Abstract
This study was aimed at evaluating the sensitivity and safety of a new technique to record triggered EMG thresholds from axillary chest wall electrodes when inserting pedicle screws in the upper thoracic spine (T2–T6). A total of 248 (36.6%) of a total of 677 thoracic screws were placed at the T2–T6 levels in 92 patients with adolescent idiopathic scoliosis. A single electrode placed at the axillary midline was able to record potentials during surgery from all T2–T6 myotomes at each side. Eleven screws were removed during surgery because of malposition according to intraoperative fluoroscopic views. Screw position was evaluated after surgery in the remaining 237 screws using a CT scan. Malposition was detected in 35 pedicle screws (14.7%). Pedicle medial cortex was breached in 24 (10.1%). Six screws (2.5%) were located inside the spinal canal. Mean EMG threshold was 24.44 ± 11.30 mA in well-positioned screws, 17.98 ± 8.24 mA (p < 0.01) in screws violating the pedicle medial cortex, and 10.38 ± 3.33 mA (p < 0.005) in screws located inside the spinal canal. Below a threshold of 12 mA, 33.4% of the screws (10/30) were malpositioned. Furthermore, 36% of the pedicle screws with t-EMG stimulation thresholds within the range 6–12 mA were malpositioned. In conclusion, assessment of upper thoracic pedicle screw placement by recording tEMG at a single axillary electrode was highly reliable. Thresholds below 12 mA should alert surgeons to suspect screw malposition. This technique simplifies tEMG potential recording to facilitate safe placement of pedicle screws at upper thoracic levels.
Keywords: Triggered EMG, Thoracic pedicle screws, Idiopathic scoliosis
Introduction
Triggered EMG testing for correct placement of pedicle screws in the thoracic spine has not proven to be as reliable as in the lumbar region. Misplaced low thoracic pedicle screws (T6–T12) can be identified by recording muscle activity from either the rectus abdominis or intercostal muscles [1–4]. However, in a recent experimental work, our research group showed that ipsilateral stimulus-triggered EMG could not discriminate screws that interfered with the medial pedicle wall, but without contact with neural tissues, from those with accurate intraosseous placement in the low thoracic spine [5]. Contrary to the report by Danesh-Clough et al. [3], we were able to obtain measurable EMG responses by direct stimulation of the spinal cord.
There is still no consensus regarding the safest technique for assessing accurate insertion of pedicle screws in the high thoracic spine (T1–T6) [6]. In a previous work recording compound motor action potentials (CMAP) from intercostal muscles corresponding to each myotome level (T3–T6), our group found a correlation between stimulation threshold values and correct screw placement [7]. The pedicle medial wall was consistently violated when threshold values dropped below 6 mA. Furthermore, a 60–65% decrease from the mean in triggered EMG threshold value predicted medially misdirected screw placement to a high degree of confidence.
In a previous study, we noted that, independently of the stimulated pedicle level, CMAP were obtained in all T3–T6 intercostal electrodes (unpublished data). To simplify the technique, a single recording bipolar electrode placed within the mid-axillary chest wall was used to record triggered EMG thresholds from levels T2 to T6, at each side. The purpose of this study is to describe this new technique and to evaluate its sensitivity in discriminating misplaced high thoracic pedicle screws. No clinical study has addressed an identical technique to assess thoracic screw placement at levels T2–T6.
Methods
A total of 677 thoracic screws were placed in 92 consecutive patients operated upon due to adolescent idiopathic scoliosis (AIS). Of these screws, 248 (36.6%) were placed at levels T2–T6. All thoracic pedicle screws were placed by senior spine surgeons according to the free-hand method [8].
Briefly, our protocol for placement of thoracic pedicles screws is as follows. The initial track at each pedicle site was created with a pedicle finder. After penetrating the screw to 35 mm in depth, the finder was removed and the surgeon palpated the walls of the entire pedicle with a ball-tipped probe. If there were no signs of pedicle breakage, the thoracic screw was inserted. Continuous monitoring of the spinal cord by posterior tibial nerve evoked somatosensory-evoked potentials; threshold-level MEP monitoring was carried out. If there were no changes in these potentials, we maintained the screw in that position. At that time, t-EMG activity was evaluated using a pedicle screw stimulation probe (Viasys™ Madison, WI, USA). These probes have a fully Teflon-insulated shaft terminating in a 3-mm ball tip as monopolar stimulator, which is manually affixed to the titanium screw once placed in the pedicle. The stimulation electrode was placed at the top of the screw stem. A constant voltage stimulus (rate of 1.0 Hz, 0.1 ms duration) was applied using the ascending current method (0.2–50 mA) until a compound muscle action potential was visually detected from the axillary chest wall electrodes (Keypoint, Alpine Biomed, Skovlunde, Denmark).
