Abstract
Objective:
Bleaching agents may not be safe for dental materials. The purpose of this in-vitro study was to evaluate the effects of Opalescent Quick “in-office bleaching gel” containing 35% carbamide peroxide on the surface roughness and hardness of microfilled (Heliomolar) and hybride (Spectrum TPH) composite resins.
Materials and Methods:
Twenty specimens of Spectrum TPH composite resins and twenty Heliomolar composite resins were fabricated using a metallic ring (6.5 mm diameter and 2.5 mm thickness) and light cured, then their surfaces were polished. Specimens of each composite resin were divided into two equal groups. Ten specimens of each type of composite were stored in water at 37°C as the control groups and 35% carbamide peroxide gel (Opalescence Quick) as the other group for 30 minutes a week for 3 weeks. Then the specimens were subject to roughness and hardness tests.
Results:
This study revealed that using 35% carbamide peroxide bleaching gels had no significant effect on the surface roughness of Spectrum TPH “hybrid” and Heliomolar “microfilled” composite resins. The surface hardness of Spectrum TPH composite treated with the subject gel significantly increased compared to heliomolar, which had no significant change after treatment with this bleaching gel.
Conclusion:
If tooth color matching of the composite had been satisfactory after office bleaching with 35% carbamide peroxide gel, this material would have been acceptable because it has no adverse effect on Heliomolar and Spectrum TPH composite resins.
Keywords: Tooth Bleaching, Composite Resins, carbamide peroxide
INTRODUCTION
Bleaching was first used to whiten teeth in the late 1870s [1]. The bleaching technique may be classified as the vital and nonvital bleaching or the office and home bleaching. The use of bleaching for improving the aesthetics of natural dentition has widened only after the introduction of home bleaching systems in the 1990s [2–5].
Although from the procedure standpoint, bleaching is safe for soft tissues, it may not be safe for dental materials that have high erosive or degradation characteristics [4]. This may be more significant in the case of home bleaching gels, because patients may not follow professional recommendations but instead apply these products more often in order to increase the “bleaching power” and speed of action. The use of bleaching agents on restorative materials has not been tested comprehensively.
Restorative materials may have different reactions by application of bleaching agents. One of the adverse effects of this material is mercury release from amalgam restoration and the bleaching agent may roughen the resin-based composite, although this may have no clinical significance [6–9].
Interestingly, some studies reported an increase, a decrease, or no change in composite surface hardness after application of carbamide peroxide gels [8,9]. This shows that the effect of carbamide peroxide gels may depend on the composite material.
Some materials, such as high-viscosity glass ionomer cements and polyacid-modified resin-based composites used by patients with a high caries risk, have been affected by preventive treatments such as acidulated phosphate fluoride gels or foams that could alter their surface roughness, micromorphology and hardness [10–13].
The purpose of this study was to determine whether in-office tooth whiteners with strong oxidizing agents cause chemical softening of microfilled and hybrid composite resins. The surface hardness of the composites were also compared after treatment.
MATERIALS AND METHODS
Two resin-based composites, Spectrum TPH (Dentsply-De Trey, Konstanz, Germany) a hybrid composite and Heliomolar (Vivadent, Schaan, Liechtenstein) a microfilled composite (Table 1), were used to represent a microfilled anterior and a hybrid composite, respectively.
Table 1.
Tested composites.
| Composite | Manufacturer | Composition |
|---|---|---|
| Spectrum TPH | Dentsply De-Trey, Konstanz, Germany | Bis-GMA, Bis-EMA, TEGDMA, Barium aluminoborosilicate glass (below 1.5 μ) Colloidal silica (0.04 μ) Filler weight: 77% |
| Heliomolar | Vivadent Schaan Liechtenstein | Bis-GMA, Urethane dimethacrylate and decandiol dimethacrylate, Silicon dioxide, ytterbium trifluoride, copolymer particle (0.04–0.2 μ) Filler weight: 66.7% |
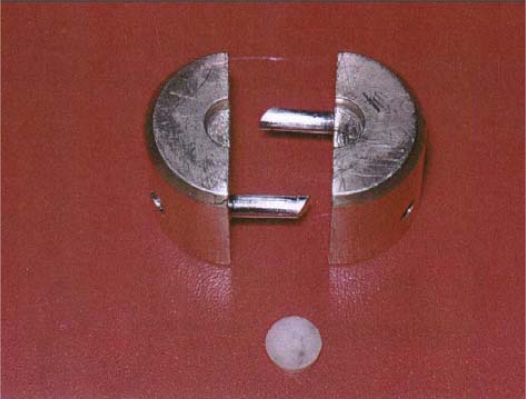
The bleaching agent was 35% carbamide peroxide gel Opalescence Quick, (Ultradent Production Inc. USA). For each resin-based composite, 20 cylindrical specimens (6.5 mm in diameter and 2.5 mm thickness) were made. To prepare the specimens, the resin was transferred into a metal mold (Fig 1), then the filling was covered with acetate strips (Hawe Neos Dental, Biggo, Switzerland). A glass slide was then placed over this and pressure was applied to extrude the excess materials. The restoratives were light polymerized according to manufacturers’ cure times (40 seconds) through the glass slide with a coltolux II light-cure unit (Coltene/Whaledent Inc. USA) the mean intensity of the light source (510 mW/cm2, SD=4) was determined with a radiometer (Cure Rite, Efos Inc, Ontario, Canada).
