Abstract
Introduction:
Children of parents who experienced trauma often present emotional and behavioral problems, a phenomenon named inter-generational transmission of trauma (IGTT). Combined with antenatal factors, parenting and the home environment contribute to the development and maintenance of sleep problems in children. In turn, infant sleep difficulty predicts behavioral and emotional problems later in life. The aim of this study was to investigate whether infant sleep problems predict early behavioral problems indicative of IGTT.
Methods:
184 first-time mothers (ages 18–47) participated. N = 83 had a history of childhood abuse and posttraumatic stress disorder (PTSD+); 38 women reported childhood abuse but did not meet diagnostic criteria for PTSD (PTSD−); and the control group (N = 63) had neither a history of abuse nor psychopathology (CON). Depression, anxiety, and sleep difficulty were assessed in the mothers at 4 months postpartum. Infant sleep was assessed using the Child Behavior Sleep Questionnaire (CSHQ). Outcome measures included the Parent Bonding Questionnaire (PBQ) at 4 months and the Child Behavior Check List (CBCL) at 18 months.
Results:
Infants of PTSD+ mothers scored higher on the CSHQ and had more separation anxiety around bedtime than PTSD− and CON, and the severity of their symptoms was correlated with the degree of sleep disturbance. Maternal postpartum depression symptoms mediated impaired mother-infant bonding, while infant sleep disturbance contributed independently to impaired bonding. Mother-infant bonding at 4 months predicted more behavioral problems at 18 months.
Conclusions:
Infant sleep difficulties and maternal mood play independent roles in infant-mother bonding disturbance, which in turn predicts behavioral problems at 18 months.
Citation:
Hairston IS; Waxler E; Seng JS; Fezzey AG; Rosenblum KL; Muzik M. The role of infant sleep in intergenerational transmission of trauma. SLEEP 2011;34(10):1373-1383.
Keywords: Child abuse, PTSD, development, depression
INTRODUCTION
The reported prevalence of sleep problems in infancy and childhood ranges between 10% and 40%.1,2 Prior work suggests that, as in adults, sleep difficulties in children are secondary to another sleep disorder such as sleep apnea or bruxism, to neurological disorders such as epilepsy, or to psychiatric problems, such as anxiety or mood disorders.2 Thus, sleep difficulty in infants may be an early risk marker for difficulties with emotion regulation potentially leading to psychopathology later in life.
Parenting and the home environment may be contributing factors to the development and/or maintenance of sleep problems in children.3 For example, a community survey on sleep difficulties in infants aged 1–2 years found that infants with more sleep problems were more likely to have mothers with psychiatric problems and family tension.4 Similarly, Armitage et al.5 reported that infants of mothers with current or a history of major depression had more sleep problems, as early as 2 weeks of age, than infants of healthy mothers.
Sleep difficulty in early childhood predicts behavioral and emotional problems later in life. Gregory et al.6 found that sleep difficulties at 3–4 years of age, as reported by parents, predicted behavioral (conduct disorder, hyperactivity) and emotional (anxiety) problems at age 7; and according to their model the effect was largely explained by environmental rather than genetic factors. Similarly, parent-reported sleep difficulties, between the ages of 5–9 predicted reduced neurocognitive and emotional function,7 temper tantrums,8 internalizing and externalizing problems,9 attention deficit disorder,10 and depression.11
Children of parents who experienced childhood trauma are at an increased risk for developing posttraumatic stress disorder (PTSD) and other psychiatric disorders, a phenomenon known as the inter-generational transmission of trauma (IGTT).12–14 A central element in understanding the development and effects of parents' PTSD on young children may lie in the infant-caregiver relationship. Bowlby's theory of attachment15 suggests that the initial relationship that exists between infant and caregiver is the foundation for the infant's mental health. While the mechanisms of IGTT are not well understood, the literature indicates that subtle differences in parent-child relationship, such as intrusiveness, rather than general parenting skills16 differentiate vulnerable mothers from mothers without a history of trauma. As poor sleep in children has been linked to parenting and home environment, as well as predicting mental health in later life, it is feasible that the development of poor sleep regulation in infants links parents psychopathology with IGTT.
In this study we investigated the role of infant sleep behaviors in IGTT, examining the hypothesis that infant sleep problems play a role in mother-infant relationship and other behavioral measures linked to the subsequent development of psychopathology. Specifically, we aimed to assess whether infants of mothers with a history of child abuse (with or without PTSD), are more likely to show sleep disturbances at 4 months, and whether sleep disruption at this age modulates the effects of mothers' psychiatric symptoms on factors implicated in IGTT, such as bonding with the infant and child behavioral problems. Thus, the rationale of our analyses was first to characterize sleep behaviors in the different maternal cohorts and to assess the role of a history of child abuse and PTSD on infant sleep; second, to identify group differences in mother-infant relationship and behavioral problems in the toddlers, as predictors of psychopathology later in life; and finally, quantify the contribution of sleep related behaviors to predictive factors. As recent studies have reported differences in arousability between male and female infants,17,18 we investigated the role of gender on infant sleep as well.
MATERIALS AND METHODS
Participants
Women were recruited for the Maternal Anxiety during Childbearing Years (MACY) study either as postpartum follow-up to a study on the prenatal effects of PTSD on childbearing when they initiated prenatal care for their first child at 14–28 weeks gestation (reported in Seng et al.19) or through community advertisement at 6-8 weeks postpartum. Recruitment sites included The University of Michigan Hospital in Ann Arbor, MI, Henry Ford Hospital in Detroit, MI, and Hutzel Women's Hospital in Detroit, MI. Recruitment in the community was conducted by posting flyers in childcare centers and pediatric offices in the Greater Ann Arbor Area. Participants were non-psychiatrically referred English-speaking women, ages 18 and older.
Observation groups included mothers with a history of child abuse before the age of 16, and who met criteria for lifetime PTSD based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR)20 at any point during the study (PTSD+, N = 83); women with a history of child abuse who did not meet criteria for lifetime PTSD (PTSD−, N = 38); and women with no history of child abuse and no PTSD (CON, N = 64).
Exclusion criteria included the use of illegal or non-prescription drugs during pregnancy, premature birth (< 36 weeks gestation), and persistent health issues reported at 4 months.
Procedures
The study was approved by the Institutional Review Board of the University of Michigan in Ann Arbor. Women who agreed to participate in the study underwent an initial screen interview to determine their eligibility and group assignment. The interview was conducted by phone, and included a demographics questionnaire; assessment of the timing, severity, and type of childhood trauma; and psychiatric assessment and diagnosis of lifetime and current PTSD. At 4 months postpartum, participants were contacted by phone for a repeat psychopathology assessment and administration of instruments regarding their infant. The interview included assessment of PTSD, postpartum depression symptoms (which included a sleep difficulty scale), assessment of the infants' sleep, and mothers' self-rating of their bonding and relationship with their infant. Finally, at an 18-month playroom-visit, at the University Research Center, toddler behavior and emotion regulation was assessed.
Measures
Demographics
Demographic information on socioeconomic status, smoking, and alcohol consumption during pregnancy, was obtained using standard items from the Center of Disease Control (CDC) Pregnancy Risk Assessment Monitoring System (PRAMS) survey,21 designed to be administered either by self-report or by phone interview. The questionnaire was administered by phone at initial contact and again at 4 months.
Trauma history
Trauma history was obtained using the short-form of the Childhood Trauma Questionnaire (CTQ-SF),22 a retrospective measure for the frequency and severity of different types of abuse and neglect. The CTQ-SF is a 28-item self-report instrument that assesses 5 types of maltreatment—emotional, physical, sexual abuse, and emotional and physical neglect, and false-negative trauma reports (minimalization/denial). Response ratings range from 0 = “never” to 5 = “very often true.” Recent studies reported high internal (α Cronbach = 0.96) and test-retest reliability (0.85),23 as well as high construct validity across diverse population samples.24 For child abuse groups (PTSD+, PTSD−), inclusion criteria required that women report childhood trauma before the age of 16, scoring above “minimal” on any of the 5 maltreatment subscales of the CTQ.22
Maternal psychopathology
Lifetime and current PTSD diagnoses were obtained during the initial interview and at 4 mo post-partum (pp) using the psychometrically established National Women's Study (NWS) PTSD Module. The NWS-PTSD is a structured interview based on the gold standard DSM-IV-TR,20 with a closed-ended response (yes/no) format to be administered by lay interviewers either in person or by phone. The psychometric properties of the instrument have been well established, with sensitivity of 0.99 and specificity of 0.79,25,26 yielding a dichotomous diagnosis based on DSM-IV criteria, and a dimensional symptom count on a scale of 0 to 17. At both assessment time points the NWS-PTSD was administered by phone. Women were assigned to PTSD+ cohort if they met criteria for lifetime diagnosis of PTSD, with a cutoff ≥ 6 (cluster B ≥ 1, cluster C ≥ 3, and cluster D ≥ 2), or the non-PTSD cohort (PTSD−). Women with childhood abuse who did not meet diagnostic criteria for PTSD at recruitment but did meet criteria at 4 mo, were included in PTSD+.
