Abstract
Objectives
The purpose of this study was to explore the extent to which individuals with back pain or other health conditions, and individuals with no health problems, report having a usual source of care (USC) for their health care needs.
Methods
This study evaluated longitudinal Medical Expenditures Panel Survey data (MEPS data pooled for survey calendar years 2000-through-2006). Comparisons were made between adult MEPS respondents identified as having a back pain condition (n=10,194) compared to those without back pain but with other health condition (n=45,541), and those with no back pain and no other condition (n=5,497).
Results
Compared to individuals with no health problems, those with back pain were almost 8 times more likely (OR=7.8, p<.001) to report having a USC; and those with other health problems besides back pain were 5 times more likely (OR=5.4, p<.001). For those with a USC, individuals with back pain, and those with other problems but not back pain, were both about one and a half times more likely than those without any health problems to report a specific provider type as their USC (p<.001).
Conclusion
Study findings suggest that relatively healthy adults without back pain are less likely to have a USC than those with back pain or other health problems.
Keywords: Back Pain, Spine, Chiropractic
INTRODUCTION
Per Congressional mandate, the US Agency for Healthcare Research and Quality (AHRQ) produces reports to the Nation about the quality of health care, and access to health care.1 The AHRQ National Healthcare Quality Report and National Healthcare Disparities Report document national trends in the effectiveness of care, patient safety, timeliness of care, patient centeredness, and efficiency of care.
The AHRQ National Healthcare Disparities Report measures trends in access to care among priority populations such as residents of rural areas, women, children, older adults, individuals with disabilities or special health care needs, and racial, ethnic, or income groups.2,3,4 Toward development of the current and future reports on healthcare disparities, policy and research working groups have vetted various data sources and methods for measuring access to care.2 The AHRQ-sponsored Medical Expenditures Panel Survey (MEPS) data is a key source for data on access to care, and other sources include data from Centers for Disease Control and Prevention (CDC), Centers for Medicare and Medicaid Services (CMS), Indian Health Service (IHS), National Committee for Quality Assurance (NCQA), National Institutes of Health (NIH), and the US Census Bureau.3 As synthesized by the multiple AHRQ working groups, an individual's access to care may be measured along a number of dimensions, such as their ability to gain initial entry into the health care system (e.g. health insurance coverage, having a usual source of care (USC), or patient perceptions of need); their ability to get needed care within the system (e.g. wait times, or obtaining referrals); patient perceptions of their care (e.g. patient-provider communication and relationship, cultural competency, health information); and their pattern of utilizing various services (e.g. general and specialty care, ambulatory care, emergency and urgent care, or avoidable admissions to hospital and inpatient care).4
Access to care as a function of an individual's having a USC, has been described using data from the AHRQ-sponsored Medical Expenditures Panel Survey (MEPS)5,6,7,8,9, National Health Interview Survey (NHIS)10,11, National Health and Nutrition Examination Survey (NHANES)12, Community Tracking Study (CTS),13 regional or local area surveys,14 or targeted surveys (e.g. using a consumer mailing list of the National Multiple Sclerosis Society)15
This study analyzes data from the Medical Expenditures Panel Survey (MEPS) to explore the extent to which individuals with back pain or other health conditions, and individuals with no health problems, report having a USC for their health care needs.
METHODS
Adult MEPS respondents (N=61,323) were identified in the 2-year longitudinal MEPS Panels 5-through-10 (MEPS survey calendar years 2000-through-2006) as reported in a previously published study.16 MEPS respondents with back pain were defined based on two condition coding classification schemes that are available in the MEPS medical conditions datafile,17 the Clinical Classification Category (CCC)18 codes and the International Classification of Diseases (ICD) codes (encompassing 66 ICD codes of acute, chronic, or recurrent episodic back pain conditions, such as spondylosis and intervertebral disc disorders, sacroiliac sprain/strain, other back sprain/strain). Each of the 61,232 adult MEPS respondents were assigned to one of three “condition groups” for this study: (a) Individuals identified as having a back pain condition (n= 10,194); (b) Individuals who did not report back pain, but did report having some other health condition (n=45,541); and (c) Individuals who reported no health condition (no back pain and no other condition) during the 2-year MEPS longitudinal panel survey (n=5,497).
