Abstract
Objective To describe one year outcomes for a national cohort of infants with gastroschisis.
Design Population based cohort study of all liveborn infants with gastroschisis born in the United Kingdom and Ireland from October 2006 to March 2008.
Setting All 28 paediatric surgical centres in the UK and Ireland.
Participants 301 infants (77%) from an original cohort of 393.
Main outcome measures Duration of parenteral nutrition and stay in hospital; time to establish full enteral feeding; rates of intestinal failure, liver disease associated with intestinal failure, unplanned reoperation; case fatality.
Results Compared with infants with simple gastroschisis (intact, uncompromised, continuous bowel), those with complex gastroschisis (bowel perforation, necrosis, or atresia) took longer to reach full enteral feeding (median difference 21 days, 95% confidence interval 9 to 39 days); required a longer duration of parenteral nutrition (median difference 25 days, 9 to 46 days) and a longer stay in hospital (median difference 57 days, 29 to 95 days); were more likely to develop intestinal failure (81% (25 infants) v 41% (102); relative risk 1.96, 1.56 to 2.46) and liver disease associated with intestinal failure (23% (7) v 4% (11); 5.13, 2.15 to 12.3); and were more likely to require unplanned reoperation (42% (13) v 10% (24); 4.39, 2.50 to 7.70). Compared with infants managed with primary fascial closure, those managed with preformed silos took longer to reach full enteral feeding (median difference 5 days, 1 to 9) and had an increased risk of intestinal failure (52% (50) v 32% (38); 1.61, 1.17 to 2.24). Event rates for the other outcomes were low, and there were no other significant differences between these management groups. Twelve infants died (4%).
Conclusions This nationally representative study provides a benchmark against which individual centres can measure outcome and performance. Stratifying neonates with gastroschisis into simple and complex groups reliably predicts outcome at one year. There is sufficient clinical equipoise concerning the initial management strategy to embark on a multicentre randomised controlled trial comparing primary fascial closure with preformed silos in infants suitable at presentation for either treatment to determine the optimal initial management strategy and define algorithms of care.
Introduction
The birth prevalence of gastroschisis in the United Kingdom1 2 and worldwide3 4 5 has increased steadily over the past few decades, with considerable financial and resource implications for healthcare providers.6 Advances in neonatal intensive care and the development of parenteral nutrition have reduced infant mortality rates for gastroschisis from 60% in the 1960s7 to 3-10% in the mid-1990s,8 9 10 with no clear evidence of a reduction in mortality since then.3 Attempts have been made to stratify neonates with gastroschisis into high and low risk groups to assess outcomes of more individualised approaches to management.11 12 13 14 15 16
Surgical strategies for gastroschisis have evolved but with limited evidence and no consensus on the optimal initial management or an effective clinical pathway. The techniques for reducing the viscera and closing the defect consist of primary or staged and operative or non-operative techniques, based on the requirement or otherwise for a silo and general anaesthetic, respectively. Recognition of the link between visceroabdominal disproportion and intra-abdominal hypertension after operative primary fascial closure led to the development of operative staged approaches in the 1960s, using various synthetic materials to gradually reduce the viscera.17 This led to an era of “individualised” management with operative staged reduction reserved for neonates with severe visceroabdominal disproportion in whom reduction and operative primary fascial closure was deemed unsafe.18 The development of preformed silastic silos in the early 1990s19 has changed the management of gastroschisis to the point where routine placement of the silo at the cotside,20 without the need for a general anaesthetic and surgery on the first day of life, has been adopted by some surgeons as the initial intended strategy.15 20 This approach has been increasingly used in the UK, whereas primary reduction of the viscera at the cotside,16 while done in selected cases, is less widely performed.21 These methods are both individualised approaches with selection criteria in that they are not appropriate with perforated or gangrenous bowel or atresia suitable for immediate anastomosis.22 23
Information regarding operative outcomes for contemporary surgical techniques in gastroschisis, however, is still primarily limited to retrospective case series24 25 26 collected over prolonged periods of time at single referral centres. To date there has been only one other prospective population based observational study of gastroschisis to provide representative outcome data in a cohort of neonates born during the same short time period,27 but this provides only short term follow-up data to death or hospital discharge. We described outcomes at one year for a national cohort of infants with gastroschisis, identified through the British Association of Paediatric Surgeons Congenital Anomalies Surveillance System (BAPS-CASS).
