Abstract
Anterior dislocation of the shoulder is a common injury which is often reduced in the emergency department, without specialist orthopedic input. We report a case of an irreducible locked anterior glenohumeral dislocation with impaction of the humeral head onto the antero-inferior glenoid rim and subsequent generation of a Hill–Sachs lesion. To our knowledge, we describe the first reported case of using computer-assisted tomography to generate a sequence of movements to safely disimpact the locked dislocation without causing further iatrogenic injury or a fracture through the humeral articular surface. This novel image-assisted closed reduction technique spared the patient from the morbidity associated with performing open reduction surgery. At 6-month follow-up, the patient reported no re-dislocations, returned to work and had excellent range of motion.
Keywords: Anterior, computer tomography, Hill–Sachs, impacted, irreducible, shoulder dislocation
INTRODUCTION
Anterior dislocation of the shoulder is a common injury,[1] which is often reduced in the emergency department without the need for specialist orthopedic input.[2] In cases where anterior shoulder dislocations cannot be reduced in the emergency department, a successful closed reduction can usually be performed under general anesthetic. In the rare instances where this fails, open surgical reduction may be required.
Mechanical obstacles may frequently impede closed reduction of an anterior dislocation.[3] These include: Interposition of the long head of biceps tendon or subscapularis tendon; impaction of the humeral head on glenoid labrum and dislocated bony fragments from the glenoid or greater tuberosity.[3,4]
We describe a case of an irreducible locked primary anterior glenohumeral dislocation with impaction of the humeral head onto the antero-inferior glenoid rim with subsequent generation of a Hill–Sachs lesion. Hill–Sachs lesions exist in 68% of primary anterior glenohumeral dislocations.[1] However, a locked irreducible impacted humerus is rare and has only been reported on an individual basis. We utilized a novel closed reduction technique using computed tompography (CT) to assist in generating a sequence of movements to disimpact the shoulder. Thus, it avoids further iatrogenic injuries and operative surgery, which is the traditional course of action in this situation and has associated complications and morbidity.
CASE REPORT
A 57-year-old gentleman, volunteer community driver, with a history of ethanol abuse, presented to the emergency department 2 days following a mechanical fall, with left shoulder pain and reduced function. He slipped on the pavement, fell backward, outstretching his left arm to break the fall, sustaining an isolated injury to the left shoulder. The only significant past medical history was recurrent deep venous thrombosis and pulmonary emboli for which he takes long-term oral anticoagulation (warfarin). On clinical examination, the patient had reduced range of motion and there was no neurovascular deficit in the left upper limb. Initial radiographs confirmed a primary glenohumeral dislocation with a possible Bankart lesion. Based on the plain radiographs [Figure 1], the patient underwent two unsuccessful left shoulder manipulations under sedation in the emergency department. Subsequently, manipulation under general anesthetic was performed the following day by the orthopedic team and was similarly unsuccessful. At this point operative intervention was considered, but given the long-term warfarin use and history of chronic alcohol abuse, it was felt on balance the case should be managed non-surgically, if at all possible.
Figure 1(a,b).