MEPS participants are surveyed on whether they have a USC, and if so the type of health care provider, their satisfaction with the USC provider's care, and any problems with accessing the USC provider. During the MEPS field interviews, USC is defined for participants as “…a particular doctor's office, clinic, or other place that the individual usually goes to if they are sick or need advice about their health…”; followed by a set of MEPS interview questions about that USC provider: “Is provider a medical doctor?”; “Is provider a nurse, nurse practitioner, physician's assistant, midwife, or some other kind of person?”; “What is provider's specialty?”.
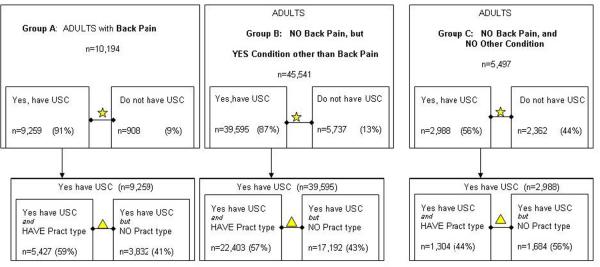
For this study, USC is operationalized using the three MEPS survey variables: “Does person have a USC”; If yes, “Does person have a specific USC provider type”; If yes, “What type of provider”. Of the 51,842 MEPS respondents who reported having a USC, 56% (n=29,134) listed a specific USC provider type (see Figure1).
Figure 1.
Two-Stage Hypothesis Testing of USC for Back Pain: Sample sizes, Hypothesis tests, and Results.
Two hypotheses were tested in this study (Figure1), comparing the three condition groups of: (a) Individuals with back pain; (b) Individuals without back pain but with some other health condition; and (c) Individuals with no condition. The null hypotheses were no significant differences between the three groups.
The first hypothesis test compared the three condition groups as to their reporting that they have a USC, operationalized as an affirmative response code for the MEPS variable “Does person have a USC”.
The second hypothesis test examined only those respondents who did report having a USC, and compared the 3 groups as to whether they report a specific “Provider Type” as their USC.
The two hypotheses were tested using Bivariate Chi-square tests and Binomial Logistic regression modeling. MEPS employs a complex sample design and oversamples certain population groups of interest, therefore longitudinal sampling weights and longitudinal adjusted variance estimators (strata, PSU) were applied during the inferential hypothesis testing to account for the MEPS sampling frame and complex survey design features. All data management and statistical analyses (unweighted and weighted, descriptive and inferential) were performed using SPSS for Windows versions 17.0 and 12.0 (SPSS Inc, Chicago, IL).
RESULTS
The three condition groups differed significantly on having a USC (Figure1). Compared to individuals with no health problems, those with back pain were almost 8 times more likely (OR=7.8, p<.001) to report having a USC; and those with other health problems besides back pain were 5 times more likely (OR=5.4, p<.001). Comparing only the two groups with health problems, those with back pain were significantly more likely to have a USC than those with other health problems but not back pain (OR=1.5, p<.001).
For those who reported having a USC (n=51,842), individuals with back pain, and those with other problems but not back pain, were both about one and a half times more likely than those without any health problems to report a specific provider type as their USC (p<.001).
The specific categories and categorical assignment of provider types has evolved over successive administrations of the MEPS survey (see Appendix 1), necessitating a panel-by-panel approach to describing the specific provider types that are identified by MEPS respondents as their USC. The USC provider types from MEPS Panels 10, 9, and 8, are presented in Table 1, for each of the three condition groups.
Table 1.
