Abstract
Ducks play an important role in the maintenance of highly pathogenic H5N1 avian influenza viruses (AIVs) in nature, and the successful control of AIVs in ducks has important implications for the eradication of the disease in poultry and its prevention in humans. The inactivated influenza vaccine is expensive, labor-intensive, and usually needs 2 to 3 weeks to induce protective immunity in ducks. Live attenuated duck enteritis virus (DEV; a herpesvirus) vaccine is used routinely to control lethal DEV infections in many duck-producing areas. Here, we first established a system to generate the DEV vaccine strain by using the transfection of overlapping fosmid DNAs. Using this system, we constructed two recombinant viruses, rDEV-ul41HA and rDEV-us78HA, in which the hemagglutinin (HA) gene of the H5N1 virus A/duck/Anhui/1/06 was inserted and stably maintained within the ul41 gene or between the us7 and us8 genes of the DEV genome. Duck studies indicated that rDEV-us78HA had protective efficacy similar to that of the live DEV vaccine against lethal DEV challenge; importantly, a single dose of 106 PFU of rDEV-us78HA induced complete protection against a lethal H5N1 virus challenge in as little as 3 days postvaccination. The protective efficacy against both lethal DEV and H5N1 challenge provided by rDEV-ul41HA inoculation in ducks was slightly weaker than that provided by rDEV-us78HA. These results demonstrate, for the first time, that recombinant DEV is suitable for use as a bivalent live attenuated vaccine, providing rapid protection against both DEV and H5N1 virus infection in ducks.
INTRODUCTION
The H5N1 highly pathogenic avian influenza viruses (AIVs) have attracted considerable attention as a result of their deadly impact on both animals and humans. To date, H5N1 AIVs have caused disease in more than 60 countries (Office International des Epizooties [OIE]; http://www.oie.int), with human infections being reported in 15 countries (World Health Organization [WHO]; http://www.who.int). Despite substantial efforts to control these outbreaks, H5N1 AIVs have continued to evolve and spread, indicating that the threat they pose to both domestic poultry and public health has not diminished.
Wild waterfowl are considered a natural reservoir for avian influenza viruses (40). Although H5N1 AIV outbreaks in domestic ducks have been documented (OIE; http://www.oie.int) and some of the strains responsible for these outbreaks are lethal to ducks in the laboratory setting (16, 21, 36, 39), most H5N1 strains replicate in ducks asymptomatically. Therefore, AIVs could circulate silently in this host, allowing them to be transmitted to susceptible animals and humans (4). The effective control of H5N1 influenza viruses in ducks thus has important implications for the eradication of H5N1 influenza virus infection in poultry and the prevention of human infections.
In many countries, ducks are bred for their meat, eggs, and down. In China, up to 4 billion ducks are reared annually, often in open fields with no biosecurity measures. Vaccination coverage of H5N1 avian influenza in these ducks (<30%) is much lower than that in chickens (about 70%), and therefore huge numbers of ducks remain susceptible and are serving as reservoirs for H5N1 viruses. The minimal oil adjuvant inactivated vaccine is the only available vaccine for ducks to control H5N1 AIV. This vaccine has several disadvantages, including its cost and the local inflammation and “egg drop” it causes animals exposed to it. Moreover, inactivated vaccine usually needs 2 to 3 weeks to provide solid immune protection (9, 41), which is a major limitation with regard to emergency vaccination to establish a buffer zone. A fast-acting, labor-saving, lower-cost vaccine for ducks is, therefore, still sought after.
Duck viral enteritis, also called duck plague, is an acute contagious disease among Anseriformes (ducks, geese, and swans) (31) that is caused by the duck enteritis virus (DEV), a herpesvirus. Lethal DEV infection can cause 100% mortality in ducks. The DEV genome is approximately 158 kb (20), composed of a unique long (ul) region, a unique short (us) region, a unique short internal repeat (irs) region, and a unique short terminal repeat (trs) region. A live attenuated DEV vaccine has been developed and used to control duck viral enteritis since the 1960s (15, 18), and billions of doses of DEV live vaccines are used in China every year. DEV attenuated live vaccine induces protective immunity within several hours of vaccination (17), and its efficacy appears to be unaffected by maternal antibodies, as is the case with Marek's disease virus-vectored vaccines (29, 37). These features make DEV a highly desirable live virus vector to generate a bivalent vaccine against H5N1 AIVs in ducks.
As with other herpesviruses that have been used successfully to construct recombinant vaccines (22, 29, 37, 38, 42), the large genome of DEV makes it a technically suitable vaccine vector to express the foreign antigen genes of other pathogens. Since the natural host range of DEV is limited to the order Anseriformes (31), its use as a vaccine vector would be safe for other domestic animals and humans. In addition, DEV can establish latency in the trigeminal ganglia, lymphoid tissues, and peripheral blood lymphocytes (33) and can induce long-term humoral and cellular immune responses. A DEV-vectored live vaccine targeted against AIV could help to control infection and prevent the spread of AIV in ducks, and therefore it could be an effective option in the control of AIV transmission to humans. In this study, we first established a system for generating DEV by transfecting overlapping fosmid DNAs and then generated two recombinant DEVs with the hemagglutinin (HA) gene of an H5N1 virus inserted at different sites in the DEV vaccine strain genome. Tests in ducks demonstrated that these DEV-vectored live vaccines were immunogenic and provided solid protection against H5N1 avian influenza and DEV in as little as 3 days postvaccination and completely prevent the replication and shedding of an H5N1 AIV after lethal challenge.
MATERIALS AND METHODS
Viruses and cells.
The virulent DEV and DEV vaccine strains were obtained from the China Veterinary Culture Collection and propagated in primary chicken embryo fibroblasts (CEFs). H5N1 avian influenza viruses A/duck/Hubei/49/05 (HB/49) (clade 2.3.4) and A/duck/Anhui/1/06 (AH/1) (clade 2.3.4) were isolated from ducks in China and have been previously characterized (21, 36). The viruses were propagated in the allantoic cavities of 10-day-old specific-pathogen-free embryonated chicken eggs and kept in a −70°C freezer before RNA extraction or the challenge study.
Construction of the DEV fosmid library.
The DEV vaccine strain was propagated in CEFs and then purified by using 20 to 60% sucrose density gradient centrifugation. DEV DNA was extracted from purified virus as described previously (24) and was used to construct the DEV fosmid library according to the manufacturer's instructions for the CopyControl fosmid library production kit (Epicentre). Briefly, viral DNA was sheared to generate approximately 25- to 50-kb fragments. After blunt treatment and the phosphorylation of the ends, the DNA fragments were separated by using pulsed-field gel electrophoresis and recovered from the agarose gel. Linker fragments with FseI-SbfI-PmeI enzyme digestion sites were introduced at both ends of the DNA fragments, which then were inserted into the cloning-ready fosmid pCC1FOS (Epicentre). The recombinant fosmids were packaged and plated on EPI300-T1 plating cells (Epicentre). The presence of the DNA fragment inserts in these fosmids was confirmed by partial sequencing with a set of specific primers (5′ TAA TAC GAC TCA CTA TAG GG and 5′ GCC AAG CTA TTT AGG TGA GA).
Construction of fosmids with the HA gene insertion.
