Abstract
Evidence supports the contribution of depression, anxiety, and poor social support to mortality of hospitalized myocardial infarction (MI) patients. The contribution of depression to survival is independent of disease severity. Pet ownership, a non-human form of social support, has also been associated with one year survival of post-MI patients. The current study addresses whether pet ownership contributes independently to long term survival beyond the contributions of depression, anxiety, or low social support in post-MI patients who have already survived at least 6 months. Data from patients (N = 460) enrolled in the “Psychosocial Responses in the Home Automated External Defibrillator Trial (PR-HAT)”were used. Seventeen patients died during a median follow-up of 2.8 years. In Cox proportional hazards regression model that included depression, lack of pet ownership, and the interaction between depression and lack of pet ownership, not owning a pet was the only significant independent predictor of mortality (p = 0.036). The interaction between pet ownership and depression tended to be significant indicating that the effect of pet ownership on survival in this group of people who have supportive spouses/companions living with them may relate to depression.
Keywords: Depression, Mortality, Psychosocial, Social support, Pet ownership
INTRODUCTION
The holistic perspective on cardiovascular health incorporates the contributions of psychological, social, and biological factors to the maintenance of health and conversely, the development and progression of chronic diseases (Audy, 1971; Lown, Verrier, and Carbalan, 1973; Skinner, 1981; Skinner, 1985; Luttik et al., 2005; Friedmann et al., 2006; Piotrowicz et al., 2007). Evidence from studies using a holistic approach to chronic disease development and progression supports the contributions of depression, anxiety, and social isolation to cardiovascular morbidity and mortality (Cossette, Frasure-Smith N., and Lesperance, 2001; Pelle et al., 2008; Thomas et al., 2008).
Considerable evidence supports the contribution of depression to mortality of patients with coronary heart disease (CHD) beyond the effects of demographics and disease severity (Welin, Lappas, and Wilhelmsen, 2000; Pfiffner & Hoffmann, 2004; van Melle et al., 2004; Frasure-Smith & Lesperance, 2008). In recognition of the causal association of depression with poor outcomes, the American Heart Association recently recognized depression as a risk factor meriting treatment in patients with CHD (Lichtman et al., 2008). Less evidence supports the contribution of anxiety to mortality in patients with CHD (Kawachi et al., 1994) or post-MI patients (Thomas et al., 1997; Friedmann et al., 2006; Frasure-Smith & Lesperance, 2008). However a recent meta-analysis concluded that anxiety predicts poorer outcomes, including mortality, in post-MI patients (Roest et al., 2010).
A number of epidemiological and observational studies concluded that low social support is associated with morbidity and mortality of post-MI patients (Ruberman et al., 1984; Ahern et al., 1990; Case et al., 1992; Berkman, Leo-Summers, and Horwitz, 1992; Thomas et al., 1997; Frasure-Smith et al., 2000; Welin, Lappas, & Wilhelmsen, 2000; Pfiffner & Hoffmann, 2004). Lower amount of social support independently predicts mortality beyond the contributions of co-morbidities and demographic variables in post-MI patients (Thomas et al., 1997; Welin, Lappas, & Wilhelmsen, 2000; Pfiffner & Hoffmann, 2004). Depression and low social support both independently predict long term mortality after MI (Welin, Lappas, & Wilhelmsen, 2000). High levels of social support also predicted improvement in depression over the first year in depressed post-MI patients (Frasure-Smith et al., 2000).
Companion animals provide a non-human source of social support that is distinct from social support from people (Friedmann & Thomas, 1995). Companion animals facilitate interaction with other people (Hart, 2000; Friedmann & Son, 2009), make people and situations appear less stressful (Friedmann & Son, 2009), and moderate cardiovascular stress responses (Friedmann, 2000; Allen, Shykoff, and Izzo, 2001; Friedmann & Son, 2009).
Epidemiological evidence supports the contribution of pet ownership to short term survival of patients with coronary heart disease. Pet ownership predicted one year survival of post-MI patients beyond the contributions of disease severity and human social support to survival in two groups of patients, patients who were hospitalized in a coronary care unit (Friedmann et al., 1980) and post-MI patients with ventricular arrhythmias (Friedmann & Thomas, 1995). In contrast, in a more recent study pet ownership was not related to the combined outcome of one year re-hospitalization or mortality in patients with acute coronary syndrome (Parker et al., 2010), which includes unstable angina as well as MI (Alpert et al., 2000; Achar, Kundu, and Norcross, 2005). The population with acute coronary syndrome was similar to the population in the first study that found an association of pet ownership with one year survival (Friedmann et al., 1980). In all of these studies the patients were recruited while hospitalized or shortly after hospitalization. The current study was conducted in stable rather than acute post-MI patients, a group in which the contribution of pet ownership to survival has not been investigated and at a time in the disease process when acute psychosocial stresses related to the acute coronary event should have subsided.
The purpose of the current study is to examine whether pet ownership contributes independently to the prediction of long term survival beyond the contributions of depression, anxiety, or low social support in post-MI patients who had already survived at least 6 months. It is a secondary analysis of data from patients enrolled in the “Psychosocial Responses in the Home Automated External Defibrillator Trial (PR-HAT)”.
METHODS
Recruitment
Patients and their spouses/companions who were enrolling in the NHLBI sponsored international Home Automated External Defibrillator Trial (HAT) at 30 sites in Australia (12), Canada (5), New Zealand (2), and the United States (11) were invited to participate in PR-HAT. Formal human subjects ethics approval was obtained at each participating institution. HAT was designed to test whether an automated external defibrillator (AED) in the homes of stable post-MI patients improved survival. Patients were eligible for recruitment into HAT if they had an anterior myocardial infarction a minimum of 6 months prior to recruitment. Complete HAT inclusion and exclusion criteria and recruitment methods have been published elsewhere (Bardy et al., 2008; Bardy et al., 2008).Participation in HAT required a spouse or companion living in the post-MI patient’s household who was physically capable of and willing to learn and use CPR and an AED. The HAT trial recruited patient-spouse pairs from January 2003 to October 2005 and randomized couples to either the CPR training or the CPR training/AED intervention group.
