Abstract
Introduction:
Stopping smoking results in weight gain. Avoidance of alcohol is often advocated to reduce cues to smoking, but the effect of alcohol consumption on body weight is unclear.
Methods:
We used regression models to examine weight change by baseline alcohol consumption in quitting and continuing smokers. Weight was measured at baseline and at 8 years, and weekly alcohol consumption was reported at baseline in participants from the Oxfordshire general practices nicotine patch/placebo trial. Of 698 smokers attempting to stop smoking, 85 were abstinent for 8 years and 613 continued to smoke.
Results:
The association between baseline alcohol consumption and weight change depended upon smoking status (p for interaction = .019). In smokers, there was no association with weight change, 0.005 (95% CI: −0.037 to 0.056) kg per UK unit (U) (8 g of ethanol) consumed each week. This was unmodified by gender and baseline body mass index (BMI). In quitters, there was a negative association with weight change, −0.174 (95% CI: −0.315 to −0.034) kg per U consumed each week (unmodified by gender and baseline BMI). Quitters who consumed 14 U (112 g ethanol) a week weighed a mean 2.4 kg less than quitters who did not drink.
Conclusions:
Quitting smokers who drink more alcohol appear to gain less weight after quitting than those who do not drink. This is consistent across studies, it may be accounted for by unmeasured confounders or it may be that alcohol reduces weight gain. If alcohol reduces weight gain, the advice for quitting smokers must balance the benefits and hazards of alcohol consumption. However, there is currently insufficient evidence to advise quitters who drink little or no alcohol to increase consumption.
Introduction
Eighty-three percent of quitting smokers gain weight, on average, 7 kg more than if they had continued to smoke (Lycett, Munafo, Johnstone, Murphy, & Aveyard, 2011). Preventing this weight gain is important because it reduces the health benefits otherwise seen by quitting (Chinn et al., 2005; Davey-Smith et al., 2005; Gerace, Hollis, Ockene, Svendsen, 1991). Avoidance of alcohol is often advocated in smoking cessation support to reduce cues to smoking. People trying to lose weight are often advised to moderate or avoid alcohol because of its relatively high combustible energy value. However, there is contrary evidence on the effect of alcohol on weight gain.
Laboratory studies of the metabolic effects of alcohol show three important effects on energy balance. First, alcohol increases energy intake (Buemann, 2002; Tremblay et al., 1995; Westerterp-Plantenga & Verwegen, 1999), particularly when consumed in combination with fat (Tremblay & St-Pierre, 1996) and the extra energy from alcohol is not compensated for by reducing subsequent food intake (De Castro & Orozco, 1990; Tremblay et al.,1995; Tremblay & St-Pierre, 1996; Yeomans, 2004). Second, alcohol suppresses fat oxidation, which increases fat storage (Suter, Schutz, & Jequier, 1992). Third, alcohol increases 24-h energy expenditure through inducing thermogenesis by up to 30%. Dietary-induced thermogenesis from alcohol is greater than that from carbohydrate, fat, or protein (Raben, Agerholm-Larsen, Flint, Holst, & Astrup, 2003; Schutz, 2000; Suter, Jequier, & Schutz, 1994; Westerterp, 2004). The first two effects point toward alcohol promoting weight gain and the last effect works against it. So what causes the balance to tip one way or the other?
The answer may depend on the pathway by which alcohol is metabolized. The alcohol dehydrogenase (ADH) pathway produces ATP more efficiently than the microsomal ethanol-oxidizing system (MEOS). It is thought that low levels of alcohol are metabolized by ADH, whereas a high blood concentration of alcohol induces MEOS; and this accounts for the high energy expenditure in people with alcohol dependence (Levine, Harris, Morgan, 2000; Suter, 2005). The threshold level of alcohol for MEOS induction is unknown, but individual variation of body weight, smoking status, gender, and genetic variation in enzymes metabolizing alcohol may explain the different effects of alcohol on body weight (Suter, 2005).
