1 Introduction
Chemical signals, or neurotransmitters, represent the fundamental mode for intercellular communication in the nervous system. (1) The classical model for neurotransmitter action involves the uptake and storage of these small molecules into synaptic vesicles, release of vesicular contents into the synaptic cleft in response to depolarization of the presynaptic terminal by an action potential, binding of released neurotransmitters to cognate protein receptors on the postsynaptic (and presynaptic) terminal, and, finally, termination of signaling by protein-mediated uptake and degradation of neurotransmitters from the synaptic cleft. This model applies to a large number of well-studied neurotransmitters, including glutamate, γ-amino butyric acid (GABA), acetylcholine, and the monoamines, all of which represent aqueous solution-soluble molecules. More recently, lipids have emerged as an important class of chemical messengers in the nervous system that operate by a distinct mechanism.
The hydrophobic nature of lipids precludes their stable uptake and storage into synaptic vesicles. Instead, lipid messengers appear to be biosynthesized and released by neurons at the moment of their intended action, which is often referred to as “on-demand” production. Similarly, the capacity of lipids to freely cross cell membranes places the burden of signal termination largely on the action of degradative enzymes. Lipid signaling systems are thus embedded within an elaborate collection of metabolic pathways, the composition and regulation of which ultimately establish the magnitude and duration of transmitter action. Here, we will review these general concepts as they relate to a specific class of lipid transmitters, the endogenous cannabinoids (endocannabinoids), and highlight how delineation of their cognate metabolic enzymes has been translated into the development of chemical and genetic tools to test the role that the endocannabinoid system plays in nervous system signaling and behavior.
Endocannabinoids are defined as endogenous small molecules that activate the cannabinoid receptors CB1 and CB2, which are G-protein-coupled receptors that also recognize Δ9-tetrahydrocannabinol (THC), the psychoactive component of marijuana. (2, 3) The CB1 receptor is the major cannabinoid receptor in the nervous system and is responsible for mediating most of the neurobehavioral effects of THC. (4, 5) The CB2 receptor is predominantly expressed in immune cells, (6) where it appears to play a role in mediating the immunosuppressive effects of cannabinoids. Two principal endocannabinoids have been identified in mammals, N-arachidonoyl ethanolamine (anandamide) (7) and 2-arachidonoylglycerol (2-AG) (8, 9) (Figure 1). Each endocannabinoid also belongs to a much larger class of lipids, termed N-acyl ethanolamines (NAEs) and monoacylglycerols (MAGs), respectively, where individual members differ in the length and degree of unsaturation of their acyl chains (Figure 1). Several NAEs and MAGs have been ascribed potential biological activities in vivo; (10) however, most of these lipids do not serve as ligands for cannabinoid receptors, a property that appears to be restricted to polyunsaturated derivatives such as anandamide and 2-AG.
Figure 1.
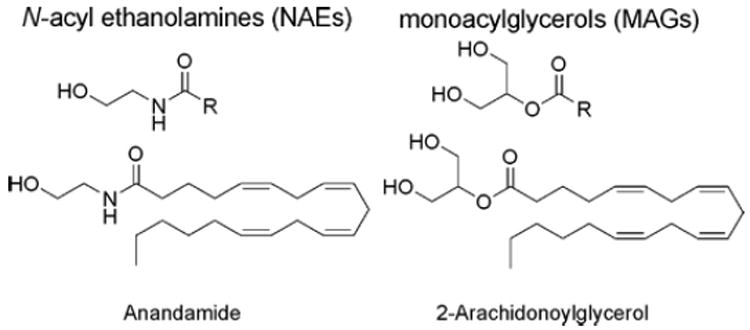
Two principle endocannabinoids, N-arachidonoyl ethanolamine (anandamide) and 2-arachidonoylglycerol (2-AG), which are members of theN-acyl ethanolamine (NAE) and monoacylglycerol (MAG) classes of lipids, respectively.
In the nervous system, endocannabinoids are hypothesized to act as retrograde messengers, being released by postsynaptic neurons and traversing the synaptic cleft to stimulate CB1 receptors on presynaptic termini (11, 12) (Figure 2). This model is supported by a large number of in vitro electrophysiological studies, (12) as well as by the restricted localization of the CB1 receptor to presynaptic structures in many regions of the nervous system. (13, 14) Once activated by endocannabinoids, CB1 receptors couple principally through the G i/G o class of G proteins to regulate calcium and potassium channels and reduce the probability of neurotransmitter release. (3) This suppression of neurotransmitter release can result in the inhibition or, paradoxically, disinhibition of neuronal circuits, depending on whether the CB1 receptor is expressed on glutamatergic or GABergic neurons.
Figure 2.
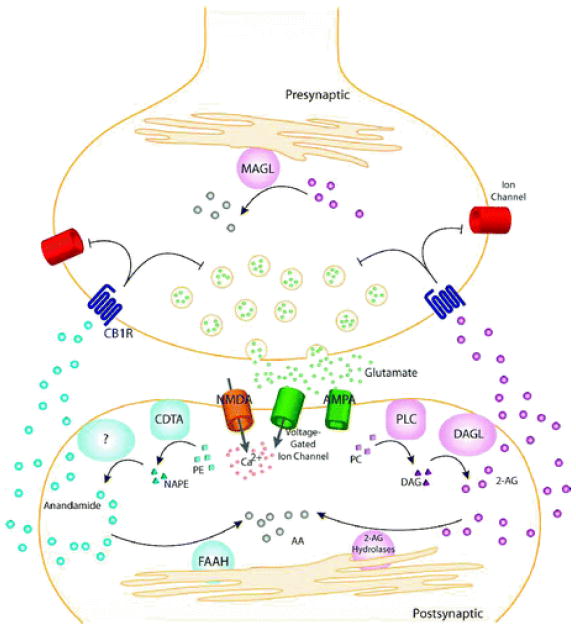
General model for endocannabinoid-based retrograde signaling. Upon release of neurotransmitter (e.g., glutamate), postsynaptic receptors (e.g., α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), N-methyl- d-aspartic acid (NMDA)) and voltage-gated ion channels are activated, allowing influx of Ca 2+ and on-demand endocannabinoid biosynthesis. Anandamide is synthesized from phospholipid precursors by a calcium-dependent transacylase (CDTA) and one or more other still uncharacterized enzymes. 2-Arachidonoylglycerol (2-AG) is synthesized from phospholipid precursors by phospholipase C (PLC) and diacylglycerol lipase (DAGL). Endocannabinoids then migrate from postsynaptic neurons to CB1 receptors (CB1R) located on presynaptic neurons. Once activated, CB1Rs couple through the G i/G o class of G-proteins to regulate ion channels and inhibit neurotransmitter release. The retrograde signaling of endocannabinoids is then terminated by degradative enzymes. Anandamide is hydrolyzed to arachidonic acid (AA) primarily by fatty acid amide hydrolase (FAAH), located in the postsynaptic neuron. 2-AG is hydrolyzed to AA primarily by monoacylglycerol lipase (MAGL) in the presynaptic neuron, though other 2-AG hydrolases may also participate in this process.
Despite sharing a common receptor and considerable structural similarity, anandamide and 2-AG can be distinguished by multiple factors. First, these endocannabinoids activate cannabinoid receptors to a differing degree in vitro, with anandamide displaying lower intrinsic efficacy than 2-AG, which results in the former lipid acting as a partial agonist (15) (it should be specified that the relevance of this distinction for signaling in vivo is unclear, especially when one considers that THC also acts as only a partial agonist for cannabinoid receptors in vitro (16)). Second, the endogenous quantities of anandamide and 2-AG differ dramatically, with the latter lipid being found at more than 100-fold higher concentrations in the nervous system. (16) Of course, these values are based on bulk tissue measurements of endocannabinoids, which almost certainly reflect a combination of metabolic and signaling pools of these lipids. Indeed, recent microdialysis studies have revealed that the extracellular concentrations of anandamide and 2-AG are nearly equivalent (within 2 5-fold), (17, 18) suggesting that, at least for the latter endocannabinoid, a large fraction of bulk tissue concentration may correspond to intracellular metabolic pools. Finally, and of greatest relevance for the subject of this review, anandamide and 2-AG are regulated by distinct biosynthetic and degradative pathways.
Over the past decade, several excellent reviews have appeared that discuss endocannabinoid metabolism and signaling. (10, 19-23) Here, we will focus on the most recent advances in our understanding of the composition and regulation of endocannabinoid metabolic pathways, especially as pertains to the nervous system. A pervasive theme throughout this review will be the importance of developing selective genetic and pharmacological tools to specifically perturb individual enzymatic pathways to test their contribution to endocannabinoid metabolism, nervous system function, and, ultimately, mammalian physiology and behavior.
2 Enzymatic Degradation of the Endocannabinoid Anandamide
Anandamide was the first identified endogenous ligand for the CB1 receptor. (7) As will be described in the following section, anandamide and other NAEs are produced upon demand through activity-dependent cleavage of membrane lipid precursors. The biological activity of anandamide in the central nervous system and in peripheral tissues is terminated by its removal from the extracellular space via cellular uptake by a putative transporter followed by enzymatic degradation. The principle enzyme responsible for anandamide degradation in the nervous system has been identified as the integral membrane protein fatty acid amide hydrolase (FAAH). (24) FAAH terminates anandamide signaling by hydrolyzing this lipid to arachidonic acid and ethanolamine (Figure 3). Here, we will review the role that FAAH plays in anandamide metabolism, as well as highlight additional enzymes that may participate in this process.
Figure 3.
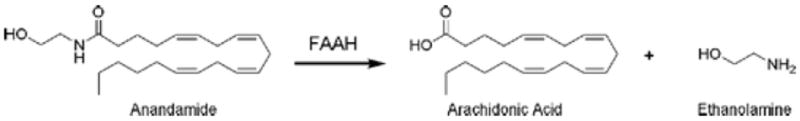
Enzymatic hydrolysis of anandamide to arachidonic acid and ethanolamine catalyzed by FAAH.
2.1 FAAH as the Principal Anandamide Hydrolase in the Nervous System
2.1.1 Molecular Characterization of FAAH
A membrane-associated enzyme activity from rat liver that hydrolyzes saturated and monounsaturated NAEs was first described in 1985 by Schmid and colleagues. (25) In 1993, an enzyme activity with similar properties that converted anandamide to arachidonic acid was characterized from N18TG2 neuroblastoma cells (26) and from rat and porcine brain tissue. (27-29) Following the identification of the fatty acid 2 primary amide oleamide as a sleep-inducing substance, an oleamide hydrolase activity was described (30) and suggested to represent the same enzyme as the anandamide/NAE hydrolase. (31) In 1996, Cravatt and colleagues succeeded in purifying this amidohydrolase activity to near homogeneity from rat liver membranes using a column covalently modified with an oleoyl trifluoromethyl ketone inhibitor derivative. (32) Cloning and transfection of the corresponding cDNA confirmed that the enzyme displayed robust hydrolysis activity for numerous fatty acid amides, including anandamide and oleamide. The enzyme was therefore named fatty acid amide hydrolase (FAAH). Human, (33) mouse, (33) and pig (34) FAAH genes have since been characterized and shown to be highly conserved in primary structure. Each enzyme possesses a single predicted NH 2-terminal transmembrane domain, an amidase signature (AS) domain, and a polyproline sequence predicted to interact with Homer and SH3 domain proteins (Figure 4A). Both the human and rat FAAH are expressed at high levels in the nervous system, but they show differences in their relative distribution among peripheral tissues. (32, 33) Immunohistochemical and immuno-electron microscopy studies have revealed that FAAH is broadly expressed in the nervous system, where the enzyme localizes predominantly to intracellular membranes (e.g., smooth endoplasmic reticulum, outer membrane of the mitochondria) in the somatodendritic compartment of neurons. (13, 35)
Figure 4.
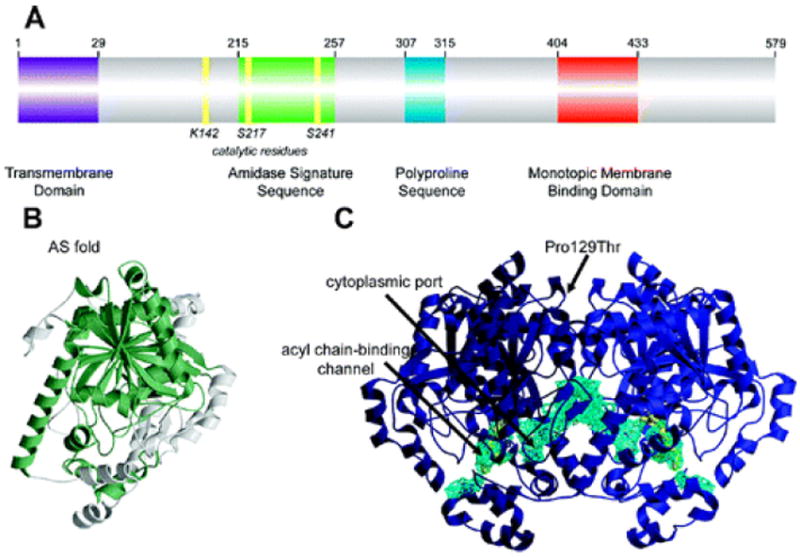
Structural features of FAAH: (A) Primary sequence analysis reveals a predicted NH 2-terminal transmembrane domain (purple), an amidase signature sequence rich in glycine and serine residues (green), a polyproline sequence predicted to interact with Homer and SH3 domain-containing proteins (blue), and a monotopic membrane binding domain that enables FAAH to bind the membrane even in the absence of the transmembrane domain (red). (B) An overlay of the known structures of amidase signature (AS) enzymes reveals a common “AS fold”, shown in green for the FAAH monomer. (C) Two channels in the FAAH X-ray crystal structure suggest possible routes for substrate binding (acyl chain-binding channel) and product release (cytoplasmic port). Structural studies also revealed that a common human single nucleotide polymorphism, which results in mutation of Pro129 to threonine, is located on the putative cytoplasmic face of FAAH.
Sequence analysis designated FAAH as the first characterized mammalian member of a large group of enzymes termed the amidase signature (AS) family. AS enzymes are characterized by a highly conserved region that is rich in serine, glycine, and alanine residues comprising approximately 130 amino acid residues. (36) There are more than 100 members of this enzyme family, most of which are bacterial and fungal in origin. Despite sharing significant sequence homology, members of this enzyme class exhibit markedly different substrate specificities.
Unlike most AS enzymes, FAAH is an integral membrane protein, a property originally assumed to be due to its predicted transmembrane domain (amino acids 9–29). However, deletion of the first 29 amino acids of rat FAAH generated a catalytically active variant, termed transmembrane domain-deleted FAAH (ΔTM-FAAH), that still bound to membranes even following treatments, such as strong base, intended to remove peripherally bound proteins. (37) These results indicated that FAAH possesses multiple domains for membrane association.
2.1.2 Recombinant Expression and Purification of FAAH
To achieve sufficient quantities of purified FAAH for mechanistic and structural studies, a bacterial expression system was developed for the rat enzyme. Both wild-type (WT) and ΔTM-FAAH were expressed with COOH- and NH2-terminal histidine tags, respectively, in E. coli and purified to near homogeneity. (37) Detergents were required to solubilize both enzymes and retain these proteins in solution throughout the purification process. Typical yields of purified WT- or ΔTM-FAAH were 1-1.5 mg/L of culture. Comparison of WT and ΔTM-FAAH showed that these enzymes possessed similar catalytic properties but differed in their solution size. While ΔTM-FAAH principally existed as a single 11S detergent–protein complex as estimated by analytical ultracentrifugation, the WT enzyme was distributed as a heterogeneous mixture of larger species ranging from 15S to 28S in size. These findings designated ΔTM-FAAH as a potentially superior protein for structural studies.
Expression of a recombinant rat FAAH with the COOH-terminal histidine tag has since been reported in a baculovirus–insect cell expression system; however, the level of expression was not reported. (38) Several reports have appeared that describe the recombinant expression of human FAAH using baculovirus–insect cell (39, 40) and E. coli (39) systems. However, the human FAAH expression levels were not reported in these studies.
2.1.3 Three-Dimensional Structure and Catalytic Mechanism of FAAH
In 2002, the X-ray crystal structure of the rat ΔTM-FAAH in complex with an irreversible inhibitor, methoxy arachidonyl fluorophosphonate (MAFP), was determined at 2.8 Å resolution. (41) The X-ray crystal structures of two other soluble bacterial AS enzymes, malonamidase E2 (42) and peptide amidase, (43) were also solved in the same year, allowing the first opportunity to compare and contrast the three-dimensional structures of widely divergent members of the AS family.