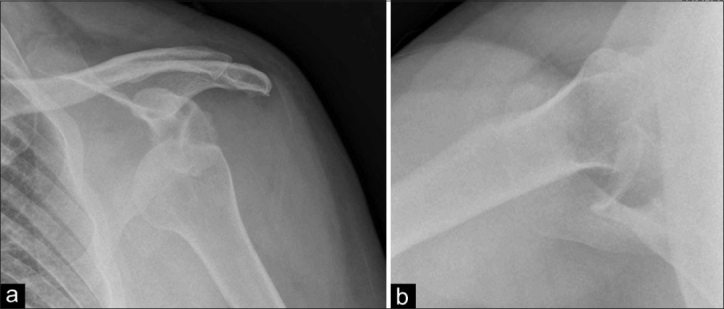
Plain radiographs, AP and axillary views identifying humeral head lying inferior to the glenoid cavity. Radiologist initially suspected a fracture of the glenoid labrum, a Bankart lesion
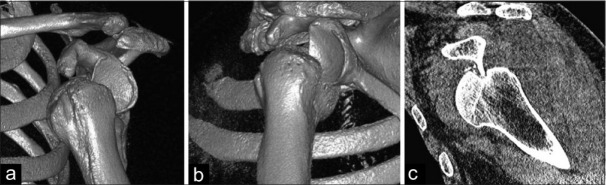
CT of the left shoulder was performed, which identified a 2-cm, >20% Hill–Sachs lesion with significant impaction of the humeral head and anterior dislocation. There were small bony fragments around inferior glenoid; these little flecks of bone might have been produced during attempted reduction under anesthesia. Figure 2 demonstrates significant undermining of the humeral articular surface. After review of the image, it was appreciated that an incorrect reduction may cause further soft tissue injury or humeral fractures. Following this, a planned sequence of movements was generated in an attempt to reduce the shoulder. The patient underwent a second manipulation under anesthetic; the arm was externally rotated by 40° with the arm in extension, after which direct lateral traction was applied and the shoulder was successfully disimpacted and reduced without causing any iatrogenic injury. Examination under anesthesia demonstrated shoulder joint stability. Patient was discharged with a shoulder immobilizer for 4 weeks and sling thereafter for 2 weeks with physiotherapy. Patient suffered initial stiffness due to immobilization, but was responding well to physiotherapy with good rotations and range of motion. At 6-month follow-up, there were no further episodes of re-dislocation reported. He has returned to work as a driver and reports no functional deficit in comparison to pre-operative levels or effect on the quality of life. On examination, the patient can abduct to 140°, has forward flexion to 170° and normal rotations.
Figure 2(a-c).
Assisted computer tomography with three-dimensional reconstruction showing an anterior sub-coracoid dislocated left shoulder with humeral head impacted on antero-inferior rim of glenoid
DISCUSSION
Failure to reduce an acute anterior shoulder dislocation is rare,[5] particulalry following manipulation under anesthesia.[6] Open reduction is the traditional course of management in this scenario, with intraopertive findings frequently reporting interposition of a structure into the joint.[5] An avulsion fracture of the greater tuberosity, for instance, occurs in 10–12% of anterior dislocations.[4] Irrespective of a high incidence of Bankart lesions and Hill–Sachs lesions, most acute primary dislocations are successfully managed in the emergency department.[2]
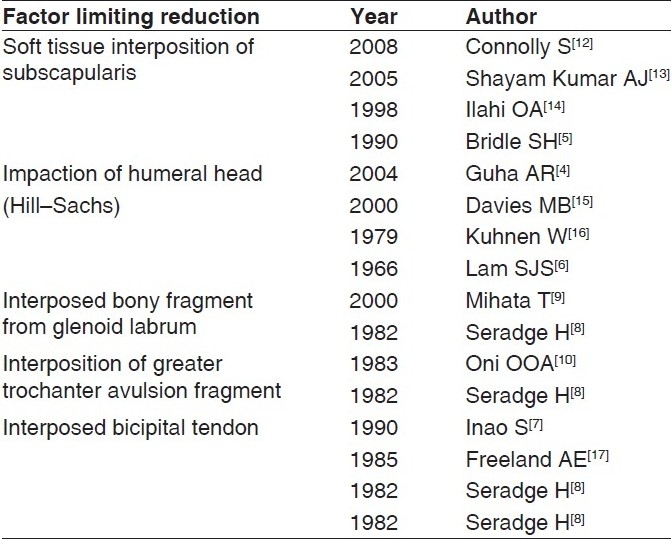
Table 1 summarizes a review of literature and causes for failed reduction. Guha et al. have reported 10 cases to date since 1966.[4] The majority of cases are males over 45 years of age. Each report identifies the structure mechanically obstructing reduction, such as a displaced glenoid labrum, interposition of the tendon of the long head of biceps,[7,8] a bony fragment from the glenoid[9] and a fragment of the greater tuberosity.[10] Most importantly, all the patients in previous reports went on to open reduction, exposing the patient to a surgical procedure and its associated morbidity, and producing reduced range of motion, particularly external rotation. Arthroscopic surgery does not sacrifice the subscapularis with better functional outcomes; it can also be performed as an outpatient. However, it has a higher re-dislocation rate and open procedure remains the gold standard.[11]
Table 1.
