Health policy now explicitly addresses the increasing inequalities arising within many countries.1 Although it is generally accepted that socioeconomic factors influence the overall rates of coronary heart disease events,2 studies of case fatality after admission to hospital for acute myocardial infarction show only modest socioeconomic gradients.3 By focusing on those who survive to reach hospital, however, such studies may underestimate the true influence of socioeconomic deprivation. Reports suggest that around 70-80% of deaths within 30 days of a myocardial infarction occur before admission to hospital, and this proportion increases with age.4 We therefore examined the effect of socioeconomic deprivation not only on case fatality in patients admitted with myocardial infarction but also on the risk of death before admission.
Participants, methods, and results
Data were obtained from the Scottish Morbidity Record and General Register Office on all Scottish residents for whom a first myocardial infarction (code 410, international classification of diseases, 9th revision) was the principal cause of death or admission to hospital between 1986 and 1995. This database is linked to the Registrar General's data on death certificates, with an accuracy of 98%. In a 1% sample of records checked in 1994, acute myocardial infarction as a principal diagnosis was 97% accurate. First myocardial infarction was defined as no previous admission for this event since 1981. Postcodes were used to assign a Carstairs deprivation category to each individual, from 1 (least deprived) to 5 (most deprived).3 These categories are derived from 1991 census data on four variables: overcrowding, the proportion of residents unemployed, those who do not have a car, and those who belong to a low occupational social class. Population rates were calculated by using the population structure by age, sex, and deprivation category.
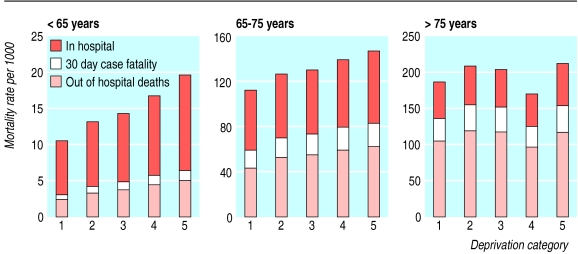
Between 1986 and 1995 in Scotland, 44 465 men (mean age (SD 11) 71.1) and 38 710 women (mean age (SD 10) 77.7) died before being admitted to hospital after a first myocardial infarction. A further 68 626 men and 49 123 women were admitted to hospital, of whom 22.3% (95% confidence interval 22.1% to 22.6%) died within 30 days. There was a socioeconomic gradient in all three parameters, which was greater in younger age groups (figure). The population based mortality in deprivation category 5 was more than twice that of category 1 in people aged under 65 (see table on website). Overall there were about 2000 excess deaths in the least affluent category compared with the most affluent (comparing the differential in observed over expected deaths in each deprivation category).
Comment
Socioeconomic deprivation has a profound effect on the risk of having a first myocardial infarction, the chance of reaching hospital alive, and the probability of surviving the first month. The effect of socioeconomic deprivation is greatest in women, with a twofold increase in death before reaching hospital in those under 65. The most deprived members of society under 65 have twice the risk of a first myocardial infarction and death before reaching hospital. Younger deprived men and women admitted to hospital are 20% more likely to die within the first month. One limitation of the study is that deprivation category is based on postcode rather than personal characteristics.
How socioeconomic deprivation increases these risks is probably multifaceted. The inverse care law is important but is only the last stage in a long sequence of events extending from the intrauterine period.5 To attain real equality requires strategies that target the wider determinants of health throughout an individual's life. As around 40% of people who experience a first myocardial infarction do not survive to reach hospital, the potential of acute treatment to reduce mortality is limited. Reducing mortality from heart disease requires a focus on primary prevention that explicitly addresses socioeconomic inequalities.
Supplementary Material
Figure.
Rates per 1000 population of hospital admission for myocardial infarction, deaths before admission, and deaths within 30 days, by deprivation category 1986-95 (1=least deprived, 5=most deprived)
Footnotes
Funding: British Heart Foundation.
Competing interests: None declared.
A table showing mortality per 1000 men and women appears on the BMJ's website
References
- 1.National Heart Forum. Social inequalities in coronary heart disease: opportunities for action. London: Stationery Office; 1999. [Google Scholar]
- 2.Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H. Effect of socioeconomic group on the incidence of management of and survival after myocardial infarction and coronary death; analysis of community coronary event register. BMJ. 1997;314:541–546. doi: 10.1136/bmj.314.7080.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Capewell S, Kendrick S, Boyd J, Juszczak E, Clarke J. Measuring outcomes: one month survival after acute myocardial infarction in Scotland. Heart. 1996;76:70–75. doi: 10.1136/hrt.76.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tunstall-Pedoe H, Morrison C, Woodward M. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991. Circulation. 1996;93:1981–1992. doi: 10.1161/01.cir.93.11.1981. [DOI] [PubMed] [Google Scholar]
- 5.Barker DJP. Fetal origins of coronary heart disease. BMJ. 1995;311:171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.