Abstract
Bovine Bacillus anthracis isolates from Cameroon were genetically characterized. They showed a strong homogeneity, and they belong, together with strains from Chad, to cluster Aβ, which appears to be predominant in western Africa. However, one strain that belongs to a newly defined clade (D) and cluster (D1) is penicillin resistant and shows certain phenotypes typical of Bacillus cereus.
TEXT
Extensive genetic analysis of a large number of strains of Bacillus anthracis, the causative agent of anthrax, led to robust molecular epidemiological data, making this bacterium a model for microbial evolution and the global spread of pathogens and even making it possible for researchers to follow migration or movement of its hosts or host products (5–8, 15). This is possible by virtue of the large data set based on canonical single nucleotide polymorphisms (canSNPs), which classify B. anthracis strains into clades (22), and on multiple-locus variable-number tandem-repeat (VNTR) analysis (MLVA), which groups them further into clusters (6). Although certain geographical regions are extensively sampled, others are poorly studied, which may lead to bias in the analysis of the spread and diversity of strain populations. This, in particular, is the case for western and central African countries, such as Cameroon, where most of Africa's anthrax outbreaks occur (22). A broader genetic diversity of B. anthracis strains is expected in that region due to the higher incidence of anthrax there than elsewhere. In order to improve our knowledge regarding the genetic diversity of B. anthracis, we analyzed bovine strains from seven sites in Cameroon and compared the results with data from a worldwide strain collection. In addition, we characterized in detail a penicillin-resistant strain that caused bovine anthrax in that area. This strain represents a new clade and a new cluster of B. anthracis and shows some genetic traits of Bacillus cereus.
Strains of B. anthracis isolated from bovines in various areas of Cameroon (Table 1) were identified using standard methods as described previously (17, 23). They all harbored the virulence factor markers pag and cap, which are specific to B. anthracis plasmids pXO1 and pXO2 (19). They were all nonhemolytic and γ phage sensitive (Table 1). One strain, JF3964, showed particular phenotypes that are normally found in B. cereus, such as resistance to the B. anthracis-specific γ phage and resistance to penicillin. However, in contrast to B. cereus, strain JF3964 was nonhemolytic. These phenotypic criteria are used to discriminate B. anthracis from B. cereus. Additionally, the chromosomal markers sap and Ba813 that were used as specific markers for B. anthracis (17, 19) were absent in JF3964. However, JF3964 contained the virulence genes which are associated with the two B. anthracis plasmids pXO1 and pXO2 (19).
Table 1.
Antibiotic susceptibilities and phage γ sensitivities of B. anthracis strains from Cameroon
| Strain | Origin, section of Cameroona | γ Phage | MIC(s) (μg/ml) ofb: |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GEN | AMI | STR | ERY | CLI | Q-D | TET | CHL | ENR | CEP | VAN | LNZ | PEN | AMC | NIT | SXT | |||
| JF3959 | Makari, NE (GI/D3405) | Sensitive | ≤2 | ≤16 | ≤4 | 1 | ≤0.5 | 1 | ≤1 | ≤4 | ≤0.25 | ≤2 | 2 | 1 | ≤0.12 | ≤2, 1 | ≤16 | 1, 19 |
| JF3960 | Garoua, N (D4863) | Sensitive | ≤2 | ≤16 | ≤4 | 0.5 | ≤0.5 | 1 | ≤1 | ≤4 | ≤0.25 | ≤2 | ≤1 | 1 | ≤0.12 | ≤2, 1 | ≤16 | ≤0.5, 9.5 |
| JF3961 | Maloum, N (FED:77) | Sensitive | ≤2 | ≤16 | ≤4 | 0.5 | ≤0.5 | 2 | ≤1 | ≤4 | ≤0.25 | ≤2 | 2 | 1 | ≤0.12 | ≤2, 1 | ≤16 | 2, 38 |
| JF3963 | Padarmé, N (No141) | Sensitive | ≤2 | ≤16 | ≤4 | 0.5 | ≤0.5 | 2 | ≤1 | ≤4 | ≤0.25 | ≤2 | 2 | 1 | ≤0.12 | ≤2, 1 | ≤16 | 2, 38 |
| JF3964 | Koza, NE (No142) | Resistant | ≤2 | ≤16 | ≤4 | 0.5 | 1 | 2 | ≤1 | ≤4 | ≤0.25 | 8 | 2 | 2 | 8 | ≤2, 1 | ≤16 | 1, 19 |
| JF3965 | Boklé, N (D5594) | Sensitive | ≤2 | ≤16 | ≤4 | 1 | ≤0.5 | 1 | ≤1 | ≤4 | ≤0.25 | ≤2 | 2 | 1 | ≤0.12 | ≤2, 1 | ≤16 | 1, 19 |
| JF3966 | Makari, NE (Makari) | Sensitive | ≤2 | ≤16 | ≤4 | 1 | ≤0.5 | 1 | ≤1 | ≤4 | ≤0.25 | ≤2 | 2 | 1 | ≤0.12 | ≤2, 1 | ≤16 | 2, 38 |
Geographical origin (original strain number). N, north; E, east; NE, northeast.