Postpartum depression was assessed using the Postpartum Depression Screening Scale (PDSS), at 4 mo pp. The PDSS is a 35-item self-report instrument with 7 dimensions: sleeping/eating disturbances, anxiety/insecurity, emotional lability, cognitive impairment, loss of self, guilt/shame, and contemplating harming oneself. Mothers rate their degree of disagreement or agreement with each item on a range from “strongly disagree” (1) to “strongly agree” (5), with the resulting score ranging from 35 to 175. The α internal consistency reliabilities for the seven dimensions were shown to range from 0.83 to 0.94,27 and construct validity was confirmed by factor analysis.28 Additionally, a cutoff ≥ 80, associated with favorable sensitivity and specificity for major depression (according to the gold standard of the DSM-IV-TR), was further ascertained in psychometric studies.29
In this study, the sleep subscale, which consisted of 5 items (max score = 25), was used to separately assess sleep difficulty in the mothers, wherein this subscale was not included in the total depression symptom count.
Infant sleep
Sleep assessment of the infants was done at 4 mo pp, using the Child Sleep Habits Questionnaire30–32 administered to the mothers. The CSHQ is a 52-item parent-report instrument that assesses domains of bedtime behavior, sleep behaviors such as parasomnias, other night awakenings, morning awakening, and daytime sleepiness. Items are rated on a 3-point scale ranging from “rarely” (0–1 times per week) to “usually” (5–7 times per week), where higher scores connote more disruption. Mothers reported average bedtime, wakeup time, and number and duration of awakenings per night in the past week. Wake after sleep onset (WASO) was calculated by multiplying the average number of awakenings (#Wake) by average duration of wake during the night.
Mother-infant bonding
Mother-child relationship was assessed using the Postpartum Bonding Questionnaire (PBQ),33 a reliable screen for mother-infant relationship disorders.34 It consists of a 25-item scale assessing the mother's feelings or attitudes towards her baby (e.g., “I feel close to my baby,” “My baby irritates me”). Participants rate agreement with statements on a 6-point Likert scale ranging from 0 “always” to 5 “never,” with reverse coding of positive items, higher scores denote worse perceived bonding. The PBQ has 4 subscales including “impaired bonding” (12 items), “rejection and anger” (7 items), “anxiety about care” (4 items), and “risk of abuse” (2 items). For ethical reasons, the risk of abuse items were not administered.
Toddler behavior problems
The Child Behavior Checklist (CBCL) was administered to mothers at 18 months, during a playroom visit. CBCL for ages 1.5 to 5 years (CBCL/1.5–5)35 is a modified version of the 1992 CBCL for children age 2–3 years (CBCL 2–3).36 The revised CBCL/1.5–5 asks parents/caregivers to rate 99 specific child behaviors (e.g., Clings) as 0 “Not True of the child,” 1 “Somewhat or Sometimes True,” or 2 “Very True or Often True,” with an opportunity to write in 3 additional problem behaviors. The items are categorized into several narrow-band clusters (e.g., Emotionally Reactive, Anxious/Depressed, etc.) that are summarized into to broadband scales Internalizing Problems score (formed by combining items from Emotionally Reactive, Anxious/Depressed, Somatic Complaints, and Withdrawn), and Externalizing Problems score (formed by combining Attention Problems and Aggressive). Sleep Problems are treated as a separate syndrome. A Total Problems score is the summation of all the items.
Statistical Analyses
Cohort and gender comparisons consisted of ANOVAs for continuous variables and χ2 test for ordinal and nominal variables. Factor analysis was used to reduce the sleep questionnaire to coherent variables; we employed SPSS principal component analysis to extract uncorrelated linear combinations of the observed variables, allowing 200 iterations to resolve convergence. Varimax method of rotation was applied to maximize shared variance loading. The factor analysis yielded 2 factors described below in the text: Sleep Resist and Sleep Anxiety. Thus, in addition to the CSHQ summary scale, bedtime, wakeup time, and number of nighttime awakenings (#Wake), the CSHQ provided 3 additional derived variables for further analyses: Sleep Anxiety, Sleep Resist, and WASO. Predictive relationships between variables of interest (e.g., maternal psychopathology and infant sleep measures) were assessed using multiple and hierarchical regressions. Indirect effects were tested using bootstrapped multiple mediator tests.37
RESULTS
One hundred eighty-four women, aged 18–47 years, met inclusion/exclusion criteria for this study; 121 had a history of child abuse before age 16, and 63 were history negative controls (CON). Of the women with a history of child abuse, 83 also met criteria for PTSD diagnosis at recruitment or on subsequent follow-up data collection (PTSD+), and 38 did not (PTSD−). Eighty-four percent of the sample was recruited prior to week 28, while the remainder was recruited 6-8 weeks postpartum. Of women recruited while pregnant, 14% reported consuming no more than 1–2 alcoholic beverages per week (n = 8 PTSD+, n = 5 PTSD−, and n = 5 CON), while the reminder reported no drinking at all. Thirteen percent reported smoking on a regular basis (n = 6 PTSD+, n = 4 PTSD−, and n = 3 CON); the remainder did not smoke.
Table 1 summarizes demographic characteristics of the groups. Groups differed in income, with significantly more PTSD+ women in the lowest income bracket (χ2 = 6.0, P = 0.047) at 4 months, and less educated (χ2 = 15.10, P = 0.054). At 4 mo, postpartum, the groups also differed in the level of employment, with significantly fewer PTSD+ mothers employed than PTSD− and CON mothers (χ2 = 12.0, P = 0.003). The majority of women across groups breastfed their infants either exclusively or in combination with formula (χ2 = 5.8, P = 0.054). As women differed on education, income, and employment, a social economic status (SES) variable was created, by summing the values on the 3 scales. A median test on SES, with group as the independent variable, yielded a significant effect (χ2 = 8.66, P = 0.013). Thus, SES regression weights were entered in ANOVAs and regression models.
Table 1.
Demographic characteristics of the 3 groups. Groups differed in income, education, and employment
| PTSD+ | PTSD− | CON | ||
|---|---|---|---|---|
| N = 83 | N = 38 | N = 63 | ||
| Recruited 14-28 wks pn | 59 | 32 | 63 | 84% |
| Recruited 6-20 wks pp | 24 | 6 | 0 | 16% |
| Age | ||||
| Mean (SD) | 27.3 (5.7) | 27.7 (6.1) | 27.5 (4.9) | P > 0.1 |
| Range | 18-38 | 20-47 | 18-39 | |
| Ethnicity | ||||
| European American | 54% | 60% | 67% | P > 0.1 |
| African American | 32% | 24% | 26% | P > 0.1 |
| Latina | 3% | 5% | 2% | P > 0.1 |
| Native American | 1% | 0% | 0% | P > 0.1 |
| Asian American | 6% | 10% | 2% | P > 0.1 |
| Other | 4% | 0% | 3% | P > 0.1 |
| Education | ||||
| < High school | 8% | 0% | 5% | P > 0.1 |
| High school/GED | 14% | 17% | 18% | P > 0.1 |
| Trade/AA/some college | 33% | 26% | 9% | χ2 = 8.5, P = 0.016 |
| Bachelor | 28% | 28% | 39% | P > 0.1 |
| Post-grad | 18% | 30% | 28% | P > 0.1 |
| Income | ||||
| < $15K | 28% | 11% | 12% | χ2 = 6.0, P = 0.05 |
| $15-25K | 13% | 16% | 18% | P > 0.1 |
| $25-50K | 23% | 24% | 13% | P > 0.1 |
| > $50K | 38% | 49% | 57% | P > 0.1 |
| Employment | ||||
| Employed | 44% | 61% | 71% | χ2 = 12.0, P = 0.003 |
| Unemployed | 16% | 7% | 11% | χ2 = 5.5, P = 0.064 |
| Student, not working | 5% | 5% | 8% | P > 0.1 |
| Homemaker | 4% | 2% | 3% | P > 0.1 |
| Retired/disabled | 1% | 0% | 0% | P > 0.1 |
| SES | ||||
| Median | 8.27 | 9.66 | 10.08 | χ2 = 8.7, P = 0.013 |
| Living Situation | ||||
| Alone | 9% | 11% | 3% | P > 0.1 |
| With husband/partner | 70% | 76% | 72% | P > 0.1 |
| Parents/relatives | 14% | 11% | 22% | P > 0.1 |
| Housemate | 4% | 3% | 2% | P > 0.1 |
| Gender | ||||
| % Females | 49% | 41% | 45% | P > 0.1 |
| Feeding | ||||
| Breastfeeding | 37% | 54% | 49% | P = 0.09 |
| Formula only | 30% | 21% | 40% | P > 0.1 |
| Both | 33% | 25% | 11% | P > 0.1 |
SES was a composite scale containing income, education, and employment. pn, prenatal; pp, postpartum.
