Abstract
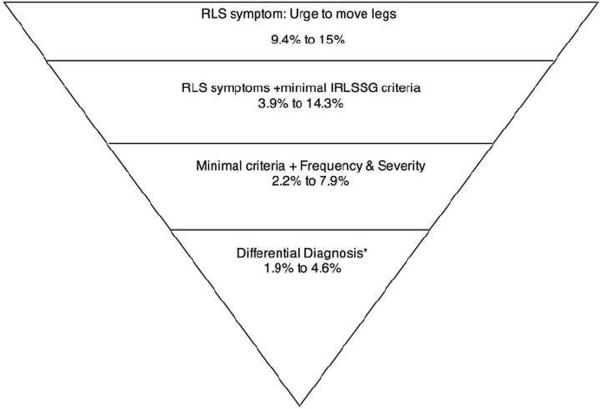
Restless legs syndrome (RLS) has gained considerable attention in the recent years: nearly 50 community-based studies have been published in the last decade around the world. The development of strict diagnostic criteria in 1995 and their revision in 2003 helped to stimulate research interest on this syndrome. In community-based surveys, RLS has been studied as: (1) a symptom only, (2) a set of symptoms meeting minimal diagnostic criteria of the IRLSSG, (3) meeting minimal criteria accompanied with a specific frequency and/or severity, and (4) a differential diagnosis. In the first case, prevalence estimates in the general adult population ranged from 9.4% to 15%. In the second case, prevalence ranged from 3.9% to 14.3%. When frequency/severity is added, prevalence ranged from 2.2% to 7.9% and when differential diagnosis is applied prevalence estimates are between 1.9% and 4.6%. In all instances, RLS prevalence is higher in women than in men. It also increases with age in European and North American countries but not in Asian countries. Symptoms of anxiety and depression have been consistently associated with RLS. Overall, individuals with RLS have a poorer health than non-RLS but evidence for specific disease associations is mixed. Future epidemiological studies should focus on systematically adding frequency and severity in the definition of the syndrome in order to minimize the inclusion of cases mimicking RLS.
Keywords: Epidemiology, Restless Legs Syndrome, Community, Primary Care, mental disorders, illness
1. INTRODUCTION
Restless Legs Syndrome (RLS) was first depicted in 1685 by Sir Thomas Willis, an English physician, in a sharp description of patients who cannot fall asleep because of ⪡leapings and contractions⪢ of the arms and legs. Sir Willis wrote that ⪡restlessness and tossing⪢ could be so severe that the patients ⪡are no more able to sleep than if they were in a place of a greatest torture⪢ (1). In the nineteen century, RLS was termed as ⪡anxietas tibiarum⪢ in Germany by Wittmaack (2). It was in 1945, while studying a group of eight patients, that the Swedish neurologist Karl-Axel Ekbom coined the term “Restless-Legs syndrome,” apparently unaware of Willis' previous description indicating the syndrome could also involve the upper extremities (3).
RLS is a sleep disorder affecting a significant portion of the general population. The syndrome has a strong family component, and several comorbid conditions may be associated with RLS. Research over the past 10 years has highlighted its heritability and has shed some interesting light to this disorder.
Clinically, RLS is characterized by disagreeable leg sensations occurring most often at sleep onset that provoke an irresistible urge to move the legs. Patients with RLS typically complain of itching, creeping, tingling in their legs, usually between the ankle and the knee. These unpleasant sensations occur when the individual is at rest and are more pronounced in the evening or at night. The unpleasant sensations are relieved temporarily with leg movements.
Here we review the data-based publications on the epidemiology of RLS in the general population and in primary care settings including RLS's impact as a disorder or comorbid condition and provide a synthesis of the available literature.
2. METHODOLOGY
The articles utilized in this review included only peer-reviewed original studies published between 1994 and 2010 and written in English, French or Spanish. Databases searched were PubMed, PsycInfo, and PsycArticles. Search terms were “Restless leg” with “community” or “epidemiology,” or “primary care.” The search returned a total of 653 peer-reviewed articles In addition, references cited in retrieved articles were screened for additional reports.
The inclusion criteria were:
-
-
Articles had to assess RLS based on either 1) a single question, 2) IRLSSG criteria of 1995, 3) IRLSSG criteria of 2003, 4) other RLS diagnostic criteria available at the time of the study.
-
-
The study has to be conducted either in general populations or in primary care practices. Studies targeting specific segments of the population (for example, specific age groups or sex) were retained as long as they were designed to be representative of the targeted population.
The exclusion criteria were:
-
-
Articles targeting specific sub-groups of the general population (for example, medical students, policemen, etc) with the exception of pregnant women.
-
-
Studies published only in an abstract form.
-
-
Sample size below 300 participants.
-
-
Studies with non-representative samples.
Articles published using the same sample were counted as a single study although information to describe the sample and methodology could come from different articles associated with that specific study sample.
3. RESULTS
In the last 10 years, there has been a surge in the evaluation of RLS in the general population. 47 studies of the general population were utilized in this review. Before 2000, there was only one epidemiological study published on RLS. Nine were published between 2000 and 2004. The number increased to 27 articles between 2005 and 2009 with a further 10 articles appearing in 2010 alone. In primary care practice, 9 studies were retained. Three were done between 2000 and 2004; 4 between 2005 and 2009 and 2 were published in 2010.
Prevalence estimates of RLS were obtained using either 1) a single question (nine studies), 2) diagnostic criteria proposed by the International Restless Legs Syndrome Study Group (IRLSSG) (4) in 1995 (10 studies) or the revised diagnostic criteria published in 2003 (5) (25 studies) or 3) diagnostic criteria such as ICSD criteria (1 study). Differential diagnosis was applied in 10 out of 47 studies conducted in the general population. Table 1 presents a detailed list of general population studies including the year published, country of the study, age range, participation rate, criteria used, if prevalence is based on differential diagnosis, prevalence and how RLS was assessed.
Table 1.
Prevalence for restless leg syndrome or symptoms in the general population
| Authors | Place | N (Participation rate) | Age | Criteria | Differential diagnosis | Prevalence | Comments |
|---|---|---|---|---|---|---|---|
| Lavigne & Montplaisir (1994) (6) | Canada | 2,019 (unkn) | ≥ 18 | None | No | 1) 15% 2) 10% |
Household interviews, prevalences based on 2 questions: 1) At bedtime, does restlessness in your legs very often, often, occasionally, or never delay your falling asleep? 2) When you wake up during the night, do you very often, often, occasionally, or never feel unpleasant sensation in your leg muscles that require you to move your legs or to walk in order to be more comfortable? |
| Phillips et al. (2000) (7) | Kentucky, USA | 1,803 (84%) | ≥ 18 | None | No | 9.4% | Telephone interviews, prevalence based on a single question: “Do you have unpleasant feelings in your legs – for example creepy-crawling or tingly feelings – when you lie down at night that make you feel restless and keep you from getting a good night's sleep?” RLS had to occur at least 5 times/month. |
| Kageyama et al. (2000) (9) | 5 cities, Japan | 4,612 (unkn) | ≥ 20 | None | No | 3%–7% W 4%–10% M |
Self-administered questionnaire, prevalence based on a single question: “Have you ever experienced sleep disturbance due to a creeping sensation or hot feeling in your legs?” (Yes/No/Sometimes) |
| Rothdach et al. (2000) (32) Berger et al. (2002) (33) |
Augsburg, Germany | 369 (60.6%) | 65–83 | IRLSSG (1995) | No | 9.8% | Face-to-face interview, 3 questions based on criteria described by the International RLS Study group (need positive answers to all questions) + Neurological examination |
| Ulfberg et al. (2001) (53) | Dalarna County, Sweden | 2,608 men (66%) | 18–64 | IRLSSG (1995) | No | 5.8% | Postal questionnaire, 4 questions based on criteria described by the International RLS Study group (need positive answers to all questions) |
| Ulfberg et al. (2001) (54) | Dalarna County, Sweden | 140 women (72%) | 18–64 | IRLSSG (1995) | No | 11.4% | Postal questionnaire, 4 questions based on criteria described by the International RLS Study group (need positive answers to all questions) |
| Ohayon and Roth (2002) (41) | 5 European countries | 18,980 (80.4%) | 15–100 | ICSD | Yes | 5.5% | Telephone interviews, prevalence based on ICSD criteria evaluated by an expert system |
| Sevim et al (2003, 2004) (34,35) | Mersin, Turkey | 3,234 (92.4%) | ≥ 18 | IRLSSG (1995) | Yes | 3.2% | Face-to-face interview, 4 questions based on criteria described by the International RLS Study group (need positive answers to all questions) + the IRLSSG severity scale and neurological examination. Symptoms had to be present in the last month. |
| Berger et al. (2004) (55) | Pomerania, Germany | 4,310 (68.8%) | 20–79 | IRLSSG (1995) | No | 10.6% | Face-to-face interview, 3 questions based on criteria described by the International RLS Study group (need positive answers to all questions) |
| Rijsman et al. (2004) (10) | Krimpen, Netherlands | 1,437 (85.4%) | 50–109 | None | No | 7.1% | Postal questionnaire sent in 1994 before the publication of IRLSSG criteria. One question assessed RLS: “Is your sleep disturbed by leg movements?” “Often” or “always” answers were used to determine possibility of RLS |
| Allen et al. (2005) (19) | United States + 5 European countries | 15,391 (86.8% to 99.2%) | ≥ 18 | IRLSSG (2003) | No | 7.2% (4 symptoms) 2.7% (>= 2t/wk + moderate/severe distress) |
Face-to-face and telephone interview, 4 screening questions+ the IRLSSG severity scale |
| Bjorvatn et al. (2005) (27) | Denmark & Norway | 2,005 (46.7%) (47.0%) | ≥ 18 | IRLSSG (2003) | No | 8.8% Denmark 14.3% Norway |
Telephone interviews, questions were adapted from the IRLSSG criteria + the IRLSSG severity scale for those who answered positively on the RLS 4 criteria. |
| Högl et al. (2005) (28) Wenning et al. (2005) (89) |
Bruneck, Italy | 701 (92%) | 50–89 | IRLSSG (1995) | No | 10.6% | Face-to-face interviews. 4 questions derived from the IRLSSG criteria + the IRLSSG severity scale + neurologic examination |
| Kim et al. (2005) (11) | South Korea | 9,939 (unkn) | 40–69 | None | No | 12.1% | Face-to-face interviews. RLS assessed using 1 question: “Have you ever experienced an urge to move your legs or unpleasant sensations like creepy-crawling feelings in your legs before sleep?” |
| Mizuno et al. (2005) (36) | Izumo city, Japan | 3,287 (36.9%) | ≥ 65 | IRLSSG (1995) | Yes | 1.06% 0.85% idiopathic RLS |
Phase 1: Postal questionnaire with 4 questions on RLS. Phase 2 all probable RLS invited to face-to-face interview+ clinical examination. Of the 150 probable RLS only 35 were positive. |
| Tison et al. (2005) (20) | France | 10,263 (unkn) | ≥ 18 | IRLSSG (1995) | No | 8.5% | Face-to-face home interviews. 5 questions derived from the IRLSSG criteria+ the IRLSSG severity scale for those who answered positively on the RLS 4 criteria. |