PR-HAT was an ancillary study to HAT and obtained data from a subgroup of the couples enrolled in HAT. PR-HAT was commenced after HAT, began recruitment in October 2003 and concluded recruitment simultaneously with HAT. PR-HAT required separate informed consent at enrollment. For enrollment in PR-HAT the patients were required to demonstrate a lack of significant cognitive impairment by scoring 17 or above on the Adult Lifestyles and Function Interview – Mini Mental State Examination (ALFI-MMSE) (Roccaforte et al., 1992; Newkirk et al., 2004). Patients were excluded from PR-HAT if they had been included in the quality of life sub-study of HAT due to concerns about participant burden.
Data Collection
Screening and baseline data collection for PR-HAT took place after recruitment into the HAT study. Couples who enrolled in HAT were asked if they would also be willing to participate in PR-HAT. If they were willing to do so, informed consent was obtained and patients completed the MMSE. If patients met the inclusion criteria, they then completed questionnaires to assess psychosocial status including depression, anxiety, social support, and pet ownership.
Instruments
The Beck Depression Inventory-2 (BDI-II) was used to assess depressive symptoms. The BDI-II consists of 21 items rated on a Likert (0–3) scale. Total BDI-II scores range from 0 to 63 with higher scores indicating increased depressive symptoms. The reliability and validity of the BDI is well established (Beck, Steer, and Garbin, 1988). Internal consistency of the scale is high, 0.86 to 0.88 among psychiatric patients and 0.81 in non-psychiatric patients (Beck, Stear, and Brown, 1996). There is ample evidence of construct and concurrent validity (Beck, Steer, & Garbin, 1988). Depression severity was categorized according to the BDI-II manual (Beck, Stear, & Brown, 1996) as absent (0–12), mild (13–19), moderate (20–28) or severe (≥ 29). Although the BDI-II measures the severity of depressive symptoms, a clinician-guided interview is required to make a diagnosis of clinical depression. Thus the outcome measure indicates depressive symptom severity but not major depressive disorder (Strik et al., 2001).
Spielberger’s State Trait Anxiety Inventory (STAI) was used to assess anxiety (Spielberger, Lushene, and Gorsuch, 1972). The state scale contains 20 items. Internal consistency reliability and concurrent validity are well established (Spielberger, Lushene, & Gorsuch, 1972). Anxiety scores range from 20 (none) to 80 (extreme). Cardiac patients with scores above 40 are considered to be anxious (Frasure-Smith, Lesperance, and Talajic, 1995). Thus the anxiety outcome measure indicates the severity of anxiety, although the diagnosis of general anxiety disorder requires clinician interview.
The Social support questionnaire – 6 (SSQ-6) was used to quantify both the amount of and satisfaction with social support perceived by the participant. The SSQ-6 provides a list of six circumstances potentially requiring social support and asked the respondent who they could rely on for help in each situation (amount) and how satisfied they would be with the help they received in each situation (satisfaction). The number of people providing each type of support is summed to obtain the amount of social support. Satisfaction with support is measured with a six point Likert scale ranging from dissatisfied to very satisfied. Total social support amount ranges from 0 to 54 and satisfaction ranges from 6 to 36 with higher scores indicating more social support. The internal reliability ranged from 0.90 and 0.93 for both amount of and satisfaction with social support on the SSQ-6 (Sarason et al., 1987). The reliability of the scale over two to three years exceeded 0.78 for both subscales. The SSQ-6 was validated by negative correlations with scales of lack of social support including the Multiple Affect Adjective Checklist loneliness scale, and the Lack of Protection Scale (Sarason et al., 1987).
A shortened version of the Pet Ownership Questionnaire (PO) developed to assess pet ownership status and attachment to pets among pet owners as a component of social support in our ancillary study in CAST (Friedmann & Thomas, 1995) was completed. The question “Do you currently have any pets?” and a list of the types/names of pets owned were used in the current study to obtain pet ownership status.
The ALFI –MMSE 26 item version of the mini mental status examination was used to establish eligibility of patients by assessing cognitive status during screening (Roccaforte et al., 1992; Newkirk et al., 2004) Validity of the ALFI-MMSE had been established with high correlation with the MMSE (Roccaforte et al., 1992; Newkirk et al., 2004). The MMSE is well validated in samples of elderly individuals with and without dementia or psychiatric disorders (Folstein, Folstein, and McHugh, 1975; Teng et al., 1987). Scores below 17 on the ALFI-MMSE indicate cognitive impairment (Roccaforte et al., 1992; Newkirk et al., 2004).
Statistical Analysis
Descriptive statistics including z-tests for skew and kurtosis and residual examination were utilized to examine the normality of the continuous outcomes prior to multivariate analyses. The skewed distribution of depression necessitated square root transformations and of anxiety necessitated log transformations, to generate normal distributions. The transformed variables were used for parametric statistical analysis.
Descriptive statistics were used to evaluate the frequency and severity of depression and anxiety. Separate Cox proportional hazards regression models were used to examine the contributions of depression, anxiety, social support, and pet ownership to survival. Each psychosocial variable that predicted survival with p < 0.20 in the initial Cox model and the interactions of these variables were then used in another Cox model. The p < 0.20 criterion for inclusion of predictors in models with multiple predictor variables minimizes bias that occurs with automatic stepwise selection and avoids under-selection of variables that occurs with a smaller criteria (Greenland, 1989). A-priori anxiety and depression were expected to be associated with worse survival and higher social support and pet ownership were expected to be associated with better survival. Therefore two-tailed p < 0.10 was considered significant.