Methods
We identified a national cohort of liveborn infants presenting with gastroschisis from October 2006 to March 2008 through BAPS-CASS.21 Each month we sent a routine reporting card to nominated reporting clinicians in all paediatric surgical units in the UK and Ireland, requesting details of the number of infants born and admitted to their unit that month with gastroschisis. In response to a monthly card return indicating that there had been a case of gastroschisis, we sent clinicians a form requesting further details including diagnosis, surgical management, operative complications, and other outcomes up to first discharge from hospital or six months of age, whichever came sooner. We maximised case ascertainment by using the UK Obstetric Surveillance System (UKOSS) and the British Isles Network of Congenital Anomalies Registers (BINOCAR) as secondary sources of cases.28 29 A second form was sent when each child was aged 1 year requesting further details of outcomes including of enteral feeding, duration of stay in hospital, unplanned reoperations, delayed complications, and mortality. Up to three reminders were sent if the first form was not returned.
Statistical analyses
Outcomes were explored in prespecified subgroups. Specifically, we looked at outcomes in infants with simple gastroschisis (defined as intact continuous bowel that is not compromised or breached at delivery or presentation) compared with those with complex gastroschisis (defined as the presence of one or more of intestinal atresia, perforation or intestinal necrosis at delivery or presentation, or missed atresia).14 Outcomes in infants with simple gastroschisis initially managed with operative primary fascial closure or preformed silo placement were also compared with Fisher’s exact test, χ2 test, and Wilcoxon-Mann-Whitney U test as appropriate for non-parametric data. Groups were classified according to their initial management—that is, first planned management strategy—thus some infants in the operative primary fascial closure group were subsequently managed with a preformed silo and vice versa.21 Median differences for non-normally distributed data were calculated with Hodges-Lehmann estimates of shift parameters. The outcomes of primary interest were duration of parenteral nutrition, time to full enteral feeding, rates of intestinal failure, liver disease associated with intestinal failure, and case fatality. For the purposes of this study we defined intestinal failure as a requirement for more than 28 days of parenteral nutrition,30 and liver disease associated with intestinal failure as liver dysfunction (cholestasis in association with raised serum alkaline phosphatase and total bilirubin concentrations) in infants receiving parenteral nutrition. We calculated relative risks with 95% confidence intervals, using the ratio of the proportion of each outcome in one group to the proportion in the comparator group. Analyses were performed with SPSS version 15 (SPSS, Chicago, IL) or STATA version 10 (StataCorp, College Station, TX), or R version 2.13.1 (R Project for Statistical Computing).
Results
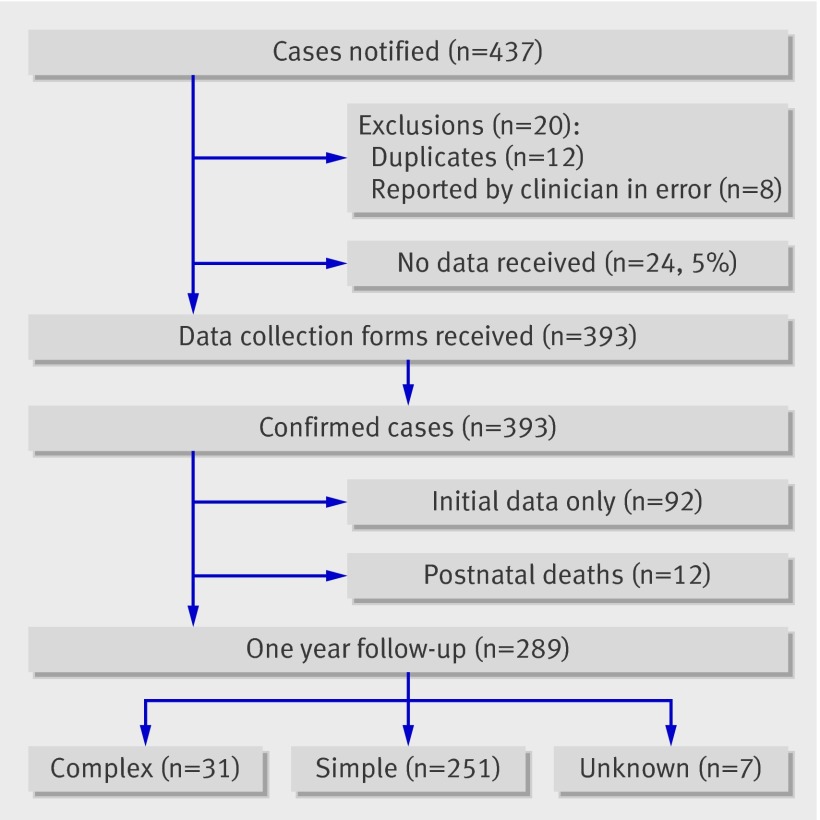
Birth data were received for 393 infants with gastroschisis in a birth cohort of 1.1 million. Information about follow-up at the age of 1 year or death (whichever occurred first) was available for 301 infants (77%) (figure). Table 1 shows the characteristics of infants with follow-up at 1 year compared with infants for whom only initial data were available. A slightly higher (but non-significant) proportion of the infants with follow-up data were initially managed with a preformed silo, and a significantly higher proportion were transferred between hospitals after birth. There were no other significant differences between the groups with and without 1 year follow-up data.