AMI, amikacin; AMC, amoxicillin-clavulanic acid (ratio, 2:1); CEP, cephalothin; CHL, chloramphenicol; CLI, clindamycin; ENR, enrofloxacin; ERY, erythromycin; GEN, gentamicin; LZD, linezolid; NIT, nitrofurantoin; PEN, penicillin; STR, streptomycin; SXT, trimethoprim-sulfamethoxazole (ratio, 1:19); Q-D, quinupristin-dalfopristin; TET, tetracycline; VAN, vancomycin.
Genetic strain characterization was performed by canSNP analysis, which best roots the phylogenetic relationship of B. anthracis strains (22), and MLVA, which allows a finer subtyping of the strains (6). The methods are complementary in studying the genetics of bacterial populations since canSNPs are slowly evolving markers, whereas VNTRs are quickly evolving markers (14). Thirteen canSNPs (A.Br.001, A.Br.002, A.Br.003, A.Br.004, A.Br.006, A.Br.007, A.Br.008, A.Br.009, B.Br.001, B.Br.002, B.Br.003, B.Br.004, and A/B. Br.001) and eight VNTR markers (VrrA, VrrB1, VrrB2, VrrC1, VrrC2, GC3, pXO1, and pXO2) for B. anthracis were amplified by PCR, using filtered lysates as template DNA (12), and sequenced. DNA sequencing was carried out with an ABI Prism 3100 genetic analyzer (Applied Biosystems, Rotkreuz, Switzerland) and a BigDye Terminator cycle sequencing kit (Applied Biosystems) according to the manufacturer's instructions. The canSNP and VNTR sequences were compared to published data (22).
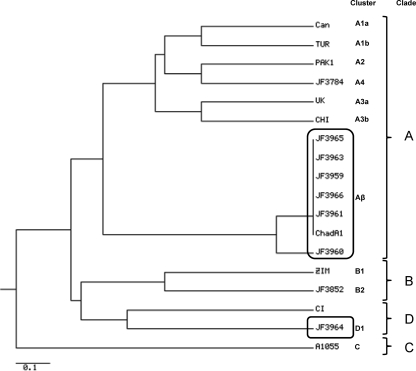
Six characteristic strains of B. anthracis from Cameroon (JF3959, JF3060, JF3961, JF3963, JF3965, and JF3966) had the following canSNP characteristics: A.Br.001, T; A.Br.002, G; A.Br.003, A; A.Br.004, T; A.Br.006, A; A.Br.007, T; A.Br.008, T; A.Br.009, A; B.Br.001, T; B.Br.002, G; B.Br.003, G; B.Br.004, T; and A/B.Br.001, A. These characteristics classified them as clade A (Fig. 1) (subclade A.Br.005/006), as defined by Van Ert and colleagues (22). These six strains showed an additional base difference in the canSNP B.Br.004: the nucleotide just downstream of the canSNP is a thymine instead of a cytosine. We confirmed that this mutation is also present in all strains from Chad that were analyzed previously (12). One strain, JF3964, showed a completely different profile that has not yet been described (the characteristics of its canSNPs are A.Br.001, T; A.Br.002, A; A.Br.003, A; A.Br.004, T; A.Br.006, C; A.Br.007, T; A.Br.008, T; A.Br.009, A; B.Br.001, T; B.Br.002, C; B.Br.003, G; B.Br.004, T; and A/B.Br.001, A) and was assigned to a novel clade, designated clade D (Fig. 1), according to the criteria of Van Ert et al. (22).