Results
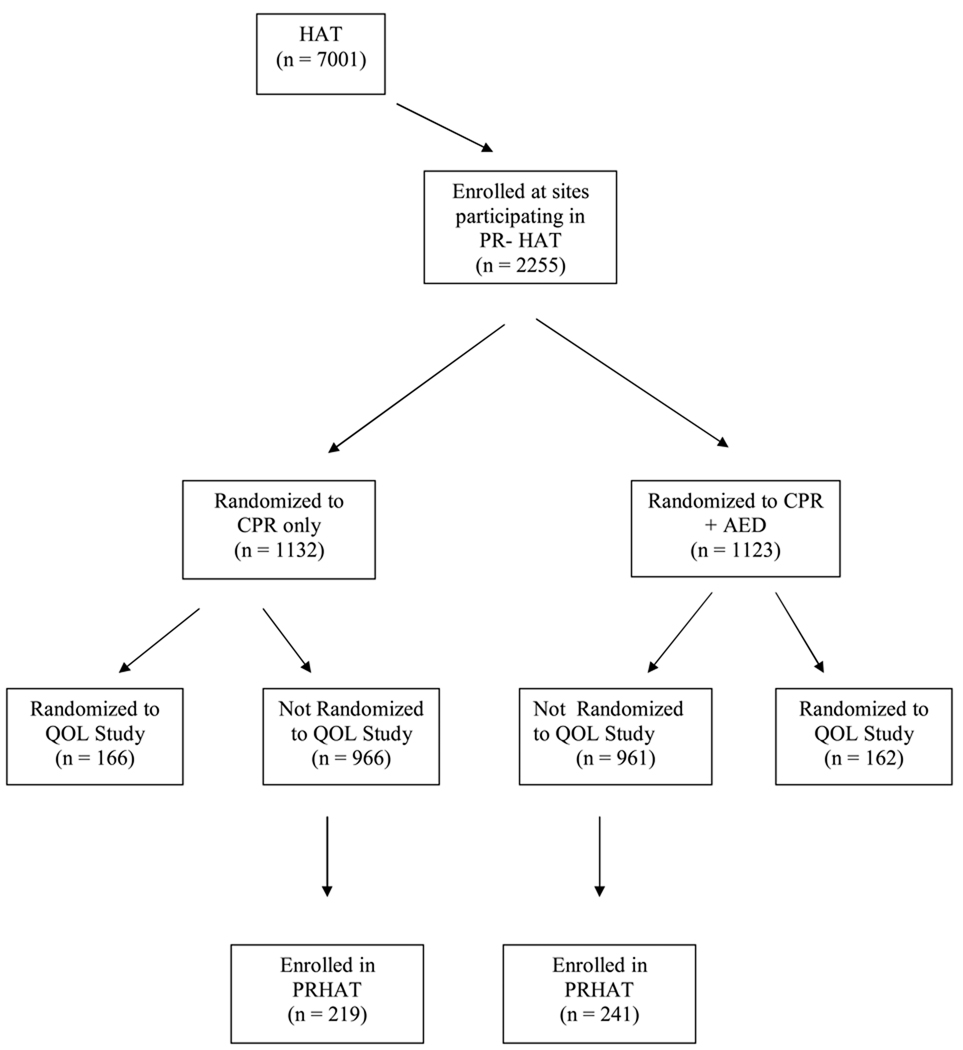
A total of 460 patients participated in the study. Figure 1 includes a consort diagram of the PR-HAT study within the context of HAT. Demographic, medical history, medication and cardiac data in patients enrolled in PR-HAT are shown in Table 1. Patients’ ages ranged from 33 to 84 years (mean = 61.09, sd = 9.69) and they were largely male (85.2%). All participants had a spouse or companion living with them who was willing to use a defibrillator and/or perform cardiopulmonary resuscitation if needed. Almost all of the participants (95%) were married. All patients had experienced a myocardial infarction (MI), approximately half had a history of hypertension, few were diabetic, and an overwhelming majority had no clinical features of heart failure. A large proportion of the patients had previous percutaneous coronary revascularization and/or coronary bypass grafting. All patients were receiving standard cardiac medications known to improve outcomes following MI and fewer than 10% were taking antidepressant medications.
Figure 1.
Consort diagram showing the relationship of enrollment in PR-HAT to enrollment in HAT. QOL = quality of life
Table 1.
