The authors suggest that blunt dissection of the upper portion of Calot's space has become the preferred technique for resident training during laparoscopic cholecystectomy.
Keywords: Laparoscopic cholecystectomy, Biliary injuries, Complications
Abstract
Background and Objectives:
Laparoscopic cholecystectomy has a 0.3% to 0.5% morbidity rate due to major biliary injuries. The majority of surgeons have routinely performed the so-called “infundibular” technique for gallbladder hilar dissection since the introduction of laparoscopy in the early nineties. The “critical view of safety” approach has only been recently discussed in controlled studies. It is characterized by a blunt dissection of the upper part of Calot's space, which does not usually contain arterial or biliary anomalies and is therefore ideal for a safe dissection, even in less experienced hands.
Materials and Methods:
We applied and compared the critical view of safety triangle approach with the infundibular approach in a retrospective cohort study. We divided 174 patients into 2 groups, with a similar case-mix (cholelithiasis, chronic cholecystitis, and acute cholecystitis). Results of operations performed by a young surgeon using critical view of safety dissection were compared to results of the infundibular approach performed by an experienced surgeon. Outcome values and operative times were examined with univariate analysis (Student t test).
Results:
No difference occurred in terms of morbidity (even though comparison for biliary injuries is inconclusive because of insufficient power) and outcome; significant differences were found in operative time, favoring the critical view of safety approach in every stage of gallbladder disease, with minor significance for acute cases.
Conclusion:
We suggest this technique as the gold standard for resident teaching, because it has a similar rate of biliary and hemorrhagic complications but has a shorter operative time, builds self-confidence, and is a simple standardized method both for complicated and uncomplicated gallbladder lithiasis.
INTRODUCTION
Sir Alfred Cuschieri, in an editorial released in 1990,1 cheered the first steps in laparoscopic cholecystectomy (LC) as the beginning of a new, exciting era, but alerted surgeons to be cautious, in order to avoid a substantial surgically induced morbidity. Twenty years later, the small increase in the rate of iatrogenic major biliary injury is tolerated, thanks to the great benefits of this minimally invasive approach. Indeed biliary morbidity with LC is not less than the 0.4% rate of traditional open surgery, but almost 3 times higher.2 Nonetheless, the National Institutes of Health consensus elected LC as the “gold standard” for cholelithiasis in 1992.3 Strasberg et al,4 in the early nineties, pointed out how a “critical view of safety” (CVS) should be achieved every time, by dissecting the entire infundibulum off the liver bed and by freeing it of all fatty tissue, both in its dorsal and ventral aspects. This, in his opinion, would have prevented accidental biliary and vascular injuries, due to uncommon variations, incautious bleeding control, or unclear anatomy. These principles have been ignored until recent years, when standardization of the technique, together with some consistent data, have appeared in the literature, asserting that this way of dissecting the gallbladder pedicle would bear a highly protective role against bile duct injuries. This would be especially important in teaching the approach to the gallbladder hilus.
METHODS
A retrospective analysis of a 2-year practice in our surgical unit has been conducted. Among a pool of “laparoscopic surgeons” equally acquainted with basic laparoscopy, 2 were selected on an age and experience basis. The youngest (<40 years old) routinely practiced CVS cholecystectomy, and the other (>50 years old) used the classic infundibular (IN) technique. Their cases (a total of 174 LC) were divided into 2 groups: the first (young surgeon, CVS tech) comprising 90 cases, the second (experienced surgeon, IN technique) comprising 84 cases. The 2 groups had a homogeneous case mix between cholelithiasis, chronic cholecystitis, and acute cholecystitis, as presented in Table 1. No significant differences were found regarding age, sex, ASA risk, obesity, or previous operations between the 2 cohorts of patients. Patients with associated pathologies or adhesions that could complicate the operation were excluded. Also converted cases (<5% of the total and equally distributed) were excluded. Operative technique was standard in both CVS and infundibular (IN) approaches, and the trocar position resembled the 4-port French scheme.
Table 1.