Fig. 1.
Dendrogram based on eight VNTR markers of B. anthracis strains from Cameroon (this work) and characteristic strains representing all clades and major clusters as reported previously (6, 12, 15). Strains from western and central Africa are boxed. The dendrogram was generated by clustering using the unweighted pair group method with arithmetic means. The scale bar indicates genetic distance. The genetic distance is presented as the absolute number of differences in marker alleles among genotypes.
The sizes of the VNTR amplicons, as determined by sequence analysis, were compared to selected published allele sizes (6), as well as to the B. anthracis genome sequences from GenBank (http://www.ncbi.nlm.nih.gov). A phylogenetic tree was derived from allelic profile data by the unweighted-pair group method with arithmetic means (UPGMA) with an online software (http://pubmlst.org/) using the PHYLIP suite of programs and the VNTR markers (4) (Fig. 1). The MLVA profiles matched the clades as defined by the canSNP profiles. Strains JF3959, JF3060, JF3961, JF3963, JF3965, and JF3966 grouped in cluster Aβ (Fig. 1), together with B. anthracis strains from Chad, as previously determined (12). The close relationship of B. anthracis strains from Cameroon with those from Chad, with both belonging to cluster Aβ, may be explained by the fact that these countries share a border in the northern part of Cameroon, where anthrax is hyperendemic and where most of the samples were collected. The fact that we observe no particular variations in strains isolated from western and central Africa (Cameroon and Chad) in spite of the high prevalence of the disease underlines the high genetic stability of the species B. anthracis. Moreover, strains of cluster Aβ also show a particular phenotype. They all lack anthrose, an unusual sugar that is specific to the exosporium of B. anthracis (20, 21). It has to be noted that two B. anthracis strains from Cameroon previously analyzed by Lista and colleagues have an MLVA profile identical to that of our strains but were grouped into a new cluster, E (11). However, our analysis showed that this cluster is identical to Aβ, which appears to be a more appropriate designation since Aβ belongs to clade A (6, 22).
Strain JF3964, which belongs to the novel clade D of B. anthracis, was also placed into a new cluster, designated D1, as determined by MLVA (Fig. 1). The most closely related strain that belongs to the same clade but to a different cluster is B. cereus biovar anthracis strain CI, which was isolated from a chimpanzee from the Ivory Coast (9, 10) (Fig. 1). Strain CI also shows phenotypic characteristics that are similar to those of strain JF3964, such as being penicillin resistant and γ phage insensitive. It also lacks the specific chromosomal marker sap but harbors cap and pag virulence genes, placing both strains JF3964 and CI between B. anthracis and B. cereus. Although such particular penicillin-resistant strains of B. anthracis were thought to be specific to primates (9, 10), we show that they are also present in cattle with typical symptoms of anthrax. These results reveal these strains to possess a pathogenicity which is very similar to that of classical B. anthracis strains.
