Abstract
Subjective assessment of quality of life (QOL) as an important aspect of outcomes research has received increasing importance during the past decades. QOL is measured with standardized questionnaires which had been tested with regard to reliability, validity, and sensitivity.
Surgical procedures of the nasal septum (septoplasty) and the external nose (rhinoplasty) are frequently performed. Since many years subjectively assessed results of these operations have been reported in the literature. However, validated QOL instruments were applied only for one decade. Beforehand, measurements were performed using retrospective assessment of satisfaction or visual analogue scales. Prospective application of validated disease-specific and general measuring instruments has to be demanded for future studies.
Most of the septoplasty patients as well as most of the rhinoplasty patients evaluate the operation being successful. However, a relevant number of patients is not satisfied with the result of surgery. In this context, QOL instruments have the potential to identify further factors influencing the outcome. Especially in rhinoplasty patients, special attention has to be drawn on potential psychosocial effects of the operation.
Keywords: validation, quality of life, nasal obstruction, nasal function
1 General introduction: Health-related quality of life
1.1 Introductory remarks
Our attitudes on health and health care are changing. Significant factors in this change are insights on the social consequences of diseases and the experience that medical interventions may lengthen life and improve quality of life (QOL) [1]. In this context outcome analysis gets increasing importance.
1.2 Methods of outcome analysis
Outcome analysis is one important tool for the assessment of quality of medical care. It evaluates to what extent the aims of medical care have been achieved. Diverse methods are in use to perform this task.
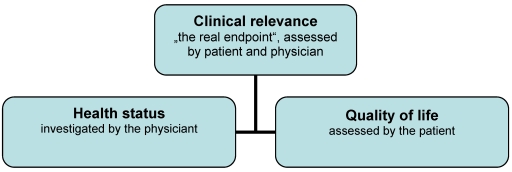
The outcome of a therapeutic intervention is considered as a theoretical construct of different end points assessed by the physician and the patient (Figure 1 (Fig. 1)) [2]. The physician evaluates health status of the patient by traditional treatment end points like survival rate, absence of recurrence, remission rate, side effects, complications, guide line conformity, or cost effectiveness. The patient assesses hermeneutic end points like quality of life, expectations, negative affects, social stigmatization, or coping strategies [3].
Figure 1. Model of components of outcome analysis (according to [2]).
Discrepancies in the outcome of different treatment modalities are not only caused by the modalities themselves. In fact, treatment indications in specific patient cohorts, expertise of the physician as well as the individual social and health situation of the patient might play an important role [4].
1.3 Quality of life research
The patients' view is one essential evaluation criterion of outcome quality. The patient assesses his or her subjective position regarding QOL by filling out appropriate questionnaires which serve as measuring instruments. These standardized questionnaires have to fulfil the requirements of reliability, validity, and sensitivity to change [3].
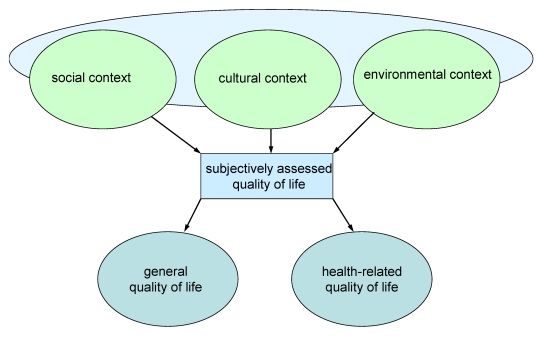
The World Health Organization (WHO) defines QOL as individuals' perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns [5]. QOL can be subdivided into general and health-related QOL. Generally, it is considered as a multidimensional phenomenon or construct (Figure 2 (Fig. 2)) [6]. According to Lawton [7], QOL consists of four main areas: objective environment, behavioural competence (including health), perceived QOL, and psychological well-being (including life satisfaction).
Figure 2. Context and fields of subjectively assessed quality of life.
1.3.1 Health-related quality of life – definition of the term
The term QOL was introduced in medicine only in the beginning of the nineteen-eighties [8], [9]. Synchronously it was requested to measure QOL of the patients [10].
Health-related QOL should be seen in terms of somatic, psychic, and social related self-perception with regard to the disease. It implies expectations, personal preferences as well as coping processes and is influenced by psychosocial factors like negative emotions or disease-associated stigmatization [4]. This is expressed in the definition of health-related QOL by Schipper et al. [11]: “Quality of life represents the functional effect of an illness and its consequent therapy upon the patient, as perceived by the patient”.
Health-related QOL is affected by the health expectations and the disease-related experiences of the patients. Furthermore, it is assessed differently by the individuals and changing over time.
Patients with different health expectation assess their QOL differently even if they have an equal health status [1]. Therefore, QOL instruments have to query the subjective view of the patient but not of the view of the physician.
1.3.2 The concept of health-related quality of life
The term “health-related quality of life” regards to the subjective perception of the disease severity in the course of time. Two fundamental aspects have to be noticed:
Multi-dimensionality (QOL covers a large variety of dimensions)
Subjectivity (the assessment of a health problem might be totally different among individuals with equal disease severity)
QOL differs from the other traditional treatment assessments like response rate or survival over time in tumor patients by changing over time. Therefore, the evaluation of QOL investigates changes during the course of the disease and its treatment.
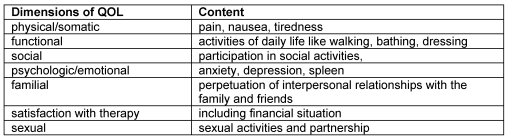
Health-related QOL includes different dimensions (Table 1 (Tab. 1)) [12], [13], [14].
Table 1. Dimensions of QOL.
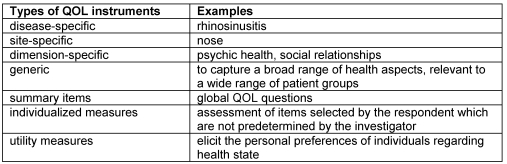
Different types of measuring instruments are applied in QOL research. Seven types of those instruments were identified by Fitzpatrick et al. (Table 2 (Tab. 2)) [15].
Table 2. Types of instruments measuring QOL (according to [15]).
1.3.3 Criteria for selecting patient-based outcome measures
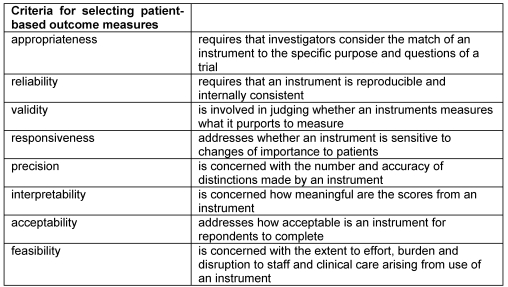
Fitzpatrick et al. defined eight criteria which should be considered for the selection of QOL instruments in clinical trials (Table 3 (Tab. 3)) [15].
Table 3. Criteria for selecting patient-based outcome measures (according to [15]).
1.3.4 Basic considerations on the analysis
Analyzing QOL data which had been collected with validated measuring instruments some problematic aspects should not be ignored. It has to be respected that patients have individual expectations and requests regarding their health-related quality of life. As a matter of fact, every patient affiliates to an individual stage of coping of the disease. Furthermore, individual assessment factors might change over time [1].