All three enzymes share a common core fold comprised of a twisted β-sheet consisting of 11 mixed strands, surrounded by a number of α-helices (shown for the FAAH monomer in Figure 4B). FAAH crystallized as a dimeric enzyme, consistent with chemical cross-linking and analytical ultracentrifuge studies. (37) The FAAH structure revealed multiple channels that appear to grant the enzyme simultaneous access to both the membrane and cytosolic compartments of the cell (Figure 4C). One channel leads from the putative membrane-binding surface of the protein to the enzyme active site and was occupied by the bound methoxyl arachidonyl phosphonate (MAP) molecule. This channel, dubbed the “acyl chain-binding” channel, is comprised almost entirely of hydrophobic residues and is thought to participate in substrate recognition. Consistent with this premise, mutagenesis studies have identified key residues in this channel that alter substrate recognition. (44) A second channel emerges from the active site at an angle of approximately 80° from the substrate-binding cavity to create a solvent-exposed “cytoplasmic port”. The overall architecture of the FAAH structure suggests a model where fatty acid amide substrates gain access to the active site by first entering into the membrane. After hydrolysis, the hydrophobic fatty acid and hydrophilic amine products would then exit via the membrane-access and cytosolic-access channels, respectively. The “cytoplasmic port” may play an additional role by providing entry to a water molecule required for turnover of the acyl–enzyme intermediate, which has been biochemically characterized previously by liquid chromatography–mass spectrometry methods. (45)
The FAAH structure also revealed that this enzyme possesses an unusual serine–serine–lysine (Ser241-Ser217-Lys142) catalytic triad that is conserved among enzymes from the AS class. Through a series of site-directed mutagenesis, enzyme kinetics, and chemical labeling studies, Ser241 was determined to be the FAAH nucleophile. (45-47) In support of this assignment, the MAFP inhibitor is covalently adducted to Ser241 in the FAAH crystal structure. The equivalent serine residue in other AS enzymes has been found to be either covalently bound (42) or in close proximity (43) to the electrophilic center of an active-site directed inhibitor. These results indicate that AS enzymes are members of the serine hydrolase superfamily.
The Ser241-Ser217-Lys142 catalytic triad of FAAH, which is distinct from the typical Ser-His-Asp catalytic triad utilized by the majority of serine hydrolases, has been the focus of extensive mutagenesis studies. Lys142 of FAAH appears to serve as a key acid and base in distinct steps of the catalytic cycle. (47, 48) As a base, Lys142 first activates the Ser241 nucleophile for attack on the substrate amide carbonyl. Evidence in support of this role for Lys142 includes the properties of a Lys142Ala mutant, which displays a dramatically reduced catalytic activity that shows linear dependence on solvent pH. (47, 48) The Lys142Ala mutant also exhibits severely reduced flurorophosphonate reactivity, indicating a weakened Ser241 nucleophile. (47, 48) Furthermore, a Lys142Glu mutant yielded a catalytically deficient enzyme with a shifted pKa value from 8 to 5–6. (48) These data are consistent with the conversion of an active site base from lysine to glutamate. The critical role of Lys142 as an acid that participates in the protonation of the substrate leaving group also has been demonstrated in the following examples. FAAH exhibits an unusual ability to hydrolyze amides and esters at equivalent rates. (48) However, this property is lost in the Lys142Ala mutant, which hydrolyzes esters at much greater rates than amides. Notably, the Lys142Glu mutant, despite its greatly reduced nucleophilic strength, still hydrolyzed amides and esters at equivalent rates.
Ser217 was also found to play a key role in catalysis as a mutation of this residue to alanine significantly reduced both hydrolytic activity and reactivity with fluorophosphonate probes. (46, 47) The structural arrangements of catalytic residues in FAAH indicates that the impact of Lys142 on Ser241 nucleophilic strength and leaving group protonation likely occurs indirectly via the bridging Ser217 of the triad, which may act as a “proton shuttle” as shown in Figure 5. In this mechanism, FAAH would force protonation of the substrate leaving group early in the transition state of acylation concomitant with the nucleophilic attack on the substrate carbonyl group. Such tight coupling of base-catalyzed nucleophilic activation and acid-catalyzed leaving group protonation could enable FAAH to hydrolyze amide and ester substrates with comparable efficiencies. This property may be relevant for FAAH function in vivo, where the enzyme likely encounters its fatty acid amide substrates in a background of high concentrations of structurally similar ester lipids.
Figure 5.
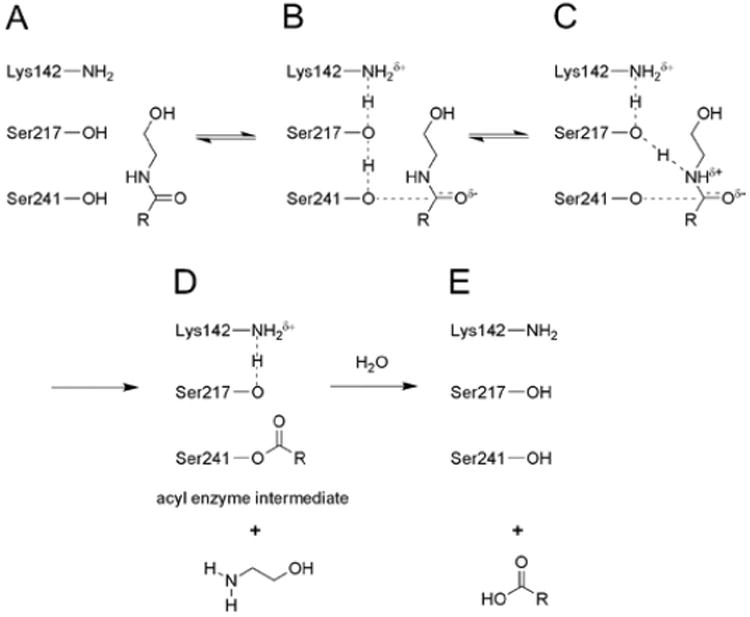
Proposed mechanism for the hydrolysis of amide and ester substrates catalyzed by FAAH (shown for amides): (A) Lys142, initially in a deprotonated state, (B) abstracts a proton from Ser217, which in turn abstracts a proton from the Ser241 nucleophile. (C) Attack of the nucleophile on the substrate carbonyl is proposed to occur in a coupled manner with proton donation from Ser217 to the nitrogen atom of the amide substrate. This latter step requires the concurrent donation of a proton from Lys142 to Ser217, resulting in (D) the formation of an acyl–enzyme intermediate where both Lys142 and Ser217 have returned to their initial protonation states. (E) Deacylation results in release of the free fatty acid product.
2.1.4 FAAH Knockout [FAAH (−/−)] Mice
The behavioral effects of anandamide are very weak and transient compared with those produced by exogenous Δ 9-THC. (49) This difference is likely due to the extremely short half-life of anandamide in vivo (less than 5 min), where the enzyme has been shown to undergo rapid hydrolysis. (50) The essential role of FAAH in mediating anandamide hydrolysis in vivo was confirmed by generation and characterization of FAAH(−/−) mice. FAAH(−/−) mice were generated by standard targeted disruption procedures and found to be viable, healthy, and fertile. (51) Tissue extracts from FAAH(−/−) mice displayed 50–100-fold reductions in hydrolysis rates for anandamide (and other fatty acid amides), indicating that FAAH is the principle anandamide hydrolase in most mouse tissues, including brain. Consistent with their inability to efficiently degrade anandamide, FAAH(−/−) mice showed striking behavioral responses to this endocannabinoid, including robust hypomobility, analgesia, hypothermia, and catalepsy. Importantly, all of the behavioral effects of anandamide in FAAH(−/−) mice were blocked by pretreatment with a CB1 receptor antagonist, indicating that anandamide acts as a selective CB1 agonist in these animals. A recent study using mice lacking both FAAH and CB1 receptor has confirmed that the CB1 receptor mediates the majority of the behavioral effects induced by anandamide in FAAH(−/−) mice. (52)
FAAH(−/−) mice were also found to possess dramatic (>10-fold) elevations in the endogenous brain levels of many fatty acid amides, including anandamide, (51) a neurochemical phenotype that was observed in several brain regions. (53) These marked changes in brain levels for anandamide and other fatty acid amides correlated with a CB1 receptor-dependent analgesic phenotype in FAAH(−/−) mice in several models of acute and inflammatory pain (54) (Table 1). FAAH(−/−) mice have also been shown to exhibit reduced inflammatory responses in models of intestinal colitis, (55) paw edema, (54, 56) and contact dermatitis. (57) These anti-inflammatory phenotypes may be mediated by a largely peripheral, rather than central mechanism because transgenic mice that express FAAH specifically in the nervous system (FAAH-NS mice) still show reduced inflammation in the carrageenan-induced paw edema model (56) (Table 1). The contribution of the CB1 and CB2 receptors to the anti-inflammatory phenotypes observed in FAAH(−/−) mice remains unclear, and at least in certain cases, evidence has been provided that the observed anti-inflammatory phenotype may be mediated by a noncannabinoid receptor mechanism. (56)
Table 1.
Comparison of Neuro-Behavioral Effects of Direct CB1 Agonists and Genetic/Pharmacological Blockade of FAAH
| CB1 agonist | FAAH KO mice | FAAH-NS mice | FAAH inhibitor | |
|---|---|---|---|---|
| Potential Therapeutic Effects | ||||
| analgesia | yes | yes | no | yes |
| anxiolysis | yes | yes | unknown | yes |
| antidepressant | yes | yes | unknown | yes |
| anti-inflammation | yes | yes | yes | yes |
| antispasticity | yes | unknown | unknown | unknown |
| antiemesis | yes | unknown | unknown | yes |
| decreased intraocular pressure | yes | unknown | unknown | unknown |
| memory improvement | unknown | yes | unknown | unknown |
| slow wave sleep improvement | unknown | yes | unknown | unknown |
| Side Effects | ||||
| hypomotility | yes | no | no | no |
| hypothermia | yes | no | no | no |
| catalepsy | yes | no | no | no |
More recently, other phenotypes have been reported in the FAAH(−/−) mice, including reductions in anxiety and depression, (58, 59) as well as improvements in slow wave sleep (60) and memory acquisition and extinction (61) (Table 1). Importantly, these phenotypes occur in the absence of alterations in motility, weight gain, or body temperature that are typically observed with direct CB1 agonists (Table 1). These findings suggest that FAAH may represent an attractive therapeutic target for the treatment of pain, inflammation, and other CNS disorders and has stimulated interest in the development of selective inhibitors of this enzyme.
2.1.5 FAAH Inhibitors and Their Pharmacological Effects
First-generation FAAH inhibitors were based closely on the structures of substrates for the enzyme. These include oleoyl and arachidonoyl derivatives of trifluoromethyl ketones (62, 63) and fluorophosphonates, (64) which were shown to be potent reversible and irreversible inhibitors of FAAH, respectively (Figure 6). However, not surprisingly, these compounds also inhibit several other serine hydrolases. (65-67)
Figure 6.
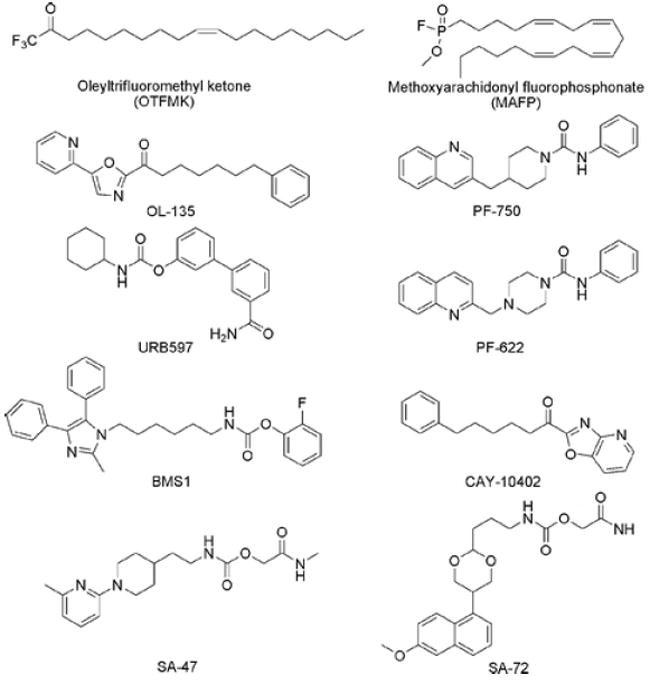
Representative FAAH inhibitors.
Boger and colleagues reported a large group of α-ketoheterocyclic inhibitors that are reversible inhibitors of FAAH and are highly potent while lacking substrate-like structures. (68, 69) Some of these α-ketoheterocycles, such as OL-135 (Figure 6), have been found to display in vivo activity, producing analgesic effects in acute thermal and noxious chemical pain assays in mice (69) (Table 1). OL-135 also resulted in a dose-responsive reversal of mechanical allodynia in both mild thermal injury and spinal nerve ligation models in the rat. (70) These pharmacological effects of OL-135 have been correlated with ~3-fold elevations in brain anandamide levels. (69)
A second class of FAAH inhibitors that displays excellent in vivo activity is the carbamates, as exemplified by URB597 (71) (Figure 6). URB597 inhibits FAAH by carbamylation of the active site Ser241 nucleophile (72) (Figure 7). URB597 has been shown to display activity in rodent models of acute, (71) inflammatory, (73, 74) and neuropathic pain, (75, 76) as well as anxiety (71) and depression (77) (Table 1). URB597 has also been found to enhance nonopioid, stress-induced analgesia. (78) The effects of URB597 on neuropathic pain are complex, because spinal administration of the agent attenuated evoked responses on neurons in neuropathic rats (76) but systemic administration was not able to reduce mechanical allodynia in the rat partial sciatic nerve-ligation model of neuropathic pain. (74) On the other hand, URB597 did reduce hyperalgesia in the mouse chronic constriction injury model of neuropathic pain. (75)
Figure 7.
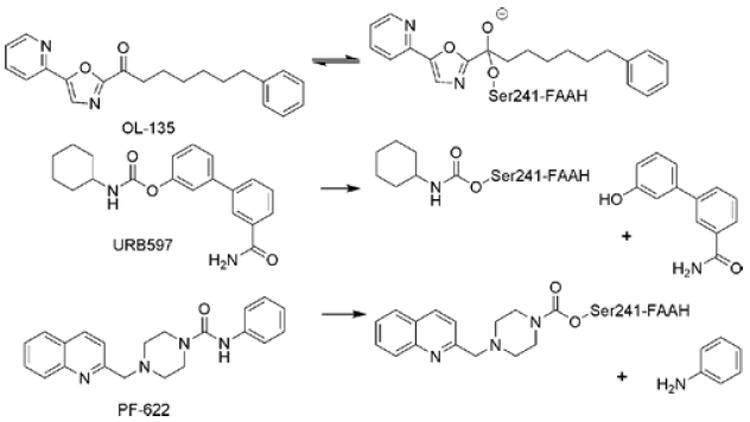
Different modes of action for classes of FAAH inhibitors. OL-135, an α-ketoheterocycle, is a covalent, reversible inhibitor of FAAH. URB597, a carbamate, and PF-622, a piperazine urea, irreversibly inhibit FAAH by carbamylation of the Ser241 nucleophile.
URB597 has been shown to display anxiolytic (59, 71, 79) and antidepressant-like (77) activities in rodents (Table 1). More recently, FAAH(−/−) mice have also been shown to display anxiolytic and antidepressant phenotypes, (58, 59) although substantial methodological changes needed to be made to observe these effects. (58) The authors speculated that the contribution of the FAAH–endocannabinoid system may depend on the levels of stress associated with the environmental conditions. Daily administration of URB597 (0.3 mg/kg, ip) for 5 weeks attenuated the reduction in body weight gain and sucrose intake in rats induced by chronic mild stress, a behavioral model of depression. (80) This treatment also resulted in a significant inhibition of brain FAAH activity with a concomitant increase in anandamide levels in midbrain, striatum, and thalamus.
Studies with FAAH inhibitors and FAAH(−/−) mice have revealed additional physiological processes regulated by the endocannabinoid system. In spontaneously hypertensive rats, URB597 reduced blood pressure, cardiac contractibility, and vascular resistance to levels in normotensive rats, and these effects were blocked by CB1 antagonist. (81) Age-associated declines in cardiac function and changes in inflammatory gene expression, nitrative stress, and apoptosis were also attenuated in FAAH(−/−) mice. (82) These results suggest that the pharmacological blockade of FAAH may represent a protective strategy to counter cardiovascular aging and atherosclerosis. URB597 (0.3 mg/kg, ip) has also been shown to suppress conditioned gaping (a model of nausea) elicited by a lithium-paired context in the rat, which was reversed by CB1 antagonists. (83)
Despite producing a provocative number of behavioral effects, α-ketoheterocycle and carbamate inhibitors of FAAH display rather short durations of action in vivo (2–3 h) (69, 84) and variable degrees of selectivity when tested against other members of the serine hydrolase family. (69, 72, 85, 86) These factors have inspired the search for additional chemotypes capable of inhibiting FAAH with high selectivity. Recently, piperidine/piperazine ureas represented by PF-750 and PF-622 were reported as a novel mechanistic class of FAAH inhibitors. (86) These agents were developed based on hits from a high-throughput screen that exploited an advanced colorimetric, coupled-enzyme assay for FAAH. (87, 88) Rather unexpectedly based on the high chemical stability of the urea functional group, PF-750 and PF-622 were found to inhibit FAAH in a time-dependent manner by covalently modifying the enzyme’s Ser241 nucleophile (Figure 7). Unlike previously reported FAAH inhibitors, PF-750 and PF-622 were found to be completely selective for FAAH relative to other mammalian serine hydrolases as judged by activity-based proteomic profiling (discussed in section). The remarkable specificity of the piperidine/piperazine urea inhibitors for FAAH may derive, at least in part, from this enzyme’s ability to function as a C(O)–N bond hydrolase, which distinguishes it from the vast majority of metabolic serine hydrolases in mammals that are restricted to hydrolyzing esters or thioesters. Notably, additional reports of urea-based inhibitors of FAAH have recently appeared in the patent literature. (89, 90) A detailed understanding of the mechanism of inhibition for these agents requires further investigation, but the studies performed on PF-750 and PF-622 discussed above (86) suggest that they likely also act in a covalent, irreversible manner.