The presence of both plasmids pXO1 and pXO2 in B. anthracis strain JF3964 was confirmed by plasmid extractions from strain JF3964 and the type strain Vollum (as the standard) using the NucleoBond PC 20 plasmid DNA purification kit (Macherey-Nagel, Oensingen, Switzerland) according to the manufacturer's protocol, followed by Southern blotting as previously described (16). Specific probes were constructed by PCR in the presence of digoxigenin-11-dUTP (Roche Diagnostics, Rotkreuz, Switzerland) using the oligonucleotide primer sets pag67/pag68 and cap57/cap58 and standard PCR conditions (16, 17). Both probes targeting plasmids pXO1 and pXO2 hybridized to two different large plasmids in JF3964, with sizes corresponding to those of the strain VollumT (data not shown). Moreover, a real-time PCR assay based on the real-time PCR assay of Coker and colleagues (2) was performed to determine the number of plasmid copies per chromosome. One modification of the protocol was carried out because of the absence of the marker Ba813 in the strain JF3964. The dnaK gene was chosen as a chromosomal marker since it is present in a single copy in the genomes of bacteria and it is, like Ba813, not located close to the origin of replication of the chromosome in B. anthracis. The primers used for the real-time PCR were dnaK_F, 5′-GCTTGCTCTTTGCTTGTTCCTAA-3′, and dnaK_R, 5′-TCGATATTGATGCGAACGGTAT-3′, and the probe was dnaK_P, 5′-FAM-TTCGCACGTACGTTAAC-TAMRA-3′, where FAM and TAMRA are 6-carboxyfluorescein and 6-carboxytetramethylrhodamine, respectively. The copy number per chromosome equivalent to the number of copies of plasmid pXO1 in strain JF3964 was calculated from the ratio of the real-time PCR signal strength for pXO1 (JF3964), normalized to the signal of dnaK (JF3964), to the real-time PCR signal strength for pXO1 (VollumT), multiplied by the copy number per chromosome equivalent to that of strain VollumT, which is 11.5 (2). Since the real-time PCR signal is reciprocal to the threshold cycle (CT) value, the corresponding formula is
For the determination of the pXO2 plasmid copy number per chromosome in the strain JF3964, the same formula was applied using the pXO2 copy number per chromosome in the strain VollumT, which is 1.6 (2).
Four dilutions were tested in triplicate by real-time PCR, and the calculated average copy number ratio for pXO1 in JF3964 was 10.89, with a standard deviation of ±0.19, while for pXO2, it was 1.59, with a standard deviation of ±0.03.
All strains were susceptible to antibiotics commonly used to treat infections caused by Gram-positive bacteria, as determined by the broth dilution method (Table 1) (1, 12), with the exception of strain JF3964. For this strain, the MIC of penicillin was 80 times higher and the MICs of oxacillin and cephalotin were higher than those for other strains of this region and higher than characteristic MIC values for B. anthracis (Table 1) (12). However, the strain was sensitive to amoxicillin-clavulanic acid (Table 1), indicating that the penicillin resistance was due to a β-lactamase activity.
The penicillin resistance mechanism of strain JF3964 is likely to be associated with the presence of the β-lactamase genes bla1 and bla2 and of a particular sigP-rsiP operon which is closely related to that of B. cereus but different from that in commonly found B. anthracis. Operon sigP-rsiP encodes sigma factor P (SigP) and the repressor of sigma factor P (RsiP), the latter of which affects the expression of the β-lactamase genes bla1 and bla2 (18). This was recently demonstrated with B. anthracis strain 32, which contains a truncated repressor gene, rsiP, resulting from one mutation in the sigP-rsiP operon. In this strain, the repressor cannot bind to the sigma factor, which enables the latter to interact with RNA polymerase and transcript bla genes, leading to a 6,000-times-higher MIC for penicillin (18). The entire sigP-rsiP operon was amplified from the penicillin-resistant strain JF3964 by PCR using FIREPol DNA polymerase I (Solis Biodyne) and primers BaSigPXL (5′-GCTTTTTCTATTTTATTATGGCTC-3′) and sigmaR (5′-TGCTGCTCTCGTTACATCAGA-3′). The PCR product obtained was subsequently sequenced using primers BaSigPXL, sigmaL2 (5′-TACGAAAGATCCACACTTATCA-3′), sigmaL4 (5′-CCCAATGGAACACCGTAAAG-3′), sigmaL5 (5′-TTGAAACCATAATAAAAGTGAGGGTA-3′), sigmaR, and sigmaR2 (5′-TGTGCTTGCTTTTGTTGGTT-3′). DNA sequencing was performed as described above. Comparison of the nucleotide (nt) sequence with sequences in the EMBL/GenBank database using Blastn software revealed the sigP-rsiP operon of strain JF3964 to be identical to that of B. cereus biovar anthracis strain CI (10). Furthermore, the amino acids of SigP are 97.7% identical and 98.3% similar to those of SigP of common B. anthracis strains, such as Ames, Sterne, and VollumT. Analogously, the amino acids of RsiP of strains JF3964 and CI are 97% similar and 99% identical to those of RsiP of common B. anthracis strains.