Fig 1.
The metallic mold used for preparing the specimens.
After polishing the surface of the specimens, they were stored for one week in distilled water at 37°C for post-irradiation hardening. Specimens were divided into four groups.
Groups 1 and 2: Ten Spectrum TPH composite discs (group 1) and 10 Heliomolar composite discs (group 2), as control groups.
Twenty group 1 and 2 specimens were stored in distilled water at 37°C for three weeks.
Groups 3 and 4: Ten specimens in groups 3 (Spectrum TPH) and 10 specimens in group 4 (Heliomolar) were treated with 35% carbamide peroxide (Opalescence Quick) for 30 minutes/week for three weeks.
The bleaching gels were removed using a water jet and a standardized one-minute rinsing time. Storage medium was distilled water at 37°C during the hiatus periods. The specimens were subjected to hardness and roughness tests.
Surface roughness (Ra) of the composite specimens was determined by mechanical profilometry (Taylor-Hobson, Leicester, England). Ra is the mathematic mean height of the surface roughness irregularities along the traverse length. The traverse speed was set at 0.25 mm per second with a cutoff control of 0.3 mm. The traverse length was 4.0 mm. The profilometric measurements were accomplished on each specimen and then averaged to obtain the surface roughness of the specimen.
Then all specimens were subjected to hardness testing using a digital micro hardness tester (Wolpert, Darmstadt, Germany). Specimens were placed centrally beneath the indenter and a 500 g load was applied through the indenter for a dwell time of 15 seconds.
The knoop hardness number (KHN) corresponding to each indentation was computed by measuring the dimensions of the indentations and using the formula KHN=1.451(F/d2), where F is the test load in Newton and d is the longer diagonal length of the indentation in millimeters.
Statistical analysis was performed using Kruskal-Wallis, Mann-Whitney and Tukey tests at the significance level of P<0.05.
RESULTS
KHN and Ra of the four groups are demonstrated in Tables 2 and 3.
Table 2.
Surface roughness (Ra) and surface hardness (KHN) in Spectrum TPH groups (groups 1 and 3).
|
Specimen |
Ra |
KHN |
|||||
|---|---|---|---|---|---|---|---|
| Name | Number | Mean | SD | SE | Mean | SD | SE |
| Spectrum TPH | 10 | 0.25 | 0.0527 | 0.0166 | 58.66 | 9.5083 | 3.0069 |
| Spectrum TPH + Opalescence Quick | 10 | 0.23 | 0.0411 | 0.1302 | 76.06 | 14.4434 | 4.5674 |
SD= Standard Deviation, SE=Standard Error
Table 3.
Surface roughness (Ra) and surface hardness (KHN) in Heliomolar groups (groups 2 and 4).
|
Specimen |
Ra |
KHN |
|||||
|---|---|---|---|---|---|---|---|
| Name | Number | Mean | SD | SE | Mean | SD | SE |
| Heliomolar | 10 | 0.24 | 0.0843 | 0.0266 | 40.73 | 7.3779 | 2.3331 |
| Heliomolar+Opalescence Quick | 10 | 0.23 | 0.1059 | 0.0335 | 41.25 | 4.1212 | 1.3032 |
SD= Standard Deviation, SE=Standard Error
Statistical analysis of the recorded results was conducted using Mann-Whitney, Kruskal Wallis and Tukey tests at a significance level of P<0.05. No statistically significant difference was observed in surface roughness between any control and experimental groups. The bleaching gel caused a significant increase in surface hardness of Spectrum TPH “hybrid” composite resin specimens (P=0.007). Spectrum TPH specimens were significantly harder than heliomolar specimens (P=0.001). No significant change was observed in surface hardness of heliomolar control and experimental groups.
