Abstract
Objective
To examine the association between maternal age at first birth and infant mortality, stunting, underweight, wasting, diarrhoea and anaemia in children in low- and middle-income countries.
Design
Cross-sectional analysis of nationally representative household samples. A modified Poisson regression model is used to estimate unadjusted and adjusted RR ratios.
Setting
Low- and middle-income countries.
Population
First births to women aged 12–35 where this birth occurred 12–60 months prior to interview. The sample for analysing infant mortality is comprised of 176 583 children in 55 low- and middle-income countries across 118 Demographic and Health Surveys conducted between 1990 and 2008.
Main outcome measures
Infant mortality in children under 12 months and stunting, underweight, wasting, diarrhoea and anaemia in children under 5 years.
Results
The investigation reveals two salient findings. First, in the sample of women who had their first birth between the ages of 12 and 35, the risk of poor child health outcome is lowest for women who have their first birth between the ages of 27 and 29. Second, the results indicate that both biological and social mechanisms play a role in explaining why children of young mothers have poorer outcomes.
Conclusions
The first-born children of adolescent mothers are the most vulnerable to infant mortality and poor child health outcomes. Additionally, first time mothers up to the age of 27 have a higher risk of having a child who has stunting, diarrhoea and moderate or severe anaemia. Maternal and child health programs should take account of this increased risk even for mothers in their early 20s. Increasing the age at first birth in developing countries may have large benefits in terms of child health.
Article summary
Article focus
The prevalence of nutritional deficiencies underscores the need to understand the basic determinants of poor child health outcomes.
Young age of the mother at their first birth is one such determinant due to biological and social mechanisms.
Comparison across low- to middle-income countries enables generalisation of cross-sectional associations between the age of the mother and child health outcomes.
Key messages
Child health outcomes remain poor in many low- to middle-income countries.
The age of the mother at their first birth is a key correlate of child health outcomes.
Teen mothers have children with the worst health outcomes and children of mothers who have their first birth in their early 20s are also at risk of poor health outcomes compared to first time mothers in their late 20s.
Strengths and limitations of this study
One of the strengths of this study is the breadth of countries included in the sample.
In applying secondary source data, the study is subject to omitted variable and recall bias.
Introduction
Progress towards reaching Millennium Development Goal 4 focuses on measurable reduction in under-5 mortality. In low- to middle-income countries, this also means “revitalising efforts against… diarrhoea, while bolstering nutrition…”.1 The risk of under-5 mortality and the prevalence of diarrhoeal disease and nutritional deficiencies that manifest themselves in outcomes such as stunting, wasting, underweight and anaemia in young children, underscore the need to understand the basic determinants of these poor child health outcomes. In India alone, 6.0% (95% CI 5.7% to 6.3%) of children die before their 5th birthday. In the same population, for children under 5, 42.2% are underweight, 47.8% are stunted, 19.7% are wasted and 69.1% are anaemic.2 A cross-country study highlights that these prevalence percentages are the norm throughout low- to middle-income countries.3 A report on adolescent girls in low- to middle-income countries by the Center for Global Development4 highlights the risk to child health associated with young motherhood. When considering child health, the report draws on intergenerational influences on child health outcomes rather than a cross-sectional observation of children alone. The effect of the age of the mother at first birth on child health outcomes has been explored in several studies in low- to middle-income countries.5–14 In the case of India, Raj et al13 showed that children born to mothers who were married below the age of 18 were at a higher risk of stunting and underweight compared to children of women who had married at age 18 or older. In another study, using the World Fertility Survey, Trussell and Hammerslough14 also found that the mother's age at first birth was a significant risk factor for infant mortality in Sri Lanka. In low- to middle-income countries, 26.5% of women have their first birth before the age of 18, and 83.1% before age 24.15 Much debate, particularly with regard to US population samples, concerns the social versus physiological influence of young motherhood on child health outcomes.16–22 Young age can be a proxy for “short stature, low body weight in relation to height, and greater likelihood of inadequate weight gain during pregnancy along with difficulty of delivery”.23 These physiological factors point to vulnerability to poor child health outcomes. Women in low- to middle-income countries who have children at a young age are also more likely to be, and remain, poor and uneducated.4 These social factors also disadvantage young mothers in terms of their child's health outcomes. Analysis that generalises across and within countries, rather than focusing on a sample from a single country, provides standardised analyses and results to assess age as a proxy for physiological immaturity and social disadvantage and its effect on child health outcomes. Earlier work by Hobcraft12 in 1992 examined the effect of age at first birth on child survival in a number of countries using Demographic and Health Surveys (DHS) available at that time. Given the prevalence of poor child health outcomes in low- to middle-income countries, and not just high infant mortality, studies that extend the monitoring of child health beyond infant mortality provide valuable information regarding health disparities and progress in achieving Millennium Development Goal 4 and its sub-goals relating to child health.
The purpose of the current study is to assess the association between maternal age at first birth and child health outcomes: infant mortality, stunting, underweight, wasting, diarrhoea and anaemia. By controlling for socioeconomic factors, the physiological effect of young motherhood on child health can be separated out from the social disadvantage that young mothers are also likely to face. The findings could critically inform family planning policies and programs aimed at delaying first birth beyond the teenage years.
Methods
Data source
Information from 118 DHS conducted in 55 countries between 1990 and 2008 provided the data for the analysis in this study.24 The DHS are nationally representative household sample surveys that measure population, health, socioeconomic and anthropometric indicators, emphasising maternal and child health.25 The DHS are an important data source for studying population health across developing countries due to their extensive coverage, comparability and data quality.26–28 To ensure standardisation and comparability across diverse sites and times, in conducting the DHS, Macro ICF employs intense interviewer training, standardised measurement tools and techniques, an identical core questionnaire and instrument pretesting.29 Each participating country's report details pretesting and quality assurance measures by survey.15 The DHS is modular in structure, and in addition to the core questionnaire, a set of country-relevant sections and country-specific variables are included. The DHS provides data with standardised variables across surveys.30
Sampling plan
The DHS involves stratified cluster randomised samples of households.31 The sampling frame was stratified by urban and rural status and additionally by country-specific geographic or administrative regions. Within each stratified area, random clusters of households were drawn from a list of all enumeration areas taken from a population census. In the second stage of sampling, all private households within the cluster were listed (institutions excluded) and an average of 25 houses within a cluster were selected by equal probability systematic sampling to be surveyed. Detailed sampling plans are available from survey final reports.15
Within each sampled household, a household questionnaire was administered and women eligible for a more detailed women's survey were identified. In most surveys all women between the ages of 15 and 49 were interviewed. In a limited number of surveys, the target group is women aged 10–49 or 15–45, or ever-married women. The child anthropometry module was conducted in a selection of the Standard DHS.32 The DHS provides weights for calculating nationally representative statistics.
Study population and sample size
Our sample consists of children born to women who had their first birth 12–60 months before the survey. The lower bound of 12 months is applied so that each child has equal exposure to 1 year of life and we can accurately calculate infant mortality (deaths within the first year of life). Detailed child health measures are only taken for children up to 60 months of age which establishes our upper bound (the upper bound is 60 months rather than 59 months to conform to the WHO age categories). Only the first birth for each woman is included in our sample; for multiple first births we only use data from the first recorded birth, although we control for this being a part of multiple births. The initial sample is 288 752 children across 72 countries from 181 surveys. Infant mortality status is not available for 5313 of these children, mother's age at their first birth is missing in 1564 and 103 563 observations are missing covariates since not all surveys collect data on our covariates of interest, yielding the final sample of 176 583 children across 55 countries and 118 surveys for our mortality study. The age of the mother is restricted to 12–35 as only 13 of the mothers had their children below the age of 12 and 1716 had their first birth at 36 or older. Details of the samples for the child health outcomes are given in online supplementary appendix table A1. These samples are smaller because the child anthropometric module was not conducted in a number of surveys. The data comprise 119 018 children with stunting, 120 246 with wasting, 122 680 with underweight, 135 121 with diarrhoea and 31 520 with anaemia.
Outcome measures
In this study, we focus on six outcomes: infant mortality, child stunting, underweight, wasting, diarrhoea and moderate to severe anaemia (which is abbreviated to moderate anaemia throughout the paper). All health measures are for children born 12–60 months before the interview. Infant mortality is a measure of whether or not the child survived to age 1 year. The birth history in the DHS individual recode files records the survival status of a woman's (the respondent's) child. A child's death and age at death are reported by the mother. For the measure of infant mortality, we count infants who died within the first year of life (<12 months). We also measure anthropometric failure. First, we calculate a z score given by the child's height minus the median height for that child's age and sex in a reference population. Then we divide the result by the standard deviation of the same age and sex in the WHO reference population of healthy children in developing countries.33 Stunting is defined as a height z score of less than −2. Similarly, underweight is defined as a z score less than −2 for weight relative to children of the same sex and age in the reference population. Wasting is defined as a z score less than −2 for weight-for-height relative to children of the same sex and age in the reference population. Biologically impossible values are defined by the WHO for height (stunting) as z scores <−6 or >6, for weight (underweight) as <−6 or >5 and for weight-for-height (wasting) as <−5 or >5. Observations with biologically impossible values are dropped from our samples.
The outcome of child diarrhoea was based on the mother's recall of whether their child had had diarrhoea within the 2 weeks prior to interview. Anaemia was measured by a fingerstick blood test from the child at the time of interview. The first two drops of blood were discarded and the third drop was taken as a sample. The blood drop was analysed using the HemoCue system. Adjustments for altitude were taken into account, and children with a haemoglobin concentration <10 g/dl were considered as having at least moderate anaemia.
Exposure and covariates
In this study we classify the covariates into four different categories: child characteristics, maternal characteristics, paternal characteristics and, finally, household and social factors. The child characteristics are child sex, singleton or multiple births and the age of the child in months. The covariate for the age of the child is not included in the infant mortality model (which depends only on survival to age 1 year) but is included in all other models. Child age in months is categorised into four groups: 12–23, 24–35, 36–47 and 48–60.
The maternal factors that we include in this study are mother's age, her height and her educational attainment. Our exposure of interest is the mother's age at her first birth. The age of the mother at the first birth is a variable reported in the DHS recode manual30 and is calculated from the CMC (century month code) of the date of the first birth and the CMC of the date of the birth of the mother. Age is categorised into 3-year intervals: ages 12–14, 15–17, 18–20, 21–23, 24–26, 27–29, 30–32 and 33–35. Online supplementary appendix table A2 shows the effect of the age of the mother at first birth, and age squared, regressed on the child health outcomes. This non-linear, continuous age variable model shows that the poor child health outcomes are minimised at age 29 for the infant mortality outcome. However, a quadratic age variable may not capture all potential heterogeneity in the effect of maternal age on child health outcomes. Furthermore, we use maternal age grouped into 3-year intervals, as opposed to single year age groups, due to the small number of infant deaths occurring for single age groups. Grouping 3 years together provides a sufficient group size to minimise random fluctuations in mortality rates. Not all surveys measure women's height. In our main results, we do not control for height but, since maternal height has been shown to be a predictor of child health,3 we do perform a sensitivity analysis where we see the effect of adding maternal height as a covariate and restrict the sample to observations where the mother's height is available. The height of the mother is in five categories: 100–144 cm, 145–149 cm, 150–154 cm, 155–159 cm and 160–200 cm. Maternal education is classified into three categories: no education or less than completed primary, completed primary, and completed secondary or higher. Paternal covariates are whether the women has a partner or not and, if so, the partner's age and educational level. Partners are typically older than the women and the partner's age is split into six categories: 12–17, 18–23, 24–29, 30–35, 36–41 and 42–59 years. Partner's education follows the same groupings as coded for the mother's education: no education or less than completed primary, completed primary, and completed secondary or higher.
Household and social factors include the wealth quintile of the household and whether the household is in a rural or an urban location. The wealth quintile is a within-country measure of the wealth of the household relative to other households in that survey based on its ownership of household assets. This measure of wealth, based on Filmer and Pritchett,34 is a linear index of asset ownership indicators using factor analysis to derive the weights. This measure has been standardised by Measure DHS across most of the DHS and is widely used as a measure of relative wealth within a country. Given we have country fixed effects and year of birth time dummies in the regression analyses, this wealth index is an indicator of how each household's wealth deviates from its own country's mean wealth. We also include indicators for piped water to the house and a flush toilet in the household. In addition to these household measures, we include a cluster level measure: the percentage of living children aged 12–60 months who have received measles vaccination in the cluster. We do not have vaccination data for children who have died and the cluster level measles vaccination percentage allows us to control for neighbourhood health system inputs. The cluster level average may be subject to the ecological fallacy, and we do not claim to measure the causal effect of measles vaccination on vaccinated children. Measles vaccine is administered between 9 and 12 months of age and is likely to have only a limited direct effect on infant mortality (deaths between 0 and 12 months). Rather, we think of vaccine coverage as being a proxy for healthcare provision, although there may also be a herd-immunity effect on younger children due to lower overall prevalence.
Statistical analysis
To measure the RR of a given outcome, we apply a modified Poisson regression following the methodology of Zou.35 We estimate the unadjusted model only controlling for country fixed effects and year of birth time dummies to account for the uneven repeated cross-section. We then estimate the adjusted model and include the covariates. While summary statistics are weighted to take into account the multistage sampling design, the regressions are not weighted.36
Results
Summary statistics
Average age at first birth across the 118 DHS is 20.18. This ranges from an average age of 17.65 in Bangladesh in 1996, to an average of 23.02 in Jordan in 2007 (table 1). Across the 118 surveys included in this study, infant mortality is as high as 17.01% of all first-born children in Mali in 1995. In 30 of the 118 surveys, average stunting is 50% or higher and 79 of the 118 surveys have stunting prevalence of 30% or higher. Madagascar in 1997 has the highest average stunting prevalence with 65.46% of first-born children being classified as stunted according to the WHO standards. Wasting (weight-for-height) is not as prevalent as stunting: 26 of the 118 surveys record an average prevalence of 10% or more. Underweight (weight-for-age) is as high as 50.01% in Niger in 1998. With regard to underweight, 32 of the 118 surveys record a prevalence of 25% or more. An average of 36.91% of first-born children in Niger in 1998 are reported to have had diarrhoea within the 2 weeks prior to the DHS interview, but across the 118 surveys the average is 13.64%. Anaemia was not recorded in all of the surveys, but in the 38 surveys that do record anaemia, average prevalence ranges from a low of 7.99% of first-born children in Egypt in 2000, to 71.55% in Burkina Faso in 2003. The average is 32.6% across the 118 surveys (table 1).
Table 1.