| Castillo et al. (2006) (58) | Guayaquil and Quito cities, Ecuador | 500 (40.9%) | 25–85 | IRLSSG (2003) | No | 3.2% in Quito 0.8% in Guayaquil |
Telephone interviews. 4 questions on RLS. Needed 4 positive answers to have RLS. |
| Elwood et al. (2006) (12) | Caerphilly, south Wales, UK | 1,986 men (89%) | 55–69 | None | No | 23% | Auto-questionnaire including 1 question on RLS. RLS was considered present when ⪡restless legs or bothersome twitches⪢ occurred once or twice a week or more. (Question not provided) |
| Lee et al. (2006, 2008) (18,58) | Baltimore, USA | 1,028 (75%) | 58 (±12) | IRLSSG (2003) | No | 4.2% | ECA study wave IV, home interviews. 7-item questionnaire on RLS based on the 4 minimal criteria defined by the IRLSSG. |
| Phillips et al. (2006) (8) | United States | 1,506 (23%) | ≥ 18 | None | No | 9.7% | 2005 National Sleep Foundation Poll, telephone interview, 2 questions based on criteria described by the International RLS Study group. “In the past year, according to your own experience or what others tell you, how often did you have unpleasant feelings in your legs like creepy, crawly, or tingly feelings at night with an urge to move when you lie down to sleep?” Participants answering “every night or almost every night” or “a few nights a week” were asked: “Would you say these feelings in your legs are worse, about the same as, or better at night or in the evening compared to other times of day?” |
| Vogl et al. (2006) (45) | Microisolate in Western part of South Tyrol | 530 (unkn) | ≥ 18 | IRLSSG (2003) | Yes | 8.9% | 2-steps design: 1) Interview with the GenNova Health questionnaire + medical screening examination; 2) Movement disorder specialist examination on positive RLS cases from screening and on case with a positive family history of RLS. |
| Hadjigeorgiou et al. (2007) (31) | Larissa, Greece | 3,033 (72.2%) | ≥ 20 | IRLSSG (2003) | No | 3.9% | Interviews by medical doctors. Screening tool for the 4 minimal criteria + the IRLSSG severity scale for those who answered positively on the 4 criteria. |
| Picchietti et al. (2007) (90) | UK and USA | 10,523 (n/a) | 8–17 | Pediatric NIH criteria | Yes | 1.9% 8–11 y.o. 2.0% 12–17 y.o. |
Households from volunteer market research panel. Survey was conducted online. 3 RLS screening questions and 6 RLS characteristics questions. Series of additional questions. |
| Rangarajan et al. (2007) (46) | Bangalore, India | 1,266 (95.9%) | 18–90 | IRLSSG (2003) | No | 2.1% | Household face-to-face interviews, screening questions covering the 4 minimal criteria + the IRLSSG severity scale for those who answered positively on the 4 criteria. |
| Ulfberg et al. (2007) (26) | Sweden | 1,000 (49.6%) | 18–90 | IRLSSG (2003) | No | 5.0% 5.7% W 3.5% M |
Telephone interviews, screening questions covering the 4 minimal criteria + the IRLSSG severity scale for those who answered positively on the 4 criteria |
| Broman et al. (2008) (62) | Uppsala, Sweden | 1,335 (68%) | 20–59 | IRLSSG (2003) | No | 18.8% 5.8%(>=2t/wk) | Postal questionnaire, 3 questions assessing IRLSSG criteria + Uppsala Sleep Inventory |
| Cho et al. (2008) (17) | 5 regions South Korea | 5,000 (50.9%) | 20–69 | IRLSSG (2003) | Yes | 3.9% definite RLS 3.6% probable RLS |
Telephone interviews, use of the Johns Hopkins telephone diagnostic interview for RLS. 4 criteria needed + frequency >=once a month for 3 consecutive months or >= 20 lifetime episodes. |
| Froese et al. (2008) (61) | British Columbia, Canada | 430 (80%) | ≥ 18 | IRLSSG (2003) | No | 17.7% | Indigenous population. Door-to-door survey. 4 questions assessing RLS symptoms. Needed positive answers on the 4 questions. |
| Happe et al. (2008) (23) | Dortmund, Germany | 1,312 (57.3%) | 25–75 | IRLSSG (2003) | No | 8.8% | Face-to-face interviews. 3 questions assessing RLS symptoms. Needed positive answers on all questions OR having been previously diagnosed with RLS. |
| Nomura et al. (2008) (42) | Daisen, Japan | 2,812 (51.1%) | ≥ 20 | IRLSSG (2003) | Yes | 1.8% | Telephone interviews. 4 questions assessing RLS. Subjects with at least 2 positive answers on RLS items were contacted by a sleep disorder expert neurologist for an interview + the IRLSSG severity scale. |
| Wesström et al. (2008, 2010) (56,91) | Dalarna county, Sweden | 3,516 women (70.3%) | 18–64 | IRLSSG (2003) | No | 15.7% | Self-administrated postal questionnaire. RLS questions based on the 4 minimal criteria defined by the IRLSSG; Need positive answers for the 4 criteria assessed with 5 questions. |
| Winkelman et al. (2008, 2009) (24,60) | United States | 3,254 (67%) | 44–98 | IRLSSG (2003) | No | 5.2% 6.8% W 3.3% M |
Self-administrated questionnaire. RLS questions based on the 4 minimal criteria proposed by the NIH-RLS; need positive answers for the 3 RLS questions + occurrence at least 5 to 15 days per month + at least moderate distress. |
| Yokoyama et al. (2008) (13) | Japan | 1,769 (54.8%) | ≥ 70 | None | No | 11.4% | Home interviews, prevalence based on a single question: “Is your sleep interrupted by a creeping sensation or hot flushes in your legs after you go to bed at night?” RLS was present when the participants answered: Sometimes, often or always |
| Cho et al. (2009) (43) | South Korea | 6,509 (81.7%) | 18–64 | IRLSSG (2003) | No | 0.9% | Face-to-face interview. RLS questions based on the 4 minimal criteria defined by the IRLSSG; need positive answers for the 4 criteria. |
| Erer et al. (2009) (22) | Orhangazi, Bursa, Turkey | 1,124 (89.6%) | 40–95 | IRLSSG (2003) | No | 9.7% | Face-to-face interviews in the household. One RSL screening question. Participants with positive answer on that question were invited to phase 2: detailed interview with movement disorder specialists. IRLSSG severity scale was also administered. |
| Gao et al. (2009) (25) | 14 states in USA | W: 65,554 (82%) M: 23,119 (85%) |
W: 38–55 M: >56 |
IRLSSG (1995) | No | >= 5t/mth (>= 15t/mth): W: 6.4% (2.7%) M: 4.1% (1.7%) |
Participants come from the NHS II cohort of nurses (first wave in 1989) and the HPFS cohort of men established in 1986 and composed of health professionals. Follow-up postal questionnaires of 2005 for the NHS II and 2002 for the HPFS included 3 items to assess RLS. Participants with diabetes, arthritis & pregnancy excluded from the analyses. |
| Tsuboi et al. (2009) (92) | Ajimu, Japan | 1251 (100%) | ≥ 65 | IRLSSG (1995) | Yes | 0.96% | 1) Written screening questionnaire. Questions based on the 4 minimal criteria defined by the IRLSSG. 2) Verification of answers with telephone interview + medical history + the IRLSSG severity scale. 3) Face-to-face interviews + neurological and physical examination. |
| Benediktsdottir et al. (2010) (48) | Reykjavik, Iceland Uppsala, Sweden |
769 (81.8%) 601 (62.2%) |
≥ 40 | IRLSSG (2003) | No | 18.3% Iceland 11.5% Sweden |
Face-to-face interviews at an outpatient clinic in each city. Used the IRLSSG questionnaire. Need positive answers for the 4 criteria. |
| Celle et al. (2010) (44) | St-Etienne, France | 667 (66%) | 68.6 (±0.8) | IRLSSG (2003) | No | 26% | Questionnaires were filled by the subjects at the sleep clinic the day of the polysomnography. 5 questions to assess RLS + the IRLSSG severity scale. Subjects had to meet the 4 RLS criteria + frequency of >= 1 time/week for the last 6 months. |
| Chen et al. (2010) (47) | Taiwan | 4,011 (34.4%) | 15–70 | IRLSSG (2003) | No | 1.57% | Telephone interviews. RLS questions based on the 4 minimal criteria defined by the IRLSSG; need positive answers for the 4 criteria. Symptoms were assessed for the past month. |
| Juuti et al. (2010) (14) | Oulu, Finland | 995 (74.5%) | 57 | None | No | 18.0% | Postal questionnaire. RLS assessed with 1 question: “Have you ever suffered from restless legs? By restless legs, we mean unpleasant feelings (often hard to describe) in the legs at rest (such as lying or sitting), especially when going to bed, which urge you to move your legs or walk.” RLS present if individuals reported a frequency >= 1 time/week. |
| Kim et al. (2010) (30) | South Korea | 714 (63.9%) | ≔ 65 | IRLSSG (2003) | No | 8.4% | Face-to-face interviews conducted by psychiatrists with expertise in sleep disorders. Questions based on the 4 minimal IRLSSG criteria+ IRLSSG severity scale. Need positive answers for the 4 criteria. |
| Park et al. (2010) (57) | South Korea | 1,000 women (78.5%) | 40–69 | IRLSSG (2003) | No | 6.5% | Questionnaires distributed to women living in 4 apartment complexes. RLS questions based on the 4 minimal criteria defined by the IRLSSG; need positive answers for the 4 criteria. |
| Ram et al. (2010) (93) | USA | 6,139 (unkn) | ≥16 | Physician-diagnosed | No | 0.4% | NHANES sample. Home interviews. No detail on how RLS was ascertained. |
| Tasdemir et al. (2010) (29) | Kandira, Turkey | 2,111 (93%) | ≔18 | IRLSSG (2003) | Yes | 3.4% | Home interviews by neurologists. Questions based on the 4 minimal IRLSSG criteria+ IRLSSG severity scale. |
| Winkler et al. (2010) (37) | Northern Tanzania | 7,654 N/A | 14–110 | IRLSSG (2003) | Yes | 0.013% | Face-to-face interviews in the household. 3 questions for RLS. All those who answered positively at least one RLS question (n=10) were re-interviewed by a neurologist. |
| Yilmaz et al. (2011) (21) | Gaziantep, Turkey | 3,304 (87.4%) | 15–18 | IRLSSG (2003) | No | 3.6% | Questionnaires distributed to students by the counselors in 9 out of 60 high schools. Questionnaire based on the IRLSSG criteria. Students suspected of RLS were further evaluated face-to-face or by telephone to confirm RLS. |
IRLSSG = International Restless Legs Syndrome Study Group; ICSD = International Classification of Sleep Disorders; RLS = Restless legs syndrome
3.1. Symptoms, syndrome, diagnosis prevalence
3.1.1 RLS as a symptom
Studies using a single question to assess the prevalence of RLS in the adult general population aged 18 to 20 years and older have reported prevalence ranging between 9.4% and 15% (6–8) with the exception of a Japanese study (9) that found a lower prevalence rate (around 5%). Five other studies have used older adult samples (40 years and older); three of them had restricted age ranges (11,12,14). In these older adult samples, prevalence of RLS is higher in two studies: 23% and 18% (13,14). The prevalence is between 7.1% and 12.1% for the three other studies. Many of these single-question studies had not aimed specifically at assessing RLS, or even sleep disorders. In some cases, the question used lacked specificity (For example, having restless legs or bothersome twitches), which, not surprisingly, yielded higher prevalences. In other cases, the question was so complex that it is not clear whether participants even understood what was being asked (For example, “Have you ever suffered from restless legs? By restless legs, we mean unpleasant feelings (often hard to describe) in the legs at rest (such as lying or sitting), especially when going to bed, which urge you to move your legs or walk.”)
