Introduction
Scope of the guidelines
These National Clinical Guidelines for stroke cover the management of patients with acute stroke and the secondary prevention of stroke. Primary prevention of stroke, rehabilitation and subarachnoid hemorrhage are excluded from the scope of these guidelines. These guidelines cover the management of stroke in adults (over 18 years) from onset to chronic care and focus on patients with a new clinical event (first stroke or recurrent stroke).
Goal and objectives of the guidelines
The primary goal of the guidelines is to continuously improve the quality of care in patients with stroke nationally. Our intention is closing the gap between best practice and actual practice.
The objective of the guidelines is to provide clinicians and administrators with explicit statements, where evidence is available, on the best way to manage specific problems. Local health service facilities (e.g. hospitals, nursing homes, etc.) will need to add detail.
The guidelines are directed primarily at practising clinicians involved in management of patients with stroke. Their aim is to help clinicians, at any level – primary, secondary or tertiary - to make the best decisions for each patient, using the evidence currently available. The focus is on the more common clinical questions faced in day-to-day practice. The guidelines may be used by all health professionals or health care planners involved in the management of the patients with stroke.
The secondary objectives of the guidelines are to identify areas where gaps in knowledge or lack of evidence exist and to stimulate research in each area.
The guidelines are concerned with the management of patients who present with a new clinical event that might be stroke. Stroke in this context is defined as ‘a clinical syndrome characterized by rapidly developing signs and symptoms of focal or at times global loss (as in subarachnoid hemorrhage or brain stem involvement) of cerebral brain functions, lasting more than 24 hours or leading to death, with no apparent cause other than of vascular origin.’
While appraisal of evidence forms the basis of the development of these guidelines, we wish to clarify some points:
Evidence related to drugs is generally stronger, because it is methodologically easier to study each intervention in contrast to studying complex intervention like occupational therapy, health education or nursing care. These do not necessarily mean that interventions with so called strong evidence are more important than those where the evidence is weak.
We believe that highest level of evidence is not always required to make strong recommendation. If the intervention is safe, logic is strong and effect is obvious, the level of evidence desirable to make strong recommendation may be lower than the highest.
We recognize that many areas of clinical importance may not have evidence available to construct guidelines, and the recommendations represent a consensus from the working group on such areas.
The working group is aware of recent developments in evaluating levels of evidence and strength of recommendations, and also that the GRADE methodology has been adopted by more than 25 organizations around the world including the WHO. The group endorses the use of GRADE methodology (Guyatt and Oxman)[1] for this purpose and will incorporate this in the next version of the guidelines.
Context and use
These guidelines should be taken as statements to inform the clinician, not as rigid rules. Practitioners may need to deviate from the guidelines in individual cases but such deviations should be justifiable and justified.
The guidelines may be used to inform decisions on standards of good practice and are likely to be used for audit of stroke services. Before the guidelines are used as ‘standards’, it is important to ensure that the relevance and appropriateness of the guidelines are discussed in the context proposed.
These guidelines do not cover specific management of associated illnesses like diabetes mellitus, cardiac problems and others as these may addressed by guidelines from related organizations or are generally expected from a physician.
Guidelines for Organization of Services for Stroke Care
Stroke care may be organized at three levels - a basic stroke care facility, a primary stroke care facility and a comprehensive stroke care facility. The basic stroke care facility should be the minimum setup at district hospitals; primary stroke care facility should be mandatory for all medical colleges and multispeciality hospitals; and well-equipped hospitals including some medical colleges should develop comprehensive stroke care facilities. The basic stroke facility may not have artificial ventilators, echocardiography and carotid Doppler facility, primary stroke care facilities may have these facilities but not neurosurgery, MRI or angiography. Comprehensive stroke care facilities should have all these facilities.
Recommendations
Patient care services
Acute stroke team
At a minimum, includes a physician and another health care professional (i.e., nurse, physician). In addition, a physiotherapist is essential for rehabilitation.
Team personnel should have experience, expertise and special interest in diagnosis and treatment of stroke patients.
Team should be available 24 × 7 and a member of the team should be at patient bedside within 15 minutes of being called.
Written care protocols
Protocols should be made available for rt-PA use in acute stroke.
Protocols for emergency care, diagnostic tests, stabilization of vital functions and use of medication should be made available.
Protocols should be reviewed and updated at least once a year.
Emergency medical services (EMS) should be developed and upgraded for stroke care at the hospital or district level to include transport and triage of patients from peripheral medical centers.
Emergency department
ED personnel should be trained to diagnose and treat all types of stroke.
ED should have good communication with the EMS and the acute stroke team
ED personnel should undergo educational activities related to stroke diagnosis and management at least twice a year.
Stroke unit
Should consist of a hospital unit with specially trained staff and a multidisciplinary approach to treatment and care of stroke patients.
Should be able to admit patients in the unstable phase, monitor the vital and neurological parameters, diagnose the etiology and subtype, treat and discharge patients with advice on physiotherapy and secondary prevention.
Should transfer severely ill and stuporous patients including those with raised intracranial pressure (ICP) and with unstable cardiopulmonary status to intensive care.
Should consider using telemedicine to improve access to treatment in rural and remote areas.
Neurosurgical services
Comprehensive stroke care facilities should have 24 × 7 on call neurosurgeon to evaluate and operate in cases requiring such consultation and neurosurgery.
A primary stroke care facility should have neurosurgical care available as early as possible (<2 hours). The patient should either be transferred to a neurosurgical care facility or should be able to call in a neurosurgeon within 2 hours.
A written protocol for transfer plan should be available.
The hospital with neurosurgical facility should be having 24 hours operating facility and support personnel (anesthesia, radiology, laboratory services, etc.).
Support services
Neuroimaging: All levels of stroke care facilities should have the capability of performing or access to either a cranial computed tomography (CT scan) or magnetic resonance imaging (MRI) scan within 30 minutes of the order being written with experienced physicians or a radiologist to interpret the imaging reports.
Laboratory services to perform routine blood tests, coagulation studies, ECG and chest roentgenograms with 24-hour services. The lab results should be available within 45 minutes of being ordered.
Commitment and Support of the Organization/Institution should be available toward the stroke care facility and the stroke unit should have a designated medical director/incharge with expertise in stroke.
Educational programs periodically and annual programs for the stroke team should be instituted and public education about prevention, recognition and management of stroke should be carried out.
Evidence: Albers,[2] Alberts,[3] Audebert,[4] Calvet,[5] Evans,[6] Intercollegiate Stroke Working Party,[7] Katzan,[8] Koton,[9] LaMonte,[10] Prabhakaran,[11] Purroy,[12] Ronning,[13] Silva,[14] Stavem,[15] Stroke Unit Trialists’ Collaboration.[16]
Acute Phase Care
Admission to hospital
Most patients with stroke should be admitted to a hospital because their neurological condition may worsen over the first few days, they may develop non-neurological complications (e.g., aspiration pneumonia), and urgent investigations (like CT scan) may be required.
Recommendations
Patients with acute stroke (onset within last 72 hours or altered consciousness due to stroke) should be admitted to hospital for initial care and assessment. Circumstances where a physician might reasonably choose not to admit selected patients with stroke include the following:
Individuals with severe pre-existing irreversible disability (e.g., severe untreatable dementia), or terminal illnesses (e.g., cancer), who have options to be cared at lower level health care facility.
Alert patients with mild neurological deficits (not secondary to ruptured saccular aneurysm) who are identified more than 72 hours after onset of symptoms, who can be evaluated expeditiously as outpatients, and who are unlikely to require surgery, invasive radiological procedures or anticoagulation;
Patients with mild neurological deficits in whom a history and examination is consistent with lacunar stroke syndrome, and a CT scan that either is normal or shows old lacunar infarcts. However, they should be evaluated expeditiously as outpatients.
Diagnosis and management of resolved or rapidly resolving acute neurological event
Patients who are first seen after fully resolved or rapidly resolving neurological symptoms need diagnosis to determine whether in fact the cause is vascular (about 50% are not) and then to identify treatable causes that can reduce the risk of stroke (greatest in first 7-14 days).
Any patient who presents with transient symptoms suggestive of a cerebrovascular event should be considered to have had a transient ischemic attack (TIA), unless neuroimaging reveals an alternative diagnosis.
All such patients except those with transient monocular blindness should have imaging of brain, either CT scan or MRI. Patients presenting with transient monocular blindness (amaurosis fugax) must have a complete ophthalmological examination to exclude primary disorders of the eye before diagnosis of TIA.
Patients who have had a TIA should be assessed as soon as possible for their risk of subsequent stroke using a validated scoring system, such as ABCD2 (Refer to Appendix -1).