Weighted mean child health outcomes and 95% CIs by survey
| Survey year | Sample size | Age at first birth | Infant mortality |
Stunting |
Wasting |
Underweight |
Diarrhoea |
Anaemia |
|||||||
| N | Mean (SD) | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||
| Armenia | 2000 | 510 | 21.04 (3.61) | 1.51 | 0.77 to 2.93 | 16.17 | 12.27 to 21.00 | 1.40 | 0.55 to 3.56 | 1.02 | 0.38 to 2.65 | 8.53 | 6.20 to 11.63 | 8.29 | 5.92 to 11.49 |
| Armenia | 2005 | 504 | 21.90 (3.15) | 1.47 | 0.51 to 4.15 | 17.19 | 11.07 to 25.72 | 3.12 | 1.63 to 5.88 | 3.57 | 1.96 to 6.41 | 15.60 | 12.00 to 20.05 | 15.78 | 10.21 to 23.57 |
| Azerbaijan | 2006 | 719 | 22.54 (3.97) | 3.11 | 1.73 to 5.55 | 25.32 | 20.80 to 30.45 | 3.93 | 2.31 to 6.61 | 7.40 | 4.81 to 11.21 | 9.79 | 7.00 to 13.53 | 17.82 | 13.55 to 23.07 |
| Bangladesh | 1996 | 1309 | 17.65 (3.24) | 9.60 | 8.11 to 11.33 | 57.25 | 53.52 to 60.89 | 16.80 | 14.37 to 19.53 | 48.81 | 45.41 to 52.22 | 8.13 | 6.43 to 10.23 | ||
| Bangladesh | 1999 | 1596 | 18.20 (3.49) | 9.86 | 8.45 to 11.48 | 56.07 | 52.65 to 59.44 | 10.46 | 8.69 to 12.53 | 40.37 | 37.31 to 43.51 | 6.30 | 5.04 to 7.85 | ||
| Bangladesh | 2004 | 1633 | 18.04 (3.29) | 7.80 | 6.49 to 9.35 | 52.60 | 49.58 to 55.60 | 14.43 | 12.29 to 16.87 | 42.73 | 39.70 to 45.81 | 5.89 | 4.70 to 7.37 | ||
| Bangladesh | 2007 | 1637 | 18.48 (3.35) | 6.14 | 4.82 to 7.79 | 43.55 | 40.14 to 47.01 | 15.12 | 12.90 to 17.64 | 40.91 | 37.40 to 44.52 | 9.98 | 8.24 to 12.03 | ||
| Benin | 1996 | 594 | 19.57 (3.02) | 8.40 | 6.46 to 10.86 | 38.94 | 32.70 to 45.58 | 14.76 | 10.67 to 20.08 | 27.60 | 22.44 to 33.45 | 27.46 | 21.91 to 33.80 | ||
| Benin | 2001 | 781 | 20.25 (3.55) | 8.27 | 6.49 to 10.48 | 40.96 | 36.75 to 45.31 | 7.25 | 5.53 to 9.46 | 21.17 | 17.80 to 24.99 | 14.54 | 11.70 to 17.92 | 55.57 | 49.74 to 61.26 |
| Benin | 2006 | 2112 | 20.42 (3.57) | 7.34 | 6.23 to 8.63 | 45.43 | 42.40 to 48.48 | 5.43 | 4.25 to 6.91 | 17.54 | 15.58 to 19.69 | 9.41 | 8.06 to 10.95 | 48.72 | 44.21 to 53.26 |
| Bolivia | 1993 | 813 | 20.82 (4.05) | 3.36 | 2.29 to 4.90 | 29.95 | 25.21 to 35.16 | 4.17 | 2.47 to 6.96 | 10.60 | 7.75 to 14.34 | 31.69 | 27.25 to 36.50 | ||
| Bolivia | 1998 | 1224 | 20.85 (4.16) | 4.54 | 3.42 to 6.00 | 24.24 | 21.38 to 27.35 | 0.56 | 0.24 to 1.32 | 3.43 | 2.47 to 4.73 | 18.66 | 16.17 to 21.44 | ||
| Bolivia | 2003 | 1987 | 20.48 (4.03) | 3.65 | 2.75 to 4.83 | 26.30 | 23.44 to 29.38 | 0.81 | 0.48 to 1.39 | 2.68 | 1.94 to 3.69 | 22.07 | 19.78 to 24.53 | 22.67 | 18.54 to 27.40 |
| Brazil | 1996 | 1280 | 21.12 (4.53) | 2.15 | 1.48 to 3.13 | 8.76 | 7.11 to 10.73 | 2.43 | 1.48 to 3.96 | 2.60 | 1.76 to 3.82 | 9.62 | 7.96 to 11.58 | ||
| Burkina Faso | 1992 | 771 | 19.12 (2.91) | 12.50 | 10.06 to 15.44 | 45.86 | 41.34 to 50.46 | 15.69 | 12.40 to 19.66 | 33.99 | 29.51 to 38.78 | 12.85 | 10.33 to 15.87 | ||
| Burkina Faso | 1998 | 730 | 19.21 (3.00) | 14.94 | 12.25 to 18.09 | 53.12 | 48.15 to 58.03 | 13.36 | 10.62 to 16.67 | 39.39 | 35.29 to 43.64 | 12.64 | 10.02 to 15.83 | ||
| Burkina Faso | 2003 | 1414 | 19.19 (2.87) | 9.07 | 7.48 to 10.95 | 48.54 | 44.36 to 52.74 | 17.97 | 15.29 to 21.00 | 33.47 | 29.58 to 37.60 | 20.82 | 17.94 to 24.02 | 71.55 | 65.66 to 76.78 |
| Cameroon | 1991 | 498 | 18.62 (3.16) | 6.67 | 4.50 to 9.78 | 35.90 | 29.95 to 42.33 | 4.38 | 2.41 to 7.86 | 16.73 | 11.94 to 22.96 | 12.10 | 8.78 to 16.45 | ||
| Cameroon | 1998 | 542 | 18.87 (3.18) | 7.27 | 5.29 to 9.91 | 43.56 | 37.05 to 50.30 | 4.52 | 2.21 to 9.03 | 17.92 | 12.98 to 24.22 | 20.23 | 15.66 to 25.74 | ||
| Cameroon | 2004 | 1146 | 19.13 (3.45) | 6.26 | 4.90 to 7.97 | 35.95 | 31.39 to 40.79 | 6.20 | 4.23 to 9.00 | 13.57 | 10.26 to 17.73 | 16.99 | 13.40 to 21.29 | 45.37 | 40.19 to 50.65 |
| Central African Rep. | 1994 | 653 | 18.78 (3.44) | 13.62 | 11.25 to 16.41 | 49.09 | 43.70 to 54.50 | 7.51 | 4.83 to 11.48 | 22.06 | 17.35 to 27.62 | 28.00 | 23.40 to 33.12 | ||
| Chad | 1996 | 1030 | 18.30 (2.98) | 12.37 | 10.37 to 14.70 | 50.36 | 46.24 to 54.47 | 13.68 | 11.22 to 16.58 | 33.95 | 30.05 to 38.08 | 21.38 | 18.25 to 24.89 | ||
| Chad | 2004 | 733 | 18.18 (3.09) | 14.00 | 10.86 to 17.85 | 42.26 | 37.35 to 47.34 | 11.23 | 8.51 to 14.68 | 36.86 | 29.66 to 44.69 | 22.83 | 18.16 to 28.29 | ||
| Colombia | 1995 | 1405 | 21.60 (4.43) | 1.58 | 1.05 to 2.38 | 15.73 | 13.68 to 18.01 | 0.92 | 0.50 to 1.68 | 4.54 | 3.42 to 6.01 | 12.44 | 10.75 to 14.35 | ||
| Colombia | 2000 | 1358 | 21.32 (4.70) | 1.85 | 1.26 to 2.70 | 15.38 | 13.06 to 18.03 | 0.49 | 0.22 to 1.09 | 3.19 | 2.21 to 4.59 | 12.77 | 10.94 to 14.85 | ||
| Colombia | 2004 | 3998 | 20.70 (4.49) | 1.04 | 0.75 to 1.44 | 12.36 | 10.92 to 13.96 | 0.85 | 0.59 to 1.24 | 3.15 | 2.50 to 3.98 | 14.14 | 12.63 to 15.79 | ||
| Comoros | 1996 | 234 | 21.20 (4.42) | 6.84 | 4.40 to 10.47 | 47.27 | 37.21 to 57.56 | 10.81 | 6.25 to 18.05 | 19.64 | 12.36 to 29.77 | 16.81 | 10.75 to 25.30 | ||
| Congo, Dem. Rep. | 2007 | 1180 | 19.86 (3.50) | 9.97 | 7.87 to 12.55 | 45.30 | 38.16 to 52.65 | 8.54 | 5.39 to 13.26 | 25.79 | 21.49 to 30.61 | 17.11 | 12.48 to 23.00 | 45.44 | 38.80 to 52.25 |
| Congo, Rep. | 2005 | 940 | 19.66 (3.63) | 8.85 | 6.69 to 11.63 | 36.58 | 31.42 to 42.07 | 5.64 | 3.85 to 8.20 | 12.69 | 9.38 to 16.94 | 13.49 | 10.72 to 16.84 | 34.19 | 27.82 to 41.19 |
| Cote d'Ivoire | 1994 | 927 | 18.28 (3.21) | 11.83 | 9.50 to 14.63 | 45.40 | 40.31 to 50.60 | 8.55 | 6.03 to 12.00 | 24.23 | 19.89 to 29.17 | 17.89 | 14.34 to 22.10 | ||
| Cote d'Ivoire | 1998 | 96 | 18.50 (3.18) | 6.75 | 2.85 to 15.16 | 36.39 | 23.85 to 51.09 | 4.53 | 1.49 to 12.96 | 17.29 | 10.34 to 27.47 | 20.92 | 13.39 to 31.16 | ||
| Dominican Republic | 1996 | 1035 | 20.31 (4.34) | 3.42 | 2.35 to 4.97 | 8.21 | 6.30 to 10.65 | 1.79 | 0.88 to 3.60 | 2.85 | 1.85 to 4.38 | 10.81 | 8.59 to 13.51 | ||
| Dominican Republic | 2002 | 2611 | 19.99 (4.19) | 2.00 | 1.41 to 2.84 | 8.13 | 6.56 to 10.04 | 1.11 | 0.66 to 1.86 | 2.35 | 1.66 to 3.31 | 13.91 | 12.04 to 16.02 | ||
| Dominican Republic | 2007 | 2632 | 20.14 (4.29) | 2.00 | 1.38 to 2.88 | 7.59 | 6.03 to 9.52 | 1.40 | 0.93 to 2.10 | 2.67 | 1.68 to 4.20 | 14.66 | 12.74 to 16.82 | ||
| Dominican Republic | 2007 | 164 | 18.72 (3.27) | 1.99 | 0.58 to 6.52 | 15.18 | 9.25 to 23.93 | 1.08 | 0.27 to 4.28 | 4.03 | 1.85 to 8.55 | 22.09 | 15.04 to 31.24 | ||
| Egypt, Arab Rep. | 1995 | 2136 | 21.41 (3.95) | 4.92 | 3.94 to 6.14 | 30.90 | 27.95 to 34.01 | 3.67 | 2.70 to 4.97 | 7.48 | 6.11 to 9.11 | 13.87 | 12.04 to 15.93 | ||
| Egypt, Arab Rep. | 2000 | 2370 | 21.81 (3.73) | 3.20 | 2.55 to 3.99 | 21.40 | 19.35 to 23.61 | 2.19 | 1.58 to 3.03 | 2.40 | 1.82 to 3.17 | 5.85 | 4.88 to 7.00 | 7.99 | 6.40 to 9.94 |
| Egypt, Arab Rep. | 2003 | 1502 | 21.45 (3.70) | 3.94 | 3.01 to 5.16 | 16.87 | 14.65 to 19.36 | 4.17 | 3.03 to 5.72 | 7.18 | 5.75 to 8.93 | 19.40 | 17.10 to 21.92 | ||
| Egypt, Arab Rep. | 2005 | 3226 | 21.78 (3.69) | 2.53 | 1.99 to 3.21 | 19.10 | 17.35 to 20.97 | 4.15 | 3.29 to 5.23 | 3.39 | 2.72 to 4.21 | 16.20 | 14.67 to 17.86 | 20.08 | 17.18 to 23.32 |
| Egypt, Arab Rep. | 2008 | 2618 | 21.91 (3.72) | 1.88 | 1.41 to 2.51 | 30.29 | 28.01 to 32.67 | 7.28 | 6.05 to 8.73 | 5.26 | 4.31 to 6.39 | 6.63 | 5.66 to 7.74 | ||
| Ethiopia | 2000 | 1689 | 20.09 (3.64) | 11.37 | 9.40 to 13.70 | 58.70 | 54.76 to 62.53 | 9.29 | 7.17 to 11.95 | 37.03 | 33.21 to 41.03 | 22.00 | 18.84 to 25.53 | ||
| Ethiopia | 2005 | 1206 | 19.55 (3.63) | 7.59 | 5.67 to 10.08 | 48.86 | 42.72 to 55.04 | 10.38 | 7.47 to 14.26 | 33.03 | 27.97 to 38.53 | 15.79 | 12.11 to 20.34 | 28.82 | 23.44 to 34.88 |
| Gabon | 2000 | 709 | 18.31 (3.21) | 5.10 | 3.60 to 7.19 | 30.15 | 25.72 to 34.99 | 2.40 | 1.31 to 4.34 | 7.57 | 5.60 to 10.16 | 21.01 | 17.52 to 24.98 | ||
| Ghana | 1993 | 427 | 20.45 (3.51) | 3.04 | 1.75 to 5.24 | 42.36 | 35.78 to 49.22 | 8.70 | 5.69 to 13.07 | 20.09 | 15.52 to 25.58 | 14.10 | 10.22 to 19.15 | ||
| Ghana | 1998 | 531 | 20.72 (3.52) | 4.76 | 3.22 to 6.96 | 33.92 | 29.21 to 38.98 | 7.52 | 5.46 to 10.26 | 20.99 | 17.56 to 24.88 | 16.21 | 13.12 to 19.86 | ||
| Ghana | 2003 | 492 | 20.92 (3.71) | 5.81 | 4.03 to 8.31 | 36.27 | 31.08 to 41.79 | 6.36 | 4.35 to 9.21 | 19.35 | 15.61 to 23.73 | 15.96 | 12.40 to 20.29 | 52.42 | 46.87 to 57.91 |
| Ghana | 2008 | 499 | 21.19 (4.19) | 4.51 | 3.05 to 6.63 | 35.08 | 29.58 to 41.00 | 6.80 | 4.47 to 10.21 | 14.88 | 11.24 to 19.44 | 20.50 | 16.69 to 24.92 | 50.44 | 44.47 to 56.40 |
| Guatemala | 1995 | 1454 | 19.52 (3.67) | 5.38 | 4.15 to 6.95 | 50.10 | 45.63 to 54.57 | 3.90 | 2.75 to 5.52 | 16.96 | 14.31 to 20.00 | 21.36 | 18.19 to 24.92 | ||
| Guinea | 1999 | 743 | 18.32 (3.36) | 10.82 | 8.73 to 13.35 | 37.23 | 32.89 to 41.79 | 6.31 | 4.47 to 8.83 | 19.86 | 16.59 to 23.58 | 22.56 | 19.45 to 26.00 | ||
| Guinea | 2005 | 666 | 18.77 (3.72) | 7.40 | 5.59 to 9.74 | 43.81 | 37.73 to 50.09 | 10.06 | 6.85 to 14.54 | 26.52 | 21.40 to 32.36 | 17.18 | 13.55 to 21.53 | 58.57 | 52.14 to 64.73 |
| Haiti | 1994 | 514 | 21.19 (4.18) | 9.24 | 6.84 to 12.39 | 33.89 | 28.47 to 39.78 | 5.65 | 3.83 to 8.26 | 20.68 | 16.67 to 25.36 | 24.12 | 19.99 to 28.80 | ||
| Haiti | 2005 | 1000 | 21.19 (4.44) | 5.52 | 4.09 to 7.41 | 23.71 | 19.13 to 29.00 | 9.22 | 6.50 to 12.92 | 16.45 | 12.85 to 20.82 | 17.80 | 13.50 to 23.12 | 34.56 | 29.27 to 40.26 |
