Abstract
Purpose
To compare and evaluate postoperative complications and treatment outcome in mandibular fracture fixation using 2.0 mm titanium miniplates and 3-D locking plates.
Method
Thirty patients were divided randomly into two groups of 15 each (including comminuted and malunited fractures). Group A was treated with open reduction internal fixation using 2.0 mm miniplates and group B with 3-D locking plates.
Results
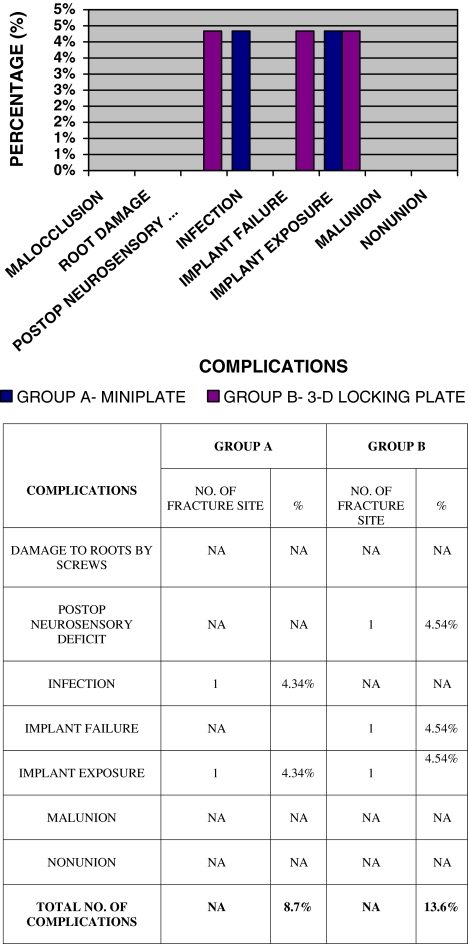
A total of five complications were observed in four patients: implant exposure and infection in miniplate group and postoperative neurosensory deficit, implant failure and implant exposure in 3-D group.
Conclusion
For fractures in symphysis and parasymphysis region, severely displaced angle fractures and for comminuted fractures 3-D locking plate could be a better option. In the angle and body region a single miniplate fixed according to Champy’s technique is easy to place with less surgical time, less surgical trauma, is more economical and has similar clinical results.
Keywords: 3-D locking plate, Mandibular fracture, Miniplates, Malunited
Introduction
Two fundamentally different philosophies have evolved in the treatment of mandibular fracture using plates and screws.
One in which Spiessl [1] believed in rigid fixation sufficient to prevent interfragmentary mobility during active use of the mandible. Large bone plates with bicortical screws were used and primary bone union by compression osteosynthesis was the goal of treatment. Bulky plates, difficult adaptation, stress shielding, scar formation due to extraoral approach, more operating time and increased chances of nerve injury were its disadvantages.
Second in which Champy et al. [2] advocated a modification of Michelet et al.’s (1973) technique [3] of mandibular osteosynthesis, which consists of monocortical juxta-alveolar and subapical osteosynthesis, without compression and without IMF. The plates were placed near the tension zone produced by physiological strain.
Since then, miniplates have been the preferred fixation method in craniomaxillofacial surgery because of their relatively small size, adaptability, ease of placement and intraoral approach [4].
However controversies abound with respect to rigidity and stability provided by miniplates especially in angle fractures and comminuted fractures, as they are considered as semirigid fixation methods by followers of AO/ASIF [5].
Farmand [6] developed 3-D plate with quadrangular design formed by joining two miniplates with interconnecting crossbars. The stability is gained over a defined surface area in three dimensions due to its configuration, not by thickness or length and offers good resistance against torsional forces. Author recommended 1.0 mm thick standard plates in mandibular osteosynthesis.
To overcome the disadvantages of loosening of hardware and need of perfect adaptation of miniplates a new Internal Mini-Locking-System [7] was developed in collaboration with the AO/ASIF-Institute.