Case Mix in the 2 Groups Based on Level of Gallbladder Inflammation
| Case Mix (no. of pts) | Group 1: Critical View of Safety + Young Surgeon | Group 2: Infundibular + Experienced Surgeon |
|---|---|---|
| Cholelithiasis | 40 | 46 |
| Chronic cholecystitis | 24 | 18 |
| Acute cholecystitis | 26 | 20 |
| Total | 90 | 84 |
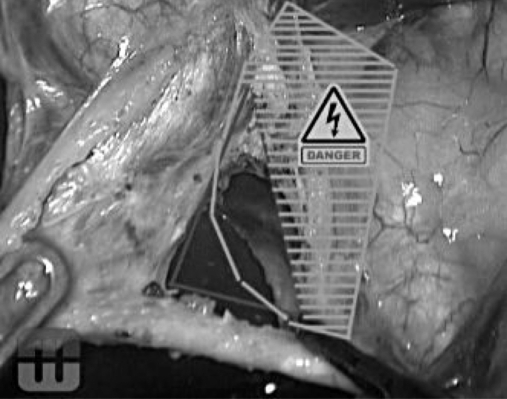
In the CVS technique, cephalad traction of the fundus is obtained by the T4 grasper, together with a lateral traction of the infundibulum by the T3 grasper. A complete incision of the serosa is performed both in the medial and lateral aspect of the infundibulum and extended upwards almost to the fundus. The medial incision is performed over the vertical fatty line visible on the gallbladder wall; it usually corresponds to the anterior cystic artery. The medial release of the artery is obtained with electrocautery by dissecting it from the gallbladder wall. The section of Calot's artery (which connects the cystic artery to the cystic duct) permits access to the critical safety triangle, set between the gallbladder wall on the right, the cystic duct inferiorly, and the cystic artery on the left. The entire fatty dissection of this triangle and the mobilization of the infundibulum, both anteriorly and posteriorly, permits visualization of the liver surface through the triangle, well above Ruviers’ sulcus, as described by Strasberg et al4 (Figure 1). The clipping and the section of the duct, next to the gallbladder, the clipping of the artery, and the retrograde dissection of the gallbladder complete the operation.
Figure 1.
Exposure of the triangle of safety (inner) compared to the triangle of Calot (outer with danger zone).
In the IN technique after suspension of the IV hepatic segment with a hanger (T4) and the lateral traction of the infundibulum (T3), the serosa is incised parallel to the cystic duct and artery, just caudally to the infundibulum edge, thus dissecting the duct and artery to open Calot's triangle. After the identification of the 2 structures, passing through a fatty-free triangle, they are sectioned between clips, and retrograde cholecystectomy is completed. All patients had a subhepatic drain positioned for 1 day, started oral intake on day 1, and generally were dismissed on the second postoperative day.
The Student t test was used to determine statistical significance in univariate analysis; power sample size was not calculated in order to obtain significance of mortality or bile injury outcomes (expected rate 0.4%), for which large prospective cohorts would have been needed. Attention was focused instead on the operating time, as an indirect measure of “ease and confidence” with an operative technique to be recommended as the ideal approach for training purposes.
RESULTS
No mortalities occurred in the series. Morbidity was 0.1% (1 patient) in group 1 and 0.2% in group 2 (2 patients). One biliary leak from the cystic duct in the first patient (acute gangrenous cholecystitis) resolved after an endoscopic sphincterotomy was performed on postoperative day 1. The other 2 patients had intraoperative hemorrhages, both controlled with bipolar coagulations and clip applications; 1 of the 2 patients required blood transfusions. No difference was found regarding pain, wound infections, time to first passage of stool, re-feeding, or discharge. Neither group required the use of high-tech instruments (LaparoSonic scissors or radiofrequency devices) apart from mono- or bipolar cautery. Cholangiography has never been performed intraoperatively. Significant differences were found in the operative times. Both median times (51.5 min vs 69.7 min) and average time divided by case-difficulty (defined by different grades of gallbladder inflammation) were in favor of the CVS approach. The difference was minor (but still significant) for acute cholecystitis (Table 2).
Table 2.