DISCUSSION
Although there is widespread use of bleaching agents, there is no agreement on the effect of bleaching agents on enamel or restorative materials. Under the conditions of this in vitro study, Opalesence Quick 35% carbamide peroxide gel had no significant effect on the surface roughness of Heliomolar and Spectrum TPH composite resins.
Little literature exists that addresses the possible detrimental effects on resin-based composites at higher concentrations of carbamide peroxide.
Yap AU and Wattanapayungkul evaluated the effect of 35% carbamide peroxide gel on the surface roughness of Spectrum TPH and Reactmer and Fuji II LC. The study revealed that this bleaching agent had no significant effect on the surface roughness of the specimens [14], which was similar to this study, suggesting that high concentration carbamide peroxide bleaching does not have a significant effect on surface roughness, either hybrid or microfilled composites.
The results of the current study agree with other researches conducted with 10% and 35% carbamide peroxide gel, confirming the mild effect, if any, that carbamide peroxide has on composite surfaces [15–16]. Most of the studies examining the effect of carbamide peroxide on resin-based composites have used 10% carbamide peroxide [2].
Although Bailey and Swift noted some softening of both hybrid and microfilled composite surfaces, these effects were not significant statistically [9]. Softening of resin based composites is believed to occur chemically in vivo, contributing to wear of the resin in stress-bearing areas [17,18]. Composite matrices composed of Bis-GMA resin polymers may be softened by chemicals with similar solubility parameters [16,19].
Although microfilled composites have higher resin content than hybrids and any difference in surface roughness might be expected to occur in this group, this did not occur in the present study. On the other hand, Soderholm et al [20] explained how the lowest crack density was found in microfilled composites, theorizing that the spherical shape of the filler may decrease stress and reduce the risk of crack growth. From the clinical standpoint, their results are interesting because several clinical studies have demonstrated that microfilled composites are more wear-resistant than other composites [21,22]; however, laboratory studies often indicate the opposite [23–25].
For Spectrum TPH composite, a significant increase in surface hardness was observed in the treated group. It means Opalescence Quick bleaching gel caused significant increase in surface hardness of this hybrid composite. It seems that active ingredients of the bleaching agent can remove the surface layer of Spectrum TPH composite specimens, which are rich of filler particles and have a harder surface. No significant difference was observed in the surface hardness of Heliomolar composite resin in the control and treated groups. In 2002, Garcia-Goody et al evaluated the effect of office bleaching gel on esthet-X, a micro-filled composite resin and achieved the same result. They found that office-bleaching gel has no significant effect on esthet-X composite resin [26].
Chemical softening of the restorative materials might also occur if the bleaching products have solubility parameters similar to that of the resin matrix. The Bis-GMA and UDMA resin polymer used in composites may be softened by chemicals with solubility parameters in the range of 1.82×104 to 2.97×104 J/m3 [27]. As the bleaching agents and many of their components are not listed in the solvent tables of the polymer handbook [28], it is unclear whether they have solubility parameters similar to that of resins used in various materials.
Although the composites used in this study were UDMA and Bis-GMA resin polymer, the result revealed that no softening had occurred on the surfaces of treated specimens.
The surface hardness of composite resins has been reported to increase [8], decrease [9,29] or remain unchanged [14,26,30–34] after using carbamide gels. Such wide variations in data suggest that some tooth-colored restorative materials may be more susceptible to alterations and some bleaching agents are more likely to cause those alterations. The latter may be attributed to differences in pH between the bleaching agents [35]. Bleaching gels contain a variety of aqueous solvents, any of which could contribute alone or in combination with other components to decrease the solubility of the resin matrix. The pH of the bleaching gel evaluated in this study was close to neutral and had minimal effect on the surface roughness of specimens. The pHs of most current bleaching products are close to neutral. The bleaching gel evaluated in this study falls into this category. In this study, Spectrum TPH composite resin without any gel treatment was significantly harder than Heliomolar composite resin. This result may be related to the type of the composites, as Spectrum is a hybrid and Heliomolar is a microfilled composite resin.
The clinical relevance of this project would indicate that high concentration carbamide peroxide bleaching gel, used as intended by the manufacturers, poses minimal risk to composite restorations. Risk of damage to soft tissues and accidental ingestion of bleaching gels also need to be investigated.
CONCLUSION
Under the conditions of this in vitro study, the effects of the in-office tooth whitener (35% carbamide peroxide gel) on surface hardness of microfilled and hybrid composite resins were material dependent. For Heliomolar composite, which is a microfilled composite, no significant effect on surface hardness was observed, but for Spectrum TPH composite, which is a hybrid composite, surface hardness was increased.