2.1.6 Evaluating the Selectivity of FAAH Inhibitors by Activity-Based Protein Profiling
In order for FAAH inhibitors to serve as useful pharmacological research tools and potentially drugs, they must display high selectivity for FAAH relative to the numerous other serine hydrolases found in mammalian proteomes. Determining the selectivity of FAAH inhibitors by conventional substrate-based assays would represent a daunting task considering the tremendous size of the serine hydrolase superfamily (>200 members in humans) as well as the large number of these enzymes that represent uncharacterized proteins (i.e., enzymes without known substrates). With these issues in mind, a functional proteomic screen based on the activity-based protein profiling (ABPP) (91, 92) technology has been implemented to evaluate the selectivity of FAAH inhibitors against numerous serine hydrolases directly in native cell/tissue samples.
Competitive ABPP for serine hydrolases involves the coordinated application of a candidate inhibitor and a reporter-tagged fluorophosphonate, (93) which serves as a general activity-based probe for the serine hydrolase superfamily (94, 95) (Figure 8). Serine hydrolases that show significant reductions in probe labeling intensity in the presence of inhibitor are scored as targets of the compound. In this way, competitive ABPP provides a global view of the proteome-wide selectivity of serine hydrolase inhibitors and has been successfully employed to address the selectivity of various FAAH inhibitors. (69, 72, 85, 86, 93, 96, 97)
Figure 8.
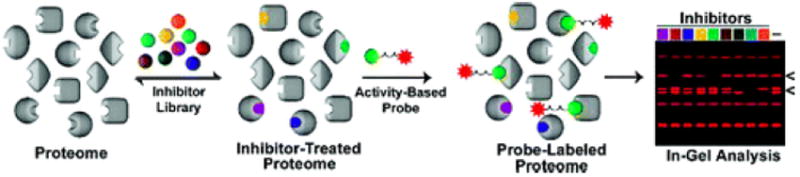
Competitive activity-based protein profiling (ABPP). To determine the selectivity of an inhibitor library against serine hydrolases, a proteome is reacted with inhibitor and subsequently labeled with a rhodamine-tagged fluorophosphonate. Reacted proteomes are then analyzed by 1-D SDS-PAGE. A decrease in fluorescent intensity of the probe in the presence of inhibitor indicates a target.
The selectivity of FAAH inhibitors was tested by competitive ABPP in multiple rat, mouse, and human tissues. Most inhibitors were selective for FAAH in brain tissue, but possessed additional targets in peripheral tissues such as liver and kidney. URB597 (1–100 μM), BMS1 (1–10 μM), OL-135 (10–100 μM), and CAY-10402 (10–100 μM) (Figure 6), for example, were found to inhibit multiple serine hydrolases, including FAAH and several members of the carboxyesterase clan. (69, 85, 86, 93, 96, 97) These carboxylesterase targets were especially sensitive to the aryloxy carbamates URB597 and BMS1. In contrast, the alkoxy carbamates SA-47 and SA-72, showed much higher selectivity for FAAH, possibly reflecting a reduction in their inherent reactivity. (85)
The selectivity of the piperidine/piperazine ureas represented by PF-750 was also assessed by competitive ABPP in multiple human and mouse tissue proteomes. The results indicated that PF-750 is a remarkably selective FAAH inhibitor, showing no discernible activity against other serine hydrolases in vitro or in vivo at concentrations up to 500 μM and 30 mg/kg (i.p.), respectively. (86)
2.1.7 Metabolomic Profiling of FAAH-Inactivated Animals
The generation of FAAH(−/−) mice and FAAH inhibitors has confirmed the enzyme’s role in anandamide/NAE metabolism in vivo, but whether these lipids represent the only endogenous substrates of FAAH remained unknown. To address this question, Saghatelian and colleagues performed a comparative metabolomic analysis of tissues from wild-type and FAAH-inactivated animals using an untargeted liquid chromatography–mass spectrometry platform. (98) These studies led to the discovery of a second structural class of lipids regulated by FAAH in vivo, theN-acyl taurines (NATs) (Figure 9). High concentrations of long chain (≥C20) saturated NATs were observed in the CNS of FAAH(−/−) mice. (98) In contrast, peripheral mouse tissues (livers and kidneys) were enriched in polyunsaturated acyl chains (e.g., C20:4, C22:6). (99) Peripheral NATs rose more than 10-fold within 1 h following pharmacological inactivation of FAAH, implicating a constitutive and highly active pathway for NAT metabolism in which FAAH plays an integral part. Polyunsaturated NATs were found to activate multiple members of the transient receptor potential (TRP) channel family, (99) suggesting that these lipids may possess signaling functions in vivo.
Figure 9.
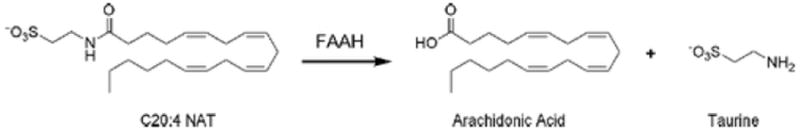
Enzymatic hydrolysis of C20:4 N-acyl taurine (NAT) to arachidonic acid and taurine catalyzed by FAAH.
The discovery of a second class of bioactive lipids regulated by FAAH raises provocative questions regarding the mechanistic basis for phenotypes observed in FAAH-inactivated animals. Might some of the noncannabinoid phenotypes observed in these animals be due to the action of NATs? To begin to address this question, McKinney and Cravatt have rationally designed a mutant of FAAH, Gly268Asp, that exhibits wild-type hydrolytic activity with NAEs but a greater than 100-fold decrease in activity with NATs. (100) “Knock-in” mice that express this G268D-FAAH variant could provide a valuable model for distinguishing behavioral phenotypes due to elevations in the NAE versus NAT classes of FAAH substrates.
2.1.8 A Role for FAAH in the Cellular Uptake of Anandamide
Unlike many classical neurotransmitters, which are stored in vesicles prior to release, lipid messengers such as fatty acid amides are thought to be enzymatically produced and released upon demand. Termination of fatty acid amide signaling involves intracellular accumulation and enzymatic degradation. While FAAH has been well established as the most prominent enzyme responsible for degrading fatty acid amides in the nervous system, the mechanisms whereby fatty acid amides are taken up into neurons have remained rather controversial.
One model of anandamide uptake involves the action of a plasma membrane-associated transporter, which has been proposed to operate by an ATP-independent, facilitated diffusion mechanism. (101-103) Despite extensive publications in the area, (104-106) the cloning and the molecular identification of this putative anandamide transporter has not yet been achieved. Another model has focused on the possibility that much of anandamide uptake is driven by FAAH itself. (107, 108) Consistent with this model, cells that express high levels of FAAH show a greatly accelerated rate of anandamide uptake. (107, 109, 110) Furthermore, most of the anandamide-derivatized transporter inhibitors described to date also inhibit FAAH, including AM404, (111) VDM11, (112) and LY218240. (113, 114) Neurons from FAAH(−/−) mice have also been shown to display impaired anandamide uptake, especially at later time points. (115) Collectively, these data suggest that FAAH may create a metabolic driving force for the cellular uptake of anandamide. (108) Further data supporting this model was recently shown by measuring anandamide uptake at 25 s, conditions where FAAH does not appreciably affect uptake. (108) Transporter inhibitors, which are reported as inhibiting FAAH weakly or not at all in vitro (UCM707, OMDM2, and AM1172), did not affect uptake at 25 s, while showing appreciable inhibition of anandamide accumulation at 5 min correlating with partial inhibition of anandamide hydrolysis. (116) Moreover, at 5 min, these inhibitors did not inhibit anandamide uptake in FAAH chemical knockout cells, which strongly suggests that the target of these inhibitors is not a transporter but rather FAAH or possibly an uncharacterized intracellular component that delivers anandamide to FAAH. (116)
Whether additional proteins other than FAAH contribute to anandamide uptake is a research topic under active investigation. Indeed, one might expect that proteins would exist to facilitate the delivery of anandamide from the cell surface to intracellular membranes that contain FAAH. In support of this general idea, AM404 and UCM707, as well as other compounds that show no detectable activity against FAAH, have been shown to inhibit anandamide uptake in neurons from FAAH(−/−) mice. (115, 117) Endocytosis has also been proposed as an alternative mode of anandamide internalization. (118, 119) It has been suggested that different cells may utilize distinct strategies for the accumulation of anandamide, (104) although it is a bit surprising that essentially every cell type that has been examined appears to possess a putative protein-mediated process for anandamide transport. The continued development of potent and selective anandamide uptake inhibitors that do not interact with FAAH should facilitate the molecular characterization of this intriguing cellular process.
2.1.9 A Human Polymorphism in the FAAH Gene Associated with Problem Drug Use and Obesity
In 2002, Sipe and colleagues reported a functional polymorphism in the human FAAH gene (C385A) that converts a conserved proline residue to threonine (Pro129Thr). (120) This proline residue is located on the surface of the predicted cytoplasmic face of FAAH (Figure 4C). The homozygous form of the C385A polymorphism was found to be associated with both street drug use and problem drug and alcohol use in a Caucasian population. (120) There was no correlation between this mutation and other behavioral or psychiatric disorders (i.e., schizophrenia, depression, alcohol problem alone, etc.). The Pro129Thr-FAAH variant displayed wild-type catalytic properties but showed reduced stability in the presence of proteases. (120) FAAH activity from T-lymphocytes isolated from patients homozygous for the C385A mutation express about half of the FAAH protein and activity observed in wild-type lymphocytes. (121) In addition, transfected COS-7 cells also express significantly lower levels of Pro129Thr-FAAH compared with WT-FAAH, indicating that the lower expression of the mutant protein is not a cell type-specific phenomenon. Initial data suggest that the reduced expression of the Pro129Thr-FAAH mutant may be due to a post-translational mechanism that precedes productive folding. (121)
Subsequent studies have provided mixed support for an association between the C385A polymorphism and drug and alcohol abuse. In a study involving adult Caucasians (N = 749), it was shown that subjects with the A/A genotype were significantly less likely to be THC dependent than subjects with either a C/C or C/A genotype. (122) Authors postulated that the reduced FAAH activity in the A/A genotype may lead to increased brain levels of anandamide, which could in turn reduce THC craving and withdrawal. No association was observed between the A/A genotype and risk for alcohol or tobacco regular use. The A/A genotype has also been linked to an increased risk for regular use of sedatives, (122) but no significant association has been found for methamphetamine dependence, schizophrenia, or alcoholism in a Japanese population. (123, 124)
A potential relationship between the C385A polymorphism and obesity was investigated in a study involving 2667 subjects of multiple ethnic backgrounds. (125) This study showed a strong correlation between the FAAH A/A genotype and being overweight or obese in both white and black populations but not in the Asian subjects. For the entire population, the median body mass index was higher in the FAAH A/A genotype than in the heterozygote and wild-type groups. (125) However, in a subsequent study that analyzed a large cohort of Danish whites, no significant association with obesity was observed for the FAAH A/A genotype. (126) In a recent 6-week low fat diet study, the FAAH A/A genotype showed a significantly greater decrease in triglycerides and total cholesterol as compared with the wild-type. (127)
In summary, studies performed to date suggest a potential link between the C385A FAAH polymorphism and problem drug use and weight gain. However, the examination of larger patient populations is required to both confirm and refine these initial findings. Additionally, the mechanistic basis for potential phenotypes caused by the C385A mutation remains to be elucidated.
2.2 Additional Enzymes That Hydrolyze Anandamide
2.2.1 FAAH-2
During the course of conducting ABPP studies on a panel of human cancer cell lines, a second amidase signature enzyme with fatty acid amide hydrolyzing activity was discovered and termed FAAH-2. (128) Despite sharing only limited sequence identity (~20%) with the original FAAH enzyme (dubbed, for the purposes of comparison, FAAH-1), FAAH-2 also possesses a predicted NH 2-terminal transmembrane domain and an AS sequence containing the serine-serine-lysine catalytic triad. FAAH-2 exhibited several distinct features in regard to its substrate specificity, inhibitor sensitivity, and tissue distribution compared with those of FAAH-1. FAAH-1 and FAAH-2 hydrolyzed primary fatty acid amide substrates such as oleamide at equivalent rates, whereas FAAH-1 hydrolyzed NAEs, including anandamide, at much greater rates than FAAH-2. The FAAH-2 gene was found in multiple primate genomes, marsupials, and more distantly related vertebrates but not in a number of lower placental mammals including mouse and rat. Tissue distributions for human FAAH-1 and FAAH-2 as judged by RT-PCR analysis were also distinct, with FAAH-1 showing robust expression in the nervous system and FAAH-2 appearing at higher relative levels in select peripheral tissues (e.g., heart, ovary). Interestingly, both enzymes were inhibited by O-aryl carbamates and α-keto heterocycles represented by URB597 and OL-135, respectively. The discovery of a second FAAH enzyme selectively present in higher mammals suggests that certain aspects of fatty acid amide metabolism may differ between humans and rodents.
2.2.2 NAE-Hydrolyzing Acid Amidase (NAAA)
A distinct NAE hydrolase enriched in immune cells that resides in the lysosome and exhibits an acidic pH optimum of 4.5–5.0 has been cloned and characterized. (129, 130) It has been termed N-acylethanolamine-hydrolyzing acid amidase (NAAA) to reflect its acidic pH optimum. This enzyme has no sequence homology with FAAH but shares 33–35% amino acid identity with acid ceramidase, a lysosomal enzyme that hydrolyzes ceramide to sphingosine and free fatty acid. Not surprisingly, in view of the high sequence similarity between NAAA and acid ceramidase, a low ceramide-hydrolyzing activity was detected in the lysate when human NAAA cDNA was transfected into HEK293 cells.
Unlike FAAH, which most prefers anandamide as a substrate, NAAA hydrolyzes N-palmitoylethanolamine (PEA) much faster than any other NAEs, especially in the presence of nonionic detergent. (129, 130) NAAA is not a serine hydrolase and is therefore much less sensitive to general serine hydrolase inhibitors such as phenylmethylsulfonyl fluoride (IC 50 = 3 mM) and MAFP (no inhibition at up to 10 μM). It is completely inhibited by 10 μM p-chloromercuribenzoic acid, a thiol-blocking reagent. (129) An effort to develop inhibitors of NAAA by derivatization of NAEs led to N-cyclohexanecarbonylpentadecylamine, which inhibited NAAA with an IC 50 value of 4.5 μM but did not inhibit FAAH. (131) In both rodent and human, NAAA shows highest relative expression in peripheral tissues. (132, 133) Using immunofluorescent microscopy, Tsuboi and colleagues showed the localization of NAAA to be in lysosomes of rat alveolar macrophages. (134) The contribution that NAAA makes to fatty acid amide hydrolysis in vivo remains largely unknown, although the high expression of the enzyme in macrophages and certain peripheral tissues points to a potential role at these sites.
2.3 Summary and Key Outstanding Questions
Tremendous progress has been gained in our understanding of multiple enzymes involved in the degradation of anandamide and related NAEs. Within a short time since the cloning and molecular identification of FAAH in 1996, (32) the requisite tools have been developed, including knockout mice and selective inhibitors, to confirm a prominent role for this enzyme in the termination of anandamide signaling in vivo. The genetic or pharmacological inactivation of FAAH elevates endogenous levels of fatty acid amides and produces analgesic, anxiolytic, antidepressant, sleep-enhancing, and anti-inflammatory phenotypes. Importantly, these behavioral phenotypes occur in the absence of alterations in motility, weight gain, or body temperature that are typically associated with direct CB1 agonists (Table 1). Therefore, FAAH inhibition appears to offer an attractive way to induce the beneficial properties of CB1 receptor activation without the undesirable side effects. Precisely how FAAH disruption selectively induces a subset of the phenotypes observed with direct CB1 agonists remains unknown but may reflect a restricted role for anandamide in specific CB1 pathways in the nervous system.