All patients with history of TIA should be started on aspirin 150 or 300 mg daily or Clopidogrel (75 mg) once a day in case of aspirin allergy; and those at high risk of stroke (ABCD2 score of 4 or above) should be assessed at primary or comprehensive stroke care facility within 24 hours for further management (as indicated under heading ‘Secondary Prevention’). Those at lower risk should be assessed within 1 week of onset of symptoms.
Patients with crescendo TIA (two or more TIAs in a week) should be treated as being at high risk of stroke, even though they may have ABCD2 score of 3 or below.
Patients who have had a TIA but who present more than one week after their last symptom has resolved should be treated as those with ABCD2 score of 3 or below.
All patients with TIA should be managed as indicated under the heading ‘Secondary Prevention’.
Appendix-1.
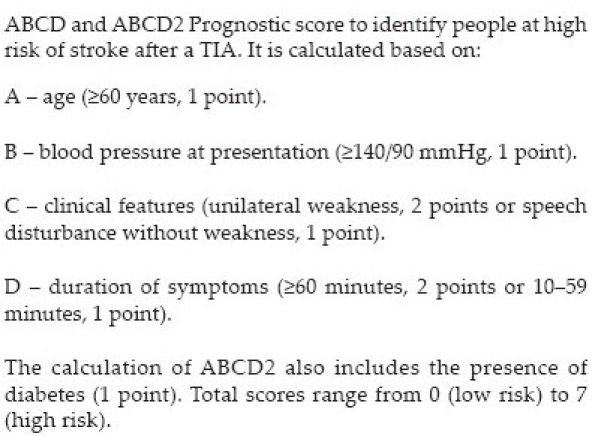
Evidence: Bray,[17] Cucchiara,[18] Lavallee,[19] Rothwell.[20]
Diagnosis of acute persistent cerebrovascular event
The aims of emergent evaluation are to:
Separate stroke (a vascular event) from other causes of rapid onset neurological dysfunction (stroke mimics);
Provide information about pathology (hemorrhage vs. ischemia);
Give clues about the most likely etiology;
Predict the likelihood of immediate complications; and
Plan appropriate treatment.
-
It should be recognized that ‘stroke’ is primarily a clinical diagnosis and that the diagnosis should be made with special care:
- In the young;
- If the sensorium is altered in presence of mild to moderate hemiparesis;
- If the history is uncertain; or
- If there are other unusual clinical features such as gradual progression over days, unexplained fever or papilloedema.
History, physical examination and common investigations
History should follow usual routine. Special attention should be paid to onset of symptoms, recent stroke, myocardial infarction, seizure, trauma, surgery, bleeding, pregnancy and use of anticoagulation/insulin/antihypertensive, history of modifiable risk actors: Hypertension, diabetes, smoking, heart disease, hyperlipidemia, migraine and history of headache or vomiting, recent child birth and risk of dehydration.
Physical examination should be on usual lines with special attention to ABC (airway, breathing, circulation), temperature, oxygen saturation, sign of head trauma (contusions), seizure (tongue laceration), carotid bruits, peripheral pulses, cardiac auscultation, evidence of petechiae, purpura or jaundice.
Validated stroke scales like NIHSS may be used to determine the degree of neurological deficit.
All patients should have neuroimaging, complete blood count, blood glucose, urea, serum creatinine, serum electrolytes, ECG and markers of cardiac ischemia. Selected patients may require liver function tests, chest radiography, arterial blood gases, EEG, lumbar puncture, blood alcohol level, toxicology studies or pregnancy test.
All patients should have their clinical course monitored and any patient whose clinical course is unusual for stroke should be reassessed for possible alternative diagnosis.
Brain imaging should be performed immediately for patients with persistent neurological symptoms if any of the following apply:
Indication for thrombolysis or early anticoagulation.
On anticoagulant treatment.
-
A known bleeding tendency.
- A depressed level of consciousness (GCS below 13).
- Severe headache at onset of stroke symptoms.
- Papilloedema, neck stiffness, subhyaloid hemorrhage or fever.
Patients with acute stroke without the above indications for immediate brain imaging, scanning should be performed within 24 hours after onset of symptoms.
Evidence: Intercollegiate stroke working party,[7] Wardlaw.[21]
Immediate specific management of ischemic stroke
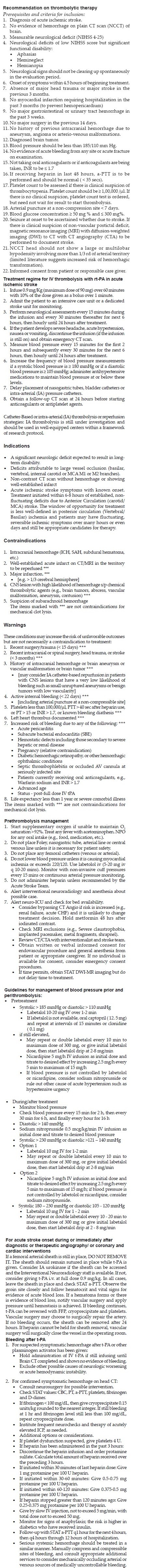
All patients with disabling acute ischemic stroke who can be treated within 3 hours (4.5 hours as soon as approved by the Drug Controlling authority) after symptom onset should be evaluated without delay to determine their eligibility for treatment with intravenous tissue plasminogen activator (alteplase).
Please see [Appendix - 2] for detailed recommendation on thrombolytic therapy.
All acute stroke patients should be given at least 150 mg of aspirin immediately after brain imaging has excluded intracranial hemorrhage (In patients with t-PA, aspirin should be delayed until after the 24-hour post-thrombolysis).
In patients with large hemispheric infarct (malignant MCA territory infarct), aspirin may be delayed until surgery or decision is made not to operate.
In dysphagic patients, aspirin may be given by enteral tube.
Aspirin (at least 150 mg) should be continued until 2 weeks after the onset of stroke symptoms, at which time any antiplatelet or anticoagulant agent is started as indicated in ‘secondary prevention’.
Any patient with acute ischemic stroke who is known to have dyspepsia with aspirin should be given a proton pump inhibitor in addition to aspirin (also see ‘secondary prevention’).
Appendix - 2.
Evidence: CAST,[22] ECASS III - Hacke,[23] Hill,[24] IST-3 Whiteley,[25] National Institute for Health and Clinical Excellence,[26] NINDS.[27]
Surgery for ischaemic stroke
Patients with middle cerebral artery (MCA) infarction who meet all of the criteria below should be considered for decompressive hemicraniectomy and operated within a maximum of 48 hours:
Age 60 years or below.
NIHSS score of above 15.
Decrease in the level of consciousness to give a score of 1 or more on item 1a of NIHSS, or GCS score between 6 and 13.
CT scan showing signs of an infarct of at least 50% of the MCA territory, with or without infraction in the territory of anterior or posterior cerebral artery on the same side or diffusion-weighted MRI showing infarct volume >145cm3.
Patients with large cerebellar infarct causing compression of brainstem and altered consciousness should be surgically managed with suboccipital craniectomy.
Symptomatic hydrocephalus should be treated surgically with ventriculostomy.
Evidence:DECIMAL, DESTINY, HAMLET - Gupta,[28] Jüttler,[29] Vahedi.[30]
Hemodilution and neuroprotection:
Hemodilution therapy is not recommended for the management of patients with acute ischemic stroke.
No neuroprotective drug is recommended outside the setting of randomized clinical studies.
Immediate specific management of intracerebral hemorrhage (ICH)
ICH related to antithrombotic or fibrinolytic therapy
ICH related to intravenous heparin requires rapid normalization of a-PTT by protamine sulphate (1 mg/100 U of heparin) with adjustment of dose according to time elapsed since the last heparin dose: For 30 to 60 min : 0.5 to 0.75 mg; for 60 to 120 min: 0.375 to 0.5 mg, for >120 min 0.25-0.3/mg). Protamine sulfate is given by slow i.v. not to exceed 5 mg/min (maximum of 50 mg). Protamine sulfate may also be used for ICH related to use of subcutaneous low molecular weight heparin.
Patients with warfarin related ICH should be managed with vitamin K, fresh frozen plasma (FFP) and wherever available prothrombin complex concentrate. Vitamin K (10 mg i.v.) should not be used alone because it takes at least 6 hours to normalize the INR. FFP (15-20 ml/kg) is an effective way of correcting INR, but there is risk of volume overload and heart failure. Prothrombin complex concentrate and factor IX complex concentrate require smaller volumes of infusion than FFP (and correct the coagulopathy faster but with greater risk of thromboembolism).
Patients with ICH related to thrombolysis should be treated with infusion of platelets and cryoprecipitate as indicated in Appendix-2.