A summary of case reports published between 1966 and 2008, with individual causes for irreducible anterior dislocation
The dislocations reported by Guha et al., Lam and Kuhnen et al. are of particular relevance.[4,6,16] In these cases, the glenohumeral joint failed to reduce due to an impacted humeral head on the glenoid rim, with subsequent Hill–Sachs type lesions and tight anterior subscapularis giving resistance. The injuries required open reduction with disimpaction following division of the subscapularis muscle. Lam and Kuhnen et al. performed Putti Platt procedures, where the subscapularis tendon is divided and re-attached, stabilizing the joint but reducing external rotation. Postoperatively, the authors report good stability with satisfactory long-term functional outcome,[6,16] whilst not commenting on any complications. The authors do not report imaging beyond plain radiographs. Intraoperative disruption to the rotator cuff has a detrimental effect on recovery, stiffness and range of movement. Our patient benefited from high-resolution CT imaging and 3D reconstruction, modifying closed reduction techniques and preventing open surgery. This is beneficial to a patient on long-term anticoagulation for recurrent deep vein thrombosis and alcohol dependence. The enhanced CT views obtained identified the need for lateral traction to disimpact the head, not apparent on mobile fluoroscopy during the initial reduction attempts.
Plain radiographs diagnosed dislocation of the glenohumeral joint, with Stryker notch views identifying Hill–Sachs lesions. However, detecting an impacted humerus is difficult on plain radiographs, with CT having greater sensitivity and identifying soft tissue components. Traditionally, CT and Magnetic Resonance Imaging (MRI) are used post reduction to assess stability in cases of recurrent dislocation. MRI is superior when identifying soft-tissue and bony injuries.[18] CT scanning is more accessible, less expensive and provides reproducible outcomes when assessing bony and soft tissue injury.[19] Three-dimensional techniques provide an accurate analysis of the location and extent of injury.[20] Table 1 summarizes the mechanical obstacles to reduction, where soft tissue causes predominate. Additionally, a case described in 2010 utilized CT imaging to identify the long head of biceps tendon causing obstructing reduction.[21] It was initially a posterior dislocation, converted to anterior during reduction attempts. The patient was definitively managed with open reduction. The authors support CT and MRI as a useful adjunct to conventional radiography, allowing identification of soft tissue obstacles to reduction with good sensitivity.[21]
Primary glenohumeral dislocation may be associated with soft-tissue and neurovascular complications. Reduction of the shoulder joint can cause iatrogenic injuries. Beeson and Visser et al. state that downward traction, rotation and abduction during manipulative reduction endangers neurovascular structures.[5,22] Hill–Sachs lesions are often clinically insignificant; however, humeral head impaction can result in more significant fractures through humeral neck during reduction.[1] Axillary artery transection, where the elderly are more susceptible, after shoulder dislocation is rare.[23] Recurrent dislocation, particularly in the young, causes significant morbidity after acute injury. In short-term follow-up, our patient did not report any neurovascular deficit and no further dislocations. Initial stiffness and reduced range of motion due to immobilization improved with physiotherapy, as expected. We are keen to follow him up to see if he develops instability and requires intervention for the large Hill–Sachs lesion. Guha et al. reported a similar case of humeral head impaction which underwent open reduction. The subscapularis was divided and subsequently repaired to allow this reduction. Three months following surgery, the patient was able to abduct to 60° with functional rotations. Interestingly, the humeral head defect interfered with extremes of abduction; however, the patient refused a hemiarthroplasty.[4] It can be seen in literature reports that primary anterior dislocation in patients aged less than 40 is invariably associated with glenoid labrum disruption and instability.[1] Rotator cuff lesions are more common with increasing age.[24] Open reduction can impair rotator cuff integrity further with increased stiffness and impaired rehabilitation.