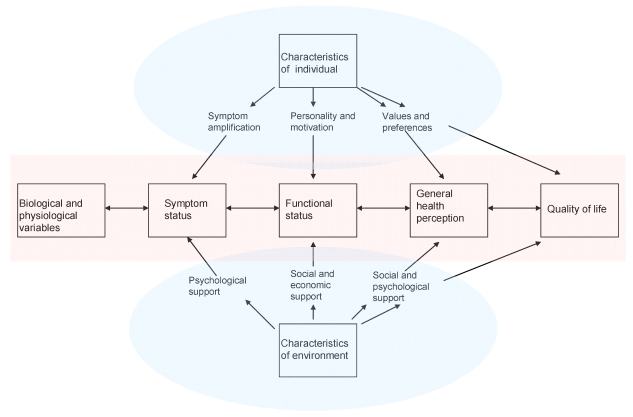
Subjectively assessed health-related QOL is the result of a multifactorial interaction of which biological and physiological variables are only one part (Figure 3 (Fig. 3)) [16]. Physicians frequently overestimate the impact of measurable biological variables on symptoms and functioning [17]. Therefore, it is not surprising that in many cases no significant correlations between objective measurements and QOL assessments could be established.
Figure 3. Relationships between quality of life, individual and environmental characteristics, and biological variables (according to [16]).
In the following we introduce some QOL instruments used in rhinologic research. With the exception of two generic measures all instruments were validated only in the English language. With regard to a requested high quality of scientific data collection the use of non-validated instruments (e.g. translations from English to German without validation) can not be recommended as these instruments have not proven reliability and generalizability in the new cultural context [18], [19]. Translated instruments have to be validated before application. Unfortunately, until now no German instruments for the evaluation of QOL after septoplasty or rhinoplasty are at disposal.
1.3.5 The intention of this review
This review is intended to give an introduction into rhinologic QOL research. In this context, the relationships between surgery of the nasal skeleton (septoplasty, septorhinoplasty) and general as well as disease-specific health-related QOL shall be highlighted. From the author’s view a chronological and methodological consideration of previous developments will be useful and be discussed in the following.
2 Health-related quality of life after septoplasty
2.1 Introduction
Septoplasty is a frequent procedure. In 2007, more than 95,000 septoplasties were performed in Germany which was 0.7% of all surgeries. According to the analyzes of the Federal Health Monitoring frequency of septoplasty occupies position 37 of all surgical procedures while tonsillectomy can be found on position 38 and inferior turbinate surgeries on position 21 (more than 132,000 surgeries, 1% of all surgeries) [20]. These data can be comprehended by bearing in mind that 25% of the population suffer from non-allergic nasal obstruction [21].
Considering the presented data one has to respect that nasal obstruction together with associated medical conditions like headache, facial pressure, or nasal discharge has to be regarded as a relevant medical problem which results in visits to the doctor’s office for many patients [22].
The above mentioned medical conditions might be caused by other factor besides septoplasty like hyperplasia of the nasal turbinates, adenoids, or chronic rhinosinusitis (CRS) with or without nasal polyposis. Therefore, besides meticulous evaluation of medical history accurate endoscopic and radiologic diagnostics have to be accomplished.
Before indicating septal surgery the otolaryngologist has to check whether the reason for nasal obstruction might be localized in the paranasal sinuses or the nasopharynx. Furthermore, he has to investigate the anatomy of the nasal cavity and potentially influencing co-morbidities like allergic rhinitis. In this context it has to be reminded that 42% of the population show septal deviation with compensatory hyperplasia of the turbinates while only 25% of these patients suffer from nasal obstruction which reversely means that not every nasal obstruction coming along with septal deviation should be caused by the deviation [23]. Further structural breathing barriers in the nose might be concha bullosa (in 40% of patients with high septal deviation [24]) or protruding inferior concha. Insufficient nasal valve function is frequently not diagnosed which leads to post-operative continuity of symptoms [25].
Pathologic alterations of the nasal mucosa might play an important role as well. Besides flow determined mucosal swellings at the nasal septum or the turbinates inflammatory mucosal alterations caused by chronic rhinosinusitis or allergic rhinitis have to be taken into consideration.
Complementary apparative diagnostics provide the investigator with additional important information. Active, anterior rhinomanometry is preferred in clinical routine work as it is less intricate compared with alternative methods like acoustic rhinometry or rhinoresistometry. However, in contrast with the other methods, rhinomanometry does not offer any information about the locus of obstruction and is reliant on the collaboration of the patient.
Measuring nasal flow before and after sympathomimetic decongestion helps to distinguish between mucosal and structural-anatomic reasons for nasal obstruction. In the end, synopsis of all the findings and information will lead to indication for surgery. Clinical experience of the decision making physician will co-determine the potential success of the operation. A recently published classification of septal deviations may help in achieving improved comprehension of pathologies of the nasal septum and the turbinates [24].
2.2 Nasal obstruction and septal surgery – objective measurements
In many patients with nasal obstruction septoplasty is performed even though evidence for causal correlation is lacking. In the past the attempt has frequently been made to prove clinical relevant improvements of nasal breathing after septal surgery by active anterior rhinomanometry, acoustic rhinometry, or peak nasal inspiratory flow (PNIF). Only three out of 982 studies fulfilled the stringent criteria of a meta-analysis by Singh et al. [26]. However, the utilizable data showed a significant reduction of nasal resistance after septal surgery.
Another study detected interesting aspects of side-specific outcomes after septoplasty [27]. Pre-operatively performed acoustic rhinometry correlated very well with subjective assessment of nasal breathing of the obstructed side but not with the assessment of the contralateral side. Though a significant narrowing of the Minimal Cross-sectional Area (MCA) was noticed in acoustic rhinometry also this study revealed a high post-operative satisfaction of the patients with the outcome. Seventy-five per cent of the patients scored zero or minimal nasal obstruction.
In many investigations the degree of nasal obstruction measured by rhinomanometry slightly correlates with the subjective assessment [28], [29]. Furthermore, poor reliability of rhinomanometry in repeated measures is objected [30]. However, rhinomanometry seems to have a predictive potential of post-operative patient satisfaction: patients with high pre-operative nasal resistance were more satisfied with the outcome of septoplasty compared with patients with normal nasal resistance (85% versus 69%). If the latter patients received conservative treatment they had a good prospect to a significant reduction of complaints [31]. Nevertheless, the severity of pre-operative symptoms could not be proven to be a predictor of post-operative satisfaction of the patients [32].
2.3 The nasal cavity as site of obstruction
As there are close relationships between anatomic-structural influences, mucosal influences, and nasal function one has to consider the whole nasal cavity including nasal mucosa, cavernous bodies, nasal valves etc. in order to assess the consequences of all these interactions on quality of life. The impact of chronic diseases of the paranasal sinuses – though it is obviously relevant – shall not be considered in this review
2.3.1 Nasal turbinates
Since a long time surgical reduction of the size of the inferior nasal turbinates has been considered as an essential additional procedure of septoplasty. This results from the clinical experience that usually septal deviation leads to a compensatory hyperplasia of the contralateral inferior nasal turbinate. The analyses of clinical observations in 1088 patients with septal deviation lead to a classification of septal deviations with special respect to turbinate hyperplasia [24]. Among other things this study pointed out that contralateral concha bullosa exists in two of six types of septal deviations (all together 22% of the patients) in each 40% of the cases. Frequently, in these cases a surgical reduction of concha bullosa by resection of the lateral lamina is required.