Evidence: Cartmill,[34] Goldstein,[35] Huttner,[36] Fredriksson,[37] Yasaka.[38]
Restarting warfarin
Patients with a very high risk of thromboembolism (those with mechanical heart valves), warfarin therapy may be restarted at 7-10 days after onset of the index ICH. Those with lower risk may be restarted on antiplatelet therapy.
Evidence: Gubitz 4,[39] Phan.[40]
Surgery for ICH
Patients with cerebellar hemorrhage (>3 cm in diameter) who are deteriorating neurologically or who have signs of brain stem dysfunction should have suboccipital craniectomy and surgical evacuation of hematoma.
Patients with supratentorial ICH causing midline shift and/or herniation with impairment of consciousness or deteriorating neurologically should have surgical evacuation of hematoma within 72 hours of onset of symptoms, unless they were dependent on others for activities of daily living prior to the event or their GCS is <6 (unless this is because of hydrocephalus).
Patients with hydrocephalus who are symptomatic from ventricular obstruction should undergo ventriculostomy.
Evidence: Auer 1989,[41] Mendelow,[42] Prasad,[43] Prasad.[44]
Acute arterial dissection
Any patient suspected of having arterial dissection should be investigated with appropriate imaging (MRI and MRA).
People with stroke secondary to arterial dissection should be treated with either anticoagulants or antiplatelet agents. In selected patients, stenting may be indicated.
Cardioembolic stroke
Patients with disabling ischemic stroke who are in atrial fibrillation should be treated with aspirin 300 mg for the first 2 weeks before starting anticoagulation.
In patients with prosthetic valves who have disabling cerebral infarction and who are at significant risk of hemorrhage transformation, anticoagulation treatment should be stopped for one week and aspirin 150-300 mg should be substituted.
Some experts, despite lack of evidence, recommend starting heparin within 48 hours of onset of cardioembolic stroke, except in patients with large infarctions.
Evidence: Butler,[49] Evans,[50] Hart,[51] Intercollegiate Stroke Working Party,[7] Scottish Intercollegiate Guidelines Network.[52]
Cerebral venous thrombosis
Patients suspected to have stroke due to cerebral venous thrombosis should be investigated by MRI/MRV/CTV only if not diagnosed by CT scan.
Patients diagnosed with stroke due to cerebral venous thrombosis (with or without hemorrhagic infarct or secondary cerebral hemorrhage) should be given full-dose anticoagulation (initially heparin and then warfarin [INR 2-3]) unless there are contraindications.
Physiological Homeostasis (Oxygen, temperature, blood pressure, glucose)
Supplemental oxygen therapy
Patients should receive supplemental oxygen if their oxygen saturation drops below 95%.
Management of body temperature
Recommendation
Temperature should be monitored every 4 hours for at least first 48 hours and preferably as long as the patient is in the ward.
Fever (>37.5°C) should be treated with paracetamol. The search for possible infection (site and cause) should be made.
Hypothermia <34°C should be avoided as it can lead to coagulopathies, electrolyte imbalance, infection and cardiac arrhythmias.
Management of blood pressure
Ischemic stroke
-
In acute ischemic stroke, paraenteral antihypertensive medication should be recommended only if there is a hypertensive emergency with one or more of the following serious concomitant medical issues:
- hypertensive encephalopathy
- hypertensive nephropathy
- hypertensive cardiac failure/myocardial infarction
- aortic dissection
- pre-eclampsia/eclampsia
- intracerebral hemorrhage with systolic blood pressure (SBP) over 200 mmHg.
Antihypertensive medication should be withheld in ischemic stroke patients unless SBP is >220 mmHg or the mean arterial blood pressure (MAP) is >120 mmHg. Lowering by approx 15% during the first 24 hours is recommended.
Except in hypertensive emergency, lowering of blood pressure should be slow and with use of oral medications.
Sublingual use of antihypertensives is not recommended.
Blood pressure reduction to 185/110 mmHg or lower should be considered in people who are candidates for thrombolysis.
Intracranial hemorrhage
If SBP is >200 mmHg or MAP is >150 mmHg (recorded twice, two or more minutes apart), then blood pressure should be aggressively treated with parenteral antihypertensives (e.g., labetolol or nitroglycerin).
If SBP is >180 mmHg or MAP is >130 mmHg (up to 150 mm Hg), then a modest reduction is advised with rapidly acting oral or parenteral medication or nitroglycerin patch.
Target BP should be 160/90 or MAP of 110 mmHg.
Management of blood glucose
Recommendation
The blood glucose level should be maintained between 70 and 190 mg/dL. Elevated blood glucose >140 mg/dL should be managed with insulin administration using the sliding scale in the first week of stroke onset.
Hypoglycemia should be monitored and accordingly 20% glucose (50 ml bolus) should be administered.
Evidence: Bruno,[65] Gray,[66] National Institute for Health and Clinical Excellence.[67]
Cerebral edema and increased intracranial pressure
Until more data are available
Corticosteroids are not recommended for the management of cerebral edema and increased ICP following stroke.
In patients whose condition is deteriorating secondary to increased ICP, including those with herniation syndromes, various options include: Hyperventilation, mannitol, furosemide, CSF drainage and surgery. If CT scan (first or repeat one after deterioration) suggests hydrocephalus as the cause of increased ICP, then continuous drainage of CSF can be used.
Initial care includes mild restriction of fluids, elevation of head end of the bed by 20 to 30 degrees and correction of factors that might exacerbate increased ICP (e.g. hypoxia, hypercarbia and hyperthermia).
Hyperventilation acts immediately (reduction of the pCO2 by 5-10 mmHg lowers ICP by 25-30%) but should be followed by another intervention to control brain edema and ICP. Hyperventilation can cause vasoconstriction that might aggravate ischemia. An intravenous bolus of 40 mg furosemide may be used in patients whose condition is rapidly deteriorating. If required, furosemide 20 mg (once daily) may be continued for the first week, Acetazolamide 250 mg (BD) may be added in those not responding to other treatment methods.
Strict intake-output chart must be maintained to avoid dehydration.
Mannitol (0.5 gm/kg IV given over 20 minutes) can be given every 6-8 hours. If clinically indicated, dose frequency may be increased to every 4 hours, but then the central venous pressure should be monitored and kept between 5 and 12 mmHg to prevent hypovolemia. This may be continued for 3-5 days.
Evidence: Bereczki,[68] Broderick,[69] Qizilbash,[70] Tyson.[71]
General Early Supportive Care
Position
Patients should be advised to undertake activities like sitting, standing or walking only with caution. An occasional patient, who deteriorates on assuming sitting or standing posture, should be advised bed rest.
Non-ambulatory patient should be positioned to minimize the risk of complications such as contractures, respiratory complications, shoulder pain and pressure sores etc.
Swallowing
Please see Appendix- 3 for detailed recommendation on bedside swallowing assessment.
All conscious patients should have assessment of the ability to swallow. A water swallow test performed at the bedside is sufficient (e.g. 50 ml water swallow test )
Testing the gag reflex is invalid as a test of swallowing.
Patients with normal swallow should be assessed for the most suitable posture and equipment to facilitate feeding. Any patient with abnormal swallow should be fed using a nasogastric tube.
Gastrostomy feeding should be considered for patients who are unable to tolerate nasogastric tube.
Patients with altered sensorium should be given only intravenous fluids (Dextrose saline or normal saline) for at least 2-3 days.
Appendix - 3.
