Abstract
Sandhigatavata is described under vatavyadhi in all ayurvedic classical texts. Osteoarthritis is the most common articular disorder which begins asymptomatically in the second and third decades and is extremely common by age 70. Here Matra Vasti (therapeutic enema) was given with Bala taila as Vasti is the best treatment for vatavyadhies. It has vatashamaka and rasayana properties. Indigenous compound drug containing Guggulu, Shallaki, Yastimadhu, Pippali, Guduchi, Nirgundi, Kupilu and Godanti was given in one group along with Matra Vasti. In this study, 33 patients of Sandhigatavata completed the treatment. Patients were randomly divided into two groups. Sixteen patients in Group-A (sarvanga Abhyanga-swedana + matravasti) and 17 patients in Group-B (sarvanga Abhyanga–swedana+ matravasti + indigenous compound drug). The results of the study indicate that the patients of both the groups obtained highly significant relief in almost all the signs and symptoms of Sandhigatavata.
Keywords: Abhyanga, indigenous compound drug, Matra Vasti, osteoarthritis, Sandhigatavata, swedana, vatavyadhi, therapeutic enema.
Introduction
Acharya Charaka has described the disease first separately by the name of ‘Sandhigata Anila’ under the chapter of Vata vyadhi. He defined it as a disease, with the symptoms of swelling(Shotha), which is palpable as air filled bag (Vata purna driti sparsha) and pain on flexion and extension of the joints (akunchana prasarane Vedana).[1] Acharya Sushruta described pain (shula), swelling (shotha) and diminution of the movements at the joints involved (hanti sandhigatah) as symptoms of Sandhigatavata.[2] Symptoms of Sandhigatavata are vatapurnadrutishopha, and akunchana prasarana janya Vedana described by Acharya Vagbhatta.[3]
In this way, the disease Sandhigatavata can be defined as a disease of sandhi (joint) with symptoms of sandhishula(joint pain), sandhishotha(swelling in joints) and akunchana prasarana pravritti savedana(pain during movements like flexion and extension of joints) and in the later stage hanti sandhigatah(restricted movements of joints). In Allopathic science, the similar condition of joint is explained as osteoarthritis. According to WHO, osteoarthritis is the second commonest musculoskeletal problem in the world population(30%) after backpain(50%).[4] Osteoarthritis is the most common joint condition.[5] It is a degenerative type of arthritis which mainly occurs in old age. It is a chronic degenerative disorder of multifactorial etiology characterized by loss of articular cartilage and periarticular bone remodeling.
In Allopathy science, mainly analgesics, anti inflammatory drugs or surgery are the options for the treatment of osteoarthritis. These do not give satisfactory relief and also cause great adverse effect. Researchers are looking for drugs that would prevent, slow down or reverse joint damage.
The present study is a humble effort in search of cure of the disease Sandhigatavata. Acharya Charaka has mentioned repeated use of snehana, svedana, Vasti and mrudu virechana for the treatment of Vatavyadhi.[6] He has not mentioned the treatment of Sandhigatavata separately. Acharya Sushruta has described specific treatment for the Sandhigatavata first time i.e. snehana, upanaha, agnikarma, bandhana and unmardana.[7]
Vasti was selected for the present study as it is shown best for the vatavyadhies. Here Matra Vasti was given with balataila. It has vatashamaka and rasayana properties. It is widely used in many hospitals, still no research work has been carried out with it in Gujarat Ayurved University. So for the present study, balataila was selected. Indigenous compound drug containing Guggulu, Shallaki, Yastimadhu, Pippali, Guduchi, Nirgundi, Kupilu and Godanti was given in one group along with Matra Vasti.
Aims and objectives
To assess the effect of Matra Vasti with Abhyanga- swedana in sandhigata Vata
To assess the effect of indigenous Ayurvedic compound drug in Sandhigatavata.