Severity of Abuse and Psychiatric Symptoms of Mothers
There were main effects of cohort on all CTQ subscales (all P values < 0.001). Post hoc analysis using Dunnett one-tail t-test (P = 0.05) found that both PTSD+ and PTSD− scored significantly higher than CON on all scales, and lower on the Minimization scale. PTSD+ scored significantly higher than PTSD− on all scales, except for the minimization scale, where the groups did not differ (see supplementary materials).
Multivariate ANOVA, with group assignment as the independent factor, and dependent factors of PTSD, postpartum depression, and sleep difficulty symptoms, with SES as a weighting factor, and α set to 0.001, was run. For all 3 symptom domains there was a main effect of group (PTSD: F1,187 = 50.29, P < 0.001, d = 1.0; depression: F1,187 = 21.51, P < 0.001, d = 0.99; sleep difficulty: F1,187 = 16.24, P < 0.001, d = 0.98). Post hoc analysis demonstrated that for all 3 symptom domains, PTSD+ mothers had more symptoms than both CON and PTSD− (P values < 0.001), while PTSD− were not different from CON (P values > 0.05, Table 2A).
Table 2.
Mothers' symptom severity at 4 mo and relationship with infants sleep
| A | PTSD Symptoms |
Depression Symptoms |
Sleep Disturbance Symptoms |
|||
|---|---|---|---|---|---|---|
| Mean (SD) | CI 99.9% | Mean (SD) | CI 99.9% | Mean (SD) | CI 99.9% | |
| PTSD+ | 5.05 (10.8)♦ | 4.1–6.0 | 69.14 (56.6)♦ | 63.1–75.2 | 11.58 (12.8)♦ | 10.3–12.9 |
| PTSD− | 1.44 (4.7) | −0.0–2.9 | 53.16 (50.3) | 43.6–62.8 | 8.29 (9.6) | 6.2–10.4 |
| CON | 1.00 (3.6) | −0.1–2.1 | 52.20 (48.2) | 44.8–59.6 | 8.56 (10.1) | 7.0–10.2 |
| B | R | P | R | P | R | P |
| # Wake | 0.154 | 0.056 | −0.050 | NS | 0.053 | NS |
| WASO | 0.231 | 0.002 | 0.147 | 0.046 | 0.183 | 0.013 |
| Sleep Resist | 0.170 | 0.038 | 0.089 | NS | 0.160 | 0.051 |
| Sleep Anxiety | 0.082 | NS | 0.214 | 0.008 | 0.105 | NS |
(A) Results of a multivariate ANOVA, with group assignment as the independent factor, PTSD, postpartum depression, and sleep difficulty symptoms as the dependent, and SES weighting factor. ‘♦’ denotes difference from control, post hoc Bonferroni correction P < 0.05. (B) Partial correlation analyses, controlling for group, were used to determine whether mothers' symptoms at 4 mo were associated with their infants' sleep behaviors.
Cohort effects on sleep
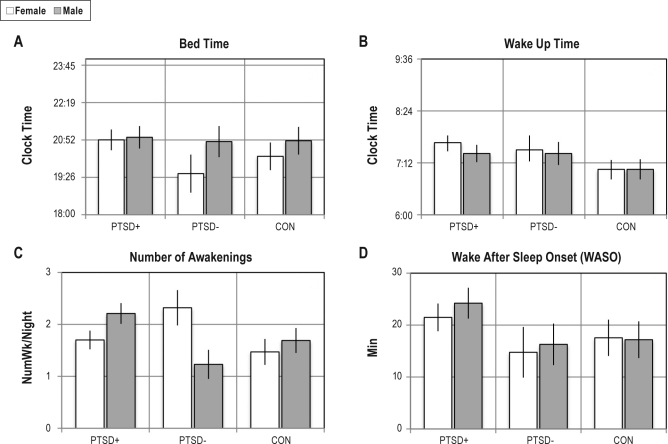
Multivariate ANOVA was used to compare male and female infants from the PTSD+, PTSD−, and CON cohorts on Bedtime, Wakeup Time, WASO, and #Wake, with SES as a weight factor, and critical α set to 0.001. There was a trend towards a main effect of cohort on WASO (F2,179 = 2.55, P = 0.081), with no main effect or interaction with gender (P > 0.05, see Figure 1). For all other measures, there was no effect of cohort, gender, or interaction (P > 0.05).
Figure 1.
Estimated marginal means derived from multivariate ANOVA comparing male and female infants from the PTSD+, PTSD−, and CON. (A-D) Bed Time, Wakeup Time, Number of Nightly Awakening (#Wake), Wake After Sleep Onset (WASO). There were no main effects or interactions.
Factor analysis was used to reduce the sleep questionnaire to coherent variables. The continuous variables Bedtime, Wakeup Time, and #Wake, were not included. After removing items with coefficients < 0.3, the Kaiser-Meyer-Olkin sampling adequacy was 0.71, and sphericity was significant (P < 0.001). With an Eigen value cutoff of 2.0, two factors, accounting for 29.1% of the total variance, emerged from this analysis: (1) items associated with resisting sleep (e.g., struggles at bedtime, resists going to bed) accounting for 19.8% of variance, where higher values denote more resistant behaviors; (2) items associated with anxiety around being alone (e.g., afraid of sleeping alone, needs parent in room to fall asleep), accounted for 9.2% of variance, where higher values denote more difficulty with separation during sleep. Despite being orthogonal, the 2 factors were both correlated with disturbed sleep (i.e., WASO and #Wake; see supplemental materials).
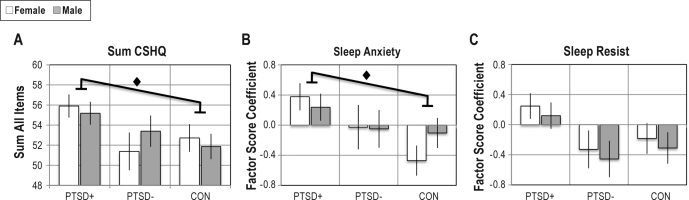
To assess whether the CSHQ scale in general, and the 2 factors specifically differed between cohorts and gender, multivariate ANOVA was used to compare male and female infants from the PTSD+, PTSD−, and CON cohorts, with SES as a weight factor, and critical α set to 0.001. There was a main effect of group on total CSHQ and Sleep Anxiety (F2,187 = 3.34, P = 0.038, d = 0.15; F2,187 = 5.08, P = 0.007, d = 0.32, respectively), with infants of PTSD+ scoring higher than CON (post hoc P values < 0.05, Figures 2A, B). There was no effect of cohort or gender for Sleep Resist (P values > 0.05, Figure 2C).
Figure 2.
Estimated marginal means derived from multivariate ANOVA comparing male and female infants from the PTSD+, PTSD−, and CON on the total score of the CSHQ, and the two derived factors. (A) Sum CSHQ: PTSD+ scored higher than CON, independent of gender. (B) Sleep Anxiety: There was a main effect of cohort, due to higher score in PTSD+ females compared with CON. (C) Sleep Resist: There were no mains effects of cohort or gender. ‘♦’ denotes main effect of cohort.
Partial correlation analyses, controlling for group, were used to determine whether mothers' symptoms at 4 mo were associated with their infants' sleep behaviors. The results of these analyses are reported in Table 2B. Briefly, WASO was positively correlated with all 3 maternal symptom domains (P values < 0.05). PTSD and sleep disturbance symptoms also correlated with sleep resisting behaviors, and depression symptoms correlated with separation anxiety around sleep.
Infant-mother relationship
The Parental Bonding Questionnaire (PBQ)38 was used to assess bonding between mother and her infant. Multivariate ANOVA was run with all the PBQ subscales and summary scale as the dependent factors, cohort and gender as fixed factors, and SES as weighting factor. There was a significant main effect of cohort for Impaired Bonding (F2,180 = 6.024, P = 0.003, d = 0.43), Rejection (F2,180 = 5.35, P = 0.005, d = 0.36), and total PBQ (F2,180 = 6.30, P = 0.002, d = 0.46), and a trend towards a main effect of cohort on Anxiety about Care (F2,180 = 2.92, P = 0.057). Additionally, there was a significant cohort by gender interaction on Impaired Bonding (F2,180 = 3.59, P = 0.029, d = 0.18) and trends towards significant interaction on Rejection and total PBQ (F2,180 = 2.96, P = 0.054, F2,180 = 2.97, P = 0.054, respectively). Interaction effects were due to higher scores in PTSD+ boys than CON boys, while CON girls tended to be higher than CON boys and not different than PTSD+ girls (Bonferroni correction P values < 0.05, Table 3). As the three subscales contribute to the summary scale, they were all highly and significantly correlated with the Total PBQ (R = 0.557-0.941, P < 0.001, data not shown), and subsequent analyses were performed using only the Total PBQ.
