Abstract
Objective:
To qualitatively and quantitatively assess the association of prehypertension with incident stroke through a meta-analysis of prospective cohort studies.
Methods:
We searched Medline, Embase, the Cochrane Library, and bibliographies of retrieved articles. Prospective cohort studies were included if they reported multivariate-adjusted relative risks (RRs) and corresponding 95%confidence intervals (CI) of stroke with respect to baseline prehypertension.
Results:
Twelve studies with 518,520 participants were included. Prehypertension was associated with risk of stroke (RR 1.55, 95% CI 1.35–1.79; p < 0.001). Seven studies further distinguished a low prehypertensive population (systolic blood pressure [SBP] 120–129 mm Hg or diastolic blood pressure [DBP] 80–84 mm Hg) and a high prehypertensive population (SBP 130–139 mm Hg or DBP 85–89 mm Hg). Among persons with lower-range prehypertension, stroke risk was not significantly increased (RR 1.22, 0.95–1.57). However, for persons with higher values within the prehypertensive range, stroke risk was substantially increased (RR 1.79, 95% CI 1.49–2.16).
Conclusions:
Prehypertension is associated with a higher risk of incident stroke. This risk is largely driven by higher values within the prehypertensive range and is especially relevant in nonelderly persons. Randomized trials to evaluate the efficacy of blood pressure reduction in persons with this designation are warranted.
In recognition of the profound impact of elevated blood pressure on cardiovascular risk, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) proposed a new category of individuals within the range of normal blood pressure at risk for developing hypertension and its untoward sequela.1 This new designation, called prehypertension, comprises persons with systolic blood pressure between 120 and 139 mm Hg or diastolic blood pressure between 80 and 89 mm Hg.1 Since the JNC 7 proposal, epidemiologic studies have shown that the prevalence of prehypertension among adults in the general population is roughly 31% in the United States.2 However, the rationale and relevance of diagnosing prehypertension in otherwise healthy patients have recently been called into question.3 Indeed, even though stroke is the condition most highly correlated with blood pressure among various vascular disease entities,4 the association of prehypertension with stroke risk in published studies has been inconsistent.
Given its high prevalence and potential to identify persons at great stroke risk who may benefit from risk reduction strategies, we undertook a meta-analysis of prospective cohort studies to qualitatively and quantitatively assess the association of baseline prehypertension and risk of incident stroke.
METHODS
Literature search.
The search was conducted according to the recommendations of the Meta-analysis of Observational Studies in Epidemiology Group.5 We performed a systematic search of PubMed (1966–August 2010), Embase (1947–August 2010), and the Cochrane Library using the following search strategy: “prehypertension” or “prehypertensive” and “stroke,” “cerebrovascular disease,” “cerebrovascular attack,” “cerebral infarct,” “intracranial hemorrhage,” “cardiovascular disease,” “myocardial ischemia,” “myocardial infarct,” “ischemic heart disease,” “coronary heart disease,” or “angina.” We restricted the search to human studies. There were no language restrictions. Further information was retrieved through a manual search of references from recent reviews and relevant published original studies.
Inclusion and exclusion criteria.
Studies were selected if they met the following entry criteria: 1) prospective cohort studies; 2) blood pressure evaluated at baseline; 3) assessment of incident stroke; 4) follow-up duration of at least 1 year; 5) reported quantitative estimates of the multivariate-adjusted relative risk and 95% confidence interval (CI) for stroke associated with prehypertension (systolic blood pressure 120–139 mm Hg or diastolic blood pressure 80–89 mm Hg) vs reference (systolic blood pressure <120 mm Hg and diastolic blood pressure <80 mm Hg). Studies were excluded if 1) the study design was cross-sectional, case-control, or retrospective cohort, 2) only unadjusted or age- and sex-adjusted relative risk was reported; 3) 95% CI was not reported; 4) they were duplicated studies, and 5) data were derived from secondary analysis of antihypertensive clinical trials. Studies that only reported estimates with a low range of prehypertension (systolic blood pressure 120–129 mm Hg or diastolic blood pressure 80–84 mm Hg) and a high range of prehypertension (systolic blood pressure 130–139 mm Hg or diastolic blood pressure 85–89 mm Hg) separately were included.
