Abstract
Paraduodenal hernias are rare hernias that result from error of rotation of the mid-gut. It can be discovered incidentally at laparotomy, seen on radiological imagining or infrequently cause intestinal obstruction. We report a case of a left paraduodenal hernia diagnosed intraoperatively after being operated on in the emergency setting for generalized peritonitis. He required resection of multiple loops of small bowel with primary anastomosis. The mouth of the sac was obliterated by suture apposition to the posterior wall. The patient was discharged on day 4 after an uneventful recovery.
Keywords: Peritonitis, Emergency laparotomy, Paraduodenal hernia, Intestinal obstruction
1. Introduction
Paraduodenal hernias are rare types of hernias resulting from incomplete rotation of the midgut. It may lead to intestinal obstruction or are typically detected incidentally at autopsy or laparotomy. More frequently paraduodenal hernias are seen on radiological imagining.1,3 We report a case of individual who presented with peritonitis and found to have a complicated paraduodenal hernia.
2. Case report
A 47-year-old man known to be diabetic, hypertensive and epileptic was admitted to the emergency department of University Hospital of the West Indies for investigation and treatment of intermittent colicky epigastric pain of 15 h duration. He reported having experienced similar episodes several times in the previous year, but the pain resolved spontaneously each time. On this occasion, his abdominal pain progressed to become generalized in nature and associated with episodes of vomiting. He stated that eating made the pain better. He complained of mild abdominal distention and passed stool 1 day prior but no flatus. He had no history of abdominal surgery. On physical examination, he was moderately dehydrated with mild tachycardia but normal blood pressure. The abdomen was soft and he had generalized tenderness with epigastric predominance. He had guarding but no rebound tenderness and no bowel sounds. Blood analysis, urine analysis, and a plain abdominal radiograph showed no abnormalities, except for leukocytosis of 16.9. The diagnosis of an acute abdomen likely secondary to perforated peptic ulcer disease was made. The decision was made for an emergency laparotomy (Figs. 1–3).
Fig. 1.
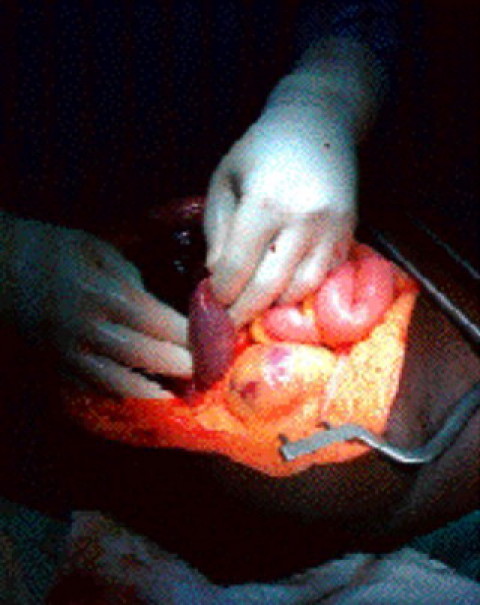
Left paraduodenal hernial sac.
Fig. 2.

Small bowel mesentery caught in hernial sac resulting in gangrene of mid-jejunum.
Fig. 3.

Multiple loops of gangrenous small bowel.
After a period of resuscitation, we performed an emergency laparotomy, which revealed that the proximal one-third of jejunum was within a sac-like structure which projected to the left of the midline. The sac wall was formed by an anomaly of the mesentery of the transverse and descending colon. The inferior mesenteric vessels were located in the medial edge of the anterior wall of the defect. The posterior wall was formed by the posterior abdominal wall. The intestinal loops were entrapped through the defect because of their anomolous fixation point in the sac by an adhesive band. Another adhesive band was noted between sac edge and duodenojejunal flexure. The bowel was easily reducible from the sac manually. Distal to the entrapped proximal one-third of jejunum, about 70 cm of mid-jejunum was necrotic.
The ischemic bowel was resected and a primary anastomosis done using continuous 3-0 silk. The peritoneal sac opening was apposed to the posterior abdominal wall obliterating the entrance. The patient had active bowel sounds on postoperative day 2 and resumed oral intake on day 3. He was discharged on day 4 and has been well since.
3. Discussion
An internal hernia is classified as the protrusion of a viscus through a peritoneal or mesenteric aperture, resulting in its encapsulation in another compartment within the confines of the peritoneal cavity. Right and left paraduodenal hernias are separate entities, differing in anatomic position and also in embryologic origin.15 They are characterized by abnormal fixation of the duodenum and jejunum.
Intestinal maturation starts in the 6 weeks old fetus when the midgut herniates into the umbilical cord. The midgut rotates a full 270° counterclockwise around the superior mesenteric artery by time it re-enters the abdomen. If the prearterial segment rotates but the postarterial segment fails to rotate the small bowel is entrapped in the right mesocolon, and right paraduodenal hernia results.12 Autopsy specimens showed a sac-like mass with encapsulation at or above the ligament of Treitz, a mass on the posterior stomach wall, and mesenteric vessel abnormality.