Population studies have shown inconsistent results, although this has been explained in part by drinking patterns, smoking status (Cooke, Frost, & Thornell, 1982; Mannisto et al., 1996; Tolstrup et al., 2005, 2008), and gender effects (women who drink alcohol seem to gain less weight) (Breslow & Smothers, 2005; Colditz et al., 1991; Gordon, Joseph, & Doyle, 1986; Gordon & Kannel, 1983; Hellerstedt, Jeffery, & Murray, 1990; Wang, Lee, Nanson, Buring, & Sesso, 2010; Wannamethee, Field, Colditz, & Rimm, 2004; Wannamethee & Shaper, 2003) (Further discussion in Supplementary web appendix 1).
In the few short-term randomized trials, alcohol consumption did not influence weight in obese people (Beulens, vanBeers, Stolk, Schaafsma, & Hendricks, 2006), but alcohol reduced weight in lean people (Clevidence, Taylor, Campbell, & Judd, 1995, Crouse & Grundy, 1984).
Three prospective studies have considered the effects of alcohol on body weight around the time of quitting smoking; these have all found an inverse effect of alcohol consumption and weight gain (Froom et al., 1999; Kawachi, Troisi, Rotnitzky, Coakley, & Colditz, 1996; Nides et al., 1994). However, these studies did not fully explore the association according to smoking status. The weight gain trajectory in quitting and continuing smokers is very different; our paper is the first to investigate the effect of alcohol consumption on post cessation weight gain in both continuously abstinent quitters and continuing smokers.
Materials and Methods
Participants
Participants from the Oxford, U.K. patch/placebo trial were followed up at 3, 6, and 12 months and 8 years (Fowler, 1994; Imperial Cancer research Fund General Practice Research Group, 1993; Yudkin et al., 2003). Eighty-five participants were continuously abstinent from 3 months to 8 years (“quitters”) and 613 smoked continuously (“smokers”) (Further details of participants in Supplementary web appendix 2). Quitters gained 8.79 kg, (SD 6.36) (95% CI 7.42, 10.17) over eight years and continuous smokers gained 2.24 kg (SD 6.65), (95% CI 1.70, 2.77) (Lycett et al., 2011).
Ethical approval for this was granted by the Central Oxford Ethics committee (ICRF, 1993), Anglia and Oxford Multicentre Research Ethics Committee, and 86 local research ethics committees (Yudkin et al., 2003).
Measurements
Smoking Status
During the nicotine patch use, smoking abstinence was confirmed by expired CO < 10 ppm and later by salivary cotinine <20 ng/ml.
Weight Gain
Height and weight were measured at trial entry; this was self-reported in some at baseline and all at 8-year follow-up. We found no significant differences between self-reported and measured weight or BMI (Lycett et al., 2011). Change in weight was taken as weight (kg) at 8 years minus weight at baseline (kg).
Alcohol Consumption
Baseline data on weekly units of alcohol was collected by a trained nurse interviewer. Participants reported daily consumption of different drink types; these were converted to UK units (U) (equivalent to 8 g ethanol) per week.
Analysis
Linear regression analysis was used with the combined cohort of continuous smokers and quitters to examine the association between baseline alcohol consumption and weight change. We used higher order terms to investigate curvilinear relationships. We investigated effect modification by gender, baseline BMI, and smoking status. As smoking status modified the association between alcohol and weight change, separate regression equations were used for smokers and quitters. Confounding was controlled for, categorical variables (treatment allocation, gender, ethnic group, and socio-economic status measured by occupation [Registrar General’s classification; Drudy, 1991]) were recoded into dummy variables. Continuous variables (BMI, height, age, number cigarettes/day, cigarette dependence measured by the Horn Russell score; [Russell, 1974], and weekly alcohol consumption) were mean-centered. To avoid over-fitting, these potential confounders were entered in a stepwise selection process with a p value of .2 for model entry (Rothman & Greenland, 1998). We used Cook’s distance to assess for outliers.
Results
Baseline Characteristics
Baseline characteristics can be found in Table 1 in the Supplementary web appendix 2.
Baseline Alcohol Consumption as an Effect Modifier of Weight Change According to Smoking Status
In the model including smokers and quitters, baseline alcohol consumption was not associated with weight change. However, there was a significant interaction between smoking status and alcohol consumption before (p = .019) and after (p = .010) adjustment for confounding variables.