Demographic and health characteristics of patients enrolled in PRHAT (N = 460)
| Characteristic | N (%) |
|---|---|
| Female | 68 (14.8) |
| White | 427 (92.8) |
| Married | 421 (91.5) |
| Unemployed | 206 (44.8) |
| Completed secondary school | 344 (74.8) |
| Medical history | |
| Hypertension | 228 (49.6) |
| Diabetes | 79 (17.2) |
| Hypercholesterolemia | 358 (77.8) |
| Stroke | 21 (4.6) |
| Cigarette smoking | 47 (10.2) |
| PCTAa | 300 (65.2) |
| CABGb | 118 (25.7) |
| NYHAc | |
| I | 352 (76.5) |
| II | 95 (20.7) |
| Medication | |
| β blocker d | 364 (79.1) |
| ACEe inhibitor | 314 (68.3) |
| ARBf | 52 (11.3) |
| Digoxin | 25 (5.4) |
| Statins | 412 (89.6) |
| Aspirin | 419 (91.1) |
| Other antiplatelet agents | 123 (30.8) |
| Antidepressant | 33 (7.0) |
percutanueous transluminal coronary angioplasty;
coronary artery bypass grafting ;
New York Heart Association heart failure class;
other than sotalol or amiodarone ;
angiotensin converting enzyme;
angiotensin II receptor blockers
The demographic and health characteristics of participants in the current study were compared to those in the HAT study and not in the PR-HAT study to see how well they represented the patients in the larger HAT study. Patients enrolled in PR-HAT were younger [means = 61.09 ± (9.69) vs 61.38 ± (9.77) years, Wilcoxon rank sum test z = 2.44, p = 0.014], more likely to be white [92.8 vs 88.4 %, χ2 (1) =8.114, p=0.0044], and had somewhat different health profiles than HAT participants not enrolled in PR-HAT. PR-HAT participants were more likely to be employed [55% vs 42%, χ2 (1) =31.61, p=0.0001], less likely to be diabetic [17.2% vs 21.8%, χ2 (1) = 5.15, p=0.0233], less likely to have NYHA class II (compared with class I) HF (20.7% vs 21.9 %, χ2 (1) =17.42, p=0.0001), more likely to have had percutanueous transluminal coronary angioplasty [65.2% vs 52.6%, χ2 (1) =26.90, p=0.0001], and more likely to take aspirin [91.1 vs 86.3%, χ2 (1) =8.13, p=0.0044] than those HAT participants who were not enrolled in PR-HAT.
At study entry, 25% of patients enrolled in PR-HAT were depressed (BDI-II score >13) and 21% were anxious (STAI score > 40). Summaries of psychosocial measures at initial assessment are in Table 2. Depression and anxiety were moderately highly correlated (r = 0.620, p < 0.001). Over half of the participants (59%) owned pets; 35% owned a dog and 33% owned a cat.
Table 2.
Psychosocial characteristics of patients enrolled in PRHAT (N = 460)
| Characteristic | N (%) | Range | Mean (SD) |
|---|---|---|---|
| Depression Score (BDI-II) | 453 | 0–41 | 8.28 (6.96) |
| Depressed (BDI-II ≥ 13) | 92 (20.31) | ||
| State Anxiety Score (STAI) | 453 | 20–71 | 31.68 (9.79) |
| Anxious (STAI ≥ 40) | 97 (21.41) | ||
| Social Support Score (SSQ-6) | |||
| Amount | 0–54 | 18.69(13.34) | |
| Satisfaction | 6–36 | 33.10 (4.37) | |
| Pet Ownership | |||
| Pet | 266 (58.7) | ||
| Dog | 159 (35.1) | ||
| Cat | 151 (33.3) |
BDI-II = Beck Depression Inventory –II; SSQ-6 = Social Support Questionniare-6; STAI = State Trait Anxiety Inventory
Seventeen patients died during a follow-up of 0 to 4.2 years, with a median follow up of 2.8 years. Cox proportional hazards regression with separate analyses for each predictor (See Table 3) indicated that depression (BDI-II score) was a significant predictor of mortality (HR = 1.53, p = 0.02). Pet ownership was the only other individual variable related to mortality at p < 0.20, the criteria for inclusion in the multivariable Cox regression. Pet owners were 67% less likely to die than non-owners (p = 0.16). Anxiety, low social support amount, and low social support satisfaction did not predict mortality at p < 0.20.
Table 3.
Summary of results of separate Cox proportional hazards regression models to predict mortality based on anxiety, depression, social support, and pet ownership.*
| B | SE | Wald | df | Sig. | HR | 90.0% CI for HR | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Depression (Sqrt) | 0.423 | 0.208 | 4.156 | 1 | 0.02 | 1.527 | 1.085 | 2.148 |
| Social Support Amount (sqrt) | 0.092 | 0.161 | 0.328 | 1 | 0.27 | 1.096 | 0.842 | 1.427 |
| Social Support Satisfaction (RLn) | −0.217 | 0.282 | 0.592 | 1 | 0.22 | 0.805 | 0.463 | 1.399 |
| State anxiety (Ln) | 0.269 | 0.845 | 0.101 | 1 | 0.38 | 1.308 | 0.326 | 5.250 |
| Pet Ownership | −0.514 | 0.518 | 0.986 | 1 | 0.16 | 0.598 | 0.222 | 1.401 |