Attempts to forecast FAAH’s potential as a drug target need to also account for the possible effects of chronic FAAH inhibition. Extended periods of FAAH inactivation do not appear to cause obvious deleterious effects, because FAAH(−/−) mice have been shown to be viable and fertile and largely indistinguishable from their wild-type littermates. The identification of a human FAAH polymorphism linked to problem drug use and obesity also points to abuse potential as a concern for FAAH inhibitors. However, administration of URB597 has been shown to have no effect on two rat models of abuse liability, conditioned place preference test or the drug discrimination test. (77) On the other hand, FAAH has been implicated in alcohol consumption, as inactivation of this enzyme increases the preference for ethanol. (135, 136) Finally, a role for FAAH and anandamide in reproduction has been described, (137-139) although it should be emphasized that FAAH(−/−) mice are fertile. Despite these potential risks, clinical study of FAAH inhibitors for the potential treatment of human diseases is awaited with great anticipation.
Although this review is mostly focused on the processes that mediated endocannabinoid metabolism in the nervous system, where FAAH appears to play a principal role in anandamide degradation, it should be stressed that other enzymes, such as FAAH-2 and NAAA, may contribute to the termination of anandamide function in peripheral tissues. Further efforts to develop selective genetic or pharmacological tools to study these enzymes should strengthen our understanding of their contribution to endocannabinoid metabolism.
3 Enzymatic Biosynthesis of the Endocannabinoid Anandamide
3.1 Original Model for the Biosynthesis of NAEs via the Sequential Actions of a Calcium-Dependent Transacylase and Phospholipase D
Initial investigations into the biosynthetic pathways for NAEs were made by Schmid and colleagues many years prior to the discovery of anandamide as an endocannabinoid. In a pioneering series of studies, these authors delineated a two-step enzymatic pathway for NAEs that involved the sequential action of (1) a calcium-dependent transacylase (CDTA) that transfers the sn-1 acyl chain of phospholipids onto the primary amine of phosphatidylethanolamine (PE) to generate N-acyl phosphatidylethanolamines (NAPEs) (Figure 10, step A) and (2) a D-type phospholipase that hydrolyzes NAPEs to produce NAEs (140, 141) (Figure 10, step B). Initial lines of evidence indicated that this two-step pathway might also contribute to the biosynthesis of anandamide. First, anandamide, along with its NAE congeners and their respective NAPE precursors, is produced by neurons in a calcium-dependent manner. (101) Second, a brain CDTA activity is capable of producing the anandamide precursor N-arachidonoyl PE in vitro. (142) Third, molecular characterization of an NAPE-selective phospholipase D (NAPE-PLD) by Ueda and colleagues revealed that this enzyme can convert N-arachidonoyl PE to anandamide in vitro. (143)
Figure 10.
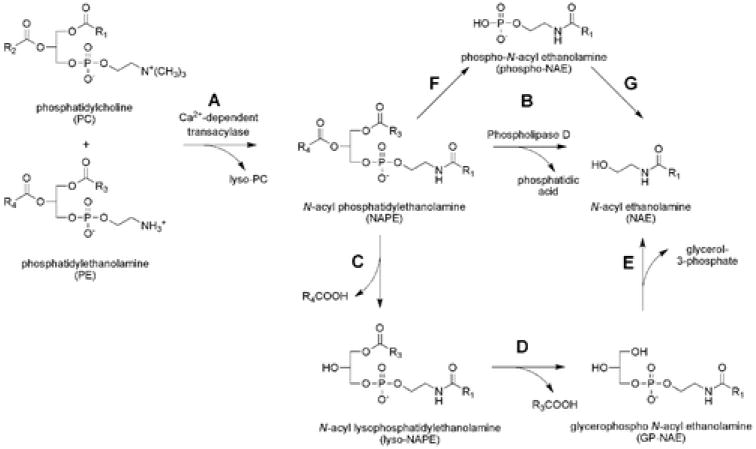
Postulated routes for the biosynthesis of anandamide and other NAEs: (A) A calcium-dependent transacylase (CDTA) converts phospholipid precursors to N-acyl phosphatidylethanolamine (NAPE). (B) Phospholipase D (PLD) then hydrolyzes NAPEs to produce NAEs. (C–E) An alternative PLD-independent pathway in which the sn-1 and sn-2 O-acyl chains of NAPEs are hydrolyzed to generate the intermediates lyso-NAPE (C) and glycerophospho (GP)-NAE (D), respectively. Subsequent cleavage of the phosphodiester bonds of lyso-NAPE and GP-NAE would then yield NAEs (E). (F, G) A third pathway for the conversion of NAPEs to NAEs involves a phospholipase C-dependent conversion of NAPEs to phospho-NAEs (F) followed by the hydrolysis of phospho-NAEs to NAEs by phosphatase-mediated hydrolysis (G).
On the basis of the aforementioned studies, it was originally assumed that most, if not all, NAEs were biosynthesized together by a common enzymatic pathway. However, as more detailed investigations into the regulated production of NAEs were performed, evidence began to surface that challenged the model of a single biosynthetic pathway for all members of this lipid class. For example, genetically obese (ob/ob) mice showed elevated hypothalamic levels of anandamide, but not other NAEs. (144) Similarly, stimulation of astrocytes with the calcium ionophore ionomycin led to elevations in anandamide and other polyunsaturated NAEs but not the saturated and monounsaturated NAEs PEA and N-oleoyl ethanolamine (OEA), respectively. (145) Finally, in vivo microdialysis studies have recorded elevations in extracellular anandamide in the brain in response to depolarizing stimuli without observed changes in the concentrations of PEA or OEA. (146) Collectively, these studies point to the potential existence of distinct enzymatic pathways for the biosynthesis of anandamide (and other polyunsaturated NAEs) compared with saturated and monounsaturated NAEs. A more direct test of this premise was afforded by the generation and characterization of mice lacking the NAPE-PLD gene.
Leung and colleagues created NAPE-PLD(−/−) mice by standard targeted disruption procedures, where exon 4 encoding amino acids 98–313 (including the conserved HXHXDH catalytic motif) was deleted. (147) NAPE-PLD(−/−) mice were viable and healthy and displayed normal cage behavior. Western blotting confirmed the loss of NAPE-PLD protein in these animals, which correlated with a nearly 5-fold decrease in NAPE-PLD activity in brain tissue as measured by a standard substrate assay. Interestingly, however, liquid chromatography–mass spectrometry (LC-MS) analysis of lipid extracts from brain tissue of NAPE-PLD(+/+) and (−/−) mice revealed that deletion of NAPE-PLD affected a specific subset of endogenous NAEs. NAEs bearing saturated and monounsaturated acyl chains were significantly decreased in NAPE-PLD(−/−) mice, and these reductions were largest in magnitude for NAEs bearing very long acyl chains (>C20). In contrast, polyunsaturated NAEs, including anandamide, were unaltered in NAPE-PLD(−/−) mice. Complementary changes were observed in brain levels of NAPEs in NAPE-PLD(−/−) mice. NAPEs bearing saturated and monounsaturated N-acyl chains were elevated in these animals, while those bearing polyunsaturated N-acyl chains were mostly unaltered.
Initial characterization of NAPE-PLD(−/−) mice has thus provided further evidence to support the existence of multiple biosynthetic pathways for NAEs in the nervous system. These pathways appear to show distinct substrate selectivities, with NAPE-PLD serving as the principal regulator of long-chain saturated/monounsaturated NAEs and an alternative pathway(s) controlling the production of polyunsaturated NAEs such as anandamide. The modest but significant decreases observed for shorter chain saturated and monounsaturated NAEs in NAPE-PLD(−/−) mice suggest that these lipids may be regulated by both NAPE-PLD-dependent and NAPE-PLD-independent pathways.
3.2 Characterization of NAPE-PLD-Independent Pathways for the Biosynthesis of NAEs
3.2.1 A Pathway for NAE Biosynthesis Proceeding through a Glycerophospho-NAE Intermediate
In their original analysis of candidate pathways for the biosynthesis of NAEs, Schmid and colleagues noted the possibility that conversion of NAPEs to NAEs could involve additional intermediates where the sn-1 or sn-2 O-acyl chains of NAPEs or both were first hydrolyzed to generate lyso-NAPEs and glycerophospho (GP)-NAEs, respectively (148) (Figure 10, steps C and D). Cleavage of the phosphodiester bond of these intermediates would then generate NAEs (Figure 10, step E). Considering that the NAPE-PLD enzyme shows very limited activity toward lyso-NAPEs or GP-NAEs as substrates, (149) biosynthetic pathways proceeding through these intermediates would presumably involve a distinct set of enzymes. Schmid and colleagues provided preliminary evidence for phospholipase A1/A2 activities in dog brain that accepted NAPEs (and lyso-NAPEs) as substrates. (148) Later, Ueda and colleagues identified a secreted phospholipase A2 that converted NAPEs to lyso-NAPEs in vitro; (150) however, this enzyme is predominantly expressed in peripheral tissues, indicating that it is unlikely to make major contributions to NAE biosynthesis in the nervous system.
Considering that the cellular hydrolysis of phospholipid O-acyl chains is commonly mediated by serine hydrolases, Simon and Cravatt tested whether inhibitors of this enzyme family would block the conversion of NAPEs to NAEs in brain tissue from NAPE-PLD(+/+) and (−/−) mice. (151) The general serine lipase inhibitor MAFP reduced the residual NAE biosynthetic activity in NAPE-PLD(−/−) brains by more than 80%. Notably, MAFP treatment also blocked ~60% of the conversion of NAPEs to NAEs in NAPE-PLD(+/+) brains, indicating that a substantial fraction of this activity in the wild-type nervous system occurs through a serine hydrolase-mediated pathway. The authors provided additional evidence that this pathway involves double-deacylation of NAPEs to generate GP-NAEs, which are then converted by an EDTA-sensitive phosphodiesterase activity to NAEs.
Simon and Cravatt next employed the functional proteomic technology ABPP to isolate and identify the previously uncharacterized serine hydrolase α/β-hydrolase-4 (Abh4 or ABHD4) as an NAPE-selective lipase. ABHD4 is broadly expressed in mouse tissues with highest levels being found in the nervous system and testis. Interestingly, the enzyme proved capable of hydrolyzing both NAPEs and lyso-NAPEs, indicating that it may catalyze both O-deacylation steps en route to generating GP-NAEs. ABHD4 accepted a wide range of lyso-NAPE substrates, including the anandamide precursor N-arachidonoyl lyso-NAPE. In contrast, the enzyme showed no activity with other lysophospholipid substrates, including lyso-PE, lyso-phosphatidylcholine, and lyso-phosphatidylserine. Collectively, these findings support the existence of an NAPE-PLD-independent route for the conversion of NAPEs to NAEs proceeding through a GP-NAE intermediate and designate ABHD4 as a candidate (lyso)NAPE-lipase involved in this pathway.
3.2.2 A Pathway for NAE Biosynthesis Proceeding through a Phospho-NAE Intermediate
Kunos and colleagues have recently described a third potential pathway for NAE biosynthesis that involves the phospholipase C-dependent conversion of NAPEs to phospho-NAEs, followed by phosphatase-mediated hydrolysis of these intermediates to generate NAEs (152, 153) (Figure 10, steps F and G). This pathway has been most thoroughly characterized in macrophages, where the authors first noted that disruption of NAPE-PLD expression by RNA-interference (RNAi) failed to block bacterial endotoxin (LPS)-induced biosynthesis of anandamide. (152) LPS treatment instead induced the expression of PTPN22, a nonreceptor tyrosine phosphatase predominantly expressed in immune cells. The authors then showed that PTPN22 could convert phospho-anandamide to anandamide, providing a candidate enzyme responsible for the second step of the PLC-phosphatase pathway for converting NAPEs to NAEs. Consistent with a role for PTPN22 in anandamide biosynthesis, overexpression of this enzyme in macrophages resulted in a 2-fold increase in anandamide levels. Finally, LC-MS techniques were used to identify the phospho-anandamide precursor as an endogenous constituent of macrophages, as well as rodent brain tissue. More recently, Kunos and colleagues have provided in vitro evidence that the PLC-phosphatase pathway may contribute to stimulated, on-demand production of anandamide in the nervous system. (153) However, the nearly equivalent levels of anandamide observed in brain tissue from PTPN22(+/+) and (−/−) mice would argue that alternative phosphatases are likely involved in this pathway in the nervous system.
3.3 Summary and Key Outstanding Questions
The discovery of multiple pathways for the biosynthesis of NAEs challenges the model that all members of this lipid family are produced by a common enzymatic route. Instead, distinct pathways appear to exist for the biosynthesis of long-chain saturated/monounsaturated NAEs and polyunsaturated NAEs, with the former set of lipids being produced in an NAPE-PLD-dependent manner and the latter being generated by an alternative mechanism. This division of labor may allow cells in the nervous system (and peripheral tissues) to produce anandamide without generating other bioactive NAEs, such as PEA and OEA (and vice versus). A provocative corollary to this model is that selective inhibitors of the different NAE biosynthetic pathways could be used to block the production of distinct subsets of bioactive NAEs.
Many critical questions about anandamide biosynthesis remain unanswered. First and foremost, it is unclear which, if any, of the alternative pathways described to date is responsible for anandamide biosynthesis in the nervous system. Answers to this question will require the development of selective genetic or pharmacological tools to perturb the function of candidate anandamide biosynthetic enzymes in vivo. None of the currently available inhibitors of the ABHD4/phosphodiesterase and PLC/phosphatase pathways display sufficient selectivity for this purpose. Ultimately, it will be critical to determine whether anandamide biosynthesis in the nervous system is mediated by a single dedicated pathway or, alternatively, regulated by multiple enzymatic routes. In the latter case, bulk measurements of this lipid in whole tissue extracts, as has been typically performed to date, may obscure the contribution made by individual enzymes that regulate anandamide in select neuronal circuits or anatomical regions of the brain. From a more mechanistic perspective, it is also not yet apparent how any of the alternative pathways might selectively regulate the production of anandamide and other polyunsaturated NAEs. In the cases where substrate selectivity has been examined (e.g., ABHD4), the participating enzymes appear to accept a wide range of NAE precursors. Here, again, coupling of enzymatic pathways to specific NAE substrates may reflect colocalization of these biomolecules to discrete cellular or subcellular sites in the nervous system.
Finally, each of the proposed routes for anandamide/NAEs still points to NAPEs as the likely precursor lipids. Molecular characterization of the CDTA enzyme that generates NAPEs therefore remains of paramount importance. A calcium-independent transacylase has recently been characterized, (154) but this enzyme’s biochemical properties and tissue distribution argue against it serving as the CDTA activity responsible for generating NAPEs in the nervous system. Considering that calcium serves as a nearly universal second messenger throughout the nervous system, the CDTA enzyme likely represents a key regulatory node to integrate endocannabinoid signaling with other neurotransmitter systems in vivo.
4 Enzymatic Degradation of the Endocannabinoid 2-AG
The signaling function of 2-AG, like anandamide, is terminated by enzymatic hydrolysis (Figure 11). The structural similarity of anandamide and 2-AG initially suggested that these endocannabinoids might be regulated by the same hydrolytic enzyme(s). Potentially consistent with this premise, FAAH has been shown to hydrolyze both anandamide and 2-AG at similar rates. (155) However, the rate of monoacylglycerol hydrolysis in brain extracts is nearly 2 orders of magnitude greater than the rate of hydrolysis of NAEs, (156) which suggests that enzyme(s) other than FAAH are predominantly responsible for regulating 2-AG degradation in the nervous system. Also in support of this idea, the 2-AG and anandamide hydrolysis activities in pig brain extracts can be physically separated by chromatographic procedures. (34) Finally, genetic or pharmacological inactivation of FAAH fails to alter the endogenous levels or extent of hydrolysis of 2-AG and other monoacylglycerides in brain tissue. (53, 71, 156) Here, we review our current state of understanding of enzymes that hydrolyze 2-AG in the nervous system.
Figure 11.
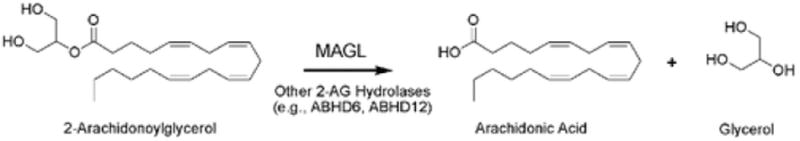
Enzymatic hydrolysis of 2-AG to arachidonic acid and glycerol catalyzed by MAGL and other hydrolases (e.g., ABHD6, ABHD12).