3.1.2 RLS criteria
Thirty-five studies (14,17–34,36,37,42–48,53–58,61,62,92,93) have used the IRLSSG diagnostic criteria in the general population (see Table 1); Seven of these studies used samples of individuals at least 50 years of age (18,28,30,32,36,44,92). Eight studies also applied some differential diagnosis rules (17,29,37,34,36,42,45,92). This section described the results of epidemiological studies for which the comorbidities and causes are unknown. Therefore, RLS prevalence rates include altogether idiopathic and secondary RLS. It is also likely that negative cases mimicking symptoms similar to RLS are also included.
General population studies
In studies where IRLSSG criteria were used without differential diagnoses, with comparable age ranges (i.e., from 18–20 years old up to 70 years or higher) and including both genders; prevalences ranged between 5.0% and 14.3% (19,20,26,27,31,34,46,55).
In the general population, some epidemiological studies have provided additional information regarding the frequency and severity of the symptoms. Nearly all the studies also assessing the frequency of RLS symptoms reported that between 50% and 60% of the participants who met minimal IRLSSG criteria had symptoms at least one time per week (17–25). For example, Allen et al. (19) reported a prevalence of 7.2% of their sample scoring positively on the four minimal IRLSSG criteria. However, when the frequency of symptoms was set to a minimum of two times per week accompanied by moderate or severe distress, the prevalence dropped to 2.7%. Cho et al., (17) reported that 3.6% of their sample had definite RLS (regardless of the frequency and severity of symptoms). This prevalence IP decreased to 1.7% when the frequency of symptoms was set at two times per week or more and decreased to 1.02% when the severity was set to at least moderate distressing symptoms. In another study (18), the prevalence decreased from 4.2% to 1.9% when frequency was set at two times/week or more. When the frequency is set at one time/week or more prevalence dropped from 8.5% to 4.5% in one study (20) and from 3.6% to 2% in a study with adolescents (21). In summary, setting the frequency of leg symptoms to at least one time per week decreased the prevalence by about 40% and setting the frequency to at least two times per week decreased prevalence by about 50%. Daily or near daily occurrence of RLS symptoms occurred in about 20% of individuals with minimal IRLSSG criteria.
Some studies have assessed the severity of RLS using the IRLSSG severity scale (17, 19, 20,22, 26–31). This scale allows categorizing RLS distress as mild, moderate, severe and very severe. Regardless of the frequency of leg symptoms, most of the studies have reported the proportion of individuals with minimal IRLSSG criteria accompanied by moderately to very severely distressing symptoms at between 55.2% to 97.2% (17,19,20,22,26–31) very severely distressing symptoms varied from 2.3% to 5% (19,20,22,27,28).
Primary care studies
Table 2 presents epidemiological studies conducted in primary care practices. Most of these studies have provided different prevalence rates according to the criteria used. Between 11.1% and 25% (15,16,95,96) of the patients had minimal IRLSSG criteria (i.e., the four RLS criteria are met regardless the frequency, severity and possibility than leg symptoms are caused by another condition than RLS); all but 2 studies (15,16) have a prevalence between 20% and 25% (38,39,95,96). In primary care studies, when the frequency of RLS symptoms was set to at least two times per week with moderate to severe distress or negative impact, prevalence rates dropped by more than half, ranging between 3.4% and 9.0% (15,38,39,95).
Table 2.
Prevalence for restless legs syndrome or symptoms in clinical settings
| Authors | Place | N (Participation rate) | Age | Criteria | Differential diagnosis | Prevalence | Comments |
|---|---|---|---|---|---|---|---|
| Tan et al. (2001) (94) | 1 primary care practice, Singapore, China | 1,000 | ≥ 21 | IRLSSG (1995) | No | 0.1% | The first 1000 consecutive patients. Neurological examination + interview with RLS-trained neurologists. Needed positive answers on the 4 RLS criteria |
| Nichols et al. (2003) (95) | 1 primary care practice Moscow, Idaho, USA | 2,099 (79.2%) | ≥ 18 | IRLSSG (1995) | No | 24% IRLSSG criteria 13.7% RLS symptoms ≥1t/wk + mild distress |
Every adult patient with an appointment at the clinic over a 1-year period Questionnaire assessing the 4 basic diagnostic criteria developed by the IRLSSG filled on-site |
| Hening et al. (2004) (15) | 182 primary care practices in 5 countries: USA, France, Germany, Spain, UK | 23,052 (unkn) | Minimum age not specified | IRLSSG (2003) | No | 11.1%IRLSSG criteria 9.6% RLS symptoms ≥ 1t/wk 3.4% RLS symptoms ≥ 2t/wk + negative impact |
1) Screening questionnaire completed by patients attending the 182 practices over a two-week period. Questions based on criteria described by the International RLS Study group. 2) Patients with positive answers for the 4 criteria + symptoms at least once a week had a supplemental questionnaire + questionnaire filled by the physician. |
| Alattar et al. (2007) (96) | 5 family practice offices, North Carolina, USA | 1,934 (65.3%) | ≥ 18 | None | No | 25% RLS symptoms ≥ 1t/wk | Every adult patients with an appointment at the clinic over a 1-month period Questionnaire assessing sleep symptoms filled on-site. 1 Question about tingling, creeping, or restless feelings in the legs while trying to sleep |
| O'Keefe et al. (2007)* (38) | 19 general practices, Ireland | 2,628 (unkn) | ≥ 18 | IRLSSG (2003) | Yes | 1) 23.5% 4 IRLSSG criteria 2) 7.4% symptoms ≥2t/wk + moderate to severe distress 3) 2.8% confirmed RLS by the GP |
1) Screening questionnaire completed by patients attending the 19 practices over a one-week period. Questions based on criteria described by the International RLS Study group. 2) Patients with positive answers for the 4 criteria + moderate to severe distressing symptoms at least twice a week had a supplemental consultation with the GP. 3) Patients confirmed with RLS by the GP completed supplemental questionnaires. |
| Perez-Romero et al. (2007) (16) | 1 Health Center, Otero, Spain | 283 (unkn) | ≥50 | IRLSSG (2003) | No | 11.6% 1.9% clinically significant RLS |
Every patient ≥ 50 years asking to consult a physician at the health center. Questionnaire assessing the 4 basic diagnostic criteria developed by the IRLSSG filled on-site. |
| Baos Vicente et al. (2009)* (39) | 10 primary care centers in Madrid, Barcelona, and Valencia, Spain | 2,047 (unkn) | ≥ 18 | IRLSSG (2003) | Yes | 1) 19.7% 4 IRLSSG criteria 2) 9.0% symptoms ≥2t/wk + moderate to severe distress 3) 4.6% confirmed RLS by the GP |
1) Screening questionnaire completed by patients attending the 10 primary care centers over a one-week period. Questions based on criteria described by the International RLS Study group. 2) Patients with positive answers for the 4 criteria + moderate to severe distressing symptoms at least twice a week had a supplemental consultation with the GP. 3) Patients confirmed with RLS by the GP completed supplemental questionnaires. |
| Allen et al. (2010) (40) | 62 primary care practices in Europe | 10,564 (unkn) | ≥ 18 | IRLSSG (2003) | Yes | 7.6% symptoms >=2t/wk + moderate to severe distress 4.4% confirmed RLS by the GP |
1) Screening questionnaire completed by patients attending the 62 practices over a one-week period. Questions based on criteria described by the International RLS Study group. 2) Patients with positive answers on RLS questions + frequency >=2t/wk + at least moderately distressing symptoms were interviewed by their physician. |
| Moller et al. (2010) (97) | 312 primary care practices in Germany | 16,531 (unkn) | ≥ 18 | IRLSSG (2003) | Yes | 10.6% | 1) Screening questionnaire completed by patients attending the 312 practices on a one-day period. RLS questions based on criteria described by the International RLS Study group. 2) Physicians reviewed the questionnaire to confirm the 4 RLS criteria were fulfilled. Physicians filled a Clinical Global Impression-Severity of Illness for each positive patient. |
Patients of this study included in Allen et al., 2010
IRLSSG = International Restless Legs Syndrome Study Group; RLS = Restless legs syndrome
3.1.3 Differential diagnosis of RLS
This section includes epidemiological studies having eliminated as much as possible disorders that may produce symptoms similar to those observed in RLS. In many of these studies, neurologists or physicians interviewed or reviewed positive cases of RLS after initial screening.