Data extraction.
Data from eligible studies were abstracted independently by 2 investigators (M.L. and B.C.). Discrepancies were resolved by discussion with a third investigator (B.O.) and by referencing the original report. Relevant data included the first author's name, year of publication, country of origin, number of participants, participants' age, duration of follow-up, number of events, outcome assessment, prevalence of prehypertension, multivariate-adjusted relative risks or hazard ratios of stroke and corresponding 95% CI, population-attributable risk for the association of stroke with prehypertension, and covariates adjusted in the statistical analysis.
Assessment of study quality.
We assessed the quality of all articles that met the selection criteria. Quality assessment was based on guidelines developed by the US Preventive Task Force as well as the modified checklist used in previous studies.6–8 We assessed the following 8 characteristics: 1) prospective study design; 2) maintenance of comparable groups; 3) adequate adjustment of potential confounders (i.e., at least 5 of 6 factors: age, sex, diabetes mellitus, body mass index or other measure of overweight/obesity, cholesterol, and smoking); 4) documented loss to follow-up rate; 5) outcome assessed blind to baseline status; 6) clear definition of exposures (prehypertension) and outcomes (stroke); 7) temporality (blood pressure measured at baseline, not at time of outcomes assessment); and 8) follow-up of at least 2 years. Studies were graded as good quality if they met 7–8 criteria, fair if they met 4–6 criteria, and poor if they met <4 criteria.
Statistical analysis.
Data analysis used multivariate-adjusted outcome data (expressed as relative risks and 95% CIs). We converted these values in every study by using their natural logarithms, and the SEs were calculated from these logarithmic numbers and their corresponding 95% CIs. The statistical analysis used the inverse variance approach to combine log relative risks and SEs. We used a random-effects model and explored for sources of inconsistency (I2) and heterogeneity. A fixed-effects model was also used for the comparison to the random-effects model on the overall risk estimate. All reported p values were 2-sided with significance set at <0.05. Heterogeneity was assessed by p value of χ2 statistics and I2, which describes the percentage of variability in the effect estimates that is due to heterogeneity rather than to chance.9,10 We regarded I2 of less than 40% as “heterogeneity might not be important” and of more than 75% as “considerable heterogeneity” based on the suggestion of Cochrane Handbook for Systematic Review of Interventions.
The leading outcome of interest was relative risk of incident stroke in prehypertension. The secondary outcomes of interest were relative risks of incident stroke in low-range prehypertension and high-range prehypertension, respectively. Subgroup analyses for prehypertension were conducted according to average participant's age (<65 years vs ≥65 years), sex (men vs women), race-ethnicity (Asians vs non-Asians), follow-up duration (<10 years vs ≥10 years), endpoints (fatal vs fatal plus nonfatal stroke), stroke type (ischemic vs hemorrhagic), participant number (<10,000 vs ≥10,000), and study quality (good [score 7–8] vs fair [score 4–6]).
Finally, we did a sensitivity analysis to further explore the robustness of our results. To identify any study that may have exerted a disproportionate influence on the overall result, we removed each individual study from the meta-analysis one at a time. A funnel plot based on the primary outcome was conducted to evaluate potential systematic bias in studies, including publication bias. The Cochrane Collaboration Review Manager Software Package (RevMan 5) was used for the meta-analysis of observational studies.7,11
Standard protocol approvals, registrations, and patient consents.
Because this was an analysis based on data obtained from a search of publicly available/accessible published scientific literature, formal review by the institutional review board at our institution was not required.