We constructed an H5 HA gene-expressing cassette. The HA gene was amplified from H5N1 AIV AH/1 by using reverse transcription-PCR (RT-PCR). The cDNA of the HA open reading frame (ORF) was modified to remove four basic amino acids at the cleavage site, as previously described (41). The modified HA gene was introduced into the pSI plasmid (Promega) to form the HA gene-expressing cassette (SV40HA), which included the simian virus 40 (SV40) promoter, the HA ORF, and the SV40 poly(A) signal. The SV40HA cassette then was used to replace the gus gene ORF in the plasmid pENTR-gus (Invitrogen). The resultant plasmid was designated pENTRsv40-HA. The kanamycin resistance gene (KanR) was amplified from pMOD6 (Epicentre) by using PCR and was used to replace the ORF of the chloramphenicol resistance gene (CmR) in the reading frame cassette A (RfA) of the Gateway vector conversion system with One Shot ccdB Survival 2 T1R competent cells (Invitrogen). About 50 nucleotides matching the sequences of different areas of UL41, US7, and US8 of the DEV genome were introduced into the two ends of the cassette (aatR1-KanR-ccdB-aatR2) by using PCR. The resultant cassettes, designated UL41ccdB and US78ccdB, respectively, were inserted into fosmids D and T (Fig. 1A), respectively, by using the CounterSelection BAC modification kit (Gene Bridges) according to the manufacturer's instructions. The resultant recombinant fosmids were designated D-ul41ccdB and T-us78ccdB. To insert the SV40HA cassette into the desired fosmids, the plasmid pENTRsv40-HA was mixed with the fosmid D-ul41ccdB or T-us78ccdB and treated with LR Clonase II enzyme (Invitrogen). The mixtures were transformed into competent Escherichia coli EPI300-T1 cells; only fosmids with the KanR-ccdB sequence replaced by the HA cassette could replicate and be selected in EPI300-T1. The resultant fosmids were designated D-ul41HA and T-us78HA, respectively (Fig. 1 B and C).
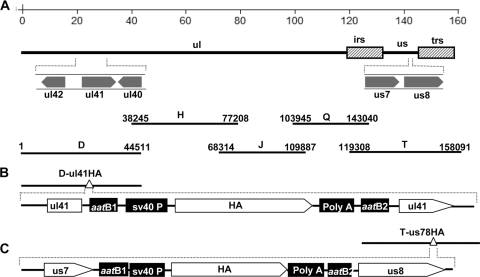
Fig. 1.
Insertion sites for the HA gene in the DEV genome. (A) Genomic structure of DEV and the five fosmid DNAs used for DEV regeneration. Numbers show the location of each fosmid fragment in the DEV genome. (B) Construction of the fosmid with HA inserted within the ul41 gene. (C) Construction of the fosmid with HA inserted between the us7 and us8 genes.
DEV rescue.
Five fosmid combinations, with or without foreign insertions that covered the entire DEV genome, were used for virus rescue. Viral DNA inserts were released from purified fosmids by digestion with SbfI or FseI enzymes and purified by phenol-chloroform extraction and ethanol precipitation. Five micrograms of DNA was used to transfect primary CEFs in 60-mm dishes by using the calcium phosphate procedure described by Morgan et al. (24). Cells were observed for CPE for 7 days after transfection, and CPE-positive samples were harvested for further characterization.
Characterization of rescued DEVs by use of enzyme digestion and Southern blotting.
The genomic DNA of wild-type and rescued DEV was extracted from purified virus as described previously (24). Viral DNA (3 μg) was digested with different enzymes and then separated by using pulsed-field gel electrophoresis. For Southern blotting, 3 μg of purified viral DNA was digested with various enzymes, separated on a 1% agarose Tris-borate EDTA (TBE) gel by using the CHEF Mapper XA pulsed-field electrophoresis system (Bio-Rad), and transferred to nylon membranes. A 500-bp HA gene fragment was amplified, labeled, and hybridized by using the digoxigenin DNA labeling and detection kit (Roche) according to the manufacturer's instructions.
Confirmation of the expression of the H5 HA gene in cells infected with the rDEV-H5HAs.
H5 HA gene expression in the recombinant DEVs was confirmed by using immunofluorescence and Western blotting. For immunofluorescence, CEFs in confocal dishes (35 mm) were infected with the rescued virus at a multiplicity of infection (MOI) of 0.2. The primary antibodies used were specific chicken polyclonal serum against H5N1 AIV or rabbit polyclonal antiserum against the gC of DEV. The secondary antibodies were fluorescein isothiocyanate-conjugated rabbit anti-chicken IgGs (for HA detection) (Sigma) or tetramethyl rhodamine isothiocyanate-conjugated goat anti-rabbit IgGs (for gC detection) (Santa Cruz). Cells were observed with a laser-scanning confocal microscope (Leica). Western blotting was performed as described previously (11). Chicken antiserum, induced by the H5 AIV HA gene DNA vaccine, rabbit polyclonal antiserum against the gC protein of DEV, and mouse monoclonal anti-β-actin antibody (Sigma) were used as primary antibodies; IRDye 700DX-conjugated rabbit anti-chicken IgGs (for HA detection), goat anti-rabbit IgGs (for gC detection), and donkey anti-mouse IgGs (For β-actin detection) (Rockland) were used as secondary antibodies. The cell nuclei were stained with 4′,6-diamidino-2-phenylindole (DAPI).
Stability and growth properties of the rescued viruses.
To evaluate the genetic stability of the foreign gene in the recombinant virus, we passaged the virus in CEFs 20 times. The detection of the inserted gene was carried out by using PCR with a pair of specific primers (5′ GGC TTG GTA GAT TTG AGG C and 5′ TTC CAT CGC AAT GAG TAG G) for rDEV-ul41HA and a pair of specific primers (5′-ACG CAA ATT ATG TCG TTG TT and 5′-TTG AGG TTC CGT AGT CTG G) for rDEV-us78HA. HA expression was confirmed by using an immunofluorescence assay as described above. To investigate the growth property of the recombinant DEVs, cells cultured in 12-well plates were inoculated with different viruses at an MOI of 0.01 and maintained at 37°C in 5% CO2. The cells and supernatants were harvested at different time points and frozen at −80°C. After the cells were thawed at room temperature, the cell debris was removed by using centrifugation and the supernatants were titrated in 96-well plates containing cultured CEFs.
Vaccine efficacy in ducks.
A total of 338 4-week-old specific-pathogen-free (SPF) ducks were used for these studies. Ducks were inoculated intramuscularly with 0.1 ml of serum-free minimum essential medium diluted virus and were challenged with lethal DEV or H5N1 AIV at different time points postvaccination (p.v.). Oropharyngeal and cloacal swabs were collected from H5N1 AIV-challenged ducks on days 3, 5, and 7 postchallenge for virus titration. Ducks also were observed for signs of disease and death for 2 weeks after the challenge. Three ducks in the H5N1 virus-challenged groups were euthanized on day 3 postchallenge, and their organs were harvested for virus titration.
Serologic tests and virus titration.