Only a set of two monopolar subdermal needle electrodes (Alpine Biomed, Skovlunde, Denmark) placed at the axillary midline was able to record potentials from all right and left T2–T6 pedicles (Fig. 1). Responses were recorded with a band-pass filter set between 20 and 5 kHz and amplifier sensitivity of 50 μV per division at 10-ms time intervals. If thresholds were below 9 mA, the surgeon checked the position of the screw by fluoroscopy. If the screw was positioned correctly, it was not removed. If fluoroscopy views indicated malposition, the surgeon removed the screw. Intraoperative repositioning of a pedicle screw was rarely attempted. We preferred to leave that pedicle without a screw since the risk of neural damage increases with such repositioning maneuvers, and because the mechanical properties of broken pedicles suffer. This technique for pedicle screw insertion is very well documented and safe enough to guarantee accurate screw position without neural damage.
Fig. 1.
Location of the needle electrodes at the axillary midline for recording t-EMG potentials from T2 to T6 pedicle screws
Screw position was also re-evaluated after surgery using a CT scan. A staff orthopedic spine surgeon and a musculoskeletal radiologist who were blinded to the intraoperative triggered EMG threshold values read these postoperative CT scans. The results of image analysis were matched with the intraoperative EMG threshold values.
Data were expressed as means ± SD. Statistical differences between the subgroups were studied using the Kruskal–Wallis ANOVA test and p values were calculated.
Results
During surgery, 14 screws showed t-EMG threshold values below 9 mA. After checking screw position by fluoroscopy in these cases, 11 screws were carefully removed because of clear signs of malposition (8 with breakage of the pedicle medial cortex, and 3 completely inside the canal). Three other screws were not taken out since these were apparently well positioned according to fluoroscopy views.
Postoperative CT scan of the remaining 237 screws revealed 35 malpositioned pedicle screws (14.7%). The pedicle medial cortex was breached by 24 (10.1%). Six screws (2.5%) were located inside the spinal canal, and five (2%) screws were placed too laterally, outside the pedicle.
Mean EMG threshold was 24.44 ± 11.30 mA for well-positioned screws, 17.98 ± 8.24 mA (p < 0.01) for screws violating the pedicle medial cortex, and 10.38 ± 3.33 mA (p < 0.001) for screws located inside the spinal canal. In all instances, thresholds were higher in screws placed at the convexity (Fig. 2).
Fig. 2.
Mean EMG thresholds according to the post-operative position of the pedicle screws on both sides of the thoracic curve
Three different t-EMG thresholds limits (12, 9 and 6 mA) were analyzed to establish the best stimulation intensity to discriminate screw misplacement. Table 1 summarizes the number of screws found at different locations according to post-operative CT scan, in relation to the various stimulation threshold limits. There were small differences among the 12, 9 and 6-mA threshold limits in detecting well-positioned screws. Below the 9 and 6-mA limits, there were many well-positioned screws (66.7 and 80%, respectively) indicating the poor accuracy of this technique for discrimination of misplaced screws. Notably, none of the screws were located outside of the vertebral column, that is, lateral deviation did not exceed 12 mA.
Table 1.