This study showed no significant differences in the surface roughness of the tested control and treated composites. There is no evidence to suggest that high-concentration carbamide peroxide bleaching gel causes significant changes in the surface roughness of either hybrid (Spectrum TPH) or microfilled (heliomolar) composite.
Acknowledgments
Authors would like to thank the Biomaterial Research center and vice chancellor for Research of Shiraz University of Medical Sciences for supporting this study.
REFERENCES
- 1.Fasanaro TS. Bleaching teeth: history, chemicals, and methods used for common tooth discolorations. J Esthet Dent. 1992 May-Jun;4(3):7–8. doi: 10.1111/j.1708-8240.1992.tb00666.x. [DOI] [PubMed] [Google Scholar]
- 2.Haywood VB, Leech T, Heymann Ho, Crumpler D, Bruggers K. Nightguard vital bleaching: effects on enamel surface texture and diffusion. Quintessence Int. 1990 Oct;21(10):801–4. [PubMed] [Google Scholar]
- 3.Haywood VB, Leonard RH, Dickinson GL. Efficacy of six months nightguard vital bleaching of tetracycline-stained teeth. J Esthet Dent. 1997;9(1):13–9. doi: 10.1111/j.1708-8240.1997.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 4.Haywood VB, Heymann Ho. Nightguard vital bleaching: how safe is it? Quintessence Int. 1991 Jul;22(7):515–23. [PubMed] [Google Scholar]
- 5.Haywood VB, Leonard RH, Nelson CF. Effectiveness, side effects and long term status of night-guard vital Bleaching. J Am Dent Assoc. 1994 Sep;125(9):1219–26. doi: 10.14219/jada.archive.1994.0154. [DOI] [PubMed] [Google Scholar]
- 6.Hummert TW, Osborne JW, Norling BK, Cardenas HL. Mercury in solution following exposure of various amalgams to carbamide peroxides. Am J Dent. 1993 Dec;6960:305–9. [PubMed] [Google Scholar]
- 7.Robertello FJ, Dishman MV, Sarrett DC, Epperly AC. Effect of home bleaching products on mercury release form an admixed amalgam. Am J Dent. 1999 Oct;12(5):227–30. [PubMed] [Google Scholar]
- 8.Cooley RL, Burger KM. Effect of carbamide peroxide on composite resins. Quintessence Int. 1991;22:817–21. [Google Scholar]
- 9.Bailey SJ, Swift EJ., Jr Effects of home bleaching products on composite resins. Quintessence Int. 1992 Jul;23(7):489–94. [PubMed] [Google Scholar]
- 10.Triana RT, Millan CP, Barrio JG, Garcia-Godoy F. Effect of APF gel on light-cured glass ionomer cements: an SEM study. J Clin Pediatr Dent. 1994 Winter;18(2):109–13. [PubMed] [Google Scholar]
- 11.Cehreli ZC, Yazici R, Garcia-Godoy F. Effect of 1.23 percent APF gel on fluoride-releasing restorative materials. ASDC J Dent Child. 2000 Sep-Oct;67(5):330–7. [PubMed] [Google Scholar]
- 12.Neuman E, Garcia-Godoy F. Effect of APF gel on glass ionomer cement: an SEM study. ASDC J Dent Child. 1992 Jul-Aug;59(4):289–95. [PubMed] [Google Scholar]
- 13.Garcia-Godoy F, Garcia Godoy A. Effect of APF minute-foam on the surface roughness, hardness, and micromorphology of high-viscosity glass ionomers. J Dent child (chic) 2003 Jan-Apr;70(1):19–23. [PubMed] [Google Scholar]
- 14.Wattanapayungkul P, Yap AU. Effects of in-office bleaching products on surface finish of tooth-colored restorations. Oper Dent. 2003 Jan-Feb;28(1):15–9. [PubMed] [Google Scholar]
- 15.Basting RT, Rodrigues AL, Jr, Serra MC. The effect of 10% carbamide peroxide, carbapol and/or glycerin on enamel and dentin microhardness. Oper Dent. 2005 Sep-Oct;30(5):608–16. [PubMed] [Google Scholar]
- 16.Swift EJ, Jr, Perdigao J. Effects of bleaching on teeth and restorations. Compend Contin Educ Dent. 1998 Aug;19(8):815–20. [PubMed] [Google Scholar]
- 17.Yap AU, Wattanapayungkul P. Effects of in-office tooth whiteners on hardness of tooth-colored restoratives. Oper Dent. 2002 Mar-Apr;27(2):137–41. [PubMed] [Google Scholar]