| Honduras | 2005 | 2390 | 19.70 (3.82) | 1.68 | 1.22 to 2.32 | 23.09 | 20.90 to 25.43 | 1.26 | 0.80 to 1.96 | 6.73 | 5.55 to 8.13 | 15.76 | 14.10 to 17.57 | 12.30 | 10.69 to 14.12 |
| India | 1992 | 12 919 | 19.93 (3.55) | 8.02 | 7.44 to 8.64 | 58.80 | 56.94 to 60.63 | 18.02 | 16.66 to 19.47 | 48.55 | 46.72 to 50.37 | 5.34 | 4.79 to 5.95 | ||
| India | 1998 | 12 763 | 20.12 (3.66) | 7.11 | 6.58 to 7.68 | 52.52 | 50.67 to 54.36 | 15.99 | 14.77 to 17.29 | 41.41 | 39.66 to 43.18 | 17.38 | 16.22 to 18.61 | ||
| India | 2005 | 13 112 | 21.13 (3.86) | 6.27 | 5.71 to 6.87 | 44.60 | 43.17 to 46.04 | 16.23 | 15.25 to 17.26 | 38.76 | 37.35 to 40.18 | 7.60 | 6.97 to 8.30 | 38.38 | 36.96 to 39.81 |
| Jordan | 1990 | 1035 | 21.22 (3.59) | 1.90 | 1.18 to 3.02 | 18.53 | 15.85 to 21.55 | 3.05 | 1.97 to 4.70 | 4.97 | 3.45 to 7.11 | 9.21 | 7.48 to 11.29 | ||
| Jordan | 1997 | 1074 | 22.17 (3.73) | 2.98 | 2.11 to 4.20 | 8.55 | 6.88 to 10.59 | 1.60 | 0.94 to 2.71 | 2.92 | 2.05 to 4.14 | 15.63 | 13.37 to 18.19 | ||
| Jordan | 2007 | 898 | 23.02 (3.90) | 1.83 | 0.77 to 4.30 | 12.20 | 9.05 to 16.26 | 5.89 | 3.66 to 9.35 | 5.23 | 3.55 to 7.64 | 16.98 | 13.21 to 21.55 | 12.29 | 9.25 to 16.16 |
| Kazakhstan | 1995 | 406 | 21.93 (3.62) | 3.68 | 2.17 to 6.20 | 17.89 | 11.91 to 25.99 | 2.59 | 1.07 to 6.14 | 5.77 | 2.97 to 10.91 | 17.56 | 11.77 to 25.39 | ||
| Kazakhstan | 1999 | 395 | 21.99 (3.69) | 4.48 | 2.69 to 7.38 | 12.66 | 8.15 to 19.15 | 2.56 | 0.97 to 6.54 | 3.86 | 1.53 to 9.42 | 17.49 | 13.32 to 22.63 | ||
| Kenya | 1998 | 867 | 19.92 (3.20) | 3.95 | 2.71 to 5.71 | 38.01 | 33.54 to 42.69 | 5.98 | 3.97 to 8.90 | 14.11 | 11.53 to 17.14 | 18.73 | 14.95 to 23.21 | ||
| Kenya | 2003 | 1114 | 19.95 (3.43) | 5.61 | 4.29 to 7.30 | 35.33 | 31.70 to 39.14 | 5.42 | 3.87 to 7.54 | 14.99 | 12.43 to 17.97 | 16.14 | 13.63 to 19.00 | ||
| Kenya | 2008 | 1059 | 19.91 (3.60) | 4.75 | 3.34 to 6.71 | 35.46 | 30.78 to 40.43 | 5.24 | 3.67 to 7.41 | 14.39 | 11.36 to 18.06 | 13.55 | 10.69 to 17.02 | ||
| Kyrgyz Republic | 1997 | 388 | 20.97 (3.14) | 5.05 | 3.22 to 7.83 | 32.43 | 24.30 to 41.77 | 2.02 | 0.73 to 5.49 | 6.77 | 3.51 to 12.64 | 19.38 | 14.01 to 26.20 | ||
| Lesotho | 2004 | 749 | 19.81 (3.24) | 6.82 | 5.09 to 9.09 | 48.43 | 41.99 to 54.93 | 2.81 | 1.50 to 5.18 | 16.97 | 13.00 to 21.84 | 13.53 | 9.92 to 18.19 | 28.47 | 22.99 to 34.65 |
| Liberia | 2006 | 940 | 19.38 (3.52) | 7.12 | 5.23 to 9.63 | 45.57 | 40.86 to 50.35 | 5.85 | 4.08 to 8.32 | 25.72 | 20.96 to 31.13 | 21.03 | 17.16 to 25.50 | ||
| Madagascar | 1997 | 915 | 19.22 (3.94) | 10.61 | 8.51 to 13.14 | 65.46 | 60.10 to 70.45 | 7.12 | 5.03 to 10.00 | 34.37 | 29.41 to 39.70 | 29.95 | 25.50 to 34.81 | ||
| Madagascar | 2003 | 951 | 20.19 (4.40) | 5.36 | 3.70 to 7.69 | 56.18 | 50.85 to 61.36 | 12.83 | 9.76 to 16.70 | 37.42 | 32.05 to 43.13 | 7.33 | 5.31 to 10.05 | 34.48 | 26.54 to 43.39 |
| Madagascar | 2008 | 1887 | 19.11 (3.82) | 4.78 | 3.78 to 6.02 | 44.72 | 40.11 to 49.42 | 9.11 | 6.96 to 11.84 | 14.62 | 11.89 to 17.85 | ||||
| Malawi | 1992 | 564 | 18.84 (2.98) | 17.00 | 13.63 to 20.98 | 64.28 | 58.09 to 70.03 | 6.08 | 3.88 to 9.41 | 22.30 | 17.79 to 27.57 | 11.15 | 8.10 to 15.17 | ||
| Malawi | 2000 | 2121 | 18.95 (2.61) | 13.71 | 12.13 to 15.46 | 62.66 | 59.57 to 65.66 | 4.79 | 3.64 to 6.27 | 22.42 | 19.99 to 25.05 | 16.49 | 14.48 to 18.71 | ||
| Malawi | 2004 | 1872 | 18.80 (2.53) | 8.53 | 7.15 to 10.15 | 58.00 | 54.61 to 61.31 | 5.87 | 4.55 to 7.55 | 18.31 | 15.91 to 20.98 | 21.50 | 18.90 to 24.34 | 39.83 | 34.10 to 45.84 |
| Mali | 1995 | 1042 | 18.48 (3.32) | 17.01 | 14.74 to 19.55 | 48.29 | 42.85 to 53.77 | 23.45 | 19.14 to 28.41 | 39.96 | 34.73 to 45.43 | 25.17 | 20.64 to 30.32 | ||
| Mali | 2001 | 1595 | 18.70 (3.44) | 15.56 | 13.36 to 18.04 | 45.95 | 42.17 to 49.77 | 12.23 | 9.96 to 14.94 | 33.63 | 30.07 to 37.38 | 19.06 | 15.93 to 22.64 | 63.91 | 56.77 to 70.49 |
| Mali | 2006 | 1844 | 18.55 (3.43) | 14.17 | 11.74 to 17.01 | 42.24 | 38.58 to 45.99 | 14.98 | 12.97 to 17.24 | 31.23 | 28.23 to 34.40 | 14.47 | 12.11 to 17.20 | 62.99 | 57.58 to 68.08 |
| Moldova | 2005 | 630 | 22.18 (3.56) | 0.93 | 0.40 to 2.15 | 8.89 | 6.70 to 11.70 | 5.19 | 3.59 to 7.44 | 3.22 | 1.95 to 5.26 | 7.01 | 5.28 to 9.26 | 9.04 | 6.38 to 12.66 |
| Morocco | 1992 | 788 | 22.21 (4.38) | 6.22 | 4.55 to 8.45 | 23.49 | 20.13 to 27.23 | 1.94 | 1.10 to 3.41 | 4.29 | 2.86 to 6.39 | 6.20 | 4.48 to 8.53 | ||
| Morocco | 2003 | 1276 | 22.57 (4.54) | 3.96 | 3.00 to 5.21 | 19.72 | 17.10 to 22.64 | 8.67 | 7.00 to 10.70 | 8.32 | 6.80 to 10.15 | 7.30 | 5.72 to 9.26 | ||
| Mozambique | 1997 | 938 | 18.80 (3.27) | 14.62 | 10.35 to 20.26 | 56.14 | 48.14 to 63.83 | 9.74 | 6.09 to 15.20 | 28.54 | 20.40 to 38.36 | 22.39 | 14.69 to 32.59 | ||
| Mozambique | 2003 | 1679 | 18.73 (3.26) | 11.68 | 9.88 to 13.75 | 51.77 | 47.94 to 55.58 | 4.75 | 3.40 to 6.60 | 21.41 | 18.50 to 24.65 | 14.41 | 12.22 to 16.91 | ||
| Namibia | 1992 | 762 | 20.32 (3.71) | 5.10 | 3.75 to 6.89 | 38.83 | 34.12 to 43.76 | 8.02 | 5.73 to 11.13 | 21.24 | 17.21 to 25.91 | 16.28 | 12.91 to 20.33 | ||
| Namibia | 2000 | 830 | 20.44 (3.83) | 3.05 | 1.95 to 4.72 | 27.82 | 23.92 to 32.10 | 8.74 | 6.18 to 12.22 | 18.69 | 14.28 to 24.08 | 12.63 | 9.55 to 16.53 | ||
| Namibia | 2006 | 1123 | 20.76 (4.00) | 3.31 | 2.44 to 4.50 | 28.69 | 24.81 to 32.90 | 5.96 | 4.41 to 8.02 | 17.92 | 14.58 to 21.84 | 16.00 | 12.96 to 19.59 | ||
| Nicaragua | 1997 | 1633 | 19.06 (3.64) | 3.75 | 2.86 to 4.90 | 25.74 | 23.01 to 28.66 | 2.18 | 1.39 to 3.40 | 8.07 | 6.33 to 10.23 | 12.33 | 10.57 to 14.34 | ||
| Nicaragua | 2001 | 1663 | 19.26 (3.75) | 2.43 | 1.78 to 3.30 | 20.84 | 18.42 to 23.48 | 1.59 | 0.88 to 2.85 | 5.03 | 3.84 to 6.56 | 12.33 | 10.48 to 14.45 | ||
| Niger | 1998 | 871 | 18.16 (3.15) | 16.42 | 13.68 to 19.58 | 56.49 | 50.91 to 61.91 | 24.52 | 19.95 to 29.75 | 50.01 | 44.60 to 55.42 | 36.91 | 31.70 to 42.44 | ||
| Niger | 2006 | 922 | 18.64 (3.42) | 9.45 | 7.42 to 11.96 | 60.64 | 55.35 to 65.69 | 9.47 | 6.85 to 12.95 | 45.40 | 40.09 to 50.81 | 18.74 | 14.93 to 23.26 | 59.43 | 53.08 to 65.49 |
| Nigeria | 1990 | 1023 | 19.80 (3.88) | 7.65 | 5.64 to 10.30 | 55.63 | 51.25 to 59.92 | 13.60 | 8.01 to 22.17 | 38.01 | 32.01 to 44.40 | 10.97 | 8.23 to 14.47 | ||
| Nigeria | 2003 | 850 | 19.82 (3.89) | 10.00 | 7.71 to 12.87 | 46.78 | 40.28 to 53.39 | 9.13 | 6.60 to 12.50 | 31.67 | 26.27 to 37.61 | 16.72 | 13.26 to 20.87 | ||
| Nigeria | 2008 | 3952 | 20.29 (4.24) | 8.17 | 7.26 to 9.19 | 39.08 | 36.76 to 41.46 | 12.00 | 10.61 to 13.53 | 24.74 | 22.65 to 26.96 | 10.41 | 9.20 to 11.77 | ||
| Pakistan | 1990 | 874 | 20.81 (3.88) | 9.97 | 7.64 to 12.90 | 53.38 | 47.78 to 58.89 | 11.52 | 7.41 to 17.49 | 33.03 | 27.96 to 38.54 | 7.11 | 4.90 to 10.21 | ||
| Paraguay | 1990 | 696 | 21.07 (4.21) | 3.09 | 2.02 to 4.69 | 12.87 | 10.24 to 16.06 | 0.34 | 0.07 to 1.55 | 1.83 | 0.98 to 3.38 | 4.93 | 3.27 to 7.35 | ||
| Peru | 1991 | 1747 | 21.13 (4.22) | 2.50 | 1.87 to 3.35 | 30.63 | 27.83 to 33.57 | 1.21 | 0.73 to 1.99 | 6.08 | 4.88 to 7.56 | 7.93 | 6.57 to 9.55 | ||
| Peru | 1996 | 3505 | 20.96 (4.15) | 3.05 | 2.45 to 3.80 | 22.42 | 20.35 to 24.65 | 0.79 | 0.51 to 1.22 | 3.17 | 2.59 to 3.88 | 15.06 | 13.51 to 16.75 | ||
| Peru | 2000 | 3151 | 21.02 (4.33) | 2.21 | 1.70 to 2.87 | 24.09 | 21.85 to 26.48 | 0.68 | 0.41 to 1.13 | 3.20 | 2.50 to 4.08 | 13.78 | 12.30 to 15.41 | 24.96 | 20.76 to 29.70 |
| Peru | 2003 | 2856 | 21.14 (4.44) | 1.57 | 1.11 to 2.24 | 20.19 | 17.77 to 22.84 | 0.71 | 0.35 to 1.43 | 2.24 | 1.70 to 2.94 | 13.72 | 11.85 to 15.82 | 17.32 | 15.22 to 19.64 |
| Rwanda | 1992 | 742 | 21.54 (3.57) | 10.06 | 8.07 to 12.48 | 58.42 | 53.98 to 62.73 | 2.91 | 1.75 to 4.82 | 19.17 | 15.79 to 23.07 | 15.52 | 12.61 to 18.96 | ||
| Rwanda | 2000 | 1209 | 21.34 (3.32) | 10.62 | 8.96 to 12.54 | 52.92 | 49.11 to 56.70 | 5.24 | 3.73 to 7.30 | 17.46 | 14.78 to 20.52 | 15.93 | 13.40 to 18.84 | ||
| Rwanda | 2005 | 979 | 21.54 (3.29) | 8.06 | 6.31 to 10.25 | 54.14 | 49.11 to 59.09 | 5.69 | 3.72 to 8.59 | 21.00 | 17.07 to 25.56 | 16.34 | 12.97 to 20.38 | 35.70 | 30.54 to 41.20 |
| Senegal | 2005 | 1260 | 20.01 (3.91) | 7.09 | 5.61 to 8.93 | 20.13 | 15.29 to 26.04 | 7.46 | 5.05 to 10.88 | 13.98 | 10.29 to 18.71 | 21.26 | 16.65 to 26.74 | 61.98 | 55.64 to 67.94 |
| Sierra Leone | 2008 | 663 | 19.85 (4.03) | 8.06 | 6.08 to 10.61 | 38.25 | 31.56 to 45.41 | 11.82 | 8.30 to 16.57 | 22.17 | 16.99 to 28.39 | 7.80 | 5.15 to 11.64 | 46.22 | 39.35 to 53.23 |
| Swaziland | 2006 | 620 | 19.48 (3.35) | 7.95 | 5.95 to 10.55 | 28.69 | 24.65 to 33.10 | 1.54 | 0.72 to 3.29 | 3.87 | 2.40 to 6.16 | 17.15 | 13.71 to 21.23 | 21.93 | 18.07 to 26.34 |
| Tanzania | 1996 | 1058 | 19.31 (2.81) | 9.38 | 7.62 to 11.50 | 56.50 | 52.22 to 60.69 | 8.52 | 6.43 to 11.20 | 26.25 | 23.01 to 29.77 | 13.45 | 11.13 to 16.17 | ||
| Tanzania | 1999 | 48 | 18.50 (2.84) | 9.86 | 3.92 to 22.69 | 57.16 | 33.20 to 78.17 | 6.31 | 1.43 to 23.83 | 26.88 | 13.03 to 47.41 | 9.32 | 3.45 to 22.82 | ||
| Tanzania | 2004 | 1405 | 19.58 (3.26) | 7.40 | 5.98 to 9.12 | 50.22 | 45.93 to 54.51 | 3.24 | 2.22 to 4.69 | 18.11 | 15.72 to 20.77 | 11.54 | 9.57 to 13.85 | 43.42 | 39.87 to 47.05 |
| Togo | 1998 | 801 | 20.30 (3.60) | 8.27 | 6.47 to 10.53 | 34.67 | 29.09 to 40.70 | 12.53 | 9.28 to 16.70 | 25.71 | 21.19 to 30.81 | 30.18 | 25.94 to 34.79 | ||