Thus, it can be hypothesized that 3-D locking plate can provide better stability and ease of plate adaptation for the open reduction internal fixation (ORIF) of mandibular fractures. Considering this, a study was conducted to compare and evaluate titanium 2.0 mm miniplates and 3-D locking plates in terms of stability, postoperative complications, duration of surgery and treatment outcome for the management of mandibular fractures.
Materials and Methods
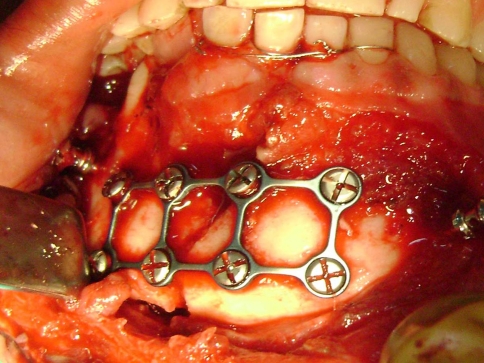
This study was conducted on 30 patients of mandibular fracture including comminuted (Fig. 1) and malunited fractures within the age group of 16–60 years. The patients were divided randomly into two groups of 15 patients each. Group A was treated with ORIF using 2.0 mm titanium miniplates and group B with 3-D locking plates. In our study we have used a modified locking system where the threads in the head of the screw (Fig. 2) are tapered (multidirectional/polyaxial) and there is a bevel within the plate (Fig. 3). On the last turn while seating the screw, the thread in screw head will engage the bevel in the plate (Fig. 4). Because of the tapered design of screw no precise meshing of the screw and plate threads required, this provides freedom to place the screw at up to a 10° angulation from the plane perpendicular to the plate. This plate can be fixed from either side (Fig. 5). This design is similar to the design of tapered locking reconstruction plate described by Colleti et al. [8]. Postoperative intermaxillary fixation was avoided and done only if required or when occlusion was deranged.
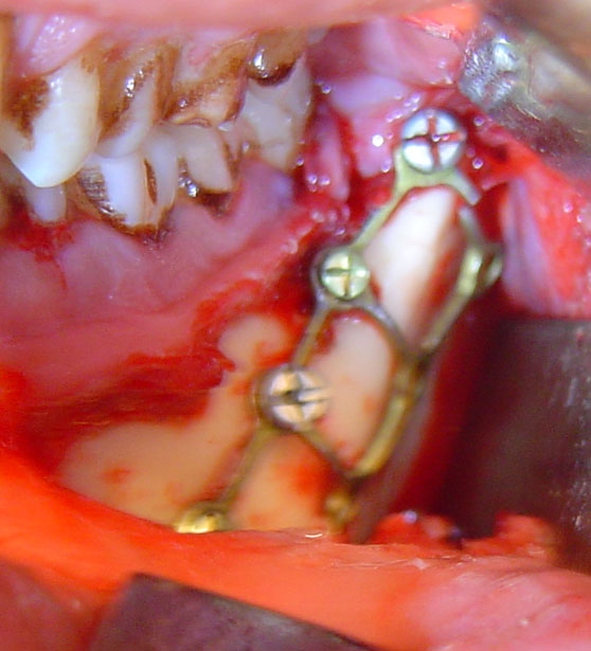
Fig. 1.
3-D plate secured at the fracture site
Fig. 2.
2.0 mm locking screw
Fig. 3.

Bevel in the plate to engage the thread in the screw head
Fig. 4.

On the last turn while seating the screw, the thread in screw head will engage the bevel in the plate
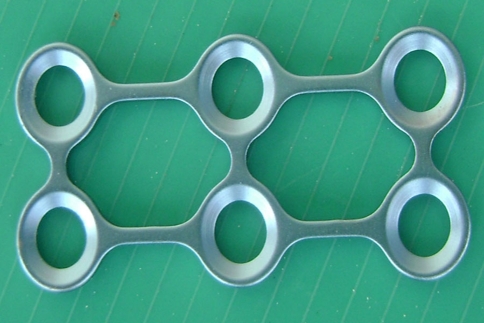
Fig. 5.