Association Between Alcohol Consumption and Weight Change in Smokers
Separate linear regression modeling in smokers found no association between alcohol consumption and weight gain (regression coefficient: 0.005, 95% CI −0.037, 0.046; p = .827). This effect did not differ by gender, (p for interaction was .73) or baseline BMI (p for interaction term .91).
Association Between Alcohol Consumption and Weight Change in Quitters
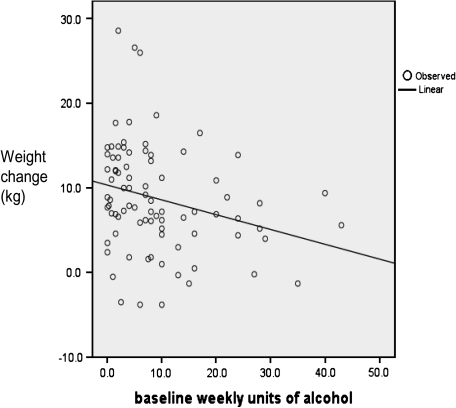
There was a significant, negative linear relationship between weight change and alcohol consumption in quitters (p = .015, r2 = .070). For every additional unit of alcohol consumed per week at time of quitting, mean weight change over eight years was −0.174 kg (95% CI: −0.315 to −0.034) p=.015 (unadjusted) (Figure 1.) (adjusted: −0.180 kg [95% CI: −0.318 to −0.043] p = .011). Fit did not improve with higher order terms and effect did not differ by gender (p for interaction was .91). This equates to those who drink alcohol at the maximum U.K. recommended weekly intake for women (14 U or 112 g ethanol) would weigh a mean 2.4 kg less than those who did not drink.
Figure 1.
Weight change over 8 years according to baseline alcohol consumption in quitters (n=84).
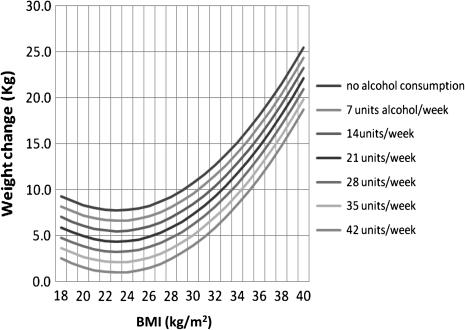
Variability of Weight Change in Quitters According to Baseline Alcohol Consumption and BMI
We have previously demonstrated that 11% of the variability in weight gain in quitters was accounted for by a J-shaped curve with baseline BMI (Lycett et al., 2011). There is no evidence that the association between alcohol and weight gain is modified by baseline BMI (p for interaction was .29). The associations of BMI and alcohol consumption are therefore independent, together they account for 17% of the variability of weight gain in quitters (Table 2 in Supplementary web appendix 3). The regression lines for mean population weight gain according to BMI at different levels of alcohol consumption are plotted (Figure 2).
Figure 2.
Weight change over 8 years according to body mass index (BMI) and baseline alcohol consumption in quitters.
Discussion
Moderate drinking, with the potential to prevent a weight gain of 2.4 kg over eight years (0.3 kg/year), in a population of ex-smokers could have a significant public health impact. An increase of 0.7 kg/year has been shown to increase the risk of developing diabetes by 86% in those with impaired fasting glycemia (Gautier et al., 2010). Those who quit smoking are at increased risk of developing diabetes for a few years after cessation, which is unexplained by weight gain alone (Hur et al., 2007; Wannamethee, Shaper, & Perry, 2001, Yeh, Duncab, Schmidt, Want, & Brancati, 2010); there is also consistent systematic review evidence which shows moderate alcohol consumption is associated with the lowest risk of developing diabetes (Baliunas et al., 2009; Koppes, Dekker, Hendriks, Bouter, & Heine, 2005).
The Role of Bias
The strength of this study lies in the long-term follow-up and the determination of continuous smoking abstinence, which was biochemically verified at each timepoint (self-report and point prevalence abstinence may overestimate quit rates and thus underestimate weight gain [Klesges et al., 1989, 1997]).