| Turkey | 1993 | 949 | 21.16 (3.44) | 4.73 | 3.47 to 6.42 | 17.98 | 15.20 to 21.15 | 1.76 | 1.00 to 3.09 | 6.15 | 4.49 to 8.37 | 14.42 | 12.09 to 17.12 | ||
| Turkey | 1998 | 929 | 21.59 (3.89) | 3.06 | 2.05 to 4.55 | 18.36 | 15.46 to 21.67 | 1.62 | 0.88 to 2.99 | 5.70 | 4.12 to 7.85 | 27.06 | 23.87 to 30.51 | ||
| Uganda | 1995 | 1067 | 18.71 (2.98) | 11.14 | 9.18 to 13.47 | 52.06 | 46.60 to 57.47 | 5.41 | 3.49 to 8.29 | 23.09 | 19.11 to 27.61 | 25.44 | 22.03 to 29.17 | ||
| Uganda | 2000 | 1035 | 18.81 (2.98) | 10.56 | 8.68 to 12.78 | 49.28 | 45.02 to 53.56 | 3.10 | 1.94 to 4.93 | 14.86 | 11.93 to 18.34 | 16.99 | 13.93 to 20.57 | 41.11 | 36.08 to 46.33 |
| Uganda | 2006 | 711 | 19.26 (2.82) | 7.63 | 5.55 to 10.39 | 42.30 | 36.02 to 48.83 | 6.65 | 3.81 to 11.35 | 15.90 | 11.62 to 21.39 | 26.83 | 21.31 to 33.17 | 41.20 | 34.42 to 48.33 |
| Uzbekistan | 1996 | 559 | 20.89 (2.71) | 3.80 | 2.51 to 5.71 | 35.89 | 29.30 to 43.06 | 7.84 | 4.63 to 13.00 | 7.63 | 4.98 to 11.53 | 6.73 | 4.11 to 10.84 | ||
| Zambia | 1996 | 1188 | 18.80 (2.81) | 13.46 | 11.48 to 15.72 | 57.98 | 54.05 to 61.81 | 4.49 | 3.18 to 6.29 | 21.31 | 18.40 to 24.55 | 24.12 | 21.17 to 27.34 | ||
| Zambia | 2001 | 1161 | 18.59 (2.68) | 10.47 | 8.82 to 12.38 | 58.17 | 54.17 to 62.06 | 5.27 | 3.70 to 7.44 | 22.43 | 19.83 to 25.27 | 23.77 | 20.83 to 26.98 | ||
| Zambia | 2007 | 972 | 19.21 (3.12) | 7.44 | 5.85 to 9.42 | 51.39 | 47.22 to 55.54 | 4.36 | 3.03 to 6.24 | 15.44 | 12.74 to 18.59 | 15.66 | 12.98 to 18.78 | ||
| Zimbabwe | 1994 | 719 | 19.53 (3.01) | 5.81 | 4.22 to 7.95 | 31.46 | 25.99 to 37.50 | 7.39 | 4.77 to 11.27 | 14.70 | 10.79 to 19.72 | 25.59 | 20.64 to 31.26 | ||
| Zimbabwe | 2005 | 1261 | 19.87 (3.19) | 5.49 | 4.08 to 7.35 | 33.26 | 30.00 to 36.69 | 6.32 | 4.77 to 8.33 | 12.57 | 10.49 to 14.98 | 13.65 | 11.40 to 16.26 | 29.68 | 25.99 to 33.65 |
| Total | 2000 | 176 583 | 20.18 (3.87) | 6.49 | 6.35 to 6.64 | 36.20 | 35.81 to 36.60 | 7.53 | 7.32 to 7.74 | 19.78 | 19.43 to 20.13 | 13.64 | 13.40 to 13.87 | 32.60 | 31.87 to 33.34 |
In the infant mortality model (n=176 583 children), 23.9% of the women are between the ages of 15 and 17 at their first birth and 35.2% are between the ages of 18 and 20 (table 2). The reference group in the regression analysis is children whose mothers were 27–29 years old at their first birth. This group represents 4.3% of the population with 7648 children. Children of multiple births are rare (0.8%), most women (92.9%) have partners, 60.1% of the children are born in rural areas, 43.6% have piped water to the house (the remainder have to leave the house to collect water) and 30.9% of the children have a flush toilet at the house. Distributions of covariates are similar across the different outcome models (table 2).
Table 2.
Weighted frequency and distribution of first-born children within 5 years of the survey aged 12–60 months across age of mother at birth and other covariates
| Infant mortality |
Stunting |
Underweight | Wasting |
Diarrhoea |
Moderate anaemia |
|||||||
| n=176 583 |
n=119 018 |
n=122 680 |
n=120 246 |
n=135 121 |
n=31 520 |
|||||||
| Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | |
| Age band in years of the mother at first birth | ||||||||||||
| 12–14 | 4497 | 0.026 | 2301 | 0.020 | 2443 | 0.020 | 2379 | 0.020 | 2851 | 0.021 | 514 | 0.016 |
| 15–17 | 42 233 | 0.239 | 25 882 | 0.219 | 26 839 | 0.220 | 26 335 | 0.220 | 30 011 | 0.222 | 6531 | 0.203 |
| 18–20 | 62 091 | 0.352 | 41 492 | 0.351 | 42 868 | 0.352 | 42 054 | 0.352 | 47 425 | 0.351 | 11 753 | 0.366 |
| 21–23 | 37 757 | 0.214 | 26 427 | 0.224 | 27 127 | 0.223 | 26 594 | 0.223 | 29 927 | 0.222 | 7563 | 0.236 |
| 24–26 | 17 383 | 0.099 | 12 669 | 0.107 | 12 936 | 0.106 | 12 690 | 0.106 | 14 258 | 0.106 | 3355 | 0.105 |
| 27–29 | 7648 | 0.043 | 5722 | 0.048 | 5883 | 0.048 | 5771 | 0.048 | 6480 | 0.048 | 1481 | 0.046 |
| 30–32 | 3377 | 0.019 | 2566 | 0.022 | 2616 | 0.022 | 2547 | 0.021 | 2884 | 0.021 | 650 | 0.020 |
| 33–35 | 1399 | 0.008 | 1075 | 0.009 | 1085 | 0.009 | 1075 | 0.009 | 1203 | 0.009 | 249 | 0.008 |
| Sex of child | ||||||||||||
| Male | 90 302 | 0.512 | 59 709 | 0.505 | 61 867 | 0.508 | 60 577 | 0.507 | 68 501 | 0.507 | 16 438 | 0.512 |
| Female | 86 083 | 0.488 | 58 424 | 0.495 | 59 929 | 0.492 | 58 867 | 0.493 | 66 539 | 0.493 | 15 658 | 0.488 |
| Type of birth | ||||||||||||
| Singleton | 174 947 | 0.992 | 117 235 | 0.992 | 120 853 | 0.992 | 118 515 | 0.992 | 134 004 | 0.992 | 31 850 | 0.992 |
| Twin | 1438 | 0.008 | 898 | 0.008 | 944 | 0.008 | 930 | 0.008 | 1036 | 0.008 | 247 | 0.008 |
| Age of child in months | ||||||||||||
| 48–60 | 44 542 | 0.253 | 24 472 | 0.207 | 24 780 | 0.203 | 24 353 | 0.204 | 27 013 | 0.200 | 7552 | 0.235 |
| 36–47 | 42 793 | 0.243 | 26 908 | 0.228 | 27 694 | 0.227 | 27 210 | 0.228 | 31 330 | 0.232 | 7867 | 0.245 |
| 24–35 | 43 082 | 0.244 | 31 485 | 0.267 | 32 603 | 0.268 | 31 950 | 0.267 | 36 595 | 0.271 | 7961 | 0.248 |
| 12–23 | 45 968 | 0.261 | 35 268 | 0.299 | 36 718 | 0.301 | 35 932 | 0.301 | 40 101 | 0.297 | 8717 | 0.272 |
| Educational level of the mother at time of interview | ||||||||||||
| Secondary or higher | 36 152 | 0.205 | 27 729 | 0.235 | 28 308 | 0.232 | 27 757 | 0.232 | 31 177 | 0.231 | 6562 | 0.204 |
| Completed primary | 57 645 | 0.327 | 40 543 | 0.343 | 41 341 | 0.339 | 40 673 | 0.341 | 45 720 | 0.339 | 12 739 | 0.397 |
| No education or incomplete primary | 82 589 | 0.468 | 49 862 | 0.422 | 52 147 | 0.428 | 51 015 | 0.427 | 58 142 | 0.431 | 12 796 | 0.399 |
| Mother has a partner | ||||||||||||
| Yes | 163 858 | 0.929 | 109 350 | 0.926 | 112 890 | 0.927 | 110 666 | 0.927 | 125 468 | 0.929 | 30 192 | 0.941 |
| No | 12 527 | 0.071 | 8784 | 0.074 | 8906 | 0.073 | 8779 | 0.074 | 9572 | 0.071 | 1904 | 0.059 |
| Educational level of the mother's partner at the time of interview | ||||||||||||
| Completed secondary or higher | 54 943 | 0.311 | 39 434 | 0.334 | 40 422 | 0.332 | 39 640 | 0.332 | 44 409 | 0.329 | 8891 | 0.277 |
| Completed primary | 56 655 | 0.321 | 38 884 | 0.329 | 39 920 | 0.328 | 39 216 | 0.328 | 44 217 | 0.327 | 12 180 | 0.379 |
| No education or incomplete primary | 64 787 | 0.367 | 39 815 | 0.337 | 41 455 | 0.340 | 40 589 | 0.340 | 46 414 | 0.344 | 11 025 | 0.344 |
| Age band in years of the mother's partner at the mother's first birth | ||||||||||||
| 12–17 | 2104 | 0.012 | 1224 | 0.010 | 1236 | 0.010 | 1211 | 0.010 | 1409 | 0.010 | 373 | 0.012 |
| 18–23 | 40 271 | 0.228 | 27 180 | 0.230 | 28 018 | 0.230 | 27 483 | 0.230 | 30 594 | 0.227 | 9132 | 0.285 |
| 24–29 | 101 722 | 0.577 | 66 806 | 0.566 | 68 828 | 0.565 | 67 569 | 0.566 | 77 555 | 0.574 | 15 792 | 0.492 |
| 30–35 | 22 072 | 0.125 | 15 954 | 0.135 | 16 483 | 0.135 | 16 125 | 0.135 | 17 661 | 0.131 | 4797 | 0.149 |
| 36–41 | 6768 | 0.038 | 4685 | 0.040 | 4846 | 0.040 | 4724 | 0.040 | 5266 | 0.039 | 1342 | 0.042 |
| 42–59 | 3448 | 0.020 | 2284 | 0.019 | 2385 | 0.020 | 2332 | 0.020 | 2555 | 0.019 | 660 | 0.021 |
| Wealth quintile of the child's household | ||||||||||||
| Richest | 36 825 | 0.209 | 24 886 | 0.211 | 25 377 | 0.208 | 24 876 | 0.208 | 28 741 | 0.213 | 6550 | 0.204 |
| Rich | 37 749 | 0.214 | 25 955 | 0.220 | 26 597 | 0.218 | 26 150 | 0.219 | 29 413 | 0.218 | 6961 | 0.217 |
| Middle | 36 203 | 0.205 | 24 554 | 0.208 | 25 319 | 0.208 | 24 853 | 0.208 | 27 932 | 0.207 | 6795 | 0.212 |
| Poorer | 34 324 | 0.195 | 22 705 | 0.192 | 23 517 | 0.193 | 23 053 | 0.193 | 25 834 | 0.191 | 6138 | 0.191 |
| Poorest | 31 285 | 0.177 | 20 035 | 0.170 | 20 986 | 0.172 | 20 512 | 0.172 | 23 120 | 0.171 | 5653 | 0.176 |
| Residence of the child's household at the time of interview | ||||||||||||
| Urban | 70 395 | 0.399 | 50 428 | 0.427 | 51 491 | 0.423 | 50 597 | 0.424 | 57 358 | 0.425 | 12 301 | 0.383 |
| Rural | 105 990 | 0.601 | 67 706 | 0.573 | 70 305 | 0.577 | 68 848 | 0.576 | 77 682 | 0.575 | 19 796 | 0.617 |
| Water piped to child's house | ||||||||||||
| Piped to house | 76 844 | 0.436 | 55 481 | 0.470 | 56 699 | 0.466 | 55 714 | 0.466 | 62 499 | 0.463 | 14 306 | 0.446 |
| Water not piped to house | 99 542 | 0.564 | 62 653 | 0.530 | 65 097 | 0.534 | 63 731 | 0.534 | 72 542 | 0.537 | 17 790 | 0.554 |
| Flush toilet at child's house | ||||||||||||
| Flush toilet at house | 54 418 | 0.309 | 41 542 | 0.352 | 42 402 | 0.348 | 41 686 | 0.349 | 46 955 | 0.348 | 10 511 | 0.327 |
| No flush toilet at house | 121 968 | 0.691 | 76 592 | 0.648 | 79 394 | 0.652 | 77 759 | 0.651 | 88 085 | 0.652 | 21 586 | 0.673 |
| Child measles vaccination | ||||||||||||
| Cluster weighted mean | 0.234 | 0.204 | 0.208 | 0.208 | 0.214 | 0.211 | ||||||
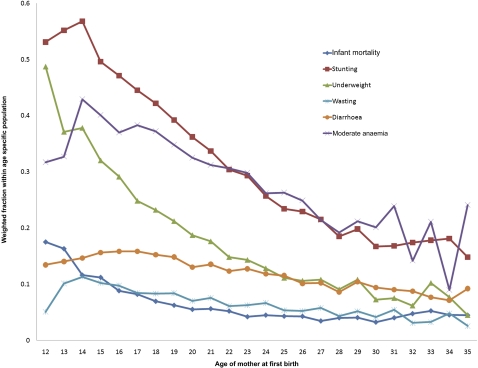
In figure 1 we plot the prevalence of the child health outcome against the age of the mother at first birth. The weighted fraction of child health outcomes by age is an extension of the statistics reported in table 2 of child health outcomes by age band. We see that, in general, the prevalence of poor child health outcomes declines with the mother's age to about age 27. The decline in poor child health outcomes with maternal age is particularly obvious for stunting, anaemia and underweight, but is also evident for diarrhoea, infant mortality and wasting.