Materials and Methods
Patients between age group of 40 - 70 years having the below mentioned symptoms were randomly selected from O.P.D. and I.P.D. of Kayachikitsa department, I.P.G.T. and R.A., G.A.U., Jamnagar:
Sandhishula (pain in joints)
Sandhishotha (swelling in joints)
Sandhigraha (Stambha)(stiffness in joints)
Akunchana Prasaranayoh Vedana(pain during flexion and extension of joints)
Sparsha Asahyata (tenderness)
Sandhisphutana (Crepitus)
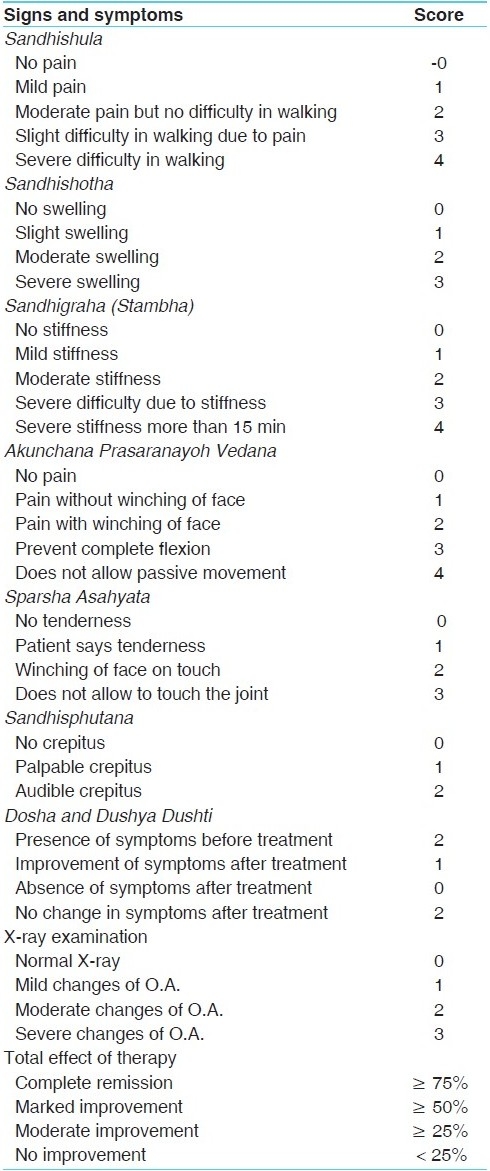
Patients having the signs and symptoms of Sandhigatavata as described in Ayurvedic texts were selected for the clinical trial. To assess the effect of the therapy objectively, a special scoring was given to all the signs and symptoms of the disease Sandhigatavata.
Routine hematological, urine, stool examination, biochemical investigations like fasting blood sugar, lipid profile, serum protein, serum calcium were carried out in all the patients before and after the treatment to evaluate the status of the patient, to exclude any other pathology as well as to see the effect of therapy in these investigations, if any. X-ray examination, joint examination and walking time examination were done in all the patients before and after the treatment to assess the effect of therapy.
Criteria for assessment
To assess the effect of therapy objectively, all the signs and symptoms were given scoring depending upon their severity [Table 1].
Table 1.
Signs and symptoms scoring depending upon their severity
Statistical analysis
To analyze the effect of therapy statistically, mean, percentage, S.D., S.E., t and P values were calculated by using paired ‘t’ test.
Method of administration of Matra Vasti
Patients were asked to take light meal i.e- neither too Snigdha nor too Ruksha and not more than three fourth of the usual quantity. Before administration of Vasti, Abhyanga with Balataila was done to the whole body. Thereafter, Bashpa Swedana was done.
After these Purvakarma, the patient was advised to take left lateral position with left lower extremity straight and right lower extremity flexed on knee and hip joint. The patient was asked to keep his left hand below the head. Balataila was applied to anus in small amount. Sixty milliliters of luke warm Balataila was taken in enema syringe. Rubber catheter oleated with Balataila was attached to enema syringe. After removing the air from enema syringe, rubber catheter was administered into the anus of the patient upto the length of 4-5 inches. The patient was asked to take deep breath while introducing the catheter and drug. The total taila was not administered in order to avoid entrance of vayu into the Pakvashaya which may produce pain.
After the administration of Vasti, patient was advised to lie in supine position and patient's buttocks were gently tapped and legs were raised few times so as to raise the waist. After a while patient was advised to get up from the table and take rest.
Abhyanga -Svedana
Sarvang Abhyanga was done approximately for 30 min with Balataila. After Abhyanga, patient was subjected to Bashpa swedana for approximately 10 min. For this, Dashamula decoction was used.
Indigenous compound drug
The ingredients of drug were Kupilu churna(1 part), Godanti Bhasma (2 parts), Pippali Churna (4 part), Yashtimadhu churna (4 parts), Shallaki (10 parts), Guggulu (10 parts). Then 3 bhavanas of Guduchi, and Nirgundi Svarasa was given to Yastimadha, Pippali and Kupilu churna.