The neutralization (NT) antibody against DEV was tested in CEFs, and H5N1 hemagglutination inhibition (HI) antibody assays were performed by following the OIE standard (25). The NT antibody against H5N1 influenza was tested in MDCK cells as described previously (19). Each swab was washed in 1 ml of cold phosphate-buffered saline (PBS). One gram of each organ was homogenized in 1 ml of cold PBS, and the solid debris was pelleted by centrifugation and discarded. Virus titration was conducted in 10-day-old SPF embryonated chicken eggs and calculated by the method of Reed and Muench (28).
Laboratory facility.
All experiments related to highly pathogenic AIVs were conducted in a biosecurity level 3 facility approved for such use. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the Ministry of Science and Technology of the People's Republic of China. The protocol was approved by the Committee on the Ethics of Animal Experiments of the Harbin Veterinary Research Institute, Chinese Academy of Agricultural Sciences (approval number JQ-YA-02).
RESULTS
Generation of the DEV vaccine strain from overlapping fosmid DNA.
As described in Materials and Methods, we first generated a DEV fosmid library, from which we selected a total of 21 fosmids with DEV DNA insertions for recombinant virus generation; the size and location of these DNA fragments in the DEV genome are shown in Fig. S1A in the supplemental material. For virus regeneration, we prepared 10 sets, each consisting of four- or five-fosmid combinations that cover the entire genome of DEV (see Fig. S1B), and transfected them into primary CEFs. Among these 10 sets of DNA fragments, the transfection of set 1, set 9, and set 10 resulted in cytopathic effects (CPE) on days 4 to 6 posttransfection (p.t.), reaching 100% on day 7 p.t. (see Fig. S1B); viruses generated from sets 1, 9, and 10 were designated rDEV1, rDEV2, and rDEV3, respectively.
The rescued viruses then were characterized. We digested the purified viral DNA with two different enzymes (EcoRI and BamHI). The digested products then were analyzed by using pulsed-field gel electrophoresis. We found that the rescued rDEVs had DNA fragment separation patterns similar to those of the wild-type parent DEV (see Fig. S2A in the supplemental material). We also evaluated the replication phenotype of the rDEVs in primary CEFs and found that the rDEVs replicated to titers similar to those of wild-type DEV (see Fig. S2B). These results indicate that we, for the first time, successfully rescued the DEV vaccine strain from overlapping fosmid DNA, and that the rescued viruses had a genotype and replication phenotype similar to those of wild-type DEV.
The sizes of the viral genome DNA fragments in fosmids D, H, J, Q, and T (set 10 in Fig.S1A in the supplemental material) are similar (range, 38,783 to 44,511 bp), and virus is easily rescued from this set of DNA fragments. Therefore, we selected the fosmid D+H+J+Q+T combination for further recombinant virus construction (Fig. 1A).
Generation of recombinant DEV expressing the HA gene of H5N1 avian influenza virus.
ul41 and the area between us7 and us8 in other herpesvirus genomes have been identified as being nonessential regions for viral replication and suitable for foreign gene insertion (1, 12). We therefore focused on the genomic regions in ul41 and the area between us7 and us8 for recombinant DEV generation.
We constructed two cassettes, each containing an HA gene of an H5N1 avian influenza virus, A/duck/Anhui/1/06 (21). DNA cassettes 1 and 2 were separately inserted into fosmids D and T, respectively, as described in Materials and Methods. The resultant fosmids were designated fosmid D-ul41HA and fosmid T-us78HA, respectively (Fig. 1B and C).
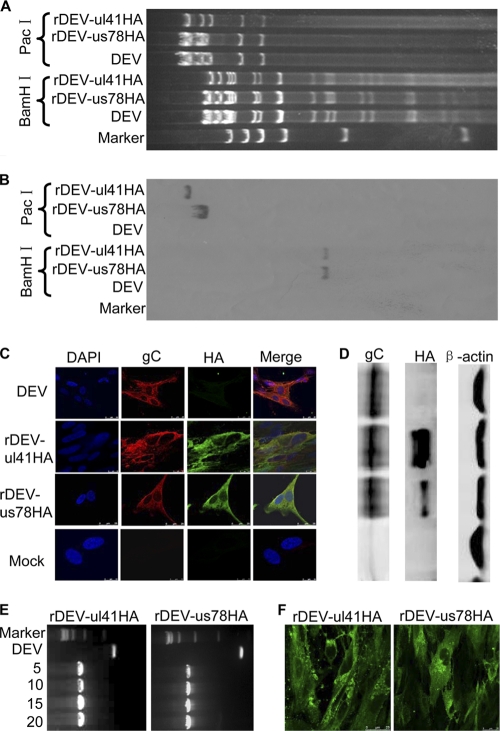
To rescue the DEV with the foreign gene inserted in different areas of the DEV genome, we used the DNA fragments of fosmid D-ul41HA or T-us78HA to replace the DNA fragments in fosmid D or fosmid T in the fragment combination (Fig. 1A) for the transfection. Four to 7 days p.t., CPE was detected in the cells transfected with the DNA combination from fosmid combination D+H+J+Q+T and both sets of fosmid combinations containing the HA insertion. We confirmed the insertion of the HA gene by using enzyme digestion and Southern blotting (Fig. 2 A and B). These results indicate that viruses containing the H5 HA gene within ul41 or between us7 and us8 of DEV were successfully generated. We designated these recombinants rDEV-ul41HA and rDEV-us78HA, respectively.
Fig. 2.
Characterization of the recombinant DEVs with the H5N1 HA gene insertion. (A) DNA patterns of the DEV genome and recombinant DEVs. Purified genomic DNA was digested with the indicated enzymes and then separated by using pulsed-field gel electrophoresis. (B) Southern blotting of recombinant viruses. (C) Detection of HA protein expression in recombinant virus-infected CEFs by using immunofluorescence. (D) Western blotting of recombinant DEV expressing the HA protein of A/duck/Anhui/1/06 (H5N1) virus. (E) Detection of the HA gene insertion in the recombinant viruses. The numbers show the passages of the recombinant viruses. The marker used was DL15000. (F) Detection of HA protein expression in recombinant virus-infected CEFs by using immunofluorescence. The recombinant viruses used were passaged in CEFs for 20 passages.
Characterization of the recombinant DEVs expressing the H5 HA gene.
We next investigated if the inserted HA gene could be expressed in recombinant DEV-infected cells. As expected, cells infected with wild-type DEV did not react with chicken antiserum to the H5 AIV HA protein but reacted with rabbit polyclonal antiserum against the glycoprotein C (gC) of DEV (Fig. 2C). In contrast, cells infected with rDEV-ul41HA and rDEV-us78HA reacted with chicken antiserum to H5 AIV HA protein as well as to the anti-gC antiserum. HA protein expression by the recombinant viruses also was confirmed by Western blotting. The levels of HA protein expression by the two recombinant viruses differed; the HA expression level for rDEV-ul41HA was notably higher than that for rDEV-us78HA (Fig. 2D).
To investigate whether the inserted gene could be stably maintained in the recombinant viruses, we passaged the viruses in CEFs 20 times. The HA gene in both recombinants could be detected by using PCR amplification (Fig. 2E), and its expression in recombinant virus-infected cells still could be confirmed by immunofluorescence after 20 passages (Fig. 2F).
