Abstract
Endovascular coiling has become the primary treatment modality for the treatment of intracranial ruptured aneurysms in many centers. A multicenter randomized controlled trial (RCT), ISAT study, has demonstrated that endovascular coiling of ruptured intracranial aneurysms has benefits over surgical clipping in those patients suitable for either treatment. Because RCT comparing conservative management with surgical clipping and with endovascular coiling have not been performed to date for unruptured intracranial aneurysms, the best management for unruptured aneurysm remains unclear. A RCT is ongoing to answer the question whether active treatment can improve the outcome of patients with unruptured intracranial aneurysms as compared with observation.
Keywords: Intracranial aneurysm, Endovascular treatment, Randomized controlled trial
The management strategy for the treatment of intracranial aneurysms differs significantly between the patients with ruptured aneurysms and those with unruptured aneurysms. Ruptured aneurysms should be treated urgently (within 72 h of bleeding) to prevent rerupture. After the results of the International Subarachnoid Aneurysm Trial (ISAT) study were released, endovascular coiling has becoming increasingly common for the treatment of intracranial ruptured aneurysms over the past decade. The best management for the unruptured intracranial aneurysms remains unclear to date. Randomized controlled trial (RCT) is one of the most powerful tools to provide the best evidence for making clinical decisions. Unfortunately, there is scarce RCT evidence on the management of intracranial aneurysms. The goal of this article is to provide a brief review on RCT for the treatment of intracranial ruptured or unruptured aneurysms.
Randomized Controlled Trials for Ruptured Intracranial Aneurysms
Endovascular occlusion with detachable platinum coils has become an established treatment for managing patients who have ruptured intracranial aneurysms (1-3). Although numerous studies regarding endovascular or surgical treatment for ruptured intracranial aneurysms have been reported in the literature, there are only two randomized, prospective studies comparing endovascular coiling and surgical clipping to date (4-6).
The results of the first, prospective randomized trial from Finland compared endovascular and surgical treatment of ruptured intracranial aneurysms was published in 1999 and 2000 (4, 5). The study included 109 patients with acute (< 72 hours) aneurysmal subarachnoid hemorrhage who were suitable for both endovascular coiling and surgical clipping. Aneurysms were considered suitable for both coiling and clipping if: 1) the neck of the aneurysm was smaller than the fundus; 2) it was not a fusiform aneurysm; 3) the neck of the aneurysm and relationship to the parent vessel was distinguishable; and 4) the diameter of the aneurysm was bigger than the smallest coil, or 2 mm, resulting in approximately half of the patients with aneurysmal subarachnoid hemorrhage suitable for randomization. The study assessed the angiographic outcome and clinical outcome at 3 and 12 months. As an immediate postembolization angiographic result, posterior circulation aneurysms showed more complete occlusion with coiling than with surgery (p = 0.045), whereas anterior circulation (anterior cerebral artery, anterior communicating aneurysm, and pericallosal artery) aneurysms showed the better angiographic outcome with surgical clipping than with endovascular coiling (p = 0.005). The procedure-related mortality rate was 2% in the endovascular group and 4% in the surgical group. One patient had early rebleeding after incomplete coil embolization. At 12 months, the clinical outcome did not significantly differ between two groups, as 79% of endovascular versus 75% of surgical patients had good or moderate recovery on Glasgow outcome scale (p = 0.3). As 12-month angiographic results, 76.9% of the endovascular group showed total obliteration of the aneurysm, whereas 86.0% of the surgical group showed total obliteration, which was not statistically significant. The authors concluded that the clinical outcome at 3 and 12 months was comparable after endovascular and surgical treatment of ruptured intracranial aneurysms.