Totally, 35 patients were selected for the study. Among them 33 patients completed the treatment and 2 patients were drop outs. These patients were randomly divided into two groups as below:-
Group-A - 16 patients of this Group were treated with sarvang Abhyanga - swedana alongwith Matra Vasti (60 ml balataila) for three weeks with three days interval at every week.
Group-B - 17 patients of this Group were treated with sarvang Abhyanga – sVedana along with Matra Vasti (60 ml of balataila) for three weeks with three days interval at every week, same as Group-A. Along with this, patients of this Group were also given indigenous compound drug in vati form 1.5 g three times daily for four weeks.
Observations
In the present study, majority of the patients were from the age group of 40-50 years (45.71%). Majority of the patients were females (77.14%), 62.85% patients were housewives, 68.57% patients were belonging to middle class and 88.57% patients were residing in urban area. All the patients were belonging to anoop desha, 77.14% patients were vegetarians, and 91.42% patients were having habit of samashana.
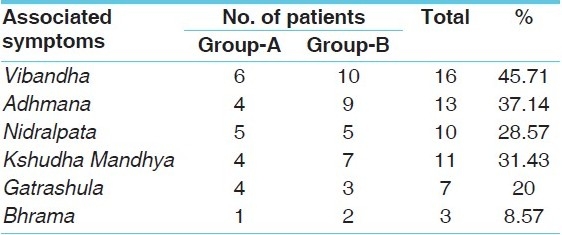
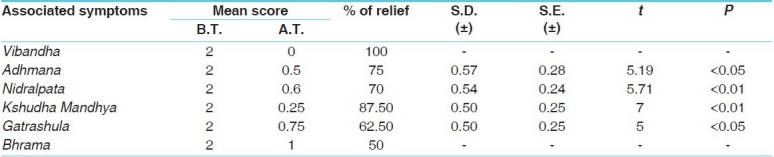
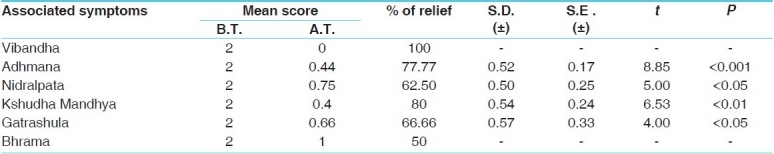
Maximum number of patients had chronicity one-two years (31.42%) followed by two-five years chronicity (25.71%), 65.71% patients were having negative family history, 80% patients were having gradual onset of the disease. In the present study, as Nidana, ati katvadi Rasa Sevana was present in 11.43% patients, ati sheeta Ahara Sevana was present in 2.86% patients, ati Ruksha and ati alpa ahara sevana were present in 2.86% patients [Table 3]. As a risk factor or causative factor [Table 4], 77.14% patients were of female sex; in 14.29% patients, family history was positive. The associated symptoms observed in this study are shown in Table 6.
Table 3.
Nidana wise distribution of 35 patients of Sandhigatavata
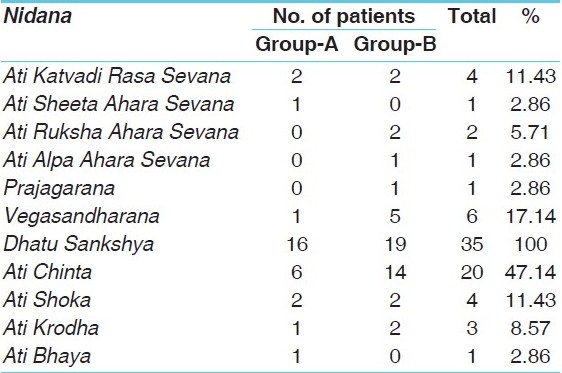
Table 4.
Risk factors wise distribution of 35 patients of Sandhigatavata
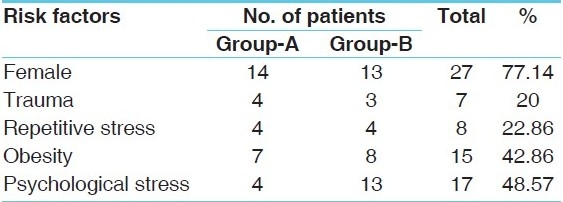
Table 6.