RESULTS
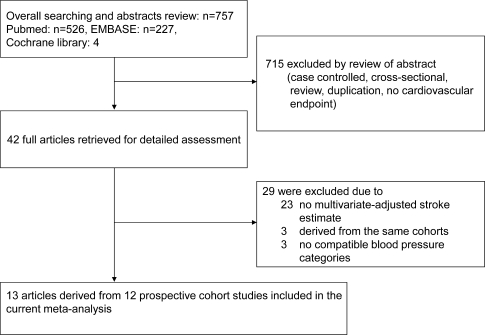
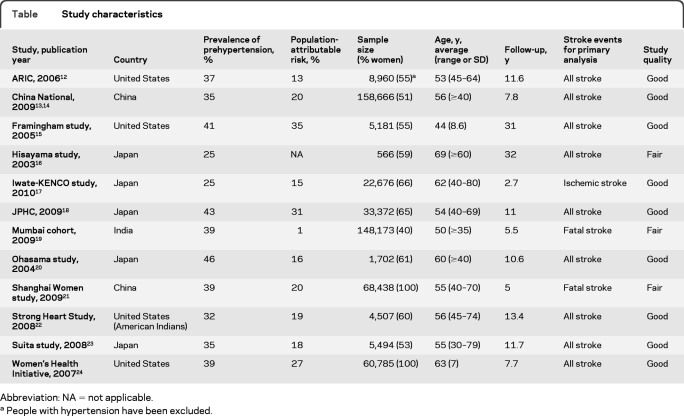
The literature review identified 42 full articles for detailed assessment, among which 23 were excluded because of the lack of a multivariate-adjusted stroke estimate, 3 because they were duplicated studies, and 3 because of no compatible blood pressure categories. Our final primary analysis included 13 articles derived from 12 prospective cohort studies (figure 1).12–24 The table shows the characteristics of the studies included, with 518,520 participants. All studies were derived from the general population. Among the 12 studies, 4 were from the United States,12,15,22,24 5 were from Japan,16–18,20,23 2 were from China,13,21 and 1 was from India.19 The prevalence of prehypertension ranged from 25%16,17 to 46%.20 In primary analysis, 9 studies reported fatal plus nonfatal stroke as an endpoint,12,13,15–18,20,23,24 2 reported fatal stroke,19,21 and 1 reported ischemic stroke.17 Sample size ranged from 1,70220 to 158,666.13 Follow-up duration ranged from 2.7 years17 to 32 years.16 Population-attributable risk for the association of stroke with prehypertension was about 19% (median value of included studies). Two studies enrolled women only,21,24 whereas the others enrolled both men and women. On a scale of 8, the overall quality of studies was good (median score 7, range 5–8).
Figure 1. Study selection.
Table.
Study characteristics
Abbreviation: NA = not applicable.
People with hypertension have been excluded.
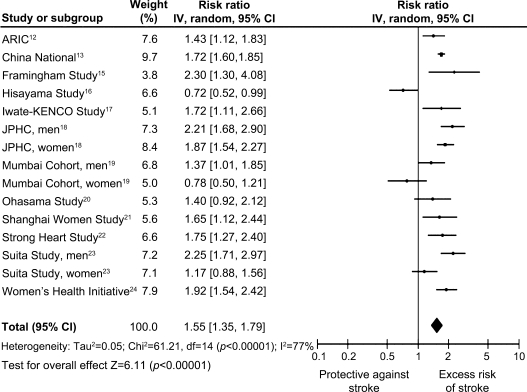
Overall, the presence of prehypertension was associated with greater incident stroke risk after adjustment for established cardiovascular risk factors (figure 2). There was evidence of heterogeneity in the magnitude of the association across studies (p for heterogeneity <0.001, I2 = 77%), but no major asymmetric appearance in the funnel plot (figure e-1 on the Neurology® Web site at www.neurology.org). The exclusion of any single study from the analysis did not alter the overall finding in a sensitivity test. The relative risk from a fixed-effect model was 1.66 (95% CI 1.57–1.75; p < 0.001).
Figure 2. Prehypertension and stroke risk.
Association of prehypertension (systolic blood pressure 120–139 mm Hg or diastolic blood pressure 80–89 mm Hg) and stroke risk in prospective cohort studies. CI = confidence interval; IV = inverse variance.