4.1 Monoacylglycerol Lipase As a Principal 2-AG Hydrolase in the Nervous System
In considering candidate enzymes responsible for degrading 2-AG in the nervous system, Dinh and colleagues have postulated a role for monoacylglycerol lipase (MAGL) in this process. (67) MAGL is a serine hydrolase originally purified and cloned from adipose tissue, (157) where it is thought to catalyze the final step of triglyceride metabolism. Dinh and colleagues showed that MAGL is also abundantly expressed in the nervous system, (67) where the enzyme localizes to presynaptic terminals of neurons that often express CB1 receptors. (35) Stella and colleagues have shown that MAGL is also expressed by astrocytes. (158)
More direct functional evidence for the involvement of MAGL in 2-AG hydrolysis has also been obtained. Piomelli and colleagues have shown that overexpression of MAGL in rat cortical neurons reduced the activity-dependent accumulation of 2-AG, (67) and RNA-interference-mediated knockdown of MAGL in HeLa cells significantly reduces 2-AG hydrolysis and elevates 2-AG levels in these cells. (159) These authors have also shown that immunodepletion of MAGL from rat brain fractions decreased 2-AG hydrolysis by ~50%. (159) Saario and colleagues have similarly demonstrated that treatment of rat cerebellar membranes with N-arachidonyl maleimide (NAM) (Figure 12), an irreversible inhibitor of MAGL, decreases 2-AG hydrolysis by ~85%. (160)
Figure 12.
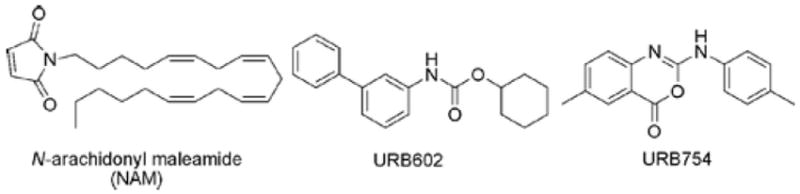
Reported MAGL inhibitors. Note that URB754 has since been shown not to inhibit MAGL.
Additional MAGL inhibitors, designated URB602 and URB754 (Figure 12), have been reported by Piomelli and colleagues to raise brain 2-AG levels and produce antihyperalgesic effects in rodents. (78, 161) However, the efficacy and selectivity of these inhibitors have since been called into question. Subsequent studies by Piomelli and others have failed to observe inhibition of MAGL by URB754. (162, 163) The original batch of this compound was apparently contaminated with a mercuric impurity that accounted for the inhibition of MAGL. URB602, which acts as a weak noncompetitive inhibitor of MAGL, has also been shown by multiple groups to inhibit FAAH with nearly equivalent potency. (164, 165) Finally, a recent study used the inhibitors MAFP and arachidonoyl trifluoromethyl ketone to indicate a role for MAGL in regulating retrograde endocannabinoid signaling in hippocampal neuronal cultures. (166) Both of these agents, however, are rather broad-spectrum inhibitors of serine hydrolases, making it difficult to ascribe their effects to a single enzyme from this class (especially when one considers that the brain proteome possesses more than 30 distinct serine hydrolases (167)).
Collectively the aforementioned studies indicate that MAGL is likely a major contributor to 2-AG hydrolysis in the nervous system. Confirmation of this hypothesis, however, requires specific experimental tools to perturb the function of MAGL in vivo. To our knowledge, MAGL(−/−) mice have not yet been generated. Additionally, the generation of selective and efficacious inhibitors of MAGL has proven, so far, to be a challenging and elusive goal. Toward this end, a more detailed understanding of the structure of MAGL would be of value. Recent reports of recombinant expression systems that yield high quantities of purified MAGL (168) should facilitate future biophysical and structural studies of the enzyme.
4.2 Additional Enzymes That Hydrolyze 2-AG in the Nervous System
Although much of the focus on 2-AG degradation has been devoted to MAGL, several lines of evidence have recently emerged to support the existence of additional enzymes that contribute to 2-AG hydrolysis. First, brain membrane extracts retain approximately 15–20% residual 2-AG hydrolysis activity following treatment with concentrations of NAM that completely block MAGL. (160, 167) Similarly, immunodepletion of MAGL from brain homogenates removes essentially all MAGL protein (as detected by Western blotting) but only reduces 2-AG hydrolase activity in these samples by ~50%. (159) Most recently, Mucciooli and colleagues reported substantial 2-AG hydrolase activity in the BV-2 microglial cell line, which does not express detectable levels of MAGL. (165) The authors further showed that only 40% of the BV-2 2-AG hydrolase activity could be attributed to FAAH, pointing to the existence of an additional 2-AG hydrolase(s) in these cells.
Inspired by the aforementioned studies, Blankman and colleagues took a functional proteomic approach to globally inventory enzymes in mouse brain that possess 2-AG hydrolase activity. (167) The rationale for this study was based on the initial finding that more than 98% of brain 2-AG hydrolase activity can be blocked by the ABPP probe fluorophosphonate–biotin (FP–biotin (94)). This result indicated that essentially all of the brain 2-AG hydrolase activity is catalyzed by enzymes from the serine hydrolase class. The full complement of FP–biotin-labeled serine hydrolases in mouse brain was then enriched and identified by the shotgun LC-MS method ABPP-MudPIT. (169) The resulting 32 brain serine hydrolases were individually expressed in COS-7 cells and assayed for 2-AG hydrolase activity.
Several brain serine hydrolases were found to convert 2-AG to arachidonic acid, including enzymes previously reported to display monoacylglycerol hydrolysis activity [MAGL, FAAH, neuropathy-target esterase (NTE), (170) hormone-sensitive lipase (171)], as well as two uncharacterized proteins α/β-hydrolase-6 (ABHD6) and α/β-hydrolase 12 (ABHD12). Normalization of the measured activities to the expression level of each hydrolase in mouse brain (as judged by spectral counts from ABPP-MudPIT data sets) assigned ~85% of the total brain 2-AG hydrolysis activity to MAGL, with the remaining 15% being mostly catalyzed by ABHD12 and ABHD6. Interestingly, MAGL, ABHD12, and ABHD6 were found to display different subcellular distributions (Figure 13), suggesting that they could control distinct pools of 2-AG in the nervous system. These findings confirm that MAGL is the principal 2-AG hydrolase in mammalian brain tissue but also point to additional enzymes that may participate in the process.
Figure 13.
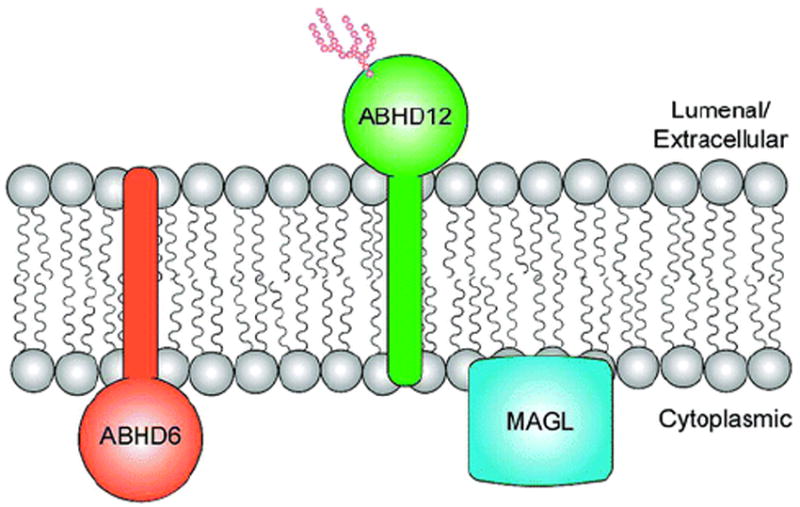
Three prominent 2-AG hydrolases in the nervous system, MAGL, ABHD6, and ABHD12, have different subcellular distributions, suggesting that they could degrade distinct pools of 2-AG.
4.3 Summary and Key Outstanding Questions
The remarkably rapid rate at which 2-AG is hydrolyzed in brain extracts suggests that this endocannabinoid is under tight regulation in vivo. Multiple lines of evidence indicate that MAGL is the principal 2-AG hydrolase in brain homogenates. Discerning the role that MAGL plays in regulating 2-AG degradation in vivo awaits the development of selective genetic and pharmacological tools to perturb the function of this enzyme. Given the high likelihood that MAGL is an important regulator of 2-AG signaling in vivo, it is hard to imagine that considerable effort has not already been put forth to develop potent and selective inhibitors of this enzyme. The fact that such agents are still lacking implies that MAGL might pose a more challenging target for inhibitor development compared with other serine hydrolases, such as FAAH, for which numerous efficacious and selective inhibitors have been described. Future efforts to develop MAGL inhibitors would certainly benefit from a more detailed understanding of the enzyme’s three-dimensional structure. Considering that high quantities of active, recombinant MAGL protein can be produced in bacteria, (168) a crystal structure of the enzyme seems like an achievable goal in the not too distant future.
In addition to MAGL, several other enzymes expressed in the nervous system have been found to possess 2-AG hydrolase activity, including FAAH, NTE, ABHD6, and ABHD12. The latter two enzymes, in particular, appear to make substantial contributions to the 2-AG hydrolase activity in brain tissue. Whether any of these enzymes is involved in 2-AG degradation in vivo is presently unclear, but multiple pieces of evidence suggest that they may play a role in this process. First, the three major 2-AG hydrolases in mouse brain, MAGL, ABHD12, and ABHD6, display different subcellular distributions, suggesting that they could access and regulate distinct pools of 2-AG. It is becoming increasingly clear that such pools likely exist in the nervous system. Indeed, bulk levels of 2-AG in brain tissue vastly exceed the extracellular concentrations of this endocannabinoid, as measured by in vivo microdialysis. (17, 18) These findings suggest that only a small fraction of the total quantity of 2-AG in the nervous system may be “signaling competent”. A major area for future investigation is consequently to determine which enzymes regulate bulk versus signaling pools of 2-AG.
A second compelling piece of data that invokes the participation of multiple enzymes in the hydrolysis of 2-AG derives from studies of non-neuronal cells. Specifically, Muccioli and colleagues have shown that 2-AG is hydrolyzed by a membrane-associated enzyme activity(ies) distinct from MAGL in BV2 microglial cells. (165) It will be interesting to determine whether this activity is due to one or more of the additional 2-AG hydrolases described above. More generally, the identification of MAGL-independent pathways for 2-AG hydrolysis should motivate researchers to explore the full complement of 2-AG hydrolases in a number of cells and tissues.
Finally, it also important to note that, while the primary route for 2-AG degradation appears to occur via enzymatic hydrolysis, alternative pathways may also participate in the regulation of this endocannabinoid. For example, 2-AG is a substrate for cyclooxygenase-2 (COX2), which converts this endocannabinoid to prostaglandin esters, (172) and some pharmacological data support a role for COX2 in regulating 2-AG signaling in specific neural circuits. (173, 174)
5 Enzymatic Biosynthesis of the Endocannabinoid 2-AG
Over the past several years, substantial attention has been given to mapping the enzymatic pathways for 2-AG biosynthesis in the nervous system. Much of this interest stems from the emerging recognition that 2-AG appears to represent the principal endocannabinoid involved in many of the CB1-dependent forms of neural plasticity characterized in neuronal slice and culture preparations. (11, 12) In neurons, 2-AG appears to be biosynthesized by at least three distinct multistep enzymatic pathways: (1) calcium-dependent endocannabinoid release (CaER), where endocannabinoid production is activated by calcium elevations alone; (2) receptor-regulated endocannabinoid release (RER), where endocannabinoid production is driven by activation of Gq/11-coupled receptors; and (3) calcium-assisted RER, where calcium and receptor activation synergize to stimulate endocannabinoid production (175) (Figure 14). Although the specific enzymes involved in each of these pathways have not yet been fully elucidated, they appear to share the same final step, the hydrolysis of diacylglyerol (DAG) to generate 2-AG. Here, we will first review progress that has been made toward characterizingsn-1-selective DAG lipases involved in this final step. We will then discuss the potential upstream enzymatic steps implicated in generating DAG in the CaER and RER pathways for 2-AG biosynthesis.
Figure 14.
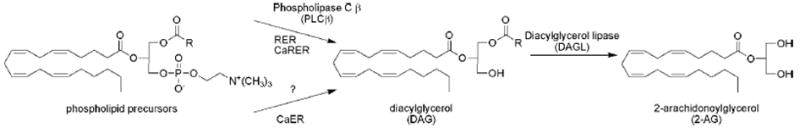
Enzymatic biosynthesis of 2-AG. Receptor-regulated endocannabinoid release (RER) and calcium-assisted RER (CaRER) employ a phospholipase C β (PLCβ)-dependent pathway to convert phospholipid precursors to diacylglycerol (DAG). The source of DAG for calcium-dependent endocannabinoid release (CaER) is currently unknown. Both pathways intersect with the formation of DAG, which is then converted to 2-AG precursors by diacylglycerol lipases (DAGL-α and -β).
5.1 A Family of sn-1-Selective DAG Lipases That Produce 2-AG
In a seminal study, Bisogno and colleagues described the molecular characterization of an unusual set of transmembrane serine hydrolases that selectively cleave the sn-1 acyl chains from DAGs to generate 2-AG. (176) These two enzymes, now referred to as DAGL-α and -β, were identified based on a clever bioinformatic search for mammalian homologues of known bacterial DAGLs. DAGL-α and -β share a similar predicted membrane topology, with four predicted transmembrane domains followed by a catalytic domain that conforms to the general sequence requirements for a serine hydrolase (including the presence of the canonical GXSXG active site motif). Both enzymes are highly enriched in the brain but show different developmental expression patterns. DAGL-β is expressed primarily in early development, while DAGL-α expression is sustained in adult brain. Interestingly, the subcellular distribution of these enzymes also displays an unusual shift from predominantly presynaptic (axonal) to postsynaptic (somatodendritic) compartments as neurons mature. Immunohistochemical and immuno-electron microscopy studies have further revealed that DAGL-α is enriched on postsynaptic structures (e.g., dendritic spines) adjacent to axon terminals expressing CB1 receptors in multiple regions of the brain. (177-179)
Multiple additional lines of evidence suggest that DAGL-α/β play a role in regulating 2-AG biosynthesis in neurons. In their initial characterization of DAGL-α/β, Bisogno and colleagues found that these enzymes were inhibited by two small-molecule agents, RHC80267 and tetrahydrolipstatin (THL) (176, 180) (Figure 15). These agents have since gained considerable popularity as pharmacological tools to evaluate contribution of DAGL-α and -β to endocannabinoid signaling in neuronal preparations. Several reports have described that RHC80267 and THL block many of the CB1-dependent forms of neuronal plasticity observed in in vitro preparations [e.g., long-term depression (LTD), depolarization-induced suppression of inhibition (DSI), depolarization-induced suppression of excitation (DSE)]. (179, 181-184) While these findings certainly suggest a role for DAGL-α and -β and, by extension, 2-AG in mediating these cellular events, a cautionary note should be raised about the selectivity of RHC80267 and THL. These agents presumably operate by covalent reaction with the serine nucleophile of DAGL-α and -β (forming carbamoylated and esterified products, respectively), which immediately raises concerns about whether they might target additional serine hydrolases in the nervous system via a similar mechanism. This is certainly the case in peripheral tissues, where, for example, THL has found wide clinical utility as antiobesity agent due to blockade of pancreatic lipases in the intestine. (185)
Figure 15.
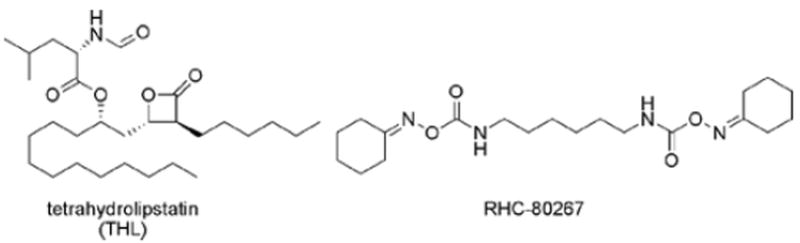
Representative DAGLα and -β inhibitors.
Further adding to the complexity of using RHC80267 and THL as probes of DAGL-α/β function are the recent findings reported by Kano, Alger, and colleagues that RHC80267 was ineffective at blocking CB1-dependent pathways activated by Gq/11-coupled receptors in hippocampal cultures or slices. (183, 184) Bisogno and colleagues have reported similarly perplexing results with a new set of DAGL-α and -β inhibitors that failed to block ionomycin-induced 2-AG production in cultured cells. (186) How these results should be interpreted is open to debate, but they do raise the possibility that DAGL-α and -β independent pathways for 2-AG biosynthesis may exist in certain neuronal circuits.