Screw position according to post-operative CT scan considering three different t-EMG stimulation thresholds
| t-EMG stimulation thresholds | ||||||
|---|---|---|---|---|---|---|
| 12 mA | 9 mA | 6 mA | ||||
| Screw position | Above N: 207 | Below N: 30 | Above N:228 | Below N:9 | Above N:232 | Below N:5 |
| Well positioned | 182 (87.9%) | 20 (66.6%) | 196 (85.9%) | 6 (66.7%) | 198 (85.3%) | 4 (80%) |
| Medial breakage | 19 (9.2%) | 5 (16.7%) | 22 (9.6%) | 2 (22.2%) | 23 (9.9%) | 1 (20%) |
| Inside canal | 1 (0.5%) | 5 (16.7%) | 5 (2.2%) | 1 (11.1%) | 6 (2.6%) | 0 |
| Outside lateral | 5 (2.4%) | 0 | 5 (2.2%) | 0 | 5 (2.2%) | 0 |
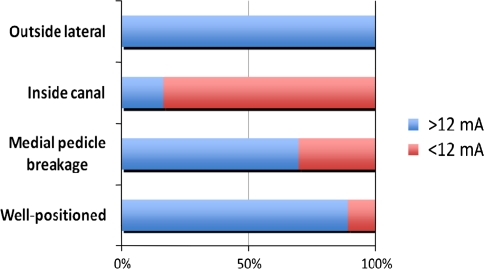
When pedicle screws with stimulation threshold values under 12 mA were analyzed, 33.4% of the screws (10/30) were determined to be malpositioned (5 screws inside the spinal canal) (Fig. 3). Screws with thresholds above 12 mA were correctly positioned inside the pedicle in 87.9% of cases. The rest were incorrectly positioned; intracanal location was observed for only one of these screws (16-mA threshold).
Fig. 3.
Percentage of pedicle screws in the different post-operative positions with EMG thresholds above and below 12 mA
Considering only the 25 pedicle screws with stimulation thresholds within the 6- to 12-mA range, an interval that has been said to only weakly discriminate between well-positioned and misplaced screws, only 9 (36%) were found to be malpositioned (Fig. 4). The percentage of screws showing medial breakage of the pedicle and that of screws inside the spinal canal were similar (16 and 20%).
Fig. 4.
Percentage of pedicle screws in the different post-operative positions with EMG thresholds within the 6- to 12-mA range
Finally, if the 11 screws removed intraoperatively because of EMG thresholds below 9 mA and fluoroscopic signs of malposition were taken into consideration, the total number of incorrectly placed screws increased to 46 out of the 248 inserted (18.5%).
There were no postoperative neurologic deficits or complaints of radicular chest wall pain that could indicate thoracic nerve root irritation.
Discussion
Despite initial resistance due to the potential risk of neural and vascular injuries [9–12], the use of thoracic pedicle screws is already a widely accepted technique for the correction of spinal deformities. Contrary to placement of lumbar pedicle screws, the safe placement of thoracic pedicle screws is technically challenging due to the particularities of their broad anatomic variability with progressively varying anteromedial and cephalic angulation [10, 13]. This is especially relevant at the upper T2–T6 levels, which renders the insertion of pedicle screws a highly demanding technique [14, 15].
Stimulus-triggered electromyography (t-EMG) has proven to be useful as an aid for precise pedicle screw insertion in the low thoracic spine, although the technique is less precise than in the lumbar spine [3, 16]. A major concern about the use of t-EMG in thoracic spine relates to monitoring the appropriate muscular group. Intercostal muscle recording has been reported to be unreliable due to the significant overlap of intercostal muscle innervation. Monitoring EMG responses in these muscles requires electrodes at all levels to ensure adequate coverage of the appropriate myotome [17]. A similar concern exists for t-EMG responses in the rectus abdominis and the external oblique muscle, since they share common intercostal and subcostal nerves (T7–T12) [4, 18].
Using intercostal EMG monitoring and 7.0 mA as a threshold, the screw stimulation technique exhibited 0.50 sensitivity and 0.83 specificity in detecting breached thoracic pedicles [19]. Assessing upper thoracic screws (T3–T6) and recording EMG responses at the intercostal muscles corresponding to each spinal level (8 pairs of electrodes), we found that medially misdirected screws always had threshold values lower than 6.0 mA [7].
A recent study described a series of thoracic screws in humans and reported that stimulation thresholds >11 mA had a 97.5% negative predictive value, suggesting that cortical violation is highly unlikely above this threshold intensity [17]. Although these authors did not recommend judging screw placement solely on stimulation thresholds, they concluded that pedicle screw stimulation might provide rapid and useful intraoperative information in humans. Our data support this conclusion. Above 12-mA thresholds, only 12.1% of the screws were misplaced. However, within the 6- to 12-mA threshold range, two-thirds of the screws were correctly positioned. These findings indicate that below the 12-mA stimulation threshold, most of the screws were positioned accurately. According to our results, only 20% of the screws had invaded the spinal canal and the other 16% exhibited pedicle medial bone–cortex breakage.