Figure 1.
Child health indicator weighted prevalence by age of the mother at first birth.
Older women are more likely to have multiple births, although the event is rare across all age groups. Young mothers are less likely to have a partner: 8.6% of 15–17-year-old mothers do not have a partner compared to 5.8% of women in the 27–29-year-old category (table 3). Young mothers have lower education than older mothers: 64.6% of mothers aged 15–17 had incomplete primary or no schooling, whereas 23.1% of women who had their first birth between the ages of 27 and 29 had only incomplete primary or no schooling (table 3). Older mothers tend to be in a higher wealth quintile: 42.9% of women who had their first birth between the ages of 27 and 29 are in the richest quintile, while 11.7% of mothers age 15–17 are in the richest quintile (table 3). Overall, 71.2% of mothers who had their first birth between the ages of 15 and 17 live in rural areas, while 35% of women who had their first birth between the ages of 27 and 29 live in rural areas (table 3). Delaying first birth is more likely in urban areas. Women who have their first birth later are also more likely to live in conditions that are more sanitary: 57.3% of women who had their first birth between the ages of 27 and 29 have a flush toilet at the house compared to 16.4% of 15–17-year-old first time mothers (table 3).
Table 3.
Weighted frequency and distribution covariates across age of the mother at first birth
| Age band in years | 12–14 |
15–17 |
18–20 |
21–23 |
24–26 |
27–29 |
30–32 |
33–35 |
||||||||
| n=4322 |
n=41 384 |
n=61 491 |
n=38 300 |
n=18 211 |
n=7939 |
n=3493 |
n=1443 |
|||||||||
| Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | Population | Weighted fraction | |
| Sex of child | ||||||||||||||||
| Male | 2323 | 0.517 | 21 627 | 0.512 | 31 995 | 0.515 | 19 017 | 0.504 | 8941 | 0.514 | 3964 | 0.518 | 1731 | 0.513 | 705 | 0.504 |
| Female | 2173 | 0.483 | 20 607 | 0.488 | 30 096 | 0.485 | 18 741 | 0.496 | 8443 | 0.486 | 3685 | 0.482 | 1646 | 0.487 | 694 | 0.496 |
| Type of birth | ||||||||||||||||
| Singleton | 4477 | 0.996 | 42 003 | 0.995 | 61 701 | 0.994 | 37 376 | 0.990 | 17 173 | 0.988 | 7532 | 0.985 | 3317 | 0.982 | 1369 | 0.979 |
| Twin | 19 | 0.004 | 230 | 0.005 | 390 | 0.006 | 382 | 0.010 | 211 | 0.012 | 116 | 0.015 | 60 | 0.018 | 30 | 0.021 |
| Age of child in months | ||||||||||||||||
| 48–60 | 1380 | 0.307 | 11 154 | 0.264 | 15 402 | 0.248 | 9272 | 0.246 | 4269 | 0.246 | 1841 | 0.241 | 890 | 0.263 | 335 | 0.240 |
| 36–47 | 1260 | 0.280 | 10 537 | 0.249 | 14 491 | 0.233 | 9378 | 0.248 | 4176 | 0.240 | 1822 | 0.238 | 822 | 0.243 | 307 | 0.219 |
| 24–35 | 995 | 0.221 | 10 125 | 0.240 | 15 252 | 0.246 | 9419 | 0.249 | 4191 | 0.241 | 1885 | 0.246 | 839 | 0.248 | 376 | 0.269 |
| 12–23 | 862 | 0.192 | 10 418 | 0.247 | 16 946 | 0.273 | 9687 | 0.257 | 4748 | 0.273 | 2100 | 0.275 | 827 | 0.245 | 381 | 0.272 |
| Educational level of the mother at time of interview | ||||||||||||||||
| Secondary or higher | 30 | 0.007 | 1518 | 0.036 | 9263 | 0.149 | 11 213 | 0.297 | 7607 | 0.438 | 3979 | 0.520 | 1836 | 0.544 | 705 | 0.504 |
| Completed primary | 957 | 0.213 | 13 415 | 0.318 | 22 837 | 0.368 | 12 459 | 0.330 | 4961 | 0.285 | 1899 | 0.248 | 781 | 0.231 | 336 | 0.241 |
| No education or incomplete primary | 3509 | 0.780 | 27 300 | 0.646 | 29 991 | 0.483 | 14 085 | 0.373 | 4816 | 0.277 | 1770 | 0.231 | 760 | 0.225 | 357 | 0.256 |
| Mother has a partner | ||||||||||||||||
| Yes | 4101 | 0.912 | 38 606 | 0.914 | 57 623 | 0.928 | 35 469 | 0.939 | 16 378 | 0.942 | 7208 | 0.942 | 3181 | 0.942 | 1291 | 0.923 |
| No | 395 | 0.088 | 3627 | 0.086 | 4468 | 0.072 | 2288 | 0.061 | 1006 | 0.058 | 440 | 0.058 | 196 | 0.058 | 108 | 0.077 |
| Educational level of the mother's partner at the time of interview | ||||||||||||||||
| Completed secondary or higher | 669 | 0.149 | 8265 | 0.196 | 17 087 | 0.275 | 14 040 | 0.372 | 8148 | 0.469 | 4113 | 0.538 | 1876 | 0.556 | 746 | 0.533 |
| Completed primary | 1107 | 0.246 | 12 977 | 0.307 | 21 683 | 0.349 | 12 533 | 0.332 | 5193 | 0.299 | 2031 | 0.266 | 802 | 0.238 | 328 | 0.235 |
| No education or incomplete primary | 2721 | 0.605 | 20 992 | 0.497 | 23 321 | 0.376 | 11 184 | 0.296 | 4042 | 0.233 | 1504 | 0.197 | 699 | 0.207 | 325 | 0.232 |
| Age band in years of the mother's partner at the mother's first birth | ||||||||||||||||
| 12–17 | 313 | 0.070 | 1250 | 0.030 | 407 | 0.007 | 109 | 0.003 | 20 | 0.001 | 4 | 0.001 | 1 | 0.000 | 1 | 0.000 |
| 18–23 | 1587 | 0.353 | 14 655 | 0.347 | 17 407 | 0.280 | 5426 | 0.144 | 898 | 0.052 | 227 | 0.030 | 55 | 0.016 | 17 | 0.012 |
| 24–29 | 2256 | 0.502 | 22 157 | 0.525 | 36 519 | 0.588 | 24 543 | 0.650 | 10 869 | 0.625 | 3671 | 0.480 | 1220 | 0.361 | 487 | 0.348 |
| 30–35 | 214 | 0.048 | 2756 | 0.065 | 5480 | 0.088 | 5634 | 0.149 | 3981 | 0.229 | 2491 | 0.326 | 1203 | 0.356 | 313 | 0.223 |
| 36–41 | 83 | 0.019 | 896 | 0.021 | 1467 | 0.024 | 1319 | 0.035 | 1155 | 0.066 | 848 | 0.111 | 631 | 0.187 | 371 | 0.265 |
| 42–59 | 44 | 0.010 | 520 | 0.012 | 812 | 0.013 | 727 | 0.019 | 461 | 0.027 | 407 | 0.053 | 267 | 0.079 | 211 | 0.151 |
| Wealth quintile of the child's household | ||||||||||||||||
| Richest | 366 | 0.081 | 4937 | 0.117 | 10 572 | 0.170 | 9490 | 0.251 | 6196 | 0.356 | 3283 | 0.429 | 1423 | 0.421 | 557 | 0.398 |
| Rich | 710 | 0.158 | 7659 | 0.181 | 13 466 | 0.217 | 9088 | 0.241 | 3972 | 0.228 | 1700 | 0.222 | 815 | 0.241 | 340 | 0.243 |
| Middle | 950 | 0.211 | 9159 | 0.217 | 13 772 | 0.222 | 7453 | 0.197 | 2950 | 0.170 | 1185 | 0.155 | 517 | 0.153 | 216 | 0.154 |
| Poorer | 1194 | 0.265 | 10 329 | 0.245 | 12 770 | 0.206 | 6330 | 0.168 | 2354 | 0.135 | 838 | 0.110 | 350 | 0.103 | 160 | 0.114 |
| Poorest | 1277 | 0.284 | 10 148 | 0.240 | 11 511 | 0.185 | 5397 | 0.143 | 1911 | 0.110 | 642 | 0.084 | 273 | 0.081 | 126 | 0.090 |
| Residence of the child's household at the time of interview | ||||||||||||||||
| Urban | 1033 | 0.230 | 12 159 | 0.288 | 22 251 | 0.358 | 16 999 | 0.450 | 9721 | 0.559 | 4969 | 0.650 | 2315 | 0.686 | 949 | 0.678 |
| Rural | 3463 | 0.770 | 30 074 | 0.712 | 39 840 | 0.642 | 20 759 | 0.550 | 7663 | 0.441 | 2679 | 0.350 | 1062 | 0.314 | 450 | 0.322 |
| Water piped to child's house | ||||||||||||||||
| Piped to house | 1082 | 0.241 | 13 530 | 0.320 | 25 731 | 0.414 | 18 816 | 0.498 | 9906 | 0.570 | 4736 | 0.619 | 2149 | 0.636 | 896 | 0.640 |
| Water not piped to house | 3415 | 0.759 | 28 704 | 0.680 | 36 360 | 0.586 | 18 942 | 0.502 | 7478 | 0.430 | 2912 | 0.381 | 1228 | 0.364 | 503 | 0.360 |
| Flush toilet at child's house | ||||||||||||||||
| Flush toilet at house | 434 | 0.097 | 6908 | 0.164 | 16 700 | 0.269 | 14 506 | 0.384 | 8551 | 0.492 | 4380 | 0.573 | 2080 | 0.616 | 859 | 0.614 |
| No flush toilet at house | 4062 | 0.903 | 35 325 | 0.836 | 45 390 | 0.731 | 23 251 | 0.616 | 8832 | 0.508 | 3269 | 0.427 | 1297 | 0.384 | 540 | 0.386 |
| Child measles vaccination | ||||||||||||||||
| Cluster weighted mean | 0.359 | 0.298 | 0.238 | 0.202 | 0.166 | 0.145 | 0.125 | 0.139 | ||||||||
Women who delay their first birth are more educated, more likely to have a partner, are richer, more likely to live in an urban area, and more likely to live in better sanitary conditions. Young mothers tend to have lower educational and socioeconomic characteristics. In the following analysis, we present both unadjusted results and results that control for these covariates (table 3).
Unadjusted and adjusted models
The unadjusted pooled results indicate that the risk of infant mortality is lowest for women who have their first birth between the ages of 27 and 29 (online supplementary appendix table A3). The RR ratio declines as age increases between the ages of 12 and 26, and is lowest for 27–29-year-old mothers (table A3). The RR ratio then increases for women who have their first birth at 33–35 years of age (table A3). This same U-shape is exhibited in many of the country-specific unadjusted regressions. Benin, Bolivia, India, Senegal and Tanzania are examples where child survival is maximised if the first birth is delayed to the ages of 27–29, and most countries (38/55) follow this pattern (table A3).
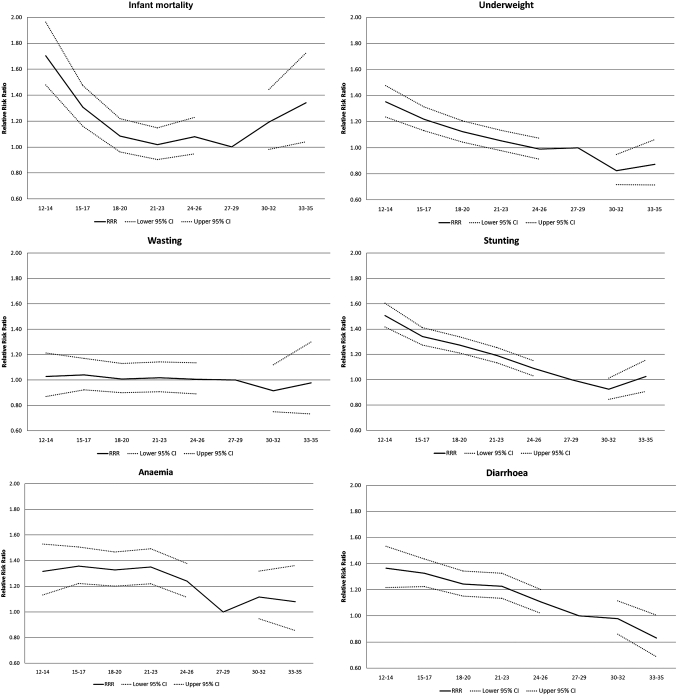
Age of the mother at first birth is a risk factor for infant mortality and adverse child health outcomes in adjusted analysis controlling for maternal, paternal, and household and social characteristics (table 4). The RR ratios of each age group (relative to 27–29 year olds who are the reference group) and 95% CIs are plotted in figure 2. Child health outcomes improve with increasing age of the mother at first birth through to age 27–29 even after controlling for maternal, paternal, household and social factor covariates (table 4, figure 2).