3-D (2.0 mm titanium) locking plate
Following parameters were evaluated: (1) need for postoperative Inter Maxillary Fixation; (2) mobility across fracture segments at 3rd, 15th, and 30th postoperative days; (3) biting efficiency was considered normal if patient was able to chew normal diet after 10 days of operation; (4) implant failure (loosening of screws, breakage of plate); (5) vertical displacement (continuity of inferior border or inferior alveolar canal was checked radiographically) and (6) duration of surgery.
Following postoperative complications were evaluated; malocclusion, damage to roots by screws, post operative neurosensory deficit, infection at the site, implant failure, implant palpability, nonunion and malunion.
Results
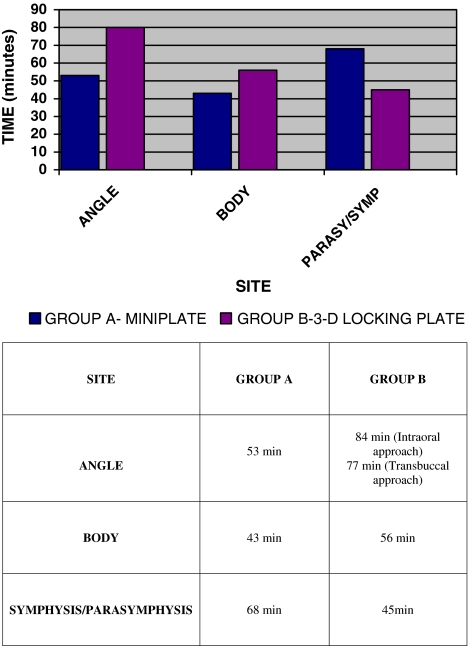
Total five complications (11.1%) were observed in 45 fracture sites. Duration of surgery was measured from the time incision was placed till the closure of wound. Fixation with 3-D plate took average 27 min extra compared to intraoral fixation of titanium miniplates in the angle region. In the body region the difference was not significant with average time 13 min more taken by 3-D plates. Whereas in symphysis and parasymphysis region 23 min less than titanium miniplates. The average operating time for the 3-D locking system was 5.6 min longer than the miniplates.
Discussion
Incidence of mandible fracture was 90% in males and the age group commonly affected was 21–30 years (60%). The principle cause of mandible fracture was road traffic accident (56.7%). The most common site was angle (46.7%), followed by body (31.1%) and parasymphysis (20%).
There was statistically no significant difference in terms of complications in both the groups (Fig. 6). In one patient the vertical strut of 3-D plate broke intraoperatively (Fig. 7) because plate was bent repeatedly to adapt it precisely according to the contour of angle. Healing occurred without infection and also there was no gap and displacement on postoperative radiographs and no mobility at the fracture site. The same patient showed implant exposure on 3 month postoperative evaluation. Incidence of postoperative neurosensory deficit (6.7%) in this study was in agreement with the reported incidence of postoperative nerve damage (8.1%) by Guimond et al. [9]. Their study was on angle fractures and according to them the postoperative neurosensory deficit was due to the large number and broad placement configuration of the screws of the 3-D plates and was transient. In our study only one patient developed neurosensory deficit out of six patients in whom we had bent the 3-D plates to preserve mental nerve. The probable region for this deficit might be inadvertent traction of nerve during the intraoperative manipulation of fracture fragments (bilateral fracture involving angle and body) for reduction rather than the broad configuration of 3-D plate.
Fig. 6.
Fractured plate due to overbending
Fig. 7.
3-D plate secured at angle region (fracture of vertical strut)
One case of infection (4.5%) in angle region of mandible was seen in the group A treated by miniplate after 1 month. In this case the fracture line was passing distal to third molar through the lamina dura and patient had poor oral hygiene. The site healed by conservative management.
In one case titanium miniplate got exposed 6 month postoperatively in the angle region. Since the fracture had healed uneventfully so the plate was removed under local anaesthesia.