We also tested whether the HA insertion affected the in vitro replication of DEV. Cells and supernatants infected by different viruses were harvested at different time points for titration in 96-well plates containing cultured CEFs. The rDEV-ul41HA and rDEV-us78HA viruses replicated to levels similar to those of the parent DEV virus, indicating that the insertion of the HA gene at these two positions did not affect the replication of the DEV vaccine strain (see Fig. S3 in the supplemental material).
Virulence and immunogenicity evaluation of the recombinant DEVs.
To investigate whether the insertion of the foreign gene influences the virulence of the parent virus, we intramuscularly inoculated groups (n = 10) of 4-week-old SPF ducks with 105 PFU (a recommended dose for DEV vaccine in the field) of wild-type DEV, rDEV, rDEV-ul41HA, and rDEV-us78HA or with PBS as a control. All of the ducks remained healthy, indicating that the insertion of the foreign gene did not increase the virulence of the attenuated DEV vaccine strain.
We then tested the NT antibody titers against DEV from the sera of ducks that were inoculated with the two recombinant DEVs, the wild-type DEV, and PBS. The NT titers of the ducks in the PBS-inoculated group were below 3 log2, the detection limit for infection with DEV virus (25), at all time points tested (Fig. 3). Two of 10 ducks in each of the recombinant virus-inoculated groups and 3 of 10 ducks in the DEV-inoculated group had NT antibody titers greater than 3 log2 at 1 week p.v., and 7 of 10 ducks in all three groups had NT antibody titers greater than 3 log2 at 2 weeks p.v.; however, the titers dropped quickly, and only a few ducks in each of the recombinant DEV- or wild-type DEV-inoculated groups maintained positive NT titers at 3 weeks p.v. (Fig. 3). Although the NT antibody titers were low and short lived, no differences were detected among the virus-inoculated groups, indicating that the insertion of the HA gene did not change the immunogenicity of the parent DEV.
Fig. 3.
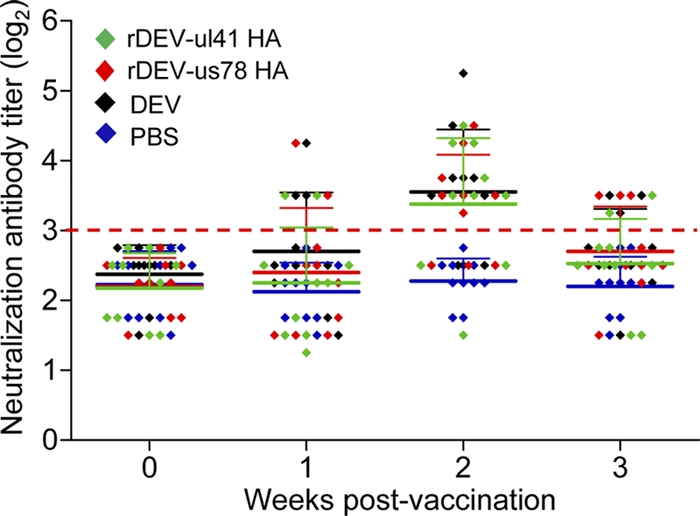
NT antibody response against DEV in ducks inoculated with recombinant or wild-type DEVs. Groups of 10 ducks were inoculated intramuscularly with 105 PFU of rDEV-ul41-HA, rDEV-us78-HA, or wild-type DEV or with PBS as a control. Sera were collected at the indicated time points to detect the NT antibody against DEV in CEFs. The data for week 0 represent the pretest values. The dashed line shows the detection limit for a positive response.
Vaccine efficacy against lethal DEV challenge in ducks.
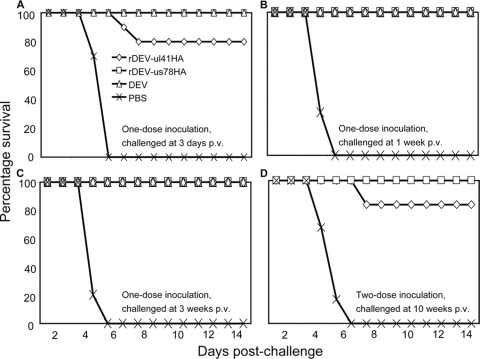
The parent DEV we used here is a live attenuated vaccine strain which rapidly induces protection against lethal DEV challenge in ducks (17). To investigate whether the inserted gene affected the protective efficacy of the parent DEV, ducks were challenged with a 100-fold 50% duck lethal dose (DLD50) of a virulent DEV by intramuscular injection at 3 days, 1 week, and 3 weeks p.v. All of the ducks in the PBS-inoculated control groups showed signs of disease, including listlessness, ruffled feathers, and anorexia, and died within 5 days (Fig. 4 A, B, and C). In contrast, all of the ducks in the groups inoculated with DEV and rDEV-us78HA remained healthy during the 2-week observation period. Two ducks in the group that was vaccinated with rDEV-ul41HA and challenged on day 3 p.v. died during the observation period (Fig. 4A). These results indicate that the recombinant viruses bearing the H5 HA gene insertion have immunogenicity similar to that of the DEV vaccine strain and induced protective immunity against lethal DEV challenge in as little as 3 days p.v., although two ducks died in the rDEV-ul41HA-vaccinated group that was challenged on day 3 p.v.
Fig. 4.
Protective efficacy of the recombinant viruses against lethal DEV challenge. Groups of 6 to 10 ducks were vaccinated intramuscularly with one (A, B, and C) (n = 10) or two doses (D) (n = 6) of the recombinant DEVs and challenged with lethal DEV at 3 days (A), 1 week (B), 3 weeks (C), or 10 weeks (D) postvaccination (p.v.). Ducks were monitored daily for 2 weeks after challenge.
Antibody responses against H5N1 virus induced by recombinant DEVs in ducks.
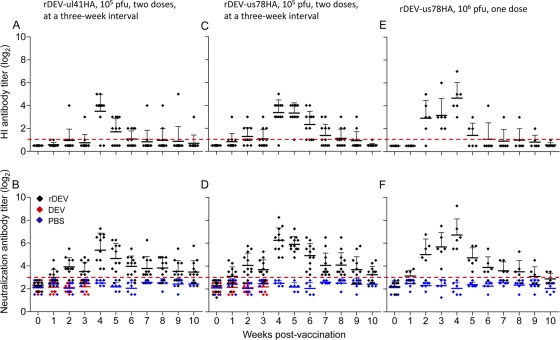
To understand the antibody response induced by the recombinant viruses, groups of 12 ducks were inoculated with two doses, 3 weeks apart, of 105 PFU of rDEV-us78HA or rDEV-ul41HA. We also inoculated a group of six ducks with a single dose of 106 PFU of rDEV-us78HA to investigate whether the antibody response was dose related. Sera from all of the ducks were collected weekly for 10 weeks for HI and NT antibody detection; a group of 12 ducks was inoculated with PBS as a control. As shown in Fig. 5, after one dose of 105 PFU of rDEV-us78HA or rDEV-ul41HA, HI antibody was detected in a limited number of animals 1, 2, and 3 weeks p.v., and the HI antibody titers were dramatically increased in both groups after the second dose (Fig. 5A and C). However, only one and two animals in the rDEV-ul41HA- and rDEV-us78HA-vaccinated groups, respectively, had detectable HI antibodies by the end of week 10 p.v. (Fig. 5A and C). After inoculation with 106 PFU of rDEV-us78HA, HI antibodies were detected in five of six ducks at 2 weeks p.v. and in all six ducks at 3 and 4 weeks p.v. The antibody titers then rapidly declined, and by 10 weeks p.v. only one animal had detectable HI antibody (Fig. 5E). To detect the NT antibody against H5N1 virus, we also included sera that were collected from ducks that were inoculated with 105 PFU of rDEV-us78HA or rDEV-ul41HA. The NT and the HI antibody responses of the ducks in the recombinant vaccine-inoculated groups were similar, although there were more NT antibody-positive ducks than HI antibody-positive ducks at all time points tested. The NT antibody titers of the PBS- and DEV-inoculated ducks all were below 3 log2, which is regarded as negative for infection (Fig. 5B, D, and F). These results indicate that the recombinant DEVs induce a dose-related response in HI and NT antibody titers in ducks and that a second dose boosts antibody titers. However, the duration of the HI antibody response in these ducks is much shorter than that induced in ducks by inactivated H5N1 vaccines (41).