Although we found no significant differences between measured and self-reported weight or weight change, we cannot exclude the possibility that weight may have been underestimated, particularly in heavier individuals, for reasons of social desirability. Similarly alcohol consumption may have been underreported. However, underreporting of both measures could not account for the association we observed. For underreporting to explain the association, those who underreported weight would have had to over-report alcohol consumption and/or vice versa and this seems counterintuitive.
Alcohol was measured by careful questioning at baseline only. There is evidence that a single measure of alcohol consumption is a reasonable estimate of average alcohol consumption over several years. The Nurses’ Health Study showed a high correlation between alcohol intake at a single point in time and alcohol intake over the following 6 years (R = .75) (Giovannucci et al., 1991). Also there is evidence from a large cohort that alcohol consumption does not change as a consequence of quitting smoking (Murray, Istvan, & Voelker, 1996).
The Role of Confounding
It is possible that confounding explains the association. As this was a smoking cessation trial, analyses on weight change were not planned; consequently, behaviors such as diet and physical activity were not assessed. It is possible that those who drank more alcohol at baseline also had better dietary behavior and did more physical activity (Westerterp, Meijer, Goris, & Kester 2004) than those who drank less, although most studies report lower weight gain after adjusting for these confounders (Wang, Lee, Nanson, Buring, & Sesso, 2010; Wannamethee & Shaper, 2003; Wannamethee et al., 2004). We explored this in an ex-smoking population using data from the Health Survey for England. We found a small positive association between alcohol intake and physical activity, but this was far less than the additional daily 45–60 min of moderate activity required to prevent weight gain (Saris et al., 2003; Wareham, van Sluijs, & Ekelund, 2005). We found inconsistent associations of nine indicators of a healthy diet with alcohol consumption. All these were too small to be meaningful (Details in Supplementary web appendix 4). Physical activity and diet are therefore unlikely to confound our results, but studies that measure and adjust for these within the same study population are needed.
Consistency of Findings
Cohort studies have shown higher alcohol consumption attenuates the rise in BMI associated with quitting smoking (Froom et al., 1999), even after adjustment for physical activity (Kawachi et al., 1996). However, these have not provided evidence of effect modification by smoking status.
The Lung Health Study (Nides et al., 1994) used similar measures of smoking status and alcohol consumption to our own. Equating their findings to UK units gave regression coefficients of −0.083 and −0.132 for men and women, respectively; these values fit within the 95% CIs of our mixed sample but suggest a slightly lower effect than we found.
Conclusion
A complex association exists between alcohol consumption and weight gain. We have found a dose response relationship in quitting smokers, which is consistent across studies. It is plausible that MESO induction may play a role in this. Therefore, advice to reduce alcohol consumption in this population may promote rather that prevent weight gain. Studies are needed to investigate the mechanisms of alcohol metabolism in quitting smokers and weigh the adverse health consequences of increasing alcohol against the benefit of smaller weight gain. Increasing alcohol should not currently be advised for preventing weight gain during smoking cessation.
Supplementary Material
Supplementary Materials can be found online at http://www.ntr.oxfordjournals.org
Funding
The original trial and 8-year follow-up was funded by Cancer Research U.K. D.L. has a PhD studentship funded by UK Centre for Tobacco Control Studies (UKCTCS); a UKCRC Public Health Research: Centre of Excellence. Funding from British Heart Foundation, Cancer Research U.K., Economic and Social Research Council, Medical Research Council, and the Department of Health, under the auspices of the U.K. Clinical Research Collaboration, is gratefully acknowledged. The National Institute of Health Research (NIHR) funds P.A.
Declaration of Interests
P.A. has done consultancy work on smoking cessation for Pfizer, McNeil, and Xenova Biotechnology. M.M. has received fees for invited lectures from the National Health Service, GlaxoSmithKline, Novartis, the Moffitt Cancer Research Center and the Karolinska Instituet and received benefits in kind (hospitality, etc.) from various pharmaceutical companies. He has received research and travel support from the European Research Advisory Board, GlaxoSmithKline, Pfizer Consumer Healthcare and Novartis. Consultancy has been provided to the European Commission, The American Institutes for Research, the National Audit Office and G-Nostics Ltd. E.J. has received consultancy income from European Network for Smoking Prevention. M.M. has received consultancy income from the European Network for Smoking Prevention and has provided scientific consultancy services through the University of Oxford ISIS Innovation to the National Audit Office and G-Nostics Ltd.