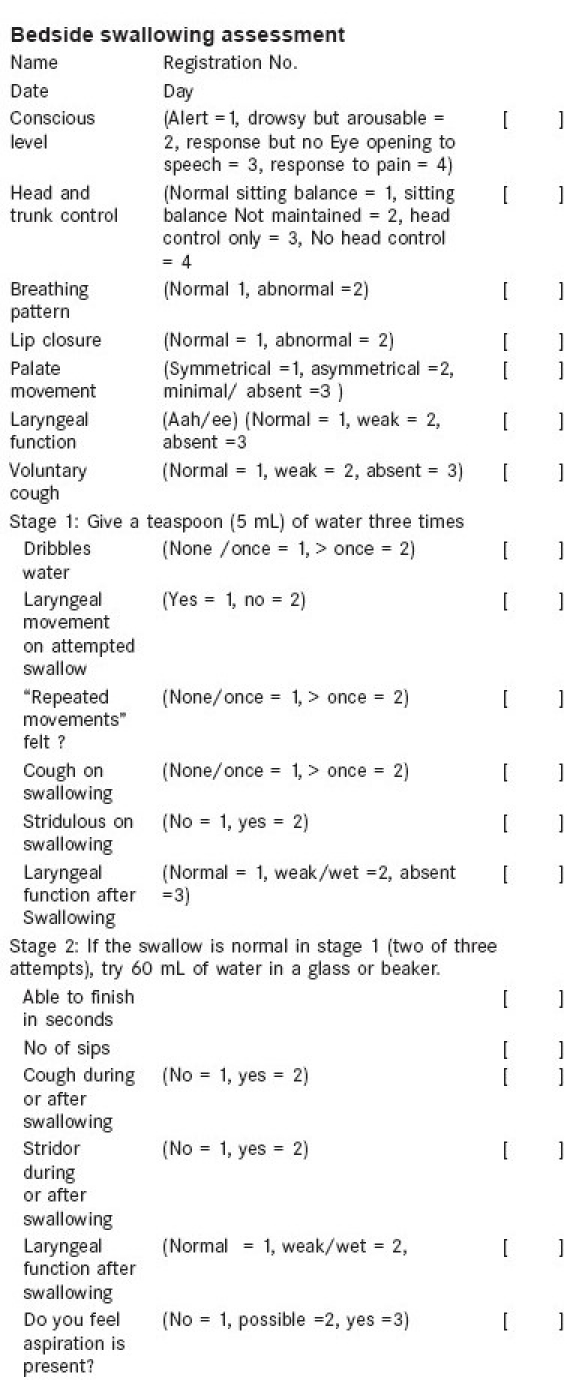
Evidence: Dennis,[73] Hamidon,[74] Norton,[75] Paciaroni,[76] Smithard.[77]
Oral care
All stroke patients should have an oral/dental assessment including dentures, signs of dental disease, etc., upon or soon after admission.
For patients wearing a full or partial denture, it should be determined if they have the neuromotor skills to safely wear and use the appliance(s).
An appropriate oral care protocol should be used for every patient with stroke, including those who use dentures. The oral care protocol should address areas including frequency of oral care (twice per day or more), types of oral care products (toothpaste, floss and mouthwash) and specific management for patients with dysphagia.
If concerns are identified with oral health and/or appliances, patients should be referred to a dentist for consultation and management as soon as possible.
Evidence: Brady.[78]
Early mobilization
Passive full-range-of-motion exercises for paralyzed limbs can be started during the first 24 hours.
All patients should be referred to a physiotherapist/rehabilitation team as soon as possible, preferably within 48 hours of admission.
The patient's need in relation to moving and handling should be assessed within 48 hours of admission.
Nutrition
Every patient should have his/her nutritional status determined using valid nutritional screening method within 48 hours of admission.
Nutritional support should be considered in any malnourished patient.
Evidence: Davalos,[81] Gariballa,[82] Milne,[83] National Institute for Health and Clinical Excellence.[84]
Management of seizures
Patients with seizure, even single should be treated with loading dose of phenytoin (15-20 mg/kg) followed by maintenance dose 5 mg/kg per day for a period of at least 3 months. If needed, carbamazepine or sodium valproate may be added. Status epilepticus should be treated as per its guidelines. At present there is insufficient data to comment on the prophylactic administration of anticonvulsants to patients with recent stroke.
Venous thromboembolism
Prophylaxis
Patients with paralyzed legs (due to ischemic stroke) should be given standard heparin (5000 units subcutaneous b.d.) or low-molecular weight heparin (with appropriate prophylactic doses as per agent) to prevent deep vein thrombosis (DVT).
For those who cannot tolerate heparin, aspirin given for treatment is of some prophylactic value.
In patients with paralyzed legs (due to ICH), routine physiotherapy and early mobilization should be carried out to prevent leg vein thrombosis.
Early mobilization and optimal hydration should be maintained for all acute stroke patients.
CLOTS trial data does not support the routine use of thigh length graduated compression stockings for prevention of DVT.
Treatment
Standard heparin (5000 U i.v.) or low molecular weight heparin (with appropriate therapeutic doses as per agent) should be started initially. When standard heparin is used, a prior baseline complete blood count and a-PTT should be done and a rebolus (80 U/kg/h) and maintenance infusion (18 U/kg/h) should be given (target a-PTT of 1.5 times the control value).
Anticoagulation (warfarin 5 mg once daily) should be started simultaneously unless contraindicated and the dose should be adjusted subsequently to achieve a target INR of 2.5 (range 2.0-3.0), when heparin should be stopped.
Bladder care
An indwelling catheter should be avoided as far as possible and if used, indwelling catheters should be assessed daily and removed as soon as possible.
Intermittent catheterization should be used for urinary retention or incontinence.
The use of portable ultrasound is recommended as preferred non-invasive method for assessing post-void residual urine.
Evidence: Thomas[90]
Bowel care
Patient with bowel incontinence should be assessed for other causes of incontinence including impacted feces with spurious diarrhea.
Patients with severe constipation should have a drug review to minimize use of constipating drugs, be given advice on diet, fluid intake and exercise (as much as possible), be offered oral laxatives and be offered rectal laxatives only if severe problems remain.
Evidence: Coggrave[91]
Infections
Development of fever after stroke should prompt a search for pneumonia, urinary tract infection or DVT.
Prophylactic administration of antibiotics is not recommended.
Appropriate antibiotic therapy should be administered early (after taking relevant culture specimens).
Evidence: Chamorro.[92]
Discharge planning
Discharge planning should be initiated as soon as a patient is stable.
Patients and families should be prepared and fully involved.
Care givers should receive all necessary training in caring for it.
Patients should be given information about discharge issues and explained the need for and timing of follow up after discharge.
Secondary Prevention
This includes measures to reduce the risk of recurrence of stroke in patients who have had TIA or stroke. These guidelines apply to vast majority of patients with TIA or stroke, although some of the recommendations may not be appropriate for those with unusual causes of stroke, like trauma, infections, etc.
Every patient should be evaluated for modifiable risk factors within one week of onset. This includes:
Hypertension
Diabetes mellitus
Smoking
Carotid artery stenosis (for those with non-disabling stroke)
Atrial fibrillation or other arrhythmias
Structural cardiac disease
In any patient where no risk factor is found, consideration for investigating for rare causes may be given. The investigations may include anti-phospholipid antibodies, protein C,S and anti-thrombin III.
Evidence: Coull,[96] Johnston,[97] Koton,[98] Lovett.[99]
Antiplatelet therapy
All patients with ischemic stroke or TIA should receive antiplatelet therapy unless there is indication for anticoagulation.
Aspirin (30-300 mg/day) or combination of aspirin (25 mg) and extended release dipyridamole (200 mg) twice or clopidogrel (75 mg OD) are all acceptable options for initial therapy. The clinician should be guided by his own preference coupled with the affordability and tolerance of the patient.
In children, the maintenance dose of aspirin is 3-5 mg/kg per day.
Combined aspirin-extended release dipyridamole as well as clopidogrel is marginally more effective than aspirin in preventing vascular events.
The combination of aspirin and clopidogrel increases the risk of hemorrhage and is not recommended unless there is indication for this therapy (i.e., coronary stent or acute coronary syndromes).
Addition of proton pump inhibitor should not be routine and should only be considered when there is dyspepsia or other significant risk of gastrointesinal bleeding with aspirin.
Evidence: CAPRIE,[100] CHARISMA Bhatt et al,[101] ESPS,[102] ESPS-2,[103] ESPIRIT,[104] MATCH – Fisher.[105]
Anticoagulation
Anticoagulation should be started in every patient with atrial fibrillation (valvular or non-valvular) unless contraindicated, if they are likely to be compliant with the required monitoring and are not at high risk for bleeding. Aspirin also provides some protection if there are constraints to the use of oral anticoagulation. [Table 1].
Anticoagulation should be considered for all patients who have ischemic stroke associated with mitral valve disease, prosthetic heart valves, or within 3 months of myocardial infarction.
Anticoagulation should not be started until brain imaging has excluded hemorrhage, and 14 days have passed from the onset of a disabling ischemic stroke (except when a demonstrable intracardiac thrombus is present).
Anticoagulation should not be used for patients in sinus rhythm unless cardiac embolism is suspected.
For effective anticoagulation target, INR is 2.5 (range 2.0-3.0) except for mechanical cardiac valves (3.0: range 2.5-3.5).
Evidence: Antithrombotic Trialists’ Collaboration,[106] De Schryver,[107] ESPRIT,[104] Hankey,[108] Ringleb,[109] Saxena.[110]
Blood pressure lowering
Blood pressure lowering treatment is recommended for all patients with history of TIA or stroke. The benefit extends to persons with or without a history of hypertension. The treatment should be initiated (or modified) prior to discharge from hospital in hospitalized and at the time of first medical assessment in non-hospitalized patients.
An optimal target for these patients is 130/80 mmHg, but for patients known to have bilateral severe (>70%) internal carotid artery stenosis, SBP of 150 mmHg may be appropriate.
The optimal drug regimen is uncertain; however the available data supports the use of diuretics or the combination of diuretics and an ACEI.