Fig. 5.
Antibody response against H5N1 virus in ducks inoculated with recombinant DEVs. Groups of ducks were inoculated intramuscularly with two doses of 105 PFU of rDEV-ul41-HA (A and B) (n = 12), rDEV-us78-HA (C and D) (n = 12) at a 3-week interval, or one dose of 106 PFU of rDEV-us78HA (E and F) (n = 6). Sera were collected from ducks weekly for HI antibody (A, C, and E) and NT antibody (B, D, and F) detection. The sera of ducks (n = 10) that were inoculated with 105 PFU of DEV also were included for comparison in panels C and D. The data for week 0 represent the pretest values. The dashed lines in A, C, and E show the limits of detection, while the dashed lines in B, D, and F show the detection limits for a positive response.
Vaccine efficacy against lethal H5N1 AIV challenge in ducks.
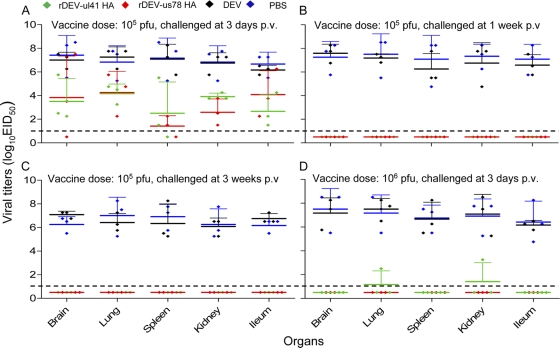
To investigate the protective efficacy of the recombinant viruses against H5N1 virus challenge, groups of 11 ducks were inoculated with 105 PFU of recombinant DEV and challenged with a 100-fold DLD50 of the H5N1 virus, A/duck/Hubei/49/05 (HB/49) (21, 36), intranasally at 3 days, 1 week, or 3 weeks p.v. Three ducks in each group were euthanized on day 3 postchallenge, and their organs were harvested for virus titration in eggs. The remaining eight ducks were observed for virus shedding and signs of deaths for 2 weeks. As shown in Fig. 4, in the DEV- and PBS-inoculated ducks, the challenge H5N1 virus was detected in the lung, kidney, spleen, ileum, and brain, with titers ranging from 4.8 to 8.5 log10 50% egg infectious doses (EID50). Ducks shed virus through both the oropharynx and cloacae and died before day 5 postchallenge (Fig. 6). In the recombinant virus-vaccinated groups that were challenged on day 3 p.v., the challenge virus was detected in multiple organs, but the titers were more than 100-fold lower than those in the control ducks (Fig. 6A). Several of the ducks in this group shed virus and died during the observation period (Table 1). However, in the rDEV-ul41HA- or rDEV-us78HA-inoculated ducks that were challenged at 1 or 3 weeks p.v., the challenge virus was not recovered from any organs tested, and all of the ducks remained healthy and survived the duration of the observation period (Fig. 6B and C and Table 1).
Fig. 6.
H5N1 virus replication in the organs of ducks that were vaccinated with recombinant DEV vaccines. Groups of three ducks were inoculated intramuscularly with 105 PFU (A, B, and C) or 106 PFU (D) of the recombinant DEVs or wild-type DEV or with PBS as a control. They then were challenged with the lethal H5N1 virus HB/49 intranasally at 3 days (A and D), 1 week (B), or 3 weeks (C) postvaccination. Three days after challenge, the ducks were euthanized and their organs were harvested for virus titration in eggs. The dashed lines show the limits of detection.
Table 1.
Protective efficacy of recombinant DEV vaccines against H5N1 lethal virus HB/49 challenge in ducksa
| Challenge time p.v. | Vaccine | Dose (PFU) | No. HI antibody positive/totalb (mean titer, log2) | No. of swabs showing shedding virus/total no. (titer in log10EID50/ml) on day p.c.c: |
No. surviving/ total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3 |
5 |
7 |
||||||||
| Oropharyngeal | Cloacal | Oropharyngeal | Cloacal | Oropharyngeal | Cloacal | |||||
| 3 Days | rDEV-ul41HA | 105 | 0/11 | 3/8 (2.5 ± 1.5) | 3/8 (2.3 ± 1.1) | 1/6 (1.3) | 0/6 | 0/5 | 0/5 | 5/8 |
| rDEV-us78HA | 105 | 0/11 | 3/8 (1.9 ± 1.2) | 1/8 (1.3) | 0/6 | 0/6 | 0/6 | 0/6 | 6/8 | |
| DEV | 105 | 0/11 | 8/8 (2.9 ± 1.4) | 8/8 (2.4 ± 0.9) | / | / | / | / | 0/8 | |
| PBS | 0/11 | 8/8 (3.1 ± 1.3) | 6/8 (1.9 ± 0.6) | / | / | / | / | 0/8 | ||
| 1 wk | rDEV-ul41HA | 105 | 3/11 (1.3) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 |
| rDEV-us78HA | 105 | 3/11 (2.6) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 | |
| DEV | 105 | 0/11 | 8/8 (4 ± 0.5) | 8/8 (3.3 ± 0.4) | 1/1 (3.5) | 1/1 (2.3) | / | / | 0/8 | |
| PBS | 0/11 | 8/8 (3.1 ± 0.6) | 8/8 (3.0 ± 0.5) | / | / | / | / | 0/8 | ||
| 3 wk | rDEV-ul41HA | 105 | 3/11 (1.6) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 |
| rDEV-us78HA | 105 | 4/11 (1.7) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 | |
| DEV | 105 | 0/11 | 8/8 (3.5 ± 1.6) | 7/8 (2.7 ± 1.5) | / | / | / | / | 0/8 | |
| PBS | 0/11 | 8/8 (3.3 ± 0.8) | 8/8 (2.8 ± 0.5) | 2/2 (3.1 ± 0.5) | 2/2 (1.9 ± 0.9) | / | / | 0/8 | ||
| 3 Days | rDEV-ul41HA | 106 | 0/11 | 1/8 (1.8) | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 |
| rDEV-us78HA | 106 | 0/11 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 0/8 | 8/8 | |
| DEV | 106 | 0/11 | 8/8 (2.1 ± 0.6) | 6/8 (1.5 ± 1.5) | 2/2 (2.9 ± 0.9) | 2/2 (2.1 ± 0.6) | / | / | 0/8 | |
| PBS | 0/11 | 8/8 (3.2 ± 1.2) | 6/8 (2.2 ± 0.6) | / | / | / | / | 0/8 | ||
| 10 wk | rDEV-ul41HA | 105d | 1/6 (3) | 1/6 (1.5) | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 6/6 |
| rDEV-us78HA | 105d | 2/6 (1) | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 6/6 | |
| rDEV-us78HA | 106 | 1/6 (1) | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 6/6 | |
| PBS | 0/6 | 6/6 (3.3 ± 1.7) | 6/6 (2.6 ± 0.9) | / | / | / | / | 0/6 | ||
Four-week-old specific-pathogen-free ducks were used in these studies. The ducks were intramuscularly injected with one or two doses of DEV or recombinant DEVs as indicated or with PBS as a control (p.v. indicates postvaccination). They then were challenged intranasally with 100-fold DLD50 of the H5N1 virus HB/49 at different time points. Three ducks in each group, excluding those that were challenged at 10 weeks p.v., were euthanized on day 3 postchallenge (p.c.) to test for viral replication in organs (Fig. 4), and the remaining ducks in each group were monitored for virus shedding and death for 2 weeks.