All continuous variables were transformed to improve normality. Sqrt = square root; Ln = natural log; RLn = reflected natural log
Tests of significance and are one tailed in hypothesized direction; 90% confidence intervals are presented
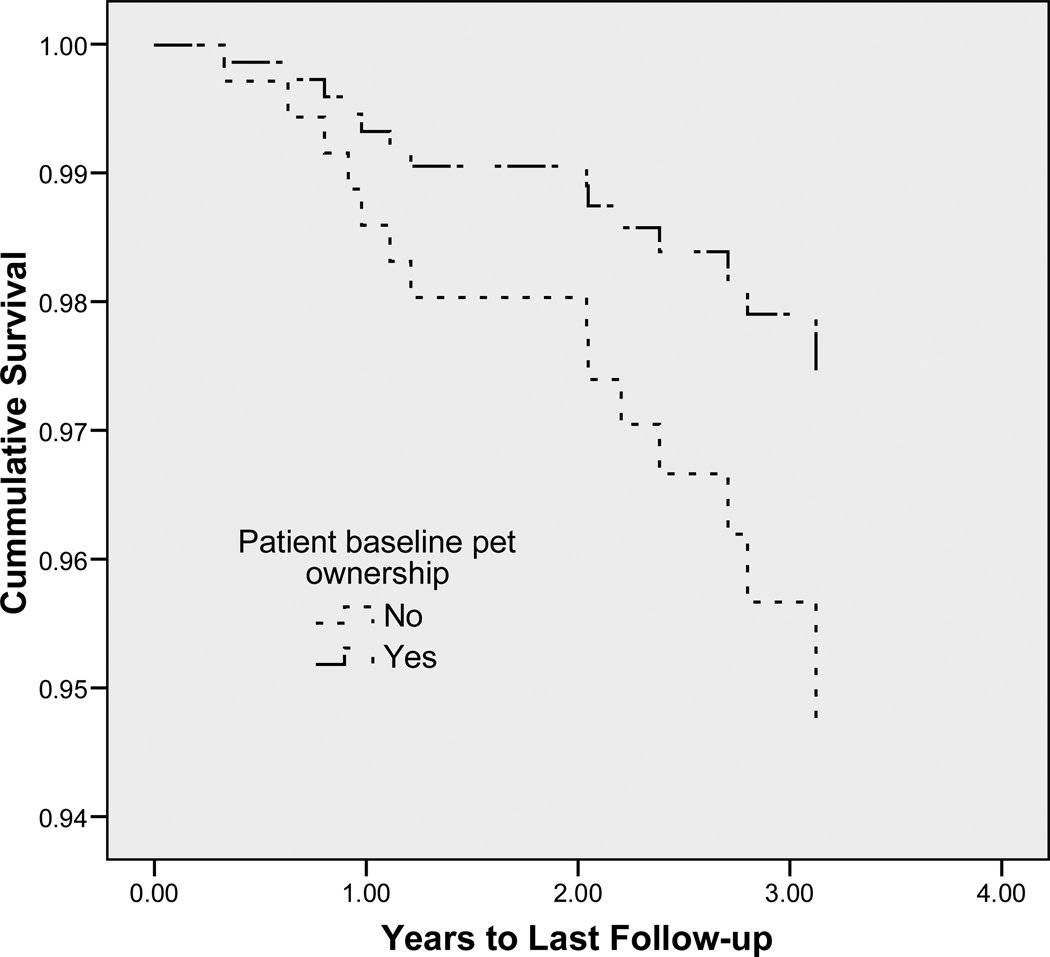
In a combined model that included depression, lack of pet ownership, and the interaction between depression and lack of pet ownership, depression was not a significant independent predictor of mortality after controlling for pet ownership and the interaction of pet ownership with depression (see Table 4). Not owning a pet was the only significant independent predictor of mortality (p = 0.036, see Figure 2).
Table 4.
Results of Cox proportional hazards regression models to predict mortality based on pet ownership status, depression, and the interaction of pet ownership with depression.
| B | SE | Wald | df | Sig. | HR | 90.0% CI for HR |
||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Depression score* | 0.205 | 0.274 | 0.559 | 1 | 0.23 | 1.228 | 0.782 | 1.928 |
| Pet Ownership | −2.626 | 1.559 | 2.838 | 1 | 0.045 | 0.072 | 0.006 | 0.940 |
| Interaction | 0.564 | 0.424 | 1.772 | 1 | 0.092 | 1.757 | 0.876 | 3.528 |
BDI-II depression scores were square root transformed to improve normality. Tests of significance and are one tailed in hypothesized direction; 90% confidence intervals are presented. Pet ownership: 1 = yes, 0 = no
B = unstandardized regression coefficient, SE = standard error of B, Wald = Wald statistic, df = degrees of freedom, Sig = significance level, HR = hazard ration, 90% CI = 90% confidence interval
Figure 2.
Survival curve comparing cumulative survival of pet owners (n = 266) with survival of non-owners (n = 187).
The interaction between pet ownership and depression tended to be significant indicating that the effect of pet ownership in this group with high social support is likely to depend on depression. Further examination of this interaction used estimates of the hazard of mortality for pet owners and non-owners who were 1 sd below and 1sd above mean BDI-II scores. Approximately 14 % of the participants (15% of pet owners, 12% of non-owners) scored more than 1 sd above the mean depression score and 18% (16% of pet owners, 22% of non-owners) scored more than 1 sd below it. Compared with those with lowest mortality (pet owners with low depression), those with moderate mortality were pet owners with high depression (6.4 times as likely to die) and non-owners with low depression (6.7 times as likely to die). The highest risk group (pet non-owners with high depression) was 10.6 times as likely to die as pet owners with low depression.
Age differed according to pet ownership status, pet owners were significantly [t (451) = 6.61, p < 0.001] younger than non-owners [mean difference = 5.79, 95% CI = 4.07, 7.51 years]. Depression was negatively correlated with age (r = − 0.128, p = 0.005); the younger the patient, the higher the depression score. Pet owners tended (χ2 = 2.94, p = 0.086) to be more likely to be depressed (21%) than non-owners (14%). Examining the contributions of age and pet ownership to depression scores with simultaneous linear regression, age was a significant independent predictor of depression (b = −0.085, p = 0.017) while pet ownership was not (b = 0.440, p = 0.556). After accounting for the effect of age on depression, pet ownership did not predict depression score.
The HAT trial forms included questions about current anti-depressant medication. Only 32 of the 460 patients reported taking antidepressant medication, 23 who owned pets and 9 who did not. Of the 32 patients who were taking anti-depressants, 11 were depressed at study intake. Patients taking antidepressant medication tended to be younger [t (395) = 1.89, p =0.06; 57.5 +/− 2.07 years) than those were not (60.9 +/− 0.5 years).
DISCUSSION
Pet ownership made a significant contribution to long term survival after controlling for the effect of depression and the interaction between depression and pet ownership in this group of patients who had experienced MI at least 6 months before entering the study. Not only was pet ownership associated with decreased mortality after adjusting for the effects of depression but also the effect of pet ownership tended to moderate the effect of depression on mortality. Pet ownership may be particularly beneficial to depressed post-MI patients.