Table 3.
Multivariate ANOVA was run with all the PBQ subscales and summary scale as the dependent factors, cohort and gender as fixed factors, and SES as weighting factor
| Girls | Impaired Bonding |
Rejection |
Anxiety About Care |
Total PBQ |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | CI 99.9 | Mean | SD | CI 99.9 | Mean | SD | CI 99.9 | Mean | SD | CI 99.9 | |
| PTSD+ | 4.90 | 11.3 | 3.1–6.8 | 1.92 | 6.6 | 0.8–3.0 | 3.01 | 6.9 | 1.9–4.1 | 9.83 | 21.9 | 6.2–13.4 |
| PTSD− | 3.68 | 10.1 | 0.5–6.9 | 1.24 | 5.0 | 0.7–3.1 | 3.11 | 10.0 | 1.2–5.0 | 8.02 | 22.3 | 1.9–14.2 |
| CON | 4.57✦ | 9.4 | 2.2–6.9 | 1.66 | 5.4 | 0.3–3.1 | 2.49 | 6.4 | 1.1–3.9 | 8.72 | 17.0 | 4.2–13.3 |
| Boys | ||||||||||||
| PTSD+ | 6.00♦ | 12.7 | 4.1–7.9 | 2.57♦ | 9.1 | 1.5–3.7 | 3.13 ♦ | 6.7 | 2.0–4.3 | 11.69♦ | 26.1 | 8.1–15.3 |
| PTSD− | 3.90 | 9.0 | 1.9–7.3 | 1.54 | 5.3 | 0.3–3.5 | 2.19 | 4.7 | 0.9–4.2 | 7.63 | 16.0 | 3.8–14.2 |
| CON | 2.50✦ | 9.5 | 0.4–4.6 | 0.58 | 3.9 | −0.7–1.9 | 1.90 | 5.2 | 0.6–3.2 | 4.97 | 15.9 | 0.8–9.1 |
‘♦’ denotes difference from control, ‘✦’ denotes gender difference, post hoc Bonferroni correction P < 0.05.
To assess the role of infant sleep disturbance in bonding, stepwise hierarchical regression with Total PBQ scale as the dependent variable, cohort and gender in the 1st level, and infant sleep behaviors, WASO, Sleep Resist, and Sleep Anxiety in the 2nd level of the model (#Wake was used to calculate WASO and therefore not included in the model). The largest P value for entering the model was set at 0.01, and smallest P value for removing form the model was set at 0.05. Both 1st and 2nd level models were significant (F2,186 = 6.81, P = 0.010, F2,186 = 7.98, P = 0.001, R2change = 0.057, P = 0.004), with cohort alone and cohort with WASO (Table 4A) significantly associated with PBQ.
Table 4.
Hierarchical regression analyses, with total PBQ as the dependent variable
| A | Adj. R2 | Unstandardized Coefficients |
Standardized Coefficients |
P | CI 99.9% | VIF | ||
|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | ||||||
| Level 1 | 0.040 | Constant | 4.259 | 1.565 | 0.007 | |||
| Cohort | 1.717 | 0.658 | 0.215 | 0.010 | −0.5–3.9 | 1.00 | ||
| Level 2 | 0.090 | Constant | 2.917 | 1.590 | 0.069 | |||
| Cohort | 1.462 | 0.646 | 0.183 | 0.025 | −0.7–3.6 | 1.01 | ||
| WASO | 0.097 | 0.033 | 0.240 | 0.004 | 0.0–0.2 | 1.01 | ||
| B | Adj. R2 | Unstandardized Coefficients |
Standardized Coefficients |
P | CI 99.9% | VIF | ||
| B | SE | Beta | ||||||
| Level 1 | 0.109 | Constant | 2.662 | 1.449 | 0.068 | |||
| Cohort | 1.558 | 0.580 | 0.188 | 0.008 | −0.4–3.5 | 1.02 | ||
| WASO | 0.118 | 0.031 | 0.265 | < 0.001 | 0.0–0.2 | 1.02 | ||
| Level 2 | 0.254 | Constant | −3.472 | 1.670 | 0.039 | |||
| Cohort | 0.291 | 0.570 | 0.035 | 0.611 | −1.6–2.2 | 1.18 | ||
| WASO | 0.092 | 0.029 | 0.207 | 0.002 | 0.0–0.2 | 1.04 | ||
| Depression sxs | 0.152 | 0.025 | 0.420 | < 0.001 | 0.1–0.2 | 1.20 | ||
(A) Stepwise hierarchical regression with total PBQ scale as the dependent variable, cohort and gender in the 1st level, infant WASO, Sleep Anxiety, and Sleep Resist in the 2nd level. Both levels were significant (P < 0.001). (B) Stepwise hierarchical regression with cohort and WASO in the 1st level, mothers' PTSD, depression, and sleep difficulty symptoms in the 2nd level. Both levels of the model were significant (P < 0.001). VIF, variance inflation factor.
As WASO was correlated with postpartum mood and anxiety symptoms, a similar hierarchical regression model was run using cohort and WASO at the 1st level, and mothers' PTSD, depression, and sleep difficulty symptoms in the 2nd level. Both levels were significant (F2,186 = 12.31, P < 0.001, F3,186 = 21.98, P < 0.001, R2change = 0.147, P < 0.001), with WASO and depression symptoms significantly associated with PBQ, while cohort was no longer significant (Table 4B). Notably, adding depression symptoms to the model explained a much larger proportion of the variance in total PBQ (adj. R2 0.254 vs. 0.090), suggesting that depression symptoms mediated the relationship between PTSD diagnosis and PBQ.
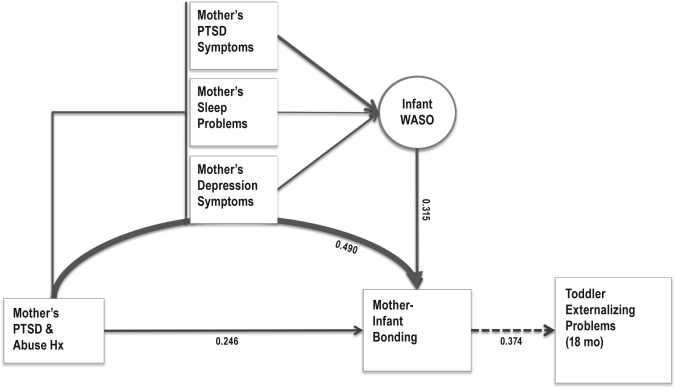
To test indirect effects of depression and WASO a bootstrapped multiple factor mediation test with 5000 bootstrap resamples37 was run, wherein PBQ was the dependent variable, cohort the independent variable, depression symptoms and WASO were mediators, and gender was a covariate. The estimated indirect effect coefficient for depression symptoms was 1.38 with CI 99% 0.56–2.49, suggesting a positive indirect effect (i.e., mediation effect) significant at α = 0.01. For WASO, the indirect effect was not significant (0.26, CI 99% −0.05–0.64), although the direct effect on PBQ remained significant (0.15, P = 0.002). Thus, depression symptoms significantly mediated the relationship between mothers' diagnosis history and mother-infant bonding, while infant sleep disturbance made an independent contribution to the mother-infant bonding outcome (Figure 3).
Figure 3.
Schematic of the model of the role of WASO and mothers symptoms in the development IGTT. Depression symptoms mediated the relationship between PTSD diagnosis and PBQ. WASO was correlated with mothers' mood and anxiety symptoms. WASO contributed independently (i.e., did not interact or mediate) to the variance in PBQ. PBQ, predicted degree of externalizing behaviors at 18 months. Thicker arrows denote a larger correlation or β coefficients. Numbers are βs derived from regression analyses.
Eighteen-month behavior problems
The Child Behavior Check List (CBCL) was administered at 18 months to 37 PTSD+, 17 PTSD−, and 20 CON. Table 5 summarizes the results of multivariate ANOVA on sleep problem, internalizing, and externalizing problems, with cohort and gender as fixed factors in both models, and SES as a weighting factor. There was a main effect of cohort on internalizing (F2,68 = 3.68, P = 0.031, d = 0.16) and a main effect of gender on externalizing (F1,68 = 6.76, P = 0.011, d = 0.21), and a trend towards a main effect of gender on internalizing (F1,68 = 3.81, P = 0.055), with girls rated lower than boys.
Table 5.