Various surgical procedures for the reduction of inferior turbinates have been described. As the enlargement of inferior turbinates might be caused by hypertrophy and/or hyperplasia of the conchal bone, the nasal mucosa or the cavernous body, different surgical concepts for the reduction of size of the turbinates have to be taken into accout.
Two main categories of turbinate surgery can be distinguished: tissue-destructive procedures for reduction of the soft tissue (monopolar or bipolar diathermy, radiofrequency therapy (RFT), laser surgery, argon-plasma coagulation) and ablative procedures (anterior turbinoplasty, conchotomy) [33].
QOL data are available for RFT of the inferior turbinates. A significant improvement of the disease-specific NOSE-Scores was demonstrated (see also chapter 2.5.4) for RFT alone or in combination with septoplasty. However, a significant difference between both groups was not detected [34]. In septoplasty patients operated with or without reduction of the inferior turbinates no significant difference could be detected with the NOSE instrument [35]. Further studies demonstrated a reduced nasal obstruction after RFT of the inferior turbinates by use of visual analogue scales (VAS) [36], [37] or by rhinomanometry and functional tests of mucociliary function [38], [39].
2.3.2 Nasal valve region
The nasal valve is the narrowest locus in the nasal cavity and generates two third of the whole nasal resistance. A relative stenosis of the nasal valve may occur in tension noses if the valvular angle is below 10–15 degree. Furthermore, after septoplasty or septorhinoplasty a nasal valve stenosis may become evident. Another reason for nasal valve insufficiency may be division of upper lateral cartilages from the cartilaginous septum or over-resection of the lateral crura of the alar cartilages [40]. This may lead to a relevant nasal obstruction and a significant impairment of the patient. Surgical techniques for treatment are butterfly grafts or suture techniques in case of collapsing of the upper lateral cartilages and alar batten grafts in case of missing or soft lateral crura of the alar cartilages.
Nasal valve surgery is increasingly combined with the primary surgery of the nasal septum. One study reports that nasal valve surgery was performed in 51% of the patients undergoing revision septoplasty [41]. Improvements of clinical findings and subjective assessments by the patients after nasal valve surgery were coincidently reported [42], [43].
While obstruction-specific instuments were not available prospective QOL measurements were performed with measures that had been developed for allergic or inflammatory nasal conditions (Rhinoconjuctivitis Quality of Life Questionnaire, Rhinosinusitis Disability Index) [44]. In these studies patients suffering from septal deviation and additional nasal valve insufficiency scored worse compared with patients with septal deviation alone. In 2005, one study dealing with the obstruction-specific NOSE scale was published [45]. A significant improvement of NOSE scores was detected each 3 and 6 months after surgery. Clinical investigation of the nasal valve correlated very well with the NOSE score.
2.4 General quality of life and septoplasty
Outcomes research applies validated measures to investigate the effects of different treatment modalities on quality of life of the patients [46]. It differs from traditional clinical research by assessing the treatment response from the patient's view. In this context disease-specific instruments were found to be superior to generic instruments when the burden of disease was below the threshold values of the generic instruments [47]. Thereby, specific symptoms which may significantly affect the patient’s life are not always completely covered by generic instruments. However, generic instruments are indispensable to detect the impact of specific diseases on general health status. They offer the opportunity to compare the impact of different diseases on general QOL. For example, it was found with generic instruments that patients with chronic rhinosinusitis assess a higher impact of the disease on QOL domains like bodily pain or social functioning compared with angina pectoris, lung emphysema, or chronic bronchitis [48].
The most frequently used generic instrument is the Short Form 36 Health Survey (SF-36) [49], [50]. It contains 36 questions which belong to eight domain resp. scales of subjective health. The German validated version of the SF-36 is likewise frequently used and offers data of the normal population (n=2914) [51]. Data of patients with septal deviation have not been published with this measure until now.
Some studies postulated that patients with septal deviation have a reduced “nose-specific” QOL but show normal levels of general QOL [52]. While nasal symptoms improved after septoplasty general scales of the Nottingham Health Profile (NHP) and the General Health Questionnaire (GHQ) remained unchanged [53]. Another study with elderly patients >65 years revealed an improvement from 52 to 77 points on a 0–100-scale while improvements were not significant in the generic SF-12 questionnaire [54]. On the other hand, a study by Buckland et al. with the Sino-Nasal Outcome Test 22 (SNOT-22) showed a significant improvement of nasal and general items after septoplasty [22].
It has to be suspected that effects of septoplasty on general QOL are smaller compared with the effects of Functional Endoscopic Sinus Surgery (FESS) on patients with chronic rhinosinusitis (CRS). However, patients with CRS are more affected by the disease in different QOL domains compared with patients who receive septoplasty for nasal obstruction alone. Therefore, the potential for improvement might be higher in CRS patients [55]. In many studies surgical treatment of CRS lead to significant QOL improvements in generic measures [56], [57]. Measurements with the Glasgow Benefit Inventory detected higher improvements for CRS patients than for septoplasty patients [58], [59], [60].
2.5 Disease-specific quality of life and septoplasty
Only few studies dealing with the disease-specific health-related QOL after septoplasty were published. Most of the papers used retrospective data which were collected with inappropriate or non-validated measures. However, some interesting conclusions can be deduced from these data.
During the last decades the subjective outcome after septoplasty was assessed increasingly systematic and with more and more improved measures. One could observe a development from the simple questioning of satisfaction, via the use of visual analogue scales (VAS) and the use of non-specific QOL measures to the use of the specific NOSE scale.
2.5.1 Assessment of satisfaction
A re-investigation ten years after septoplasty revealed 84% satisfaction (31 out of 37 patients) [61]. Further studies detected a range from 70.5% to 86% satisfied patients [62], [63], [64], [65]. Jessen reported 74% respectively 69% satisfied patients nine months respectively nine years after septoplasty while the proportion of patients reporting to be free of obstruction halved from 51% to 26% [66]. In a rhinomanometry study patients with post-operatively reduced nasal resistance were more often satisfied compared with patients with increased nasal resistance (67 out of 83 versus 7 out of 17) [32]. However, the quality of the data regarding validity and reliability of the used questionnaire is arguable. A bias during questioning cannot be precluded while the conclusions are blurred and data collection was retrospective in all studies.
2.5.2 Measurements with visual analogue scales (VAS)
Visual analogue scales (VAS) have been used repeatedly for the assessment of septoplasty results as disease-specific QOL instruments were not available. Compared with assessment of satisfaction they stand for methodic progress.
A retrospective long-term evaluation 2–10 years after septoplasty yielded a mean satisfaction of 6 on a 1–10-scale [67]. Furthermore, the authors stated a significant correlation between anterior septal deviation and satisfaction with the result of surgery. In a comparison of conventional versus endoscopic septoplasty subjective assessment of obstruction by VAS did not detect a difference between the two techniques [68].
