Abstract
Background
In patients with scoliosis, the morphology of the pedicles differs from those in normal spines. Preoperative three-dimensional information of these complex anatomic situations means a great advantage for the surgeon in order to assess which pedicles can be instrumented safely avoiding screw misplacement and for the decisions in choosing the appropriate screw size. The objective of this study was to measure pedicle dimensions in scoliotic spines on three-dimensional computed tomographic (CT) scans and to determine the intra- and interobserver reliability of the method. Additionally, the pedicles that cannot be instrumented safely by available screws were identified.
Methods
All pedicles from T1 to L5 in 30 patients with scoliosis were measured by two independent observers. The pedicle width, height and length were assessed for two times with a 3-week interval. Intraclass correlation coefficients were used to determine the intra- and interobserver reliabilities. The diameters of the pedicles were matched with the dimensions of the smallest available pedicle screws of scoliosis implant systems.
Results
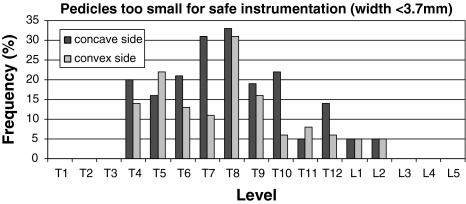
The intrarater reliability was strong in 60% of the parameters and moderate in 40%. The interrater reliability was strong in all parameters but in pedicle length. The concave-sided pedicles in the curve revealed to be smaller compared to the convex-sided ones. The highest percentage of size mismatch was found in levels T7 (31%) and T8 (33%).
Conclusions
Measurement of pedicle dimensions on three-dimensional CT scans is a reliable but time-consuming procedure to assess pedicle dimensions. CT measuring should be reserved for special cases, where the anatomic situation remains unclear despite X-ray. In scoliotic spines, one-third of the mid-thoracic pedicles cannot be instrumented safely with pedicle screws.
Keywords: Intraobserver reliability, Interobserver reliability, Scoliosis, Pedicle morphology, Three-dimensional CT
Introduction
The pedicle morphology in scoliotic spines differs from those in normal spines [2, 5–7, 10, 11]. For a safe pedicle screw placement in scoliosis surgery, the morphometry of the pedicles has to be taken into account by the surgeon to choose the appropriate screw sizes and to reduce the risk of screw misplacement. Therefore, preoperative imaging is necessary. Usually this planning has been done on plain X-rays. But as X-rays provide only two-dimensional information, three-dimensional imaging by computed tomography (CT) is getting more and more common in preoperative assessment. Especially in complex anatomic situations, the three-dimensional information means a great advantage for the surgeon. Pedicle size measurement on CT scans has been described in the literature [2]. Thus, the method has not been evaluated yet by determination of intra- and interobserver reliability.
The actual study was designed to assess the intra- and interobserver reliability of three-dimensional CT measurement of length, width and height of thoracic and lumbar pedicles in 30 scoliotic spines. Additionally, the pedicle diameters have been matched with the diameter of the smallest available pedicle screw.
Materials and methods
Preoperative CT scans of 30 patients with scoliosis scheduled for posterior fusion were analysed by two independent raters for two times with a 3-week interval between each session. The raters were two experienced orthopaedic spine surgeons. They were not informed about the second part of the study where pedicle dimensions were compared to pedicle screw sizes. The observers were blinded to their prior measurements and to the other observer.
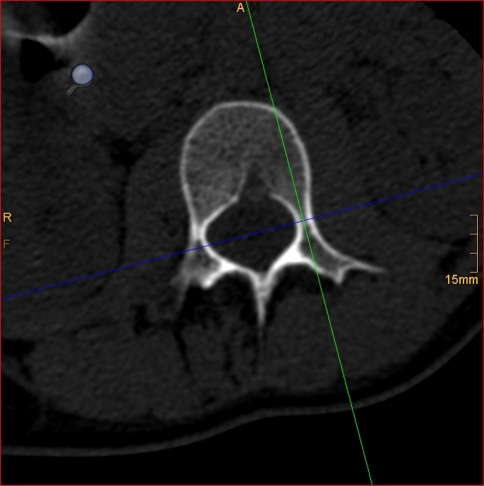
After reformatting with a slice thickness of 0.6–1.25 mm, pedicle width and height were measured perpendicular to each other (Figs. 1, 2, 3). Width was measured at the narrowest portion of the pedicle. The minimal distance between the outer borders (“outer diameter”) and between the inner borders (“inner diameter”) of the pedicles were measured.
Fig. 1.
For measuring diameters individual reformating of each pedicle was done, adjusted along a longitudinal axis through the pedicle. Pedicle width was measured perpendicular to this axis after reformatting with a slice thickness of 0.6–1.25 mm. The minimal distance between the outer borders (“outer diameter”) and between the inner borders (“inner diameter”) of the pedicles were measured
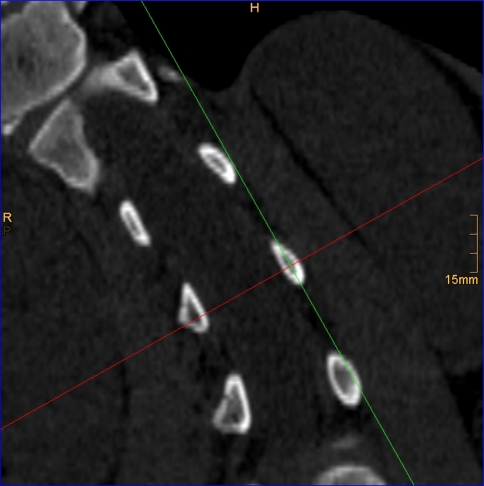
Fig. 2.