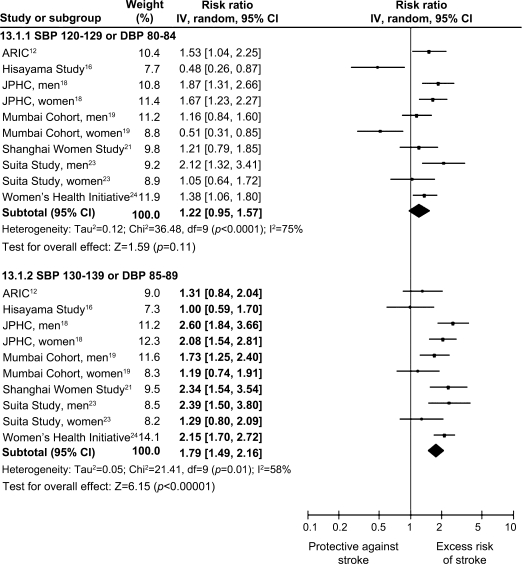
Seven studies further distinguished low-range prehypertensive populations and high-range prehypertensive populations. Among low-range prehypertensive populations, incident stroke risk was not significantly increased, but for higher values within the prehypertensive range, stroke risk was substantially increased (figure 3). Only one study compared the effects of systolic vs diastolic prehypertension in the higher range: systolic blood pressure 130–139 mm Hg vs diastolic blood pressure 85–89 mm Hg vs systolic blood pressure 130–139 mm Hg or diastolic blood pressure 85–89 mm Hg and did not find any differences in incident stroke risk (2.31 [95% CI 1.39–3.82] vs 2.55 [1.42–4.56] vs 2.34 [1.32–4.12], respectively).21
Figure 3. Low and high range of prehypertension vs stroke risk.
Association of prehypertension subsets, low range of prehypertension (systolic blood pressure [SBP] 120–129 mm Hg or diastolic blood pressure [DBP] 80–84 mm Hg), and high range of prehypertension (SBP 130–139 mm Hg or DBP 85–89 mm Hg) and stroke risk in prospective cohort studies. CI = confidence interval; IV = inverse variance.
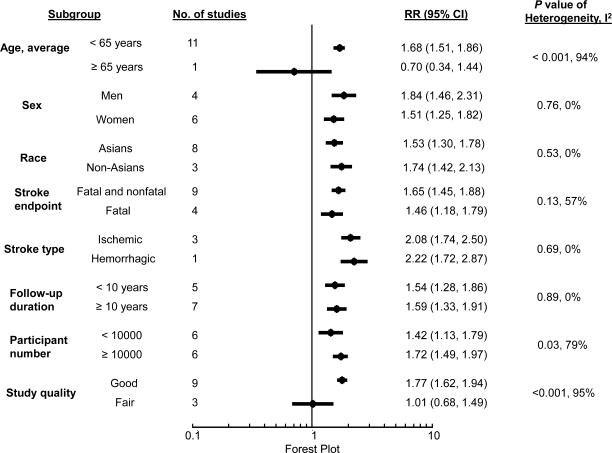
In subgroup analyses, prehypertension significantly predicted higher stroke risk across sex (men vs women), race-ethnicity (Asians vs non-Asians), stroke endpoint (fatal vs all stroke), stroke subtypes (ischemic vs hemorrhagic stroke), and follow-up duration (<10 years vs ≥10 years) (figure 4). However, significant heterogeneity existed between estimates among participants with different average age at entry (<65 years vs ≥65 years), sample size of studies (<10,000 vs ≥10,000), and study quality (good vs fair). There was no heterogeneity within good-quality studies (p = 0.19, I2 = 23%).
Figure 4. Subgroup analyses according to patient characteristics.
Influence of other patient characteristics on relation between prehyptertension and stroke risk in prospective cohort studies. CI = confidence interval; RR = relative risk.
