.cell.2010.01.022. 2010. [DOI] [PubMed] [Google Scholar]
- 39).Akira S, Umematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2010;124:783–201. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 40).Beutler B, Jiang Z, Georgei P. Genetic analysis of host resistance: Toll-like receptor signaling and immunity at large. Annu. Rev. Immunol. 2006;24:353–389. doi: 10.1146/annurev.immunol.24.021605.090552. [DOI] [PubMed] [Google Scholar]
- 41).Blasius AL, Beutler B. Intracellular Toll-like receptors (review) Immunity. 2010;32:305–315. doi: 10.1016/j.immuni.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 42).Larange A, Antonios D, Pallardy M. TLR7 and TLR8 agonists trigger different signaling pathways for human dendritic cell maturation. J. Leukoc. Biol. 2009;85:673–83. doi: 10.1189/jlb.0808504. [DOI] [PubMed] [Google Scholar]
- 43).Gaspari AA, Tyring SK, Rosen T. Beyond a Decade of 5% Imiquimod Topical Therapy. Journal of Drugs in Dermatology. 2009;8(5):467–474. Review. [PubMed] [Google Scholar]
- 44).Sullivan TP, Dearaujo T, Vincek V, Berman B. Evaluation of superficial basal cell carcinomas after treatment with imiquimod 5% cream or vehicle for apoptosis and lymphocyte phenotyping. Dermatol Surg. 2003;29:1181–1186. doi: 10.1111/j.1524-4725.2003.29399.x. [DOI] [PubMed] [Google Scholar]
- 45).Hurwitz DJ, Pincus L, Kupper TS. Imiquimod: a topically applied link between innate and acquired immunity. Arch Dermatol. 2003;139:1347–1350. doi: 10.1001/archderm.139.10.1347. [DOI] [PubMed] [Google Scholar]
- 46).Stary G, Bangert C, Tauber M, Strohal R, Kopp T, G Stingl G. Tumoricidal activity of TLR7/8-activated inflammatory dendritic cells. J Exp Med. 2007;204:1441–1451. doi: 10.1084/jem.20070021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47).Schon MP, Schon M. Immune modulation and apoptosis induction. Two sides of the antitumoral activity of imiquimod. Apoptosis. 2004;9:291–8. doi: 10.1023/b:appt.0000025805.55340.c3. [DOI] [PubMed] [Google Scholar]
- 48).Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S. Recognition of commensal microflora by TLR is required for intestinal homeostasis. Cell. 2004;118:229–41. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 49).Zheng L, Asprodites N, Keene AH. TLR9 engagement on CD4 T lymphocytes represses g-radiation-induced apoptosis through activation of checkpoint kinase response elements. Blood. 2008;111:2704–13. doi: 10.1182/blood-2007-07-104141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50).Li X, Jiang S, Tapping RI. TLR receptor signaling in cell proliferation and survival. Cytokine. 2010;49:1–9. doi: 10.1016/j.cyto.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Clement JF, Meloche S, Servant MJ. The IKK-related kinases: from innate immunity to oncogenesis. Cell Res. 2008;18:889–99. doi: 10.1038/cr.2008.273. [DOI] [PubMed] [Google Scholar]
- 52).Vallabhapurapu S, M Karin M. Regulation and function of NF-kappaB transcription factors in the immune system. Annu. Rev. Immunol. 2009;27:693–733. doi: 10.1146/annurev.immunol.021908.132641. [DOI] [PubMed] [Google Scholar]
- 53).Schwarz T, Schwarz A. DNA repair and cytokine responses. J.Investig. Dermatol. 2008;14:63–66. doi: 10.1038/jidsymp.2009.3. [DOI] [PubMed] [Google Scholar]
- 54).Arad S, Konnikov N, Goukassian DA. T-oligos augment UVR-induced protective responses in human skin. FASEB J. 2006;20:1895–7. doi: 10.1096/fj.06-5964fje. [DOI] [PubMed] [Google Scholar]
- 55).Goukassian DA, Helms H, van Steeg H. Topical DNA oligonucleotide therapy reduces UV-induced mutations and photocarcinogenesis in hairless mice. Proc. Natl. Acad. Sci. USA. 2001;101:3933–8. doi: 10.1073/pnas.0306389101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56).Katiyar SK, Elmets CA, Agarwal R. Protection against UVB induced local and systemic suppression of contact hypersensitivity and edema responses in C3H/HeN mice by green tea polyphenols. Photochem. Photobiol. 1995;62:855–61. doi: 10.1111/j.1751-1097.1995.tb09147.x. [DOI] [PubMed] [Google Scholar]
- 57).Meeran SM, Mantena SK, Katiyar SK. Prevention of UV radiation-induced immunosuppression by epigallocatechin-3-galleate in mice is mediated through IL-12 dependent DNA-repair. Cancer Res. 2006;66:5512–20. [Google Scholar]