The sigP-rsiP operon contains −10 and −35 consensus sequences for a putative transcription promoter, followed by a strong ribosome binding site (RBS) upstream from the alternative start codon for SigP, TTG. The open reading frame for gene rsiP overlaps the last 11 nucleotides of sigP and is preceded by a characteristic RBS 5 nt upstream of the common start codon for RsiP, ATG. It is worth noting that the start codon for SigP in B. anthracis strains, except in JF3964 and CI, is generally ATG, whereas in B. cereus and B. thuringiensis, it is TTG. We interpret the moderate resistance to penicillin (MIC, 8 μg/ml) in strain JF3964 to be due to a partial repression of SigP by the corresponding RsiP, in contrast to what occurs in common B. anthracis strains, which are assumed to exhibit full repression of their SigP by RsiP, and in contrast to B. anthracis strain 32, where a truncated RsiP is unable to repress SigP, leading to very high penicillin resistance (18). Although strain JF3964 has additional characteristics specific to B. cereus, it harbors the virulence genes which are associated with the virulence plasmids pXO1 and pXO2 in B. anthracis. The unusual and penicillin-resistant strains of B. anthracis, such as JF3964 and CI, may have evolved from a closely related species of the B. cereus group, which, in turn, comprises six closely related members, namely, B. anthracis, B. cereus, B. mycoides, B. pseudomycoides, B. thuringiensis, and B. weihenstephanensis (3), since it has been shown that plasmids can be transmitted or transferred spontaneously from one species to another (10, 13).
In conclusion, our analysis of B. anthracis strains isolated from cattle in Cameroon revealed that strains isolated from cattle with anthrax in western and central Africa are generally tightly clustered genetically and belong to phylogenetic group Aβ, which has not yet been identified outside this area. Furthermore, a particular subtype of B. anthracis belonging to a novel clade (D) with close similarity to B. cereus is also present in this region, causing symptoms of anthrax in cattle as well as in primates in western and central Africa. This rarely described type of B. anthracis currently contains only two described strains, and both of them belong to clade D but to different clusters (Fig. 1). They deserve particular attention both from the point of view of the microbial evolution of the B. cereus group and from a medical and diagnostic point of view.
Nucleotide sequence accession numbers.
The nucleotide sequence of the sigP-rsiP operon is deposited under GenBank/EMBL accession number FR750362. The nucleotide sequences of the VNTRs are deposited under GenBank/EMBL accession numbers FR872834 to FR872889.
Acknowledgments
This work was financed by a research grant of the Institute of Veterinary Bacteriology. P.P. was supported by a grant from the Swiss Federal Health Ministry (BAG) to the National Center of Anthrax (NANT) at the Institute of Veterinary Bacteriology. We are grateful to Yaya Aboubakar for his support for this study.