Supplementary Material
Acknowledgments
Funding from British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, and the Department of Health, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
References
- Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, et al. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;32:2123–2132. doi: 10.2337/dc09-0227. doi:10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beulens JWJ, vanBeers RM, Stolk RP, Schaafsma G, Hendricks HFJ. The effect of moderate alcohol consumption on fat distribution and adipocytokine. Obesity. 2006;14(1):60–66. doi: 10.1038/oby.2006.8. doi:10.1038/oby.2006.8. [DOI] [PubMed] [Google Scholar]
- Breslow RA, Smothers BA. Drinking patterns and body mass index in never smokers: National Health Interview Survey, 1997–2001. American Journal of Epidemiology. 2005;161:368–376. doi: 10.1093/aje/kwi061. doi:10.1093/aje/kwi061. [DOI] [PubMed] [Google Scholar]
- Buemann B. The effect of wine or beer versus a carbonated soft drink, served at a meal, on ad libitum energy intake. International Journal of Obesity. 2002;26:1367–1372. doi: 10.1038/sj.ijo.0802069. doi:10.1038/sj.ijo.0802069. [DOI] [PubMed] [Google Scholar]
- Chinn S, Jarvis D, Melotti R, Luczynska C, Ackermann-Liebrich U, Anto JM, et al. Smoking cessation, lung function, and weight gain: A follow-up study. The Lancet. 2005;365:1629–1635. doi: 10.1016/S0140-6736(05)66511-7. doi:10.1016/S0140-6736(05)66511-7. [DOI] [PubMed] [Google Scholar]
- Clevidence BA, Taylor PR, Campbell WS, Judd JT. Lean and heavy women may not use energy from alcohol with equal efficiency. Journal of Nutrition. 1995;125:2536–2540. doi: 10.1093/jn/125.10.2536. [DOI] [PubMed] [Google Scholar]
- Colditz GA, Giovannucci E, Rimm EB, Stampfer MJ, Rosner B, Speizer FE, et al. Alcohol intake in relation to diet and obesity in women and men. American Journal of Clinical Nutrition. 1991;54:49–55. doi: 10.1093/ajcn/54.1.49. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Cooke KM, Frost GW, Thornell IR. Alcohol consumption and blood pressure. Survey of the relationship at a health-screening clinic. Medical Journal Australia. 1982;1:65–69. [PubMed] [Google Scholar]
- Crouse JR, Grundy SM. Effects of alcohol on plasma lipoproteins and cholesterol and triglyceride metabolism in man. Journal of Lipid Research. 1984;25:486–496. Retrieved from http://www.jlr.org. [PubMed] [Google Scholar]
- Davey-Smith G, Bracha Y, Svendsen KH, Neaton JD, Haffner SM, Kuller LH, et al. Incidence of type 2 diabetes in the randomized multiple risk factor intervention trial. Annals of Internal Medicine. 2005;142:313–322. doi: 10.7326/0003-4819-142-5-200503010-00006. Retrieved from http://www.annals.org/content/142/5/313.full.pdf. [DOI] [PubMed] [Google Scholar]
- De Castro JM, Orozco S. Moderate alcohol intake and spontaneous eating patterns of humans: Evidence of unregulated supplementation. American Journal of Clinical Nutritionr. 1990;52:246–253. doi: 10.1093/ajcn/52.2.246. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Drudy S. The classification of social class in sociological research. The British Journal of Sociology. 1991;42:21–41. Retrieved from http://www.jstor.org/stable/590833. [Google Scholar]
- Fowler G. Randomised trial of nicotine patches in general practice: Results at one year. British Medical Journal. 1994;308:1476–1477. Retrieved from http://www.bmj.com. [PMC free article] [PubMed] [Google Scholar]