Adjustment of the two axes perpendicular on the longitudinal axis of the pedicle. Related to the vertebra, it is a longitudinal and a transversal line
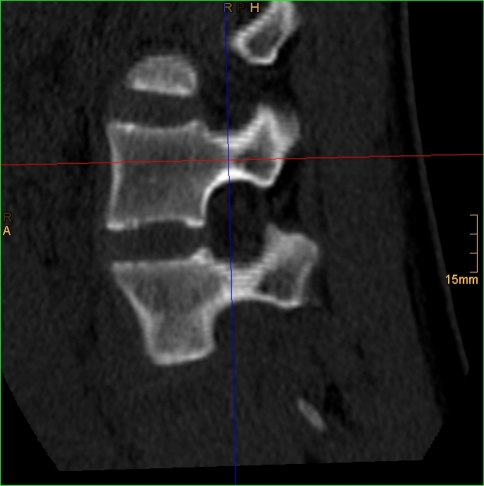
Fig. 3.
For measuring diameters individual reformatting of each pedicle was done, adjusted along a longitudinal axis through the pedicle. Pedicle height was measured perpendicular to this axis after reformatting with a slice thickness of 0.6–1.25 mm. The minimal distance between the outer borders (“outer diameter”) and between the inner borders (“inner diameter”) of the pedicles were measured
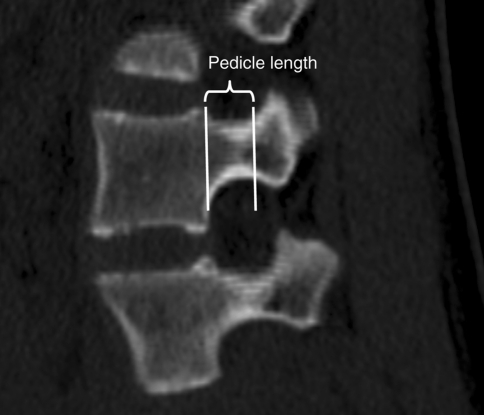
The pedicle length was measured along the longitudinal axis from the dorsal edge of the vertebral body to the articular processes (Fig. 4). In the anterior and posterior third of the pedicle, the width of the pedicle was measured from one cortical border to the other and this distance was bisected to find the pedicle axis.
Fig. 4.
Definition of pedicle length measured along the longitudinal axis from the dorsal edge of the vertebral body to the articular processes
All pedicles from the upper thoracic spine to the lower lumbar spine (T1–L5) were included. The results of both raters were compared and main values evaluated.
For measuring diameters, individual reformatting of each pedicle was done, adjusted along a longitudinal axis through the pedicle (Tiani 3D PACS software, version 3.3.16, Agfa-Gevaert N.V., Mortsel, Belgium).
There is a learning curve for digital measurement on the screen. However, because digital measurement is routinely used in the authors’ hospital since 2002, the two participating observers in the current study were already used to this technique.
In a second step, the measured pedicle diameters have been matched with the diameter of the smallest available screw for scoliosis instrumentation (Synthes, Oberdorf, Switzerland; 4.2 mm).
Appropriate size matching was defined when the diameter of the screw did not exceed 115% of the outer diameter, because the pedicles in paediatric spines are known to provide significant flexibility [8, 9]. As the smallest available screw has got a diameter of 4.2 mm, a minimum outer diameter of the pedicles of 3.6 mm (85% of the smallest screw diameter) was defined as “matching”.
Statistical evaluation
Descriptive statistics were done using the Excel program (Microsoft, Seattle, WA, USA). For group comparisons, the Mann–Whitney U test was performed where applicable. A p < 0.05 was considered significant.
Absolute differences between first and second measurement of the same observer was computed. Data are expressed as median (Md) and interquartile range (IQR). Intra- and interrater reliability was computed by rank correlation of Spearman’s rho (rs).
Correlations between 0.2 and 0.4 can be expressed as slight, >0.4 and 0.6 as moderate, >0.6 and 0.8 as strong and over 0.8 as very strong.
Statistical analyses were performed using SPSS 12.0 software (SPSS Inc., Chicago, IL, USA).
There was no ethical consent obtained especially for the study, as all CT scans were performed for preoperative planning routinely.
Results
Computed tomographic scans of 30 patients aged 9–24 years (mean 14.3 years) were evaluated (Table 1). The comparison of the age group 9–15 with 16–24 did not show statistically significant differences. So there was no age effect.
Table 1.