Neither anxiety nor low social support was related to mortality in the current study. The finding that social support was not associated with mortality in this study (N = 460, 95% married), contrasts with findings of the relationship of social support amount to one year survival of patients (N = 369, 72% married) with ventricular arrhythmias post-MI (Friedmann & Thomas, 1995) and of long term survival of patients (N = 974, 69% married) with heart failure and atrial fibrillation (Frasure-Smith et al., 2009). All of the participants in the current study had higher amounts of social support based on the inclusion criteria of having a spouse or companion living with the patient who was willing to actively participate in the HAT clinical trial. This requirement excluded post-MI patients with low levels of social support and likely eliminated any possible demonstration of a relationship of low social support and mortality.
The finding that anxiety did not predict survival in the current study is consistent with several previous studies of post-MI patients (Thomas et al., 1997). However the small number of deaths in the current study provides inadequate power (12% for anxiety and 54% for social support from post hoc analysis). Thus we are unable to conclude reliably that anxiety and social support do not have a systematic effect on survival.
The finding that pet ownership contributed to long term survival of post –MI patients was consistent with and extends our previous findings about the relationship of pet ownership to survival in cardiac patients. In one of the first studies evaluating the health benefits of pets, one-year mortality among coronary heart disease patients (N = 92) was significantly lower for pet owners than for non-owners. Pet ownership made a significant addition to the predictive power of disease severity, independent of human social support (Friedmann et al., 1980). Pet ownership was a significant independent predictor of one year survival of post-MI patients (N = 369) with ventricular arrhythmias, after controlling for disease severity (Friedmann & Thomas, 1995). The current study contains patients who may differ in important ways, e.g. usage of proven beneficial treatments, including statins, beta-blockers and angiotensin converting enzyme (ACE) inhibitors, and possible different usage of aspirin compared with the 1980 and 1995 studies showing a relationship of pet ownership to one year survival. This, however, underscores the importance of the present study against a background of proven contemporary therapies.
In the current study, 35% of the participants owned a dog and 33% owned a cat. According to the Humane Society of the US, 39% of US households have at least one dog and 33% have at least one cat (Humane Society of the United States, 2010). Thus the rate of pet ownership in the study participant is similar to the rate in the general US population.
The negative relationship of age with depression in the post-MI patients in the current study is similar to that found in patients with heart failure (HF) (Gottlieb et al., 2004). In the current study, when examining contributions of age and pet ownership to depression scores, age was the only independent predictor of depression.
In HF patients, depression has been associated with both younger age and disease severity, the more severe the HF, the worse the depression (Gottlieb et al., 2004). The paucity of disease severity data obtained in the HAT from which the subjects for the current study were recruited preclude the analysis of the interrelationship of disease severity, depression, pet ownership, and mortality.
Limitations
The small number of deaths in this sample limited the number of variables that could be included in the predictive models as well as the power of the analyses. Recent simulations indicate that 5–9 deaths per predictor yield reliable results in logistic and Cox regression (Vittinghoff & McCulloch, 2007). With 17 deaths, the multivariable analysis is restricted to three predictors. It was not possible to control for the effects of disease severity variables on mortality because disease severity data were not collected in HAT trial. It is possible that the observed relationships between pet ownership and survival and depression and mortality are due to differences in disease severity between pet owners and non-owners and between those with low and high depression scores. It is also important to note that although the relationships of low social support and anxiety to mortality are not statistically significant, there is inadequate power to make a definitive statement that low social support or high anxiety do not contribute to mortality.
As patients were enrolled in a clinical trial, the results may not be generalizable without caveats to the general population. Participants were followed up closely every 6 months and received support as requested on an ongoing basis from clinical trial staff. This support may also promote health among study participants.
Depression was assessed multiple times in the PR-HAT study, only the initial assessment was included in this analysis. One small clinical trial has demonstrated that aggressively treating depression may reduce mortality among cardiac patients with persistent depressive symptoms (Davidson et al., 2010). Decreases in depression over time may reduce the influence of pet ownership on survival. Likewise, acquiring a pet or losing a pet may influence survival.
The effect of attachment to pets also was not assessed in the current study. A much larger number of participants and more deaths would be required to evaluate the relationship of attachment to survival. The previous studies that examined the relationship of pet ownership to survival did not examine pet attachment as a predictor (Friedmann et al., 1980; Friedmann & Thomas, 1995). The one study that included a composite outcome of re-hospitalization or survival also did not include a measure of pet attachment as a predictor (Parker et al., 2010).
Conclusion
This is the first study to demonstrate an effect of pet ownership on survival beyond the immediate one-year post-MI period. It extends the finding that pet ownership contributes to survival in the first year after MI to demonstrate that pet ownership contributes to longer term survival in people who had survived at least six months after experiencing a MI. The positive effect of pet ownership on survival in this period was demonstrated after adjusting for the effect of depression and the interaction between pet ownership and depression. In this period, the effect of pet ownership tends to depend on depression status. Pet ownership tends to enhance survival most in patients who remain depressed at least six months after their MI.
Depression screening for patients with ischemic heart disease to identify patients at greatest risk was recommended recently by the American Heart Association (Lichtman et al., 2008). Pet ownership was associated with younger age and younger patients were more depressed. Pets may be particularly useful for younger post-MI patients. Both drug and behavioral therapies are equally effective at reducing depression in patients with ischemic heart disease as in the general population (Frasure-Smith et al., 2009). One clinical trial suggests the effectiveness of reducing depression for reducing mortality in this population (Lichtman et al., 2008; Davidson et al., 2010). However, it required a significantly enhanced intervention compared with the usual therapy for depression (Davidson et al., 2010). It involved enhanced support in addition to either pharmacologic and/or behavioral therapy. According to Frasure-Smith, depression “should be considered as a risk marker identifying patients who may require additional treatment efforts to manage their cardiac and modify other known risk factors” (Frasure-Smith et al., 2009). The current study indicates that pets may improve survival among patients who are depressed. The results of this study suggest the timeliness of an intervention trial to examine the effects of adopting pets on mortality among depressed patients with ischemic heart disease, even those receiving standard therapy for depression.