Operative Time in the 2 Groups
| Group 1: Critical View of Safety + Young Surgeon | Group 2: Infundibular + Experienced Surgeon | P | |
|---|---|---|---|
| Cholelithiasis (min) | 41.2 | 58.3 | <.005 |
| Chronic cholecystitis (min) | 50.5 | 94.0 | <.005 |
| Acute cholecystitis (min) | 75.6 | 94.7 | .012 |
| Total (min) | 51.5 | 69.7 | <.005 |
DISCUSSION
Prevention of iatrogenic bile injuries is still a matter of significant concern, despite almost 25 years passing since the first laparoscopic cholecystectomy was performed. The debate has sparked renewed interest since the introduction of natural orifice surgery (NOTES) and single port access surgery.5 In Italy, a national survey shows an incidence of 0.42% of major bile injuries during LC in 56 591 patients, with higher rates in cholecystitis and low-volume practice subgroups.6 The approach to the gallbladder's pedicle is of utmost importance for the prevention of injuries. Three main techniques have been standardized. The oldest and most common approach is the infundibular one. The classic dissection of Calot's triangle might misrepresent vascular or biliary anatomical variants, which are frequently located in the medial part of the area. Strasberg7 identified an “error trap” to avoid, regarding the IN technique, in which the common hepatic duct might be mistaken for the gallbladder wall in severe inflammation. Katkhouda et al8 suggest the extension of the cystic duct's dissection to the confluence with the common hepatic duct, to perform what he calls a “visual cholangiography.” Another way to prevent injuries, more frequently performed in open surgery (but also described in LC, mostly with the use of ultrasonic sharp dissection9), is the “dome-down” or “fundus-first” technique, often advocated for acute cholecystitis.10 The error trap of this technique (following Strasberg) concerns the possible injury to the right hepatic artery, which might be retracted downwards, along with the gallbladder.7 Routine intraoperative cholangiography has been advocated by many authors11: its use, especially in emergencies, calls for some organization in the operating theater and operative expertise. Alas, intraoperative cholangiography (IOC) does not seem to prevent bile duct injuries, even if it helps with immediate identification of the injury.12 IOC ineffectiveness at lowering the rate of biliary lesions has been confirmed in large multicenter trials.6 There was no need, in either of our groups, for intraoperative cholangiograms, which are not routinely performed in our patients. The importance of cholangiography in clarifying unclear anatomy is ascertained, but largely unnecessary in our opinion, both for the rate of failure of cystic duct cannulation and for the possible injuries that may be caused by the incautious forcing of the biliary catheter through the cystic valve, especially in inflammatory entanglement of the duct. The effort to standardize an approach to the cystic artery and duct that could effectively avoid the area where ductal and arterial anomalies are likely to be encountered brought Strasberg et al4 to outline the “critical view of safety.” Since 1995, their suggestion has been little mentioned, until the initial papers and retrospective series started analyzing the results of the technique.13,14 After these studies, other authors15,16 from around the world have started collecting cases and standardizing the operative technique. The results seem promising, as in large single-institution series, the “observed BDI rate drops from 1/9 to 1/15, representing an order-of-magnitude of improvement in the safety of LC”: the authors consider these results as superior to routine cholangiography.17 Other authors18 have tested the validity of the technique even in acute cholecystitis (performed by entering the inner subserosal layer for dissection). The approach is considered viable even for NOTES gallbladder surgery.19 A safe cholecystectomy technique is particularly important when considering trainees or young surgeons, who have scarce experience in biliary anatomical variance and are at risk of causing a major injury under emergency conditions (intraoperative bleedings, difficult anatomy, severe inflammation).20 Our results show no difference in terms of complications between an experienced laparoscopic surgeon using the IN approach and a younger colleague using CVS; a minor number of intraoperative bleedings, without statistical significance, could validate the rationale of the CVS approach towards dissection of an area without vascular abnormalities; moreover, the distal clipping of the cystic artery may favor easier dissection and consequently fewer accidental bleedings, especially in inflammatory conditions. The power of our study is not sufficient to analyze the outcome of the “bile duct injury rate,” as multicenter trials are required because of the low expected rate of events. The shorter operative times are symptomatic of increased confidence due to the technique, which probably makes the surgeon feel more secure, both with inflamed and uninflamed anatomy. We believe that a diffusion of this simple, practical technique might be desirable in training hospitals, residencies, and district hospitals, or anywhere laparoscopic experience might be basic or limited to standard operations.21 The results of CVS in the literature and in the present study forecast the approach as the future gold standard in the dissection of the gallbladder elements, and a further dissemination of the technique is important, especially for training purposes.
Contributor Information
Nereo Vettoretto, Laparoscopic Surgery, M. Mellini Hospital, Chiari (BS), Italy..
Cristiano Saronni, General and Vascular Surgery, M. Mellini Hospital, Chiari (BS), Italy..
Asaf Harbi, Surgical Clinic, University of Brescia, Italy (Dr. Harbi)..
Luca Balestra, General and Vascular Surgery, M. Mellini Hospital, Chiari (BS), Italy..
Lucio Taglietti, General and Vascular Surgery, M. Mellini Hospital, Chiari (BS), Italy..
Maurizio Giovanetti, General and Vascular Surgery, M. Mellini Hospital, Chiari (BS), Italy..