Classification of scoliosis in all subjects
| Patients initials | Age | Cobb angle | King’s classification | Cranial endvertebra | Caudal endvertebra |
|---|---|---|---|---|---|
| KS | 14 | 113 | 3 | T2 | L1 |
| SK | 14 | 100 | 3 | T2 | L1 |
| DP | 15 | 69 | 1 | T3 | T8 |
| KS | 28 | 50 | 1 | T11 | L5 |
| LC | 15 | 74 | 2 | T5 | T12 |
| PA | 19 | 53 | 4 | T6 | L3 |
| RS | 15 | 74 | 1 | T11 | L5 |
| SR | 10 | 46 | 3 | T4 | T12 |
| MS | 11 | 78 | 4 | T5 | L4 |
| ZS | 14 | 62 | 4 | T6 | L3 |
| GM | 16 | 46 | 4 | T5 | L5 |
| JS | 15 | 75 | 2 | T3 | T12 |
| PT | 9 | 30 | 4 | T3 | L4 |
| AJ | 14 | 30 | 4 | T8 | L3 |
| GF | 16 | 85 | 3 | T5 | L1 |
| DM | 18 | 70 | 2 | T5 | L2 |
| BL | 16 | 58 | 1 | T8 | L5 |
| BM | 14 | 100 | 1 | T11 | L4 |
| KS | 14 | 80 | 1 | T5 | L5 |
| ZL | 14 | 72 | 4 | T9 | L3 |
| SC | 15 | 110 | 4 | T4 | L5 |
| ZA | 15 | 106 | 4 | T9 | L5 |
| BM | 10 | 110 | 2 | T6 | T11 |
| BS | 16 | 55 | 2 | T5 | T12 |
| LF | 16 | 75 | 1 | T12 | L5 |
| SM | 9 | 73 | 4 | T1 | L1 |
| DM | 20 | 80 | 1 | T11 | L5 |
| GJ | 10 | 86 | 1 | T9 | L5 |
| GM | 12 | 30 | 1 | T11 | L5 |
| MG | 12 | 30 | 1 | T11 | L5 |
The mean Cobb angle was 70.8° (range 30°–130°). By definition, 20 cases were below 80°. 11 patients had very small pedicles on the concavity and in the proximal thoracic region. In cases with lower Cobb angles, the CT was performed either because of other reasons but the spine procedure (paediatric, internal or anaesthesiologic chest or abdominal assessment) or because the treating spine surgeon was in doubt about pedicle dimensions on plain X-rays.
Four of the five King curves types were represented. 13 patients suffered from idiopathic, 17 from neuropathic scoliosis.
A total of 1,020 pedicles from T1 to L5 were analyzed (Tables 2, 3, 4, 5, 6, 7).
Table 2.
Pedicle length
| Pedicle | Left | Right |
|---|---|---|
| T1 | 4.6 (2.3–6.6) | 4.6 (1.3–7.5) |
| T2 | 4.6 (2.1–9.0) | 4.5 (2.2–8.6) |
| T3 | 4.7 (2.1–9.0) | 4.6 (2.3–11.3) |
| T4 | 4.7 (2.7–7.8) | 4.7 (2.8–7.9) |
| T5 | 4.8 (2.3–8.5) | 4.9 (2.0–8.8) |
| T6 | 4.9 (2.1–9.3) | 5.2 (2.4–8.4) |
| T7 | 5.1 (1.6–8.2) | 5.2 (2.7–11.7) |
| T8 | 4.8 (1.4–8.1) | 5.2 (2.2–8.8) |
| T9 | 4.8 (2.6–9.4) | 4.6 (2.7–7.0) |
| T10 | 4.6 (1.9–9.3) | 5.0 (1.9–9.9) |
| T11 | 4.7 (1.8–9.0) | 4.9 (2–8.8) |
| T12 | 5.1 (1.3–9) | 5.3 (1.6–8.9) |
| L1 | 5.6 (1.2–11.3) | 5.8 (2.4–10.9) |
| L2 | 6.3 (3.7–10.5) | 6.0 (1.2–10.7) |
| L3 | 6.9 (3.1–10.9) | 6.4 (2.2–11.0) |
| L4 | 6.7 (2.6–11.4) | 6.7 (1.7–10.7) |
| L5 | 7.0 (0–11.7) | 6.2 (0–13.5) |
Table 3.