Case reporting and completeness of 1 year follow-up in infants with gastroschisis
Table 1.
Characteristics of infants with gastroschisis according to duration of follow-up. Figures are percentages* (numbers) of infants
| Characteristic | Follow-up to age 1 year (n=301†) | Initial data only (n=92) | P value |
|---|---|---|---|
| Ethnicity: | |||
| White | 91 (264) | 91 (79) | 0.9 |
| Non-white | 9 (25) | 9 (8) | |
| Sex: | |||
| Male | 46 (138) | 42 (39) | 0.5 |
| Female | 54 (162) | 58 (53) | |
| Birth weight (g): | |||
| ≥2500 | 41 (121) | 43 (40) | 0.6 |
| <2500 | 59 (177) | 57 (52) | |
| Gestational age (weeks): | |||
| ≥37 | 53 (159) | 57 (52) | 0.6 |
| <37 | 47 (139) | 43 (40) | |
| Antenatally diagnosed | 99 (294) | 99 (91) | 0.8 |
| Associated anomalies (non-bowel) | 6 (17) | 7 (6) | 0.8 |
| Type of delivery: | |||
| Caesarean before labour | 14 (41) | 13 (12) | 0.4 |
| Caesarean after onset of labour | 27 (80) | 20 (18) | |
| Other | 59 (177) | 67 (61) | |
| Transferred after birth | 40 (119) | 20 (18) | <0.001 |
| Type of gastroschisis: | |||
| Unknown | 2 (7) | 5 (5) | 0.1 |
| Complex | 11 (32) | 15 (14) | |
| Simple | 87 (262) | 79 (73) | |
| Initial surgical management: | |||
| Operative fascial closure | 46 (139) | 59 (54) | 0.1 |
| Preformed silo | 37 (112) | 28 (26) | |
| Other | 17 (50) | 13 (12) | |
| Received parenteral nutrition‡: | |||
| <28 days | 55 (158) | 53 (47) | 0.7 |
| ≥28 days | 44 (127) | 47 (41) | |
*Percentages of those with data.
†Includes 12 infants who died in first year of life.
‡Excludes 6 infants who died in neonatal period.
Outcomes for simple and complex gastroschisis
There were no significant differences in the demographic and clinical characteristics listed in table 1 of infants with simple or complex gastroschisis with follow-up data. Table 2 shows the outcomes for infants with simple and complex gastroschisis. Seven cases had insufficient information to enable classification into complex or simple and have been excluded. Infants with complex gastroschisis took longer to reach full enteral feeding (median difference 21 days, 95% confidence interval 9 to 39 days) and were more likely to develop intestinal failure and liver disease associated with intestinal failure. Infants with complex gastroschisis were also more likely to require unplanned reoperation and a prolonged stay in hospital. The median length of stay was 84 days (interquartile range (IQR) 47-197, range 20-365) for infants with complex gastroschisis and 36 days (IQR 23-57, range 8-365) for those with simple gastroschisis (including four infants (three simple and one complex) still in hospital at the age of 1 year) (median difference 57 days, 29 to 95 days; P<0.001). The median duration of parenteral nutrition was 51 days (IQR 29-92, range 9-297) for infants with complex gastroschisis and 23 days (IQR 16-38, range 2-365) for those with simple gastroschisis (including two infants still receiving parenteral nutrition at 1 year of age) (median difference 25 days, 9 to 46 days; P<0.001).