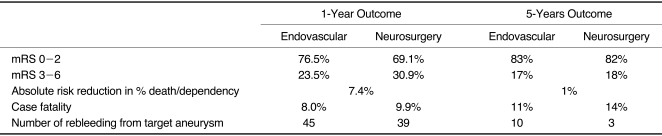
ISAT was a randomized, multicenter trial compared surgical clipping with endovascular coiling in patients with ruptured intracranial aneurysms (6-8). Between 1994 and 2002, 2143 patients were enrolled in the study from 43 neurosurgical centers, most in the United Kingdom and Europe. The primary objective of the ISAT was to determine whether there was a reduction in the proportion of patients who were dead or dependent (defined as modified Rankin Scale, mRS 3-6) at 1 year by following a coiling strategy compared with a clipping strategy. Recruitment of patients was stopped after an interim analysis showed a benefit of endovascular treatment on the primary outcome at 1 year. The complete 1-year data from ISAT was published in The Lancet in 2005 (7). Two-hundred-fifty of 1,063 (23.5%) patients allocated to endovascular coiling were dead or dependent at 1 year, compared with 326 of 1,055 (30.9%) patients allocated to surgical clipping: an absolute risk reduction of 7.4% (95% CI 3.6% to 11.2%, p = 0.0019). The early survival advantage in the coiled group was maintained for up to 7 years and was statistically significant (log rank p = 0.03).The risk of epilepsy was substantially lower with endovascular coiling than with clipping: relative risk 0.52 (95% CI 0.37 to 0.74). There was no significant difference in the frequency of rebleeding between the groups (log rank p = 0.22). The rebleeding risk after 1 year in the coiled group is approximately 0.2% per patient year with follow-up from 1 to 8 years with a mean of 4 years. ISAT concluded that endovascular coiling of ruptured intracranial aneurysms, when a patient is in good clinical grade and the aneurysm anatomy is suitable for endovascular treatment, is more likely than neurosurgical treatment to lead to independent survival at l year. Since the 1-year results of ISAT study were released, treatment of patients with a ruptured intracranial aneurysm has changed significantly over the past decade. In many centers, coiling has become the mainstay of treatment of ruptured intracranial aneurysms when both coiling and clipping are considered suitable.
The long-term follow-up results of ISAT were published in The Lancet Neurology in 2009 (8). At 5 years, the proportion of independent survivors did not differ between the two groups. Six-hundred-twenty-six of 755 (83%) patients treated by endovascular coiling were independent at 1 year, compared with 584 of 713 (82%) patients treated by surgical clipping. However, the risk of death was still significantly lower in the coiling group than in the clipping group (relative risk 0.77, 95% CI 0.61-0.98; p = 0.03). At 5 years, 112 of 1,046 (11%) patients in the coiling group have died, compared with 144 of 1,041 (14%) patients in the clipping group (log rank, p = 0.03). The annual risk of the treated aneurysm rebleeding is higher in the patients treated by the coiling than in those treated by the clipping: 10 rebleeding occurred in the coiling group and 3 in the clipping group. However, the risk remains low and is at a similar level to the risk of further subarachnoid hemorrhage (SAH) from another source, either a pre-existing aneurysm or a newly formed aneurysm. The main finding of the study is that rates of independence become essentially equivalent at 5 years, whereas mortality rates still favor the patients treated by endovascular coiling. The major contribution to the achievement of equivalent long-term functional outcomes might be the continuing improvement in the neurological function of less severely disabled patients in the clipping group between year 2 and year 5. Table 1 summarizes the 1-year and 5-year clinical outcomes of ISAT study. In summary, ISAT has demonstrated that endovascular coiling of ruptured intracranial aneurysms has benefits over surgical clipping in those patients suitable for either treatment, but this difference decreases over time (9).
Table 1.
Clinical Outcome at 1-Year and 5-Year in the International Subarachnoid Aneurysm Trials (ISAT)
mRS: modified Rankin scale
Randomized Controlled Trials for Unruptured Intracranial Aneurysms
With the significant advances in the imaging techniques and widespread use of noninvasive intracranial imaging studies such as CT or MR angiography, the incidental detection of unruptured intracranial aneurysm (UIA) has increased greatly. The management of patients with UIAs becomes an important public health issue, but still remains a controversial topic. There has been no published randomized, controlled trial with regard to compare natural history and coiling or clipping, or clipping and coiling for the management of patients with UIAs, but one such trial is currently ongoing.
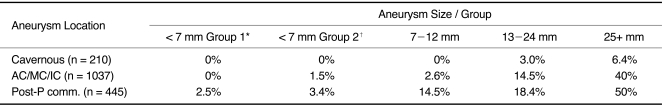
The natural history of UIA remains uncertain. International Study of Unruptured Intracranial Aneurysms (ISUIA) is the largest natural history study of UIA (10,11). A prospective cohort study from ISUIA showed that the 5-year cumulative rupture risk of UIAs smaller than 7 mm in the anterior circulation with no history of SAH to be 0% and that with a history of SAH 1.5% (11). Aneurysms at posterior circulations (basilar tip and the posterior communicating artery), aneurysms larger than 10 mm, and aneurysms that are found in patients who had bled from a prior aneurysm were found to have higher risks (about 0.5% per year). These rupture rates were somewhat lower than previous estimates. Table 2 shows the 5-year cumulative rupture rates of UIA among patients in the unopearated prospective cohort of ISUIA. ISUIA data provided the first, international prospective data set, but there have been many criticisms of the ISUIA study, especially with regard to patient selection bias. Detailed discussion about these criticisms is out of range for this review and is well described elsewhere.
Table 2.