General population studies
Studies that applied some differential diagnoses rules either based on elderly samples (36,92) or in countries other than those in North America or Europe (17,29,33,37,42,45). For example, in Turkey, Sevim et al. (34,35) reported an RLS prevalence of 3.2% in their representative sample of 3,234 adults of the general population; a similar result (3.4%) was found in another Turkish study using the same age range (29). A Japanese study conducted among elderly people (36) found an RLS prevalence of 1.06%. In that study, the first screening, based on a questionnaire assessing the minimal IRLSSG criteria, identified 150 probable cases of RLS. After face-to-face interview and clinical examination, only 35 of the 150 were confirmed with RLS. The lowest prevalence, 0.013%, was observed in a Tanzanian study (37).
Primary care studies
For three primary care practice studies, positive cases were further reviewed by the treating physician to confirm the diagnosis and eliminate cases where RLS symptoms could be attributed to other diseases. In one study (38) prevalence dropped from 7.4% to 2.8%; in another (39) from 9.0% to 4.6% and in the last (40) from 7.6% to 4.4%.
Figure 1 illustrates how RLS prevalence rates are related to various ways of defining RLS. Prevalence rates decrease with increasingly precise definitions of RLS.
Figure 1.
Changes in RLS prevalence rates in North America and Europe general population according to used definitions
*Prevalence rates for differential diagnosis came from primary care samples. Prevalence estimates are based on samples including participants from 18 to >= 65 years.
3.2 Modifying factors of prevalence
3.2.1 Sex
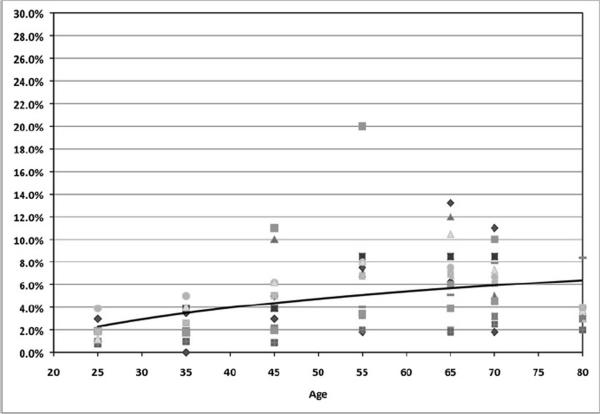
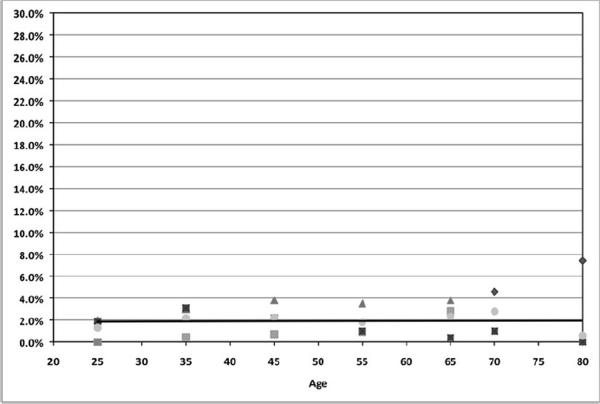
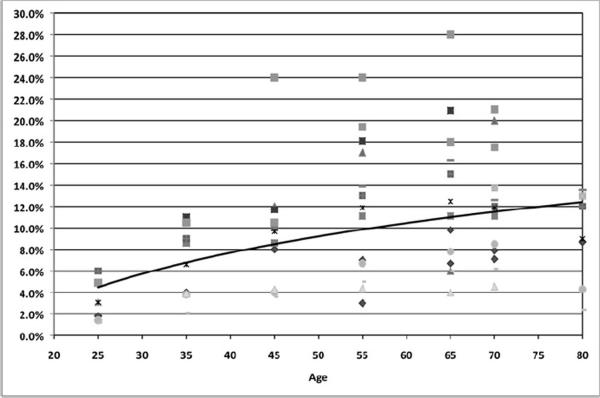
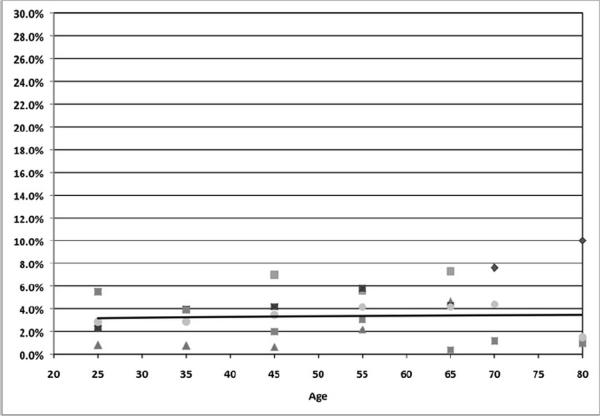
Many studies have reported a higher prevalence of RLS among women than in men (17–20,22,27,29,30,32,34,36,41–44). In some other studies, RLS was not sex related (26,45–48). Other studies have found higher rates in women but only in specific age groups. One has reported higher rates in women in the 20–29 and 50–59 age groups (42). For another study, prevalence was higher in men in the 40–49 age group (9) while in another it was higher in women only among subjects younger than 48 years (24). In yet another it was only among the 60 to 79 years old subjects (31). Sex differences in RLS prevalence are illustrated in Figure 1a to Figure 1d. As can be seen, prevalence is about twice as high in women than in men.
3.2.2 Pregnancy
RLS is the most common movement disorder occurring during pregnancy. It develops more frequently during the third trimester and disappears within the first month after delivery in most cases. One of the oldest RLS studies (49) examined 500 women at 33–34 weeks' gestation and four weeks after delivery. The prevalence of RLS was 19.5%. Severe RLS, defined as sensations in the legs lasting for more than 30 minutes and occurring at least three times/week with frequent sleep disturbances, was observed only in seven women. Four weeks after delivery, only three women still had RLS symptoms. A large Japanese study (50) involving 16,528 pregnant women examined RLS prevalence using a single question answered on a scale ranging from never to always. A total of 19.9% of women reported sometimes to always having the sensation of insects running across the skin or hot flashes inside the legs after going to bed at night. The prevalence of RLS increased with the length of pregnancy: 15% in the first trimester and 23% in the last trimester. Two studies have used IRLSSG criteria to assess RLS in pregnant women. The first study (51) was conducted in Italy with 606 women at the time of delivery. Symptoms were assessed retrospectively from the beginning of pregnancy using the IRLSSG criteria of 1995. An RLS prevalence (any frequency) of 26.6% was found; 62.7% of these women had never experienced RLS symptoms prior to pregnancy. As in the general population, RLS prevalence decreased with frequency of symptoms: 20.1% of the sample experienced symptoms two times per week or more and 14.8% had them at least three times per week. Prevalence decreased to 13% in the month following delivery. After six months, only eight women still had RLS symptoms. A Brazilian study (52), using the IRLSSG criteria of 2003, reported an RLS prevalence of 13.5% in their sample of 524 women; 94.4% were in the second or third trimester. RLS prevalence in the first trimester was 5.3%; 14.7% in the second trimester and 15.2% in the third trimester. Proportion of severe RLS also increased by trimester: 41.9% of women in the second trimester and 63.9% of those in the third trimester had severe or very severe RLS. A follow-up study (98) interviewed 207 women about 6.5 years after delivery to compare the incidence of RLS among women without RLS symptoms and those who had RLS during their pregnancy. The results showed that women who had transient RLS during their pregnancy had a 4-fold increased risk of developing chronic RLS. These women were also more likely to experience again RLS symptoms in a subsequent pregnancy (58%) than the other women (3%).
3.2.3 Age
Results for age are not as conclusive as for sex. Some studies showed that RLS increased with age (19,31,35,41,53–56). Some studies have also reported an increase up to 60–70 years and then a decrease in prevalence in older subjects (19,20,29,31,43). In some studies, the peak in prevalence was observed around 30–40 years (17,27). Finally, many studies have no increase in prevalence with age (18,22,34,47,48). Most of the studies performed in elderly samples did not report an increase in RLS prevalence with older age (30,32,36).
RLS may begin at any age but most individuals suffering from RLS are over age 40. This information was collected in some of the epidemiological studies. Two studies have examined the age of onset in relationship to etiology. Both studies find a similar age of onset for idiopathic RLS. In one study (45), the age of onset for idiopathic RLS was at 33.7 years and in the other study, the age at onset was 35.4 years (57); Age at onset for secondary RLS was at 47.4 (±5.3) years (57). Another study reported that RLS begun before the age of 45 years in 70.2% of cases but without details regarding whether RLS was idiopathic or secondary (17).
3.2.4 Summary
To better understand the relationship between RLS, age and sex, each article was reviewed in light of 1) comparison of criteria used and 2) availability of the data by age groups and sex. Eighteen studies provided this information. Seven of these studies were performed using the IRLSG minimal diagnostic criteria of 1995 and eleven studies used the 2003 IRLSG minimal diagnostic criteria. Since it appears Asian countries might be different; results for Asian men and women are presented separately from those observed in North America and Europe. Figures 1a to 1d present the findings. It clearly shows that the prevalence of RLS increases steadily with age up to 65 years for both men and women living in North America or Europe: the prevalence appears to double every 20 years and peak around 65 years. It is not observed in Asian countries. RLS prevalence appears to remain unchanged with age in men and in women.
Overall, it is difficult to have a clear image of the prevalence of RLS around the world. However, so far, it appears that Asian countries have a lower prevalence of RLS than European and North American countries. In Europe, it would appear that Northern European countries (Finland, Sweden, Norway) have a higher prevalence of RLS than Southern European countries. However, many of the Asian studies have used more strict definitions of RLS than European studies. Two of them (17,36) had participants with positive answers on screening questions reviewed by a neurologist of sleep specialist to eliminate false positive RLS cases. In one study (36), 77% of participants were false positives after clinical examination. Therefore, methodological aspects are in part responsible of the disparities in prevalence observed between Asia, Europe and North America.