Fortunately, the evidence in support of DAGL-α as a regulator of 2-AG biosynthesis in neurons has not been restricted to pharmacological studies using enzyme inhibitors. Jung and colleagues have shown that overexpression of DAGL-α in the mouse neuroblastoma cell line Neuro-2a results in a significant increase in basal 2-AG levels. (187) Elevated 2-AG levels correlated with a decrease in 1-stearoyl-2-arachidonoyl glycerol, suggesting that this DAG may serve as the principal source of 2-AG in Neuro-2a cells. The authors further demonstrated that RNA interference-mediated knockdown of DAGL-α in Neuro-2a cells reduced basal levels of 2-AG and blocked the production of this endocannabinoid stimulated by agonists of group 1 metabotropic glutamate receptors. Additionally, the DAGL-α and -β inhibitor RHC80267 blocks 2-AG accumulation in brain slice cultures induced by agonists of metabotropic glutamate receptors. (188) Collectively, these findings support a role for DAGL-α and -β in both basal and Gq/11-receptor-activated pathways for 2-AG biosynthesis.
5.2 Candidate Enzymatic Pathways Generating the 2-AG Precursor DAG in the Nervous System
As mentioned above, pathways for 2-AG biosynthesis appear to diversify at the steps upstream of formation of DAG. Hashimotodani and colleagues have shown that both RER and calcium-assisted RER are dependent on phospholipase C-β (PLCβ), (175, 189) indicating that the 2-AG generated as part of these signaling pathways derives from a two-step pathway involving, first, the PLCβ-catalyzed release of DAG from phospholipid precursors, followed by the DAGL-mediated conversion of DAG to 2-AG precursors (Figure 14). PLCβ is a particularly interesting enzyme in this pathway because it is stimulated by both Gq/11-coupled receptors and calcium, which enables the protein to serve as a “coincidence detector” for these two signals. This calcium-assisted RER may represent the most physiologically relevant mechanism for 2-AG production because it requires a more modest elevation in calcium than pure CaER.
The source of DAG for CaER, which is thought to represent the major form of endocannabinoid production leading to DSI/DSE, remains enigmatic. Hashimotodani and colleagues recently reported that DSI/DSE is unperturbed in neuronal preparations from PLCβ or PLCδ mice. (184) Although there are still other PLC isoenzymes that could prove responsible for generating DAG in CaER, alternative pathways for endocannabinoid production should be considered, especially considering that DAGLα and -β inhibitors have also shown variable effects on DSI/DSE. (183, 184)
5.3 Summary and Key Outstanding Questions
Substantial progress has been made in our understanding of the enzymatic pathways that generate 2-AG in the nervous system. The molecular characterization of two DAGL enzymes (α and β) that convert DAG to 2-AG represents a major breakthrough, providing targets for future genetic and pharmacological studies aimed at selectively disrupting 2-AG production in vivo. The current set of available DAGL-α and -β inhibitors, such as RHC80267 and THL, do not appear to be sufficiently efficacious or selective for in vivo studies. It is also difficult to interpret recent findings where one but not both of these inhibitors blocks putative endocannabinoid-mediated forms of synaptic plasticity. Does this reflect the failure of the inactive agent to inhibit DAGL-α and -β specific neuronal preparations or, alternatively, the blockade of additional enzymatic targets by the active compound? One could raise similar concerns about the selectivity of PLC inhibitors, which exert deleterious effects on neuronal activity that have precluded their use in certain physiological studies. (184)
As selective tools emerge to probe DAGL-α and -β in vivo, it will be interesting to elucidate the contribution made by these enzymes to bulk levels versus signaling (i.e., CaER/RER-stimulated) pools of 2-AG. Preliminary studies in neurons suggest that DAGL-α and -β may regulate both forms of 2-AG in neurons. (187) These studies also have provided evidence that DAGL-α controls DAG levels in neurons, which indicates that blockade of this enzyme could affect signaling pathways outside of the endocannabinoid system (e.g., phosphorylation cascades catalyzed by protein kinase C, which is activated by DAG). Finally, the relative contribution of DAGL-α and -β to 2-AG production in the nervous system, as well as the possible involvement of other biosynthetic pathways (e.g., the proposed phospholipase A1–lysophospholipase C route (21)), remains largely unexplored. Alternative pathways could also play a significant role in 2-AG biosynthesis in peripheral tissues, many of which express low levels of DAGL-α and -β.
6 Conclusion
Here, we have attempted to review the current state of our understanding of the four major pathways for endocannabinoid metabolism: (1) anandamide degradation, (2) anandamide biosynthesis, (3) 2-AG degradation, and (4) 2-AG biosynthesis. Some of these pathways, such as anandamide degradation, are relatively well characterized, at least in terms of the participating enzymes and the advent of specific research tools to probe their function in vivo. For other pathways, candidate enzymes have been identified, but the specific roles that these proteins play in regulating endocannabinoid metabolism in vivo remains to be elucidated. Although each endocannabinoid metabolic pathway presents a unique set of experimental opportunities and challenges, which have been detailed in the separate sections presented above, common themes can also be culled from a global review of research into their composition and regulation.
One theme that warrants mention is the strong correlation between the extent of understanding of a specific metabolic pathway and the quality of genetic and pharmacological tools available to probe its function. In the case of anandamide degradation, knockout mice and selective inhibitors have assigned a principal role to FAAH. These research tools have in turn revealed roles for FAAH-regulated anandamide in a range of neurophysiological processes, including pain sensation, inflammation, anxiety, and depression. Since candidate enzymes have now been identified for the three major endocannabinoid metabolic pathways, we anticipate that selective tools to study their function will soon emerge.
A second theme relates the molecular events that occur between endocannabinoid production and degradation. We currently understand very little about how endocannabinoids move from their sites of biosynthesis to their sites of action and eventually to their sites of degradation. Transport proteins have been described but await molecular characterization. Original models for the cellular uptake of endocannabinoids invoked the existence of a plasma membrane transporter, a model that was largely based on mechanisms for the uptake of more classical, hydrophilic transmitters (e.g., monoamines). As our understanding of the unusual physicochemical properties of endocannabinoids has matured, other types of proteins have been proposed that might transport these hydrophobic lipids between aqueous compartments either within or outside the cell. Although the identity of such putative endocannabinoid-binding proteins remains enigmatic, the huge number of lipid-binding proteins present in mammalian proteomes argues strongly for their existence.
A final theme is the discrimination of specific physiological functions for anandamide and 2-AG. Simply put, why are there two classes of endocannabinoids? Do anandamide and 2-AG activate CB1 receptors in different neural circuits, or alternatively, might these two endocannabinoids also function within the same neural pathways but display distinct signaling kinetics (as has been recently suggested for circuits that regulate stress-induced analgesia (78))? Either model is attractive because it invokes a mechanism for regulating specific endocannabinoid pathways within the nervous system. Indeed, with a single receptor abundantly expressed in the nervous system (CB1), the endocannabinoid system may differ from more classical neurotransmitter pathways, which often achieve diversification of signaling by implementing several receptor subtypes.
Although it is still too early to ascribe specific functions to anandamide versus 2-AG in vivo, physiological studies using in vitro neuronal preparations have more consistently invoked a role for 2-AG in the regulation of synaptic plasticity. On the other hand, the disruption of FAAH activity has provided strong evidence that anandamide-mediated pathways are involved in the control of select behavioral processes in vivo. When one further considers that the bulk tissue levels of 2-AG exceed those of anandamide by 2 orders of magnitude, it is perhaps enticing to suggest that 2-AG may represent the “workhorse” endocannabinoid in the nervous system, while anandamide is utilized in a more select number of neural circuits. This model is not entirely supported by recent in vivo microdialysis studies, which have shown that the large differences in tissue levels of 2-AG and anandamide are not reflective of their extracellular concentrations. (17, 18) Regardless, from a translational perspective, differences in the endogenous modes of signaling for anandamide and 2-AG could provide unique therapeutic opportunities. For instance, elevations in anandamide signaling by FAAH inhibition have been found to produce analgesia, anxiolysis, antidepression, and anti-inflammation, without the gross alterations in motility or cognition that are observed with direct CB1 agonists. We eagerly await the emergence of selective inhibitors for additional endocannabinoid pathways, which should uncover new physiological functions and biomedical prospects for this fascinating lipid signaling system.
Acknowledgments
We gratefully acknowledge the support of the NIH (Grants DA015197 and DA017259), the Helen L. Dorris Institute for the Study of Neurological and Psychiatric Disorders in Children and Adolescents, and the Skaggs Institute for Chemical Biology.
Biographies
Kay Ahn studied Chemistry (B.S.) at Yonsei University in Seoul, South Korea, and received her Ph.D. in Chemistry from The Ohio State University. She was a Postdoctoral fellow with Judith Klinman at University of California at Berkeley and with Arthur Kornberg at Stanford University. She joined Parke-Davis/Pfizer in 1990 and is currently a Research Fellow at Pfizer. She has been involved in several enzyme target drug discovery programs at Pfizer including the most recent FAAH inhibitor discovery project.
Michele McKinney studied biology and chemistry (B.S.) at Gordon College in Wenham, Massachusetts. She then completed graduate studies under the direction of B. Cravatt at The Scripps Research Institute and received her Ph.D. in 2006. She has remained in the Cravatt lab as a postdoctoral fellow, continuing research into endocannabinoid-terminating enzymes.
Benjamin Cravatt obtained his undergraduate education at Stanford University, receiving a B.S. in the Biological Sciences and a B.A. in History. He then trained with Drs. Dale Boger and Richard Lerner and received a Ph.D. in Macromolecular and Cellular Structure and Chemistry from The Scripps Research Institute (TSRI) in 1996. Professor Cravatt joined the faculty at TSRI in 1997 as a member of the Skaggs Institute for Chemical Biology and the Department of Chemical Physiology. His research group is interested in developing and applying new technologies to elucidate the roles that enzymes play in physiological and pathological processes, especially as pertains to the nervous system and cancer.
References
- 1.Siegel GJ, Agranoff BW, Albers RW, Molinoff PB. Basic Neurochemistry. Raven Press; New York: 1994. [Google Scholar]
- 2.Mechoulam R. The Pharmacohistory of Cannabis sativa. CRC Press; Boca Raton, FL: 1986. [Google Scholar]
- 3.Mackie K. Annu Rev Pharmacol Toxicol. 2006;46:101. doi: 10.1146/annurev.pharmtox.46.120604.141254. [DOI] [PubMed] [Google Scholar]
- 4.Ledent C, Valverde O, Cossu G, Petitet F, Aubert JF, B F, Bohme GA, Imperato A, Pedrazzini T, Roques BP, Vassart G, Fratta W, Parmentier M. Science. 1999;283:401. doi: 10.1126/science.283.5400.401. [DOI] [PubMed] [Google Scholar]
- 5.Zimmer A, Zimmer AM, Hohmann AG, Herkenham M, Bonner TI. Proc Natl Acad Sci U S A. 1999;96:5780. doi: 10.1073/pnas.96.10.5780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lunn CA, Reich EP, Bober L. Expert Opin Ther Targets. 2006;10:653. doi: 10.1517/14728222.10.5.653. [DOI] [PubMed] [Google Scholar]
- 7.Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R. Science. 1992;258:1946. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 8.Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, Gopher A, Almog S, Martin BR, Compton DR. Biochem Pharmacol. 1995;50:83. doi: 10.1016/0006-2952(95)00109-d. [DOI] [PubMed] [Google Scholar]
- 9.Sugiura T, Kondo S, Sukagawa A, Nakane S, Shinoda A, Itoh K, Yamashita A, Waku K. Biochem Biophys Res Commun. 1995;215:89. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- 10.Di Marzo V, Bisogno T, De Petrocellis L. Chem Biol. 2007;14:741. doi: 10.1016/j.chembiol.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Piomelli D. Nat Rev Neurosci. 2003;4:873. doi: 10.1038/nrn1247. [DOI] [PubMed] [Google Scholar]
- 12.Chevaleyre V, Takahashi KA, Castillo PE. Annu Rev Neurosci. 2006;29:37. doi: 10.1146/annurev.neuro.29.051605.112834. [DOI] [PubMed] [Google Scholar]
- 13.Egertova M, Giang DK, Cravatt BF, Elphick MR. Proc R Soc London Ser B. 1998;265:2081. doi: 10.1098/rspb.1998.0543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katona I, Sperlagh B, Sik A, Kafalvi A, Vizi ES, Mackie K, Freund TF. J Neurosci. 1999;19:4544. doi: 10.1523/JNEUROSCI.19-11-04544.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gonsiorek W, Lunn C, Fan X, Narula S, Lundell D, Hipkin RW. Mol Pharmacol. 2000;57:1045. [PubMed] [Google Scholar]
- 16.Shen M, Thayer SA. Mol Pharmacol. 1999;55:8. doi: 10.1124/mol.55.1.8. [DOI] [PubMed] [Google Scholar]