- 18.van Groeningen G, Jongebloed W, Arends J. Composite degradation in vivo. Dent Mater. 1986 Oct;2(5):225–7. doi: 10.1016/S0109-5641(86)80018-5. [DOI] [PubMed] [Google Scholar]
- 19.WU W, McKinney JE. Influence of chemicals on wear of dental composites. J Dent Res. 1982 Oct;61(10):1180–3. doi: 10.1177/00220345820610101501. [DOI] [PubMed] [Google Scholar]
- 20.Soderholm KJ, Zigan M, Ragan M, Fischlschweiger W, Bergman M. Hydrolytic degradation of dental composites. J Dent Res. 1984 Oct;63(10):1248–54. doi: 10.1177/00220345840630101701. [DOI] [PubMed] [Google Scholar]
- 21.Jorgensen KD, Horsted P, Janum O, Krogh J, Schultz J. Abrasion of class 1 restorative resins. Scand J Dent Res. 1979 Apr;87(2):140–5. doi: 10.1111/j.1600-0722.1979.tb00665.x. [DOI] [PubMed] [Google Scholar]
- 22.Christensen RP, Christensen GJ. In vivo comparison of a microfilled and a composite resin: a three-year report. J Prosthet Dent. 1982 Dec;48(6):657–63. doi: 10.1016/s0022-3913(82)80024-3. [DOI] [PubMed] [Google Scholar]
- 23.Powers JM, Allen LJ, Craig RG. Two-body abrasion of commercial and experimental restorative and coating resins and an amalgam. J Am Dent Assoc. 1974 Nov;89(5):1118–22. doi: 10.14219/jada.archive.1974.0579. [DOI] [PubMed] [Google Scholar]
- 24.Craig RG, Powers JM. Wear of dental tissues and materials. Int Dent J. 1976 Jun;26(2):121–33. [PubMed] [Google Scholar]
- 25.Prasad SV, Calvert PD. Abrasive wear of particle-filled polymers. J Mater Sci. 1980;15:1746–54. [Google Scholar]
- 26.Garcia-Godoy F, Garcia-Godoy A, Garcia-Godoy F. Effect of bleaching gels on the surface roughness, hardness, and micromorphology of composites. Gen Dent. 2002 May-Jun;50(3):247–50. [PubMed] [Google Scholar]
- 27.Wu W, Toth EE, Moffa JF, Ellison JA. Subsurface damage layer of in vivo worn denal composite restorations. J Dent Res. 1984 May;63(5):675–80. doi: 10.1177/00220345840630051401. [DOI] [PubMed] [Google Scholar]
- 28.Bandrup J, Immergut EH. Polymer Handbook. 3rd ed. New York: John Wiley and Sons; 1989. pp. 519–59. [Google Scholar]
- 29.Attin T, Hannig C, Wiegand A, Attin R. Effect of bleaching on restorative materials and restorations--a systematic review. Dent Mater. 2004 Nov;20(9):852–61. doi: 10.1016/j.dental.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Campos I, Briso AL, Primenta LA, Ambrosano G. Effects of bleaching with carbamide peroxide gels on microhardness of restoration materials. J Esthet Restore Dent. 2003;15(3):175–82. doi: 10.1111/j.1708-8240.2003.tb00187.x. [DOI] [PubMed] [Google Scholar]
- 31.urker SB, Biskin T. The effect of bleaching agents on the microhardness of dental aesthetic restorative materials. J Oral Rehabil. 2002 Jul;29(7):657–61. doi: 10.1046/j.1365-2842.2002.00896.x. [DOI] [PubMed] [Google Scholar]
- 32.Langsten RE, Dunn WJ, Hartup GR, Murchison DF. Higher-concentration carbamide peroxide effects on surface roughness of composites. J Esthet Restor Dent. 2002;14(2):92–6. doi: 10.1111/j.1708-8240.2002.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 33.Turker SB, Biskin T. Effect of three bleaching agents on the surface properties of three different esthetic restorative materials. J Prosthet Dent. 2003 May;89(5):466–73. doi: 10.1016/s0022-3913(03)00105-7. [DOI] [PubMed] [Google Scholar]
- 34.Wattanapayungkul P, Yap AU, Chooi KW, Lee MF, Selamat RS, Zhou RD. The effect of home bleaching agents on the surface roughness of tooth-colored restoratives with time. Oper Dent. 2004 Jul-Aug;29(4):398–403. [PubMed] [Google Scholar]
- 35.Price RB, Sedarous M, Hiltz GS. The PH of tooth-whitening products. J Can Dent Assoc. 2002 Sep;66(8):421–6. [PubMed] [Google Scholar]