Pedicle width
| Pedicle | Left | Right | ||
|---|---|---|---|---|
| Outer diameter | Inner diameter | Outer diameter | Inner diameter | |
| T1 | 6.9 | 3.8 | 6.3 | 3.4 |
| (4.3–9.3) | (0.5–6.7) | (2.1–10.4) | (0–8.0) | |
| T2 | 5.9 | 3.3 | 5.1 | 2.5 |
| (3.3–8.5) | (1.3–6.9) | (1.5–8.7) | (0–6.8) | |
| T3 | 5.2 | 2.5 | 4.2 | 1.8 |
| (3.0–7.8) | (0.2–5.6) | (1.2–7.4) | (0–4.5) | |
| T4 | 4.8 | 2.1 | 3.8 | 1.3 |
| (1.3–10) | (0–4.3) | (1.0–6.8) | (0–4.2) | |
| T5 | 4.5 | 1.9 | 4.3 | 1.7 |
| (0.8–8.4) | (0–5.2) | (1.3–7.5) | (0–4.5) | |
| T6 | 4.4 | 1.7 | 4.7 | 2.1 |
| (1.2–9.0) | (0–4.5) | (2.0–7.7) | (0–4.5) | |
| T7 | 4.2 | 1.5 | 4.9 | 2.2 |
| (1.1–8.8) | (0–4.5) | (1.2–8.2) | (0–5.2) | |
| T8 | 4.4 | 1.7 | 4.9 | 2.2 |
| (1.4–9.3) | (0–7.4) | (0.9–8) | (0–7.2) | |
| T9 | 4.7 | 2.1 | 5.5 | 2.7 |
| (2.1–8.7) | (0.0–7.5) | (1.4–9.4) | (0–6) | |
| T10 | 5.0 | 2.1 | 5.8 | 2.9 |
| (1.4–9.7) | (0–6.7) | (2.3–9.9) | (0.1–8.3) | |
| T11 | 6.1 | 3.3 | 6.4 | 3.4 |
| (0.8–10.2) | (0–8.9) | (2.8–10.8) | (0–8.0) | |
| T12 | 6.4 | 3.3 | 6.3 | 3.2 |
| (1.5–13.5) | (0–10.7) | (2.4–12.5) | (0–9.4) | |
| L1 | 5.9 | 3.0 | 6.1 | 3.2 |
| (2.1–11.7) | (0–8.1) | (1.5–10.4) | (0–7.6) | |
| L2 | 6.1 | 3.3 | 6.6 | 3.6 |
| (2.5–11.6) | (0.0–7.8) | (1.2–13.1) | (0.0–8.8) | |
| L3 | 7.7 | 4.7 | 8.2 | 5.0 |
| (3.8–11.7) | (1–10) | (3.3–16) | (0.8–12) | |
| L4 | 9.5 | 6.2 | 9.3 | 5.9 |
| (3.7–15.1) | (2.0–11.7) | (4.0–15.1) | (2.8–12.8) | |
| L5 | 12.4 | 9.0 | 11.6 | 7.9 |
| (4.6–19.1) | (2.2–16.3) | (5.1–18.4) | (2.6–14.4) | |
Table 4.
Pedicle height
| Pedicle | Left | Right | ||
|---|---|---|---|---|
| Outer diameter | Inner diameter | Outer diameter | Inner diameter | |
| T1 | 7.5 | 4.3 | 7.2 | 4.3 |
| (4.6–11.2) | (1.4–7.9) | (3.7–10.4) | (1.4–7.9) | |
| T2 | 8.8 | 5.4 | 8.2 | 4.8 |
| (6.3–12.3) | (2.2–8.7) | (2.4–13) | (0.0–9.6) | |
| T3 | 8.7 | 5.4 | 8.5 | 4.7 |
| (4.5–13.5) | (1.2–10.3) | (4.1–13.8) | (0.0–13.8) | |
| T4 | 8.8 | 5.3 | 8.7 | 4.4 |
| (4.2–13.8) | (0–10.6) | (4.6–12.9) | (0–8.3) | |
| T5 | 8.6 | 5.0 | 8.4 | 4.7 |
| (3.0–13.8) | (0.0–9.1) | (1.9–11.3) | (0.0–9.4) | |
| T6 | 8.2 | 4.5 | 9.0 | 5.2 |
| (2.0–13.0) | (0–8.4) | (5.3–14.2) | (0–9.2) | |
| T7 | 8.4 | 4.3 | 9.3 | 5.8 |
| (3.2–14.3) | (0–10) | (5.1–12.0) | (0–9.8) | |
| T8 | 8.5 | 4.7 | 9.5 | 5.7 |
| (2.7–14.2) | (0–9.7) | (2.6–14.0) | (0–9.4) | |
| T9 | 9.7 | 5.9 | 10.4 | 6.6 |
| (1.8–14) | (0.0–11) | (4.1–17.4) | (0–12.4) | |
| T10 | 11.0 | 6.7 | 11.3 | 7.7 |
| (6.1–15) | (0.0–13) | (5.7–16.4) | (3.0–13.7) | |
| T11 | 11.7 | 7.9 | 11.7 | 8.1 |
| (5.0–16.5) | (0–14) | (7.4–15.6) | (0–13.4) | |
| T12 | 12.6 | 8.0 | 11.5 | 7.5 |
| (5.7–20.0) | (0–13.6) | (6.5–17.6) | (0.0–15.0) | |
| L1 | 11.7 | 7.1 | 11.2 | 7.2 |
| (6.3–16.6) | (0–13) | (6.7–15.4) | (0.0–12.6) | |
| L2 | 11.7 | 6.9 | 10.8 | 6.6 |
| (7.4–17.2) | (0.0–12.2) | (7.2–14.7) | (0.0–11.3) | |
| L3 | 11.3 | 7.3 | 11.4 | 7.0 |
| (7.3–16.0) | (4.7–12.5) | (8.1–15.3) | (3.9–11.6) | |
| L4 | 10.7 | 7.1 | 10.7 | 6.6 |
| (7.2–14.1) | (2.8–10.4) | (8.2–14.8) | (2.6–11.6) | |
| L5 | 11.2 | 7.5 | 11.1 | 7.3 |
| (6.8–19.9) | (4.1–14.8) | (7.1–20.6) | (3.1–17.9) | |
Table 5.