Table 4.
Adjusted RR (95% CI) of infant mortality and child health outcome by age of the mother at first birth
| Infant mortality | Stunting | Underweight | Wasting | Diarrhoea | Moderate anaemia | |
| Age band in years of the mother at first birth | ||||||
| 27–29 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 12–14 | 1.703 (1.478 to 1.962) | 1.507 (1.416 to 1.603) | 1.351 (1.236 to 1.477) | 1.027 (0.870 to 1.211) | 1.365 (1.216 to 1.533) | 1.315 (1.131 to 1.528) |
| 15–17 | 1.307 (1.160 to 1.474) | 1.341 (1.274 to 1.412) | 1.218 (1.131 to 1.313) | 1.040 (0.923 to 1.170) | 1.326 (1.224 to 1.436) | 1.357 (1.222 to 1.507) |
| 18–20 | 1.083 (0.963 to 1.219) | 1.272 (1.210 to 1.338) | 1.122 (1.043 to 1.207) | 1.007 (0.899 to 1.129) | 1.244 (1.151 to 1.343) | 1.327 (1.200 to 1.468) |
| 21–23 | 1.018 (0.903 to 1.148) | 1.191 (1.132 to 1.254) | 1.052 (0.976 to 1.132) | 1.018 (0.908 to 1.141) | 1.227 (1.135 to 1.326) | 1.349 (1.219 to 1.493) |
| 24–26 | 1.079 (0.948 to 1.228) | 1.087 (1.028 to 1.148) | 0.989 (0.912 to 1.071) | 1.004 (0.889 to 1.135) | 1.108 (1.019 to 1.203) | 1.239 (1.114 to 1.378) |
| 30–32 | 1.191 (0.981 to 1.445) | 0.925 (0.845 to 1.013) | 0.824 (0.717 to 0.947) | 0.915 (0.749 to 1.119) | 0.979 (0.860 to 1.115) | 1.117 (0.947 to 1.317) |
| 33–35 | 1.340 (1.041 to 1.725) | 1.025 (0.908 to 1.156) | 0.872 (0.715 to 1.062) | 0.976 (0.733 to 1.299) | 0.831 (0.687 to 1.006) | 1.079 (0.854 to 1.362) |
| Sex of child | ||||||
| Male (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 0.787 (0.759 to 0.815) | 0.900 (0.888 to 0.913) | 0.915 (0.895 to 0.935) | 0.854 (0.821 to 0.889) | 0.927 (0.903 to 0.951) | 0.956 (0.927 to 0.985) |
| Type of birth | ||||||
| Singleton (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Twin | 4.998 (4.609 to 5.421) | 1.302 (1.207 to 1.404) | 1.627 (1.459 to 1.814) | 1.264 (1.018 to 1.570) | 0.918 (0.782 to 1.077) | 1.135 (0.963 to 1.337) |
| Age of child in months | ||||||
| 48–59 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 36–47 | 1.146 (1.119 to 1.174) | 1.023 (0.986 to 1.062) | 0.986 (0.916 to 1.060) | 1.392 (1.311 to 1.477) | 1.219 (1.147 to 1.296) | |
| 24–35 | 1.246 (1.217 to 1.275) | 1.123 (1.083 to 1.164) | 1.145 (1.066 to 1.229) | 2.446 (2.316 to 2.582) | 1.609 (1.513 to 1.711) | |
| 12–23 | 1.169 (1.141 to 1.198) | 1.114 (1.073 to 1.156) | 1.572 (1.466 to 1.686) | 3.818 (3.625 to 4.021) | 2.240 (2.102 to 2.386) | |
| Educational level of the mother at time of interview | ||||||
| Secondary or higher (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Completed primary | 1.266 (1.160 to 1.382) | 1.286 (1.243 to 1.329) | 1.282 (1.214 to 1.354) | 1.022 (0.945 to 1.105) | 1.143 (1.092 to 1.196) | 1.079 (1.009 to 1.154) |
| No education or incomplete primary | 1.626 (1.480 to 1.786) | 1.482 (1.429 to 1.536) | 1.586 (1.495 to 1.681) | 1.243 (1.141 to 1.355) | 1.192 (1.131 to 1.256) | 1.159 (1.075 to 1.248) |
| Mother has a partner | ||||||
| Yes (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 0.977 (0.881 to 1.084) | 1.148 (1.106 to 1.193) | 1.237 (1.158 to 1.322) | 1.232 (1.101 to 1.379) | 1.105 (1.043 to 1.170) | 1.110 (1.022 to 1.206) |
| Educational level of the mother's partner at the time of interview | ||||||
| Higher (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Completed primary | 1.099 (1.027 to 1.176) | 1.068 (1.040 to 1.097) | 1.097 (1.052 to 1.144) | 1.037 (0.969 to 1.109) | 1.059 (1.015 to 1.104) | 1.053 (0.993 to 1.117) |
| No education or incomplete primary | 1.232 (1.147 to 1.324) | 1.131 (1.099 to 1.163) | 1.233 (1.180 to 1.288) | 1.151 (1.070 to 1.238) | 1.068 (1.019 to 1.120) | 1.098 (1.029 to 1.172) |
| Age band in years of the mother's partner at the mother's first birth | ||||||
| 24–29 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 12–17 | 1.410 (1.237 to 1.606) | 1.148 (1.081 to 1.219) | 1.125 (1.017 to 1.245) | 1.008 (0.801 to 1.269) | 1.049 (0.932 to 1.181) | 1.090 (0.937 to 1.269) |
| 18–23 | 1.077 (1.026 to 1.130) | 1.054 (1.035 to 1.073) | 1.026 (0.997 to 1.056) | 0.979 (0.927 to 1.034) | 1.032 (0.997 to 1.068) | 1.050 (1.010 to 1.092) |
| 30–35 | 0.942 (0.884 to 1.005) | 0.964 (0.939 to 0.990) | 0.953 (0.918 to 0.990) | 0.941 (0.882 to 1.004) | 0.958 (0.915 to 1.002) | 0.997 (0.949 to 1.046) |
| 36–41 | 0.996 (0.904 to 1.097) | 0.986 (0.945 to 1.028) | 0.932 (0.875 to 0.992) | 0.929 (0.835 to 1.034) | 1.032 (0.960 to 1.108) | 1.069 (0.994 to 1.149) |
| 42–59 | 1.046 (0.932 to 1.173) | 1.036 (0.983 to 1.093) | 1.030 (0.954 to 1.111) | 0.977 (0.855 to 1.118) | 1.101 (1.004 to 1.207) | 0.962 (0.874 to 1.060) |
| Wealth quintile of the child's household | ||||||
| Richest (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rich | 1.138 (1.063 to 1.219) | 1.182 (1.148 to 1.216) | 1.272 (1.216 to 1.331) | 1.110 (1.032 to 1.194) | 1.171 (1.117 to 1.227) | 1.157 (1.093 to 1.224) |
| Middle | 1.223 (1.136 to 1.316) | 1.257 (1.218 to 1.297) | 1.416 (1.348 to 1.486) | 1.276 (1.176 to 1.384) | 1.209 (1.149 to 1.272) | 1.246 (1.170 to 1.326) |
| Poorer | 1.268 (1.173 to 1.371) | 1.332 (1.289 to 1.376) | 1.524 (1.448 to 1.604) | 1.344 (1.233 to 1.466) | 1.244 (1.177 to 1.314) | 1.287 (1.203 to 1.378) |
| Poorest | 1.289 (1.187 to 1.399) | 1.445 (1.397 to 1.496) | 1.671 (1.585 to 1.762) | 1.458 (1.331 to 1.598) | 1.289 (1.213 to 1.369) | 1.338 (1.245 to 1.438) |
| Residence of the child's household at the time of interview | ||||||
| Urban (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.043 (0.991 to 1.099) | 1.082 (1.059 to 1.106) | 1.029 (0.996 to 1.064) | 0.943 (0.891 to 0.998) | 0.939 (0.905 to 0.974) | 0.981 (0.937 to 1.026) |
| Water piped to the child's house | ||||||
| Piped to house (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Water not piped to house | 1.100 (1.047 to 1.156) | 0.956 (0.938 to 0.975) | 1.031 (1.000 to 1.063) | 1.034 (0.980 to 1.092) | 1.002 (0.969 to 1.037) | 0.988 (0.950 to 1.029) |
| Flush toilet at child's house | ||||||
| Flush toilet at house (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| No flush toilet at house | 1.137 (1.062 to 1.217) | 1.224 (1.191 to 1.259) | 1.137 (1.091 to 1.184) | 1.045 (0.978 to 1.116) | 1.041 (0.997 to 1.087) | 1.035 (0.982 to 1.090) |
| Child measles vaccination | ||||||
| Vaccinated (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Not vaccinated | 1.108 (1.038 to 1.183) | 1.070 (1.042 to 1.100) | 1.164 (1.120 to 1.209) | 1.195 (1.113 to 1.284) | 1.072 (1.020 to 1.127) | 1.109 (1.051 to 1.170) |
| Observations | 176 583 | 119 018 | 122 680 | 120 246 | 135 121 | 31 520 |
Figure 2.
Plot of adjusted RR ratios and 95% CIs as per the results in table 4.
Maternal and paternal age have different effects on child health outcomes (table 4). In the cases of infant mortality, underweight, wasting and anaemia, maternal and paternal age have similar effect sizes, indicating the role of social mechanisms (table 4). In the case of stunting and diarrhoea, while having a very young father increases the RR of poor child health outcomes, the effect is significantly smaller than that of the mother's age, strengthening the case that the effect has a biological component for these two child health outcomes (table 4). There may be concern that the effect of the age of the mother on child health outcomes may be changing over time. Although the year of birth is controlled for, this only controls for year-specific events and not for an interaction between the age of the mother and the year of birth. To explore this possibility, online supplementary table A4 is the same model as that in table 4 but the sample is restricted to surveys between 2000 and 2005. Comparison of results in table A4 and table 4 shows that the effect of the age of the mother on child health is similar across the two samples. This comparison suggests that the effect of age on child health outcomes is not changing over the study period.
The effect of the young age of the mother at first birth on poor child health outcomes reflects a combination of biological and social factors. If the effect were solely social, then we would expect no age gradient for women grouped into high and low socioeconomic status (SES). That is, if all women are of the same SES, then any age gradient reflects the biological mechanism. This hypothesis is explored by stratifying low and high SES. For the high SES group, we select children who have mothers who have completed at least primary school, in households that are in one of the top two wealth quintiles and who live in an urban area (table 5). In contrast, we select the children with mothers who have not completed primary school, are in households that are in the bottom two wealth quintiles and live in a rural area into the low SES group. At the top of table 5 we report the absolute prevalence of the child health outcome by this stratification. In the high SES group, 3.0% of the infants die, while in the low SES households, 10.4% of the infants die (table 5). Stunting, underweight, wasting, diarrhoea and anaemia are all much more prevalent in low SES households than in high SES households (table 5). However, when considering the RR ratios across the age groups for the outcomes of stunting, underweight and diarrhoea, the RR of a poor health outcome for young mothers is higher in the high SES households than in the low SES households (table 5). The difference in the RR of age on these child health outcomes across the two groups indicates that early childbearing is not just a risk factor in lower socioeconomic groups, and that the biological mechanism of young mothers plays a role in determining child health outcomes.
Table 5.