2.5.3 Measurements with rhinosinusitis-specific instruments
A prospective study with 93 septoplasty patients using the Nasal Health Survey (NHS, analogical to the Chronic Sinusitis Survey) demonstrated a significant reduction of symptoms and use of medication after surgery [57]. A clinical significant improvement which was indicated by a 50 per-cent reduction of nasal symptoms was found in 71% of the patients. Revision surgery and female gender were identified to be predictors for a worse outcome [52]. Similar results were found in another study with 40 patients above 65 years showing a significant increase of the NHS score from 52 to 77 [54]. A further study with 121 patients using the Fairley Nasal Symptom Score revealed a post-operative improvement of nasal obstruction in 74%, facial pain in 72%, and nasal discharge in 64% of the patients [53].
2.5.4 Measurements with an obstruction-specific instrument (NOSE scale)
The application of validated disease-specific measures in prospective studies is required to achieve a high level of Evidence-Based Medicine (EBM). Stewart et al addressed themselves to this task and developed the Nasal Obstruction Symptom Evaluation (NOSE) Scale within the scope of a multicenter study [69]. A team of experts developed an alpha-version of the instrument with 10 obstruction-specific items that were scored using a 5-point Likert scale. This measure was validated by the assessment and calculation of reliability (test-retest reliability, internal consistency), validity (content validity, construct validity, discrimination validity, concurrent validity) and response sensitivity (standardized response mean, effect size). During this process the measure was reduced to 5 items which are the following: nasal congestion or stuffiness, nasal blockage or obstruction, trouble breathing through the nose, trouble sleeping, unable to get enough air through the nose during exercise or exertion.
The NOSE scale was then subsequently used in a prospective study with 59 patients addressing outcome evaluation after septoplasty, the multicenter so-called Nasal Obstruction Septoplasty Evaluation (NOSE) Study [35]. Data revealed a significant improvement of the mean NOSE score from 67 to 23 points (p<0.001) on a 0–100 scale after 3 months which was also detectable after 6 months. Patient satisfaction was high with 63% of the patients being very or extremely satisfied. Furthermore, reduced use of medication was observed. Another study with 12 patients treated with extracorporeal septoplasty detected an improvement of the NOSE score from 77 to 13 points [70].
However, even if the above mentioned studies have a high quality the data represent short term results. Prospective long-term studies have not been published until today.
3 Health-related quality of life after rhinoplasty
3.1 Introductory remarks
For the last years QOL research in facial plastic surgery has boomed while validated QOL measures for many other fields of otolaryngology have been developed much earlier. The late onset of QOL research in this field might astonish as subjective evaluation of results with special regard to the patient’s satisfaction is a daily challenge [71]. It was potentially objected to misinterpret psychologic specifics of the patients [72].
Three substantial aspects of the outcome of rhinoplasty have been highlighted in the literature:
quantitative measurement of nasal appearance changes
quantitative and qualitative changes of nasal function
subjective assessment of patient satisfaction and health-related QOL [73].
3.2 Functional outcome after rhinoplasty
3.2.1 Retrospective Studies
The degree of nasal obstruction is the most important parameter of functional outcome in rhinoplasty patients as well. One study detected an improved nasal breathing after nasal valve surgery with alar batten grafts in 45 out of 46 patients [74].
Another study investigating the effects of rhinoplasty in 468 patients found an improvement of nasal breathing in 40% of the patients while a deterioration occurred in 10% [75] Both studies used non-validated measuring instruments in a retrospective study design which reduced the significance of the studies.
3.2.2 Prospective Studies
Prospective studies have repeatedly been performed. In 1983, Courtiss et al showed that rhinoplasty combined with septoplasty and surgery of the turbinates may result in a significant improvement of nasal breathing [30]. The data showed similar or better results compared with the data of a control group without nasal problems. Another study confirmed these results and revealed an improvement of nasal resistance by the use of spreader grafts in narrow nasal valves [76]. A significant pre-operative asymmetry (>80%) of the respiratory flow was detected to be a prognostic factor for post-operative dissatisfaction with nasal breathing [77].
3.3 Quality of life measurements after rhinoplasty with validated instruments
The assessment of satisfaction with the result of rhinoplasty was used as a subjective outcome parameter for many years. More than 90% of the patients were satisfied with nasal appearance and breathing in retrospective studies [75], [78]. The measures were developed ad hoc and were used without validation. QOL measurements with validated instruments have been performed in few studies. However, it has been highlighted that such instruments should be used in studies [79].
3.3.1 General quality of life and rhinoplasty
In a SF-36 study rhinoplasty patients without nasal obstruction which wanted surgery for aesthetic reasons scored general health status significantly worse compared with the normal population. This difference was not detectable six months after surgery [80].
Another study with the Health Measurement Questionnaire (HMQ) showed improvements of general QOL after rhinoplasty. However, the degree of improvement was significantly smaller compared with other plastic procedures (mammaplasty, abdominoplasty) [81].
The Glasgow Benefit Inventory (GBI) was developed in 1996 as a general measure for retrospective assessment of benefit after otolaryngologic procedures [82]. With this instrument rhinoplasty patients which were operated for nasal trauma were investigated. Factor analysis showed that subjective benefit of rhinoplasty was strongly associated with surgical success of the operation but less associated with psychologic factors [83]. This is consistent with the results of another study which detected more psychic alterations in rhinoplasty patients without nasal trauma compared with trauma patients [84].
3.3.2 Disease-specific quality of life and rhinoplasty
The NOSE scale (see chapter 2) was applied in 41 rhinoplasty patients [85]. The fact has to be mentioned that this measure covers only functional outcome of nasal breathing but no psycho-social aspects. Nasal obstruction improved in these prospectively investigated rhinoplasty patients whereby the use of spreader grafts or the reduction of inferior turbinates did not show significant advantages.
A disease-specific measure named Rhinoplasty Outcome Evaluation (ROE) was validated in 2001 reporting the data of 26 patients [71]. Long-term results of revision rhinoplasty were retrospectively investigated with 88% of the patients being satisfied with the result. Satisfaction was reduced with increasing number of revision surgeries [86]. Retrospective assessment of preoperative conditions and ex post comparison with present conditions is intended to compensate the disadvantages of prospective evaluations. The phenomenon of response shift has to be regarded in such questionings. Post-operatively a shift of responses regarding the pre-operative conditions occurs as a result of success or failure of the intervention and the pre-operatively misinterpreted impact of the disease on health status [87].
Furhtermore, the ROE was administered in a prospective study with 58 patients [88]. Independently from the initial indication for surgery (traumatic, aesthetic, functional) improvements of the scores were reported. The authors did not detect any impact of age, gender, or primary versus revision surgery.
3.4 The impact of psyche
The psycho-social effects of rhinoplasty must not be underestimated. Some studies in psychiatric literature report a high incidence of psycho-pathologies in patients desiring rhinoplasty [72], [89], [90]. Furthermore, it has to be pointed out that rhinoplasty significantly changes the appearance of the patient (“type change”) which requires more psychological support compared with restoring interventions like facelift [91]. However, most of the patients benefit from rhinoplasty regardless of the motivation for surgery [92]. These effects continue to exist even 5 years after the operation [93]. Another study confirmed these results and highlighted that the patients felt to be better accepted in social relationships [94].
However, a small group of patients will not be satisfied even if the surgery was objectively successful. These patients who are suffering from Body Dysmorphic Disorder (BDD) or dysmorphophobia count around 5% of all patients desiring for aesthetic surgery. Those patients are typically young, depressive, and anxious. They observe little or imaginary deformities of the nose. They feel unattractive and frequently have multiple bodily complaints [95]. In many cases these patients live in social isolation and have enormous but not warranted expectations regarding post-operative change of life [96]. It is desirable to identify such patients before the operation. However, until now no reliable test exists which fulfils this requirement.