In respect of ethnic background, one of the most interesting studies was performed in Ecuador in two cities (58). One of these cities was composed mainly of individuals of European descendants. In the other city the population was mainly of individuals of indigenous descendants. The city with European descendants had an RLS prevalence of 3.2% while the city with indigenous descendants had an RLS prevalence of 0.8%. This suggests that genetic makeup may play a role in RLS. However, further studies are needed to elucidate the role of race in RLS. In addition to the Ecuadorian study, only two other studies have presented data on race. One study conducted in the U.S. found a similar prevalence in African-Americans (4.7%) and Caucasians (3.8%) (59). On the other hand, another American survey (25) reported higher rates in Caucasians (6.6% in women and 4.2% in men) than in non-Caucasians (3.8% in women and 2.4% in men).
3.3. Associated factors
3.3.1 Insomnia symptoms and excessive sleepiness
Symptoms of RLS are worse in the evening or at night, therefore it is expected that RLS causes some sleep disturbances. All the epidemiological studies that have examined the association between RLS and insomnia symptoms: Difficulty initiating sleep (DIS), difficulty maintaining sleep (DMS) and non-restorative sleep (NRS), have found that individuals with RLS were two to three times more likely to report these symptoms than non-RLS subjects (19,21,27,44,48,53,54,56,60,62). Proportions differ between studies depending on how insomnia symptoms were defined and the population studied (for example, elderly only). The proportion of RLS individuals who reported having DIS varied from 27.9% to 69.2% and having DMS varied from 24% to 50.5%. NRS was more seldom studied but appeared to be at least twice more frequent in RLS individuals (53,54,56).
Excessive sleepiness in RLS has been assessed using the Epworth Sleepiness Scale (ESS) or with questions addressing the propensity to sleep during periods of wakefulness. Of the six studies using the ESS to evaluate excessive sleepiness, three did not find significant differences between RLS and non-RLS individuals (30,44,61) and three studies found RLS individuals had higher ESS scores than non-RLS subjects (48,53,54). When individuals were questioned about the propensity to sleep during periods of wakefulness, all studies found that RLS individuals were two to three times more likely to report excessive sleepiness than non-RLS participants: between 32% and 42% of RLS individuals complained of excessive sleepiness (14,26,27,48,53,56).
3.3.2 Medical condition
Several medical conditions can be associated with RLS. All epidemiological studies that have examined the general health status of individuals with RLS converge to say that such individuals have a poorer health status than individuals without RLS.
Cardiovascular disease, coronary artery disease and heart problems were associated with RLS in many studies; individuals with any of these conditions being twice as likely to have RLS than those without these health problems (14,24,56,41,43,47,53). One study also examined the strength of the association in relationship to the frequency and severity of RLS symptoms (24). It found that RLS symptoms occurring fewer than 16 times per month were not associated with cardiovascular and coronary artery disease. The association was significant only when symptoms were present at least 16 times per month and the association was stronger in RLS individuals who were severely bothered by RLS symptoms. Three studies did not find associations between heart-related conditions and RLS (48,59,61). Hypertension was unrelated to RLS in six studies (14,30,31,46,56,61) but was significantly associated to RLS in five other studies (32,41,44,47,53).
Obesity and increased BMI have been associated with a greater likelihood of having RLS in many studies (7,11,25,41,47) but just as many others have found no such association (21,28,32, 44,48,60,61). Gao et al. (25) did the most comprehensive epidemiological study on this topic. In addition to BMI, participants also reported waist and hip circumferences. Besides overall obesity (BMI > 30 kg/m2), they found that greater abdominal adiposity (waist circumference) was also associated with a higher likelihood of RLS. They also found that a greater BMI in early adulthood (18–21 years) and subsequent weight gain were associated with a higher risk of developing RLS. The association remained even after controlling for several variables (age, ethnicity, physical activity, smoking, use of antidepressants, anxiety score and the presence of a number of chronic diseases).
Diabetes also had mixed results: nine studies found no increased risk of RLS in diabetes (30,31,32,43,46,47,56,59,61) and four studies found that individuals with diabetes were at greater risk of having RLS (7,29,44,48).
Some studies have examined whether chronic pain and other painful conditions such as arthritis and neuropathy were associated with RLS. Most studies have found that such associations existed. Individuals with RLS are more likely to have arthritic diseases (14,41,47) backache or other pain (43,47,56), headaches (53,56). RLS was associated with polyneuropathy in one study (29) but was not in another one (28).
Other studies have examined the association between RLS and a variety of diseases that could be involved in RLS. A presence of anemia has given mixed results. The association was positive in some epidemiological studies (29) but not in others (30,31,47).
One of the main problems in RLS epidemiological studies is the heterogeneity of the RLS individuals. As we have shown in the first section, almost all studies did not take into account the frequency and/or severity of symptoms to determine the presence of RLS. Therefore, a large part of RLS samples have symptoms occurring less than weekly. One of the consequences is that it weakens associations between RLS and diseases. The study by Winkelman et al (24) is a good illustration: cardiovascular and coronary artery diseases were significantly associated with RLS only when it occurred at least 16 times per month.
The etiology of RLS is not well known but several pathophysiological mechanisms were proposed. RLS has been also linked with lower serum ferritin levels. Up to 31% of RLS older-age patients would have iron deficiency (63). Oral iron supplement therapy produced a significant reduction in RLS symptoms (64) but this was not confirmed in another study (65). The relationship between RLS and iron deficiency was not supported in uremic patients with or without RLS (66). However, the results of recent research has shown that idiopathic RLS patients with normal serum ferritin levels have a 65% reduction in CSF ferritin and an increase in CSF transferrin (67). Therefore, brain iron storage may be reduced in idiopathic RLS patients.
Uremia is another possible cause for RLS (68). In a study of 136 uremic patients, 23% of them were found to have RLS (66). Another study reported RLS rate of 58.3% in a group of 48 uremic patients (99). Similarly, uremia was found to be the cause of RLS in 22.3% of 300 RLS patients (69).
Other factors have also been identified to cause RLS: folate deficiency, vascular insufficiency (70), chronic obstructive pulmonary disease (71), gastroctomy (72) and caffeine abuse (73).
3.3.3 Mental disorders
Depressive and anxious moods among RLS individuals have been evaluated in several epidemiological studies (7,26,27,30,32,34,42,44,53,56). Some of these studies have used a single question (e.g. 27,53) while others have used well-known validated scales such as the CES-D scale or the Hamilton anxiety or depression scales. All these studies have pointed out that RLS individuals are at least twice as likely to have scores indicating the presence of a depressive or an anxiety disorder than individuals without RLS. Only two studies (18,41) used DSM-IV diagnoses. Depressive mood and major depressive disorder are the most common psychiatric problems in RLS individuals.
3.4. RLS and genetic links
RLS appears to have a familial component in many cases. Several epidemiological studies have examined family history of RLS (20,21,23,26,27,29,34,45,46). The proportion of RLS individuals with a positive family history of RLS varies from a low 18.5% in a sample from India (46) to a high 59.6% in a microisolate of South Tyrol (45). Other studies reported rates between 28.3% in a Swedish sample (26) and 40.9% in a French sample (20).
RLS inheritance was initially thought to follow an autosomal dominant pattern in at least one third of the familial cases especially in families with an earlier age at Ronset (74,75,76). For example, Montplaisir et al. (76) reported that 63% of the 127 studied RLS patients said there was at least one family member with similar symptoms. Another study found that 42.3% of patients with idiopathic RLS and 11.7% of those with RLS due to uremia had a clear positive hereditary RLS (69). Some studies have pointed out that inheritance is bimodal; earlier onset being associated with an autosomal-dominant mode while RLS at a later age is more compatible with an inheritance model of free transmission probabilities (77). One study has examined RLS inheritance in twins (78). In that study, the authors reported a high RLS concordance rate (83.3%) between identical twins. However, age at onset, disease severity and symptom descriptions often varied within the concordant pairs. Another twin study in which RLS was assessed using 2 questions in a sample of 4,503 monozygotic and dizygotic twins estimated RLS heritability to be 0.6 (79).
Familial and sporadic RLS cases presented similar signs, symptoms and clinical course. The only differences between the two groups consisted of a significantly earlier age of onset and a more frequent worsening during pregnancy in patients with hereditary RLS (69).
At the genetic level, linkage studies have to-date described five genomic loci associated with RLS. In studies that used an autosomal recessive model of inheritance, family studies have reported a linkage to chromosome 12q (RLS1). The first studies describing this linkage were done with French Canadian samples (80,81). The findings were replicated in subsets of Icelandic and German families (82, 83).
Using a dominant model of inheritance, different RLS family studies have shown a linkage to chromosome 14q (RLS2) (84), 9p (RLS3) (85), 2q (RLS4) (86) and 20p (RLS5) (87).
4. CONCLUSIONS
Epidemiologic knowledge of RLS has increased considerably recently, in fact, since 2005 epidemiological research on RLS has effectively blossomed.
This synthesis of the literature reveals that RLS prevalence rates are linked to:
-
1)
The way RLS is evaluated. Single-item studies have provided the highest RLS prevalence followed by studies having limited the assessment to the 4 minimal criteria described by the International Restless Legs Syndrome Study Group. In this last case, prevalence of RLS in the adult general population ranges between 5% and 8.8%. However, at least half of these cases have infrequent and/or mild RLS.
-
2)
Sex of the individuals: In most of studies, RLS is about twice higher in women than in men.
-
3)
Age: As illustrated in Figures 1a and 1c, prevalence of RLS increases with age in North America and Europe. However, the same trend is not observed in Asian countries.
-
4)
Race: Data on race are still too fragmentary to reach definite conclusions but from what we know to date Asian countries appear to have much lower prevalence of RLS.
-
5)
Co-morbid conditions. Insomnia symptoms, excessive sleepiness and depressive and/or anxiety symptoms have been consistently associated with RLS. Several medical conditions have been less consistently associated with RLS, e.g.; cardiovascular diseases, hypertension, diabetes, obesity and pain. The effects of medications on RLS symptoms have not been investigated in epidemiological studies.
RLS is common in the general population but a full appreciation of its severity and impact on daily life remains unclear. The earliest epidemiological studies using IRLSSG criteria are based on the 1995 criteria, while the most recent have used the 2003 revised criteria, which makes direct comparison of these studies difficult. There is also problem of participation rates, as in at least 10 studies where the percentage is below 60%. The overwhelming majority of prevalence rates reported in epidemiological studies of RLS are based solely on the presence of one symptom or a constellation of symptoms (four minimal criteria proposed by the IRLSSG group) that might occur only infrequently, regardless of the severity of the symptoms. While this may be defensible from an epidemiological point of view; for the physicians, it raises the question of “When does one need to treat these people?”. Two studies (19,27) have examined more closely who are the individuals with RLS who seek medical advice or help for their symptoms. Treatment seeking is closely associated with the severity of symptoms: nearly all of those with severe or very severe RLS symptoms consulted while this proportion decreased to half in those with moderate symptoms and to 10% with those with mild symptoms (27).