Sera were collected from all ducks before challenge, and HI antibody titers were determined by using 0.5% chicken red blood cells. The titers shown are the means for the ducks that had detectable HI antibodies.
Swabs were collected from all of the available ducks on days 3, 5, or 7 p.c. for virus titration in eggs. The titer shown is the means ± standard deviations for the ducks that shed viruses. A backslash indicates that the animals had died by that time point.
Ducks were vaccinated with two doses of 105 PFU of the indicated recombinant DEVs at a 3-week interval.
These results indicate that 105 PFU of recombinant DEV can induce partial protection against lethal H5N1 virus challenge in as little as 3 days p.v. We then investigated whether a higher dose could induce better protection. Groups of 11 ducks were inoculated with 106 PFU of the two recombinant DEVs, wild-type DEV, and PBS as a control and were challenged 3 days p.v. with 100 DLD50 of HB/49. The challenge H5N1 virus was not detected in any organs tested in the ducks that were vaccinated with rDEV-us78HA, and only low titers of challenge H5N1 virus were recovered from the lungs and kidneys of ducks that were vaccinated with rDEV-ul41HA (Fig. 6D). All of the ducks in both groups remained healthy and survived the duration of the 2-week observation period, although virus shedding was detected from the oropharyngeal swab of one duck in the rDEV-ul41HA-vaccinated group (Table 1). In the DEV- and PBS-inoculated groups, the H5N1 virus replicated to high titers in all organs tested (Fig. 6D); the ducks shed virus from their oropharynx and cloacae and died within 5 days postchallenge (Table 1).
We also challenged the ducks that were previously used to monitor the antibody duration (shown in Fig. 5) with lethal DEV or H5N1 HB/49 virus at 10 weeks p.v. As shown in Fig. 4D, after challenge with lethal DEV, the ducks that received two doses of 105 PFU of rDEV-us78HA were completely protected, whereas one of the six ducks in the rDEV-ul41HA-inoculated group and all six ducks in the PBS-inoculated group died within the 2-week observation period. After challenge with the H5N1 virus, all of the birds in the recombinant virus-inoculated groups remained healthy and survived the duration of the 2-week observation period, although virus shedding was detected from one duck in the group that was vaccinated with two doses of 105 PFU of rDEV-ul41HA. All ducks in the PBS-inoculated groups shed virus and died within 4 days of challenge (Table 1).
These studies indicate that recombinant DEVs expressing the H5N1 HA can induce protective immunity in ducks against H5N1 virus challenge and offer protection against challenge with lethal DEV. Although both the rDEV-ul41HA and the rDEV-us78HA viruses have similar replication phenotypes in CEFs and HA protein expression in rDEV-ul41HA-infected cells was notably higher than that in rDEV-us78HA-infected cells, it appears that rDEV-us78HA provided better protection against both DEV and H5N1 virus challenge than did rDEV-ul41HA. The protection against the lethal DEV and H5N1 virus challenge was independent of the antibody levels in ducks.
DISCUSSION
We established a system to regenerate a DEV vaccine strain by using the transfection of overlapping fosmid DNAs. The rescued virus maintained replication and immunogenic properties that were similar to those of the parent DEV strain. We further generated two recombinant DEVs, rDEV-ul41HA and rDEV-us78HA, by inserting the HA gene of an H5N1 AIV at different positions in the DEV vaccine strain genome. The HA protein was stably expressed in both recombinant virus-infected cells. The insertion of this foreign gene at these two sites in the genome did not affect the replication phenotype of DEV in cell culture and did not increase the virulence of the DEV vaccine strain in ducks. Animal studies in ducks showed that both rDEV-ul41HA and rDEV-us78HA were immunogenic, providing solid protection against challenge with lethal DEV and with an H5N1 virus. More importantly, rDEV-us78HA induced full protection against challenge with an H5N1 virus and completely prevented the H5N1 virus from replicating and shedding within 3 days of vaccination. These results demonstrate the immense value of a DEV-vectored live bivalent vaccine in the control and eradication of H5N1 virus in ducks, a large and important reservoir for H5N1 viruses in nature.
Live attenuated DEV vaccines have been developed and used in different countries to control lethal DEV infections in ducks. The DEV vaccine seed virus used in our study was derived by passaging the lethal DEV in CEFs and has been used in the field since the 1960s (15); however, the genetic basis for its attenuation is not known. We compared the sequence of the ul41 gene and the area between the us7 and us8 genes of the lethal virus and the DEV vaccine strain and did not find any changes (data not shown), indicating that the ul41 gene and the area between the us7 and us8 genes do not contribute to the attenuation phenotype of this vaccine strain. The development of a fosmid-based rescue system for DEV allows the full manipulation of the DEV genome and, therefore, facilitates the study of the mechanism underlying DEV pathogenesis.
The full genome of DEV was sequenced recently (20), and the sequencing revealed that DEV and Marek's disease virus (MDV) have similar gene structures in their genomes. The us areas in MDV have proven to be suitable for foreign gene insertion, including the sites within Sorf1, Sorf2, us1, us10, Sorf3, us2, us3, and us6 (26, 27, 30). In our preliminary studies, we tried to insert foreign genes into the us2 and us10 genes of DEV but failed to rescue any recombinant viruses, suggesting that these genes are essential for DEV replication and that the function of these areas in DEV differs from those in other herpesviruses. The us7 and us8 genes are essential for MDV replication (32). Therefore, we generated the recombinant virus rDEV-us78HA by inserting the HA gene between us7 and us8. This recombinant virus showed protective efficacy against lethal DEV challenge in ducks similar to that shown by the parent DEV vaccine strain and also showed stable HA expression during passage in CEFs, indicating that the region between the us7 and us8 genes of DEV is suitable for foreign gene insertion.