Beside these hardly detectable personality disorders also psychoses and neuroses might complicate the patient management. The potential surgeon should refer the patient to a psychological and/or psychiatric examination to reassess applicability of surgery. In the worst case surgery might lead to exacerbation of a psychiatric disorder.
4 General conclusion
Over the past years several validated QOL measures for rhinologic research have been developed. Therewith, important preconditions for intensified efforts in this research field have been established. However, this should only be regarded as a beginning. The number and quality of studies in rhinologic QOL research related to the evidence criteria of the Oxford Centre for Evidence-based Medicine are not sufficient. Publications in this field rarely reach high levels of evidence. One important challenge for the future is the implementation of rhinologic QOL research using validated measures into randomized, controlled trials. Well-established English QOL instruments should be validated in other languages. Alternatively, new instruments should be developed and validated.
References
- 1.Carr AJ, Gibson B, Robinson PG. Is quality of life determined by expectations or experience? BMJ. 2001;322:1240–1243. doi: 10.1136/bmj.322.7296.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nies C, Celik I, Lorenz W, Koller M, Plaul U, Krack W, Sitter H, Rothmund M. Outcome nach minimal-invasiver Chirurgie – Qualitative Analyse und Bewertung der klinischen Relevanz von Studienendpunkten durch Patient und Arzt. Chirurg. 2001;72:19–29. DOI. 10. doi: 10.1007/s001040051262. [DOI] [PubMed] [Google Scholar]
- 3.Kopp I, Albert US, Lorenz W. Gesamtergebnis diagnostischer und therapeutischer Maßnahmen in der Medizin (Outcome) Gynäkologe. 2002;35:1073–1077. [Google Scholar]
- 4.Kopp I, Müller W, Lorenz W. Die zentrale Rolle von Outcome in Leitlinien und Disease-Management Programmen. HNO Informationen. 2003;28:350–354. [PubMed] [Google Scholar]
- 5.The WHOQOL group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol Med. 1998;28:551–558. doi: 10.1017/S0033291798006667. Available from: http://dx.doi.org/10.1017/S0033291798006667. [DOI] [PubMed] [Google Scholar]
- 6.Browne JP, O'Boyle CA, McGee HM, Joyce CRB, McDonald NJ, O'Malley K, Hiltbrunner B. Individual quality of life in the healthy elderly. Qual Life Res. 1994;3:235–244. doi: 10.1007/BF00434897. Available from: http://dx.doi.org/10.1007/BF00434897. [DOI] [PubMed] [Google Scholar]
- 7.Lawton MP. A multidimensional view of quality of life in frail elders. San Diego, New York, Boston, London, Sydney, Tokyo, Toronto: Academic Press; 1991. [Google Scholar]
- 8.Maille AR, Kaptein AA, de Haes JC, Everaerd WT. Assessing quality of life in chronic non-specific lung disease--a review of empirical studies published between 1980 and 1994. Qual Life Res. 1996;5:287–301. doi: 10.1007/BF00434751. Available from: http://dx.doi.org/10.1007/BF00434751. [DOI] [PubMed] [Google Scholar]
- 9.Kaasa S, Hjermstad MJ, Jordhov MS, Wisloff F, Loge JH. Compliance in quality of life data: a Norwegian experience. Stat Med. 1998;17:623–632. doi: 10.1002/(SICI)1097-0258(19980315/15)17:5/7<623::AID-SIM809>3.0.CO;2-5. Available from: http://dx.doi.org/10.1002/(SICI)1097-0258(19980315/15)17:5/7<623::AID-SIM809>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 10.Bullinger M. Erfassung der gesundheitsbezogenen Lebensqualität mit dem SF-36 Health Survey. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2000;43:190–197. doi: 10.1007/s001030050034. Available from: http://dx.doi.org/10.1007/s001030050034. [DOI] [Google Scholar]
- 11.Schipper H, Clinch J, Olweny C. Quality of life studies: definitions and conceptual issues. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lipincott-Raven Publishers; 1996. pp. 11–23. [Google Scholar]
- 12.Schipper H, Levitt M. Measuring quality of life: risks and benefits. Cancer Treat Rep. 1985;69:1115–1125. [PubMed] [Google Scholar]
- 13.Spilker B. Introduction to the field of quality of life trials. In: Spilker B, editor. Quality of life and pharmaeconomics in clinical trials. Philadelphia: Lipincott-Raven Publishers; 1996. pp. 1–10. [Google Scholar]
- 14.Kornblith AB, Holland JC. Handbook of measures for psychological, social, and physical function in cancer. New York: Memorial Sloan-Kettering Cancer Center; 1994. [Google Scholar]
- 15.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assessment. 1998;2(14) [PubMed] [Google Scholar]
- 16.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273:59–65. [PubMed] [Google Scholar]
- 17.Hopkins C. Patient reported outcome measures in Rhinology. Rhinology. 2009;47:10–17. [PubMed] [Google Scholar]
- 18.International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonized tripartite guidelines. General considerations for clinical trials E8, 17 July 1997. 1997. Available from: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E8/Step4/E8_Guideline.pdf. [Google Scholar]
- 19.Kirkova J, Davies MP, Walsh D, Tiernan E, O'Leary N, LeGrand SB, Lagman RL, Russell KM. Cancer symptom assessment instruments: A systematic review. J Clin Oncol. 2006;24:1459–1473. doi: 10.1200/JCO.2005.02.8332. Available from: http://dx.doi.org/10.1200/JCO.2005.02.8332. [DOI] [PubMed] [Google Scholar]
- 20.Gesundheitsberichterstattung des Bundes. Bonn: Statistisches Bundesamt; 2011. Available from: http://www.gbe-bund.de/ [Google Scholar]
- 21.Jessen M, Malm L. Definition, prevalence and development of nasal obstruction. Allergy. 1997;52(Suppl):3–6. doi: 10.1111/j.1398-9995.1997.tb04876.x. Available from: http://dx.doi.org/10.1111/j.1398-9995.1997.tb04876.x. [DOI] [PubMed] [Google Scholar]
- 22.Buckland JR, Thomas S, Harries PG. Can the Sino-nasal Outcome Test (SNOT-22) be used as a reliable outcome measure for successful septal surgery? Clin Otolaryngol. 2003;28:43–47. doi: 10.1046/j.1365-2273.2003.00663.x. Available from: http://dx.doi.org/10.1046/j.1365-2273.2003.00663.x. [DOI] [PubMed] [Google Scholar]