- 17.Caille S, Alvarez-Jaimes L, Polis I, Stouffer DG, Parsons LH. J Neurosci. 2007;27:3695. doi: 10.1523/JNEUROSCI.4403-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bequet F, Uzabiaga F, Desbazeille M, Ludwiczak P, Maftouh M, Picard C, Scatton B, Le Fur G, Eur J. Neurosci. 2007;26:3458. doi: 10.1111/j.1460-9568.2007.05900.x. [DOI] [PubMed] [Google Scholar]
- 19.Patricelli MP, Cravatt BF. Vitam Horm. 2001;62:95. doi: 10.1016/s0083-6729(01)62002-8. [DOI] [PubMed] [Google Scholar]
- 20.Lambert DM, Fowler CJ. J Med Chem. 2005;48:5059. doi: 10.1021/jm058183t. [DOI] [PubMed] [Google Scholar]
- 21.Sugiura T, Kishimoto S, Oka S, Gokoh M. Prog Lipid Res. 2006;45:405. doi: 10.1016/j.plipres.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Okamoto Y, Wang J, Morishita J, Ueda N. Chem Biodiversity. 2007;4:1842. doi: 10.1002/cbdv.200790155. [DOI] [PubMed] [Google Scholar]
- 23.Basavarajappa BS. Protein Pept Lett. 2007;14:237. doi: 10.2174/092986607780090829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKinney MK, Cravatt BF. Annu Rev Biochem. 2005;74:411. doi: 10.1146/annurev.biochem.74.082803.133450. [DOI] [PubMed] [Google Scholar]
- 25.Schmid PC, Zuzarte-Augustin ML, Schmid HH. J Biol Chem. 1985;260:14145. [PubMed] [Google Scholar]
- 26.Deutsch DG, Chin SA. Biochem Pharmacol. 1993;46:791. doi: 10.1016/0006-2952(93)90486-g. [DOI] [PubMed] [Google Scholar]
- 27.Desarnaud F, Cadas H, Piomelli D. J Biol Chem. 1995;270:6030. doi: 10.1074/jbc.270.11.6030. [DOI] [PubMed] [Google Scholar]
- 28.Ueda N, Kurahashi Y, Yamamoto S, Tokunaga T. J Biol Chem. 1995;270:23823. doi: 10.1074/jbc.270.40.23823. [DOI] [PubMed] [Google Scholar]
- 29.Hillard CJ, Wilkison DM, Edgemond WS, Campbell WB. Biochim Biophys Acta. 1995;1257:249. doi: 10.1016/0005-2760(95)00087-s. [DOI] [PubMed] [Google Scholar]
- 30.Cravatt BF, Prospero-Garcia O, Siuzdak G, Gilula NB, Henriksen SJ, Boger DL, Lerner RA. Science. 1995;268:1506. doi: 10.1126/science.7770779. [DOI] [PubMed] [Google Scholar]
- 31.Maurelli S, Bisogno T, De Petrocellis L, Di Luccia A, Marino G, Di Marzo V. FEBS Lett. 1995;377:82. doi: 10.1016/0014-5793(95)01311-3. [DOI] [PubMed] [Google Scholar]
- 32.Cravatt BF, Giang DK, Mayfield SP, Boger DL, Lerner RA, Gilula NB. Nature. 1996;384:83. doi: 10.1038/384083a0. [DOI] [PubMed] [Google Scholar]
- 33.Giang DK, Cravatt BF. Proc Natl Acad Sci U S A. 1997;94:2238. doi: 10.1073/pnas.94.6.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goparaju SK, Ueda N, Taniguchi K, Yamamoto S. Biochem Pharmacol. 1999;57:417. doi: 10.1016/s0006-2952(98)00314-1. [DOI] [PubMed] [Google Scholar]
- 35.Gulyas AI, Cravatt BF, Bracey MH, Dinh TP, Piomelli D, Boscia F, Freund TF. Eur J Neurosci. 2004;20:441. doi: 10.1111/j.1460-9568.2004.03428.x. [DOI] [PubMed] [Google Scholar]
- 36.Chebrou H, Bigey F, Arnaud A, Galzy P. Biochim Biophys Acta. 1996;1298:285. doi: 10.1016/s0167-4838(96)00145-8. [DOI] [PubMed] [Google Scholar]
- 37.Patricelli MP, Lashuel HA, Giang DK, Kelly JW, Cravatt BF. Biochemistry. 1998;37:15177. doi: 10.1021/bi981733n. [DOI] [PubMed] [Google Scholar]
- 38.Katayama K, Ueda N, Katoh I, Yamamoto S. Biochim Biophys Acta. 1999;1440:205. doi: 10.1016/s1388-1981(99)00124-9. [DOI] [PubMed] [Google Scholar]
- 39.Kage KL, Richardson PL, Traphagen L, Severin J, Pereda-Lopez A, Lubben T, Davis-Taber R, Vos MH, Bartley D, Walter K, Harlan J, Solomon L, Warrior U, Holzman TF, Faltynek C, Surowy CS, Scott VE. J Neurosci Methods. 2007;161:47. doi: 10.1016/j.jneumeth.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 40.Huang H, Nishi K, Tsai HJ, Hammock BD. Anal Biochem. 2007;363:12. doi: 10.1016/j.ab.2006.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bracey MH, Hanson MA, Masuda KR, Stevens RC, Cravatt BF. Science. 2002;298:1793. doi: 10.1126/science.1076535. [DOI] [PubMed] [Google Scholar]
- 42.Shin S, Lee TH, Ha NC, Koo HM, Kim SY, Lee HS, Kim YS, Oh BH. EMBO J. 2002;21:2509. doi: 10.1093/emboj/21.11.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Labahn J, Neumann S, Buldt G, Kula MR, Granzin J. J Mol Biol. 2002;322:1053. doi: 10.1016/s0022-2836(02)00886-0. [DOI] [PubMed] [Google Scholar]
- 44.Patricelli MP, Cravatt BF. Biochemistry. 2001;40:6107. doi: 10.1021/bi002578r. [DOI] [PubMed] [Google Scholar]
- 45.Patricelli MP, Lovato MA, Cravatt BF. Biochemistry. 1999;38:9804. doi: 10.1021/bi990637z. [DOI] [PubMed] [Google Scholar]
- 46.Patricelli MP, Cravatt BF. J Biol Chem. 2000;275:19177. doi: 10.1074/jbc.M001607200. [DOI] [PubMed] [Google Scholar]
- 47.McKinney MK, Cravatt BF. J Biol Chem. 2003;278:37393. doi: 10.1074/jbc.M303922200. [DOI] [PubMed] [Google Scholar]
- 48.Patricelli MP, Cravatt BF. Biochemistry. 1999;38:14125. doi: 10.1021/bi991876p. [DOI] [PubMed] [Google Scholar]
- 49.Smith PB, Compton DR, Welch SP, Razdan RK, Mechoulam R, Martin BR. J Pharmacol Exp Ther. 1994;270:219. [PubMed] [Google Scholar]
- 50.Willoughby KA, Moore SF, Martin BR, Ellis EF. J Pharmacol Exp Ther. 1997;282:243. [PubMed] [Google Scholar]
- 51.Cravatt BF, Demarest K, Patricelli MP, Bracey MH, Giang DK, Martin BR, Lichtman AH. Proc Natl Acad Sci U S A. 2001;98:9371. doi: 10.1073/pnas.161191698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wise LE, Shelton CC, Cravatt BF, Martin BR, Lichtman AH. Eur J Pharmacol. 2007;557:44. doi: 10.1016/j.ejphar.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 53.Osei-Hyiaman D, Depetrillo M, Harvey-White J, Bannon AW, Cravatt BF, Kuhar MJ, Mackie K, Palkovits M, Kunos G. Neuroendocrinology. 2005;81:273. doi: 10.1159/000087925. [DOI] [PubMed] [Google Scholar]
- 54.Lichtman AH, Shelton CC, Advani T, Cravatt BF. Pain. 2004;109:319. doi: 10.1016/j.pain.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 55.Massa F, Marsicano G, Hermann H, Cannich A, Monory K, Cravatt BF, Ferri G-L, Sibaev A, Storr M, Lutz B. J Clin Inv. 2004;113:1202. doi: 10.1172/JCI19465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cravatt BF, Saghatelian A, Hawkins EG, Clement AB, Bracey MH, Lichtman AH. Proc Natl Acad Sci U S A. 2004;101:10821. doi: 10.1073/pnas.0401292101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karsak M, Gaffal E, Date R, Wang-Eckhardt L, Rehnelt J, Petrosino S, Starowicz K, Steuder R, Schlicker E, Cravatt B, Mechoulam R, Buettner R, Werner S, Di Marzo V, Tuting T, Zimmer A. Science. 2007;316:1494. doi: 10.1126/science.1142265. [DOI] [PubMed] [Google Scholar]
- 58.Naidu PS, Varvel SA, Ahn K, Cravatt BF, Martin BR, Lichtman AH. Psychopharmacology (Berlin) 2007;192:61. doi: 10.1007/s00213-006-0689-4. [DOI] [PubMed] [Google Scholar]
- 59.Moreira FA, Kaiser N, Monory K, Lutz B. Neuropharmacology. 2008;54:141. doi: 10.1016/j.neuropharm.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 60.Huitron-Resendiz S, Sanchez-Alavez M, Wills DN, Cravatt BF, Henriksen SJ. Sleep. 2004;27:857. doi: 10.1093/sleep/27.5.857. [DOI] [PubMed] [Google Scholar]
- 61.Varvel SA, Wise LE, Niyuhire F, Cravatt BF, Lichtman AH. Neuropsychopharmacology. 2007;32:1032. doi: 10.1038/sj.npp.1301224. [DOI] [PubMed] [Google Scholar]
- 62.Boger DL, Sato H, Lerner AE, Austin BJ, Patterson JE, Patricelli MP, Cravatt BF. Bioorg Med Chem Lett. 1999;9:265. doi: 10.1016/s0960-894x(98)00734-3. [DOI] [PubMed] [Google Scholar]
- 63.Koutek B, Prestwich GD, Howlett AC, Chin SA, Salehani D, Akhavan N, Deutsch DG. J Biol Chem. 1994;269:22937. [PubMed] [Google Scholar]
- 64.Deutsch DG, Omir R, Arreaza G, Salehani D, Prestwich GD, Huang Z, Howlett A. Biochem Pharmacol. 1997;53:255. doi: 10.1016/s0006-2952(96)00830-1. [DOI] [PubMed] [Google Scholar]
- 65.Ackermann EJ, Conde-Frieboes K, Dennis EA. J Biol Chem. 1995;270:445. doi: 10.1074/jbc.270.1.445. [DOI] [PubMed] [Google Scholar]
- 66.Kell PJ, Creer MH, Crown KN, Wirsig K, McHowat J. J Pharmacol Exp Ther. 2003;307:1163. doi: 10.1124/jpet.103.055392. [DOI] [PubMed] [Google Scholar]
- 67.Dinh TP, Freund TF, Piomelli D. Chem Phys Lipids. 2002;2002:149. doi: 10.1016/s0009-3084(02)00150-0. [DOI] [PubMed] [Google Scholar]
- 68.Boger DL, Sato H, Lerner AE, Hedrick MP, Fecik RA, Miyauchi H, Wilkie GD, Austin BJ, Patricelli MP, Cravatt BF. Proc Natl Acad Sci U S A. 2000;97:5044. doi: 10.1073/pnas.97.10.5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lichtman AH, Leung D, Shelton C, Saghatelian A, Hardouin C, Boger D, Cravatt BF. J Pharmacol Exp Ther. 2004;311:441. doi: 10.1124/jpet.104.069401. [DOI] [PubMed] [Google Scholar]
- 70.Chang L, Luo L, Palmer JA, Sutton S, Wilson SJ, Barbier AJ, Breitenbucher JG, Chaplan SR, Webb M. Br J Pharmacol. 2006;148:102. doi: 10.1038/sj.bjp.0706699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kathuria S, Gaetani S, Fegley D, Valino F, Duranti A, Tontini A, Mor M, Tarzia G, La Rana G, Calignano A, Giustino A, Tattoli M, Palmery M, Cuomo V, Piomelli D. Nat Med. 2003;9:76. doi: 10.1038/nm803. [DOI] [PubMed] [Google Scholar]
- 72.Alexander JP, Cravatt BF. Chem Biol. 2005;12:1179. doi: 10.1016/j.chembiol.2005.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Holt S, Comelli F, Costa B, Fowler CJ. Br J Pharmacol. 2005;146:467. doi: 10.1038/sj.bjp.0706348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jayamanne A, Greenwood R, Mitchell VA, Aslan S, Piomelli D, Vaughan CW. Br J Pharmacol. 2006;147:281. doi: 10.1038/sj.bjp.0706510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Russo R, Loverme J, La Rana G, Compton TR, Parrott J, Duranti A, Tontini A, Mor M, Tarzia G, Calignano A, Piomelli D. J Pharmacol Exp Ther. 2007;322:236. doi: 10.1124/jpet.107.119941. [DOI] [PubMed] [Google Scholar]
- 76.Jhaveri MD, Richardson D, Kendall DA, Barrett DA, Chapman V. J Neurosci. 2006;26:13318. doi: 10.1523/JNEUROSCI.3326-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gobbi G, Bambico FR, Mangieri R, Bortolato M, Campolongo P, Solinas M, Cassano T, Morgese MG, Debonnel G, Duranti A, Tontini A, Tarzia G, Mor M, Trezza V, Goldberg SR, Cuomo V, Piomelli D. Proc Natl Acad Sci U S A. 2005;102:18620. doi: 10.1073/pnas.0509591102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hohmann AG, Suplita RL, Bolton NM, Neely MH, Fegley D, Mangieri R, Krey JF, Walker JM, Holmes PV, Crystal JD, Duranti A, Tontini A, Mor M, Tarzia G, Piomelli D. Nature. 2005;435:1108. doi: 10.1038/nature03658. [DOI] [PubMed] [Google Scholar]
- 79.Patel S, Hillard CJ. J Pharmacol Exp Ther. 2006;318:304. doi: 10.1124/jpet.106.101287. [DOI] [PubMed] [Google Scholar]
- 80.Bortolato M, Mangieri RA, Fu J, Kim JH, Arguello O, Duranti A, Tontini A, Mor M, Tarzia G, Piomelli D. Biol Psychiatry. 2007;62:1103. doi: 10.1016/j.biopsych.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 81.Batkai S, Pacher P, Osei-Hyiaman D, Radaeva S, Liu J, Harvey-White J, Offertaler K, Mackie K, Rudd MA, Bukoski RD, Kunos G. Circulation. 2004;110:1996. doi: 10.1161/01.CIR.0000143230.23252.D2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Batkai S, Rajesh M, Mukhopadhyay P, Hasko G, Liaudet L, Cravatt BF, Csiszar A, Ungvari Z, Pacher P. Am J Physiol Heart Circ Physiol. 2007;293:H909. doi: 10.1152/ajpheart.00373.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rock EM, Limebeer CL, Mechoulam R, Piomelli D, Parker LA. Psychopharmacology (Berlin) 2008;196:389. doi: 10.1007/s00213-007-0970-1. [DOI] [PubMed] [Google Scholar]
- 84.Fegley D, Gaetani S, Duranti A, Tontini A, Mor M, Tarzia G, Piomelli D. J Pharmacol Exp Ther. 2005;313:352. doi: 10.1124/jpet.104.078980. [DOI] [PubMed] [Google Scholar]
- 85.Zhang D, Saraf A, Kolasa T, Bhatia P, Zheng GZ, Patel M, Lannoye GS, Richardson P, Stewart A, Rogers JC, Brioni JD, Surowy CS. Neuropharmacology. 2007;52:1095. doi: 10.1016/j.neuropharm.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 86.Ahn K, Johnson DS, Fitzgerald LR, Liimatta M, Arendse A, Stevenson T, Lund ET, Nugent RA, Nomanbhoy TK, Alexander JP, Cravatt BF. Biochemistry. 2007;46:13019. doi: 10.1021/bi701378g. [DOI] [PubMed] [Google Scholar]
- 87.De Bank PA, Kendall DA, Alexander SP. Biochem Pharmacol. 2005;69:1187. doi: 10.1016/j.bcp.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 88.Ahn K. WO/2006/085196. World Patent. 2006
- 89.Apodaca R, Breitenbucher JG, Pattabiraman K, Seierstad M, Xiao W. WO 2006/074025. World Patent. 2006
- 90.Matsumoto T, Kori M, Miyazaki J, Kiyota Y. WO 2006/054652. 2006
- 91.Jessani N, Cravatt BF. Curr Opin Chem Biol. 2004;8:54. doi: 10.1016/j.cbpa.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 92.Speers AE, Cravatt BF. ChemBioChem. 2004;5:41. doi: 10.1002/cbic.200300721. [DOI] [PubMed] [Google Scholar]
- 93.Leung D, Hardouin C, Boger DL, Cravatt BF. Nat Biotechnol. 2003;21:687. doi: 10.1038/nbt826. [DOI] [PubMed] [Google Scholar]
- 94.Liu Y, Patricelli MP, Cravatt BF. Proc Natl Acad Sci U S A. 1999;96:14694. doi: 10.1073/pnas.96.26.14694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Patricelli MP, Giang DK, Stamp LM, Burbaum J. J Proteomics. 2001;1:1067. doi: 10.1002/1615-9861(200109)1:9<1067::AID-PROT1067>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 96.Leung D, Du W, Hardouin C, Cheng H, Hwang I, Cravatt BF, Boger DL. Bioorg Med Chem Lett. 2005;15:1423. doi: 10.1016/j.bmcl.2004.12.085. [DOI] [PubMed] [Google Scholar]
- 97.Boger DL, Miyauchi H, Du W, Hardouin C, Fecik RA, Cheng H, Hwang I, Hedrick MP, Leung D, Acevedo O, Guimaraes CR, Jorgensen WL, Cravatt BF. J Med Chem. 2005;48:1849. doi: 10.1021/jm049614v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Saghatelian A, Trauger SA, Want EJ, Hawkins EG, Siuzdak G, Cravatt BF. Biochemistry. 2004;43:14332. doi: 10.1021/bi0480335. [DOI] [PubMed] [Google Scholar]
- 99.Saghatelian A, McKinney MK, Bandell M, Smith CA, Patapoutian A, Cravatt BF. Biochemistry. 2006;45:9007. doi: 10.1021/bi0608008. [DOI] [PubMed] [Google Scholar]
- 100.McKinney MK, Cravatt BF. Biochemistry. 2006;45:9016. doi: 10.1021/bi0608010. [DOI] [PubMed] [Google Scholar]
- 101.Di Marzo V, Fontana A, Cadas H, Schinelli S, Cimino G, Schwartz J-C, Piomelli D. Nature. 1994;372:686. doi: 10.1038/372686a0. [DOI] [PubMed] [Google Scholar]
- 102.Beltramo M, Stella N, Calignano A, Lin SY, Makriyannis A, Piomelli D. Science. 1997;277:1094. doi: 10.1126/science.277.5329.1094. [DOI] [PubMed] [Google Scholar]
- 103.Hillard CJ, Edgemond WS, Jarrahian A, Campbell WB. J Neurochem. 1997;69:631. doi: 10.1046/j.1471-4159.1997.69020631.x. [DOI] [PubMed] [Google Scholar]