Table 2.
Outcomes in infants with simple or complex gastroschisis*. Figures are percentages* (numbers) of infants
| Simple (n=251) | Complex (n=31) | Relative risk (95% CI) | P value | |
|---|---|---|---|---|
| Liver disease associated with intestinal failure | 4 (11) | 23 (7) | 5.13 (2.15 to 12.3) | 0.001 |
| Required unplanned reoperation | 10 (24) | 42 (13) | 4.39 (2.50 to 7.70) | <0.001 |
| Unplanned reoperations by indication for surgery†: | ||||
| Ischaemic bowel | 1 (3) | 10 (3) | 8.10 (1.71 to 38.4) | 0.02 |
| Necrotising enterocolitis | 0.4 (1) | 3 (1) | 8.09 (0.52 to 126.2) | 0.2 |
| Adhesional small bowel obstruction | 4 (10) | 13 (4) | 3.23 (1.08 to 9.71) | 0.06 |
| Infective complication | 1 (2) | 0 (0) | 0 (0 to 43.6) | 1.0 |
| Anastomotic stricture | 1 (2) | 10 (3) | 12.1 (2.11 to 69.9) | 0.01 |
| Complications related to stoma | 0 (0) | 3 (1) | ∞ (0.21 to ∞) | 0.1 |
| Silo related | 1 (3) | 0 (0) | 0 (0 to 20.0) | 1.0 |
| Bowel lengthening procedure | 0 (0) | 3 (1) | ∞ (0.21 to ∞) | 0.1 |
| Liver transplantation | 0 (0) | 3 (1) | ∞ (0.21 to ∞) | 0.1 |
| Other unplanned laparotomy | 0.5 (1) | 6 (2) | 16.2 (1.51 to 173.5) | 0.03 |
| Other unplanned operation | 3 (7) | 10 (3) | 3.47 (0.95 to 12.7) | 0.09 |
| Parenteral nutrition >28 days‡ | 41 (102) | 81 (25) | 1.96 (1.56 to 2.46) | <0.001 |
| Days to discharge§: | ||||
| <30 | 37 (91) | 7 (2) | — | <0.001 |
| 31-59 | 35 (85) | 27 (8) | ||
| ≥60 | 28 (68) | 67 (20) | ||
*In seven cases there was insufficient information to enable classification into complex or simple; these cases have been excluded.
†Some infants required more than one unplanned reoperation.
‡Includes two infants who had not attained full enteral feeding at one year. Median time (days) to full enteral feeding (excluding infants who died in neonatal period) was 24 (interquartile range 17-39, range 3->365) in infants with simple gastroschisis and 47 (30-83, range 15-297) in infants with complex gastroschisis (P<0.001).
§Excludes all infants who died.
Outcomes for primary fascial closure and preformed silo in simple gastroschisis
The two most commonly performed initial procedures for simple gastroschisis in the UK are primary operative primary fascial closure and application of a preformed silo with delayed fascial closure.21 There were no significant differences in the demographic and clinical characteristics listed in table 1 of infants with simple gastroschisis managed with these procedures and with follow-up data, with the exception of the proportion transferred after birth. A higher proportion of infants managed with a preformed silo were transferred: 55% (62) compared with 28% (39) managed with operative primary fascial closure. Table 3 shows the outcomes at 1 year for these procedures in neonates with simple gastroschisis. Infants managed with application of a preformed silo took significantly longer to reach full enteral feeding (median difference 5 days, 1 to 9 days), were significantly more likely to develop intestinal failure, and had a tendency to stay longer in hospital. The median duration of parenteral nutrition was 20 days (IQR 14-34, range 2->365) for infants managed initially with operative primary fascial closure and 29 days (IQR 9-41, range 2->365) for those managed with a preformed silo (median difference 5 days, 1 to 9 days; P=0.02) (includes one infant in each group still receiving parenteral nutrition at one year). The median length of stay was 34 days (IQR 23-51, range 12->365) for infants managed initially with operative primary fascial closure (includes two infants still in hospital at 1 year of age) and 38 days (IQR 26-65, range 8->365) for those managed with a preformed silo (includes one infant still in hospital at 1 year of age) (median difference 4 days longer in the preformed silo group, 2 days shorter to 10 days longer; P=0.08). Event rates in the other outcomes were low, and there were no other significant differences in any of the outcomes we examined.