Associated symptoms wise distribution of 35 patients of Sandhigatavata
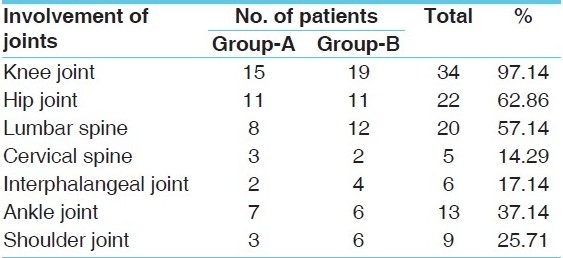
In this study, all the patients (100%) were having sandhi shula and sandhi sphutana. Akunchana prasaranayoh Vedana and stambha were present in 80% patients, sandhi shotha was present in 71.43% patients and sparsha-asahyata was present in 62.86% patients [Table 5]. The involvement of joints in patients is shown in Table 2.
Table 5.
Cardinal symptoms wise distribution of 35 patients of Sandhigatavata
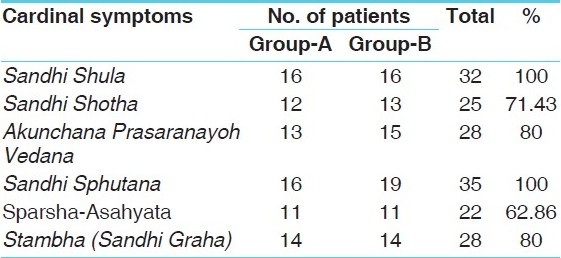
Table 2.
Involvement of joints wise distribution of 35 patients of Sandhigatavata
Basti retention time was observed as minimum of 1 hr., maximum upto 18 hrs with mean of 6 hrs.
Results
Group-A: In this study, 16 patients of Sandhigatavata were treated with Sarvanga Abhyanga – Svedana and Matra Vasti (60 ml Bala taila) for three weeks The effects are shown in Tables 7–10.
Table 7.
Effect of therapy on cardinal symptoms in Group A
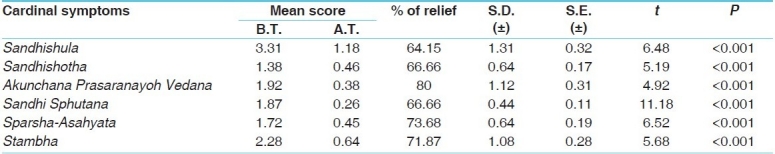
Table 10.
Effect of therapy on joint examination in Group A
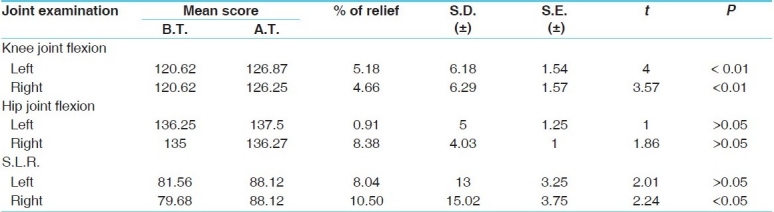
Table 8.
Effect of therapy on associated symptoms in Group A
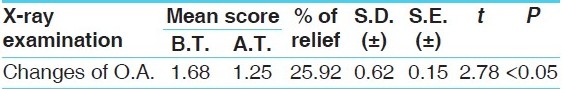
Effect on X-ray Examination: Before treatment, mean score of arthritic changes in X-ray was 1.68, which was reduced to 1.25 after the treatment. The 25.92% relief was noted which was statistically significant (P<0.05) [Table 11].
Table 11.
Effect of therapy on X-ray examination in Group A
Before treatment, joint effusion was present in one patient which was absent after the treatment.
Mean score before and after treatment of all the pathological and biochemical investigations which were done for the present study was almost same. All the values were in its normal range before and after the treatment.
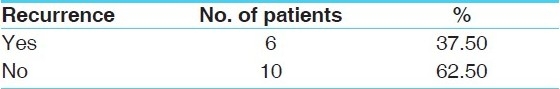
In 62.50% patients (10 patients), no recurrence was noted while 37.50% patients (six patients) got recurrence of symptoms in the follow up period i.e. two months after the completion of the therapy [Table 13].