Anatomically there are a number of paraduodenal fossae. The most important ones are the left paraduodenal fossa or fossa of Landzert and the right paraduodenal fossa or the fossa of Waldeyer.12 The fossa of Landzert is to the left of the fourth part of the duodenum and extends behind the descending mesocolon. It is very important to recognize the inferior mesenteric vein where it joins the splenic vein or the superior mesenteric vein as this marks the duodenojejunal flexure. These borders are also important surgically, as the inferior border of the hernia opening is the safest place to incise to widen the neck and allow reduction without risk of damage to vital structures.12 The fossa of Waldeyer extends inferior to the third and fourth part opening being just inferior to the duodenojejunal junction and bound anteriorly by the inferior mesenteric vein and the ascending left colic artery. The inferior mesenteric vein and the left ascending colic artery displaced anteriorly by a cluster of jejunal bowel loops is the most important sign on CT of left paraduodenal hernia.12
Internal hernias are rare, but they are been detected more commonly on radiological imagining.3,9 Paraduodenal hernias account for 53% of all internal hernias,4,3 and have an autopsy incidence of 0.2–0.9%.4,3 Right paraduodenal hernias account for only 25% of paraduodenal hernias and left-sided paraduodenal hernias for the rest.3 These account for less than 1% of all small intestinal obstructions overall.13
There are few reports in the literature, with the total number of reported cases being less than 500.14 Infrequently, paraduodenal hernia cause intestinal obstruction.10 The natural history of this type of internal hernia is to remain asymptomatic during the lifetime of a person.12 Although not high on the list of differentials, there however is a 50% lifetime risk of obstruction when a paraduodenal hernia is present.5,14 Clinically, most patients present with ill-defined episodes of abdominal pain, often progressing to partial or complete intestinal obstruction.4,9 Paraduodenal hernia presents dramatically, causes a non-specific clinical picture, and often reduces spontaneously, leading to diagnostic difficulties.6 Although a rare cause of intestinal obstruction, it has a high mortality.10
On X-ray, paraduodenal hernias were classically described as a clustering of small-bowel loops in the upper right or left quadrants. CT has become the method of choice in diagnosing any internal hernia, but it can also be diagnosed on plain film and barium follow-through. With a significant lifetime risk of intestinal obstruction, elective repair is usually recommended.5,14 Barlett et al.2 summarized the management of this condition with real change in approach seen in the literature. It is essential to recognize whether it has occurred on the right or left side, since the technical problem involved is quite different. With right paraduodenal hernia the aim should be to replace intestine in the positions they would normally occupy at the end of the first stage of rotation, with the duodenum, jejunum, and most of the ileum to the right and the terminal ileum, cecum and colon on the left of the midline. This is in an effort to eliminate the small opening from the hernia sac through which the terminal ileum passes and through which additional loops of small bowel may prolapse. This is accomplished by dividing the lateral attachments of the colon on the right side and transferring it to the left side of the abdomen. In this maneuver, the hernia sac is widely opened and the small opening through which the terminal ileum passes is eliminated. The hernia sac is now a part of the general peritoneal cavity. The superior mesenteric artery and its branches to the cecum and ascending colon lie in the anterior wall of the hernia sac. Manual reduction is never attempted, as injury to these vessels would render a significant part of the bowel ischemic. In dealing with a left paraduodenal hernia, manual reduction of the small bowel into the peritoneal cavity is often possible, followed be simply obliteration of hernial opening. However, the neck of the sac is small and often obscured by adhesions and difficult to identify accurately. In such a case the hernia sac should be opened by an incision into an avascular area of the mesentery of the descending colon, allowing the small bowel to be delivered into the peritoneal cavity. When there is a tight or obscured hernia ring, the inferior mesenteric vein has to be sacrificed in that case to facilitate reduction of the hernia contents.2,14 This will allow the hernia sac to become, in effect, a part of the general peritoneal cavity.