- Froom P, Kristal-Boneh E, Melamed S, Gofer D, Benbassat J, Ribak J. Smoking cessation and body mass index of occupationally active men: The Israeli CORDIS Study. American Journal of Public Health. 1999;89:718–722. doi: 10.2105/ajph.89.5.718. Retrieved from http://www.ajph.alphapublications.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier A, Roussel R, Ducluzeau PH, Lange C, Vol S, Balkau B, et al. Increases in waist circumference and weight as predictors of type 2 diabetes in individuals with impaired fasting glucose: Influence of baseline BMI: Data from the DESIR study. Diabetes Care. 2010;33:1850–1852. doi: 10.2337/dc10-0368. doi:10.2337/dc10-0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerace TA, Hollis JF, Ockene JK, Svendsen KH. Smoking cessation and change in diastolic blood pressure, body weight, and plasma lipids. MRFIT Research Group. Preventive Medicine. 1991;20:602–620. doi: 10.1016/0091-7435(91)90058-c. [DOI] [PubMed] [Google Scholar]
- Giovannucci E, Colditz G, Stampfer MJ, Rimm EB, Ljtjn L, Sampson L, et al. The assessment of alcohol consumption by a simple self-administered questionnaire. American Journal of Epidemiology. 1991;133:812–817. doi: 10.1093/oxfordjournals.aje.a115960. Retrieved from http://www.aje.oxfordjournals.org. [DOI] [PubMed] [Google Scholar]
- Gordon T, Joseph T, Doyle JT. Alcohol consumption and its relationship to smoking, weight, blood pressure, and blood lipids. The Albany Study. Archives of Internal Medicine. 1986;146:262–265. Retrieved from http://www.archinte.ama-assn.org. [PubMed] [Google Scholar]
- Gordon T, Kannel B. Drinking and its relation to smoking, BP, blood lipids, and uric acid. The Framingham Study. Archives of Internal Medicine. 1983;143:1366–1374. [PubMed] [Google Scholar]
- Hellerstedt JWI, Jeffery JRW, Murray DM. The association between alcohol intake and adiposity in the general population. American Journal of Epidemiology. 1990;132:594–611. doi: 10.1093/oxfordjournals.aje.a115703. Retrieved from http://www.aje.oxfordjournals.org. [DOI] [PubMed] [Google Scholar]
- Hur NW, Kim HC, Nam CM, Jee SH, Lee HC, Suh I. Smoking cessation and risk of type 2 diabetes mellitus: Korea Medical Insurance Corporation Study. European Journal of Cardiovascular Prevention and Rehabilitation. 2007;14:244–249. doi: 10.1097/01.hjr.0000239474.41379.79. [DOI] [PubMed] [Google Scholar]
- Imperial Cancer research Fund General Practice Research Group. Effectiveness of a nicotine patch in helping people stop smoking: Results of a randomised trial in general practice. British Medical Journal. 1993;306:1304–1308. doi: 10.1136/bmj.306.6888.1304. doi:10.1136/bmj.306.6888.1304 Retrieved from http://www.bmj.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Troisi RJ, Rotnitzky AG, Coakley EH, Colditz GA. Can physical activity minimize weight gain in women after smoking cessation? American Journal of Public Health. 1996;86:999–1004. doi: 10.2105/ajph.86.7.999. Retrieved from http://www.ajph.alphapublications.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. Smoking, body weight and their effects on smoking behavior: A comprehensive review of the literature. Psychological Bulletin. 1989;106:204–230. doi: 10.1037/0033-2909.106.2.204. doi:10.1037/0033-2909.106.2.204. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of Consulting & Clinical Psychology. 1997;65:286–291. doi: 10.1037//0022-006x.65.2.286. doi:10.1037/0022-006X.65.2.286. [DOI] [PubMed] [Google Scholar]
- Koppes LLJ, Dekker JM, Hendriks HFJ, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: A meta-analysis of prospective observational studies. Diabetes Care. 2005;28:719–725. doi: 10.2337/diacare.28.3.719. doi:10.2337/diacare.28.3.719. [DOI] [PubMed] [Google Scholar]