Evidence: ALLAHAT,[111] Blood Pressure Lowering Treatment Trialists’ Collaboration,[112] EXPRESS – Rothwell,[113] HOPE,[114] PROGRESS.[115]
Carotid intervention
Patients with TIA or non-disabling stroke and ipsilateral 70-99% internal carotid artery stenosis (measured by two concordant non-invasive imaging modalities or on a catheter angiogram) should be offered carotid endarterectomy or stenting (see below) within 2 weeks of the incident event unless contraindicated.
Carotid intervention is recommended for selected patients with moderate (50-69%) stenosis in symptomatic patients.
Carotid ultrasound / angiogram should be performed on all patients who would be considered for carotid endarterectomy or angioplasty.
Carotid endarterectomy should be performed by a surgeon with a known perioperative morbidity and mortality of <6%.
Carotid angioplasty and/or stenting should be considered for patients who are not operative candidates for technical, anatomic or medical reasons or when adequate surgical expertise is not available.
Carotid intervention is not recommended for patients with mild (<50%) stenosis.
All those with carotid stenosis should receive all secondary prevention measures, whether or not they receive carotid intervention.
Evidence: Cina,[116] ECST,[117] Ederle,[118] Fairhead,[119] NASCET - Eliasziw,[120] Inzitari,[121] Paty,[122] Rothwell.[123]
Lipid lowering therapy
All patients with history of TIA or ischemic stroke should be treated with a statin if they have a total cholesterol of > 200 mg%, or LDL cholesterol > 100 mg%.
The treatment goals should be a total cholesterol of <200 mg%, and LDL cholesterol of <100 mg% (<70 mg% for very high risk individuals).
Treatment with statin therapy should be avoided or used with caution in patients with history of hemorrhgic stroke.
Evidence: Baigent,[124] Collins,[125] HPS,[126] SPARCL - Amarenco.[127,128]
Lifestyle measures
All patients who smoke should be advised to stop smoking and to avoid environmental smoke.
All patients who can do regular exercise should be advised to do so for at least 30 minutes each day. They should be advised to start with low intensity exercise and gradually increase to moderate levels (sufficient to become slightly breathless).
All patients should be advised to use low fat dairy products and products based on vegetable and plant oils, and reduce intake of red meat.
Patients’ body mass index or waist circumference should be measured, and those who are overweight or obese should be offered advice and support to lose weight.
All patients, but especially those with hypertension, should be advised to reduce their salt intake by not adding extra table salt to food, using as little as possible in cooking, and avoiding preserved foods, pickles etc. and choosing low salt foods.
Patients who drink alcohol should be advised to keep within recognized safe drinking limits of no more than three units per day for men and two units per day for women.
Evidence: Brunner,[129] He,[130] Hooper,[131] Lancaster,[132] Rice,[133] Silagy,[134] Toole,[135] Wang.[136]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue-type plasminogen activator for treatment of acute stroke: The Standard Treatment with Alteplase to Reverse Stroke study. JAMA. 2000;283:1145–50. doi: 10.1001/jama.283.9.1145. [DOI] [PubMed] [Google Scholar]
- 3.Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al. Recommendations for the establishment of primary stroke centers.Brain Attack Coalition. JAMA. 2000;283:3102–9. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 4.Audebert HJ, Schenkel J, Heuschmann PU, Bogdahn U, Haberl RL. Effects of the implementation of a telemedical stroke network: The Telemedic Pilot Project for Integrative Stroke Care in Bavaria, Germany. Lancet Neurol. 2006;5:742–8. doi: 10.1016/S1474-4422(06)70527-0. [DOI] [PubMed] [Google Scholar]
- 5.Calvet D, Lamy C, Touzé E, Oppenheim C, Meder J-F, Mas J-L. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis. 2007;24:80–5. doi: 10.1159/000103120. [DOI] [PubMed] [Google Scholar]
- 6.Evans A, Perez I, Harraf F, Melbourn A, Steadman J, Donaldson N, et al. Can differences in management processes explain different outcomes between stroke unit and stroke-team care? Lancet. 2001;358:1586–92. doi: 10.1016/S0140-6736(01)06652-1. [DOI] [PubMed] [Google Scholar]
- 7.National clinical guidelines for stroke. Clinical Effectiveness & Evaluation Unit, Royal College of Physicians; 2004. Stroke IWP for, Unit RC of P of LCE and E. [Google Scholar]
- 8.Katzan IL, Hammer MD, Furlan AJ, Hixson ED, Nadzam DM. Quality improvement and tissue-type plasminogen activator for acute ischemic stroke: A Cleveland update. Stroke. 2003;34:799–800. doi: 10.1161/01.STR.0000056944.42686.1E. [DOI] [PubMed] [Google Scholar]
- 9.Koton S, Schwammenthal Y, Merzeliak O, Philips T, Tsabari R, Bruk B, et al. Effectiveness of establishing a dedicated acute stroke unit in routine clinical practice in Israel. Isr Med Assoc J. 2005;7:688–93. [PubMed] [Google Scholar]
- 10.LaMonte MP, Bahouth MN, Hu P, Pathan MY, Yarbrough KL, Gunawardane R, et al. Telemedicine for acute stroke: Triumphs and pitfalls. Stroke. 2003;34:725–8. doi: 10.1161/01.STR.0000056945.36583.37. [DOI] [PubMed] [Google Scholar]
- 11.Prabhakaran S, Chong JY, Sacco RL. Impact of abnormal diffusion-weighted imaging results on short-term outcome following transient ischemic attack. Arch Neurol. 2007;64:1105–9. doi: 10.1001/archneur.64.8.1105. [DOI] [PubMed] [Google Scholar]
- 12.Purroy F, Montaner J, Rovira A, Delgado P, Quintana M, Alvarez-Sabín J. Higher risk of further vascular events among transient ischemic attack patients with diffusion-weighted imaging acute ischemic lesions. Stroke. 2004;35:2313–9. doi: 10.1161/01.STR.0000141703.21173.91. [DOI] [PubMed] [Google Scholar]
- 13.Rønning OM, Guldvog B, Stavem K. The benefit of an acute stroke unit in patients with intracranial haemorrhage: A controlled trial. J Neurol Neurosurg Psychiatr. 2001;70:631–4. doi: 10.1136/jnnp.70.5.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva Y, Puigdemont M, Castellanos M, Serena J, Suñer RM, García MM, et al. Semi-intensive monitoring in acute stroke and long-term outcome. Cerebrovasc Dis. 2005;19:23–30. doi: 10.1159/000081908. [DOI] [PubMed] [Google Scholar]
- 15.Stavem K, Rønning OM. Quality of life 6 months after acute stroke: Impact of initial treatment in a stroke unit and general medical wards. Cerebrovasc Dis. 2007;23:417–23. doi: 10.1159/000101465. [DOI] [PubMed] [Google Scholar]
- 16.Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2004;4:CD000197. doi: 10.1002/14651858.CD000197.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Bray JE, Coughlan K, Bladin C. Can the ABCD Score be dichotomised to identify high-risk patients with transient ischaemic attack in the emergency department? Emerg Med J. 2007;24:92–5. doi: 10.1136/emj.2006.041624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cucchiara BL, Messe SR, Taylor RA, Pacelli J, Maus D, Shah Q, et al. Is the ABCD score useful for risk stratification of patients with acute transient ischemic attack? Stroke. 2006;37:1710–4. doi: 10.1161/01.STR.0000227195.46336.93. [DOI] [PubMed] [Google Scholar]
- 19.Lavallée PC, Meseguer E, Abboud H, Cabrejo L, Olivot J-M, Simon O, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): Feasibility and effects. Lancet Neurol. 2007;6:953–60. doi: 10.1016/S1474-4422(07)70248-X. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell PM, Giles MF, Flossmann E, Lovelock CE, Redgrave JN, Warlow CP, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005;366:29–36. doi: 10.1016/S0140-6736(05)66702-5. [DOI] [PubMed] [Google Scholar]
- 21.Wardlaw JM, Seymour J, Cairns J, Keir S, Lewis S, Sandercock P. Immediate computed tomography scanning of acute stroke is cost-effective and improves quality of life. Stroke. 2004;35:2477–83. doi: 10.1161/01.STR.0000143453.78005.44. [DOI] [PubMed] [Google Scholar]