Results of analyses with sleep problems and the 2 broadband scales of the 1.5–5 Child Behavior Check List (CBCL)
| Girls | Sleep Problems |
Internalizing Problems |
Externalizing Problems |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | CI 99.9% | Mean | SD | CI 99.9% | Mean | SD | CI 99.9% | |
| PTSD+ | 2.50 | 1.8 | 0.6–4.4 | 6.25 | 4.6 | 2.9–9.6 | 11.44 | 6.2 | 5.3–17.6 |
| PTSD− | 3.00 | 2.0 | −0.1–6.1 | 4.83 | 4.4 | −0.6–10.3 | 10.33 | 6.9 | 0.3–20.4 |
| CON | 1.00 | 1.2 | 0.6–5.0 | 2.75 | 1.9 | −1.9–7.4 | 9.13 | 4.4 | 0.4–17.8 |
| Boys | |||||||||
| PTSD+ | 3.00 | 2.7 | 1.4–4.7 | 7.90 | 4.2 | 5.0–10.8 | 15.71 | 10.1 | 10.3–21.1 |
| PTSD− | 2.60 | 2.2 | 0.8–5.4 | 6.00 | 2.4 | 2.5–10.5 | 16.20 | 5.2 | 8.7–23.5 |
| CON | 2.83 | 2.0 | −1.7–3.7 | 5.67 | 3.6 | 1.8–9.5 | 13.33 | 4.8 | 6.2–20.5 |
Multivariate ANOVAs on sleep problem, internalizing, and externalizing, with cohort and gender as fixed factors in each of the models, and SES as weighting factor.
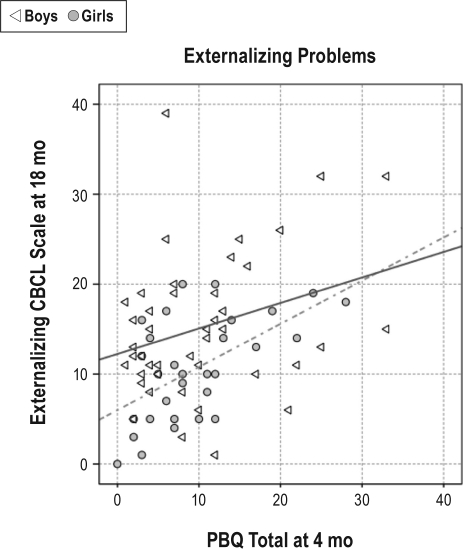
We first assessed whether the sleep problem scale was associated with any of the sleep variables acquired at 4 months, using correlation analyses. This analysis indicated that Sleep Anxiety was significantly correlated with CBCL sleep problems (R = 0.417, P = 0.002, data not shown). To determine whether internalizing and externalizing behavioral problems were associated with infant sleep disturbance and/or mother infant bonding at 4 months, stepwise regression analyses were run, in which WASO, Sleep Anxiety, and total PBQ were the independent variables, and gender was a weighting factor. The model for internalizing was not significant, but the model for externalizing was (F1,68 = 9.509 P = 0.003, Adj. R2 = 0.110), with PBQ significantly predicting externalizing problems (β = 0.350, Figure 4).
Figure 4.
Scatter plot of the correlation between PBQ at 4 mo (abscissa) and externalizing behaviors at 18 mo (ordinate), separated by gender. Gray circles for girls (R = 0.562, P = 0.001), white triangles for boys (R2 = 0.268, P = 0.082).
DISCUSSION
The primary aim of this study was to investigate sleep in infants of mothers with PTSD due to child abuse, as a potential contributing factor to mechanisms of intergenerational transfer of trauma-related symptoms (IGTT). Two notable observations appear to be that mothers' postpartum depression symptoms, rather than PTSD symptoms, predicted the degree of mother-infant bonding impairment, which in turn predicted externalizing problems at 18 months; and that the amount of wake during the night (WASO), while associated with mothers' symptom severity (in particular PTSD), contributed independently to the degree of mother-infant bonding impairment.
Participating mothers in this study were survivors of childhood abuse before the age of 16, with (PTSD+) or without (PTSD−) a lifetime diagnosis of posttraumatic stress disorder, and community controls (CON). The difference between PTSD+ and PTSD− women was clearly the severity and multi-dimensionality of abuse history, as the two groups did not differ in their degree of minimization and denial, as measured by the Childhood Trauma Questionnaire (see supplemental materials). Additionally, women in the PTSD+ group had a lower level of education and lower income, and fewer were employed (Table 1), consistent with the literature showing that the consequences of multi-type abuse produces more serious and less reversible consequences.39 PTSD+ women had more postpartum depression symptoms and sleep difficulty, and women with PTSD also reported more difficulty bonding with their infants (Table 3). These observations are in agreement with the literature on the impact of a history of child abuse, especially sexual abuse, on parental coping.14,40,41
The Child Sleep Habits Questionnaire (CSHQ) addresses an array of common sleep related problems in infants and toddlers and provides several quantitative measures of sleep, including bedtime, wakeup time, and frequency and duration of wake during the night. Although there are no established norms for the CSHQ, nor has it been validated in infants, it has been shown to be sufficiently sensitive for distinguishing clinical from community samples.30–32 Indeed in this study the CSHQ differentiated infants of the three cohorts (Figure 2A). Using factor analysis, we distilled two behavioral components that the CSHQ questionnaire addresses, one associated with sleep resisting behaviors, and a second associated with the child's separation anxiety and capacity to be alone during the sleep period. This distinction is analogous to the formulation put forward by Anders,42 who suggested that early development of sleep regulation has two components, an individual self-regulatory component associated with self-soothing, and a relational (parent-infant) component. Although orthogonal to each other, the two components were both highly correlated with sleep maintenance difficulty (WASO, #Wake, see supplementary materials).
Overall infant groups did not differ on quantitative sleep measures. Infants' bed- and wakeup time were similar across groups (Figures 1A, B), suggesting that the time allocated for night sleep was similar across cohorts independent of abuse history or PTSD. However, a tendency for more WASO in the PTSD group was found, a measure that was also strongly correlated with the severity of mothers' PTSD, mood, and sleep difficulty symptoms at that time. Although others have reported that parents are fairly accurate in estimating quantitative sleep measures when compared with actigraphy,43,44 our observations should be confirmed with objective measures. It is further unknown whether these differences in nighttime sleep were compensated for with naps during the day, which would point to either maturational or innate differences in the capacity to maintain a consolidated sleep period at night.
Infants of the PTSD+ cohort scored higher (worse) on the CSHQ, and specifically on the Sleep Anxiety factor (but not Sleep Resist, Figure 2B, C). The Sleep Anxiety factor was derived mainly from items that addressed the relationship aspect of sleep behaviors, in particular the ability of the infant to deal with the separation associated with sleep. It has been proposed that separation from caregivers and environment at bedtime challenge the infant's sense of security and comfort.45 Several studies have reported that more parent-infant interactions46,47 and active soothing behaviors (e.g., rocking)48 while the infant is falling asleep are associated with more nightly awakenings. Further, studies using objective measures of infant sleep report that while most infants wake up 1–3 times per night, as they mature they frequently return to sleep without arousing their parents, resulting in parents reporting that their child “slept through the night.” The problem sleepers are those infants who have difficulty with self-soothing, and require the parents' presence in order to return to sleep.42,45,49,50 As Sleep Anxiety was strongly correlated with WASO and #Wake, it may be that mothers with a history of child abuse, and especially those with PTSD, had a greater difficulty disengaging and encouraging their infants to self-soothe, resulting in more bedtime interactions.
The preliminary CBCL sleep data suggest that, at the very least, mothers' perception of their child's sleep problems was stable from 4 to 18 months. This is consistent with other reports of the persistence of sleep problems from infancy to early childhood.9 As increasing evidence suggests that persistent early-life sleep problems predict behavioral and emotional problems later in life,7,11,51 this observation supports the notion that antecedents of psychiatric disorders may lie in early life dysregulation of self-regulatory processes such as sleep behavior.
It has been suggested that intrusive and/or disengaged behaviors toward the infant52 adversely affect the attachment process, becoming a vehicle for intergenerational transfer of trauma.41,53,54 Although the PBQ does not assess attachment per se, the quality of the early mother-infant relationship likely makes an important contribution to the development of infant attachment style. Here we observed that mothers' diagnostic status and symptom severity were associated with her bonding experience. Specifically, PTSD+ mothers reported more difficulty with bonding compared with PTSD− and CON, an effect more pronounced with male infants. Interestingly, this relationship was mediated by the severity of postpartum depression symptoms (Figure 3), suggesting that it was the depressed mood, rather than anxiety symptoms that most impacted mother-infant relationship. Infant sleep disturbance, specifically WASO, also negatively affected mother-infant bonding, an effect that was independent of mothers' mood.