Because of more number of screws (6/8 hole) and broad size of plate, fixation of 3-D plates in angle region took more time (Fig 8). Intraoral placement of six hole 3-D plate was more cumbersome and 8 hole plate placement required transbuccal approach. In the body region the difference was not significant. Whereas in symphysis and parasymphysis region fixation of 3-D plates took less time. The average operating time for the 3-D locking system was 5 min 6 s longer than the miniplates.
Fig. 8.
Duration of surgery
Functional occlusion was restored in all the cases. Minor occlusal discrepancies seen in two patients were managed by selective occlusal adjustments. In one case of comminuted fracture the intraoperative intermaxillary fixation was left as such for 24 h, to check the reduction in immediate postoperative radiograph before releasing inter maxillary fixation. No mobility across the fracture site was found on 3rd, 15th and 30th postoperative days. One patient complained of inability to chew normal diet in 3-D group probably because of pain due to injury to the mucosa by the broken strut. In one patient with titanium miniplate, 3 months postoperative radiograph showed change in alignment of fracture fragments when compared to immediate postoperative radiograph. But the number is not significant enough to comment on stability of titanium miniplates. The evaluation of above clinical parameters showed no statistically significant difference in both the groups in terms of stability. However, the patients in our study were divided randomly and the number of patients with severe displacement (>5 mm) were more in 3-D locking group compared to miniplate group. The use of single 3-D plate in cases of comminuted and severely displaced fractures with considerable gap (malunited fractures) where more than the usual number of miniplates for that site is required shows that 3-D locking plates are biomechanically more stable than the miniplates.
The theoretical advantages (Collins et al. [10]) of locking system developed for miniplates are; less screw loosening, greater stability across fracture site, less precision required in plate adaptation and less alteration in occlusal or osseous relationship upon screw tightening. In our study no case of screw loosening was observed. We didn’t adapted 3-D plates before fixation, despite that it provided sufficient stability for fracture healing. The intraoperative reduction of fracture fragments was done manually, which has more chances of producing displacement, but no case showed alteration in alignment/occlusal relationship upon screw tightening.
Because of the conflicting articles published in literature it’s still not clear that this increased biomechanical stability is due to the design of plate or due to the locking mechanism. Collins et al. [10] found no statistically significant difference in clinical outcome using 2.0 mm locking and 2.0 mm standard plates. Ellis and Graham [11] reported 15% complication rate with 2.0 mm locking plates, out of which 50% were major (malocclusion and nonunion). Increased vertical displacement (Wittenberg et al. [12]) and infection rates of 8.2, 5.5 and 6.6% have been shown by Bui et al. [13] and Guimond et al. [9] at angle and by Parmar et al. [14] on mandible using 3-D plates. However, in our study only three complications were observed with 3-D locking group; First was implant breakage as we were using this system for the first time we repeatedly bent it to adapt it according to the contour of angle region, the second complication was the exposure of above plate probably because of continuous trauma to mucosa by the broken strut, and thirdly postoperative neurosensory deficit due to inadvertent stretching of nerve during reduction. So, these three complications can’t be related to the implant material or design. If we exclude them then there was no complication in 3-D locking group. Thus it can be assumed that the combined properties of locking system and 3-D design are responsible for good results and favorable biomechanical behavior (even in the presence of comminuted and severely displaced fractures) observed in our study.
Conclusion
There is no major difference in terms of treatment outcome and both the systems are equally effective in mandibular fracture treatment and provided sufficient rigidity often avoiding/decreasing the need for inter maxillary fixation.
In cases of comminuted and severely displaced fractures with considerable gap (malunited fractures) the precise adaptation and placement of each miniplate becomes more difficult and time consuming whereas 3-D locking plate is easier and quicker to place, is less expensive and has more favourable biomechanical behavior. The number of patients with such fractures was small in our study therefore studies with larger sample size are necessary to corroborate the above observations and evaluate the effectiveness of 3-D locking plates in comminuted and malunited fractures.