Table 3.
Outcomes in infants with simple gastroschisis according to initial management. Figures are percentages (numbers) of infants
| Operative primary fascial closure group (n=120) | Preformed silo group (n=99) | Risk ratio (95% CI) | P value | |
|---|---|---|---|---|
| Liver disease associated with intestinal failure | 4 (5) | 5 (5) | 1.22 (0.36 to 4.11) | 0.8 |
| Required unplanned re-operation | 12 (14) | 7 (7) | 0.61 (0.25 to 1.44) | 0.4 |
| Unplanned reoperations by indication for surgery*: | ||||
| Ischaemic bowel | 2 (2) | 1 (1) | 0.61 (0.06 to 6.59) | 1.0 |
| Necrotising enterocolitis | 0 (0) | 0 (0) | — | — |
| Adhesional small bowel obstruction | 5 (6) | 3 (3) | 0.61 (0.15 to 2.36) | 0.5 |
| Infective complication | 2 (2) | 0 (0) | — | 0.5 |
| Anastomotic stricture | 0 (0) | 1 (1) | — | 0.5 |
| Complications related to stoma | 0 (0) | 0 (0) | — | — |
| Silo related | 1 (1) | 1 (1) | 1.21 (0.08 to 19.1) | 1.0 |
| Bowel lengthening procedure | 0 (0) | 0 (0) | — | — |
| Liver transplantation | 0 (0) | 0 (0) | — | — |
| Other unplanned laparotomy | 0 (0) | 1 (1) | — | 0.5 |
| Other unplanned operation | 3 (3) | 4 (4) | 1.62 (0.37 to 7.05) | 0.7 |
| Parenteral nutrition >28 days† | 32 (38) | 52 (50) | 1.61 (1.17 to 2.24) | 0.004 |
| Days to discharge‡: | ||||
| <30 | 46 (53) | 28 (27) | — | 0.03 |
| 31-59 | 30 (35) | 40 (38) | ||
| ≥60 | 24 (28) | 32 (31) | ||
*Some infants required more than one unplanned re-operation.
†Excludes six infants who died in neonatal period. Median time (days) to full enteral feeding (including two infants in operative primary fascial closure group and one in preformed silo group who had not attained full enteral feeding at one year) was 22 (interquartile range 15-37, range 3->365) and 28 (20-49, range 7->365), respectively, P=0.02.
‡Excludes all infants who died before age 1 year.
Mortality
There were six deaths in the neonatal period and six in the post-neonatal period. All the neonatal deaths occurred in the simple gastroschisis group, with three infants dying from ischaemic bowel after initial management with a preformed or custom silo. The other neonatal deaths were from causes unrelated to the gastroschisis. Two infants died from necrotising enterocolitis in the second month after birth, two infants died from sepsis, and two died from liver failure before 1 year of age. The overall case fatality was 4% (12/302, 2% to 7%). The case fatality for the complex and simple groups was 3% (0% to 17%) and 4% (2% to 8%), respectively.
Discussion
Principal findings
Infants with complex gastroschisis are significantly more likely to develop intestinal failure and liver disease associated with intestinal failure compared with infants with simple gastroschisis. They also take twice as long to achieve full enteral feeding (47 versus 24 days, respectively). In addition, infants with complex gastroschisis are more likely to require an unplanned reoperation and a prolonged stay in hospital.
The two most commonly performed initial procedures for simple gastroschisis in the UK are either operative primary fascial closure or application of a preformed silo with delayed fascial closure.21 The results of our national observational study suggest that infants with simple gastroschisis managed with a preformed silo take longer to reach full enteral feeding and are more likely to develop intestinal failure. There was no significant difference between the groups in the proportion of infants going on to develop liver disease associated with intestinal failure (operative primary fascial closure 4% versus preformed silo 6%; P=0.5), suggesting that this observed trend did not have a sustained clinically important effect (that is, they had self limiting intestinal failure), although as the numbers involved are small this possibility cannot be excluded completely. Infants in the preformed silo group had a tendency to require longer stays in hospital. There were no other significant differences between the groups. It remains important to note, however, that this is an observational study and not a randomised controlled trial; therefore it is likely that individual characteristics of patients that we have not captured and the preferences of surgeons influenced the choice of initial surgical strategy and its subsequent success, and hence the results should be viewed with appropriate caution. The three neonatal deaths from ischaemic bowel in infants with simple gastroschisis managed initially with a preformed silo provide a clear reminder that silos do not eliminate the risk of torsion of the bowel or inadequate intestinal perfusion, emphasising the importance of appropriate case selection for this type of treatment.