- Levine JA, Harris MM, Morgan MY. Energy expenditure in chronic alcohol abuse. European Journal of Clinical Investigation. 2000;30:779–786. doi: 10.1046/j.1365-2362.2000.00708.x. doi:10.1046/j.1365-2362.2000.00708.x. [DOI] [PubMed] [Google Scholar]
- Lycett D, Munafo M, Johnstone E, Murphy M, Aveyard P. Associations between weight change over 8 years and baseline body mass index in a cohort of continuing and quitting smokers. Addiction. 2011;106:188–196. doi: 10.1111/j.1360-0443.2010.03136.x. doi:10.1111/j.1360-0443.2010.03136.x. [DOI] [PubMed] [Google Scholar]
- Mannisto S, Pietinen P, Haukka J, Ovaskainen ML, Albanes D, Virtamo J. Reported alcohol intake, diet and body mass intake in male smokers. European Journal of Clinical Nutrition. 1996;50:239–245. Retrieved from http://www.nature.com/ejcn. [PubMed] [Google Scholar]
- Murray P, Istvan JA, Voelker HT. Does cessation of smoking cause a change in alcohol consumption? Evidence from the Lung Health Study. Substance Use & Misuse. 1996;31:141–156. doi: 10.3109/10826089609045804. doi:10826089609045804. [DOI] [PubMed] [Google Scholar]
- Nides M, Rand C, Dolce J, Murray R, O’Hara P, Voelker H, et al. Weight gain as a function of smoking cessation and 2-mg nicotine gum use among middle-aged smokers with mild lung impairment in the first 2 years of the Lung Health Study. Health Psychology. 1994;13:354–361. doi: 10.1037//0278-6133.13.4.354. doi: 10.1037/0278-6133.13.4.354. [DOI] [PubMed] [Google Scholar]
- Raben A, Agerholm-Larsen L, Flint A, Holst JJ, Astrup A. Meals with similar energy densities but rich in protein, fat, carbohydrate, or alcohol have different effects on energy expenditure and substrate metabolism but not on appetite and energy intake. American Journal of Clinical Nutrition. 2003;77:91–100. doi: 10.1093/ajcn/77.1.91. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S. Modern Epidemiology. 2nd edition. Philadelphia, PA: Lippincott-Raven; 1998. [Google Scholar]
- Russell MA. The classification of smoking by factorial structure of motives. The Journal of the Royal Statistical Society. 1974;137:313–333. [Google Scholar]
- Saris WHM, Blair SN, van Baak MA, Eaton SB, Davies PSW, Di Pietro L, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st stock conference and consensus statement. Obesity Reviews. 2003;4:101–114. doi: 10.1046/j.1467-789x.2003.00101.x. doi:10.1046/j.1467-789X.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- Schutz Y. 2nd Plenary Session: ‘Body-weight balance and regulation’ Role of substrate utilization and thermogenesis on body-weight control with particular reference to alcohol. Proceedings of the Nutrition Society. 2000;59:511–517. doi: 10.1017/s0029665100000744. doi:10.1017/S0029665100000744. [DOI] [PubMed] [Google Scholar]
- Suter PM. Is alcohol consumption a risk factor for weight gain and obesity? Critical Reviews in Clinical Laboratory Sciences. 2005;42:197–227. doi: 10.1080/10408360590913542. doi:10.1080/10408360590913542. [DOI] [PubMed] [Google Scholar]
- Suter PM, Jequier E, Schutz Y. Effect of ethanol on energy expenditure. American Journal of Physiology—Regulatory, Integrative and Comparative Physiology. 1994;266:R1204–R1212. doi: 10.1152/ajpregu.1994.266.4.R1204. [DOI] [PubMed] [Google Scholar]
- Suter PM, Schutz Y, Jequier E. The effect of ethanol on fat storage in healthy subjects. New England Journal of Medicine. 1992;326:983–987. doi: 10.1056/NEJM199204093261503. http://www.nejm.org/doi/full/10.1056/NEJM199204093261503. [DOI] [PubMed] [Google Scholar]