In the present study, using only a single pair of electrodes at a single axillary level of upper chest wall muscles, our previous data [7] could not be clearly confirmed and demonstrated the necessity of reevaluation. Screws located inside the spinal canal exhibited a mean threshold of 10.38 ± 3.33 mA (range, 6–16 mA). These data are in agreement with the 11-mA threshold limit proposed by Shi et al. [17]. Five out of six screws located inside the spinal canal showed thresholds below 12 mA, a much higher limit than the 6 mA described in our previous study [7]. Again, a change in the recording site seems to significantly modify the threshold response. In the present study, EMG potentials evoked from different upper thoracic levels were recorded at a single axillary level.
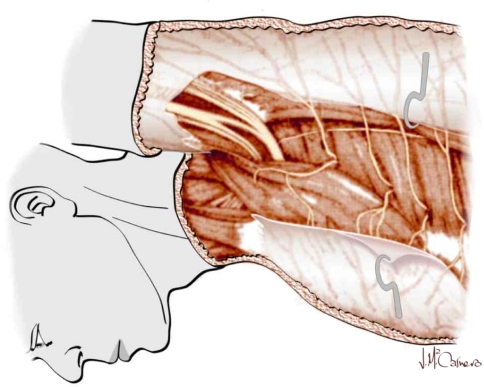
The lower thoracic nerves (spinal roots T7–T11) segmentally innervate rectus, obliquus and transversus abdominis musculature, but there is no single multimetameric muscle innervated by the upper thoracic nerves (spinal roots T2–T6) in the axillary line. Due to the anatomical relations of the subdermal recording electrodes, our hypothesis is that recorded biphasic potentials arise either from the numerous slender muscular filaments from the upper thoracic nerves that supply the intercostals, the subcostals, the levatores costarum, the serratus postero-superior and the transversus thoracis muscles or from the subdermal lateral perforant branches of the intercostal nerves (T2–T6) (Fig. 5).
Fig. 5.
Innervation of intercostal and transversus thoracis muscles by the perforant branches of the intercostal muscles. Patient in operative position
The great variability of EMG thresholds recorded intraoperatively highlights the advantages of combining other techniques such as palpation of the pedicle track before insertion of the screw and/or fluoroscopy in challenging cases. Checking with fluoroscopy. all screws with EMG thresholds below 9 mA helped us to identify malposition in two-thirds of these cases. However, fluoroscopy alone was not entirely reliable to check the correct screw position.
The reasons for EMG threshold variability are still unknown. Apart from inter-subject variability in tissue impedance, other factors may be considered. The anatomic particularities of the thoracic spine are suggested as the most important factor to explain such discordances. Alternately, the variable distance from screws to neural tissues may explain this discrepancy. In any case, this technique does not have 100% sensitivity and specificity. In our study, the 12-mA limit identified 88% of well-positioned screws. Thresholds above 12 mA accurately predict screw position. Pursuant to the results of this study, we have adjusted our clinical approach in cases below 12 mA. We reevaluated all screws with t-EMG thresholds below 12 mA and removed all those with thresholds below 6 mA. In other words, t-EMG recording below 12 mA after direct screw stimulation cannot be used to discriminate screw misplacement, because it is not completely reliable. Rather, this technique may be used in combination with others to decrease the uncertainty of intraoperative decisions.
In conclusion, assessment of upper thoracic pedicle screw placement (T2–T6) by recording triggered EMG thresholds at a single pair of axillary electrodes was highly reliable. Thresholds below 12 mA should alert surgeons to suspect either medial pedicle wall breach or intracanal screw position and should be reevaluated by other techniques. Future research can provide other more accurate EMG threshold limits.
Conflict of interest
No conflict of interest.