Table 13.
Recurrence of symptoms (Follow up – two months) in Group A
Group-B: In the present study, in this group, 17 patients were treated with sarvang Abhyanga-swedana and Matra Vasti (60 ml bala taila) for three weeks along with indigenous compound drug was given for four weeks. The effect of therapy in group B is shown in Tables 14–19.
Table 14.
Effect of therapy on cardinal symptoms in Group B
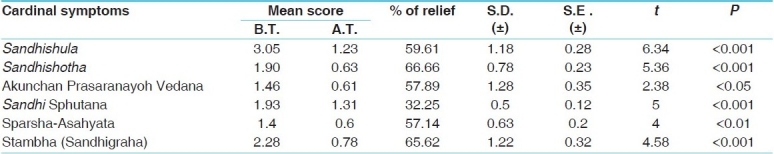
Table 19.
Total effect of therapy in Group B
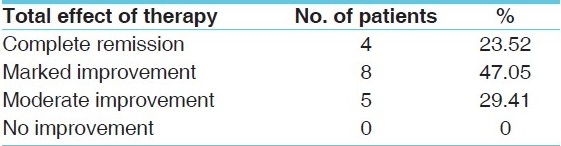
Table 15.
Effect of therapy on associated symptoms in Group B
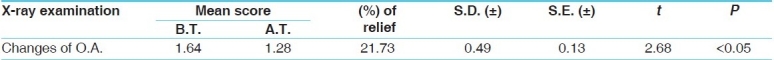
Effect on X-ray Examination: The mean score of arthritic changes in X-ray was 1.64 before treatment, which was reduced to 1.28 after the treatment. Here 21.73% relief was obtained which was statistically significant (P<0.05) [Table 18].
Table 18.
Effect of therapy on X-ray examination in Group B
In this group, in four patients effusion was present in the joint before treatment which was absent after the treatment. Mean score before and after treatment of all the pathological and biochemical investigations which were done in the present study was almost same. All the values of the investigations were in normal range both the time.
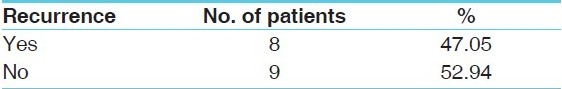
In 52.94% patients (nine patients) no recurrence was noted while 47.05% patients (eight patients) got recurrence of symptoms in the follow up period i.e. two months after the completion of the therapy [Table 20].
Table 20.
Recurrence of symptoms (follow up – two months) in Group B
Discussion
It is interesting to note that dhatukshaya was found in all patients. It can be understood that sandhivata is a geriatric problem. Ati chinta was found in 47.14% patients, atishoka found in 11.43% patients, atikrodha found in 8.57% patients and atibhaya found in 2.86% patients. These manasikanidanas cause agnivaishamya and Vata prakopa, thus leading to the production of Sandhigatavata.
In this series, 77.14% patients were of female sex, 48.57% patients were having psychological stress, and obesity found in 42.86% patients, repetitive stress at the joints found in 22.86% patients, history of trauma was present in 20% patients and hereditary involvement found in 14.29% patients. These factors are mentioned as risk factors for osteoarthritis in the texts and same has been found in the present study. High prevalence of female in osteoarthritis is known. Psychological stress has relation with the severity of the disease. Stress aggravates the pain and other symptoms and may also cause more joint damage. Obesity gives over burden to the joint and causes joint damage. Repetitive stress and trauma directly damages the joint. Heredity plays a role for the production of osteoarthritis especially involvement of interphalangeal joint (heberden's node). Prognosis is good if these risk factors are not present in the patient or if we are able to decrease these risk factors like obesity, repetitive stress etc.
The treatment modality selected for the present study aims at finding out safe, effective and cost free management of Sandhigatavata which can also be applied at OPD level. Vasti is very well known as the best treatment for vatavyadhies. According to acharya charaka, matra vasti is always applicable to those emaciated due to overwork, physical exercise, weight lifting, way faring, journey on vehicles and indulgence in women in debilitated person as well as in those afflicted with Vata disorders. The matra vasti is promotive of strength without any demand of strict regimen of diet, causes easy elimination of mala and mutra. It performs the function of brimhana and cures vatavyadhi.[8]
Indegnious compound drug has properties like Vedanasthapana, shothahara, balya, rasayan, sandhaniya, deepana, anulomana etc. Its pharmacological activities include anti inflammatory, analgesic, anti oxidant, immunostimulant etc. By these properties, this drug is beneficial for the shamana of Sandhigatavata.