Epidemiological studies conducted in clinical settings were more rigorous in the attribution of RLS diagnosis. Most of them required a frequency of symptoms of at least two times per week accompanied by moderate to severe distress and the diagnosis confirmed by the treating physician. Such studies yield prevalence estimates about five times lower than when prevalence is based solely on RLS minimal criteria. As the International RLS Study Group has pointed out, the minimal criteria were not intended to confirm the presence of RLS but to indicate the possibility of the syndrome. Minimal RLS criteria without applying frequency and severity yield a false positive rate around 50% (88). Consequently, using only the four minimal symptoms to determine the prevalence of RLS in the general population can cause an inflation of the prevalence of RLS. It is especially true when studies seek only yes/no answers or presence/absence of criteria. Several conditions can produce symptoms similar to RLS, for example, leg cramps or arthritic pain in lower limbs. It is therefore important that epidemiological studies include some questions that allow excluding individuals for whom, leg symptoms can be attributed to other disorders. Additionally, quantification of the frequency and severity of the symptoms will allow eliminating a sizable number of individuals for whom a RLS diagnosis is not warranted.
It should be kept in mind that prevalence observed in primary care practices cannot be applied to the general population: 1) even when comparable age groups were used, the mean age of subjects in primary care practice samples was higher than the one of general population samples and 2) only a portion of the general population consults at least once a year a primary care practitioner and mostly because the individuals have some health problem concerns: as it was shown, individuals of the general population with RLS are more likely to have health problems than non-RLS people and, therefore, have greater needs to consult a physician.
Another consequence of using cases with infrequent RLS in general population-based studies is that it can mask the presence of some risk factors. This is probably one of the reasons why there are so many conflicting results when it comes to identifying medical conditions associated with RLS.
PRACTICE POINTS.
Prevalence of RLS decreases as defining criteria increase in strictness in European and North American general adult populations.
When a differential diagnostic approach is taken, prevalence estimates are 1.9–4.6% of European and North American general adult populations.
European and North American populations demonstrate higher RLS prevalences compared to Asian populations.
European and North American populations demonstrate an age-increase in RLS prevalence, while Asian populations do not.
RLS prevalance in women is approximately double that of men across all populations and ages.
RESEARCH AGENDA.
Future epidemiological studies should focus on the general population and include systematic assessment using diagnostic criteria including frequency and severity of symptoms.
Additional epidemiological studies outside of Europe and North America are needed to clarify apparent population differences in RLS prevalence.
Studies should seek to determine the conditions associated with RLS, particularly severe RLS, as well as its functional consequences.
Figure 2a.
Prevalence of RLS in men – North America and Europe
Included 12 studies that had provided prevalence by age groups for men. These studies are based on minimal IRLSSG criteria. A total of 23,282 men aged >=18 are included in the scatter plot.
Figure 2b.
Prevalence of RLS in men – Asia
Included 5 studies that had provided prevalence by age groups for men. These studies are based on minimal IRLSSG criteria. A total of 8,081 men aged >=18 are included in the scatter plot.
Figure 2c.
Prevalence of RLS in women – North America and Europe
Included 12 studies that had provided prevalence by age groups for women. These studies are based on minimal IRLSSG criteria. A total of 26,150 women aged >=18 are included in the scatter plot.
Figure 2d.
Prevalence of RLS in women – Asia
Included 6 studies that had provided prevalence by age groups for women. These studies are based on minimal IRLSSG criteria. A total of 11,253 women aged >=18 are included in the scatter plot.
Acknowledgment
MM Ohayon was supported by National Institutes of Health grant R01NS044199
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Willis T. The London Practice of Physic. Bassett and Crooke; London: 1685. [Google Scholar]
- 2.Wittmaack T. Lehrbuch der Nervenkrankheiten, Ted 1: Pathologie and Therapie der Sensiblen Neurosen. E. Schafer; Leipzig: 1861. Pathologic and therapie des sensibilitats-neurosen. [Google Scholar]
- 3.Ekbom KA. Restless legs: a clinical study. Acta Med Scand. 1945;158(Suppl.):1–123. [Google Scholar]
- 4.Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group. Mov Disord. 1995;10:634–642. doi: 10.1002/mds.870100517. [DOI] [PubMed] [Google Scholar]
- 5*.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J, Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health. International Restless Legs Syndrome Study Group Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 6.Lavigne GJ, Montplaisir JY. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep. 1994;17:739–743. [PubMed] [Google Scholar]
- 7.Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160:2137–2141. doi: 10.1001/archinte.160.14.2137. [DOI] [PubMed] [Google Scholar]
- 8.Phillips B, Hening W, Britz P, Mannino D. Prevalence and correlates of restless legs syndrome: results from the 2005 National Sleep Foundation Poll. Chest. 2006;129:76–80. doi: 10.1378/chest.129.1.76. [DOI] [PubMed] [Google Scholar]
- 9.Kageyama T, Kabuto M, Nitta H, Kurokawa Y, Taira K, Suzuki S, Takemoto T. Prevalences of periodic limb movement-like and restless legs-like symptoms among Japanese adults. Psychiatry Clin Neurosci. 2000;54:296–298. doi: 10.1046/j.1440-1819.2000.00685.x. [DOI] [PubMed] [Google Scholar]
- 10.Rijsman R, Neven AK, Graffelman W, Kemp B, de Weerd A. Epidemiology of restless legs in The Netherlands. Eur J Neurol. 2004;11:607–611. doi: 10.1111/j.1468-1331.2004.00848.x. [DOI] [PubMed] [Google Scholar]
- 11.Kim J, Choi C, Shin K, Yi H, Park M, Cho N, Kimm K, Shin C. Prevalence of restless legs syndrome and associated factors in the Korean adult population: the Korean Health and Genome Study. Psychiatry Clin Neurosci. 2005;59:350–353. doi: 10.1111/j.1440-1819.2005.01381.x. [DOI] [PubMed] [Google Scholar]
- 12.Elwood P, Hack M, Pickering J, Hughes J, Gallacher J. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60:69–73. doi: 10.1136/jech.2005.039057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yokoyama E, Saito Y, Kaneita Y, Ohida T, Harano S, Tamaki T, Ibuka E, Kaneko A, Nakajima H, Takeda F. Association between subjective well-being and sleep among the elderly in Japan. Sleep Med. 2008;9:157–164. doi: 10.1016/j.sleep.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Juuti AK, Läärä E, Rajala DU, Laakso M, Härkönen P, Keinänen-Kiukaanniemi S, Hiltunen L. Prevalence and associated factors of restless legs in a 57-year-old urban population in northern Finland. Acta Neurol Scand. 2010;122:63–69. doi: 10.1111/j.1600-0404.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- 15.Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini-Strambi L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med. 2004;5:237–246. doi: 10.1016/j.sleep.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Pérez-Romero T, Comas-Fuentes A, Debán-Fernández M, González-Nuevo Quiñones JP, Maujo-Fernández J. Prevalencia del síndrome de piernas inquietas en las consultas de atención primaria. Rev Neurol. 2007;44:647–651. [PubMed] [Google Scholar]
- 17.Cho YW, Shin WC, Yun CH, Hong SB, Kim JH, Allen RP, Earley CJ. Epidemiology of restless legs syndrome in Korean adults. Sleep. 2008;31:219–223. doi: 10.1093/sleep/31.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee HB, Hening WA, Allen RP, Kalaydjian AE, Earley CJ, Eaton WW, Lyketsos CG. Restless legs syndrome is associated with DSM-IV major depressive disorder and panic disorder in the community. J Neuropsychiatry Clin Neurosci. 2008;20:101–105. doi: 10.1176/jnp.2008.20.1.101. [DOI] [PubMed] [Google Scholar]
- 19*.Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, Ferini-Strambi L. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–1292. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 20.Tison F, Crochard A, Léger D, Bouée S, Lainey E, El Hasnaoui A. Epidemiology of restless legs syndrome in French adults: a nationwide survey: the INSTANT Study. Neurology. 2005;65:239–246. doi: 10.1212/01.wnl.0000168910.48309.4a. [DOI] [PubMed] [Google Scholar]
- 21.Yilmaz K, Kilincaslan A, Aydin N, Kor D. Prevalence and correlates of restless legs syndrome in adolescents. Dev Med Child Neurol. 2011;53:40–47. doi: 10.1111/j.1469-8749.2010.03796.x. [DOI] [PubMed] [Google Scholar]
- 22.Erer S, Karli N, Zarifoglu M, Ozcakir A, Yildiz D. The prevalence and clinical features of restless legs syndrome: a door to door population study in Orhangazi, Bursa in Turkey. Neurol India. 2009;57:729–733. doi: 10.4103/0028-3886.59467. [DOI] [PubMed] [Google Scholar]