Pedicle length
| Pedicle | concave | convex | p value |
|---|---|---|---|
| T1 | 4 | ||
| (3.4, 4.6) | |||
| T2 | 4.4 | ||
| (3.8, 5) | |||
| T3 | 4.6 | 6.1 | 0.3 |
| (2.8, 6.4) | (4.6, 7.5) | ||
| T4 | 5.1 | 4.5 | 0.1 |
| (3.8, 6.9) | (2.7, 6.8) | ||
| T5 | 4.5 | 4.5 | 0.5 |
| (2.6, 6.9) | (2, 7.9) | ||
| T6 | 4.8 | 4.9 | 0.7 |
| (2.4, 7.7) | (1.3, 8.4) | ||
| T7 | 4.8 | 5.1 | 0.9 |
| (2.6, 8.2) | (2.3, 7.9) | ||
| T8 | 4.4 | 5.1 | 0.3 |
| (2.5, 7.7) | (2.2, 9.4) | ||
| T9 | 4.8 | 4.7 | 0.7 |
| (2.6, 8.9) | (1.5, 9.4) | ||
| T10 | 4.6 | 4.8 | 1.0 |
| (1.3, 8.6) | (1.9, 8.8) | ||
| T11 | 4.8 | 4.6 | 0.4 |
| (0.2, 9.9) | (0, 8.9) | ||
| T12 | 5.2 | 5.1 | 0.8 |
| (2.6, 8.1) | (0, 8.7) | ||
| L1 | 5.3 | 5.5 | 0.7 |
| (2.2, 8.8) | (2.5, 10.9) | ||
| L2 | 6.0 | 6.2 | 0.5 |
| (3.1, 8.5) | (3.9, 9.9) | ||
| L3 | 6.2 | 6.5 | 0.6 |
| (2.8, 11) | (3.3, 9.8) | ||
| L4 | 5.8 | 6.5 | 0.2 |
| (1.4, 9.4) | (1.7, 9.7) | ||
| L5 | 6.4 | 6.8 | 0.4 |
| (3.7, 13.5) | (3.8, 11.7) |
Table 6.
Pedicle width
| Pedicle | Concave outer diameter | Convex outer diameter | P value | Concave inner diameter | Convex inner diameter | p value |
|---|---|---|---|---|---|---|
| T1 | 7.2 | 4.8 | ||||
| (6, 8.4) | (3.9, 5.6) | |||||
| T2 | 7.8 | 5.4 | ||||
| (7.1, 8.9) | (4.7, 6.2) | |||||
| T3 | 5.9 | 5.6 | 0.7 | 3.1 | 2.8 | 0.8 |
| (4.4, 7.5) | (5, 6.1) | (1.4, 5.6) | (2.4, 3.1) | |||
| T4 | 5.0 | 4.9 | 0.93 | 2.2 | 2.3 | 0.8 |
| (2.7, 7.1) | (3.2, 6.8) | (0.9, 4.3) | (0.3, 4.2) | |||
| T5 | 4.8 | 4.6 | 1.0 | 2.1 | 2.0 | 0.8 |
| (1.3, 8.4) | (1.3, 6.9 | (0, 4.9) | (0, 5) | |||
| T6 | 5.0 | 5.3 | 0.1 | 2.4 | 2.4 | 0.4 |
| (2.2, 9.1) | (2.4, 7.8) | (0, 5.8) | (0, 4.5) | |||
| T7 | 4.6 | 5.3 | 0.05 | 2.0 | 2.6 | 0.03 |
| (2.5, 9.1) | (2.3, 9.4) | (0, 5.7) | (0.1, 5.3) | |||
| T8 | 4.4 | 4.7 | 0.4 | 1.9 | 2.3 | 0.3 |
| (0, 6.2) | (0, 7.4) | |||||
| (1.7, 9.9) | (1.2, 9.3) | |||||
| T9 | 5.4 | 5.5 | 0.5 | 2.7 | 2.9 | 0.4 |
| (0, 6.6) | (0, 7.5) | |||||
| (1.4, 10.7) | (1.3, 9.5) | |||||
| T10 | 6.1 | 6.2 | 0.6 | 3.0 | 3.2 | 0.6 |
| (0, 7.29) | (0.1, 8.5) | |||||
| (2, 10.6) | (0.1, 11.2) | |||||
| T11 | 7.4 | 8.0 | 0.5 | 4.3 | 3.9 | 0.6 |
| (0, 9.5) | (0.1, 8.9) | |||||
| (2.3, 12.5) | (2, 12.2) | |||||
| T12 | 6.4 | 7.3 | 0.1 | 3.3 | 4.2 | 0.1 |
| (0, 9.3) | (0.1, 10.7) | |||||
| (2.9, 12.6) | (3.4, 13.5) | |||||
| L1 | 7.4 | 6.3 | 0.1 | 3.9 | 3.3 | 0.3 |
| (0.1, 7.3) | (0, 6.7) | |||||
| (2.8, 11.8) | (3.3, 11.8) | |||||
| L2 | 7.5 | 6.3 | 0.02 | 4.0 | 2.9 | 0.03 |
| (0, 8.4) | (0.5, 6.5) | |||||
| (2.4, 11.9) | (2.5, 10.6) | |||||
| L3 | 9.2 | 8.3 | 0.2 | 5.7 | 5 | 0.3 |
| (1.6, 12.8) | (1.7, 9.6) | |||||
| (4.4, 16.6) | (4.4, 12.9) | |||||
| L4 | 9.4 | 10.3 | 0.1 | 5.5 | 6.4 | 0.2 |
| (2.1, 10.9) | (1.6, 12.3) | |||||
| (5.1, 13.7) | (5, 16) | |||||
| L5 | 11.6 | 12.7 | 0.2 | 7.8 | 8.5 | 0.4 |
| (2.9, 14.4) | (3.2, 15.8) | |||||
| (5.3, 18.4) | (6.9, 20.1) |
Table 7.