Although preliminary, CBCL externalizing behavioral problems were predicted by bonding difficulties (Figure 4), such that mothers who reported more bonding impairment had toddlers who rated higher on the externalizing scale. It has been proposed that mother-infant relationship predicts externalizing behaviors,55 although the evidence on this is mixed and causality is difficult to infer.56 It may be that the child's and/or mother's temperament, or other innate qualities, cause both bonding difficulty as well as high scores on the externalizing scale. Clearly, one such factor seemed to be gender, as women with PTSD reported more bonding difficulties with their male infants, and male toddlers also rated higher on the externalizing scale. Nevertheless, our findings suggest that variation in early mother-infant bonding explained a significant portion of the variation in externalizing behaviors more than a year later.
Some important limitations of the study should be noted. First, the mothers were the primary source of information on all measures, including their own symptom severity as well as their child's sleep and toddler's behavior difficulties (CBCL). It is possible that maternal mood and anxiety affected their perception of their child's sleep and behavior problems, which could explain the described relationships. Additional studies, using objective sleep measures, and corroborating measures on child behavior, will help bolster these results. Second, we note the absence of real-time information regarding prenatal mood and anxiety status during pregnancy, which may have played a role in the infants sleep patterns. Studies in rodents, non-human and human primates provide evidence that prenatal stress has significant effects on offspring development, increasing the risk for behavioral and affect problems.57 In fact, O'Connor et al. found that prenatal maternal anxiety and depression predicted sleep problems in infants at 18 and 30 months.58 Further expanding the study by recruiting women during pregnancy and expanding the sample at 18 months will help solidify the observations, and perhaps provide insight into the gender differences in CBCL scores. Third, a history of child abuse was clearly associated with participants SES. Although this covariance is expected based on prior research indicating associations between abuse, psychopathology, and SES outcomes,39 it is unclear how much SES contributes to symptomatology and the impact of home environment on infant sleep. Finally, while our findings (and those of others) indicate that mothers' symptoms contribute to sleep problems, how this relationship is propagated is unclear. Thus, the effect of mother's mood and anxiety symptoms on sleep may be due directly to nighttime interactions, or secondary to other aspects of maternal care, which also influence child behavior.
In sum, a novel observation in this report was the convergence of infant sleep difficulty and maternal mood as key independent factors in infant-mother bonding disturbance, which in turn predicted behavioral problems at 18 months. First, this suggests that the phenomenon of IGTT is mediated by maternal mood rather than maternal anxiety. While mood disorders are common in child abuse survivors and comorbid with PTSD,59 these findings indicate that mood difficulty may confer additional risk within the context of parenting and IGTT. Second, our findings suggest that the degree of infant sleep disturbance was potentially associated with parenting patterns linked with maternal PTSD, but independently exacerbated difficulty with mother-infant bonding. A more extensive study, including interventions focused on alleviating sleep related problems, may help shed light on the functional role of sleep in this cascade, revealing whether sleep is a biomarker of other emotional and behavioral problems, or plays a causal role in transgenerational transmission of psychopathology.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was performed at the University of Michigan, Ann Arbor, MI. It was funded by The University of Michigan, Addiction Research Center Postdoctoral Training Fellowship (IH); NIMH/NICHD K23-MH080147, PI: Muzik, the Rachel Upjohn Clinical Scholars Award, University of Michigan (MM), the Robert Wood Johnson Foundation Health & Society Scholars Program Fund (MM), and by NIH R01 NR008767-01 A1, PI: Seng, J. Additional support from NIAAA 5R37AA007065-S1.
Analysis of CTQ
Group difference in scores on the Child Trauma Questionnaire (CTQ). Multivariate ANOVA was used to assess group difference on the different scales. PTSD+ scored higher than PTSD− and CON, and PTSD− scored higher than CON on all scales. PTSD+ and PTSD− did not differ in minimization, although the both rated higher than CON. Post-hoc Dunnett t-test were used for paired comparisons. ‘♦’ difference from control P ≤ 0.001; ‘★’ difference from control, P ≤ 0.05; ‘+’ difference between PTSD+ and PTSD−, P ≤ 0.004.
| PTSD+ | PTSD− | CON | ||
|---|---|---|---|---|
| CTQ – Emotional Abuse | 12.21 (4.8)♦ | 8.50 (3.3)♦+ | 5.63 (0.9) | F(2,165) = 52.5, P < 0.001 |
| CTQ – Physical Abuse | 9.31 (4.7)♦ | 6.82 (2.9)★+ | 5.17 (0.5) | F(2,165) = 23.2, P < 0.001 |
| CTQ – Sexual Abuse | 9.48 (6.0)♦ | 6.76 (3.2)★+ | 5.00 (0.0) | F(2,165) = 17.2, P < 0.001 |
| CTQ – Emotional Neglect | 11.49 (4.7)♦ | 8.47 (3.3)♦+ | 5.70 (1.2) | F(2,165) = 41.3, P < 0.001 |
| CTQ – Physical Neglect | 8.04 (3.9)♦ | 6.29 (2.3)★+ | 5.02 (0.1) | F(2,165) = 17.9, P < 0.001 |
| CTQ – Minimization/Denial | 0.23 (0.6)♦ | 0.35 (0.7)♦ | 1.33 (1.2) | F(2,165) = 57.2, P < 0.001 |
‘♦’ difference from control P ≤ 0.001; ‘★’ difference from control, P ≤ 0.05 ‘+’ difference between PTSD+ and PTSD−, P ≤ 0.004
Factor Analysis of CSHQ:
Results of factor analysis on the CSHQ, not including Bedtime, Wakeup Time, #Wake, and WASO, and dichotomous items related to specific strategies of soothing. Using and Eigen value cutoff of 2.0, and removing items with coefficients below 0.3, 20 items remained, accounting for 29.1% of the total variance. Two factors remained, factor 1, ‘Sleep Resist’, 19.8% of variance; factor 2, ‘Sleep Anxiety’, 9.2% of variance. B. Alpha Cronbach Reliability Test for internal consistency was run on the items included within each of the two factors. C. Correlation analyses between the factors in the model and the quantitative variables.
Total Variance Explained
| Component | Initial Eigenvalues |
Extraction Sums of Squared Loadings |
Rotation Sums of Squared Loadings |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 4.618 | 15.393 | 15.393 | 4.618 | 15.393 | 15.393 | 3.875 | 12.918 | 12.918 |
| 2 | 2.094 | 6.978 | 22.371 | 2.094 | 6.978 | 22.371 | 2.836 | 9.453 | 22.371 |
| 3 | 1.988 | 6.627 | 28.998 | ||||||
| 4 | 1.857 | 6.191 | 35.189 | ||||||
| 5 | 1.567 | 5.223 | 40.412 | ||||||
| 6 | 1.403 | 4.678 | 45.090 | ||||||
| 7 | 1.271 | 4.238 | 49.327 | ||||||
| 8 | 1.235 | 4.118 | 53.445 | ||||||
| 9 | 1.165 | 3.884 | 57.329 | ||||||
| 10 | 1.085 | 3.616 | 60.945 | ||||||
| 11 | 1.030 | 3.434 | 64.380 | ||||||
| 12 | 1.013 | 3.376 | 67.755 | ||||||
| 13 | 0.903 | 3.010 | 70.766 | ||||||
| 14 | 0.871 | 2.904 | 73.670 | ||||||
| 15 | 0.805 | 2.685 | 76.355 | ||||||
| 16 | 0.775 | 2.584 | 78.939 | ||||||
| 17 | 0.722 | 2.407 | 81.346 | ||||||
| 18 | 0.662 | 2.207 | 83.553 | ||||||
| 19 | 0.620 | 2.068 | 85.621 | ||||||
| 20 | 0.586 | 1.954 | 87.575 | ||||||
| 21 | 0.517 | 1.722 | 89.297 | ||||||
| 22 | 0.484 | 1.614 | 90.910 | ||||||
| 23 | 0.458 | 1.528 | 92.438 | ||||||
| 24 | 0.437 | 1.457 | 93.895 | ||||||
| 25 | 0.384 | 1.279 | 95.174 | ||||||
| 26 | 0.352 | 1.172 | 96.346 | ||||||
| 27 | 0.325 | 1.084 | 97.430 | ||||||
| 28 | 0.285 | 0.949 | 98.379 | ||||||
| 29 | 0.257 | 0.858 | 99.237 | ||||||
| 30 | 0.229 | 0.763 | 100.000 | ||||||
Extraction Method: Principal Component Analysis.