DISCUSSION
We found that persons with a baseline presence of prehypertension had a robust and significant risk of future stroke that was consistent across diverse race-ethnicities. The size of the studies included and restriction to only prospective cohort studies strengthened the robustness of our findings, because selection bias, recall bias, and reverse causality were unlikely. In addition, all studies included in our meta-analysis reported a multivariate adjusted relative risk, which probably mitigated the possibility of known confounders influencing our results.
Importantly, we observed that incident stroke risk appeared more strongly driven by higher systolic blood pressure or diastolic blood pressure values within the prehypertensive range. However, at this time, it is not clear how best to avert stroke risk in these patients. According to JNC 7, such persons should receive urgent lifestyle modification,1 but there is no robust evidence indicating that such a strategy will actually prevent stroke occurrence. It has been shown that treatment of the higher range of prehypertension with pharmacotherapy is well tolerated and reduces the incidence of frank hypertension,25 but again the impact of this strategy on hard vascular outcomes is unknown. Although evidence showing a major benefit of pharmacologic intervention in prehypertension is currently lacking, it may not be unreasonable to strongly recommend nonpharmacologic approaches with minimal side effects, such as salt reduction, for these patients.26 Moreover, at an individual level, the combination of excessive caloric intake, lack of physical activity, and genetic susceptibility has resulted in a dramatic increase in the prevalence of obesity worldwide,27 which is one of the most important causes for the increase in the incidence of hypertension and prehypertension. Accordingly, it seems important to introduce lifestyle modifications to control the increase in central obesity in the primary prevention of hypertension and prehypertension at the level of the overall population.28
An immediate potential implication of our findings is that young and middle-aged persons with higher systolic or diastolic blood pressure values within the prehypertensive range may benefit from relatively safe, nonpharmacologic blood pressure–lowering methods, such as reduction in salt intake and weight to reduce their risk of stroke. Nonetheless, randomized controlled trials evaluating the effect/efficacy of blood pressure reduction on reducing subsequent risk for stroke are warranted. As such, a potential implication of our study is that a focus on nonelderly individuals with higher blood pressure values within the prehypertensive range should be considered for future randomized controlled trials.
Our subgroup analysis showed that elderly persons with prehypertension did not have a higher risk of incident stroke.16 This finding may not be that surprising, given the immense impact of elderly status itself on stroke risk,4 as well as observational data indicating that the contribution of frank hypertension to the risk of stroke is rather diminished in elderly cohorts.29,30 Obvious heterogeneity was also found among studies with good vs fair quality. There was no heterogeneity within good-quality studies, but there was significant heterogeneity within fair-quality studies. The precise reason for the positive link between prehypertension and stroke risk in good-quality but not fair-quality studies is not immediately clear. It is conceivable that there may have been inherent validity concerns in the fair-quality studies. For instance, one study of fair quality noted that the cause-of-death registries, from which stroke endpoints were derived, were sometimes inaccurate, and this may have affected the precision of the stroke estimate.19
Our study has several limitations. First, baseline blood pressure in most of studies included was obtained by a single-day measurement, which may lead to a misclassification of blood pressure levels and a dilution bias.31 However, previous epidemiologic evidence has suggested that blood pressure measurements taken on a single day may be adequate.32 A single-day measurement also is insufficient to characterize blood pressure variability. Recent studies have suggested that blood pressure variability may be an important determinant of stroke, independent of mean arterial pressure.33 Data on blood pressure variability were not available from the cohort studies we analyzed. Second, meta-analyses can be biased when the literature search fails to identify all relevant studies or the selection criteria for including a study are applied in a subjective manner. To minimize these risks, we performed thorough searches across multiple databases and used explicit criteria for study selection, data abstraction, and data analysis. Third, substantial heterogeneity was observed in the studies included. To explore the potential heterogeneity, we did subgroup analyses to identify plausible biologic and selection sources of the variation. When we restricted our analysis to good-quality studies, the impact of baseline prehypertension on stroke risk was even larger, and there was no obvious heterogeneity between these good-quality studies. Despite these limitations, the results of this systematic review probably represent the most precise and accurate estimate of the strength of the relation between prehypertension and incident stroke currently available.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Yueh Lee, MSc, for article retrieval.