Considering the above aspects, the present study was undertaken and the results supported the hypothesis of the study which are as follows-
Comparative effect of therapies on cardinal symptoms
In Group-A and Group-B, highly significant relief (P < 0.001) was found in sandhishula with relief of 64.15% and 59.61% respectively. In Group-A, percentage relief is higher than Group-B where only matra vasti was given [Tables 7 & 14].
In Group-A and Group-B, highly significant relief was found (P < 0.001) in the symptom sandhishotha with the relief of 66.66% in both the groups. So the percentage of relief was same in both the groups.
In Group-A , highly significant relief (P < 0. 001) was found in akunchana prasaranayoh Vedana while in Group-B, the relief was significant (P < 0.05). In Group-A, 80% relief was achieved while in Group-B, percentage relief was 57.89%. Here, in the symptom of akunchana prasaranayoh Vedana, in Group-A higher percentage relief was found than Group-B.
In Group-A and Group-B, highly significant result was found (P < 0.001) in the symptom Sandhi Sphutana in both the groups with percentage relief 66.66% and 32.25%, respectively. Though highly significant result found in both the groups, percentage relief was greater in Group-A.
In Group-A, highly significant relief (P < 0.001) was found in Sparsha Asahyata. Also in Group-B, highly significant relief was found at the level of P < 0.01. Percentage relief of 73.68% and 57.14% was noted respectively. Here also percentage relief was higher in Group-A.
In Group-A and Group-B, highly significant relief (P <0.001) was found in the symptom Stambha with percentage relief 71.87% and 65.62%, respectively. Percentage relief was greater in Group-A.
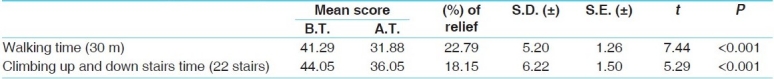
Effect of therapies on walking and climbing stairs time
Highly significant result was found in both Groups. In Group-A, percentage relief in walking time was 20.70% and in climbing stairs time was 16.28% [Table 9]. In Group-B, percentage relief in walking time was 22.79% and in climbing stairs was 18.15% [Table 16]. In walking time and climbing stairs time, slightly greater relief was found in Group-B in comparison to Group-A. This could be due to the indigenous compound drug.
Table 9.
Effect of therapy on walking and climbing stairs time in Group A
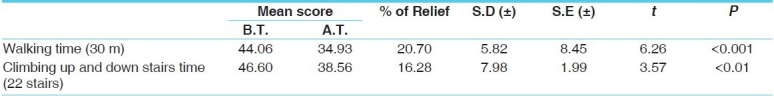
Table 16.
Effect of therapy on walking and climbing stairs time in Group B
Effect of therapies on joint examination
In Group-A, relief in knee joint flexion was highly significant. Relief found in hip joint flexion was insignificant. Relief found in S.L.R. (right leg) was significant while S.L.R. (left leg) was insignificant. Percentage relief obtained was knee joint flexion Lf. (5.18%) Rt. (4.66%), hip joint flexion Lt. (0.91%), Rt. (8.38%), S.L.R. Lt (8.04), Rt(10.5%) [Table 10].
In Group-B, relief in knee joint flexion was highly significant. Improvement in S.L.R. was significant. Improvement in hip joint flexion (right leg) was significant and it was insignificant to left hip joint. Percentage relief found was knee joint flexion Lf. (4.28%). Rt. (6.86%), hip joint flexion Lf. (3.13%), Rt. (4.07%) S.L.R. Lf. (8.57%), Rt. (10.21%) [Table 17].
Table 17.
Effect of therapy on joint examination in Group B
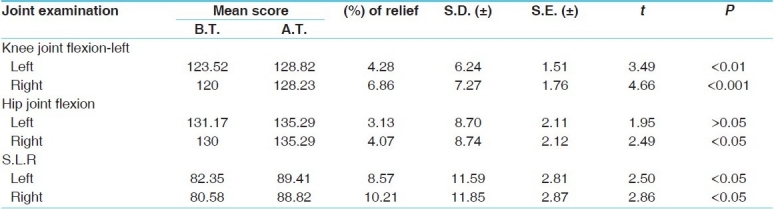
Percentage relief of knee joint flexion left in Group-A was 5.18% and in Group-B was 4.28%. Here better relief was in Group-A. On Rt. knee joint, percentage relief was 4.66% in Group-A and 6.86% in Group-B. Here more relief was in Group-B.