- 23.Happe S, Vennemann M, Evers S, Berger K. Treatment wish of individuals with known and unknown restless legs syndrome in the community. J Neurol. 2008;255:1365–1371. doi: 10.1007/s00415-008-0922-7. [DOI] [PubMed] [Google Scholar]
- 24*.Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70:35–42. doi: 10.1212/01.wnl.0000287072.93277.c9. [DOI] [PubMed] [Google Scholar]
- 25*.Gao X, Schwarzschild MA, Wang H, Ascherio A. Obesity and restless legs syndrome in men and women. Neurology. 2009;72:1255–1261. doi: 10.1212/01.wnl.0000345673.35676.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulfberg J, Bjorvatn B, Leissner L, Gyring J, Karlsborg M, Regeur L, Skeidsvoll H, Polo O, Partinen M, Nordic RLS Study Group Comorbidity in restless legs syndrome among a sample of Swedish adults. Sleep Med. 2007;8:768–772. doi: 10.1016/j.sleep.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 27.Bjorvatn B, Leissner L, Ulfberg J, Gyring J, Karlsborg M, Regeur L, Skeidsvoll H, Nordhus IH, Pallesen S. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. 2005;6:307–312. doi: 10.1016/j.sleep.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Högl B, Kiechl S, Willeit J, Saletu M, Frauscher B, Seppi K, Müller J, Rungger G, Gasperi A, Wenning G, Poewe W. Restless legs syndrome: a community-based study of prevalence, severity, and risk factors. Neurology. 2005;64:1920–1924. doi: 10.1212/01.WNL.0000163996.64461.A3. [DOI] [PubMed] [Google Scholar]
- 29.Taşdemir M, Erdoğan H, Börü UT, Dilaver E, Kumaş A. Epidemiology of restless legs syndrome in Turkish adults on the western Black Sea coast of Turkey: A door-to-door study in a rural area. Sleep Med. 2010;11:82–86. doi: 10.1016/j.sleep.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Kim KW, Yoon IY, Chung S, Shin YK, Lee SB, Choi EA, Park JH, Kim JM. Prevalence, comorbidities and risk factors of restless legs syndrome in the Korean elderly population - results from the Korean Longitudinal Study on Health and Aging. J Sleep Res. 2010;19(1 Pt 1):87–92. doi: 10.1111/j.1365-2869.2009.00739.x. [DOI] [PubMed] [Google Scholar]
- 31.Hadjigeorgiou GM, Stefanidis I, Dardiotis E, Aggellakis K, Sakkas GK, Xiromerisiou G, Konitsiotis S, Paterakis K, Poultsidi A, Tsimourtou V, Ralli S, Gourgoulianis K, Zintzaras E. Low RLS prevalence and awareness in central Greece: an epidemiological survey. Eur J Neurol. 2007;14:1275–1280. doi: 10.1111/j.1468-1331.2007.01966.x. [DOI] [PubMed] [Google Scholar]
- 32.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Memory and Morbidity in Augsburg Elderly. Neurology. 2000;54:1064–1068. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 33.Berger K, von Eckardstein A, Trenkwalder C, Rothdach A, Junker R, Weiland SK. Iron metabolism and the risk of restless legs syndrome in an elderly general population--the MEMO-Study. J Neurol. 2002;249:1195–1199. doi: 10.1007/s00415-002-0805-2. [DOI] [PubMed] [Google Scholar]
- 34.Sevim S, Dogu O, Camdeviren H, Bugdayci R, Sasmaz T, Kaleagasi H, Aral M, Helvaci I. Unexpectedly low prevalence and unusual characteristics of RLS in Mersin, Turkey. Neurology. 2003;61:1562–1569. doi: 10.1212/01.wnl.0000096173.91554.b7. [DOI] [PubMed] [Google Scholar]
- 35.Sevim S, Dogu O, Kaleagasi H, Aral M, Metin O, Camdeviren H. Correlation of anxiety and depression symptoms in patients with restless legs syndrome: a population based survey. J Neurol Neurosurg Psychiatry. 2004;75:226–230. [PMC free article] [PubMed] [Google Scholar]
- 36.Mizuno S, Miyaoka T, Inagaki T, Horiguchi J. Prevalence of restless legs syndrome in non-institutionalized Japanese elderly. Psychiatry Clin Neurosci. 2005;59:461–465. doi: 10.1111/j.1440-1819.2005.01399.x. [DOI] [PubMed] [Google Scholar]
- 37.Winkler AS, Trendafilova A, Meindl M, Kaaya J, Schmutzhard E, Kassubek J. Restless legs syndrome in a population of northern Tanzania: a community-based study. Mov Disord. 2010;25:596–601. doi: 10.1002/mds.22806. [DOI] [PubMed] [Google Scholar]
- 38.O'Keeffe ST, Egan D, Myers A, Redmond S. The frequency and impact of restless legs syndrome in primary care. Ir Med J. 2007;100:539–542. [PubMed] [Google Scholar]
- 39.Baos Vicente V, Grandas Pérez F, Kulisevsky Bojarski J, Lahuerta Dal-Ré J, Luquin Piudo R, Cummings Donadio P, Delgado Nicolás MA, Ibáñez Bernabéu V, Iglesias Rodal M, Jover Blanca A, Muñoz Rodríguez A, Navarro Pérez J, Palancar de la Torre JL, Sanfélix Genovés J. El síndrome de piernas inquietas: detección, diagnóstico, consecuencias sobre la salud y utilización de recursos sanitarios. Rev Clin Esp. 2009;209:371–381. doi: 10.1016/s0014-2565(09)72340-9. [DOI] [PubMed] [Google Scholar]
- 40*.Allen RP, Stillman P, Myers AJ. Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in western Europe: Prevalence and characteristics. Sleep Med. 2010;11:31–37. doi: 10.1016/j.sleep.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 41.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–554. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 42.Nomura T, Inoue Y, Kusumi M, Uemura Y, Nakashima K. Prevalence of restless legs syndrome in a rural community in Japan. Mov Disord. 2008;23:2363–2369. doi: 10.1002/mds.22274. [DOI] [PubMed] [Google Scholar]
- 43.Cho SJ, Hong JP, Hahm BJ, Jeon HJ, Chang SM, Cho MJ, Lee HB. Restless legs syndrome in a community sample of Korean adults: prevalence, impact on quality of life, and association with DSM-IV psychiatric disorders. Sleep. 2009;32:1069–1076. [PMC free article] [PubMed] [Google Scholar]
- 44.Celle S, Roche F, Kerleroux J, Thomas-Anterion C, Laurent B, Rouch I, Pichot V, Barthélémy JC, Sforza E. Prevalence and clinical correlates of restless legs syndrome in an elderly French population: the synapse study. J Gerontol A Biol Sci Med Sci. 2010;65:167–73. doi: 10.1093/gerona/glp161. [DOI] [PubMed] [Google Scholar]
- 45.Vogl FD, Pichler I, Adel S, Pinggera GK, Bracco S, De Grandi A, Volpato CB, Aridon P, Mayer T, Meitinger T, Klein C, Casari G, Pramstaller PP. Restless legs syndrome: epidemiological and clinicogenetic study in a South Tyrolean population isolate. Mov Disord. 2006;21:1189–1195. doi: 10.1002/mds.20922. [DOI] [PubMed] [Google Scholar]
- 46.Rangarajan S, Rangarajan S, D'Souza GA. Restless legs syndrome in an Indian urban population. Sleep Med. 2007;9:88–93. doi: 10.1016/j.sleep.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 47.Chen NH, Chuang LP, Yang CT, Kushida CA, Hsu SC, Wang PC, Lin SW, Chou YT, Chen RS, Li HY, Lai SC. The prevalence of restless legs syndrome in Taiwanese adults. Psychiatry Clin Neurosci. 2010;64:170–178. doi: 10.1111/j.1440-1819.2010.02067.x. [DOI] [PubMed] [Google Scholar]
- 48.Benediktsdottir B, Janson C, Lindberg E, Arnardóttir ES, Olafsson I, Cook E, Thorarinsdottir EH, Gislason T. Prevalence of restless legs syndrome among adults in Iceland and Sweden: Lung function, comorbidity, ferritin, biomarkers and quality of life. Sleep Med. 2010;11:1043–1048. doi: 10.1016/j.sleep.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Goodman JD, Brodie C, Ayida GA. Restless leg syndrome in pregnancy. BMJ. 1988;297:1101–1102. doi: 10.1136/bmj.297.6656.1101-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Suzuki K, Ohida T, Sone T, Takemura S, Yokoyama E, Miyake T, Harano S, Motojima S, Suga M, Ibuka E. The prevalence of restless legs syndrome among pregnant women in Japan and the relationship between restless legs syndrome and sleep problems. Sleep. 2003;26:673–677. doi: 10.1093/sleep/26.6.673. [DOI] [PubMed] [Google Scholar]
- 51.Manconi M, Govoni V, De Vito A, Economou NT, Cesnik E, Casetta I, Mollica G, Ferini-Strambi L, Granieri E. Restless legs syndrome and pregnancy. Neurology. 2004;63:1065–1069. doi: 10.1212/01.wnl.0000138427.83574.a6. [DOI] [PubMed] [Google Scholar]
- 52.Alves DA, Carvalho LB, Morais JF, Prado GF. Restless legs syndrome during pregnancy in Brazilian women. Sleep Med. 2010;11:1049–1054. doi: 10.1016/j.sleep.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Ulfberg J, Nyström B, Carter N, Edling C. Prevalence of restless legs syndrome among men aged 18 to 64 years: an association with somatic disease and neuropsychiatric symptoms. Mov Disord. 2001;16:1159–1163. doi: 10.1002/mds.1209. [DOI] [PubMed] [Google Scholar]
- 54.Ulfberg J, Nyström B, Carter N, Edling C. Restless Legs Syndrome among working-aged women. Eur Neurol. 2001;46:17–19. doi: 10.1159/000050750. [DOI] [PubMed] [Google Scholar]
- 55.Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Arch Intern Med. 2004;164:196–202. doi: 10.1001/archinte.164.2.196. [DOI] [PubMed] [Google Scholar]
- 56.Wesstrom J, Nilsson S, Sundstrom-Poromaa I, Ulfberg J. Restless legs syndrome among women: prevalence, co-morbidity and possible relationship to menopause. Climacteric. 2008;11:422–428. doi: 10.1080/13697130802359683. [DOI] [PubMed] [Google Scholar]
- 57.Park YM, Lee HJ, Kang SG, Choi HS, Choi JE, Cho JH, Kim L. Prevalence of idiopathic and secondary restless legs syndrome in Korean Women. Gen Hosp Psychiatry. 2010;32:164–168. doi: 10.1016/j.genhosppsych.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 58*.Castillo PR, Kaplan J, Lin SC, Fredrickson PA, Mahowald MW. Prevalence of restless legs syndrome among native South Americans residing in coastal and mountainous areas. Mayo Clin Proc. 2006;81:1345–1347. doi: 10.4065/81.10.1345. [DOI] [PubMed] [Google Scholar]