Provider Types* specified by Adult MEPS Respondents as their Usual Source of Care, for the three groups: Individuals with Back Pain, Individuals reporting Other Condition but not Back Pain, and Individuals reporting No Condition during the MEPS 2-year longitudinal data collection timeframe (MEPS Panels 10, 9, 8).
| Back Pain | Other Condition not Back Pain | No Condition | |
|---|---|---|---|
| MEPS Panel 10 | (n=856) | (n=3,341) | (n = 184) |
| MD-GP / FP / Internist | MD-GP / FP / Internist | MD-GP / FP / Internist | |
| MD-OB/Gyn | MD-OB/Gyn | MD-OB/Gyn | |
| MD-Cardiologist | MD-Cardiologist | ||
| DO-Osteopath | DO-Osteopath | ||
| MD-Geriatrician | MD-Geriatrician | ||
| MD (Other Specialist) | MD (Other Specialist) | MD (Other Specialist) | |
| Nurse/Nurse Practitioner | Nurse/Nurse Practitioner | Nurse/Nurse Practitioner | |
| Physician Assistant (PA) | Physician Assistant (PA) | ||
| DC-Chiropractor | DC-Chiropractor | ||
| MEPS Panel 9 | (n=951) | (n=3,415) | (n=203) |
| MD-GP / FP / Internist | MD-GP / FP / Internist | MD-GP / FP / Internist | |
| MD-OB/Gyn | MD-OB/Gyn | MD-OB/Gyn | |
| MD-Cardiologist | MD-Cardiologist | ||
| DO-Osteopath | DO-Osteopath | DO-Osteopath | |
| MD-Geriatrician | MD-Geriatrician | ||
| MD (Other Specialist) | MD (Other Specialist) | MD (Other Specialist) | |
| Nurse/Nurse Practitioner | Nurse/Nurse Practitioner | ||
| Physician Assistant (PA) | Physician Assistant (PA) | Physician Assistant (PA) | |
| DC-Chiropractor | DC-Chiropractor | ||
| MEPS Panel 8 | (n=907) | (n=3,705) | (n=227) |
| MD-GP / FP / Internist | MD-GP / FP / Internist | MD-GP / FP / Internist | |
| MD-OB/Gyn | MD-OB/Gyn | MD-OB/Gyn | |
| MD-Cardiologist | MD-Cardiologist | MD-Cardiologist | |
| DO-Osteopath | DO-Osteopath | ||
| MD-Geriatrician | |||
| MD (Other Specialist) | MD (Other Specialist) | MD (Other Specialist) | |
| Nurse/Nurse Practitioner | Nurse/Nurse Practitioner | Nurse/Nurse Practitioner | |
| Physician Assistant (PA) | Physician Assistant (PA) | ||
| DC-Chiropractor | DC-Chiropractor |
note: For cogency of data presentation, the following MD Specialist types are infrequently identified as USC Provider Type and are grouped within “MD (Other Specialist)” category in this table: Neurologist, Endocrinologist, Gastroenterologist, Nephrologist, Oncologist, Pulmonologist, Rheumatologist, Psychiatrist, Surgery.
DISCUSSION
These findings suggest that relatively healthy adults, i.e. those who report no active health problems during the course of the MEPS 2-year longitudinal data collection timeframe, are also less likely to have a USC. This is consistent with other studies that have found that many adults may not have a USC simply because they choose not to, most probably because they do not perceive the need since they are relatively healthy.19,5,20 Interestingly, some individuals with no USC or who use the Emergency Department (ED) as their usual source when care is needed, may have lower overall costs than those who use MD generalists or MD specialists as their USC.9
The finding that back pain sufferers are significantly, and substantially, more likely to have a USC is also understandable, given that the nature of back pain may characteristically be a recurrent, episodic, or longterm chronic condition,16 for which individuals may use the services of spine care specialists on an ongoing basis. Paradoxically, the recurrent, episodic nature of back pain may also partly explain the finding that chiropractors are identified as a USC for adult MEPS respondents without back pain, in that these may be persons who utilize ongoing care to manage a sporadic recurring back problem, although they may not have experienced an active flare-up episode of their back pain during their 2-year MEPS data collection window. Minden, et al, found that individuals with multiple sclerosis (MS) who had experienced a past recent flare-up (one or two relapses in the preceding year) were more likely to identify a neurologist as their usual source of MS care in the current year, as compared to MS sufferers with no recent relapses.15 Another possible explanation is that some individuals may be using chiropractors as their USC for conditions other than back pain, or for other reasons altogether such as general wellness care.