The ul41 gene of alphaherpesviruses encodes the viral host shutoff (vhs) protein, which triggers global mRNA destabilization in infected cells, an effect that generally is assumed to fully account for its role in host shutoff (34). The deletion of the ul41 gene increases the immunogenicity of herpes simplex virus type 1 (HSV1) (12). The deletion of this gene also may benefit HA gene expression. For these reasons, we generated a recombinant virus, rDEV-ul41HA, by replacing part of the ul41 gene with the HA gene cassette. We found that rDEV-ul41HA had a replication titer similar to that of the DEV vector vaccine virus and that of rDEV-us78HA. HA expression in rDEV-ul41HA-infected cells was notably higher than that in rDEV-us78HA-infected cells. However, from the challenge study, it appears that the protective efficacy against DEV or the H5N1 virus was slightly impaired rather than increased in rDEV-ul41HA-inoculated ducks relative to that of DEV vector virus- or rDEV-us78HA-inoculated ducks with respect to challenge virus shedding, replication in organs, and duck survival rates during the observation period. These results indicate that us41 is not an ideal site for foreign gene insertion.
It is highly notable that a single dose of 106 PFU of rDEV-us78HA induced very early solid protection against both lethal DEV and H5N1 virus challenge and completely prevented H5N1 virus replication and shedding at 3 days p.v. This feature makes this vaccine extremely valuable, especially if used in buffer zone animals to prevent the spread of H5N1 virus during an outbreak. Clearly, the rapid protection against H5N1 virus challenge is the result of adaptive immunity or HA-activated innate immunity, since all of the ducks in the DEV- and PBS-inoculated groups died within 3 to 5 days of being challenged. Many studies have demonstrated that live virus vaccines successfully induce specific cellular immune responses, especially CD8+ cytotoxic T-lymphocyte (CTL) responses, and may provide immune protection independently of specific antibody responses (13, 14). We did not conduct any tests for cellular immune responses; however, it is highly unlikely that the vaccine can elicit enough H5N1 virus-specific CD8+ CTLs to provide complete protection in such a short time. Therefore, the mechanism for the rapid and complete protection induced by the DEV-vectored vaccine still remains to be determined. The HA protein of influenza viruses, including H5 AIVs, may activate natural killer (NK) cells (8). Since DEV can infect and establish latency in lymphoid tissues and peripheral blood lymphocytes (33), the HA protein expressed by the recombinant DEVs may have a greater opportunity to interact with the receptors on NK cells and activate their antiviral function. Similar rapid protection has been reported for recombinant vesicular stomatitis virus-vectored vaccines against Marburg hemorrhagic fever virus and Ebola virus (6, 10), although the mechanistic basis for such rapid specific immune protection remains largely unknown.
Influenza virus easily undergoes antigenic drift while circulating in nature. Therefore, the strains used in the human influenza vaccine are updated regularly based on viral epidemiology information. Similarly, vaccine strains for H5N1 avian influenza control have been regularly updated (3). The traditional methods for generating recombinant herpesvirus, such as plasmid transfection plus virus coinfection, often are inefficient, labor-intensive, and time-consuming due to the need for cloning and purification processes. In addition, a selection marker has to be included (5). Infectious bacterial artificial chromosomes (BACs) of herpesviruses are powerful tools for genetic manipulation (2, 7, 23). However, the presence of BAC vector sequence in the viral genomes often causes genetic and phenotypic alterations, and the excision of the BAC sequence is time-consuming (35, 43–45). Here, we established and optimized a highly efficient and stable fosmid system for rescuing recombinant DEV; in this system, a selection marker is not necessary. With this system, we could generate a DEV-vectored H5 AIV vaccine candidate strain within 2 weeks, which demonstrates that vaccine update would be easy and feasible.
Recombinant Newcastle disease virus (NDV) expressing the HA gene of H5N1 influenza virus has been used as a bivalent vaccine against both NDV and H5N1 viruses in chickens in China since 2006 (3, 11). The recombinant NDV vaccine has been used to replace the regular NDV live vaccine in routine vaccination programs on many chicken farms. The recombinant DEV vaccine could similarly be used to replace the regular DEV live vaccine in routine vaccination programs in ducks. Although more studies are required to determine an ideal vaccination protocol, the recombinant DEV vaccine holds great promise and is highly likely to be used to combat infection with two important lethal pathogens in ducks.
Supplementary Material
ACKNOWLEDGMENTS
We thank Susan Watson for editing the manuscript.
This work was supported by the NSFC (30825032); by the 973 programs (2011CB505000 and 2010CB534000); by the National S&T Plan (2006BAD06A05); by the National Key Infectious Disease Surveillance Program (2009ZX10004-214) of China; by a contract research fund from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases; by a grant-in-aid for Specially Promoted Research from the Ministries of Education, Culture, Sports, Science, and Technology; by grants-in-aid from Health, Labor, and Welfare of Japan; by ERATO; and by National Institute of Allergy and Infectious Diseases Public Health Service research grants.
Footnotes
Supplemental material for this article may be found at http://jvi.asm.org/.
Published ahead of print on 24 August 2011.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1. Balan P., et al. 1994. An analysis of the in vitro and in vivo phenotypes of mutants of herpes simplex virus type 1 lacking glycoproteins gG, gE, gI or the putative gJ. J. Gen. Virol. 75:1245–1258 [DOI] [PubMed] [Google Scholar]
- 2. Borst E. M., Hahn G., Koszinowski U. H., Messerle M. 1999. Cloning of the human cytomegalovirus (HCMV) genome as an infectious bacterial artificial chromosome in Escherichia coli: a new approach for construction of HCMV mutants. J. Virol. 73:8320–8329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen H., Bu Z. 2009. Development and application of avian influenza vaccines in China. Curr. Top. Microbiol. Immunol. 333:153–162 [DOI] [PubMed] [Google Scholar]
- 4. Chen H., et al. 2004. The evolution of H5N1 influenza viruses in ducks in southern China. Proc. Natl. Acad. Sci. U. S. A. 101:10452–10457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cunningham C., Davison A. J. 1993. A cosmid-based system for constructing mutants of herpes simplex virus type 1. Virology 197:116–124 [DOI] [PubMed] [Google Scholar]
- 6. Daddario-DiCaprio K. M., et al. 2006. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet 367:1399–1404 [DOI] [PubMed] [Google Scholar]
- 7. Delecluse H. J., Hilsendegen T., Pich D., Zeidler R., Hammerschmidt W. 1998. Propagation and recovery of intact, infectious Epstein-Barr virus from prokaryotic to human cells. Proc. Natl. Acad. Sci. U. S. A. 95:8245–8250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Du N., et al. 2010. Differential activation of NK cells by influenza A pseudotype H5N1 and 1918 and 2009 pandemic H1N1 viruses. J. Virol. 84:7822–7831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ellis T. M., et al. 2004. Vaccination of chickens against H5N1 avian influenza in the face of an outbreak interrupts virus transmission. Avian Pathol. 33:405–412 [DOI] [PubMed] [Google Scholar]