Strengths and weaknesses of the study
This study provides a comprehensive assessment of outcomes at 1 year for a national cohort of infants with gastroschisis. This was achieved through a collaboration of all tertiary paediatric surgical centres in the UK and Ireland, which enabled initial data to be collected on all cases nationally with follow-up at 1 year, providing a representative sample of recently treated infants with outcome data beyond the initial perioperative period. Follow-up to 1 year was undertaken to ensure we identified all “late” mortality, organ transplantation, or ongoing dependency on parenteral nutrition. Additional sources were used to safeguard the completeness of this national cohort.21 We have complete data, however, for only 75% of infants at 1 year of age, and, although the group without follow-up data seems comparable with those we followed up, and therefore systematic bias as a consequence of this incomplete follow-up is unlikely, we cannot exclude the possibility that the study results could differ if we had 1 year data on all infants.
The population based nature of the study means that the data presented are an accurate description of outcomes for current surgical management strategies in the UK. The data are free from the case selection and information biases inherent in retrospective single centre series, which necessitate cases to be collected over prolonged periods to gain adequate numbers and as such are a blunt tool with which to study contemporary management of rare congenital anomalies. In this study, the responsibility for reporting cases and collecting data lay with the surgeons caring for the infants and did not rely on data collected “second hand” from administrative databases, which are not usually population based, are unable to determine the temporal relation between events and hence causality, and are reliant on accurate diagnostic coding, which is often carried out by clerks rather than the clinician responsible for providing care.31 The outcome data in this study are nationally representative and can thus be used as benchmark against which practice and outcomes in single centres can be compared and future innovations in practice or service provision measured. As we have noted above, however, this is an observational study and not a randomised trial, and it is therefore possible that uncontrolled confounding, such as from other factors involved in surgical decision making, could account for some of the differences we observed.
Comparison with other studies
We used the classification proposed by Molik et al to divide cases into “simple” and “complex” groups based on the presence or absence of intestinal atresia, perforation, or necrosis at delivery or presentation.14 This classification has been validated with US national inpatient databases and shown to predict survival and use of resources.32 The only other national prospective population based study examining outcomes in gastroschisis did not apply any form of risk stratification, perhaps because of the lower number of cases enrolled.10 In our data, 87% and 11% of cases were classified as simple and complex, respectively, in keeping with previous studies.11
Our findings support the use of the classification of Molik et al as a simple, immediately available prognostic tool, which reliably identifies two subgroups of patients with divergent outcomes and postnatal courses. It did not, however, predict case fatality, although with such a low event rate and disparate range of causes of death this is perhaps not surprising. Other scoring systems have been successfully applied to patients with gastroschisis to predict outcome. The score for neonatal acute physiology-II (SNAP-II) predicts mortality and other survival variables33 but relies on the collection of several physiological variables. A risk stratification index, developed and validated on two US hospital databases, used logistic regression analysis to identify four coexisting conditions—intestinal atresia, necrotising enterocolitis, lung hypoplasia, and cardiac anomalies—which predict use of resources and mortality.12 Although the authors report a greater ability to discriminate between low and high risk patients using the index, the rarity of lung hypoplasia (0.4%) and cardiac malformations (8.7%) limit the ability of the index to discriminate between outcomes for most cases of gastroschisis, which do not have these associated anomalies. The onset of necrotising enterocolitis, which typically occurs late in an infant’s clinical course, further limits the efficacy of the index as an early predictor of outcome.
The time to full tolerance of enteral feeding is an important outcome measure as it determines the duration of parenteral nutrition and hence the risk of complications, including central line sepsis, hepatic dysfunction associated with parenteral nutrition, and liver transplant.34 The intestinal failure working group of the British Society of Paediatric Gastroenterology, Hepatology and Nutrition and the British Association of Paediatric Surgeons define intestinal failure as a requirement for parenteral nutrition exceeding 28 days.30 A Centers for Disease Control analysis in the United States and a population based study in Canada reported mean parenteral nutrition requirements of 28 and 29 days, respectively.6 10 In our study, 81% and 41% of infants with complex and simple gastroschisis, respectively, had a requirement for parenteral nutrition exceeding 28 days. Over a quarter of infants meeting the criteria for intestinal failure in the complex group progressed to liver disease associated with intestinal failure compared with less than half in the simple group.