Adjusted RR (95% CI) ratios in high SES and low SES households
| Infant mortality |
Stunting |
Underweight |
Wasting |
Diarrhoea |
Moderate anaemia |
|||||||
| High SES | Low SES | High SES | Low SES | High SES | Low SES | High SES | Low SES | High SES | Low SES | High SES | Low SES | |
| Prevalence (weighted %) | 2.99 | 10.4 | 18.6 | 54.2 | 7.92 | 33.6 | 4.46 | 11.7 | 11 | 15.4 | 21.4 | 42.2 |
| Age band in years of the mother at first birth | ||||||||||||
| 27–29 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 12–14 | 1.757 (1.015 to 3.040) | 1.747 (1.338 to 2.283) | 1.899 (1.473 to 2.449) | 1.244 (1.118 to 1.385) | 1.750 (1.169 to 2.619) | 1.167 (1.004 to 1.355) | 0.875 (0.358 to 2.140) | 1.062 (0.776 to 1.452) | 1.792 (1.229 to 2.612) | 1.342 (1.057 to 1.702) | 0.388 (0.108 to 1.400) | 1.438 (1.047 to 1.974) |
| 15–17 | 1.297 (0.984 to 1.710) | 1.315 (1.029 to 1.681) | 1.474 (1.313 to 1.655) | 1.143 (1.040 to 1.257) | 1.377 (1.147 to 1.654) | 1.066 (0.935 to 1.215) | 1.234 (0.950 to 1.602) | 0.968 (0.744 to 1.258) | 1.377 (1.172 to 1.618) | 1.181 (0.964 to 1.446) | 1.234 (1.001 to 1.521) | 1.504 (1.144 to 1.978) |
| 18–20 | 1.087 (0.846 to 1.398) | 1.104 (0.865 to 1.409) | 1.308 (1.179 to 1.452) | 1.085 (0.987 to 1.192) | 1.260 (1.071 to 1.482) | 0.984 (0.863 to 1.121) | 1.181 (0.951 to 1.467) | 0.964 (0.743 to 1.250) | 1.395 (1.214 to 1.603) | 1.107 (0.905 to 1.354) | 1.154 (0.964 to 1.381) | 1.433 (1.092 to 1.880) |
| 21–23 | 1.020 (0.800 to 1.300) | 1.016 (0.790 to 1.307) | 1.221 (1.102 to 1.352) | 1.065 (0.968 to 1.171) | 1.156 (0.985 to 1.357) | 0.948 (0.830 to 1.084) | 1.198 (0.976 to 1.472) | 0.990 (0.759 to 1.292) | 1.318 (1.152 to 1.508) | 1.126 (0.917 to 1.382) | 1.203 (1.008 to 1.437) | 1.500 (1.141 to 1.972) |
| 24–26 | 1.015 (0.783 to 1.315) | 1.116 (0.848 to 1.470) | 1.083 (0.972 to 1.208) | 0.989 (0.890 to 1.100) | 1.028 (0.871 to 1.215) | 0.941 (0.811 to 1.091) | 1.207 (0.979 to 1.489) | 1.076 (0.811 to 1.428) | 1.206 (1.048 to 1.388) | 1.139 (0.911 to 1.425) | 1.105 (0.925 to 1.320) | 1.424 (1.066 to 1.901) |
| 30–32 | 1.647 (1.183 to 2.291) | 0.710 (0.414 to 1.216) | 0.918 (0.771 to 1.093) | 0.911 (0.760 to 1.093) | 0.875 (0.666 to 1.150) | 0.827 (0.624 to 1.097) | 0.971 (0.697 to 1.351) | 0.832 (0.488 to 1.418) | 0.940 (0.757 to 1.167) | 1.111 (0.777 to 1.590) | 1.151 (0.886 to 1.496) | 1.270 (0.820 to 1.966) |
| 33–35 | 1.407 (0.846 to 2.341) | 0.956 (0.525 to 1.740) | 1.049 (0.822 to 1.338) | 1.222 (1.013 to 1.473) | 0.743 (0.471 to 1.170) | 0.860 (0.594 to 1.245) | 1.128 (0.713 to 1.785) | 0.650 (0.287 to 1.473) | 0.769 (0.555 to 1.065) | 0.821 (0.488 to 1.379) | 1.036 (0.686 to 1.565) | 1.438 (0.826 to 2.502) |
| Sex of child | ||||||||||||
| Male (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 0.700 (0.627 to 0.782) | 0.829 (0.781 to 0.881) | 0.850 (0.814 to 0.888) | 0.929 (0.908 to 0.951) | 0.911 (0.850 to 0.977) | 0.921 (0.890 to 0.954) | 0.886 (0.802 to 0.979) | 0.843 (0.786 to 0.905) | 0.913 (0.859 to 0.969) | 0.959 (0.910 to 1.011) | 0.942 (0.868 to 1.021) | 0.963 (0.910 to 1.019) |
| Type of birth | ||||||||||||
| Singleton (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Twin | 5.439 (4.278 to 6.916) | 4.557 (3.932 to 5.281) | 1.212 (0.991 to 1.482) | 1.271 (1.111 to 1.454) | 1.704 (1.290 to 2.251) | 1.448 (1.179 to 1.778) | 1.365 (0.898 to 2.074) | 1.392 (0.917 to 2.112) | 0.768 (0.533 to 1.106) | 1.015 (0.716 to 1.437) | 1.061 (0.733 to 1.534) | 1.183 (0.860 to 1.627) |
| Age of child in months | ||||||||||||
| Age 48–59 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| 36–47 | 1.239 (1.145 to 1.341) | 1.118 (1.076 to 1.162) | 1.037 (0.919 to 1.170) | 1.037 (0.976 to 1.102) | 0.877 (0.741 to 1.039) | 0.994 (0.868 to 1.138) | 1.410 (1.229 to 1.617) | 1.453 (1.289 to 1.638) | 1.258 (1.064 to 1.487) | 1.219 (1.095 to 1.357) | ||
| 24–35 | 1.415 (1.310 to 1.528) | 1.172 (1.129 to 1.216) | 1.182 (1.049 to 1.331) | 1.142 (1.077 to 1.211) | 0.956 (0.806 to 1.133) | 1.236 (1.086 to 1.408) | 2.466 (2.174 to 2.796) | 2.507 (2.246 to 2.799) | 1.763 (1.493 to 2.081) | 1.469 (1.319 to 1.637) | ||
| 12–23 | 1.392 (1.287 to 1.506) | 1.081 (1.040 to 1.124) | 1.107 (0.977 to 1.254) | 1.151 (1.084 to 1.222) | 1.156 (0.974 to 1.371) | 1.853 (1.632 to 2.104) | 3.891 (3.449 to 4.389) | 3.720 (3.347 to 4.135) | 2.585 (2.163 to 3.090) | 1.927 (1.727 to 2.149) | ||
| Educational level of the mother at time of interview | ||||||||||||
| Secondary or higher (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Completed primary | 1.220 (1.049 to 1.420) | 1.266 (1.191 to 1.346) | 1.208 (1.101 to 1.325) | 1.103 (0.969 to 1.255) | 1.177 (1.085 to 1.277) | 1.099 (0.987 to 1.223) | ||||||
| Mother has a partner | ||||||||||||
| Omitted category: yes | ||||||||||||
| No | 1.012 (0.811 to 1.263) | 0.960 (0.739 to 1.246) | 1.215 (1.108 to 1.332) | 1.038 (0.949 to 1.135) | 1.333 (1.127 to 1.577) | 1.180 (1.012 to 1.377) | 1.249 (0.985 to 1.583) | 1.608 (1.179 to 2.193) | 1.038 (0.926 to 1.163) | 1.223 (1.030 to 1.451) | 1.100 (0.930 to 1.301) | 1.063 (0.814 to 1.388) |
| Educational level of the mother's partner at the time of interview | ||||||||||||
| Secondary or higher (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Completed primary | 1.046 (0.911 to 1.201) | 1.100 (0.902 to 1.341) | 1.115 (1.052 to 1.182) | 0.997 (0.926 to 1.074) | 1.137 (1.041 to 1.242) | 1.056 (0.940 to 1.187) | 0.910 (0.807 to 1.027) | 1.266 (0.994 to 1.613) | 1.071 (0.989 to 1.159) | 0.989 (0.852 to 1.148) | 1.087 (0.979 to 1.208) | 0.987 (0.782 to 1.246) |
| No education or incomplete primary | 1.303 (1.059 to 1.602) | 1.277 (1.059 to 1.540) | 1.206 (1.109 to 1.312) | 1.039 (0.968 to 1.116) | 1.381 (1.218 to 1.566) | 1.224 (1.094 to 1.370) | 1.180 (0.981 to 1.420) | 1.452 (1.149 to 1.834) | 1.209 (1.069 to 1.368) | 1.002 (0.869 to 1.156) | 1.221 (1.043 to 1.428) | 0.974 (0.777 to 1.222) |
| Age band in years of the mother's partner at the mother's first birth | ||||||||||||
| 24–29 (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 12–17 | 1.284 (0.668 to 2.470) | 1.528 (1.261 to 1.851) | 1.010 (0.697 to 1.466) | 1.087 (0.996 to 1.186) | 1.106 (0.627 to 1.952) | 1.085 (0.937 to 1.256) | 0.551 (0.141 to 2.147) | 0.959 (0.672 to 1.368) | 1.206 (0.847 to 1.715) | 1.091 (0.883 to 1.349) | 1.124 (0.664 to 1.901) | 1.005 (0.785 to 1.285) |
| 18–23 | 1.122 (0.948 to 1.327) | 1.090 (1.008 to 1.178) | 1.141 (1.070 to 1.217) | 1.036 (1.006 to 1.068) | 1.072 (0.970 to 1.186) | 1.015 (0.970 to 1.063) | 1.028 (0.872 to 1.211) | 0.977 (0.889 to 1.073) | 0.967 (0.881 to 1.061) | 1.076 (1.006 to 1.149) | 1.069 (0.954 to 1.198) | 1.061 (0.989 to 1.138) |
| 30–35 | 0.907 (0.770 to 1.069) | 0.970 (0.863 to 1.090) | 0.937 (0.875 to 1.004) | 0.964 (0.919 to 1.012) | 0.917 (0.825 to 1.019) | 0.960 (0.898 to 1.026) | 1.012 (0.880 to 1.163) | 0.878 (0.767 to 1.004) | 0.911 (0.831 to 1.000) | 0.990 (0.895 to 1.094) | 0.892 (0.795 to 1.000) | 1.122 (1.027 to 1.226) |
| 36–41 | 0.784 (0.587 to 1.048) | 0.950 (0.797 to 1.132) | 0.962 (0.852 to 1.086) | 1.030 (0.963 to 1.101) | 0.760 (0.614 to 0.940) | 0.970 (0.880 to 1.069) | 1.070 (0.842 to 1.360) | 0.851 (0.701 to 1.034) | 0.994 (0.851 to 1.160) | 0.993 (0.855 to 1.152) | 0.876 (0.715 to 1.074) | 1.180 (1.044 to 1.334) |
| 42–59 | 0.698 (0.413 to 1.178) | 1.100 (0.912 to 1.327) | 1.106 (0.907 to 1.349) | 1.054 (0.973 to 1.141) | 1.119 (0.807 to 1.550) | 0.960 (0.854 to 1.079) | 1.388 (0.940 to 2.052) | 0.885 (0.711 to 1.103) | 0.949 (0.731 to 1.233) | 1.078 (0.909 to 1.280) | 0.910 (0.656 to 1.263) | 1.012 (0.869 to 1.178) |
| Wealth quintile of the child's household | ||||||||||||
| Richest (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Rich | 1.267 (1.111 to 1.445) | 1.223 (1.161 to 1.290) | 1.288 (1.187 to 1.398) | 1.045 (0.926 to 1.180) | 1.143 (1.065 to 1.226) | 1.121 (1.023 to 1.228) | ||||||
| Middle | ||||||||||||
| Poorer | 0.996 (0.938 to 1.057) | 0.936 (0.913 to 0.959) | 0.923 (0.891 to 0.956) | 0.937 (0.870 to 1.008) | 0.957 (0.905 to 1.012) | 0.977 (0.922 to 1.037) | ||||||
| Poorest (reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Water piped to the child's house | ||||||||||||
| Piped to house (reference) | ||||||||||||
| Water not piped to house | 1.066 (0.924 to 1.229) | 1.138 (1.017 to 1.273) | 0.936 (0.883 to 0.993) | 0.964 (0.925 to 1.004) | 1.001 (0.919 to 1.089) | 1.066 (0.995 to 1.142) | 0.991 (0.874 to 1.123) | 1.163 (1.015 to 1.333) | 0.966 (0.884 to 1.055) | 1.065 (0.979 to 1.159) | 0.976 (0.886 to 1.076) | 1.028 (0.933 to 1.133) |
| Flush toilet at child's house | ||||||||||||
| Flush toilet at house (reference) | ||||||||||||
| No flush toilet at house | 0.948 (0.818 to 1.098) | 1.369 (1.075 to 1.745) | 1.158 (1.089 to 1.232) | 1.173 (1.064 to 1.294) | 1.082 (0.988 to 1.185) | 1.239 (1.037 to 1.481) | 1.011 (0.879 to 1.164) | 0.996 (0.753 to 1.318) | 1.088 (0.994 to 1.191) | 1.057 (0.889 to 1.257) | 0.984 (0.872 to 1.110) | 0.982 (0.797 to 1.209) |
| Child measles vaccination | ||||||||||||
| Not vaccinated | 1.653 (1.309 to 2.088) | 1.000 (0.905 to 1.106) | 1.190 (1.072 to 1.320) | 1.066 (1.022 to 1.111) | 1.211 (1.037 to 1.414) | 1.200 (1.130 to 1.275) | 1.229 (0.969 to 1.559) | 1.185 (1.050 to 1.337) | 1.045 (0.907 to 1.204) | 1.030 (0.940 to 1.129) | 1.299 (1.101 to 1.531) | 1.127 (1.035 to 1.228) |
| Observations | 40 299 | 38 612 | 28 797 | 23 657 | 29 345 | 24 846 | 28 783 | 24 251 | 32 809 | 27 435 | 8027 | 6026 |
High SES includes children who are in households that are in the rich or richest wealth quintiles, have mothers with completed primary school or higher, and live in an urban area. Low SES includes children who are in households that are in the poor and poorest wealth quintiles, have mothers with incomplete primary or no education, and live in a rural area.
SES, socioeconomic status.
Sensitivity analysis
Recent work by Subramanian et al2 and Ozaltin et al3 indicates that maternal height is a significant predictor of infant mortality, anthropometric failure and anaemia in India. At the cost of a smaller sample (n=101 054), height is included as a control variable in the regression, in addition to the controls used in the adjusted regressions, to examine whether in the sub-set of countries for which the DHS have data on women's height, the age effect that we observe is confounded by maternal height. Household religion is also included as a control variable as in many low- to middle-income countries religion has a bearing on household decision-making that may include health seeking behaviour. Moreover, religion may influence the autonomy of women to make decisions over the timing of their first birth. Even after controlling for height and religion, the age of the mother at first birth remains a significant risk factor for infant mortality, anthropometric failure and child health outcomes (online supplementary table A5). When height, which is an additional biological covariate, and religion, which is an additional social covariate, are controlled for, the general relationship between the age of the mother at their first birth and child health outcomes persists (table A5).
Discussion
Principal findings
In this paper we show that, controlling for maternal, paternal and household and social factors, there is an improvement in child health outcomes as the age of the mother at first birth increases to age 27–29. This is a much higher age than has been previously reported, where teen pregnancy is emphasised as a risk factor. In the adjusted model, we show that there is an elevated risk of infant mortality in first-born children to mothers below the ages of 27–29, although the effect is only statistically significant for women below age 18. However, the lack of significance may be because cases of infant mortality in our sample are relatively rare, whereas we find that mothers below age 27–29 have elevated and statistically significant risks for stunting, diarrhoea and anaemia outcomes.
Our results indicate that children to mothers below age 27–29 are at higher risk of poor health outcomes. In our sample of low- to middle-income countries, only 7% of women delay their first birth until the age of 27 or older. The USA has seen a steady rise in the average age at first birth from 21 in 1970 to 25 in 2000.37 Age at first birth is increasing in some of our sample countries, but is still lagging behind the level seen in the USA. For example, in the 1993 Bangladesh DHS, the mean age for first births in the last 5 years was 18.2, but in 2007 had risen to 18.5. In Ghana, age for first births increased from a mean of 19.8 in 1988 to 21.2 in 2008. In Tanzania, mean age at first birth increased from 19.2 in 1991 to 19.6 in 2004. Bongaarts found that family planning programs can reduce the child mortality rate by delaying the age at first birth, preventing high parity births and improving birth spacing.38 The results in this paper indicate that delaying the age at first birth even for women in their early 20s reduces infant mortality and improves child health.
Overall, the risk of a poor health outcome dissipates by age 21, but the general trend of improvement continues through to age 27–29. Thus, while the early 20s present a lower risk of a poor child health outcome than a first birth to a teen mother, delaying to the late 20s means that the risk of a poor child health outcome is minimised. Moreover, we find evidence of a paternal age gradient, although it is weaker than the maternal age gradient. This indicates that social mechanisms play some role, but the biological maturity of the mother also helps determine child health outcomes. This finding was also supported by the stratification by low and high SES, where we found that the age gradient was not solely reflecting socioeconomic differences across the ages.