Percentage relief of hip joint flexion left in Group-A was 0.91% and in Group-B was 3.13%. Here higher relief was in Group-B. On right hip joint, percentage relief was 8.38% in Group-A and 4.07% in Group-B. Here more relief was obtained in Group-A.
Percentage relief in S.L.R. left in Group-A was 8.04% and in Group-B was 8.57%. Almost same relief was found in both the Groups. On right side, percentage relief was 10.50% in Group-A and 10.21% in Group-B. Same relief was found in both the groups.
Effect of therapies on X-ray examination
In both the groups, significant relief was found (P < 0.05). Percentage relief in Group-A was 25.92% [Table 11] and in Group-B, it was 21.73% [Table 18]. Slightly greater relief was found in Group-A in comparison to Group-B in X-ray examination.
Effect of therapies on joint effusion (X-ray examination)
In Group-A, in one patient, knee joint effusion was present in X-ray examination before treatment and it was absent after treatment. In Group-B, in four patients, knee joint effusion was present before treatment. Among them, in three patients, it was absent after treatment in X-ray examination. Here, both the groups obtained good result in joint effusion.
Though joint effusion is not a characteristic feature of osteoarthritis, the pathological condition in knee joint associated with oseteoarthirtis can also be treated successfully by this modality.
Probable mode of action
Vasti - Vasti is the best treatment for Vata as said by Acharya Charaka “Vastihi Vataharanam”. Vasti drug first reaches to the Pakvashaya(large intestine). Pakvashaya is the chief site of Vatadosha. Thus, by its action on the chief site, Vasti gets control on Vata all over the body. Pakvashaya is the site of Purishadharakala. Commentator Dalhana has said Purishadhara and Asthidhara kala are one and same.[9] Vasti drugs directly acts on Purishadharakala so we can take its direct action on Asthidharakala also. Sushruta has mentioned 6th Vasti nourishes Mamsa Dhatu, 7th Vasti nourishes Meda Dhatu, 8th Vasti nourishes Asthi Dhatu and 9th Vasti nourishes Majja Dhatu.[10] Thus, through Vasti, we achieve Vata Dosha Shamana and Snehana of Asthi Dhatu. So we achieve the Shamana of Sandhigatavata by breaking the Samprapti. According to modern medical science, as per Vasti /Enema concerned, in trans rectal route, the rectum has a rich blood and lymph supply and drug can cross the rectal mucosa like other lipid membrane. Thus by entering in general circulation, Vasti drugs acts on whole the body.
Vasti may act through the nervous system or through the enteric receptors. It may increase the secretion of local enzyme or neurotransmitters. Vasti influences the normal bacterial flora, thus it increases the endogenous synthesis of vitamin B12, vitamin K etc.
Bala used in matravasti gives “Bala” to the body. It has Vatasansaman and Rasayana properties. So it is very good in Vatavyadhies i.e. degenerative disorders. Its pharmacological activities include rejuvinative, anti inflammatory, analgesic etc. Balataila is good in all types of Vatavyadhi, Raktapitta, Yoniroga, Talushosha,etc.[11]
In osteoarthritis, there is disruption of glue which binds the cells of the cartilage, so cartilage damage takes place. Taila by its qualities like tikshna, suksma penetrate the cartilage and by its Snigdha, Guru qualities provides glue which binds the cartilage cells. This action of taila is considered as “sandhaniya”.
Abhyanga(massage) - Abhyanga directly acts on muscles and makes them strong. The root of Mamsavaha Srotas is Snayu(ligaments), Tvacha(skin) and Raktavahini(blood vessels). So here, Abhyanga is done over Tvacha and Snayu and also it involves Raktavahini. So here, direct benefit is achieved at Mamsavaha Srotas. Abhyanga nourishes deeper Dhatus also. Here, one thing we can say that Abhyanga makes the muscles strong and thus get the stable joint.