A broad representation of provider types may be identified as a USC for individuals with back pain (Table1). Everett et al found that utilization of physician assistants and nurse practitioners (PA/NPs) as a USC was associated with chiropractor visits, which they reasoned may reflect a greater willingness of PA/NPs to recommend non-drug or CAM therapies for their patients.14 As suggested by this study, USC varies for individuals with back pain (Table1), and may include the use of physician assistants, nurse practitioners, chiropractors, or a broad range of other provider types, as their USC.
Identification of optimal arrangements for USC to ensure that patients receive both specialized and primary care services as appropriate to their needs, may vary by patient preference and may also vary by geographic location. For instance, since the dispersion of neurologists is not uniform across the US, then the appropriateness (or patient preference) for a “primary care” vs “principal care” model may vary as a function of geographic access to specialized neurological services, for persons with neurological disorders.15 In a “primary care model” generalists provide all primary care including referral to specialist. Within a “principal care model” some primary care services may be provided by specialists, such as neurologists, who also serve as an individual's USC. Variants on the “principal care model” theme includes the provision of primary care services by multidisciplinary teams that may be co-located (or coordinated if dispersed across the community) with such teams taking a patient-centered and family-centered approach and emphasizing wellness, maximal functioning, and ongoing integrated care.15
The distribution of generalist MD provider types also varies by geography and by location in Medicare Primary Care Service Areas (PCSAs). The geographic distribution of generalist MDs trained in family practice and general practice (FPs/GPs) more closely mirrors the distribution of the general population, with FPs/GPs tending to be located in areas of lowest Medicare reimbursements per beneficiary; whereas generalist MDs trained as internists tend to cluster toward areas with highest Medicare reimbursements (urban and northeast).9 The geographic distribution and use of chiropractors varies,22 and the use of outpatient physical therapy (PT) services for musculoskeletal conditions may also vary as a function of geographic access, with individuals in urban and northeast areas being more likely to use PT than those in other areas.21
Limitations and future studies
A serious limitation to using MEPS data, is that the structure and format of the MEPS only allows respondents to identify a single location or single provider type as their USC. This “single USC provider” logic of the MEPS would presume that all individuals surveyed by MEPS can, or should, fit neatly into a “primary care model” rather than a “principal care model” for their use of health services, despite the fact that a “principal care model” may actually be preferred by many individuals.15 It is quite possible, and perhaps likely, that MEPS respondents would identify more than one provider type as their USC if allowed to do so (i.e. reflecting a care-seeking behavior more along the lines of a “principal care” rather than “primary care” model).
A further limitation, or caution, to using MEPS data, is that certain provider types, such as chiropractors, may be systematically under-reported as USC in the MEPS. For instance, the MEPS survey queries have changed over time, therefore certain provider types cannot even be discerned in earlier iterations of MEPS data (chiropractors were not listed as a provider type for the USC queries prior to MEPS survey year 2002, see Appendix). Less apparent, though just as important, is that the MEPS methodology may inadvertently introduce recall bias as a function of the interviewer protocol prompts, again resulting in systematic under-reporting of certain provider types. MEPS constructs a composite variable for “Usual Source Provider Type” from the set of MEPS interview questions: “Is provider a medical doctor?”; “Is provider a nurse, nurse practitioner, physician's assistant, midwife, or some other kind of person?”; “What is provider's specialty?”. Provider types that are specifically prompted by MEPS interviewers (e.g. MDs, PAs, NPs) may be recalled more readily by MEPS survey participants as their USC, more so than other provider types that are not specifically elicited by the MEPS interviewer protocol (e.g. doctors of chiropractic, osteopaths are not specifically prompted as a response to the USC queries).