Reduction technique is often decided on an individual patient basis, with pain relief, patient anxiety, operator preference, and resource allocation influencing the choice of the method. The techniques have similar success rates, but complications can vary.[11] Repeated forceful manipulation may have increased risk of fracture and neurovascular injury. To our knowledge, this is the first reported case of an acute primary traumatic irreducible anterior shoulder dislocation being successfully manipulated under anesthesia, without surgery, due to enhanced images obtained through CT identifying a Hill–Sachs lesion and locked anterior dislocation.
CONCLUSIONS
An irreducible anterior glenohumeral dislocation with an impacted humeral head is rare. The long head of biceps tendon, subscapularis muscle and glenoid labrum lesions may also obstruct shoulder reduction.
Anterior shoulder dislocations that do not reduce should not undergo repeated manipulation to avoid iatrogenic neurovascular injury and fractures.
Failure to reduce anterior glenohumeral dislocations should prompt CT imaging to define injury and cause of obstruction to reduction, prior to further manipulation or operative intervention.
CT imaging defines the manipulative maneuvers required to disimpact and reduce the shoulder without resorting to open surgical techniques thus avoiding its associated morbidities.
CT imaging is sensitive and accessible. Additional information on soft-tissue and bony deficits, identifying potential instability, assists long-term treatment plans.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Beeson MS. Complications of shoulder dislocation. Am J Emerg Med. 1999;17:288–95. doi: 10.1016/s0735-6757(99)90127-4. [DOI] [PubMed] [Google Scholar]
- 2.Perron AD, Ingerski MS, Brady WJ, Erling BF, Ullman EA. Acute complications associated with shoulder dislocation at an academic emergency department. J Emerg Med. 2003;24:141–5. doi: 10.1016/s0736-4679(02)00717-5. [DOI] [PubMed] [Google Scholar]
- 3.Connolly S, Ritchie D, Sinopidis C, Brownson P, Aniq H. Irreducible anterior dislocation of the shoulder due to soft tissue interposition of subscapularis tendon. Skeletal Radiol. 2010;37:63–5. doi: 10.1007/s00256-007-0370-y. [DOI] [PubMed] [Google Scholar]
- 4.Guha AR, Jago ER. Irriducible acute anterior shoulder dislocation. Int J Clin Pract. 2004;58:1184–6. doi: 10.1111/j.1742-1241.2004.00132.x. [DOI] [PubMed] [Google Scholar]
- 5.Bridle SH, Ferris BD. Irreducible acute anterior dislocation of the shoulder: Interposed Scapularis. J Bone Joint Surg Br. 1990;72B:1078–9. doi: 10.1302/0301-620X.72B6.2246295. [DOI] [PubMed] [Google Scholar]
- 6.Lam SJ. Acute irreducible anterior dislocation of the shoulder. J Bone Joint Surg. 1966;48B:132–3. [PubMed] [Google Scholar]
- 7.Inao S, Hirayama T, Takemitsu Y. Irreducible acute anterior dislocation of the shoulder: Interposed bicipital tendon. J Bone Joint Surg Br. 1990;72B:1079–80. doi: 10.1302/0301-620X.72B6.2246296. [DOI] [PubMed] [Google Scholar]
- 8.Seradge H, Orme G. Acute irreducible anterior dislocation of the shoulder. J Trauma. 1982;22:330–2. doi: 10.1097/00005373-198204000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Mihata T, Doi M, Abe M. Case report: Irreducible acute anterior dislocation of the shoulder caused by interposed fragment of anterior glenoid rim. J Orthop Sci. 2000;5:404–6. doi: 10.1007/pl00021457. [DOI] [PubMed] [Google Scholar]