HAT Executive Committee
Gust H. Bardy, MD (Chair), Seattle Institute for Cardiac Research, Seattle; Kerry L. Lee, PhD (Co-Chair), Duke Clinical Research Institute, Durham; Daniel B. Mark, MD, MPH, Duke Clinical Research Institute, Durham, NC; Jeanne E. Poole, MD, University of Washington, Seattle, WA; Andrew Tonkin, MD, Monash University, Melbourne, AU; William D. Toff, MD, University of Leicester, Leicester, UK; Warren Smith, MBChB, Auckland City Hospital, Auckland, NZ; Paul Dorian, MD, St. Michael’s Hospital, Toronto, ON, Canada; Will Longstreth, M.D., University of Washington, Seattle, WA; Douglas L. Packer, M.D., Mayo Clinic Foundation, Rochester, MN; Roger D. White, MD, Mayo Clinic College of Medicine, Rochester, MN, Eleanor Schron, PhD, RN and Yves Rosenberg, MD, MPH, National Heart, Lung, and Blood Institute, Bethesda, MD.
Reference List
- Bardy GH, Lee KL, Mark DB, Poole JE, Toff WD, Tonkin AM, Smith W, Dorian P, Packer DL, White RD, Longstreth WT, Jr, Anderson J, Johnson G, Bischoff E, Yallop JJ, McNulty S, Ray LD, Clapp-Channing NE, Rosenberg Y, Schron EB. Home use of automated external defibrillators for sudden cardiac arrest. The New England journal of medicine. 2008;358:1793–1804. doi: 10.1056/NEJMoa0801651. [DOI] [PubMed] [Google Scholar]
- Skinner JE. Blockade of frontocardial-brain stem pathway prevents ventricular fibrillation of ischemic heart. Am J Physiol. 1981;240:156–163. doi: 10.1152/ajpheart.1981.240.2.H156. [DOI] [PubMed] [Google Scholar]
- Skinner JE. Regulation of cardiac vulnerability by the cerebral defense system. J Am Coll Cardiol. 1985;5:88B–94B. doi: 10.1016/s0735-1097(85)80534-9. [DOI] [PubMed] [Google Scholar]
- Lown B, Verrier RL, Carbalan R. Psychological stress and thresholds of repetitive ventricular response. Science. 1973;182:834–836. doi: 10.1126/science.182.4114.834. [DOI] [PubMed] [Google Scholar]
- Audy RJ. Measurement and diagnosis of health in environmental essays on the planet as home. Boston Mass: Houghton Mifflin; 1971. [Google Scholar]
- Piotrowicz K, Noyes K, Lyness JM, McNitt S, Andrews ML, Dick A, Hall WJ, Moss AJ, Zareba W. Physical functioning and mental well-being in association with health outcome in patients enrolled in the Multicenter Automatic Defibrillator Implantation Trial II. Eur.Heart J. 2007;28:601–607. doi: 10.1093/eurheartj/ehl485. [DOI] [PubMed] [Google Scholar]
- Luttik ML, Jaarsma T, Moser D, Sanderman R, van Veldhuisen DJ. The importance and impact of social support on outcomes in patients with heart failure: an overview of the literature. Journal of Cardiovascular Nursing. 2005;20:162–169. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am.Heart J. 2006;152:940–948. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Pelle AJ, Gidron YY, Szabo BM, Denollet J. Psychological predictors of prognosis in chronic heart failure. J.Card Fail. 2008;14:341–350. doi: 10.1016/j.cardfail.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Thomas SA, Chapa DW, Friedmann E, Durden C, Ross A, Lee MC, Lee HJ. Depression in patients with heart failure: prevalence, pathophysiological mechanisms, and treatment. Crit Care Nurse. 2008;28:40–55. [PubMed] [Google Scholar]
- Cossette S, Frasure-Smith N, Lesperance F. Clinical Implications of Reduction in Psychological Distress on Cardiac Prognosis in Patients Participation in a Psychosocial Intervention Program. Psychosomatic Medicine. 2001;63:257–266. doi: 10.1097/00006842-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Archives of General Psychiatry. 2008;65:62–71. doi: 10.1001/archgenpsychiatry.2007.4. [DOI] [PubMed] [Google Scholar]
- Pfiffner D, Hoffmann A. Psychosocial predictors of death for low-risk patients after a first myocardial infarction: a 7-year follow-up study. J.Cardiopulm.Rehabil. 2004;24:87–93. doi: 10.1097/00008483-200403000-00004. [DOI] [PubMed] [Google Scholar]
- van Melle JP, de JP, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, van den Brink RH, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom.Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. J.Intern.Med. 2000;247:629–639. doi: 10.1046/j.1365-2796.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Sparrow D, Volonas PS, Weiss S. Symptoms of anxiety and risk of coronary heart disease: The normative aging study. Circulation. 1994;90:2225–2229. doi: 10.1161/01.cir.90.5.2225. [DOI] [PubMed] [Google Scholar]
- Thomas SA, Friedmann E, Wimbush F, Schron EB. Psychological factors and survival in the cardiac arrhythmia suppression trial (CAST): a reexamination. Am J CritCare. 1997;6:16–26. [PubMed] [Google Scholar]
- Roest AM, Martens EJ, Denollet J, deJonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosom.Med. 2010;72:563–569. doi: 10.1097/PSY.0b013e3181dbff97. [DOI] [PubMed] [Google Scholar]
- Ahern DK, Gorkin L, Anderson JL, Tierney C, Hallstrom A, Ewart C, Capone RJ, Schron E, Kornfeld D, Herd JA. Biobehavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS) Am J Cardiol. 1990;66:59–62. doi: 10.1016/0002-9149(90)90736-k. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Annals of Internal Medicine. 1992;117:1003–1009. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- Case RB, Moss AJ, Case N, McDermott M, Eberly S. Living alone after myocardial infarction. Impact on prognosis. JAMA. 1992;267:515–519. [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101:1919–1924. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- Ruberman W, Weinbalatt E, Goldburg JD, Chaudhary BS. Psychosocial influences on mortality after myocardial infarction. N Engl J Med. 1984;311:552–559. doi: 10.1056/NEJM198408303110902. [DOI] [PubMed] [Google Scholar]