Footnotes
Published ahead of print on 24 June 2011.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1. Clinical Laboratory Standards Institute 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 7th ed, vol. 26, no. 2. Approved standard M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 2. Coker P. R., et al. 2003. Bacillus anthracis virulence in guinea pigs vaccinated with anthrax vaccine adsorbed is linked to plasmid quantities and clonality. J. Clin. Microbiol. 41:1212–1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Daffonchio D., Cherif A., Borin S. 2000. Homoduplex and heteroduplex polymorphisms of the amplified ribosomal 16S–23S internal transcribed spacers describe genetic relationships in the “Bacillus cereus group.” Appl. Environ. Microbiol. 66:5460–5468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Felsenstein J. 2005. PHYLIP (Phylogeny Inference Package) version 3.6. Department of Genome Sciences, University of Washington, Seattle, WA [Google Scholar]
- 5. Keim P., et al. 2009. The genome and variation of Bacillus anthracis. Mol. Aspects Med. 30:397–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Keim P., et al. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928–2936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keim P., Smith K. L. 2002. Bacillus anthracis evolution and epidemiology. Curr. Top. Microbiol. Immunol. 271:21–32 [DOI] [PubMed] [Google Scholar]
- 8. Kenefic L. J., et al. 2009. Pre-Columbian origins for North American anthrax. PLoS One 4:e4813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Klee S. R., et al. 2010. The genome of a Bacillus isolate causing anthrax in chimpanzees combines chromosomal properties of B. cereus with B. anthracis virulence plasmids. PLoS One 5:e10986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Klee S. R., et al. 2006. Characterization of Bacillus anthracis-like bacteria isolated from wild great apes from Côte d'Ivoire and Cameroon. J. Bacteriol. 188:5333–5344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lista F., et al. 2006. Genotyping of Bacillus anthracis strains based on automated capillary 25-loci multiple locus variable-number tandem repeats analysis. BMC Microbiol. 6:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maho A., et al. 2006. Antibiotic susceptibility and molecular diversity of Bacillus anthracis strains in Chad: detection of a new phylogenetic subgroup. J. Clin. Microbiol. 44:3422–3425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Perreten V., Frey J. 2009. Use of a microchip to detect antibiotic resistance genes in Bacillus anthracis, p. 147–152In Kostic T., Butaye P., Schrenzel J. (ed.) Detection of highly dangerous pathogens: microarray methods for BSL3 and BSL4 agents. Wiley-VCH Verlag GmbH & Co., Weinheim, Germany [Google Scholar]
- 14. Pilo P., Frey J. 27 May 2011. Bacillus anthracis: molecular taxonomy, population genetics, phylogeny and patho-evolution. Infect. Genet. Evol. [Epub ahead of print.] doi:10.1016/j.meegid.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 15. Pilo P., Perreten V., Frey J. 2008. Molecular epidemiology of Bacillus anthracis: determining the correct origin. Appl. Environ. Microbiol. 74:2928–2931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pilo P., et al. 2005. A metabolic enzyme as a primary virulence factor of Mycoplasma mycoides subsp. mycoides Small Colony. J. Bacteriol. 187:6824–6831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ramisse V., Patra G., Garrigue H., Guesdon J. L., Mock M. 1996. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pXO1 and pXO2 and chromosomal DNA. FEMS Microbiol. Lett. 145:9–16 [DOI] [PubMed] [Google Scholar]
- 18. Ross C. L., Thomason K. S., Koehler T. M. 2009. An extracytoplasmic function sigma factor controls β-lactamase gene expression in Bacillus anthracis and other Bacillus cereus group species. J. Bacteriol. 191:6683–6693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ryu C., Lee K., Yoo C., Seong W. K., Oh H. B. 2003. Sensitive and rapid quantitative detection of anthrax spores isolated from soil samples by real-time PCR. Microbiol. Immunol. 47:693–699 [DOI] [PubMed] [Google Scholar]
- 20. Tamborrini M., et al. 13 May 2011. Identification of an African Bacillus anthracis lineage that lacks expression of the spore surface associated anthrose containing oligosaccharide. J. Bacteriol. doi:10.1128/JB.00078-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tamborrini M., Werz D. B., Frey J., Pluschke G., Seeberger P. H. 2006. Anti-carbohydrate antibodies for the detection of anthrax spores. Angew. Chem. Int. Ed. Engl. 45:1–3 [DOI] [PubMed] [Google Scholar]
- 22. Van Ert M. N., et al. 2007. Global genetic population structure of Bacillus anthracis. PLoS One 2:e461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. WHO 1998. Guidelines for the surveillance and control of anthrax in humans and animals, 3rd ed. World Health Organization, Geneva, Switzerland [Google Scholar]