Results of Factor Analysis Results of Factor Analysis
| Item | Component |
|
|---|---|---|
| Sleep Resist | Sleep Anxiety | |
| sleeps the right amount | −0.704 | −0.141 |
| struggles at bedtime | 0.662 | 0.059 |
| resists going to bed at bedtime | 0.584 | 0.041 |
| Is ready to go to bed at bedtime | −0.584 | −0.169 |
| sleeps the same amount each day | −0.576 | −0.097 |
| sleeps too little | 0.570 | < 0.010 |
| falls asleep within 20 minutes | −0.535 | −0.225 |
| goes to bed at same time at night | −0.472 | −0.011 |
| Is restless during sleep | 0.422 | < 0.010 |
| moves to someone | 0.359 | −0.012 |
| naps during the day | −0.343 | −0.153 |
| Is afraid of the dark | 0.317 | 0.190 |
| returns to sleep without help after waking | −0.311 | −0.277 |
| has trouble sleeping away from home | 0.289 | 0.012 |
| wakes more than once during night | 0.243 | 0.192 |
| snores loudly | 0.173 | 0.059 |
| baby sleeps in parent/sibling bed | 0.124 | −0.067 |
| needs parent in room to fall asleep | 0.086 | 0.697 |
| falls asleep alone in own bed | −0.127 | −0.685 |
| falls asleep in parents or siblings bed | 0.017 | 0.679 |
| falls asleep with rocking | 0.052 | 0.562 |
| Is afraid of sleeping alone | 0.296 | 0.489 |
| awakens alarmed by a dream | 0.111 | 0.433 |
| awakens screaming, sweating, or inconsolable | 0.289 | 0.354 |
| sleeps too much | 0.148 | 0.305 |
| seems to stop breathing during sleep | −0.099 | 0.249 |
| needs an object to fall asleep | −0.163 | 0.206 |
| Dad is in the house at bedtime | −0.017 | −0.187 |
| Mom is in the house at bedtime | 0.111 | −0.134 |
| wakes once during night | −0.039 | −0.082 |
Correlations with Quantitative Variables
| Component |
||
|---|---|---|
| Sleep Resist | Sleep Anxiety | |
| WASO | R = 0.343*** | R = 0.255** |
| #Wake | R = 0.290*** | R = 0.266** |
| Bedtime | R = −0.026 | R = −0.016 |
| Wakeup time | R = 0.133 | R = 0.228* |
P ≤ 0.05;
P ≤ 0.01;
P ≤ 0.001
REFERENCES
- 1.Fricke-Oerkermann L, Pluck J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–7. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anders TF, Eiben LA. Pediatric sleep disorders: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:9–20. doi: 10.1097/00004583-199701000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Schwichtenberg AJ, Goodlin-Jones B. Causes and correlates of frequent night awakenings in early childhood. Int Rev Neurobiol. 93:177–91. doi: 10.1016/S0074-7742(10)93008-0. [DOI] [PubMed] [Google Scholar]
- 4.Richman N. A community survey of characteristics of one- to two-year-olds with sleep disruptions. J Am Acad Child Psychiatry. 1981;20:281–91. doi: 10.1016/s0002-7138(09)60989-4. [DOI] [PubMed] [Google Scholar]
- 5.Armitage R, Flynn H, Hoffmann R, Vazquez D, Lopez J, Marcus S. Early developmental changes in sleep in infants: the impact of maternal depression. Sleep. 2009;32:693–6. doi: 10.1093/sleep/32.5.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gregory AM, Eley TC, O'Connor TG, Plomin R. Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. J Am Acad Child Adolesc Psychiatry. 2004;43:744–51. doi: 10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- 7.Gregory AM, Caspi A, Moffitt TE, Poulton R. Sleep problems in childhood predict neuropsychological functioning in adolescence. Pediatrics. 2009;123:1171–6. doi: 10.1542/peds.2008-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zuckerman B, Stevenson J, Bailey V. Sleep problems in early childhood: continuities, predictive factors, and behavioral correlates. Pediatrics. 1987;80:664–71. [PubMed] [Google Scholar]
- 9.Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics. 2003;111:e203–7. doi: 10.1542/peds.111.3.e203. [DOI] [PubMed] [Google Scholar]
- 10.Cortese S, Konofal E, Yateman N, Mouren MC, Lecendreux M. Sleep and alertness in children with attention-deficit/hyperactivity disorder: a systematic review of the literature. Sleep. 2006;29:504–11. [PubMed] [Google Scholar]
- 11.Sadeh A, McGuire JP, Sachs H, et al. Sleep and psychological characteristics of children on a psychiatric inpatient unit. J Am Acad Child Adolesc Psychiatry. 1995;34:813–9. doi: 10.1097/00004583-199506000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol. 2001;13:733–53. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- 13.Smith AK, Brennan PA, Galanti MB, Newport DJ, Cubells JF, Stowe ZN. Evaluation of child behavioral problems in the offspring of women with early sexual abuse history: implications of transgeneration effects. Biol Psychiatry. 2009;65:285. [Google Scholar]
- 14.Bifulco A, Moran PM, Ball C, et al. Childhood adversity, parental vulnerability and disorder: examining inter-generational transmission of risk. J Child Psychol Psychiatry. 2002;43:1075–86. doi: 10.1111/1469-7610.00234. [DOI] [PubMed] [Google Scholar]
- 15.Bowlby J. Separation. New York, NY: Basic Books; 1969. [Google Scholar]
- 16.Moehler E, Biringen Z, Poustka L. Emotional availability in a sample of mothers with a history of abuse. Am J Orthopsychiatry. 2007;77:624–8. doi: 10.1037/0002-9432.77.4.624. [DOI] [PubMed] [Google Scholar]
- 17.Anuntaseree W, Mo-suwan L, Vasiknanonte P, Kuasirikul S, Ma-a-lee A, Choprapawan C. Night waking in Thai infants at 3 months of age: association between parental practices and infant sleep. Sleep Med. 2008;9:564–71. doi: 10.1016/j.sleep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Richardson HL, Walker AM, Horne RS. Sleeping like a baby--does gender influence infant arousability? Sleep. 2010;33:1055–60. doi: 10.1093/sleep/33.8.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol. 2009;114:839–47. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 21.Beck LF, Morrow B, Lipscomb LE, et al. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. MMWR Surveill Summ. 2002;51:1–27. [PubMed] [Google Scholar]
- 22.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measures of child abuse and neglect. Am J Psychiatry. 1994;151:1132–6. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 23.Paivio SC, Cramer KM. Factor structure and reliability of the Childhood Trauma Questionnaire in a Canadian undergraduate student sample. Child Abuse Negl. 2004;28:889–904. doi: 10.1016/j.chiabu.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–90. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 25.Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984–91. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- 26.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- 27.Beck C, Gable RK. Postpartum depression screening scale: Development and psychometric testing. Nurs Res. 2000;49:272–82. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Beck C, Gable RK. Further validation of the postpartum depression screening scale. Nurs Res. 2001;50:155–63. doi: 10.1097/00006199-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Beck C, Gable RK. Comparative analysis of the performance of the Postpartum Depression Screening Scale with two other depression instruments. Nurs Res. 2001;50:242–50. doi: 10.1097/00006199-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Seifer R, Sameroff AJ, Dickstein S, Hayden L, Schiller M. Parental psychopathology and sleep variation in children. Child Adolesc Psychiatr Clin North Am. 1996;5:715–27. [Google Scholar]
- 31.Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. [PubMed] [Google Scholar]
- 32.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The children's sleep habits questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008;29:82–8. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- 33.Brockington IF, Fraser C, Wilson D. The Postpartum Bonding Questionnaire: a validation. Arch Womens Ment Health. 2006;9:233–42. doi: 10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- 34.Klier CM, Muzik M. Mother–infant bonding disorders and use of Parental Bonding Questionnaire in clinical practice. World Psychiatry. 2004;3:102–3. [PMC free article] [PubMed] [Google Scholar]
- 35.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2000. [Google Scholar]
- 36.Achenbach TM. Manual for Child Behavior Checklist/2-3 and 1992 Profile. Burlington, VT: University of Vermont; 1992. [Google Scholar]