- 22.CAST: Randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (Chinese Acute Stroke Trial) Collaborative Group. Lancet. 1997;349:1641–9. [PubMed] [Google Scholar]
- 23.Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: Pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–74. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 24.Hill MD, Buchan AM. Thrombolysis for acute ischemic stroke: Results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172:1307–12. doi: 10.1503/cmaj.1041561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whiteley W, Lindley R, Wardlaw J, Sandercock P. Third international stroke trial. Int J Stroke. 2006;1:172–6. doi: 10.1111/j.1747-4949.2006.00043.x. [DOI] [PubMed] [Google Scholar]
- 26.Altepase for the treatment of acute ischaemic stroke (TA 122) London: NICE; 2007. National Institute for Health and Clinical Excellence. [Google Scholar]
- 27.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 28.Gupta R, Connolly ES, Mayer S, Elkind MS. Hemicraniectomy for massive middle cerebral artery territory infarction: A systematic review. Stroke. 2004;35:539–43. doi: 10.1161/01.STR.0000109772.64650.18. [DOI] [PubMed] [Google Scholar]
- 29.Jüttler E, Schwab S, Schmiedek P, Unterberg A, Hennerici M, Woitzik J, et al. Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery (DESTINY): A randomized, controlled trial. Stroke. 2007;38:2518–25. doi: 10.1161/STROKEAHA.107.485649. [DOI] [PubMed] [Google Scholar]
- 30.Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: A pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6:215–22. doi: 10.1016/S1474-4422(07)70036-4. [DOI] [PubMed] [Google Scholar]
- 31.Dávalos A, Castillo J, Alvarez-Sabín J, Secades JJ, Mercadal J, López S, et al. Oral citicoline in acute ischemic stroke: An individual patient data pooling analysis of clinical trials. Stroke. 2002;33:2850–7. doi: 10.1161/01.str.0000038691.03334.71. [DOI] [PubMed] [Google Scholar]
- 32.Muir KW, Lees KR, Ford I, Davis S. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): Randomised controlled trial. Lancet. 2004;363:439–45. doi: 10.1016/S0140-6736(04)15490-1. [DOI] [PubMed] [Google Scholar]
- 33.Shuaib A, Lees KR, Lyden P, Grotta J, Davalos A, Davis SM, et al. NXY-059 for the treatment of acute ischemic stroke. N Engl J Med. 2007;357:562–71. doi: 10.1056/NEJMoa070240. [DOI] [PubMed] [Google Scholar]
- 34.Cartmill M, Dolan G, Byrne JL, Byrne PO. Prothrombin complex concentrate for oral anticoagulant reversal in neurosurgical emergencies. Br J Neurosurg. 2000;14:458–61. doi: 10.1080/02688690050175265. [DOI] [PubMed] [Google Scholar]
- 35.Goldstein JN, Thomas SH, Frontiero V, Joseph A, Engel C, Snider R, et al. Timing of fresh frozen plasma administration and rapid correction of coagulopathy in warfarin-related intracerebral hemorrhage. Stroke. 2006;37:151–5. doi: 10.1161/01.STR.0000195047.21562.23. [DOI] [PubMed] [Google Scholar]
- 36.Huttner HB, Schellinger PD, Hartmann M, Köhrmann M, Juettler E, Wikner J, et al. Hematoma growth and outcome in treated neurocritical care patients with intracerebral hemorrhage related to oral anticoagulant therapy: Comparison of acute treatment strategies using vitamin K, fresh frozen plasma, and prothrombin complex concentrates. Stroke. 2006;37:1465–70. doi: 10.1161/01.STR.0000221786.81354.d6. [DOI] [PubMed] [Google Scholar]
- 37.Fredriksson K, Norrving B, Strömblad LG. Emergency reversal of anticoagulation after intracerebral hemorrhage. Stroke. 1992;23:972–7. doi: 10.1161/01.str.23.7.972. [DOI] [PubMed] [Google Scholar]
- 38.Yasaka M, Minematsu K, Naritomi H, Sakata T, Yamaguchi T. Predisposing factors for enlargement of intracerebral hemorrhage in patients treated with warfarin. Thromb Haemost. 2003;89:278–83. [PubMed] [Google Scholar]
- 39.Gubitz G, Sandercock P, Counsell C. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev. 2004;3:CD000024. doi: 10.1002/14651858.CD000024.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Phan TG, Koh M, Wijdicks EF. Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Arch Neurol. 2000;57:1710–3. doi: 10.1001/archneur.57.12.1710. [DOI] [PubMed] [Google Scholar]
- 41.Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: A randomized study. J Neurosurg. 1989;70:530–5. doi: 10.3171/jns.1989.70.4.0530. [DOI] [PubMed] [Google Scholar]
- 42.Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage: A randomised trial. Lancet. 2005;365:387–97. doi: 10.1016/S0140-6736(05)17826-X. [DOI] [PubMed] [Google Scholar]
- 43.Prasad K, Mendelow AD, Gregson B. Surgery for primary supratentorial intracerebral haemorrhage. Cochrane Database Syst Rev. 2008;4:CD000200. doi: 10.1002/14651858.CD000200.pub2. [DOI] [PubMed] [Google Scholar]
- 44.Prasad K, Mendelow AD, Gregson B. Surgery for Primary Supratentorial Intracerebral Hematoma. A Meta-Analysis of 10 Randomized Controlled Trials. Stroke. 2009. Sep 24, [Cited 2011 Mar 10]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19797178 .
- 45.Arauz A, Hoyos L, Espinoza C, Cantú C, Barinagarrementeria F, Román G. Dissection of cervical arteries: Long-term follow-up study of 130 consecutive cases. Cerebrovasc Dis. 2006;22:150–4. doi: 10.1159/000093244. [DOI] [PubMed] [Google Scholar]
- 46.Desfontaines P, Despland PA. Dissection of the internal carotid artery: Aetiology, symptomatology, clinical and neurosonological follow-up, and treatment in 60 consecutive cases. Acta Neurol Belg. 1995;95:226–34. [PubMed] [Google Scholar]
- 47.Han DH, Kwon OK, Oh CW. Clinical characteristics of vertebrobasilar artery dissection. Neurol Med Chir (Tokyo) 1998;38:107–13. doi: 10.2176/nmc.38.suppl_107. [DOI] [PubMed] [Google Scholar]
- 48.Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Cochrane Database Syst Rev. 2003;3:CD000255. doi: 10.1002/14651858.CD000255. [DOI] [PubMed] [Google Scholar]
- 49.Butler AC, Tait RC. Restarting anticoagulation in prosthetic heart valve patients after intracranial haemorrhage: A 2-year follow-up. Br J Haematol. 1998;103:1064–6. doi: 10.1046/j.1365-2141.1998.01078.x. [DOI] [PubMed] [Google Scholar]
- 50.Evans A, Perez I, Yu G, Kalra L. Should stroke subtype influence anticoagulation decisions to prevent recurrence in stroke patients with atrial fibrillation? Stroke. 2001;32:2828–32. doi: 10.1161/hs1201.099520. [DOI] [PubMed] [Google Scholar]
- 51.Hart RG, Palacio S, Pearce LA. Atrial fibrillation, stroke, and acute antithrombotic therapy: Analysis of randomized clinical trials. Stroke. 2002;33:2722–7. doi: 10.1161/01.str.0000035735.49388.4a. [DOI] [PubMed] [Google Scholar]
- 52.Antithrombotic therapy (36) Edinburgh: SIGN; 1999. AScottish Intercollegiate Guidelines Network. [Google Scholar]
- 53.Bousser M-G, Ferro JM. Cerebral venous thrombosis: An update. Lancet Neurol. 2007;6:162–70. doi: 10.1016/S1474-4422(07)70029-7. [DOI] [PubMed] [Google Scholar]
- 54.Stam J, De Bruijn SF, DeVeber G. Anticoagulation for cerebral sinus thrombosis. Cochrane Database Syst Rev. 2002;4:CD002005. doi: 10.1002/14651858.CD002005. [DOI] [PubMed] [Google Scholar]
- 55.Chiu EH, Liu C-S, Tan T-Y, Chang K-C. Venturi mask adjuvant oxygen therapy in severe acute ischemic stroke. Arch Neurol. 2006;63:741–4. doi: 10.1001/archneur.63.5.741. [DOI] [PubMed] [Google Scholar]
- 56.Rønning OM, Guldvog B. Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke. 1999;30:2033–7. doi: 10.1161/01.str.30.10.2033. [DOI] [PubMed] [Google Scholar]
- 57.Castillo J, Dávalos A, Noya M. Aggravation of acute ischemic stroke by hyperthermia is related to an excitotoxic mechanism. Cerebrovasc Dis. 1999;9:22–7. doi: 10.1159/000015891. [DOI] [PubMed] [Google Scholar]
- 58.Fukuda H, Kitani M, Takahashi K. Body temperature correlates with functional outcome and the lesion size of cerebral infarction. Acta Neurol Scand. 1999;100:385–90. doi: 10.1111/j.1600-0404.1999.tb01057.x. [DOI] [PubMed] [Google Scholar]