- 23.Gray LP. Deviated nasal septum. Incidence and etiology. Ann Otol Rhinol Laryngol. 1978;87(Suppl):3–20. doi: 10.1177/00034894780873s201. [DOI] [PubMed] [Google Scholar]
- 24.Baumann I, Baumann H. A new classification of septal deviations. Rhinology. 2007;45:220–223. [PubMed] [Google Scholar]
- 25.Becker SS, Dobratz EJ, Stowell N, Barker D, Park SS. Revision septoplasty: review of sources of persistent nasal obstruction. Am J Rhinol. 2008;22:440–444. doi: 10.2500/ajr.2008.22.3200. Available from: http://dx.doi.org/10.2500/ajr.2008.22.3200. [DOI] [PubMed] [Google Scholar]
- 26.Singh A, Patel N, Kenyon G, Donaldson G. Is there objective evidence that septal surgery improves nasal airflow? J Laryngol Otol. 2006;120:916–920. doi: 10.1017/S0022215106003410. Available from: http://dx.doi.org/10.1017/S0022215106003410. [DOI] [PubMed] [Google Scholar]
- 27.Pirilä T, Tikanto J. Unilateral and bilateral effects of nasal septum surgery demonstrated with acoustic rhinometry, rhinomanometry, and subjective assessment. Am J Rhinol. 2001;15:127–133. doi: 10.2500/105065801781543664. Available from: http://dx.doi.org/10.2500/105065801781543664. [DOI] [PubMed] [Google Scholar]
- 28.Pinkpank A. Beziehungen zwischen Selbsteinstufung der Nasenatmung, Rhinoskopie und Rhinomanometrie. HNO. 1986;34:194–197. [PubMed] [Google Scholar]
- 29.Naito K, Cole P, Chaban R, Oprysk D. Nasal resistance, sensation of obstruction and rhinoscopic findings compared. Am J Rhinol. 1988;2:65–69. doi: 10.2500/105065888781693177. Available from: http://dx.doi.org/10.2500/105065888781693177. [DOI] [Google Scholar]
- 30.Courtiss EH, Goldwyn RM. The effects of nasal surgery on airflow. Plast Reconstr Surg. 1983;72:9–19. doi: 10.1097/00006534-198307000-00003. Available from: http://dx.doi.org/10.1097/00006534-198307000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Sipilä J, Suonpää J. A prospective study using rhinomanometry and patient clinical satisfaction to determine if objective measurements of nasal airway resistance can improve the quality of septoplasty. Eur Arch Otorhinolaryngol. 1997;254:387–390. doi: 10.1007/BF01642556. Available from: http://dx.doi.org/10.1007/BF01642556. [DOI] [PubMed] [Google Scholar]
- 32.Broms P, Jonson B, Malm L. Rhinomanometry. IV. A pre- and postoperative evaluation in functional septoplasty. Acta Otolaryngol. 1982;94:523–529. doi: 10.3109/00016488209128943. Available from: http://dx.doi.org/10.3109/00016488209128943. [DOI] [PubMed] [Google Scholar]
- 33.Farmer SEJ, Eccles R. Chronic inferior turbinate enlargement and the implications for surgical intervention. Rhinology. 2006;44:234–238. [PubMed] [Google Scholar]
- 34.Harrill WC, Pillsbury HC, III, McGuirt WF, Stewart MG. Radiofrequency turbinate reduction: a NOSE evaluation. Laryngoscope. 2007;117:1912–1919. doi: 10.1097/MLG.0b013e3181271414. Available from: http://dx.doi.org/10.1097/MLG.0b013e3181271414. [DOI] [PubMed] [Google Scholar]
- 35.Stewart MG, Smith TL, Weaver EM, Witsell DL, Yueh B, Hannley MT, Johnson JT the NOSE study investgators. Outcomes after nasal septoplasty: Results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004;130:283–290. doi: 10.1016/j.otohns.2003.12.004. Available from: http://dx.doi.org/10.1016/j.otohns.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Lin HC, Lin PW, Su CY, Chang HW. Radiofrequency for the treatment of allergic rhinitis refractory to medical therapy. Laryngoscope. 2003;113:673–678. doi: 10.1097/00005537-200304000-00017. Available from: http://dx.doi.org/10.1097/00005537-200304000-00017. [DOI] [PubMed] [Google Scholar]
- 37.Porter MW, Hales NW, Nease CJ, Krempl GA. Long-term results of inferior turbinate hypertrophy with radiofrequency treatment: a new standard of care? Laryngoscope. 2006;116:554–557. doi: 10.1097/01.MLG.0000201986.82035.6F. Available from: http://dx.doi.org/10.1097/01.MLG.0000201986.82035.6F. [DOI] [PubMed] [Google Scholar]
- 38.Rhee CS, Kim DY, Won TB, et al. Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. Laryngoscope. 2001;111:153–158. doi: 10.1097/00005537-200101000-00026. Available from: http://dx.doi.org/10.1097/00005537-200101000-00026. [DOI] [PubMed] [Google Scholar]
- 39.Coste A, Yona L, Blumen M, et al. Radiofrequency is a safe and effective treatment of turbinate hypertrophy. Laryngoscope. 2001;111:894–899. doi: 10.1097/00005537-200105000-00025. Available from: http://dx.doi.org/10.1097/00005537-200105000-00025. [DOI] [PubMed] [Google Scholar]
- 40.Wittkopf M, Wittkopf J, Russel Ries W. The diagnosis and treatment of nasal valve collaps. Curr Opin Otolaryngol Head Neck Surg. 2008;16:10–13. doi: 10.1097/MOO.0b013e3282f396ef. Available from: http://dx.doi.org/10.1097/MOO.0b013e3282f396ef. [DOI] [PubMed] [Google Scholar]
- 41.Becker SS, Dobratz EJ, Stowell N, Barker D, Park SS. Revision septoplasty: review of sources of persistent nasal obstruction. Am J Rhinol. 2008;22:440–444. doi: 10.2500/ajr.2008.22.3200. Available from: http://dx.doi.org/10.2500/ajr.2008.22.3200. [DOI] [PubMed] [Google Scholar]
- 42.André RF, Vuyk HD. Nasal valve surgery: our experience with the valve suspension technique. Rhinology. 2008;46:66–69. [PubMed] [Google Scholar]
- 43.Kantas I, Balatsouras DG, Vafiadis M, Apostolidou MT, Korres S, Danielidis V. Management of inner nasal valve insufficiency. J Otolaryngol Head Neck Surg. 2008;37:212–218. [PubMed] [Google Scholar]
- 44.Rhee JS, Book DT, Burzynski M, Smith TL. Quality of life assessment in nasal airway obstruction. Laryngoscope. 2003;113:1118–1122. doi: 10.1097/00005537-200307000-00004. Available from: http://dx.doi.org/10.1097/00005537-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Rhee JS, Poetker DM, Smith TL, Bustillo A, Burzynski M, Davies RE. Nasal valve surgery improves disease-specific quality of life. Laryngoscope. 2005;115:437–440. doi: 10.1097/01.mlg.0000157831.46250.ad. Available from: http://dx.doi.org/10.1097/01.mlg.0000157831.46250.ad. [DOI] [PubMed] [Google Scholar]