GLOSSARY
- CI
confidence interval
- JNC 7
Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
Footnotes
Editorial, page 1322
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
M.L., J.L.S., and B.O. conceived the study. M.L. and B.O. designed the inclusion and exclusion criteria. M.L., B.C., and K.-H.C. participated in the study search and data collection and extraction. M.L. did the statistical analysis with guidance from J.L.S. and B.O., M.L. wrote the first draft of the report, and J.L.S., Q.H., and B.O. did the major revision and made comments. All other authors commented on the draft and approved the final version. M.L. and B.O. had full access to all the data and had the final decision to submit for publication.
DISCLOSURE
Dr. Lee has received research support from Chang Gung Memorial Hospital, Taiwan (CMRPG 660311, Taiwan). Dr. Saver has served/serves on scientific advisory boards for CoAxia, Inc., Concentric Medical, Talecris Biotherapeutics, Grupo Ferrer Internacional SA, AGA Medical Corporation, BrainsGate, PhotoThera, ev3 Inc., and SYGNIS; serves on the editorial boards of Stroke, Reviews in Neurologic Disease, the Journal of Neuroimaging, and the Journal of Stroke and Cerebrovascular Diseases; has received speaker honoraria from Grupo Ferrer Internacional SA; and receives research support from the NIH/NINDS and the American Heart Association. B. Chang, Dr. Chang, and Dr. Hao report no disclosures. Dr. Ovbiagele serves as an Assistant Editor of Stroke, as an Associate Editor of BMC Public Health, and on the editorial boards of the Journal of Stroke and Cerebrovascular Diseases and Stroke Research and Treatment.
REFERENCES
- 1. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 2. Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new Joint National Committee guidelines: new challenges of the old problem. Arch Intern Med 2004;164:2126–2134 [DOI] [PubMed] [Google Scholar]
- 3. Moynihan R. Who benefits from treating prehypertension? BMJ 2010;341:c4442. [DOI] [PubMed] [Google Scholar]
- 4. Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics: 2010 update: a report from the American Heart Association. Circulation 2010;121:e46–e215 [DOI] [PubMed] [Google Scholar]
- 5. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–2012 [DOI] [PubMed] [Google Scholar]
- 6. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 2001;20:21–35 [DOI] [PubMed] [Google Scholar]
- 7. Lee M, Saver JL, Chang KC, Liao HW, Chang SC, Ovbiagele B. Low glomerular filtration rate and risk of stroke: a meta-analysis. BMJ 2010;341:c4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee M, Saver JL, Chang KH, Liao HW, Chang SC, Ovbiagele B. Impact of microalbuminuria on incident stroke: a meta-analysis. Stroke 2010;41:2625–2631 [DOI] [PubMed] [Google Scholar]
- 9. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–1558 [DOI] [PubMed] [Google Scholar]
- 11. Lee M, Saver JL, Huang WH, Chow J, Chang KC, Ovbiagele B. Impact of elevated cystatin C level on cardiovascular disease risk in predominantly high cardiovascular risk populations: a meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:675–683 [DOI] [PubMed] [Google Scholar]
- 12. Kshirsagar AV, Carpenter M, Bang H, Wyatt SB, Colindres RE. Blood pressure usually considered normal is associated with an elevated risk of cardiovascular disease. Am J Med 2006;119:133–141 [DOI] [PubMed] [Google Scholar]
- 13. Gu D, Chen J, Wu X, et al. Prehypertension and risk of cardiovascular disease in Chinese adults. J Hypertens 2009;27:721–729 [DOI] [PubMed] [Google Scholar]
- 14. He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009;374:1765–1772 [DOI] [PubMed] [Google Scholar]
- 15. Qureshi AI, Suri MF, Kirmani JF, Divani AA, Mohammad Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke 2005;36:1859–1863 [DOI] [PubMed] [Google Scholar]