- 59.Hajat C, Hajat S, Sharma P. Effects of poststroke pyrexia on stroke outcome : A meta-analysis of studies in patients. Stroke. 2000;31:410–4. doi: 10.1161/01.str.31.2.410. [DOI] [PubMed] [Google Scholar]
- 60.Reith J, Jørgensen HS, Pedersen PM, Nakayama H, Raaschou HO, Jeppesen LL, et al. Body temperature in acute stroke: Relation to stroke severity, infarct size, mortality, and outcome. Lancet. 1996;347:422–5. doi: 10.1016/s0140-6736(96)90008-2. [DOI] [PubMed] [Google Scholar]
- 61.Ahmed N, Näsman P, Wahlgren NG. Effect of intravenous nimodipine on blood pressure and outcome after acute stroke. Stroke. 2000;31:1250–5. doi: 10.1161/01.str.31.6.1250. [DOI] [PubMed] [Google Scholar]
- 62.Bath PM, Willmot M, Leonardi-Bee J, Bath FJ. Nitric oxide donors (nitrates), L-arginine, or nitric oxide synthase inhibitors for acute stroke. Cochrane Database Syst Rev. 2002;4:CD000398. doi: 10.1002/14651858.CD000398. [DOI] [PubMed] [Google Scholar]
- 63.Horn J, Limburg M. Calcium antagonists for acute ischemic stroke. Cochrane Database Syst Rev. 2000;2:CD001928. doi: 10.1002/14651858.CD001928. [DOI] [PubMed] [Google Scholar]
- 64.Schrader J, Lüders S, Kulschewski A, Berger J, Zidek W, Treib J, et al. The ACCESS Study: Evaluation of Acute Candesartan Cilexetil Therapy in Stroke Survivors. Stroke. 2003;34:1699–703. doi: 10.1161/01.STR.0000075777.18006.89. [DOI] [PubMed] [Google Scholar]
- 65.Bruno A, Biller J, Adams HP, Jr, Clarke WR, Woolson RF, Williams LS, et al. Acute blood glucose level and outcome from ischemic stroke. Trial of ORG 10172 in Acute Stroke Treatment (TOAST) Investigators. Neurology. 1999;52:280–4. doi: 10.1212/wnl.52.2.280. [DOI] [PubMed] [Google Scholar]
- 66.Gray CS, Hildreth AJ, Sandercock PA, O’Connell JE, Johnston DE, Cartlidge NEF, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: The UK Glucose Insulin in Stroke Trial (GIST-UK) Lancet Neurol. 2007;6:397–406. doi: 10.1016/S1474-4422(07)70080-7. [DOI] [PubMed] [Google Scholar]
- 67.Type 2 diabetes: National clinical guideline for management in primary and secondary care (CG066) London: NICE; 2008. National Institute for Health and Clinical Excellence. [Google Scholar]
- 68.Bereczki D, Liu M, do Prado GF, Fekete I. Mannitol for acute stroke. Cochrane Database Syst Rev. 2001;1:CD001153. doi: 10.1002/14651858.CD001153. [DOI] [PubMed] [Google Scholar]
- 69.Broderick JP, Hacke W. Treatment of acute ischemic stroke: Part II: Neuroprotection and medical management. Circulation. 2002;106:1736–40. doi: 10.1161/01.cir.0000030407.10591.35. [DOI] [PubMed] [Google Scholar]
- 70.Qizilbash N, Lewington SL, Lopez-Arrieta JM. Corticosteroids for acute ischaemic stroke. Cochrane Database Syst Rev. 2002;2:CD000064. doi: 10.1002/14651858.CD000064. [DOI] [PubMed] [Google Scholar]
- 71.Tyson SF, Nightingale P. The effects of position on oxygen saturation in acute stroke: A systematic review. Clin Rehabil. 2004;18:863–71. doi: 10.1191/0269215504cr840oa. [DOI] [PubMed] [Google Scholar]
- 72.Turkington PM, Bamford J, Wanklyn P, Elliott MW. Prevalence and predictors of upper airway obstruction in the first 24 hours after acute stroke. Stroke. 2002;33:2037–42. doi: 10.1161/01.str.0000023576.94311.27. [DOI] [PubMed] [Google Scholar]
- 73.Dennis M, Lewis S, Cranswick G, Forbes J. FOOD: A multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke. Health Technol Assess. 2006;10:1–120. doi: 10.3310/hta10020. [DOI] [PubMed] [Google Scholar]
- 74.Hamidon BB, Nabil I, Raymond AA. Risk factors and outcome of dysphagia after an acute ischaemic stroke. Med J Malaysia. 2006;61:553–7. [PubMed] [Google Scholar]
- 75.Norton B, Homer-Ward M, Donnelly MT, Long RG, Holmes GK. A randomised prospective comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding after acute dysphagic stroke. BMJ. 1996;312:13–6. doi: 10.1136/bmj.312.7022.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, et al. Dysphagia following Stroke. Eur Neurol. 2004;51:162–7. doi: 10.1159/000077663. [DOI] [PubMed] [Google Scholar]
- 77.Smithard DG, Smeeton NC, Wolfe CD. Long-term outcome after stroke: Does dysphagia matter? Age Ageing. 2007;36:90–4. doi: 10.1093/ageing/afl149. [DOI] [PubMed] [Google Scholar]
- 78.Brady M, Furlanetto D, Hunter RV, Lewis S, Milne V. Staff-led interventions for improving oral hygiene in patients following stroke. Cochrane Database Syst Rev. 2006;4:CD003864. doi: 10.1002/14651858.CD003864.pub2. [DOI] [PubMed] [Google Scholar]
- 79.Fang Y, Chen X, Li H, Lin J, Huang R, Zeng J. A study on additional early physiotherapy after stroke and factors affecting functional recovery. Clin Rehabil. 2003;17:608–17. doi: 10.1191/0269215503cr655oa. [DOI] [PubMed] [Google Scholar]
- 80.Richards CL, Malouin F, Wood-Dauphinee S, Williams JI, Bouchard JP, Brunet D. Task-specific physical therapy for optimization of gait recovery in acute stroke patients. Arch Phys Med Rehabil. 1993;74:612–20. doi: 10.1016/0003-9993(93)90159-8. [DOI] [PubMed] [Google Scholar]
- 81.Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996;27:1028–32. doi: 10.1161/01.str.27.6.1028. [DOI] [PubMed] [Google Scholar]
- 82.Gariballa SE, Parker SG, Taub N, Castleden CM. A randomized, controlled, a single-blind trial of nutritional supplementation after acute stroke. JPEN J Parenter Enteral Nutr. 1998;22:315–9. doi: 10.1177/0148607198022005315. [DOI] [PubMed] [Google Scholar]
- 83.Milne AC, Potter J, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2002;3:CD003288. doi: 10.1002/14651858.CD003288. [DOI] [PubMed] [Google Scholar]
- 84.Nutrition support in adults (CG32) London: NICE; 2006. National Institute for Health and Clinical Excellence. [Google Scholar]
- 85.Meierkord H, Boon P, Engelsen B, Göcke K, Shorvon S, Tinuper P, et al. EFNS guideline on the management of status epilepticus. Eur J Neurol. 2006;13:445–50. doi: 10.1111/j.1468-1331.2006.01397.x. [DOI] [PubMed] [Google Scholar]
- 86.Passero S, Rocchi R, Rossi S, Ulivelli M, Vatti G. Seizures after spontaneous supratentorial intracerebral hemorrhage. Epilepsia. 2002;43:1175–80. doi: 10.1046/j.1528-1157.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 87.Vespa PM, O’Phelan K, Shah M, Mirabelli J, Starkman S, Kidwell C, et al. Acute seizures after intracerebral hemorrhage: A factor in progressive midline shift and outcome. Neurology. 2003;60:1441–6. doi: 10.1212/01.wnl.0000063316.47591.b4. [DOI] [PubMed] [Google Scholar]
- 88.Berge E, Sandercock P. Anticoagulants versus antiplatelet agents for acute ischaemic stroke. Cochrane Database Syst Rev. 2002;4:CD003242. doi: 10.1002/14651858.CD003242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bath PM, England TJ. Thigh-length compression stockings and DVT after stroke. Lancet. 2009;373:1923–4. doi: 10.1016/S0140-6736(09)60990-9. [DOI] [PubMed] [Google Scholar]
- 90.Thomas LH, Cross S, Barrett J, French B, Leathley M, Sutton CJ, et al. Treatment of urinary incontinence after stroke in adults. Cochrane Database Syst Rev. 2008;1:CD004462. doi: 10.1002/14651858.CD004462.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Coggrave M, Wiesel PH, Norton C. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev. 2006;2:CD002115. doi: 10.1002/14651858.CD002115.pub3. [DOI] [PubMed] [Google Scholar]
- 92.Chamorro A, Horcajada JP, Obach V, Vargas M, Revilla M, Torres F, et al. The Early Systemic Prophylaxis of Infection After Stroke study: A randomized clinical trial. Stroke. 2005;36:1495–500. doi: 10.1161/01.STR.0000170644.15504.49. [DOI] [PubMed] [Google Scholar]
- 93.Gräsel E, Schmidt R, Biehler J, Schupp W. Long-term effects of the intensification of the transition between inpatient neurological rehabilitation and home care of stroke patients. Clin Rehabil. 2006;20:577–83. doi: 10.1191/0269215506cr978oa. [DOI] [PubMed] [Google Scholar]
- 94.Langhorne P, Taylor G, Murray G, Dennis M, Anderson C, Bautz-Holter E, et al. Early supported discharge services for stroke patients: A meta-analysis of individual patients’ data. Lancet. 2005;365:501–6. doi: 10.1016/S0140-6736(05)17868-4. [DOI] [PubMed] [Google Scholar]