- Friedmann E, Thomas SA. Pet ownership, social support, and one-year survival after acute myocardial infarction in the Cardiac Arrhythmia Suppression Trial (CAST) The American Journal of Cardiology. 1995;76:1213–1217. doi: 10.1016/s0002-9149(99)80343-9. [DOI] [PubMed] [Google Scholar]
- Hart LA. Psychosocial benefits of animal companionship. In: Fine A, editor. Handbook on Animal Assisted Therapy. Newbury Park, CA: Sage Publications; 2000. pp. 59–78. [Google Scholar]
- Friedmann E, Son H. The human -- animal bond: How humans benefit. Vet.Clin.North Am.Small Anim Pract. 2009;39:293–326. doi: 10.1016/j.cvsm.2008.10.015. [DOI] [PubMed] [Google Scholar]
- Friedmann E. The animal-human bond: Health and wellness. In: Fine A, editor. Handbook on Animal Assisted Therapy. Newbury Park, CA: Sage Publications; 2000. pp. 41–58. [Google Scholar]
- Allen K, Shykoff BE, Izzo JL. Pet ownership, but not ACE inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38:815–820. [PubMed] [Google Scholar]
- Friedmann E, Katcher AH, Lynch JJ, Thomas SA. Animal companions and one-year survival of patients after discharge from a coronary care unit. Public health reports (Washington, D.C.: 1974) 1980;95:307–312. [PMC free article] [PubMed] [Google Scholar]
- Parker GB, Gayed A, Owen CA, Hyett MP, Hilton TM, Heruc GA. Survival following an acute coronary syndrome: a pet theory put to the test. Acta Psychiatr.Scand. 2010;121:65–70. doi: 10.1111/j.1600-0447.2009.01410.x. [DOI] [PubMed] [Google Scholar]
- Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J.Am.Coll.Cardiol. 2000;36:959–969. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- Achar SA, Kundu S, Norcross WA. Diagnosis of acute coronary syndrome. Am.Fam.Physician. 2005;72:119–126. [PubMed] [Google Scholar]
- Bardy GH, Lee KL, Mark DB, Poole JE, Toff WD, Tonkin AM, Smith W, Dorian P, Yallop JJ, Packer DL, White RD, Longstreth W, Anderson J, Johnson G, Bischoff E, Munkers CD, Brown A, McNulty S, Ray LD, Clapp-Channing NE, Rosenberg Y, Salive M, Schron EB. Rationale and design of the Home Automatic External Defibrillator Trial (HAT) Am.Heart J. 2008;155:445–454. doi: 10.1016/j.ahj.2007.12.008. [DOI] [PubMed] [Google Scholar]
- Newkirk LA, Kim JM, Thompson JM, Tinklenberg JR, Yesavage JA, Taylor JL. Validation of a 26-point telephone version of the Mini-Mental State Examination. J.Geriatr.Psychiatry Neurol. 2004;17:81–87. doi: 10.1177/0891988704264534. [DOI] [PubMed] [Google Scholar]
- Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Validation of a telephone version of the mini-mental state examination. J.Am.Geriatr.Soc. 1992;40:697–702. doi: 10.1111/j.1532-5415.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory - 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Stear RA, Brown GK. The Beck Depression Inventory Second Edition. Boston MA: Houghton Mifflin; 1996. [Google Scholar]
- Strik JJ, Honig A, Lousberg R, Denollet J. Sensitivity and specificity of observer and self-report questionnaires in major and minor depression following myocardial infarction. Psychosomatics. 2001;42:423–428. doi: 10.1176/appi.psy.42.5.423. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Lushene RE, Gorsuch RL. STAI Manual. Palo Alto, CA: Consulting Psychology Press; 1972. [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support - practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4:497–510. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Teng EL, Chui HC, Schneider LS, Metzger LE. Alzheimer's dementia: Performance on the mini-mental state examination. Journal of Consulting and Clinical Psychology. 1987;55:96–100. doi: 10.1037//0022-006x.55.1.96. [DOI] [PubMed] [Google Scholar]
- Greenland S. Modeling and variable selection in epidemiologic analysis. Am.J.Public Health. 1989;79:340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Habra M, Talajic M, Khairy P, Dorian P, Roy D. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009;120:134–140. doi: 10.1161/CIRCULATIONAHA.109.851675. 3p. [DOI] [PubMed] [Google Scholar]
- Humane Society of the United States. U.S. Pet Ownership Status. 2010 [On-line] http://www.humanesociety.org/issues/pet_overpopulation/facts/pet_ownership_statistics.html.
- Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, Marshall J, Minshall S, Robinson S, Fisher ML, Potenza M, Sigler B, Baldwin C, Thomas SA. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J.Am.Coll.Cardiol. 2004;43:1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am.J.Epidemiol. 2007;165:710–718. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- Davidson KW, Rieckmann N, Clemow L, Schwartz JE, Shimbo D, Medina V, Albanese G, Kronish I, Hegel M, Burg MM. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch.Intern.Med. 2010;170:600–608. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]