During emergency surgery, a strong index of suspicion usually directs you to that diagnosis. Due to the fact that these hernias can reduce spontaneously preoperatively, and because all the peritoneal spaces are not always routinely examined intraoperatively, they can go undiagnosed during open surgery.3 The diagnosis should particularly be borne in mind in the case of intestinal obstruction in patients who have not had previous abdominal surgery hernia.8
Palanivelu et al.14 reported on his experience with the laparoscopic approach. He examined four patients with paraduodenal hernias causing intestinal obstruction. They were all successfully managed by a laparoscopic repair. There were no conversions. The operating time was 55–72 min. Only one patient had ileus for 3 days with spontaneous recovery. Hospital stay was in the range 2–6 days. One patient had recurrent paraduodenal hernia, for which a laparoscopic mesh repair was successfully performed. The laparoscopic approach seems to be effective in the repair of paraduodenal hernias. It carries all of the benefits of minimal access surgery, while providing a sound repair.14,11
4. Conclusion
Paraduodenal hernia is a rare congenital anomaly arising from an error of rotation of the midgut. The duodenum and small intestine become trapped in a sac, lined by peritoneum, behind the mesentery of the colon, either to the right or left of the midline. This may be an incidental discovery at laparotomy or a rare cause of small bowel obstruction progressing to strangulation and perforation. Increasingly the diagnosis is made on CT scan in patients with non-specific abdominal pain or imaging for other reasons. Bearing this diagnosis in mind, it may be suspected on preoperative X-ray examination. The small bowel loops are all on the right or on the left of the midline. Barium enema is also helpful. With a lifetime risk of obstruction being 50% I would consider treatment mandatory even in uncomplicated cases. The surgical approach is dictated by the nature of the hernia. Careful consideration is required with respect to vasculature and sac contents. Obliterating sac opening is essential. Right-sided hernias may be considered more technically difficult. Failure of the surgeon to recognize the nature of this anomaly has disastrous outcome. Fortunately they are less common. Laparoscopic repair is a feasible option to repair of these hernias.
Conflicts of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- 1.Amodio P.M., Alberti A., Bigonzoni E., Piciollo M., Fortunati T., Alberti D. Left paraduodenal hernia: a case report and review of the literature. Chir Ital. 2008;60(September–October (5)):721–724. [PubMed] [Google Scholar]
- 2.Barlett M.K., Wang C., Williams W.H. The surgical management of paraduodenal hernia. Ann Surg. 1968;168(2):249–254. doi: 10.1097/00000658-196808000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blachar A., Federle M.P. Internal hernia: an increasingly common cause of small bowel obstruction. Semin Ultrasound CT MRI. 2002;23:174–183. doi: 10.1016/s0887-2171(02)90003-x. [DOI] [PubMed] [Google Scholar]
- 4.Brigham R.A., d’Avis J.C. Paraduodenal hernia. In: Nyhus L.M., Condon R.E., editors. Hernia. 3rd ed. Lippincott; Philadelphia: 1989. pp. 481–486. [Google Scholar]
- 5.Brigham R.A., Fallon W.F., Saunders J.R., Harmon J.W., d’Avis J.C. Paraduodenal hernia: diagnosis and surgical management. Surgery. 1984;96:498–502. [PubMed] [Google Scholar]
- 6.Cingi A., Demirkalem P., Manukyan M.N., Tuney D., Yegen C. Left-sided paraduodenal hernia: report of a case. Surg Today. 2006;36(7):651–654. doi: 10.1007/s00595-006-3205-x. [DOI] [PubMed] [Google Scholar]
- 8.Fan H.P., Yang A.D., Chang Y.J., Juan C.W., Wu H.P. Clinical spectrum of internal hernia: a surgical emergency. Surg Today. 2008;38(10):899–904. doi: 10.1007/s00595-007-3756-5. [DOI] [PubMed] [Google Scholar]
- 9.Huang Y.M., Chou A.B., Wu Y.K., Wu C.C., Lee M.C., Chen H.T. Left paraduodenal hernia presenting as recurrent small bowel obstruction. World J Gastroenterol. 2005;11(November (41)):6557–6559. doi: 10.3748/wjg.v11.i41.6557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan M.A., Lo A.Y., Vande Maele D.M. Paraduodenal hernia. Am Surg. 1998;64:1218–1222. [PubMed] [Google Scholar]
- 11.Jeong G.A., Cho G.S., Kim H.C., Shin E.J., Song O.P. Laparoscopic repair of paraduodenal hernia: comparison with conventional open repair. Surg Laparosc Endosc Percutan Tech. 2008;18(December (6)):611–615. doi: 10.1097/SLE.0b013e3181825733. [DOI] [PubMed] [Google Scholar]
- 12.Manji R., Warnock G.L. Left paraduodenal hernia: an unusual cause of small bowel obstruction. Can J Surg. 2001;46:455–456. [PMC free article] [PubMed] [Google Scholar]
- 13.Moon C.H., Chung M.H., Lin K.M. Diagnostic laparoscopy and laparoscopic repair of a left paraduodenal hernia can shorten hospital stay. JSLS. 2006;10(January–March (1)):90–93. [PMC free article] [PubMed] [Google Scholar]
- 14.Palanivelu C., Rangarajan M., Jategaonkar P.A., Anand N.V., Senthilkumar K. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12(December (6)):649–653. doi: 10.1007/s10029-008-0376-y. [DOI] [PubMed] [Google Scholar]
- 15.Shinohara T., Okugawa K., Furuta C. Volvulus of the small intestine caused by right paraduodenal hernia: a case report. J Pediatr Surg. 2004;39:e8–e9. doi: 10.1016/j.jpedsurg.2003.10.029. [DOI] [PubMed] [Google Scholar]