- 46.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. Available from: http://dx.doi.org/10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 47.Gliklich RE, Hilinski JM. Longitudinal sensitivity of generic and specific health measures in chronic sinusitis. Qual Life Res. 1995;4:27–32. doi: 10.1007/BF00434380. Available from: http://dx.doi.org/10.1007/BF00434380. [DOI] [PubMed] [Google Scholar]
- 48.Becker DG. Sinusitis. J Long Term Eff Med Implants. 2003;13:175–194. doi: 10.1615/JLongTermEffMedImplants.v13.i3.50. Available from: http://dx.doi.org/10.1615/JLongTermEffMedImplants.v13.i3.50. [DOI] [PubMed] [Google Scholar]
- 49.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. Available from: http://dx.doi.org/10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ. 2002;324:1417–1422. doi: 10.1136/bmj.324.7351.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bullinger M, Kirchberger I. SF-36. Handanweisung zum Fragebogen. Göttingen: Hogrefe; 1998. [Google Scholar]
- 52.Siegel NS, Gliklich RE, Taghizadeh F, Chang Y. et al. Outcomes of septoplasty. Otolaryngol Head Neck Surg. 2000;112:228–232. doi: 10.1016/S0194-5998(00)70244-0. Available from: http://dx.doi.org/10.1016/S0194-5998(00)70244-0. [DOI] [PubMed] [Google Scholar]
- 53.Arunchalam PS, Kitcher E, Gray J, Wilson JA. Nasal septum surgery: evaluation of symptomatic and general health outcomes. Clin Otolaryngol. 2001;26:367–370. doi: 10.1046/j.0307-7772.2001.00481.x. Available from: http://dx.doi.org/10.1046/j.0307-7772.2001.00481.x. [DOI] [PubMed] [Google Scholar]
- 54.Busaba NY, Hossain M. Clinical outcome of septoplasty and inferior turbinate reduction in the geriatric veterans' population. Am J Rhinol. 2004;18:343–347. [PubMed] [Google Scholar]
- 55.Bhattacharyya N. Symptom and disease severity differences between nasal septal deviation and chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;133:173–177. doi: 10.1016/j.otohns.2005.03.082. Available from: http://dx.doi.org/10.1016/j.otohns.2005.03.082. [DOI] [PubMed] [Google Scholar]
- 56.Baumann I, Blumenstock G, Praetorius M, Sittel C, Piccirillo JF, Plinkert PK. Krankheitsspezifische und allgemeine gesundheitsbezogene Lebensqualität bei Patienten mit chronischer Rhinosinusitis. HNO. 2006;54:544–549. doi: 10.1007/s00106-006-1402-y. [DOI] [PubMed] [Google Scholar]
- 57.Metson RB, Gliklich RE. Clinical outcomes in patients with chronic sinusitis. Laryngoscope. 2000;94(110 Suppl):24–28. doi: 10.1097/00005537-200003002-00007. Available from: http://dx.doi.org/10.1097/00005537-200003002-00007. [DOI] [PubMed] [Google Scholar]
- 58.Konstantinidis I, Triaridis S, Triaridis A, Karagiannidis K, Kontzoglou G. Long term results following nasal septal surgery. Focus on patients' satisfaction. Auris Nasus Larynx. 2005;32:369–374. doi: 10.1016/j.anl.2005.05.011. Available from: http://dx.doi.org/10.1016/j.anl.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 59.Baumann I, Blumenstock G, Klingmann C, Praetorius M, Plinkert PK. Subjektive Nutzenbewertung 1 Jahr nach funktioneller endonasaler Nasennebenhöhlenoperation bei Patienten mit chronischer Rhinosinusitis. HNO. 2007;55:858–861. doi: 10.1007/s00106-006-1529-x. [DOI] [PubMed] [Google Scholar]
- 60.Newton JR, Shakeel M, Ram B. Evaluation of endoscopic sinus surgery by Glasgow benefit inventory. J Laryngol Otol. 2008;122:357–360. doi: 10.1017/S0022215107008936. Available from: http://dx.doi.org/10.1017/S0022215107008936. [DOI] [PubMed] [Google Scholar]
- 61.Bohlin L, Dahlqvist A. Nasal airway resistance and complications following functional septoplasty: A ten-year follow-up study. Rhinology. 1994;32:195–197. [PubMed] [Google Scholar]
- 62.Samad I, Stevens HE, Maloney A. The efficacy of nasal septal surgery. J Otolaryngol. 1992;21:88–91. [PubMed] [Google Scholar]
- 63.Denholm SW, Sim DW, Sanderson RJ, Mountain RE, Marais J, Maran AG. Otolaryngological indicator operations: one year's experience. J R Coll Surg Edinb. 1993;38:1–3. [PubMed] [Google Scholar]
- 64.Sherman AH. A study of nasal airway function in the postoperative period of nasal surgery. Laryngoscope. 1977;87:299–303. doi: 10.1288/00005537-197703000-00001. Available from: http://dx.doi.org/10.1288/00005537-197703000-00001. [DOI] [PubMed] [Google Scholar]
- 65.Stocksted P. Long-term results, following plastic septum surgery. Rhinology. 1969;7:53–61. [Google Scholar]
- 66.Jessen M, Ivarsson A, Malm L. Nasal airway resistance and symptoms after functional septoplasty: comparison of findings at 9 months and 9 years. Clin Otolaryngol Allied Sci. 1989;14:231–234. doi: 10.1111/j.1365-2273.1989.tb00366.x. Available from: http://dx.doi.org/10.1111/j.1365-2273.1989.tb00366.x. [DOI] [PubMed] [Google Scholar]
- 67.Dinis PB, Haider H. Septoplasty: Long-term evaluation of results. Am J Otolaryngol. 2002;23:85–90. doi: 10.1053/ajot.2002.30987. Available from: http://dx.doi.org/10.1053/ajot.2002.30987. [DOI] [PubMed] [Google Scholar]
- 68.Bothra R, Mathur NN. Comparative evaluation of conventional versus endoscopic septoplasty for limited septal deviation and spur. J Laryngol Otol. 2008;123(7):737–747. doi: 10.1017/S0022215108004192. Available from: http://dx.doi.org/10.1017/S0022215108004192. [DOI] [PubMed] [Google Scholar]
- 69.Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) Scale. Otolaryngol Head Neck Surg. 2004;130:157–163. doi: 10.1016/j.otohns.2003.09.016. Available from: http://dx.doi.org/10.1016/j.otohns.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 70.Most SP. Anterior septal reconstruction. Outcomes after a modified extracorporeal septoplasty technique. Arch Facial Plast Surg. 2006;8:202–207. doi: 10.1001/archfaci.8.3.202. Available from: http://dx.doi.org/10.1001/archfaci.8.3.202. [DOI] [PubMed] [Google Scholar]
- 71.Alsarraf R, Larrabee WF, Jr, Anderson S, Murakami CS, Johnson CM. Measuring cosmetic facial plastic outcomes. A pilot study. Arch Facial Plast Surg. 2001;3:198–201. doi: 10.1001/archfaci.3.3.198. Available from: http://dx.doi.org/10.1001/archfaci.3.3.198. [DOI] [PubMed] [Google Scholar]
- 72.Hern J, Hamann J, Tostevin P, Rowe-Jones J, Hinton A. Assessing psychological morbidity in patients with nasal deformity using the CORE questionnaire. Clin Otolaryngol. 2002;27:359–364. doi: 10.1046/j.1365-2273.2002.00595.x. Available from: http://dx.doi.org/10.1046/j.1365-2273.2002.00595.x. [DOI] [PubMed] [Google Scholar]