- 95.Larsen T, Olsen TS, Sorensen J. Early home-supported discharge of stroke patients: A health technology assessment. Int J Technol Assess Health Care. 2006;22:313–20. doi: 10.1017/s0266462306051208. [DOI] [PubMed] [Google Scholar]
- 96.Coull AJ, Lovett JK, Rothwell PM. Oxford Vascular Study. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ. 2004;328:326. doi: 10.1136/bmj.37991.635266.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Johnston SC, Rothwell PM, Nguyen-Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369:283–92. doi: 10.1016/S0140-6736(07)60150-0. [DOI] [PubMed] [Google Scholar]
- 98.Koton S, Rothwell PM. Performance of the ABCD and ABCD2 scores in TIA patients with carotid stenosis and atrial fibrillation. Cerebrovasc Dis. 2007;24:231–5. doi: 10.1159/000104483. [DOI] [PubMed] [Google Scholar]
- 99.Lovett JK, Coull AJ, Rothwell PM. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology. 2004;62:569–73. doi: 10.1212/01.wnl.0000110311.09970.83. [DOI] [PubMed] [Google Scholar]
- 100.A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329–39. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 101.Bhatt DL, Flather MD, Hacke W, Berger PB, Black HR, Boden WE, et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial. J Am Coll Cardiol. 2007;49:1982–8. doi: 10.1016/j.jacc.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 102.The European Stroke Prevention Study (ESPS). Principal endpoints. The ESPS Group. Lancet. 1987;2:1351–4. [PubMed] [Google Scholar]
- 103.Second European Stroke Prevention Study. ESPS-2 Working Group. J Neurol. 1992;239:299–301. doi: 10.1007/BF00867583. [DOI] [PubMed] [Google Scholar]
- 104.Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): Randomised controlled trial. Lancet. 2006;367:1665–73. doi: 10.1016/S0140-6736(06)68734-5. [DOI] [PubMed] [Google Scholar]
- 105.Fisher M, Davalos A. The MATCH study results in the context of secondary stroke prevention. Stroke. 2004;35:2609. doi: 10.1161/01.STR.0000145051.05149.99. [DOI] [PubMed] [Google Scholar]
- 106.Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.De Schryver EL, Algra A, van Gijn J. Dipyridamole for preventing stroke and other vascular events in patients with vascular disease. Cochrane Database Syst Rev. 2007;3:CD001820. doi: 10.1002/14651858.CD001820.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hankey GJ, Sudlow CL, Dunbabin DW. Thienopyridine derivatives (ticlopidine, clopidogrel) versus aspirin for preventing stroke and other serious vascular events in high vascular risk patients. Cochrane Database Syst Rev. 2000;2:CD001246. doi: 10.1002/14651858.CD001246. [DOI] [PubMed] [Google Scholar]
- 109.Ringleb PA, Bhatt DL, Hirsch AT, Topol EJ, Hacke W. Benefit of clopidogrel over aspirin is amplified in patients with a history of ischemic events. Stroke. 2004;35:528–32. doi: 10.1161/01.STR.0000110221.54366.49. [DOI] [PubMed] [Google Scholar]
- 110.Saxena R, Koudstaal PJ. Anticoagulants for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischaemic attack. Cochrane Database Syst Rev. 2004;2:CD000185. doi: 10.1002/14651858.CD000185.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) JAMA. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 112.Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: Results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–35. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 113.Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JNE, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): A prospective population-based sequential comparison. Lancet. 2007;370:1432–42. doi: 10.1016/S0140-6736(07)61448-2. [DOI] [PubMed] [Google Scholar]
- 114.Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145–53. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 115.Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41. doi: 10.1016/S0140-6736(01)06178-5. [DOI] [PubMed] [Google Scholar]
- 116.Cina CS, Clase CM, Haynes RB. Carotid endarterectomy for symptomatic carotid stenosis. Cochrane Database Syst Rev. 2000;2:CD001081. doi: 10.1002/14651858.CD001081. [DOI] [PubMed] [Google Scholar]
- 117.Randomised trial of endarterectomy for recently symptomatic carotid stenosis: Final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–87. [PubMed] [Google Scholar]
- 118.Ederle J, Featherstone RL, Brown MM. Percutaneous transluminal angioplasty and stenting for carotid artery stenosis. Cochrane Database Syst Rev. 2007;4:CD000515. doi: 10.1002/14651858.CD000515.pub3. [DOI] [PubMed] [Google Scholar]
- 119.Fairhead JF, Rothwell PM. The need for urgency in identification and treatment of symptomatic carotid stenosis is already established. Cerebrovasc Dis. 2005;19:355–8. doi: 10.1159/000085201. [DOI] [PubMed] [Google Scholar]
- 120.Eliasziw M, Spence JD, Barnett HJ. Carotid endarterectomy does not affect long-term blood pressure: Observations from the NASCET. North American Symptomatic Carotid Endarterectomy Trial. Cerebrovasc Dis. 1998;8:20–4. doi: 10.1159/000015819. [DOI] [PubMed] [Google Scholar]
- 121.Inzitari D, Eliasziw M, Gates P, Sharpe BL, Chan RK, Meldrum HE, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis.North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 2000;342:1693–700. doi: 10.1056/NEJM200006083422302. [DOI] [PubMed] [Google Scholar]
- 122.Paty PS, Darling RC, 3rd, Feustel PJ, Bernardini GL, Mehta M, Ozsvath KJ, et al. Early carotid endarterectomy after acute stroke. J Vasc Surg. 2004;39:148–54. doi: 10.1016/j.jvs.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 123.Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet. 2004;363:915–24. doi: 10.1016/S0140-6736(04)15785-1. [DOI] [PubMed] [Google Scholar]
- 124.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 125.Collins R, Armitage J, Parish S, Sleight P, Peto R. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004;363:757–67. doi: 10.1016/S0140-6736(04)15690-0. [DOI] [PubMed] [Google Scholar]
- 126.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: A randomised placebocontrolled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 127.Amarenco P, Bogousslavsky J, Callahan A, 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–59. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 128.Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A, 3rd, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007;38:3198–204. doi: 10.1161/STROKEAHA.107.493106. [DOI] [PubMed] [Google Scholar]
- 129.Brunner EJ, Rees K, Ward K, Burke M, Thorogood M. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2007;4:CD002128. doi: 10.1002/14651858.CD002128.pub3. [DOI] [PubMed] [Google Scholar]
- 130.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: Meta-analysis of cohort studies. Lancet. 2006;367:320–6. doi: 10.1016/S0140-6736(06)68069-0. [DOI] [PubMed] [Google Scholar]
- 131.Hooper L, Bartlett C, Davey SG, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database Syst Rev. 2004;1:CD003656. doi: 10.1002/14651858.CD003656.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2002;3:CD001292. doi: 10.1002/14651858.CD001292. [DOI] [PubMed] [Google Scholar]
- 133.Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev. 2004;1:CD001188. doi: 10.1002/14651858.CD001188.pub2. [DOI] [PubMed] [Google Scholar]
- 134.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2002;4:CD000146. doi: 10.1002/14651858.CD000146. [DOI] [PubMed] [Google Scholar]
- 135.Toole JF, Malinow MR, Chambless LE, Spence JD, Pettigrew LC, Howard VJ, et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: The Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA. 2004;291:565–75. doi: 10.1001/jama.291.5.565. [DOI] [PubMed] [Google Scholar]
- 136.Wang C, Harris WS, Chung M, Lichtenstein AH, Balk EM, Kupelnick B, et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: A systematic review. Am J Clin Nutr. 2006;84:5–17. doi: 10.1093/ajcn/84.1.5. [DOI] [PubMed] [Google Scholar]