References:
- 1. Cuschieri A, Terblanche J. Laparoscopic cholecystectomy: evolution, not revolution. Surg Endosc. 1990; 4: 125–126 [DOI] [PubMed] [Google Scholar]
- 2. Gigot JF. Bile duct injury during laparoscopic cholecystectomy: risk factors, mechanisms, type, severity and immediate detection. Acta Chir Belg. 2003; 103: 154–160 [DOI] [PubMed] [Google Scholar]
- 3. NIH Gallstones and laparoscopic cholecystectomy, NIH Consens Statement 1992Sep 14-16;10(3):1–20. http://consensus.nih.gov/1992/1992gallstonesLaparoscopy090html.htm 1992. Accessed 10 October 2010 [PubMed]
- 4. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180: 101–125 [PubMed] [Google Scholar]
- 5. Vettoretto N, Arezzo A. Human natural orifice translumenal endoscopic surgery: on the way to two different philosophies? Surg Endosc. 2010; 24: 490–492 [DOI] [PubMed] [Google Scholar]
- 6. Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during laparoscopic cholecystectomy. Results of an Italian national survey on 56591 cholecystectomies. Arch Surg. 2005; 140: 986–992 [DOI] [PubMed] [Google Scholar]
- 7. Strasberg SM. Error traps and vasculo-biliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg. 2008; 15: 284–292 [DOI] [PubMed] [Google Scholar]
- 8. Katkhouda N, Mavor E, Mason RJ. Visual identification of the cystic duct-CBD junction during laparoscopic cholecystectomy (visual cholangiography). An additional step for prevention of CBD injuries. Surg Endosc. 2000; 14: 88–89 [DOI] [PubMed] [Google Scholar]
- 9. Fullum TM, Kim S, Dan D, Turner PL. Laparoscopic “dome-down” cholecystectomy with the LSC-5 harmonic scalpel. JSLS. 2005; 9: 51–57 [PMC free article] [PubMed] [Google Scholar]
- 10. Rosemberg J, Leinskold T. Dome down laparosonic cholecystectomy. Scandinavian J Surg. 2004; 93: 48–51 [DOI] [PubMed] [Google Scholar]
- 11. Flum DR, Koepsell T, Haegerty P, Sinanan M, Dellinger EP. Common bile duct injury during laparoscopic cholecystectomy and the use of intraoperative cholangiography. Adverse outcome or preventable error? Arch Surg. 2001; 136: 1287–1292 [DOI] [PubMed] [Google Scholar]
- 12. Debru E, Dawson A, Leibman S, Richardson M, Glen L, Hollinshead J, Falck GL. Does routine cholangiography prevent bile duct transection? Surg Endosc. 2005; 19: 589–593 [DOI] [PubMed] [Google Scholar]
- 13. Callery MP. Avoiding biliary injury during laparoscopic cholecystectomy: technical considerations. Surg Endosc. 2006; 20: 1654–1658 [DOI] [PubMed] [Google Scholar]
- 14. Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008; 74(10): 985–987 [PubMed] [Google Scholar]
- 15. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009; 13: 498–503 [DOI] [PubMed] [Google Scholar]
- 16. Almutairi AF, Hussain YAMS. Triangle of safety technique: a new approach to laparoscopic cholecystectomy. HPB Surg. 2009: ID476159: 1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yegiyants S, Tejirian T, Collins JC. The “critical view of safety” is superior to intraoperative cholangiography for prevention of common bile duct injury. [abstract] Presented at the 2008 Annual Meeting of the Pacific Coast Surgical Association [Google Scholar]
- 18. Honda G, Iwanaga T, Kurata M, Watanabe F, Satoh H, Iwasaki K. The critical view of safety in laparoscopic cholecystectomy is optimized by exposing the inner layer of the subserosal layer. J Hepatobiliary Pancreat Surg. 2009; 16: 445–449 [DOI] [PubMed] [Google Scholar]
- 19. Auyang E, Vaziri K, Hungness ES, Martin JA, Soper NJ. NOTES: dissection of the critical view of safety during transcolonic cholecystectomy. [abstract] Presented at 2009 Congress of the Society for the Surgery of the Alimentary Tract [DOI] [PubMed] [Google Scholar]
- 20. Nagral S. Anatomy relevant to cholecystectomy. J Min Access Surg. 2005; 1: 53–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khan MN, Nordon I, Ghauri AS, Ranaboldo C, Carty N. Urgent cholecystectomy for acute cholecystitis in a district general hospital: is it feasible? Ann R Coll Surg Engl. 2009; 91(1): 30–34 [DOI] [PMC free article] [PubMed] [Google Scholar]