Pedicle height
| Pedicle | Concave outer diameter | Convex outer diameter | p value | Concave inner diameter | Convex inner diameter | p value |
|---|---|---|---|---|---|---|
| T1 | 5.9 | 2.5 | ||||
| (5.6, 6.1) | (0, 7.4) | |||||
| T2 | 9.1 | 5.3 | ||||
| (7.7, 10.7) | (3.9, 7.7) | |||||
| T3 | 8 | 7.6 | 0.5 | 5.3 | 5.6 | 0.9 |
| (6.9, 12) | (5.9, 9.2) | (3.4, 8.6) | (5, 6.2) | |||
| T4 | 9.1 | 8.9 | 0.9 | 5.2 | 4.9 | 0.8 |
| (4.9, 11.7) | (6.2, 11.7) | (1.4, 8.4) | (2.1, 8.3) | |||
| T5 | 8.3 | 8.3 | 0.7 | 4.9 | 4.3 | 0.5 |
| (5, 11.3) | (2.8, 11.8) | (0, 9.9) | (0, 7.5) | |||
| T6 | 7.9 | 8.8 | 0.03 | 4.2 | 4.9 | 0.1 |
| (4.5, 10.5) | (4.2, 12) | (0.1, 7.9) | (0, 8.1) | |||
| T7 | 8.1 | 9.2 | 0.05 | 3.6 | 5.2 | 0.008 |
| (4.2, 11.6) | (4.8, 14.3) | (0, 6.8) | (0, 8.9) | |||
| T8 | 8.7 | 9.7 | 0.1 | 4.4 | 5.4 | 0.1 |
| (5.1, 14.5) | (3.6, 14) | (0.2, 9.3) | (0, 9.7) | |||
| T9 | 8.9 | 10.6 | 0.01 | 5.4 | 6.2 | 0.2 |
| (3.2, 14.9) | (3.2, 16) | (0.1, 9) | (0, 11.6) | |||
| T10 | 10.2 | 11.0 | 0.3 | 5.9 | 7.7 | 0.01 |
| (5.7, 16.4) | (4.7, 15.3) | (0, 12) | (2.3, 12) | |||
| T11 | 11.1 | 12.0 | 0.1 | 7.4 | 8.3 | 0.2 |
| (7.4, 15) | (6.2, 16.3) | (3.1, 12.5) | (4.1, 13.2) | |||
| T12 | 10.8 | 11.5 | 0.6 | 6.3 | 7.3 | 0.3 |
| (6.7, 15.8) | (0, 15.9) | (0, 11.2) | (0, 11.8) | |||
| L1 | 11.1 | 11.7 | 0.4 | 6.8 | 7.0 | 0.7 |
| (6.7, 16.3) | (4.1, 16.7) | (2.5, 12.6) | (0, 12.6) | |||
| L2 | 11.0 | 11.2 | 0.5 | 5.5 | 6.6 | 0.04 |
| (7.2, 16.3) | (5.7, 17) | (0, 10.2) | (0, 11.3) | |||
| L3 | 11.4 | 11.5 | 0.8 | 6.7 | 7.1 | 0.5 |
| (7.5, 16) | (8.3, 15) | (3.6, 12.5) | (3.8, 11.5) | |||
| L4 | 10.9 | 10.3 | 0.2 | 6.7 | 6.4 | 0.6 |
| (8.1, 14.7) | (7.3, 13.7) | (2.6, 11.6) | (3, 10.2) | |||
| L5 | 11.1 | 10.8 | 0.9 | 6.6 | 6.5 | 0.004 |
| (6.1, 20.6) | (7.7, 14) | (1.6, 17.9) | (3.8, 10) |
The measurements of all parameters of one level took the raters between 2 and 10 min.
Upper thoracic spine (T1–T4)
The mean pedicle widths of the upper thoracic spine were 6.5 mm (range 2.7–8.9 mm) on the concave side and 5.3 mm (range 3.2–6.8 mm) on the convex side for the outer diameter, and 3.9 mm (range 0.9–6.2 mm) on the concave side and 2.6 mm (range 0.3–4.2 mm) on the convex side for the inner diameter. The mean pedicle heights of the upper thoracic spine were 8.0 mm (range 4.9–12 mm) on the concave side and 8.3 mm (range 5.9–11.7 mm) on the convex side for the outer diameter, and 4.6 mm (range 0–8.6 mm) on the concave side and 5.3 mm (range 2.1–8.3 mm) on the convex side for the inner diameter.
The mean concave pedicle transverse width appeared to be slightly larger than the corresponding mean measurements on the convex side in all vertebrae. The differences between the pedicle width and height of the concave and convex side were not significant.
Middle thoracic spine (T5–T8)
The mean pedicle widths of the middle thoracic spine were 4.7 mm (range 1.3–9.9 mm) on the concave side and 5 mm (range 1.3–9.4 mm) on the convex side for the outer diameter and 2.1 mm (range 0–6.2 mm) on the concave side and 2.3 mm (range 0–7.4 mm) on the convex side for the inner diameter. The mean pedicle heights of the middle thoracic spine were 8.3 mm (range 4.2–14.5 mm) on the concave side and 9 mm (range 2.8–14 mm) on the convex side for the outer diameter and 4.3 mm (range 0–9.9 mm) on the concave side and 5.0 mm (range 0–9.7 mm) on the convex side for the inner diameter.