- 10.Oni OO. Irreducible anterior dislocation of the shoulder due to a loose fragment from an associated fracture of the greater tuberosity. Injury. 1983;15:138. doi: 10.1016/0020-1383(83)90043-8. [DOI] [PubMed] [Google Scholar]
- 11.Wen DY. Current concepts in the treatment of anterior shoulder dislocation. Am J Emerg Med. 1999;17:401–7. doi: 10.1016/s0735-6757(99)90097-9. [DOI] [PubMed] [Google Scholar]
- 12.Connolly S, Ritchie D, Sinopidis C, Brownson P, Aniq H. Irreducible anterior dislocation of the shoulder due to soft tissue interposition of subscapularis tendon. Skeletal Radiol. 2008;37:63–5. doi: 10.1007/s00256-007-0370-y. [DOI] [PubMed] [Google Scholar]
- 13.Shayam Kumar AJ, Charity R, Periera A, Deshmukh SC. Interposed subscapularis: A rare cause of irreducible shoulder dislocation. Eur J Orthop Surg Traumatol. 2005;15:42–44. [Google Scholar]
- 14.Ilahi OA. Irreducible anterior shoulder dislocation with fracture of the greater tuberosity. Am J Orthop (Belle Mead NJ) 1998;27:576–8. [PubMed] [Google Scholar]
- 15.Davies MB, Rajasekhar C, Bhamra MS. Irreducible anterior shoulder dislocation: The greater tuberosity Hill-Sachs lesion. Injury. 2000;31:470–1. doi: 10.1016/s0020-1383(00)00016-4. [DOI] [PubMed] [Google Scholar]
- 16.Kuhnen W, Groves RJ. Irreducible acute anterior dislocation of the shoulder: Case report. Clin Orthop Relat Res. 1979;139:167–8. [PubMed] [Google Scholar]
- 17.Freeland AE, Higgins RW. Anterior shoulder dislocation with posterior displacement of the long head of the biceps tendon.Arthrographic findings. A case report. Orthopedics. 1985;8:468–9. doi: 10.3928/0147-7447-19850401-06. [DOI] [PubMed] [Google Scholar]
- 18.Owens BD, Nelson BJ, Duffey ML, Mountcastle SB, Taylor DC, Cameron KL, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am. 2010;92:1605–11. doi: 10.2106/JBJS.I.00851. [DOI] [PubMed] [Google Scholar]
- 19.Fogerty S, King DG, Groves C, Scally A, Chandramohan M. Interobserver variation in reporting CT Arthrograms of the shoulder 2010 Nov 10. Eur J Radiol. 2010 Nov 10; doi: 10.1016/j.ejrad.2010.10.009. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Kirtland S, Resnick D, Sartoris DJ, Pate D, Greenway G. Chronic unreduced dislocations of the glenohumeral joint: Imaging strategy and pathologic correlation. J Trauma. 1988;28:1622–31. doi: 10.1097/00005373-198812000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Day MS, Epstein DM, Young BH, Jazrawi LM. Irreducible anterior and posterior dislocation of the shoulder due to incarceration of the biceps tendon. Int J Shoulder Surg. 2010;4:83–5. doi: 10.4103/0973-6042.76970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Visser CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery. J Bone Joint Surg Br. 1999;81:679–85. doi: 10.1302/0301-620x.81b4.9005. [DOI] [PubMed] [Google Scholar]
- 23.Karkos CD, Karamanos DG, Papazoglou KO, Papadimitriou DN, Zambas N, Gerogiannis IN, et al. Axillary artery transection after recurrent anterior shoulder dislocation. Am J Emerg Med. 2010;28:119.e5–7. doi: 10.1016/j.ajem.2009.04.033. [DOI] [PubMed] [Google Scholar]
- 24.Toolanen G, Hildingsson C, Hedlund T, Knibestol M, Oberg L. Early complications after anterior dislocation of the shoulder in patients over 40 years. Acta Orthop Scand. 1993;64:549–52. doi: 10.3109/17453679308993690. [DOI] [PubMed] [Google Scholar]