5-Year Cumulative Rupture Rates According to Size and Location of Unruptured Aneurysm and According to Patient Group, Among Patients in the Unoperated Cohort of ISUIA
AC, anterior communicating or anterior cerebral artery; Cavernous, cavernous carotid artery; IC, internal carotid artery (not cavernous carotid artery); MC, middle cerebral artery; Post-P comm, vertebrobasilar, posterior cerebral artery system, or the posterior communicating artery.
*Patients in group 1 had no history of subarachnoid hemorrhage.
†Patients in group 2 had a history of subarachnoid hemorrhage from a separate aneurysm.
It is generally believed that the risk of rupture for a UIA is approximately 1% per year for lesions 7-10 mm in diameter (12, 13). In a single-center, observational study published in 2009, Ishibashi et al. reported that the annual rupture rate for 529 UIAs was 1.4% during mean follow-up period of 905.3 days (14). In their study, a previous history of SAH (the hazard ratio 7.3; 95% CI, 2.5 to 21.2), posterior circulation aneurysm (the hazard ratio 2.9; 95% CI, 1.1 to 8), and large size were significant independent predictors for aneurysm rupture. The hazard ratio in the large sized (> 10 mm) and giant (> 25 mm) aneurysm were 12.3 and 50 compared with that for small sized (< 5 mm) UIAs. More recently, a prospective multi-center, observational study to determine the optimal management for small UIAs has been published by Japanese group (15). In that study, 448 UIAs < 5 mm in size have been followed up for a mean of 41 months. The annual rupture rate for small UIAs smaller than 5mm is quite low: 0.54% overall, 0.34% for single aneurysms, and 0.95% for multiple aneurysms. Patient < 50 years of age, aneurysm diameter of > 4 mm, hypertension, and aneurysm multiplicity were found to be significant predictive factors for rupture of small UIAs. Other reported risk factors for rupture of UIAs in the literature include cigarette smoking and female sex.
Endovascular coiling of UIAs can be performed with relative safety. A recently published systematic review and meta-analysis found an overall risk of poor outcomes (mRS 3-6) is in the range of 4-5% after endovascular coiling in patients with UIA (16). Recurrence rate is high: 24.4% of the patients followed up for 0.4-3.2 years. The annual risk of bleeding per patient-year after endovascular coiling was 0.2%, but the lack of systematic follow-up, short observation periods, and missing data hampered the assessment of clinical efficacy of endovascular coiling (16).
A RCT is ongoing to answer the question whether active treatment can improve the outcome of patients with UIA as compared with observation. TEAM trial (Trial on Endovascular Aneurysm Management) is an international, randomized, multicenter, controlled trial comparing endovascular treatment versus conservative management of UIAs (17). Primary endpoint is mortality and morbidity (mRS 3-6) from intracranial hemorrhage or treatment. Secondary endpoints include incidence of hemorrhagic events, morbidity related to endovascular coiling, morphological results, overall clinical outcome and quality of life. The study will be conducted in 60 international centers and will enroll 2,002 patients equally divided between the two groups. The duration of the study is 14 years, the first three years being for patient recruitment plus a minimum of 10 years of follow-up. The study investigators are currently enrolling participating centers and patients.
Preventive treatment with coiling or clipping in patients with UIA can be justified when the benefits outweigh the risks of such treatments, with strong evidence supported by valid data. Currently, in the absence of randomized controlled studies, any proposed treatment algorithms for UIAs remain invalid (16, 17).
In conclusions, short-term results of ISAT study showed that endovascular coiling of ruptured intracranial aneurysms, when a patient is in good clinical grade and the aneurysm anatomy is suitable for endovascular treatment, is more likely than neurosurgical treatment to lead to independent survival at l year. Long-term follow-up results of ISAT study showed that rates of independence become essentially equivalent at 5 years, whereas mortality rates still favor the patients treated by endovascular coiling. Thus, ISAT study has demonstrated that endovascular coiling of ruptured intracranial aneurysms has benefits over surgical clipping in those patients suitable for either treatment, but this difference decreases over time.
Because RCT comparing conservative management with surgical clipping and with endovascular coiling have not been performed to date for unruptured intracranial aneurysms, the best management for UIAs remains unclear. A RCT is ongoing to answer the question whether active treatment can improve the outcome of patients with UIA as compared with observation.