The difference between the concave and convex side was significant for the outer pedicle width and for the inner pedicle height only in T7.
Lower thoracic spine (T9–T12)
The mean pedicle widths of the lower thoracic spine were 6.3 mm (range 1.4–12.6 mm) on the concave side and 6.8 mm (range 0.1–13.5 mm) on the convex side for the outer diameter and 3.3 mm (range 0–9.5 mm) on the concave side and 3.6 mm (range 0–10.7 mm) on the convex side for the inner diameter. The mean pedicle heights in the lower thoracic spine were 10.3 mm (range 3.2–16.4 mm) on the concave side and 11.3 mm (range 0–16.3 mm) on the convex side for the outer diameter and 6.3 mm (range 0–12.5 mm) on the concave side and 7.4 mm (range 0–13.2 mm) on the convex side for the inner diameter.
The difference between the pedicle width of the concave and convex side was not significant in these levels. The concave-sided pedicle height in T9 was significantly smaller than the convex-sided in T9 and the concave-sided length in T10 was significantly smaller than the convex-sided in T10.
Lumbar spine (L1–L5)
The mean pedicle widths of the lumbar spine were 9.0 mm (range 2.4–18.4 mm) on the concave side and 8.8 mm (range 2.5–20.1 mm) on the convex side for the outer diameter and 5.4 mm (range 0–14.4 mm) on the concave side and 5.2 mm (range 0–15.8 mm) on the convex side for the inner diameter. The mean pedicle heights of the lumbar spine were 11.1 mm (range 6.1–20.2 mm) on the concave side and 11.1 mm (range 4.1–16.7 mm) on the convex side for the outer diameter and 6.5 mm (range 0–17.9 mm) on the concave side and 6.7 mm (range 0–12.6 mm) on the convex side for the inner diameter (Table 8).
Table 8.
List of abbreviations
| PWO left | Pedicle width outer diameter left |
| PWI left | Pedicle width inner diameter left |
| PWO right | Pedicle width outer diameter right |
| PWI right | Pedicle width inner diameter right |
| PL left | Pedicle length left |
| PL right | Pedicle length right |
| PHO left | Pedicle height outer diameter left |
| PHI left | Pedicle height inner diameter left |
| PHO right | Pedicle height outer diameter right |
| PHI right | Pedicle height inner diameter right |
Intra- and interrater reliability
The IRR of observer 1 was strong (>0.6) in six parameters and moderate (0.4–0.6) in four of ten parameters. Among the four parameters with moderate correlation, there was the pedicle length, which is not relevant for choosing the diameter of the pedicle screws.
Similar to observer 1 the IRR of observer 2 was strong (>0.6) in six parameters and moderate (0.4–0.6) in four of ten parameters. Among the four parameters with moderate correlation, there was the pedicle length (Table 9).
Table 9.
Intra-rater-reliability
| Parameter | Observer 1 | Observer 2 | ||
|---|---|---|---|---|
| IRR | p value | IRR | p value | |
| PWO left | 0.676** | <0.001 | 0.612** | <0.001 |
| PWI left | 0.646** | <0.001 | 0.650** | <0.001 |
| PWO right | 0.655** | <0.001 | 0.631** | <0.001 |
| PWI right | 0.581** | <0.001 | 0.645** | <0.001 |
| PL left | 0.509** | <0.001 | 0.550** | <0.001 |
| PL right | 0.583** | <0.001 | 0.537** | <0.001 |
| PHO left | 0.652** | <0.001 | 0.678** | <0.001 |
| PHI left | 0.593** | <0.001 | 0.570** | <0.001 |
| PHO right | 0.650** | <0.001 | 0.627** | <0.001 |
| PHI right | 0.627** | <0.001 | 0.584** | <0.001 |
The IRR between the two raters was strong in all parameters, but pedicle length, where it was only slight (Table 10).
Table 10.
Inter-rater-reliability
| Parameter | Measurement 1 | Measurement 2 | ||
|---|---|---|---|---|
| IRR | p value | IRR | p value | |
| PWO left | 0.687** | <0.001 | 0.721** | <0.001 |
| PWI left | 0.634** | <0.001 | 0.681** | <0.001 |
| PWO right | 0.679** | <0.001 | 0.682** | <0.001 |
| PWI right | 0.634** | <0.001 | 0.645** | <0.001 |
| PL left | 0.389** | <0.001 | 0.310** | <0.001 |
| PL right | 0.397** | <0.001 | 0.344** | <0.001 |
| PHO left | 0.620** | <0.001 | 0.683** | <0.001 |
| PHI left | 0.607** | <0.001 | 0.632** | <0.001 |
| PHO right | 0.638** | <0.001 | 0.652** | <0.001 |
| PHI right | 0.687** | <0.001 | 0.621** | <0.001 |
Size matching of pedicles with pedicle screws
Pedicles were rated as too small for safe instrumentation, when the outer diameter was smaller than 115% of the smallest available screw (diameter 4.2 mm), which was 3.7 mm.
Some of the pedicles between T4 and L2 revealed to be too small. The highest percentage of size mismatch was found in levels T7 (31%) and T8 (33%) on the concave side and in T8 (31%) on the convex side (Fig. 5).