- 73.Most SP, Alsarraf R, Larrabee WF. Outcomes of facial cosmetic procedures. Facial Plast Surg. 2002;18:119–124. doi: 10.1055/s-2002-32202. Available from: http://dx.doi.org/10.1055/s-2002-32202. [DOI] [PubMed] [Google Scholar]
- 74.Toriumi DM, Josen J, Weinberger M, Tardy ME Jr. Use of alar batten grafts for correction of nasal valve collaps. Arch Otolaryngol Head Neck Surg. 1997;123:802–808. doi: 10.1001/archotol.1997.01900080034002. [DOI] [PubMed] [Google Scholar]
- 75.Guyuron B, Bokhari F. Patient satisfaction following rhinoplasty. Aest Plast Surg. 1996;20:153–157. doi: 10.1007/BF02275535. Available from: http://dx.doi.org/10.1007/BF02275535. [DOI] [PubMed] [Google Scholar]
- 76.Constantinides MS, Adamson PA, Cole P. The long-term effects of open cosmetic septorhinoplasty on nasal air flow. Arch Otolaryngol Head Neck Surg. 1996;122:41–45. doi: 10.1001/archotol.1996.01890130035005. [DOI] [PubMed] [Google Scholar]
- 77.McKee GJ, O'Neill G, Roberts C, Lesser TH. Nasal airflow after septorhinoplasty. Clin Otolaryngol Allied Sci. 1994;19:254–257. doi: 10.1111/j.1365-2273.1994.tb01226.x. Available from: http://dx.doi.org/10.1111/j.1365-2273.1994.tb01226.x. [DOI] [PubMed] [Google Scholar]
- 78.Dziewulski P, Dujon D, Spyriounis P, et al. A retrospective analysis of the results of 218 consecutive rhinoplasties. Br J Plast Surg. 1995;48:451–454. doi: 10.1016/0007-1226(95)90119-1. Available from: http://dx.doi.org/10.1016/0007-1226(95)90119-1. [DOI] [PubMed] [Google Scholar]
- 79.Alsarraf R. Outcomes instruments in facial plastic surgery. Facial Plast Surg. 2002;18:77–86. doi: 10.1055/s-2002-32197. Available from: http://dx.doi.org/10.1055/s-2002-32197. [DOI] [PubMed] [Google Scholar]
- 80.Klassen A, Jenkinson C, Fitzpatrick R, Goddacre T. Patients' health related quality of life before and after aesthetic surgery. Br J Plast Surg. 1996;49:433–438. doi: 10.1016/S0007-1226(96)90025-9. Available from: http://dx.doi.org/10.1016/S0007-1226(96)90025-9. [DOI] [PubMed] [Google Scholar]
- 81.Cole RP, Shakespeare V, Shakespeare P, Hobby JAE. Measuring outcome in low-priority plastic surgery patients using quality of life indices. Br J Plast Surg. 1994;47:117–121. doi: 10.1016/0007-1226(94)90170-8. Available from: http://dx.doi.org/10.1016/0007-1226(94)90170-8. [DOI] [PubMed] [Google Scholar]
- 82.Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol. 1996;105:415–422. doi: 10.1177/000348949610500601. [DOI] [PubMed] [Google Scholar]
- 83.Stewart EJ, Robinson K, Wilson JA. Assessing of patient's benefit from rhinoplasty. Rhinology. 1996;34:57–59. [PubMed] [Google Scholar]
- 84.Slator R. Rhinoplasty patients revisited. Br J Plast Surg. 1993;46:327–331. doi: 10.1016/0007-1226(93)90014-3. Available from: http://dx.doi.org/10.1016/0007-1226(93)90014-3. [DOI] [PubMed] [Google Scholar]
- 85.Most SP. Analysis of outcomes after functional rhinoplasty using a disease-specific quality-of-life instrument. Arch Facial Plast Surg. 2006;8:306–309. doi: 10.1001/archfaci.8.5.306. Available from: http://dx.doi.org/10.1001/archfaci.8.5.306. [DOI] [PubMed] [Google Scholar]
- 86.Hellings PW, Nolst Trenite GJ. Long-term patient satisfaction after revision rhinoplasty. Laryngoscope. 2007;117:985–989. doi: 10.1097/MLG.0b013e31804f8152. Available from: http://dx.doi.org/10.1097/MLG.0b013e31804f8152. [DOI] [PubMed] [Google Scholar]
- 87.Timmerman AA, Anteunis LJ, Meesters CM. Response-shift bias and parent-reported quality of life in children with otitis media. Arch Otolaryngol Head Neck Surg. 2003;129:987–991. doi: 10.1001/archotol.129.9.987. Available from: http://dx.doi.org/10.1001/archotol.129.9.987. [DOI] [PubMed] [Google Scholar]
- 88.Meningaud JP, Lantieri L, Bertrand JC. Rhinoplasty: An outcome research. Plast Reconstr Surg. 2008;121:251–257. doi: 10.1097/01.prs.0000293866.57517.d4. Available from: http://dx.doi.org/10.1097/01.prs.0000293866.57517.d4. [DOI] [PubMed] [Google Scholar]
- 89.Jerome L. Body dysmorphic disorder: a controlled study of patients requesting cosmetic rhinoplasty. Am J Psychiatry. 1992;149:577–578. doi: 10.1176/ajp.149.4.577. [DOI] [PubMed] [Google Scholar]
- 90.Thomas CS, Goldberg DP. Appearance, body image and distress in facial dysmorphophobia. Acta Psychiatr Scand. 1995;92:231–236. doi: 10.1111/j.1600-0447.1995.tb09574.x. Available from: http://dx.doi.org/10.1111/j.1600-0447.1995.tb09574.x. [DOI] [PubMed] [Google Scholar]
- 91.Castle DJ, Honigman RJ, Phillips KA. Does cosmetic surgery improve psychosocial wellbeing? Med J Aust. 2002;176:601–604. doi: 10.5694/j.1326-5377.2002.tb04593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ercolani M, Baldoro B, Rossi N, Trombini E, Trombini G. Short-term outcome of rhinoplasty for medical or cosmetic indication. J Psychosom Res. 1999;47:277–281. doi: 10.1016/S0022-3999(99)00042-2. Available from: http://dx.doi.org/10.1016/S0022-3999(99)00042-2. [DOI] [PubMed] [Google Scholar]
- 93.Ercolani M, Baldoro B, Rossi N, Trombini G. Five-year follow-up of cosmetic rhinoplasty. J Psychosom Res. 1999;47:283–286. doi: 10.1016/S0022-3999(99)00041-0. Available from: http://dx.doi.org/10.1016/S0022-3999(99)00041-0. [DOI] [PubMed] [Google Scholar]
- 94.Dinis PB, Dinis M, Gomes A. Psychosocial consequences of nasal aesthetic and functional surgery: a controlled prospective study in an ENT setting. Rhinology. 1998;36:32–36. [PubMed] [Google Scholar]
- 95.Phillips KA, Dufresne RG. Body Dismorphic Disorder. A guide for dermatologists and cosmetic surgeons. Am J Clin Dermatol. 2000;1:235–243. doi: 10.2165/00128071-200001040-00005. Available from: http://dx.doi.org/10.2165/00128071-200001040-00005. [DOI] [PubMed] [Google Scholar]
- 96.Veale D, De Haro L, Lambrou C. Cosmetic rhinoplasty in body dysmorphic disorder. Br J Plast Surg. 2003;56:546–551. doi: 10.1016/S0007-1226(03)00209-1. Available from: http://dx.doi.org/10.1016/S0007-1226(03)00209-1. [DOI] [PubMed] [Google Scholar]