References
- 1.Qureshi AI, Janardhan V, Hanel RA, Lanzino G. Comparison of endovascular and surgical treatments for intracranial aneurysms: an evidence-based review. Lancet Neurol. 2007;6:816–825. doi: 10.1016/S1474-4422(07)70217-X. [DOI] [PubMed] [Google Scholar]
- 2.Raja PV, Huang J, Germanwala AV, Gailloud P, Murphy KP, Tamargo RJ. Microsurgical clipping and endovascular coiling of intracranial aneurysms: a critical review of the literature. Neurosurgery. 2008;62:1187–1202. doi: 10.1227/01.neu.0000333291.67362.0b. [DOI] [PubMed] [Google Scholar]
- 3.van der Schaaf I, Algra A, Wermer M, Molyneux A, Clarke M, van Gijn J, et al. Endovascular coiling versus neurosurgical clipping for patients with aneurysmal subarachnoid hemorrhage. Cochrane Database Syst Rev. 2005;(4):CD003085. doi: 10.1002/14651858.CD003085.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Vanninen R, Koivisto T, Saari T, Hernesniemi J, Vapalahti M. Ruptured intracranial aneurysms: acute endovascular treatment with Electrolytically detachable coils - a prospective study. Radiology. 1999;211:325–336. doi: 10.1148/radiology.211.2.r99ap06325. [DOI] [PubMed] [Google Scholar]
- 5.Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M. Outcomes of early endovascular versus surgical treatment of ruptured cerebral aneurysms. Stroke. 2000;31:2369–2377. doi: 10.1161/01.str.31.10.2369. [DOI] [PubMed] [Google Scholar]
- 6.Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International subarachnoid aneurysm trial collaborative group. International subarachnoid aneurysm trial (ISAT) of neurological clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 7.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International subarachnoid aneurysm trial (ISAT) of neurological clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809–817. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 8.Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M, et al. ISAT Collaborators. Risk of recurrent subarachnoid hemorrhage, death, or dependence and standardized mortality ratios after clipping or coiling of an intracranial aneurysm in the international subarachnoid aneurysm trial (ISAT): long-term follow-up. Lancet Neurol. 2009;8:427–433. doi: 10.1016/S1474-4422(09)70080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broderick J. Clipping or coiling: the first step for ruptured aneurysms. Lancet Neurol. 2009;8:414–415. doi: 10.1016/S1474-4422(09)70086-9. [DOI] [PubMed] [Google Scholar]
- 10.International study of unruptured intracranial aneurysms investigators. Unruptured intracranial aneurysms - risk of rupture and risks of surgical intervention. N Engl J Med. 1998;339:1725–1733. doi: 10.1056/NEJM199812103392401. [DOI] [PubMed] [Google Scholar]
- 11.Wiebers DO, Whisnant JP, Huston J, 3rd, Meissner I, Brown RD, Jr, Piepgras DG, et al. International study of unruptured intracranial aneurysms investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–110. doi: 10.1016/s0140-6736(03)13860-3. [DOI] [PubMed] [Google Scholar]
- 12.Komotar RJ, Mocco J, Solomon RA. Guidelines for the surgical treatment of unruptured intracranial aneurysms: the first annual J. Lawrence pool memorial research symposium - controversies n the management of cerebral aneurysms. Neurosurgery. 2008;62:183–194. doi: 10.1227/01.NEU.0000311076.64109.2E. [DOI] [PubMed] [Google Scholar]
- 13.Raymond J. Incidental intracranial aneurysms: rationale for treatment. Curr Opin Neurol. 2009;22:96–102. doi: 10.1097/wco.0b013e32831fee91. [DOI] [PubMed] [Google Scholar]
- 14.Ishibashi T, Murayama Y, Urashima M, Saguchi T, Ebara M, Arakawa H, et al. Unruptured intracranial aneurysms: indidence of rupture and risk factors. Stroke. 2009;40:313–316. doi: 10.1161/STROKEAHA.108.521674. [DOI] [PubMed] [Google Scholar]
- 15.Sonobe M, Yamazaki T, Yonekura M, Kikuchi H. Small unruptured intracranial aneurysm verification study: SUAVe study, Japan. Stroke. 2010;41:1969–1977. doi: 10.1161/STROKEAHA.110.585059. [DOI] [PubMed] [Google Scholar]
- 16.Naggara ON, White PM, Guilbert F, Roy D, Weill A, Raymond J. Endovascular treatment of intracranial unruptured aneusysms: systematic review and meta-analysis of the literature on safety and efficacy. Radiology. 2010;256:887–897. doi: 10.1148/radiol.10091982. [DOI] [PubMed] [Google Scholar]
- 17.Raymond J, Molyneux AJ, Fox AJ, Johnston SC, Collet JP, Rouleau I TEAM Collaborative Group. The TEAM trial: safety and efficacy of endovascular treatment of unruptured intracranial aneurysms in the prevention of aneurysmal hemorrhages: a randomized comparison with indefinite deferral of treatment in 2002 patients followed for 10 years. Trials. 2008;9:43. doi: 10.1186/1745-6215-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]