- 104.Hillard CJ, Jarrahian A. Br J Pharmacol. 2003;140:802. doi: 10.1038/sj.bjp.0705468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Glaser ST, Kaczocha M, Deutsch DG. Life Sci. 2005;77:1584. doi: 10.1016/j.lfs.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 106.Fowler CJ. Fundam Clin Pharmacol. 2006;20:549. doi: 10.1111/j.1472-8206.2006.00442.x. [DOI] [PubMed] [Google Scholar]
- 107.Deutsch DG, Glaser ST, Howell JM, Kunz JS, Puffenbarger RA, Hillard CJ, Abumrad N. J Biol Chem. 2001;276:6967. doi: 10.1074/jbc.M003161200. [DOI] [PubMed] [Google Scholar]
- 108.Glaser ST, Abumrad N, Fatade F, Kaczocha M, Studholme KM, Deutsch DG. Proc Natl Acad Sci U S A. 2003;100:4269. doi: 10.1073/pnas.0730816100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Day TA, Rakhshan F, Deutsch DG, Barker EL. Mol Pharmacol. 2001;2001:1369. doi: 10.1124/mol.59.6.1369. [DOI] [PubMed] [Google Scholar]
- 110.Moore SA, Nomikos GG, Dickason-Chesterfield AK, Schober DA, Schaus JM, Ying BP, Xu YC, Phebus L, Simmons RM, Li D, Iyengar S, Felder CC. Proc Natl Acad Sci U S A. 2005;102:17852. doi: 10.1073/pnas.0507470102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jarrahian A, Manna S, Edgemond WS, Campbell WB, Hillard CJ. J Neurochem. 2000;74:2597. doi: 10.1046/j.1471-4159.2000.0742597.x. [DOI] [PubMed] [Google Scholar]
- 112.Vandevoorde S, Fowler CJ. Br J Pharmacol. 2005;145:885. doi: 10.1038/sj.bjp.0706253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Alexander JP, Cravatt BF. J Am Chem Soc. 2006;128:9699. doi: 10.1021/ja062999h. [DOI] [PubMed] [Google Scholar]
- 114.Dickason-Chesterfield AK, Kidd SR, Moore SA, Schaus JM, Liu B, Nomikos GG, Felder CC. Cell Mol Neurobiol. 2006;26:405. doi: 10.1007/s10571-006-9072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ortega-Gutierrez S, Hawkins EG, Viso A, Lopez-Rodriguez ML, Cravatt BF. Biochemistry. 2004;43:8184. doi: 10.1021/bi049395f. [DOI] [PubMed] [Google Scholar]
- 116.Kaczocha M, Hermann A, Glaser ST, Bojesen IN, Deutsch DG. J Biol Chem. 2006;281:9066. doi: 10.1074/jbc.M509721200. [DOI] [PubMed] [Google Scholar]
- 117.Fegley D, Kathuria S, Mercier R, Li C, Goutopoulos A, Makriyannis A, Piomelli D. Proc Natl Acad Sci U S A. 2004;101:8756. doi: 10.1073/pnas.0400997101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McFarland MJ, Porter AC, Rakhshan FR, Rawat DS, Gibbs RA, Barker EL. J Biol Chem. 2004;279:41991. doi: 10.1074/jbc.M407250200. [DOI] [PubMed] [Google Scholar]
- 119.Bari M, Battista N, Fezza F, Finazzi-Agro A, Maccarrone M. J Biol Chem. 2005;280:12212. doi: 10.1074/jbc.M411642200. [DOI] [PubMed] [Google Scholar]
- 120.Sipe JC, Chiang K, Gerber AL, Beutler E, Cravatt BF. Proc Natl Acad Sci U S A. 2002;99:8394. doi: 10.1073/pnas.082235799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chiang KP, Gerber AL, Sipe J, Cravatt BF. Hum Mol Genet. 2004;13:2113. doi: 10.1093/hmg/ddh216. [DOI] [PubMed] [Google Scholar]
- 122.Tyndale RF, Payne JI, Gerber AL, Sipe JC. Am J Med Genet Part B. 2007;144:660. doi: 10.1002/ajmg.b.30491. [DOI] [PubMed] [Google Scholar]
- 123.Morita Y, Ujike H, Tanaka Y, Uchida N, Nomura A, Ohtani K, Kishimoto M, Morio A, Imamura T, Sakai A, Inada T, Harano M, Komiyama T, Yamada M, Sekine Y, Iwata N, Iyo M, Sora I, Ozaki N, Kuroda S. Neurosci Lett. 2005;376:182. doi: 10.1016/j.neulet.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 124.Iwasaki S, Ishiguro H, Higuchi S, Onaivi ES, Arinami T. Psychiatr Genet. 2007;17:215. doi: 10.1097/YPG.0b013e32809913d8. [DOI] [PubMed] [Google Scholar]
- 125.Sipe JC, Waalen J, Gerber A, Beutler E. Int J Obes (London) 2005;29:755. doi: 10.1038/sj.ijo.0802954. [DOI] [PubMed] [Google Scholar]
- 126.Jensen DP, Andreasen CH, Andersen MK, Hansen L, Eiberg H, Borch-Johnsen K, Jorgensen T, Hansen T, Pederson O. J Mol Med. 2007;85:445. doi: 10.1007/s00109-006-0139-0. [DOI] [PubMed] [Google Scholar]
- 127.Aberle J, Fedderwitz I, Klages N, George E, Beil FU. Horm Metab Res. 2007;39:395. doi: 10.1055/s-2007-977694. [DOI] [PubMed] [Google Scholar]
- 128.Wei BQ, Mikkelsen TS, McKinney MK, Lander ES, Cravatt BF. J Biol Chem. 2006;281:36569. doi: 10.1074/jbc.M606646200. [DOI] [PubMed] [Google Scholar]
- 129.Ueda N, Yamanaka K, Yamamoto S. J Biol Chem. 2001;276:35552. doi: 10.1074/jbc.M106261200. [DOI] [PubMed] [Google Scholar]
- 130.Tsuboi K, Sun YX, Okamoto Y, Araki N, Tonai T, Ueda N. J Biol Chem. 2005;280:11082. doi: 10.1074/jbc.M413473200. [DOI] [PubMed] [Google Scholar]
- 131.Tsuboi K, Hilligsmann C, Vandevoorde S, Lambert DM, Ueda N. Biochem J. 2004;379:99. doi: 10.1042/BJ20031695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sun YX, Tsuboi K, Zhao LY, Okamoto Y, Lambert DM, Ueda N. Biochim Biophys Acta. 2005;1736:211. doi: 10.1016/j.bbalip.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 133.Hong SB, Li CM, Rhee HJ, Park JH, He X, Levy B, Yoo OJ, Schuchman EH. Genomics. 1999;62:232. doi: 10.1006/geno.1999.5953. [DOI] [PubMed] [Google Scholar]
- 134.Tsuboi K, Zhao LY, Okamoto Y, Araki N, Ueno M, Sakamoto H, Ueda N. Biochim Biophys Acta. 2007;1771 doi: 10.1016/j.bbalip.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 135.Vinod KY, Sanguino E, Yalamanchili R, Manzanares J, Hungund BL. J Neurochem. 2008;104:233. doi: 10.1111/j.1471-4159.2007.04956.x. [DOI] [PubMed] [Google Scholar]
- 136.Blednov YA, Cravatt BF, Boehm SL, Walker D, Harris RA. Neuropsychopharmacology. 2007;32:1570. doi: 10.1038/sj.npp.1301274. [DOI] [PubMed] [Google Scholar]
- 137.Maccarrone M, Valensise H, Bari M, Lazzarin N, Romanini C, Finazzi-Agro A. Lancet. 2000;355:1326. doi: 10.1016/S0140-6736(00)02115-2. [DOI] [PubMed] [Google Scholar]
- 138.Maccarrone M, Bisogno T, Valensise H, Lazzarin N, Fezza F, Manna C, Di Marzo V, Finazzi-Agro A. Mol Hum Reprod. 2002;8:188. doi: 10.1093/molehr/8.2.188. [DOI] [PubMed] [Google Scholar]
- 139.Wang H, Xie H, Guo Y, Zhang H, Takahashi T, Kingsley PJ, Marnett LJ, Das SK, Cravatt BF, Dey SK. J Clin Invest. 2006;116:2122. doi: 10.1172/JCI28621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Natarajan V, Reddy PV, Schmid PC, Schmid HH. Biochim Biophys Acta. 1982;712:342. doi: 10.1016/0005-2760(82)90352-6. [DOI] [PubMed] [Google Scholar]
- 141.Schmid PC, Reddy PV, Natarajan V, Schmid HH. J Biol Chem. 1983;258:9302. [PubMed] [Google Scholar]
- 142.Cadas H, Gaillet S, Beltramo M, Venance L, Piomelli D. J Neurosci. 1996;16:3934. doi: 10.1523/JNEUROSCI.16-12-03934.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cadas H, di Tomaso E, Piomelli D. J Neurosci. 1997;17:1226. doi: 10.1523/JNEUROSCI.17-04-01226.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Okamoto Y, Morishita J, Tsuboi K, Tonai T, Ueda N. J Biol Chem. 2004;279:5298. doi: 10.1074/jbc.M306642200. [DOI] [PubMed] [Google Scholar]
- 145.Di Marzo V, Goparaju SK, Wang L, Liu J, Batkai S, Jarai Z, Fezza F, Miura GI, Palmiter RD, Sugiura T, Kunos G. Nature. 2001;410:822. doi: 10.1038/35071088. [DOI] [PubMed] [Google Scholar]
- 146.Walter L, Franklin A, Witting A, Moller T, Stella N. J Biol Chem. 2002;277:20869. doi: 10.1074/jbc.M110813200. [DOI] [PubMed] [Google Scholar]
- 147.Leung D, Saghatelian A, Simon GM, Cravatt BF. Biochemistry. 2006;45:4720. doi: 10.1021/bi060163l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Natarajan V, Schmid PC, Reddy PV, Schmid HH. J Neurochem. 1984;42:1613. doi: 10.1111/j.1471-4159.1984.tb12750.x. [DOI] [PubMed] [Google Scholar]
- 149.Wang J, Okamoto Y, Morishita J, Tsuboi K, Miyatake A, Ueda N. J Biol Chem. 2006;281:12325. doi: 10.1074/jbc.M512359200. [DOI] [PubMed] [Google Scholar]
- 150.Sun YX, Tsuboi K, Okamoto Y, Tonai T, Murakami M, Kudo I, Ueda N. Biochem J. 2004;380:749. doi: 10.1042/BJ20040031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Simon GM, Cravatt BF. J Biol Chem. 2006;281:26465. doi: 10.1074/jbc.M604660200. [DOI] [PubMed] [Google Scholar]
- 152.Liu J, Wang L, Harvey-White J, Osei-Hyiaman D, Razdan R, Gong Q, Chan AC, Zhou Z, Huang BX, Kim HY, Kunos G. Proc Natl Acad Sci U S A. 2006;103:13345. doi: 10.1073/pnas.0601832103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Liu J, Wang L, Harvey-White J, Huang BX, Kim HY, Luquet S, Palmiter RD, Krystal G, Rai R, Mahadevan A, Razdan RK, Kunos G. Neuropharmacology. 2008;54:1. doi: 10.1016/j.neuropharm.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Jin XH, Okamoto Y, Morishita J, Tsuboi K, Tonai T, Ueda N. J Biol Chem. 2007;282:3614. doi: 10.1074/jbc.M606369200. [DOI] [PubMed] [Google Scholar]
- 155.Goparaju SK, Ueda N, Yamaguchi H, Yamamoto S. FEBS Lett. 1998;422:69. doi: 10.1016/s0014-5793(97)01603-7. [DOI] [PubMed] [Google Scholar]
- 156.Lichtman AH, Hawkins EG, Griffin G, Cravatt BF. J Pharmacol Exp Ther. 2002;302:73. doi: 10.1124/jpet.302.1.73. [DOI] [PubMed] [Google Scholar]
- 157.Karlsson M, Contreras JA, Hellman U, Tornqvist H, Holm C. J Biol Chem. 1997;272:27218. doi: 10.1074/jbc.272.43.27218. [DOI] [PubMed] [Google Scholar]
- 158.Walter L, Dinh T, Stella N. J Neurosci. 2004;24:8068. doi: 10.1523/JNEUROSCI.2419-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dinh TP, Kathuria S, Piomelli D. Mol Pharmacol. 2004;66:1260. doi: 10.1124/mol.104.002071. [DOI] [PubMed] [Google Scholar]
- 160.Saario SM, Salo OM, Nevalainen T, Poso A, Laitinen JT, Jarvinen T, Niemi R. Chem Biol. 2005;12:649. doi: 10.1016/j.chembiol.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 161.Makara JK, Mor M, Fegley D, Szabo SI, Kathuria S, Astarita G, Duranti A, Tontini A, Tarzia G, Rivara S, Freund TF, Piomelli D. Nat Neurosci. 2005;8:1139. doi: 10.1038/nn1521. [DOI] [PubMed] [Google Scholar]
- 162.Saario SM, Palomaki V, Lehtonen M, Nevalainen T, Jarvinen T, Laitinen JT. Chem Biol. 2006;13:811. doi: 10.1016/j.chembiol.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 163.Makara JK, Mor M, Fegley D, Szabo SI, Kathuria S, Astarita G, Duranti A, Tontini A, Tarzia G, Rivara S, Freund TF, Piomelli D. Nat Neurosci. 2007;10:134. doi: 10.1038/nn1521. [DOI] [PubMed] [Google Scholar]
- 164.Vandevoorde S, Jonsson KO, Labar G, Persson E, Lambert DM, Fowler CJ. Br J Pharmacol. 2007;150:186. doi: 10.1038/sj.bjp.0706971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Muccioli GG, Xu C, Odah E, Cudaback E, Cisneros JA, Lambert DM, Lopez Rodriguez ML, Bajjalieh S, Stella N. J Neurosci. 2007;27:2883. doi: 10.1523/JNEUROSCI.4830-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hashimotodani Y, Ohno-Shosaku T, Kano M. J Neurosci. 2007;27:1211. doi: 10.1523/JNEUROSCI.4159-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Blankman JL, Simon GM, Cravatt BF. Chem Biol. 2007;14:1347. doi: 10.1016/j.chembiol.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Labar G, Bauvois C, Muccioli GG, Wouters J, Lambert DM. ChemBioChem. 2007;8:1293. doi: 10.1002/cbic.200700139. [DOI] [PubMed] [Google Scholar]
- 169.Jessani N, Niessen S, Wei BQ, Nicolau M, Humphrey M, Ji Y, Han W, Noh DY, Yates JR, 3rd, Jeffrey SS, Cravatt BF. Nat Methods. 2005;2:691. doi: 10.1038/nmeth778. [DOI] [PubMed] [Google Scholar]
- 170.van Tienhoven M, Atkins J, Li Y, Glynn P. J Biol Chem. 2002;277:20942. doi: 10.1074/jbc.M200330200. [DOI] [PubMed] [Google Scholar]
- 171.Belfrage P, Jergil B, Strålfors P, Tornqvist H. FEBS Lett. 1977;75:259. doi: 10.1016/0014-5793(77)80099-9. [DOI] [PubMed] [Google Scholar]
- 172.Kozak KR, Rowlinson SW, Marnett LJ. J Biol Chem. 2000;275:33744. doi: 10.1074/jbc.M007088200. [DOI] [PubMed] [Google Scholar]
- 173.Kim J, Alger BE. Nat Neurosci. 2004;7:697. doi: 10.1038/nn1262. [DOI] [PubMed] [Google Scholar]
- 174.Slanina KA, Roberto M, Schweitzer P. Neuropharmacology. 2005;49:660. doi: 10.1016/j.neuropharm.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 175.Hashimotodani Y, Ohno-Shosaku T, Watanabe M, Kano M. J Physiol. 2007;584:373. doi: 10.1113/jphysiol.2007.137497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bisogno T, Howell F, WIlliams G, Minassi A, Cascio MG, Ligresti A, Matias I, Schiano-Moriello A, Paul P, Williams EJ, Gangadharan U, Hobbs C, Di Marzo V, Doherty P. J Cell Biol. 2003;163:463. doi: 10.1083/jcb.200305129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Katona I, Urban GM, Wallace M, Ledent C, Jung KM, Piomelli D, Mackie K, Freund TF. J Neurosci. 2006;26:5628. doi: 10.1523/JNEUROSCI.0309-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yoshida T, Fukaya M, Uchigashima M, Miura E, Kamiya H, Kano M, Watanabe M. J Neurosci. 2006;26:4740. doi: 10.1523/JNEUROSCI.0054-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Uchigashima M, Narushima M, Fukaya M, Katona I, Kano M, Watanabe M. J Neurosci. 2007;27:3663. doi: 10.1523/JNEUROSCI.0448-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Safo PK, Regehr WG. Neuron. 2005;48:647. doi: 10.1016/j.neuron.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 181.Straiker A, Mackie K. J Physiol. 2005;569:501. doi: 10.1113/jphysiol.2005.091918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Szabo B, Urbanski MJ, Bisogno T, Di Marzo V, Mendiguren A, Baer WU, Freiman I. J Physiol. 2006;577:263. doi: 10.1113/jphysiol.2006.119362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Edwards DA, Kim J, Alger BE. J Neurophysiol. 2006;95:67. doi: 10.1152/jn.00813.2005. [DOI] [PubMed] [Google Scholar]
- 184.Hashimotodani Y, Ohno-Shosaku T, Maejima T, Fukami K, Kano M. Neuropharmacology. 2008;54:58. doi: 10.1016/j.neuropharm.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 185.Henness S, Perry CM. Drugs. 2006;66:1625. doi: 10.2165/00003495-200666120-00012. [DOI] [PubMed] [Google Scholar]
- 186.Bisogno T, Cascio MG, Saha B, Mahadevan A, Urbani P, Minassi A, Appendino G, Saturnino C, Martin B, Razdan R, Di Marzo V. Biochim Biophys Acta. 2006;1761:205. doi: 10.1016/j.bbalip.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 187.Jung KM, Astarita G, Zhu C, Wallace M, Mackie K, Piomelli D. Mol Pharmacol. 2007;72:612. doi: 10.1124/mol.107.037796. [DOI] [PubMed] [Google Scholar]
- 188.Jung KM, Mangieri R, Stapleton C, Kim J, Fegley D, Wallace M, Mackie K, Piomelli D. Mol Pharmacol. 2005;68:1196. doi: 10.1124/mol.105.013961. [DOI] [PubMed] [Google Scholar]
- 189.Hashimotodani Y, Ohno-Shosaku T, Tsubokawa H, Ogata H, Emoto K, Maejima T, Araishi K, Shin HS, Kano M. Neuron. 2005;45:257. doi: 10.1016/j.neuron.2005.01.004. [DOI] [PubMed] [Google Scholar]