References
- 1.Calanchie B, Lebwohl N, Madsen P, Klose KJ. Intraoperative evoked EMG monitoring in an animal model. Spine. 1992;17:1229–1235. doi: 10.1097/00007632-199210000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Lenke LG, Padberg AM, Russo MH, Bridwell Kh, Gelb DE. Triggered electromyographic threshold for accuracy of pedicle screw placement. An animal model and clinical correlation. Spine. 1995;20:1585–1591. doi: 10.1097/00007632-199507150-00006. [DOI] [PubMed] [Google Scholar]
- 3.Danesh-Clough T, Taylor P, Hodgson B, Walton M. The use of evoked EMG in detecting misplaced thoracolumbar pedicle screws. Spine. 2001;26:1313–1316. doi: 10.1097/00007632-200106150-00008. [DOI] [PubMed] [Google Scholar]
- 4.Raynor BL, Lenke LG, Kim Y, Hanson DS, Wilson-Holden TJ, Bridwell KH, Padberg AM. Can triggered electromyography thresholds predict safe thoracic pedicle screw placement? Spine. 2002;27:2030–2035. doi: 10.1097/00007632-200209150-00012. [DOI] [PubMed] [Google Scholar]
- 5.Blas G, Burgos J, Regidor I, Barrios C, Solá R, García-Urquiza S, Hevia E. Recording diffusion responses from contralateral intercostal muscles after stimulus-triggered electromyography. Refining a tool for the assessment of thoracic pedicle screw placement in an experimental porcine model. Spine. 2009;34:391–396. doi: 10.1097/BRS.0b013e3181a273a6. [DOI] [PubMed] [Google Scholar]
- 6.Norton JA, Hedden DM. Monitoring placement of high thoracic pedicle screws by triggered electromyography of the intercostal muscles. Can J Surg. 2009;52:E47–E48. [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Olaverri JC, Zimick NC, Merola A, Blas G, Burgos J, Piza-Vallespir G, Hevia E, Vicente J, Sanpera I, Domenech P, Regidor I. Using triggered electromyographic threshold in the intercostal muscles to evaluate the accuracy of upper thoracic pedicle screw placement (T3–T6) Spine. 2008;33:194–197. doi: 10.1097/BRS.0b013e3181696094. [DOI] [PubMed] [Google Scholar]
- 8.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 9.Suk S, Lee C, Kim W, Chung Y, Park Y. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 10.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM. Placement of pedicle screws in the thoracic spine: I. Morphographic analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinkas C, An HS. Placement of pedicle screws in the thoracic spine: II. An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Xu R, Ebraheim N, Ou Y, Yeasting RA. Anatomic considerations of pedicle screw placement in the thoracic spine. Spine. 1998;23:1065–1068. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein J, Rydevik B, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop. 1992;284:34–46. [PubMed] [Google Scholar]
- 14.Panjabi MM, O’Holleran JD, Crisco JJ, 3rd, Kothe R. Complexity of the thoracic spine pedicle anatomy. Eur Spine J. 1997;6:19–24. doi: 10.1007/BF01676570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ugur HC, Attar A, Uz A, Tekdemir I, Egemen N, Genç Y. Thoracic pedicle: surgical anatomic evaluation and relations. J Spinal Disord. 2001;14:39–45. doi: 10.1097/00002517-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Lewis SJ, Lenke LG, Raynor B, Long J, Bridwell KH, Padberg A. Triggered electromyographic threshold for accuracy of thoracic pedicle screw placement in a porcine model. Spine. 2001;26:2485–2489. doi: 10.1097/00007632-200111150-00017. [DOI] [PubMed] [Google Scholar]
- 17.Shi Y-B, Binette M, Martin WH, Pearson JM, Hart RA. Electrical stimulation for intraoperative evaluation of thoracic pedicle screw placement. Spine. 2003;28:595–601. doi: 10.1097/01.BRS.0000049926.43292.93. [DOI] [PubMed] [Google Scholar]
- 18.Holland N. Intraoperative electromyography during thoracolumbar spinal surgery. Spine. 1998;23:1915–1922. doi: 10.1097/00007632-199809010-00023. [DOI] [PubMed] [Google Scholar]
- 19.Reidy DP, Houlden D, Nolan PC, Kim M, Finkelstein JA. Evaluation of electromyographic monitoring during insertion of thoracic pedicle screws. J Bone Joint Surg Br. 2001;83:1009–1014. doi: 10.1302/0301-620X.83B7.12017. [DOI] [PubMed] [Google Scholar]