- Tolstrup JS, Halkjaer J, Heitmann BL, Tjonneland AM, Overvad K, Sorensen TIA, et al. Alcohol drinking frequency in relation to changes in waist circumference. American Journal Clinical Nutrition. 2008;87:957–962. doi: 10.1093/ajcn/87.4.957. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Tolstrup JS, Heitmann BL, Tjonneland AM, Overvad OK, Sorensen TIA, Gronbaek MN. The relation between drinking pattern and body mass index and waist and hip circumference. International Journal of Obesity. 2005;29:490–497. doi: 10.1038/sj.ijo.0802874. [DOI] [PubMed] [Google Scholar]
- Tremblay A, St-Pierre S. The hyperphagic effect of a high-fat diet and alcohol intake persists after control for energy density. American Journal of Clinical Nutrition. 1996;63:479–482. doi: 10.1093/ajcn/63.4.479. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Tremblay A, Wouters E, Wenker M, St-Pierre S, Bouchard C, Despres JP. Alcohol and a high-fat diet: A combination favoring overfeeding. American Journal of Clinical Nutrition. 1995;62:639–644. doi: 10.1093/ajcn/62.3.639. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Wang L, Lee IM, Nanson JE, Buring JE, Sesso HD. Alcohol consumption, weight gain, and risk of becoming overweight in middle-aged and older women. Archives of Internal Medicine. 2010;170:453–461. doi: 10.1001/archinternmed.2009.527. Retrieved from http://www.archinte.ama-assn.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG. Alcohol, body weight, and weight gain in middle-aged men. American Journal of Clinical Nutrition. 2003;77:1312–1317. doi: 10.1093/ajcn/77.5.1312. 1–3. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG, Perry IJ. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes Care. 2001;24:1590–1595. doi: 10.2337/diacare.24.9.1590. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Field AE, Colditz GA, Rimm EB. Alcohol intake and 8-year weight gain in women: A prospective study. Obesity Research. 2004;12:1396. doi: 10.1038/oby.2004.175. doi: 10.1038/oby.2004.175. [DOI] [PubMed] [Google Scholar]
- Wareham NJ, van Sluijs EMF, Ekelund U. Symposium on ‘Prevention of obesity’ Physical activity and obesity prevention: A review of the current evidence. Proceedings of the Nutrition Society. 2005;64:229–247. doi: 10.1079/pns2005423. doi: 10.1079/PNS2005423. [DOI] [PubMed] [Google Scholar]
- Westerterp KR. Diet induced thermogenesis. Nutrition and Metabolism. 2004;1:1–5. doi: 10.1186/1743-7075-1-5. Article Number: 5. doi:10.1186/1743-7075-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerterp KR, Meijer EP, Goris AHC, Kester ADM. Alcohol energy intake and habitual physical activity in older adults. British Journal of Nutrition. 2004;91:149–152. doi: 10.1079/bjn20031013. doi: 10.1079/BJN20031013. [DOI] [PubMed] [Google Scholar]
- Westerterp-Plantenga MS, Verwegen CRT. The appetizing effect of an aperitif in overweight and normal-weight humans. American Journal of Clinical Nutrition. 1999;69:205–212. doi: 10.1093/ajcn/69.2.205. Retrieved from http://www.ajcn.org. [DOI] [PubMed] [Google Scholar]
- Yeh HC, Duncan BB, Schmidt MI, Wang NY, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: A Cohort Study. Annals of Internal Medicine. 2010;152:10–17. doi: 10.7326/0003-4819-152-1-201001050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans MR. Effects of alcohol on food and energy intake in human subjects: Evidence for passive and active over-consumption of energy. British Journal of Nutrition. 2004;92(Suppl. 1):S31–S34. doi: 10.1079/bjn20041139. doi:10.1079/BJN20041139. [DOI] [PubMed] [Google Scholar]
- Yudkin P, Hey K, Roberts S, Welch S, Murphy M, Walton R. Abstinence from smoking eight years after participation in randomised controlled trial of nicotine patch. British Medical Journal. 2003;327:28–29. doi: 10.1136/bmj.327.7405.28. Retrieved from http://www.bmj.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.