To date one multicentre randomised controlled trial compared outcomes for preformed silos and primary operative primary fascial closure either on the ward or under general anaesthesia.35 This study randomised 55 of 195 infants eligible for inclusion at three centres. There was no difference between the groups in any outcome variable examined including duration of ventilation, parenteral nutrition, and stay in hospital or the incidence of sepsis and necrotising enterocolitis. The only other population based study to date found a significant reduction in length of stay and duration of parenteral nutrition in infants managed with “urgent [primary fascial] closure” compared with initial application of a preformed silo, although the surgical strategy and perinatal management were not standardised.27 After multivariate logistic regression, the Canadian Pediatric Surgery Network (CAPSNET) group concluded that the techniques of abdominal wall closure are not associated with functional outcomes in infants with gastroschisis. The key predictor of an adverse outcome was failure to achieve successful fascial closure by whichever method was initially used.10 Current evidence suggests that in the absence of clear clinically relevant benefit with either technique, there is still a need for an adequately powered multicentre randomised controlled trial of application of a preformed silo versus primary operative primary fascial closure.
Conclusions
This study provides a comprehensive picture of current UK practice and outcomes that will inform and enhance the processes of antenatal counselling and postnatal prognosis. The outcome data provide a national benchmark against which individual centres can assess their own performance. The classification of gastroschisis into simple and complex groups, as defined by Molik et al,14 provides a pragmatic readily available method of risk stratification that we have now shown can predict outcome on a population based level. There is, however, a place for future work to define the relative indications for the use of primary fascial closure and preformed silos. A multicentre randomised controlled trial is the next logical step to compare operative primary fascial closure with application of a preformed silo in infants suitable at presentation for either type of treatment to determine the optimal initial management strategy and define algorithms of care.
What is already known on this topic
The worldwide birth prevalence of gastroschisis is increasing, with considerable economic and resource implications for healthcare providers
Gastroschisis has been transformed from a uniformly fatal condition to one with survival rates exceeding 90%, prompting research directed at risk stratification to predict outcome
What this study adds
This population based cohort study of gastroschisis provides representative “benchmark” 1 year outcome data on a national basis
This study validates the classification of gastroschisis into simple and complex subgroups that predict length of stay in hospital, duration of parenteral nutrition, and risk of late complications
The lack of clinically relevant differences in most outcome measures between neonates managed with operative primary fascial closure or application of a preformed silo confirms the position of equipoise required for a national randomised controlled trial
This study would not have been possible without the collaboration of BAPS-CASS reporting clinicians throughout the UK and Ireland: Addenbrooke’s Hospital (Adil Aslam, Christopher Parsons, Marcin Kamierski), Birmingham Children’s Hospital (Anthony Lander, Andrew Robb, Humza Malik), Bristol Royal Hospital For Children (Eleri Cusick, Evelyn Ong), Chelsea and Westminster Healthcare Trust (Nicholas Madden, Clare Skerritt, Anindya Niyogi), Edinburgh Royal Hospital for Sick Children (Gordon MacKinlay, Boma Adikibi), Glasgow Royal Hospital for Sick Children (Atul Sabharwal), Great Ormond Street Hospital for Sick Children (Joe Curry), Hull Royal Infirmary (Sanja Besarovic), John Radcliffe Hospital (Paul Johnson, Javaid Sadiq), King’s College Hospital (Mark Davenport), Leeds General Infirmary (Ian Sugarman, Anthony Owen), Leicester Royal Infirmary (Shawqui Nour), Norfolk and Norwich University Hospital (Thomas Tsang), Nottingham University Hospitals NHS Trust (Brian Davies, Richard Stewart), Our Lady’s Hospital for Sick Children (Prem Puri, Farhan Tareen), Queen Charlotte’s and Chelsea Hospital (Robin Abel), Royal Aberdeen Children’s Hospital (Christopher Driver), Royal Alexandra Children’s Hospital (Anies Mahomed, Rebecca Lisle), Royal Belfast Hospital for Sick Children (William A McCallion, Suzanne Lawther), Royal Liverpool Children’s Hospital (Paul Losty, David Wilkinson), Royal London Hospital (Catherine Cord-Udy, Simon Phelps), Royal Manchester Children’s Hospital (Antonino Morabito, Anju Goyal), Royal Victoria Infirmary (Gareth Hosie), Sheffield Children’s Hospital (Sean Marven, Karen Lloyd), Southampton General (David Burge, Melanie Drewett), St George’s Hospital (Bruce Okoye), University Hospital Lewisham (Catherine Richards), University Hospital of Wales (Simon Huddart, Daniela Vieten, Ram Shrestha).