- 59.Lee HB, Hening WA, Allen RP, Earley CJ, Eaton WW, Lyketsos CG. Race and restless legs syndrome symptoms in an adult community sample in east Baltimore. Sleep Med. 2006;7:642–645. doi: 10.1016/j.sleep.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 60*.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32:772–778. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Froese CL, Butt A, Mulgrew A, Cheema R, Speirs MA, Gosnell C, Fleming J, Fleetham J, Ryan CF, Ayas NT. Depression and sleep-related symptoms in an adult, indigenous, North American population. J Clin Sleep Med. 2008;4:356–361. [PMC free article] [PubMed] [Google Scholar]
- 62.Broman JE, Mallon L, Hetta J. Restless legs syndrome and its relationship with insomnia symptoms and daytime distress: epidemiological survey in Sweden. Psychiatry Clin Neurosci. 2008;62:472–475. doi: 10.1111/j.1440-1819.2008.01825.x. [DOI] [PubMed] [Google Scholar]
- 63.O'Keeffe ST, Noel J, Lavan JN. Restless legs syndrome in the elderly. Postgrad Med J. 1993;69:701–703. doi: 10.1136/pgmj.69.815.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–203. doi: 10.1093/ageing/23.3.200. [DOI] [PubMed] [Google Scholar]
- 65.Davis BJ, Rajput A, Rajput ML, Aul EA, Eichhorn GR. A randomized, double-blind placebo-controlled trial of iron in restless legs syndrome. Eur Neurol. 2000;43:70–75. doi: 10.1159/000008138. [DOI] [PubMed] [Google Scholar]
- 66.Collado-Seidel V, Kohnen R, Samtleben W, Hillebrand GF, Oertel WH, Trenkwalder C. Clinical and biochemical findings in uremic patients with and without restless legs syndrome. Am J Kidney Dis. 1998;31:324–328. doi: 10.1053/ajkd.1998.v31.pm9469505. [DOI] [PubMed] [Google Scholar]
- 67.Earley CJ, Connor JR, Beard JL, Malecki EA, et al. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54:1698–1700. doi: 10.1212/wnl.54.8.1698. [DOI] [PubMed] [Google Scholar]
- 68.Callaghan N. Restless legs syndrome an uremic neuropathy. Neurology. 1966;16:359–361. doi: 10.1212/wnl.16.4.359. [DOI] [PubMed] [Google Scholar]
- 69*.Winkelmann J, Wetter TC, Collado-Seidel V, Gasser T, Dichgans M, Yassouridis A, Trenkwalder C. Clinical characteristics and frequency of the hereditary restless legs syndrome in a population of 300 patients. Sleep. 2000;23:597–602. [PubMed] [Google Scholar]
- 70.Harvey JC. Cholesterol crystal microembolization: a cause of the restless leg syndrome. South Med J. 1976;69:269–272. [PubMed] [Google Scholar]
- 71.Spillane JD. Restless legs syndrome in chronic pulmonary disease. Br Med J. 1970;4:774–775. doi: 10.1136/bmj.4.5738.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Banerji NK, Hurwitz LJ. Restless legs syndrome with particular reference to its occurrence after gastric surgery. Br Med L. 1970;4:774–775. doi: 10.1136/bmj.4.5738.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lutz EG. Restless legs, anxiety and caffeinism. J Clin Psychiatry. 1978;39:693–698. [PubMed] [Google Scholar]
- 74.Walters AS, Picchietti D, Hening W, Lazzarini A. Variable expressivity in familial restless legs syndrome. Arch Neurol. 1990;47:1219–1220. doi: 10.1001/archneur.1990.00530110079020. [DOI] [PubMed] [Google Scholar]
- 75.Trenkwalder EC, Seidel VC, Gasser T, Oertel WH. Clinical symptoms and possible anticipation in a large kindred of familial restless legs syndrome. Mov Disord. 1996;11:389–394. doi: 10.1002/mds.870110407. [DOI] [PubMed] [Google Scholar]
- 76.Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Movement Disord. 1997;11:61–65. doi: 10.1002/mds.870120111. [DOI] [PubMed] [Google Scholar]
- 77.Winkelmann J, Muller-Myhsok B, Wittchen HU, Hock B, Prager M, Pfister H, Strohle A, Eisensehr I, Dichgans M, Gasser T, Trenkwalder C. Complex segregation analysis of restless legs syndrome provides evidence for an autosomal dominant mode of inheritance in early age at onset families. Ann Neurol. 2002;52:297–302. doi: 10.1002/ana.10282. [DOI] [PubMed] [Google Scholar]
- 78.Ondo WG, Vuong KD, Wang Q. Restless legs syndrome in monozygotic twins: clinical correlates. Neurology. 2000;55:1404–1406. doi: 10.1212/wnl.55.9.1404. [DOI] [PubMed] [Google Scholar]
- 79.Desai AV, Cherkas LF, Spector TD, Williams AJ. Genetic influences in self-reported symptoms of obstructive sleep apnoea and restless legs: a twin study. Twin Res. 2004;7:589–595. doi: 10.1375/1369052042663841. [DOI] [PubMed] [Google Scholar]
- 80.Desautels A, Turecki G, Montplaisir J, et al. Identification of major susceptibility locus for restless legs syndrome on chromosome 12q. Am J Hum Genet. 2001;69:1266–1270. doi: 10.1086/324649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Desautels A, Turecki G, Montplaisir J, Xiong L, Walters AS, Ehrenberg BL, Brisebois K, Desautels AK, Gingras Y, Johnson WG, Lugaresi E, Coccagna G, Picchietti DL, Lazzarini A, Rouleau GA. Restless legs syndrome: confirmation of linkage to chromosome 12q, genetic heterogeneity, and evidence of complexity. Arch Neurol. 2005;62(4):591–596. doi: 10.1001/archneur.62.4.591. [DOI] [PubMed] [Google Scholar]
- 82.Hicks AA, Rye DB, Kristjansson K, Sigmundsson T, Sigurdsson AP, Eiriksdottir I. Population-based confirmation of the 12q RLS locus in Iceland. Mov Disord. 2005;20:S34–S34. [Google Scholar]
- 83.Winkelmann J, Lichtner P, Pütz B, Trenkwalder C, Hauk S, Meitinger T, Strom T, Muller-Myhsok B. Evidence for further genetic locus heterogeneity and confirmation of RLS-1 in restless legs syndrome. Mov Disord. 2006;21:28–33. doi: 10.1002/mds.20627. [DOI] [PubMed] [Google Scholar]
- 84.Bonati MT, Ferini-Strambi L, Aridon P, Oldani A, Zucconi M, Casari G. Autosomal dominant restless legs syndrome maps on chromosome 14q. Brain. 2003;126:1485–1492. doi: 10.1093/brain/awg137. [DOI] [PubMed] [Google Scholar]
- 85.Chen S, Ondo WG, Rao S, Li L, Chen Q, Wang Q. Genomewide linkage scan identifies a novel susceptibility locus for restless legs syndrome on chromosome 9p. Am J Hum Genet. 2004;74:876–885. doi: 10.1086/420772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pichler I, Marroni F, Volpato CB, Gusella JF, Klein C, Casari G, De Grandi A, Pramstaller PP. Linkage analysis identifies a novel locus for restless legs syndrome on chromosome 2q in a South Tyrolean population isolate. Am J Hum Genet. 2006;79:716–723. doi: 10.1086/507875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Levchenko A, Provost S, Montplaisir JY, Xiong L, St-Onge CRJ, Thibodeau P, Rivière JB, Desautels A, Turecki G, Dubé MP, Rouleau GA. A novel autosomal dominant restless legs syndrome locus maps to chromosome 20p13. Neurology. 2006;67(5):900–901. doi: 10.1212/01.wnl.0000233991.20410.b6. [DOI] [PubMed] [Google Scholar]
- 88*.Hening WA, Allen RP, Washburn M, Lesage SR, Earley CJ. The four diagnostic criteria for Restless Legs Syndrome are unable to exclude confounding conditions (“mimics”;) Sleep Med. 2009;10:976–981. doi: 10.1016/j.sleep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wenning GK, Kiechl S, Seppi K, Müller J, Högl B, Saletu M, Rungger G, Gasperi A, Willeit J, Poewe W. Prevalence of movement disorders in men and women aged 50–89 years (Bruneck Study cohort): a population-based study. Lancet Neurol. 2005;4:815–820. doi: 10.1016/S1474-4422(05)70226-X. [DOI] [PubMed] [Google Scholar]
- 90*.Picchietti D, Allen RP, Walters AS, Davidson JE, Myers A, Ferini-Strambi L. Restless legs syndrome: prevalence and impact in children and adolescents - the Peds REST study. Pediatrics. 2007;120:253–266. doi: 10.1542/peds.2006-2767. [DOI] [PubMed] [Google Scholar]
- 91.Wesström J, Nilsson S, Sundström-Poromaa I, Ulfberg J. Health-related quality of life and restless legs syndrome among women in Sweden. Psychiatry Clin Neurosci. 2010;64:574–579. doi: 10.1111/j.1440-1819.2010.02116.x. [DOI] [PubMed] [Google Scholar]
- 92.Tsuboi Y, Imamura A, Sugimura M, Nakano S, Shirakawa S, Yamada T. Prevalence of restless legs syndrome in a Japanese elderly population. Parkinsonism Relat Disord. 2009;15:598–601. doi: 10.1016/j.parkreldis.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 93.Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 94.Tan EK, Seah A, See SJ, Lim E, Wong MC, Koh KK. Restless legs syndrome in Asian population: A study in Singapore. Mov Disord. 2001;16:577–579. doi: 10.1002/mds.1102. [DOI] [PubMed] [Google Scholar]
- 95.Nichols DA, Allen RP, Grauke JH, Brown JB, Rice ML, Hyde PR, Dement WC, Kushida CA. Restless legs syndrome symptoms in primary care: a prevalence study. Arch Intern Med. 2003;163:2323–2329. doi: 10.1001/archinte.163.19.2323. [DOI] [PubMed] [Google Scholar]
- 96.Alattar M, Harrington JJ, Mitchell CM, Sloane P. Sleep problems in primary care: a North Carolina Family Practice Research Network (NC-FP-RN) study. J Am Board Fam Med. 2007;20:365–374. doi: 10.3122/jabfm.2007.04.060153. [DOI] [PubMed] [Google Scholar]
- 97.Möller C, Wetter TC, Köster DJ, Stiasny-Kolster K. Differential diagnosis of unpleasant sensations in the legs: prevalence of restless legs syndrome in a primary care population. Sleep Med. 2010;11:161–166. doi: 10.1016/j.sleep.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 98.Cesnik E, Casetta I, Turri M, Govoni V, Granieri E, Strambi LF, Manconi M. Transient RLS during pregnancy is a risk factor for the chronic idiopathic form. Neurology. 2010;75:2117–2120. doi: 10.1212/WNL.0b013e318200d779. [DOI] [PubMed] [Google Scholar]
- 99.Rijsman RM, de Weerd AW, Stam CJ, Kerkhof GA, Rosman JB. Periodic limb movement disorder and restless legs syndrome in dialysis patients. Nephrology (Carlton) 2004;9:353–361. doi: 10.1111/j.1440-1797.2004.00330.x. [DOI] [PubMed] [Google Scholar]