Much more research is needed to better understand the outcomes and costs associated with various USC utilization behaviors, including the possibility that shorter-term savings may be more than offset by longer-term costs and consequences associated with individual choices for their usual sources of care. Further research needs also to be directed toward better clarifying how individuals do, or should, use the Emergency Department (ED) as a community-based USC for their urgent vs non-urgent health care needs.6,10
CONCLUSION
The findings from this study suggest that adults with back pain are more likely to report having a USC than those with other health problems but not back pain. Relatively healthy adults are least likely to have a USC, than those with back pain or other health problems. More research is needed to identify optimal arrangements for USC to ensure that patients receive both specialized and primary care services as appropriate to their needs.
Practical applications.
Back pain sufferers are more likely to have a USC than those without back pain.
Given that the nature of back pain may characteristically be a recurrent, episodic, or longterm chronic condition, individuals may use the services of spine care specialists on an ongoing basis.
Health Care Providers identified as USC should coordinate the delivery of optimal health care, to ensure that patients receive both specialized and primary care services as appropriate to their needs.
Acknowledgments
FUNDING SOURCES This project was supported by Grant Number K01 AT002391, a grant from National Institutes for Health National Center for Complementary and Alternative Medicine.
State funding sources (grants, funding sources, equipment, and supplies). Include name and number of grant if available. Clearly state if study received direct NIH funding.
This project was supported by Grant Number K01 AT002391, a grant from National Institutes for Health National Center for Complementary and Alternative Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
List any present or potential conflict s of interest for all authors: none
CONFLICTS OF INTEREST No conflicts of interest were reported for this study.
BIBLIO/REFERENCES
- 1.Agency for Healthcare Research and Quality (AHRQ, Rockville, MD) 2009 National Healthcare Quality Report (NHQR), and 2009 National Healthcare Disparities Report (NHDR) http://www.ahrq.gov/qual/qrdr09.htm (downloaded July 15,2010)
- 2.Agency for Healthcare Research and Quality (AHRQ, Rockville, MD) National Healthcare Disparities Report: Background on the Measures Development Process. http://www.ahrq.gov/qual/nhdr02/nhdrprelim.htm (downloaded July 15,2010)
- 3.Agency for Healthcare Research and Quality (AHRQ, Rockville, MD) 2009 National Healthcare Quality and Disparities Reports: Data Sources Appendix. http://www.ahrq.gov/qual/qrdr09/datasources/ (downloaded July 15,2010)
- 4.Agency for Healthcare Research and Quality (AHRQ, Rockville, MD) National Healthcare Disparities Report: List of Measures. http://www.ahrq.gov/qual/nhdrmeasures/listmeasure.htm (downloaded July 15,2010)
- 5.Viera AJ, Pathman DE, Garrett JM. Adults' lack of a usual source of care: A matter of preference? Annals of Family Medicine. 2006 July/Aug;4(No4):359–365. doi: 10.1370/afm.557. 2006. doi: 10.1370/afm.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002 Sept;9(9):916–23. doi: 10.1111/j.1553-2712.2002.tb02193.x. 2002. [DOI] [PubMed] [Google Scholar]
- 7.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: Insurance status and usual source of care. Am J Public Health. 2003 May;93(No 5):786–791. doi: 10.2105/ajph.93.5.786. 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeVoe JE, Wallace LS, Pandhi N, Solotaroff R, Fryer GE. Comprehending care in a medical home: A usual source of care and patient perceptions about healthcare communication. Journal American Board of Family Medicine. 2008;21(5):441–450. doi: 10.3122/jabfm.2008.05.080054. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phillips RL, Dodoo MS, Green LA, Fryer GE, Bazemore AW, McCoy KI, Petterson SM. Usual source of care: An important source of variation in health care spending. Health Affairs. March/April;28(No 2):567–577. doi: 10.1377/hlthaff.28.2.567. 2009. [DOI] [PubMed] [Google Scholar]