- 16. Arima H, Tanizaki Y, Kiyohara Y, et al. Validity of the JNC VI recommendations for the management of hypertension in a general population of Japanese elderly: the Hisayama study. Arch Intern Med 2003;163:361–366 [DOI] [PubMed] [Google Scholar]
- 17. Tanaka F, Makita S, Onoda T, et al. Prehypertension subtype with elevated C-reactive protein: risk of ischemic stroke in a general Japanese population. Am J Hypertens 2010;23:1108–1113 [DOI] [PubMed] [Google Scholar]
- 18. Ikeda A, Iso H, Yamagishi K, Inoue M, Tsugane S. Blood pressure and the risk of stroke, cardiovascular disease, and all-cause mortality among Japanese: the JPHC Study. Am J Hypertens 2009;22:273–280 [DOI] [PubMed] [Google Scholar]
- 19. Pednekar MS, Gupta R, Gupta PC. Association of blood pressure and cardiovascular mortality in India: Mumbai cohort study. Am J Hypertens 2009;22:1076–1084 [DOI] [PubMed] [Google Scholar]
- 20. Asayama K, Ohkubo T, Kikuya M, et al. Prediction of stroke by self-measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the Joint National Committee 7 classification: the Ohasama study. Stroke 2004;35:2356–2361 [DOI] [PubMed] [Google Scholar]
- 21. Dorjgochoo T, Shu XO, Zhang X, et al. Relation of blood pressure components and categories and all-cause, stroke and coronary heart disease mortality in urban Chinese women: a population-based prospective study. J Hypertens 2009;27:468–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhang Y, Galloway JM, Welty TK, et al. Incidence and risk factors for stroke in American Indians: the Strong Heart Study. Circulation 2008;118:1577–1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kokubo Y, Kamide K, Okamura T, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: the Suita study. Hypertension 2008;52:652–659 [DOI] [PubMed] [Google Scholar]
- 24. Hsia J, Margolis KL, Eaton CB, et al. Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation 2007;115:855–860 [DOI] [PubMed] [Google Scholar]
- 25. Julius S, Nesbitt SD, Egan BM, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med 2006;354:1685–1697 [DOI] [PubMed] [Google Scholar]
- 26. Appel LJ, Anderson CA. Compelling evidence for public health action to reduce salt intake. N Engl J Med 2010;362:650–652 [DOI] [PubMed] [Google Scholar]
- 27. Katzmarzyk PT, Mason C. Prevalence of class I, II and III obesity in Canada. CMAJ 2006;174:156–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Markus MR, Stritzke J, Siewert U, et al. Variation in body composition determines long-term blood pressure changes in pre-hypertension: the MONICA/KORA (Monitoring Trends and Determinants on Cardiovascular Diseases/Cooperative Research in the Region of Augsburg) cohort study. J Am Coll Cardiol 2010;56:65–76 [DOI] [PubMed] [Google Scholar]
- 29. Trenkwalder P, Hendricks P, Schoniger R, Rossberg J, Lydtin H, Hense HW. Hypertension as a risk factor for cardiovascular morbidity and mortality in an elderly German population; the prospective STEPHY II study: Starnberg Study on Epidemiology of Parkinsonism and Hypertension in the Elderly. Eur Heart J 1999;20:1752–1756 [DOI] [PubMed] [Google Scholar]
- 30. Casiglia E, Mazza A, Tikhonoff V, et al. Weak effect of hypertension and other classic risk factors in the elderly who have already paid their toll. J Hum Hypertens 2002;16:21–31 [DOI] [PubMed] [Google Scholar]
- 31. MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease: part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990;335:765–774 [DOI] [PubMed] [Google Scholar]
- 32. Markovic N, Olomu IN, Bunker CH, Huston SL, Ukoli FA, Kuller LH. Adequacy of a single visit for classification of hypertensive status in a Nigerian civil servant population. Int J Epidemiol 1994;23:723–729 [DOI] [PubMed] [Google Scholar]
- 33. Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.