Comparisons to other studies
Consistent with country studies, in this paper we show that delaying first birth beyond the teen years and into the 20s has a positive impact on child survival. While from the 2005–2006 India sample, Raj et al13 found that maternal age only has a significant effect on stunting and underweight, in the current study that applies to 55 low- to middle-income countries, we find that older maternal age has a significant effect on reducing infant mortality, stunting, underweight, diarrhoea and moderate to severe anaemia. The broadening of the significant results to include other child health outcomes results from the inclusion of more countries, and also from a wider time span. As the 2005–2006 India National Family Health Survey-3 is one of the 118 surveys within our current study, the comparison between our study and that of Raj et al13 highlights the fact that generalising across countries does not always reflect each country's experience. Thus we include the country-specific examples in the online supplementary appendix (table A3). Even so, for the case of India in our sample we include three National Family Health Surveys (1992, 1998, 2005–2006). Thus, even the country-specific results may differ from the survey-specific results. Taking a broad view, however, the two papers yield the same fundamental conclusion that delaying first birth beyond the teen years is beneficial for child health outcomes.
The results in this paper also compare to those of Subramanian et al39 which tease out the biological from the socioeconomic predictors of child health outcomes. If being a young mother is associated with low SES in ways we have not controlled for, maternal age at first birth may simply be a proxy for SES. However, if this were true, we would expect the effect of young fathers to be similar to that of mothers (Subramanian et al39 put forward this idea of looking at the differential effects of maternal and paternal indicators on child health as a method of distinguishing between biological and social mechanisms).
Limitations of the study
Although this study provides important insights into the benefits to child health of delaying first birth to age 27–29, there are certain limitations that should be considered when interpreting the results. The primary variable of interest, the age of the mother at first birth, is subject to measurement error as data collection of this variable relies on recall by the respondent. The same holds true for identifying the population of children within the 0–11- and 12–60-month age ranges. We already include the 60-month-old children (which would normally be restricted to 12–59 months) as it is common for the mother to round up in her recall of the child's age. The result is that a larger fraction of children are reported to be 60 months rather than 59 months. As this inconsistency is attributed to recall error, we follow the WHO guidelines and include the 60-month-old children in the child group. For the women's age, we assume that measurement error increases with actual age. Given our concern over young mothers, then the measurement error on the age will be minimised for this group of interest.
A further limitation of the model is that the socioeconomic measures of male and female education, along with the wealth index, may not fully capture the SES of the woman and her child. While we include information about location of residence, piped water to the house and flush toilet, these all serve as proxies for actual SES. Any unobserved wealth captured in the residual will confound the current results. Factors such as actual household income and education quality are such variables that we are unable to control for in the regression and may significantly influence child health outcomes and shape our understanding of the role of SES factors.
Observational studies are subject to the limitation of omitted variables. In this case, there may be variables that are correlated with the age of the mother at birth, but for which we do not control. This would mean that the significance attributed to the age of the mother as a significant correlate of child health outcomes, may in fact be a proxy for other omitted factors. Fixed effects on year of birth are included in both the unadjusted and adjusted regressions to control for common factors in a given year, and secular changes over time. Country fixed effects are also included in the unadjusted and adjusted regressions to control for factors that may be common to women within the same country and are unchanging over time. The covariates control for deviations from the country average and the global time trends in the variables included in the adjusted regressions. However, there may be some factors that are correlated to the explanatory variable of interest that is omitted from the regression. In which case, the regression coefficients have omitted variable bias. Omitted variables correlated to the age of the mother could include place of delivery, trained or untrained birth attendance and breastfeeding.
One of the key outcomes of interest in this study is infant mortality. Infant mortality is aggregated across all causes of death. However, it could be reasonably expected that the age of the mother affects infant mortality outcomes by cause of death. Using a range of child health outcomes in this study, we have illustrated how the age of the mother is differentially (or similarly) related to various outcomes. However, an investigation of the vulnerability to death by, say, pneumonia, diarrhoea, malaria or AIDS, by the age of the mother is beyond the scope of this study as cause of death for children is not recorded in the DHS.
Conclusions and implications
The current study documents that the first-born child of a woman aged <27–29 in low- to middle-income countries, is at a higher risk of infant mortality, stunting, underweight, diarrhoea and moderate to severe anaemia, but not wasting. Children born to women aged 12–14 or 15–17 are significantly more likely to die in their first year of life than children born to women aged 27–29. The risk of stunting, diarrhoea and anaemia diminishes significantly as a woman delays her first birth through to age 27–29, when the risk is minimised. The risk of underweight decreases significantly as a woman delays her first birth and is minimised by age 21. These results offer support to the evidence of the benefits of delaying first birth to offspring. Importantly, beyond just avoiding teen pregnancy, the results in this study show that it is optimal to delay first birth until age 27–29. The results reveal that interventions designed to target adolescents potentially omit a group of women in their early 20s who are also at risk of having children with poor health outcomes. The development of programmes targeting women in general, and not just teen mothers, should provide women and families with the tools to make informed decisions over the timing of their first birth. These programmes can highlight the benefits of delaying the first birth, allowing women to mature biologically, and provide a mechanism for young female family members to improve their knowledge and skills in childcare and family planning, and empowering female autonomy in decision making within the household.
Our results indicated that while the absolute risk of poor child health outcomes is lower when mothers are in a high SES household, there remains a high RR of poor child health outcomes for young mothers even in high SES households. The persistence of the age gradient across the SES groups highlights that child and maternal health issues associated with the age of the mother cut across socioeconomic lines and the children of young rich women are not shielded from the RR of a poor health outcome. This indicates that the biological immaturity of young mothers also affects child health outcomes in addition to the social disadvantage young mothers often face.
When encouraging women to delay their first birth, and encouraging families to permit the delay when the women are not granted autonomy over their reproductive health decisions, this should be accompanied by the provision of viable and valuable alternatives. Education programs aimed at encouraging women to stay in school, take on meaningful employment opportunities, and provide service to the community, relieve the immediacy of the need or desire for childbearing. It also empowers women by demonstrating to themselves and their families that their contribution to society need not only be defined by their reproductive life. By delaying a few years and engaging in other activities the women contribute to society as well as broadening their skills and knowledge to go on to be more informed and better educated mothers. These benefits to the women then trickle down through the generations and benefit their offspring. In this paper, we show what those benefits are in terms of health, but future studies may highlight the educational and social benefits for children if women delay their first birth.
Supplementary Material
Acknowledgments
The authors thank Laura Khan and June Po for their invaluable research assistance in helping with the preparation of the manuscript draft.
Footnotes
To cite: Finlay JE, Özaltin E, Canning D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: evidence from 55 low- and middle-income countries. BMJ Open 2011;2:e000226. doi:10.1136/bmjopen-2011-000226
Funding: We thank the William and Flora Hewlett Foundation for support of this research. Conception of this paper was funded by the Center for Global Development. Researchers operated independently from the funders of this work, and funders neither provided nor were required to provide review and approval of this research.
Competing interests: None.
Ethics approval: The Demographic and Health Surveys data collection procedures were approved by ICF Macro International (Calverton, Maryland, USA) Institutional Review Board as well as by the relevant body in each country which approves research studies on human subjects. Oral informed consent for the interview/survey was obtained from respondents by interviewers. The current study was reviewed by the Harvard School of Public Health Institutional Review Board (Protocol #20069-101) and was ruled exempt from full review because the study was based on an anonymous public use data set with no identifiable information on the survey participants.
Contributors: JEF co-led the conception and interpretation of results in this study. She assisted with drafting the manuscript. She prepared the data, empirical analysis and tables presented in the paper. As guarantor, she accepts full responsibility for this submitted work, had access to the data and controlled the decision to publish. EÖ assisted with conception of the article themes, compilation of the data set and empirical analysis for this study, and critical revision of the paper. DC led the conception of this study and interpretation of study findings as well as assisting with the drafting of the manuscript. All authors have seen and approved the final version of the manuscript.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available on request to Macro ICF at http://www.measuredhs.com/.
References
- 1.United Nations We Can End Poverty 2015: Millennium Development Goals, United Nations, 2011 [Google Scholar]
- 2.Subramanian SV, Ackerson LK, Davey Smith G, et al. Association of maternal height with child mortality, anthropometric failure, and anemia in India. JAMA 2009;301:1691–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozaltin E, Hill K, Subramanian SV. Association of maternal stature with offspring mortality, underweight, and stunting in low- to middle-income countries. JAMA 2010;303:1507–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Temin M, Levine R. Start with a Girl: A New Agenda for Global Health. A Girls Count Report on Adolescent Girls. Washington, DC: Center for Global Development, 2009 [Google Scholar]
- 5.Kembo J, Van Ginneken JK. Determinants of infant and child mortality in Zimbabwe: results of multivariate hazard analysis. Demogr Res 2009;21:367–84 [Google Scholar]
- 6.Knodel J, Herman AT. Effects of birth rank, maternal age, birth interval and sibship on infant and child mortality: Evidence from 18th and 19th Century Reproductive Histories. Am J Public Health 1984;74:1098–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manda SO. Birth intervals, breastfeeding and determinants of childhood mortality in Malawi. Soc Sci Med 1999;48:301–12 [DOI] [PubMed] [Google Scholar]
- 8.Reynolds HW, Wong EL, Tucker H. Adolescents' use of maternal and child health services in developing countries. Int Fam Plann Persp 2006;32:6–16 [DOI] [PubMed] [Google Scholar]
- 9.Villar J, Belizan J. The relative contribution of prematurity and fetal growth retardation to low birth weight in developing and developed societies. Am J Obstet Gynecol 1982;143:793–8 [DOI] [PubMed] [Google Scholar]
- 10.Vitolo MR, Gama CM, Bortolini GA, et al. Some risk factors associated with overweight, stunting and wasting among children under 5 years old. J Pediatr (Rio J) 2008;84:251–7 [DOI] [PubMed] [Google Scholar]
- 11.Wang SC, Lee SH, Lee MC, et al. The effects of age and aboriginality on the incidence of low birth weight in mountain townships of Taiwan. J Public Health (Oxf) 2009;31:406–12 [DOI] [PubMed] [Google Scholar]
- 12.Hobcraft J. Fertility patterns and child survival: a comparative analysis. Popul Bull UN 1992;33:1–31 [PubMed] [Google Scholar]
- 13.Raj A, Saggurti N, Winter M, et al. The effect of maternal child marriage on morbidity and mortality of children under 5 in India: cross sectional study of a nationally representative sample. BMJ 2010;340:b4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trussell J, Hammerslough C. A hazards-model analysis of the covariates of infant and child mortality in Sri Lanka. Demography 1983;20:1–26 [PubMed] [Google Scholar]
- 15.ICF Macro DHS final reports. In: DHS M, ed. Calverton, 2011 [Google Scholar]
- 16.Cooper LG, Leeland NL, Alexander G. Effect of maternal age on birth outcomes among young adolescents. Soc Biol 1995;42:22–35 [DOI] [PubMed] [Google Scholar]
- 17.Fraser AM, Brockert JE, Ward RH. Association of young maternal age with adverse reproductive outcomes. N Engl J Med 1995;332:1113–18 [DOI] [PubMed] [Google Scholar]
- 18.Geronimus AT. On teenage childbearing and neonatal mortality in the United States. Popul Dev Rev 1987;13:245–79 [Google Scholar]
- 19.Geronimus AT, Korenman S, Hillemeier MM. Does young maternal age adversely affect child development? Evidence from cousin comparisons in the United States. Popul Dev Rev 1994;20:585–609 [Google Scholar]
- 20.Horon IL, Strobino DM, MacDonald HM. Birth weights among infants born to adolescent and young adult women. Am J Obstet Gynecol 1983;146:444–9 [DOI] [PubMed] [Google Scholar]
- 21.Trussell J. Teenage pregnancy in the United States. Fam Plann Perspect 1988;20:262–72 [PubMed] [Google Scholar]
- 22.Ventura SJ, Mathews TJ, Hamilton BE. Births to teenagers in the United States, 1940-2000. Natl Vital Stat Rep 2001;49:1–23 [PubMed] [Google Scholar]
- 23.Alam N. Teenage motherhood and infant mortality in Bangladesh: maternal age-dependent effect of parity one. J Biosoc Sci 2000;32:229–36 [DOI] [PubMed] [Google Scholar]
- 24.DHS Demographic and Health Surveys. Calverton, MD: MEASURE DHS, 2009 [Google Scholar]
- 25.Rutstein SO, Rojas G. Guide to DHS Statistics. Calverton, MD: ORC Macro, MEASURE DHS+, 2003 [Google Scholar]
- 26.Wirth ME, Wirth E, Delamonica E, et al. Monitoring Health Equity in the MDGs: A Practical Guide. New York: CIESIN/UNICEF, 2006 [Google Scholar]
- 27.Vaessen M. The potential of the demographic and health surveys (DHS) for the evaluation and monitoring of maternal and child health indicators. In: Khlat M, ed. Demographic Evaluation of Health Programmes (Proceedings). Paris: CICRED/UNFPA, 1996 [Google Scholar]
- 28.Pullum TW. An Assessment of the Quality of Data on Health and Nutrition in the DHS Surveys, 1993-2003. Calverton, MD, USA: Macro International Inc, 2008 [Google Scholar]
- 29.ICF Macro Demographic and health survey interviewer's manual. In: Macro International, ed. Calverton, MD, USA: ICF Macro, 2006 [Google Scholar]
- 30.ICF Macro 2008. Description of the demographic and health surveys individual recode data file. MEASURE DHS Basic Documentation No. 2. Calverton, Maryland, USA: ICF Macro; http://www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1 (accessed 1 Jun 2011). [Google Scholar]
- 31.ICF Macro 2011. Demographic and Health Survey Interviewer's Manual. MEASURE DHS Basic Documentation No. 2. Calverton, Maryland, USA: ICF Macro [Google Scholar]
- 32.ICF Macro Measure DHS biomarkers inventory. In: DHS M, ed. 2011. http://www.measuredhs.com/aboutsurveys/biomarkers/surveys.cfm (accessed 1 Jun 1 2011). [Google Scholar]
- 33.Borghi E, de Onis M, Garza C, et al. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med 2006;25:247–65 [DOI] [PubMed] [Google Scholar]
- 34.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32 [DOI] [PubMed] [Google Scholar]
- 35.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6 [DOI] [PubMed] [Google Scholar]
- 36.Deaton A. The Analysis of Household Surveys: A Microeconometric Approach to Development Policy. Baltimore: World Bank, 1997 [Google Scholar]
- 37.Mathews TJ, Hamilton BE. Mean age of mother, 1970-2000. Natl Vital Stat Rep 2002;51:1–13 [PubMed] [Google Scholar]
- 38.Bongaarts J. Does family planning reduce infant mortality rates? Popul Dev Rev 1987;13:323–34 [Google Scholar]
- 39.Subramanian SV, Ackerson LK, Smith GD. Parental BMI and childhood undernutrition in India: an assessment of intrauterine influence. Pediatrics 2010;126:663–71 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.