- 37.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods Instrum Comput. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 38.Brockington IF, Oates J, George S, et al. A Screening Questionnaire for mother-infant bonding disorders. Arch Womens Ment Health. 2001;3:133–40. [Google Scholar]
- 39.Higgins DJ, McCabe MP. Multiple forms of child abuse and neglect: adult retrospective reports. Aggr Violent Behav. 2001;6:547–78. [Google Scholar]
- 40.Neigh GN, Gillespie CF, Nemeroff CB. The neurobiological toll of child abuse and neglect. Trauma Violence Abuse. 2009;10:389–410. doi: 10.1177/1524838009339758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lyons-Ruth K, Block D. The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Ment Health J. 1996;17:257–75. [Google Scholar]
- 42.Anders TF, Halpern LF, Hua J. Sleeping through the night: a developmental perspective. Pediatrics. 1992;90:554–60. [PubMed] [Google Scholar]
- 43.So K, Adamson TM, Horne RC. The use of actigraphy for assessment of the development of sleep/wake patterns in infants during the first 12 months of life. J Sleep Res. 2007;16:181–7. doi: 10.1111/j.1365-2869.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 44.Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children's sleep patterns. Arch Pediatr Adolesc Med. 2008;162:350–8. doi: 10.1001/archpedi.162.4.350. [DOI] [PubMed] [Google Scholar]
- 45.Anders TF. Infant sleep, nighttime relationships, and attachment. Psychiatry. 1994;57:11–21. doi: 10.1080/00332747.1994.11024664. [DOI] [PubMed] [Google Scholar]
- 46.Adair R, Bauchner H, Philipp B, Levenson S, Zuckerman B. Night waking during infancy: role of parental presence at bedtime. Pediatrics. 1991;87:500–4. [PubMed] [Google Scholar]
- 47.Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: A cross-cultural comparison. Sleep Med. 2010;11:393–9. doi: 10.1016/j.sleep.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 48.Johnson M. Infant and toddler sleep: A telephone survey of parents in one community. J Dev Behav Pediatr. 1991;12:108–14. [PubMed] [Google Scholar]
- 49.Goodlin-Jones BL, Burnham MM, Gaylor EE, Anders TF. Night waking, sleep-wake organization, and self-soothing in the first year of life. J Dev Behav Pediatr. 2001;22:226–33. doi: 10.1097/00004703-200108000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14:89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 51.Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009;10:787–96. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–90. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 53.Lyons-Ruth K. Contributions of the mother-infant relationship to dissociative, borderline, and conduct symptoms in young adulthood. Infant Ment Health J. 2008;29:203–18. doi: 10.1002/imhj.20173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hesse E, Main M. Second generation effects of unresolved trauma in nonmaltreating parents: Dissociated, frightening, and threatening parental behavior. Psychoanalytic Inquiry. 1999;19:440–81. [Google Scholar]
- 55.Pasco Fearon RM, Belsky J. Infant-mother attachment and the growth of externalizing problems across the primary-school years. J Child Psychol Psychiatry. 2011 doi: 10.1111/j.1469-7610.2010.02350.x. [DOI] [PubMed] [Google Scholar]
- 56.Rutter M. Environmentally mediated risks for psychopathology: research strategies and findings. J Am Acad Child Adolesc Psychiatry. 2005;44:3–18. doi: 10.1097/01.chi.0000145374.45992.c9. [DOI] [PubMed] [Google Scholar]
- 57.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–45. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 58.O'Connor TG, Caprariello P, Blackmore ER, Gregory AM, Glover V, Fleming P. Prenatal mood disturbance predicts sleep problems in infancy and toddlerhood. Early Hum Dev. 2007;83:451–8. doi: 10.1016/j.earlhumdev.2006.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilson DR. Health consequences of childhood sexual abuse. Perspect Psychiatr Care. 2010;46:56–64. doi: 10.1111/j.1744-6163.2009.00238.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
| PTSD+ | PTSD− | CON | ||
|---|---|---|---|---|
| CTQ – Emotional Abuse | 12.21 (4.8)♦ | 8.50 (3.3)♦+ | 5.63 (0.9) | F(2,165) = 52.5, P < 0.001 |
| CTQ – Physical Abuse | 9.31 (4.7)♦ | 6.82 (2.9)★+ | 5.17 (0.5) | F(2,165) = 23.2, P < 0.001 |
| CTQ – Sexual Abuse | 9.48 (6.0)♦ | 6.76 (3.2)★+ | 5.00 (0.0) | F(2,165) = 17.2, P < 0.001 |
| CTQ – Emotional Neglect | 11.49 (4.7)♦ | 8.47 (3.3)♦+ | 5.70 (1.2) | F(2,165) = 41.3, P < 0.001 |
| CTQ – Physical Neglect | 8.04 (3.9)♦ | 6.29 (2.3)★+ | 5.02 (0.1) | F(2,165) = 17.9, P < 0.001 |
| CTQ – Minimization/Denial | 0.23 (0.6)♦ | 0.35 (0.7)♦ | 1.33 (1.2) | F(2,165) = 57.2, P < 0.001 |
‘♦’ difference from control P ≤ 0.001; ‘★’ difference from control, P ≤ 0.05 ‘+’ difference between PTSD+ and PTSD−, P ≤ 0.004
| Component | Initial Eigenvalues |
Extraction Sums of Squared Loadings |
Rotation Sums of Squared Loadings |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 4.618 | 15.393 | 15.393 | 4.618 | 15.393 | 15.393 | 3.875 | 12.918 | 12.918 |
| 2 | 2.094 | 6.978 | 22.371 | 2.094 | 6.978 | 22.371 | 2.836 | 9.453 | 22.371 |
| 3 | 1.988 | 6.627 | 28.998 | ||||||
| 4 | 1.857 | 6.191 | 35.189 | ||||||
| 5 | 1.567 | 5.223 | 40.412 | ||||||
| 6 | 1.403 | 4.678 | 45.090 | ||||||
| 7 | 1.271 | 4.238 | 49.327 | ||||||
| 8 | 1.235 | 4.118 | 53.445 | ||||||
| 9 | 1.165 | 3.884 | 57.329 | ||||||
| 10 | 1.085 | 3.616 | 60.945 | ||||||
| 11 | 1.030 | 3.434 | 64.380 | ||||||
| 12 | 1.013 | 3.376 | 67.755 | ||||||
| 13 | 0.903 | 3.010 | 70.766 | ||||||
| 14 | 0.871 | 2.904 | 73.670 | ||||||
| 15 | 0.805 | 2.685 | 76.355 | ||||||
| 16 | 0.775 | 2.584 | 78.939 | ||||||
| 17 | 0.722 | 2.407 | 81.346 | ||||||
| 18 | 0.662 | 2.207 | 83.553 | ||||||
| 19 | 0.620 | 2.068 | 85.621 | ||||||
| 20 | 0.586 | 1.954 | 87.575 | ||||||
| 21 | 0.517 | 1.722 | 89.297 | ||||||
| 22 | 0.484 | 1.614 | 90.910 | ||||||
| 23 | 0.458 | 1.528 | 92.438 | ||||||
| 24 | 0.437 | 1.457 | 93.895 | ||||||
| 25 | 0.384 | 1.279 | 95.174 | ||||||
| 26 | 0.352 | 1.172 | 96.346 | ||||||
| 27 | 0.325 | 1.084 | 97.430 | ||||||
| 28 | 0.285 | 0.949 | 98.379 | ||||||
| 29 | 0.257 | 0.858 | 99.237 | ||||||
| 30 | 0.229 | 0.763 | 100.000 | ||||||
Extraction Method: Principal Component Analysis.
| Item | Component |
|
|---|---|---|
| Sleep Resist | Sleep Anxiety | |
| sleeps the right amount | −0.704 | −0.141 |
| struggles at bedtime | 0.662 | 0.059 |
| resists going to bed at bedtime | 0.584 | 0.041 |
| Is ready to go to bed at bedtime | −0.584 | −0.169 |
| sleeps the same amount each day | −0.576 | −0.097 |
| sleeps too little | 0.570 | < 0.010 |
| falls asleep within 20 minutes | −0.535 | −0.225 |
| goes to bed at same time at night | −0.472 | −0.011 |
| Is restless during sleep | 0.422 | < 0.010 |
| moves to someone | 0.359 | −0.012 |
| naps during the day | −0.343 | −0.153 |
| Is afraid of the dark | 0.317 | 0.190 |
| returns to sleep without help after waking | −0.311 | −0.277 |
| has trouble sleeping away from home | 0.289 | 0.012 |
| wakes more than once during night | 0.243 | 0.192 |
| snores loudly | 0.173 | 0.059 |
| baby sleeps in parent/sibling bed | 0.124 | −0.067 |
| needs parent in room to fall asleep | 0.086 | 0.697 |
| falls asleep alone in own bed | −0.127 | −0.685 |
| falls asleep in parents or siblings bed | 0.017 | 0.679 |
| falls asleep with rocking | 0.052 | 0.562 |
| Is afraid of sleeping alone | 0.296 | 0.489 |
| awakens alarmed by a dream | 0.111 | 0.433 |
| awakens screaming, sweating, or inconsolable | 0.289 | 0.354 |
| sleeps too much | 0.148 | 0.305 |
| seems to stop breathing during sleep | −0.099 | 0.249 |
| needs an object to fall asleep | −0.163 | 0.206 |
| Dad is in the house at bedtime | −0.017 | −0.187 |
| Mom is in the house at bedtime | 0.111 | −0.134 |
| wakes once during night | −0.039 | −0.082 |
| Component |
||
|---|---|---|
| Sleep Resist | Sleep Anxiety | |
| WASO | R = 0.343*** | R = 0.255** |
| #Wake | R = 0.290*** | R = 0.266** |
| Bedtime | R = −0.026 | R = −0.016 |
| Wakeup time | R = 0.133 | R = 0.228* |
P ≤ 0.05;
P ≤ 0.01;
P ≤ 0.001