Swedana(fomentation): Swedana is Sandhichestakar (improvises the movements of joints), Srotoshuddhikar (clears up the micro channels), Agni Deepaka, Kaphavatanirodhan(antagonist of Kapha). It decreases Sthambha(stiffness). Heat administration by Swedana may produce hypno analgesic effect by diverted stimuli. In Sandhigatavata, Sanga type of Srotodushti is present Swedana, by doing Srotoshuddhi, this Sanga is releaved.
Indigenous compound drug: It has properties like Vedanasthapana (analgesic), shothahara (anti-inflammatory), balya, rasayan, sandhaniya, deepana, anulomana etc. Its pharmacological activities include anti inflammatory, analgesic, anti oxidant, immunostimulant etc. By these properties, this drug is beneficial for the shamana of Sandhigatavata.
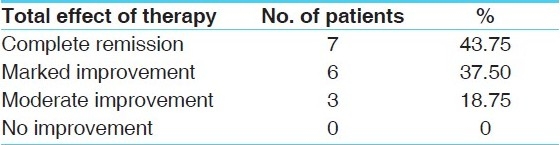
Conclusion
Complete remission was found in 43.75% patients in Group-A [Table 12] and 23.52% patients in Group-B [Table 19]. Marked improvement was found in 37.50% patient in Group-A while 47.05% in Group-B. Moderate improvement was found in 18.75% patients in Group-A and 29.41% patients in Group-B. In Group-A, more number of patients got complete remission in comparison to Group-B. Otherwise, almost equal result is obtained in both the groups.
Table 12.
Total effect of therapy in Group A
With these results, it can be said that sarvang Abhyanga-swedana and Matra Vasti serve all the needs which are required for the shamana of Sandhigatavata. Along with present therapy, addition of sthaulyahara treatment in sthula patients and long duration of therapy may provide better relief. Addition of exercise may help in improving joint function.
References
- 1.Aacharya Y.T, editor. 5th edition. Vol. 28. Varanasi: Chaukhamba Sanskrit Sansthan; 1990. Agnivesha, Charaka, Dridhabala, Charaka samhita, Chikitsa Sthana, Vatavyadhi Chikitsa Adhyaya; pp. 72–74. 618. [Google Scholar]
- 2.Shastri Ambikadutta., translator. 9th edition. 28. Vol. 1. New Delhi: Motilal banarasidas publications; 2002. Sushruta, Sushruta Samhita, Nidanashtana, Vatavyadhinidana Adhyaya; p. 230. [Google Scholar]
- 3.Gupta Kaviraj Atridev., editor. 14. Vol. 15. Varanasi: Chaukhambha Orientalia; Vagbhatta, Ashtanga Hridaya, Nidana sthana, Vatavyadhinidana Adhyaya; p. 277. [Google Scholar]
- 4.Das Siddharth Kumar, Malaviya Anand N. Rheumatology, Oseteoarthritis and crystal deposition disease, API textbook of medicine. In: Shah S.N, editor. 7th edition. Published by The Association of Physicians of India; 2003. p. 1151. Malaviya, Rheumatology, Oseteoarthritis and crystal deposition disease, API textbook of medicine,edited by SN Shah, Published by The Association of Physicians of India,7 th edition 2003;1151. [Google Scholar]
- 5.Murray Longmore, Lan B, Wilkinson, Rajagopalan Supraj. 7th edition. oxford university press; 2004. Rheumatology, Osteoarthritis, Oxford Handbook of Clinical medicine; p. 416. [Google Scholar]
- 6.Ibidem Charaka Samhita(1), Vatavyadhi Chikitsa Adhyaya. 28:73–82. 620. [Google Scholar]
- 7.Ibidem, Sushruta Samhita (2), Vatavyadhichikitsa Adhaya. 4(8):26. [Google Scholar]
- 8.Ibidem, Charaka Samhita (1), snehavyapatsiddhi Adhaya. 4:52–54. 701. [Google Scholar]
- 9.Kasutre Vd.H.S. 6th edition. Baidynath Ayurveda Bhavan; Ayurved Panchkarmavijnana. 471. [Google Scholar]
- 10.Ibidem, Sushruta Samhita(2), Anuvasanauttarbastichikitsa Adhyaya. 37:1–76. 164. [Google Scholar]
- 11.Pandey Ganga Sahaya., editor. Vol. 2. Taila Adhikar: Chaukhambha Sanskrit Bhavan; Sodhal, Gadanigraha; pp. 6–10. 74-75. [Google Scholar]