Fig. 5.
Size matching of pedicles and available screws
Discussion
This study aimed to provide clinically relevant data for spine surgeons regarding the dimensions of thoracic and lumbar pedicles in patients with scoliosis. The high inter- and intraobserver reliability confirmed the high value of this method.
Similar to prior anatomic studies [4], we found a tendency that the concave pedicles were slightly smaller than the convex-sided ones, but this was only statistically significant in some parameters at the levels T9 and T10.
The smallest pedicles were identified in the mid-thoracic region from T5 to T8 with the proximal thoracic pedicles (T1–T3) being slightly larger. The largest thoracic pedicles were found from T9 to T12. The corresponding dimensions for concave, the pedicles were smaller compared to the convex-sided ones. Usually, preoperative planning in scoliosis surgery is done on plain radiographs. But due to the windswept appearance of pedicles in scoliosis the two-dimensional information is not sufficient. As preoperative CT scans are sometimes performed in complex scoliosis cases, in order to detect deformities and to get distinct information on the individual anatomy, pedicle CT measurements can be done in many cases without submitting the patients to additional radiation. Former studies confirmed a good correlation between CT-based and true morphometric measurements of vertebral morphometry in cadavers [1, 3, 10, 11]. For choosing the appropriate screw size, the outer cortical diameter is the most important factor [8, 9]. As studies have shown that screws that are 80% [3] (adults) to 115% [8, 9] (adolescents) of the outer diameter can safely be inserted in the thoracic pedicles, we compared these to the diameter of the smallest available pedicle screw, which has a diameter of 4.2 mm. Our measurements confirmed the experience of spine surgeons that up to one-third of the pedicles in the middle thoracic spine are smaller than the screws and therefore not appropriate for a safe instrumentation. Alternative fixation techniques can be used like extrapedicular placement between the outer cortex of the pedicle and the rib or employment of hooks, sublaminar wires and bands (universal clamps).
We conclude that measuring pedicle diameters on CT scans is a very reliable method, but time-consuming procedure. To assess an X-ray takes just some seconds to decide if a pedicle can be instrumented or not. Measuring a CT scan takes at least 2 min to identify the appropriate level and calculate the given values.
Special software and high resolution screens are necessary. If CT scans are not performed for other questions, the additional high dosage of radiation should be avoided, as patients with scoliosis are known to obtain high cumulative radiation dosages through routine X-ray controls anyway. CT measuring should be reserved for special cases, where the anatomic situation remains unclear despite X-ray.
In most patients, the combination of long cassette ap X-rays and bending films gives a good impression regarding pedicle dimensions. There are, however, patients with very small pedicles on the concave side or in the upper thoracic spine especially in high grade, rigid curves leaving uncertainty, which pedicles may be instrumented. The greater the uncertainty on plain X-rays the more these patients would be candidates for preoperative CT scanning. In our experience, we use preoperative CT scans in most congenital cases and in idiopathic or neuropathic cases with more than 80°.
In screw positioning, the most important factor for avoiding misplacement and size mismatch remains the diligent palpation with the awl and pedicle feeler.
Our results confirm the clinical experience that up to one-third of the pedicles in the middle thoracic spine are not appropriate for a safe intrapedicle screw placement.
Acknowledgments
Conflict of interest None.
References
- 1.Krag M, Weaver D, Beynnon B, Haugh L. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine. 1988;13:27–32. doi: 10.1097/00007632-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Lilijenqvist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine. 2000;25(10):1247–1253. doi: 10.1097/00007632-200005150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Misenhimer GR, Peek RD, Wiltse LL, Rothman SLG, Widell EH. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine. 1989;15:367–372. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien MF, Lenke LG, Mardjetko S, Lowe TG, Kong Y, Eck K, Smith D. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine. 2000;25(18):2285–2293. doi: 10.1097/00007632-200009150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Panjabi MM, O’Holleran JD, Crisco JJ, 3rd, Kothe R. Complexity of the thoracic spine pedicle anatomy. Eur Spine J. 1997;6(1):19–24. doi: 10.1007/BF01676570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parent S, Labelle H, Skalli W, Guise J. Thoracic pedicle morphometry in vertebrae from scoliotic spines. Spine. 2004;29(3):239–248. doi: 10.1097/01.BRS.0000109995.64028.FE. [DOI] [PubMed] [Google Scholar]
- 7.Smith RM, Pool RD, Butt WP, Dickson RA. The transverse plane deformity of structural scoliosis. Spine. 1991;16(9):1126–1129. doi: 10.1097/00007632-199109000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77(8):1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77(8):1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Xiong B, Sevastik B, Sevastik J, Hedlund R, Suliman I, Kristjansson S. Horizontal plane morphometry of normal and scoliotic vertebrae. Eur Spine J. 1995;4:6–10. doi: 10.1007/BF00298410. [DOI] [PubMed] [Google Scholar]
- 11.Xiong B, Sevastik B, Willers U, Sevastik J, Hedlund R. Structural vertebral changes in the horizontal plane in idiopathic scoliosis and the long-term corrective effect of spine instrumentation. Eur Spine J. 1995;4(1):11–14. doi: 10.1007/BF00298411. [DOI] [PubMed] [Google Scholar]