- 10. Feldmann H., et al. 2007. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 3:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ge J., et al. 2007. Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. J. Virol. 81:150–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Geiss B. J., Smith T. J., Leib D. A., Morrison L. A. 2000. Disruption of virion host shutoff activity improves the immunogenicity and protective capacity of a replication-incompetent herpes simplex virus type 1 vaccine strain. J. Virol. 74:11137–11144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haglund K., et al. 2002. High-level primary CD8(+) T-cell response to human immunodeficiency virus type 1 gag and env generated by vaccination with recombinant vesicular stomatitis viruses. J. Virol. 76:2730–2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hoelscher M. A., et al. 2006. Development of adenoviral-vector-based pandemic influenza vaccine against antigenically distinct human H5N1 strains in mice. Lancet 367:475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang Y., Ou S., Lin W. 1980. Investigations on duck plague virus. J. S. China Agric. College 1:21–35 [Google Scholar]
- 16. Hulse-Post D. J., et al. 2005. Role of domestic ducks in the propagation and biological evolution of highly pathogenic H5N1 influenza viruses in Asia. Proc. Natl. Acad. Sci. U. S. A. 102:10682–10687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jansen J., Sr 1964. The Interference phenomenon in the development of resistance against duck plague. J. Comp. Pathol. 74:3–7 [DOI] [PubMed] [Google Scholar]
- 18. Jansen J. S., Kurst H., Wemmenhove R. 1963. The active immunization of duck plague. Tijdschr. Diergeneeskd. 88:927–932 [Google Scholar]
- 19. Jiang Y., et al. 2007. Enhanced protective efficacy of H5 subtype avian influenza DNA vaccine with codon optimized HA gene in a pCAGGS plasmid vector. Antiviral Res. 75:234–241 [DOI] [PubMed] [Google Scholar]
- 20. Li Y., et al. 2009. Molecular characterization of the genome of duck enteritis virus. Virology 391:151–161 [DOI] [PubMed] [Google Scholar]
- 21. Li Y., et al. 2010. Continued evolution of H5N1 influenza viruses in wild birds, domestic poultry, and humans in China from 2004 to 2009. J. Virol. 84:8389–8397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lüschow D., Werner O., Mettenleiter T. C., Fuchs W. 2001. Protection of chickens from lethal avian influenza A virus infection by live-virus vaccination with infectious laryngotracheitis virus recombinants expressing the hemagglutinin (H5) gene. Vaccine 19:4249–4259 [DOI] [PubMed] [Google Scholar]
- 23. Messerle M., Crnkovic I., Hammerschmidt W., Ziegler H., Koszinowski U. H. 1997. Cloning and mutagenesis of a herpesvirus genome as an infectious bacterial artificial chromosome. Proc. Natl. Acad. Sci. U. S. A. 94:14759–14763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Morgan R. W., Cantello J. L., McDermott C. H. 1990. Transfection of chicken embryo fibroblasts with Marek's disease virus DNA. Avian Dis. 34:345–351 [PubMed] [Google Scholar]
- 25. Office International des Epizooties 2004. OIE manual of diagnostic tests and vaccines for terrestrial animals. Office International des Epizooties, Paris, France [Google Scholar]
- 26. Parcells M. S., Anderson A. S., Cantello J. L., Morgan R. W. 1994. Characterization of Marek's disease virus insertion and deletion mutants that lack US1 (ICP22 homolog), US10, and/or US2 and neighboring short-component open reading frames. J. Virol. 68:8239–8253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Parcells M. S., Anderson A. S., Morgan R. W. 1994. Characterization of a Marek's disease virus mutant containing a lacZ insertion in the US6 (gD) homologue gene. Virus Genes 9:5–13 [DOI] [PubMed] [Google Scholar]
- 28. Reed L. J., Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. (London) 27:493–497 [Google Scholar]
- 29. Sakaguchi M., et al. 1998. Protection of chickens with or without maternal antibodies against both Marek's and Newcastle diseases by one-time vaccination with recombinant vaccine of Marek's disease virus type 1. Vaccine 16:472–479 [DOI] [PubMed] [Google Scholar]
- 30. Sakaguchi M., et al. 1993. Marek's disease virus protein kinase gene identified within the short unique region of the viral genome is not essential for viral replication in cell culture and vaccine-induced immunity in chickens. Virology 195:140–148 [DOI] [PubMed] [Google Scholar]
- 31. Sandhu T., Shawky S. 2003. Duck virus enteritis (duck plague), p. 354–363 In Saif Y. M., Barnes H. J., Glisson J. R. (ed.), Diseases of poultry, 11th ed. Iowa State University Press, Ames, IA [Google Scholar]
- 32. Schumacher D., Tischer B. K., Reddy S. M., Osterrieder N. 2001. Glycoproteins E and I of Marek's disease virus serotype 1 are essential for virus growth in cultured cells. J. Virol. 75:11307–11318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shawky S., Schat K. A. 2002. Latency sites and reactivation of duck enteritis virus. Avian Dis. 46:308–313 [DOI] [PubMed] [Google Scholar]
- 34. Smiley J. R. 2004. Herpes simplex virus virion host shutoff protein: immune evasion mediated by a viral RNase? J. Virol. 78:1063–1068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Smith G. A., Enquist L. W. 2000. A self-recombining bacterial artificial chromosome and its application for analysis of herpesvirus pathogenesis. Proc. Natl. Acad. Sci. U. S. A. 97:4873–4878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Song J., et al. 2011. The PA protein directly contributes to the virulence of H5N1 avian influenza viruses in domestic ducks. J. Virol. 85:2180–2188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sonoda K., et al. 2000. Development of an effective polyvalent vaccine against both Marek's and Newcastle diseases based on recombinant Marek's disease virus type 1 in commercial chickens with maternal antibodies. J. Virol. 74:3217–3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Staprans S. I., et al. 2004. Enhanced SIV replication and accelerated progression to AIDS in macaques primed to mount a CD4 T cell response to the SIV envelope protein. Proc. Natl. Acad. Sci. U. S. A. 101:13026–13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sturm-Ramirez K. M., et al. 2004. Reemerging H5N1 influenza viruses in Hong Kong in 2002 are highly pathogenic to ducks. J. Virol. 78:4892–4901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sturm-Ramirez K. M., et al. 2005. Are ducks contributing to the endemicity of highly pathogenic H5N1 influenza virus in Asia? J. Virol. 79:11269–11279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tian G., et al. 2005. Protective efficacy in chickens, geese and ducks of an H5N1-inactivated vaccine developed by reverse genetics. Virology 341:153–162 [DOI] [PubMed] [Google Scholar]
- 42. van Zijl M., et al. 1991. Live attenuated pseudorabies virus expressing envelope glycoprotein E1 of hog cholera virus protects swine against both pseudorabies and hog cholera. J. Virol. 65:2761–2765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wagner M., Jonjic S., Koszinowski U. H., Messerle M. 1999. Systematic excision of vector sequences from the BAC-cloned herpesvirus genome during virus reconstitution. J. Virol. 73:7056–7060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhao Y., Petherbridge L., Smith L. P., Baigent S., Nair V. 2008. Self-excision of the BAC sequences from the recombinant Marek's disease virus genome increases replication and pathogenicity. Virol. J. 5:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhou F., Li Q., Wong S. W., Gao S. J. 2010. Autoexcision of bacterial artificial chromosome facilitated by terminal repeat-mediated homologous recombination: a novel approach for generating traceless genetic mutants of herpesviruses. J. Virol. 84:2871–2880 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.