- 10.Walls CA, Rhodes KV, Kennedy JJ. The emergency department as a usual source of medical care: Estimates from the 1998 National Health Interviews Survey. Acad Emerg Med. 2002 Nov;9(11):1140–1145. doi: 10.1111/j.1553-2712.2002.tb01568.x. 2002. [DOI] [PubMed] [Google Scholar]
- 11.Blewett LA, Johnson PJ, Lee B, Scal PB. When a usual source of care and usual provider matter: Adult prevention and screening services. J Gen Intern Med. 2008;23(9):1354–60. doi: 10.1007/s11606-008-0659-0. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winters P, Tancredit D, Fiscella K. The role of usual source of care in cholesterol treatment. J Am Board Fam Med. 2010 March/April;23(No 2):179–185. doi: 10.3122/jabfm.2010.02.090084. 2010. doi: 10.3122/jabfm.2010.02.090084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith MA, Bartell JM. Changes in usual source of care and perceptions of health care access, quality, and use. Medical Care. 2004 Oct;42(No 10):975–984. doi: 10.1097/00005650-200410000-00006. 2004. [DOI] [PubMed] [Google Scholar]
- 14.Everett CM, Schumacher JR, Wright A, Smith MA. Physician assistants and nurse practitioners as a usual source of care. Journal of Rural Health. 2009 Fall;25(No 4):407–414. doi: 10.1111/j.1748-0361.2009.00252.x. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minden SL, Hoaglin DC, Hadden L, Frankel D, Robbins T, Perloff J. Access to and utilization of neurologists by people with multiple sclerosis. Neurology. 2008;70:1141–1149. doi: 10.1212/01.wnl.0000306411.46934.ef. 2008. doi: 10.1212/01.wnl0000306411.46934.ef. [DOI] [PubMed] [Google Scholar]
- 16.Smith M. Identifying episodes of back pain using Medical Expenditures Panel Survey (MEPS) data: Patient experience, use of services, and chronicity. Journal of Manipulative and Physiological Therapeutics. 2010 October;33(No8):562–575. doi: 10.1016/j.jmpt.2010.08.017. 2010. doi:10.1016/j.jmpt.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality (AHRQ) Medical Expenditures Panel Survey (MEPS) Access page to Online Workbook: http://www.meps.ahrq.gov/mepsweb/about_meps/online_workbook.jsp.
- 18.Elixhauser A, Steiner CA, Whittington CA, McCarthy E. Healthcare cost and utilization project, HCUP-3 research note. Agency for Healthcare Research and Quality; Rockville, MD: 1998. Clinical classifications for health policy research: Hospital inpatient statistics, 1995. AHCPR Pub. No. 98-0049. [Google Scholar]
- 19.Hayward RA, Bernard AM, Freeman HE, Corey CR. Regular source of ambulatory care and access to health services. Am J Public Health. 1991 April;80(No4):434–438. doi: 10.2105/ajph.81.4.434. 1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams CH. The Synthesis Project, Issue 1. Robert Wood Johnson Foundation; 2002. From Coverage to Care: Exploring Links Between Health Insurance, a Usual Source of Care and Access. Published: September 2002 http://www.rwjf.org/pr/product.jsp?id=20113. [Google Scholar]
- 21.Carter SK, Rizzo JA. Use of outpatient physical therapy services by people with musculoskeletal conditions. Physical Therapy. 2007 May;87(No 5):497–512. doi: 10.2522/ptj.20050218. 2007. [DOI] [PubMed] [Google Scholar]
- 22.Smith M, Carber L. Chiropractic health care in Health Professional Shortage Areas (HPSAs) of the U.S. American Journal of Public Health. 2002 Dec;92(No. 12):2001–2009. doi: 10.2105/ajph.92.12.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCann J, Phillips RL, Green LA, Fryer GE. Chiropractors are not a usual source of primary health care. [Accessed April 6, 2011];Am Fam Physician. 2004 69(11):2544. 2004. http://www.graham-center.org/online/graham/home/publications/onepagers/2004/op28-chiropractors-source.html. [PubMed] [Google Scholar]