Precise adaptation of 3-D locking plates is not required and does not affect their mechanical behavior. Therefore plate placement becomes easier and less time consuming.
In the mental nerve region we can bend the plate over the nerve so that it can lie in the concavity and thus we can prevent nerve injury due to pressure of plate without altering the ideal line of osteosynthesis.
For fractures in symphysis and parasymphysis region, severely displaced angle fractures and for comminuted fractures 3-D locking plate could be a better option compared to miniplates.
The placement of 6 or 8 hole 3-D plate in angle often requires percutaneous approach, is more time taking and clinically not much is gained. In the angle and body region a single miniplate fixed according to Champy’s technique is easy to place with less surgical time, less surgical trauma, is more economical and has similar clinical results.
Contributor Information
Manoj Goyal, Email: drmanojgoyal@rediffmail.com.
Richa Pandey, Email: richaomfs2006@rediffmail.com.
References
- 1.Spiessl B. Rigid internal fixation of fractures of lower jaw. Reconstr Surg Traumtol. 1972;13:124–140. [PubMed] [Google Scholar]
- 2.Champy M, Lodde JP, Schmitt R, et al. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978;6:14–21. doi: 10.1016/S0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 3.Michelet FX, Deymes J, Dessus B. Osteosynthesis with miniaturized screwed plates in maxillofacial surgery. J Maxillofac Surg. 1973;1(2):79–84. doi: 10.1016/S0301-0503(73)80017-7. [DOI] [PubMed] [Google Scholar]
- 4.Cawood JL. Small plate osteosynthesis of mandibular fractures. Br J Oral Maxillofac Surg. 1985;23:77–91. doi: 10.1016/0266-4356(85)90057-9. [DOI] [PubMed] [Google Scholar]
- 5.Kroon HM, Mathison M, Cordey JR, Rahn BR. The use of miniplates in mandibular fractures. J Craniomaxillofac Surg. 1991;19:199. doi: 10.1016/s1010-5182(05)80547-5. [DOI] [PubMed] [Google Scholar]
- 6.Farmand M (1995) Three-dimensional plate fixation of fractures and osteotomies. Facial Plast Surg Clin North Am 3(1):39–56
- 7.Gutwald R, Alpert B, Schmelzeisen R. Principle & stability of locking plates. Keio J Med. 2003;52:21. doi: 10.2302/kjm.52.21. [DOI] [PubMed] [Google Scholar]
- 8.Coletti DP, Caccamese JF, Norby C, et al. Comparative analysis of the threaded & tapered locking reconstruction plates. J Oral Maxillofac Surg. 2007;65:2587. doi: 10.1016/j.joms.2006.05.054. [DOI] [PubMed] [Google Scholar]
- 9.Guimond C, Johnson J, Marchena J. Fixation of mandibular angle fractures with a 2.0 mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg. 2005;63:209. doi: 10.1016/j.joms.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Collins CP, Leonard GP, Tolas A, et al. A prospective randomized clinical trial comparing 2.0 mm locking plates to 2.0 mm standard plates in treatment of mandible fractures. J Oral Maxillofac Surg. 2004;62:1392. doi: 10.1016/j.joms.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 11.Ellis E, Graham J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642. doi: 10.1053/joms.2002.33110. [DOI] [PubMed] [Google Scholar]
- 12.Wittenberg JM, Mukherjee DP, Smith BR, Kruse RN. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg. 1997;26:68–73. doi: 10.1016/S0901-5027(97)80852-1. [DOI] [PubMed] [Google Scholar]
- 13.Bui P, Demian N, Beetar P. Infection rate in mandibular angle fractures treated with a 2.0 mm 8-hole curved strut plate. J Oral Maxillofac Surg. 2009;67:804–808. doi: 10.1016/j.joms.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 14.Parmar S, Menat S, Raghani M, Kapadia T. Three dimensional miniplate rigid fixation in fracture mandible. J Maxillofac Oral Surg. 2007;6(2):14. [Google Scholar]