We also thank Judith Budd, Mary Bythell, Catherine Rounding, Rosie Thompson, Ann Tonks, David Tucker, and Diana Wellesley from the British Isles Network of Congenital Anomalies Registers and clinicians reporting cases to the UK Obstetric Surveillance System (UKOSS), who helped with additional case ascertainment. The support of the British Association of Paediatric Surgeons contributed greatly to the success of the study.
Contributors: TJB carried out the analysis and wrote the first draft of the paper. SM assisted with the design of the study, provided clinical input, and contributed to the analysis and writing the paper. AO assisted with the design of the study. PJ provided clinical input to the study and contributed to the analysis and writing of the paper. JJK assisted with the design of the study and contributed to the analysis and writing of the paper. PS assisted with data coding and conducted validation of the data and some analysis. MK designed the study, coordinated data collection, coded the data, supervised the analysis, and contributed to the writing and editing of the paper. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. MK is guarantor.
Funding: This study was funded by the charity BDF Newlife and the British Association of Paediatric Surgeons. The study funders played no part in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All authors are independent of the funders.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by the London multicentre research ethics committee (reference 05/MRE02/82).
Data sharing: Data sharing is governed by the National Perinatal Epidemiology Unit Data Sharing Policy, which can be obtained from the corresponding author.
Cite this as: BMJ 2011;343:d6749
References
- 1.Keys C, Drewett M, Burge DM. Gastroschisis: the cost of an epidemic. J Pediatr Surg 2008;43:654-7. [DOI] [PubMed] [Google Scholar]
- 2.Kilby MD. The incidence of gastroschisis. BMJ 2006;332:250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvarez SM, Burd RS. Increasing prevalence of gastroschisis repairs in the United States: 1996-2003. J Pediatr Surg 2007;42:943-6. [DOI] [PubMed] [Google Scholar]
- 4.European Surveillance of Congenital Anomalies (EUROCAT). EUROCAT report 8: Surveillance of congenital anomalies 1980-1999. EUROCAT Central Registry, University of Ulster, 2001.
- 5.Laughon M, Meyer R, Bose C, Wall A, Otero E, Heerens A, et al. Rising birth prevalence of gastroschisis. J Perinatol 2003;23:291-3. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects—United States, 2003. MMWR Morb Mortal Wkly Rep 2007;56:25-9. [PubMed] [Google Scholar]
- 7.Knutrud O, Bjordal RI, Ro J, Bo G. Gastroschisis and omphalocele. Prog Pediatr Surg 1979;13:51-61. [PubMed] [Google Scholar]
- 8.Chang DC, Salazar-Osuna JH, Choo SS, Arnold MA, Colombani PM, Abdullah F. Benchmarking the quality of care of infants with low-risk gastroschisis using a novel risk stratification index. Surgery 2010;147:766-71. [DOI] [PubMed] [Google Scholar]
- 9.Nembhard WN, Waller DK, Sever LE, Canfield MA. Patterns of first-year survival among infants with selected congenital anomalies in Texas, 1995-1997. Teratology 2001;64:267-75. [DOI] [PubMed] [Google Scholar]
- 10.Weinsheimer RL, Yanchar NL, Bouchard SB, Kim PK, Laberge JM, Skarsgard ED, et al. Gastroschisis closure—does method really matter? J Pediatr Surg 2008;43:874-8. [DOI] [PubMed] [Google Scholar]
- 11.Arnold MA, Chang DC, Nabaweesi R, Colombani PM, Bathurst MA, Mon KS, et al. Risk stratification of 4344 patients with gastroschisis into simple and complex categories. J Pediatr Surg 2007;42:1520-5. [DOI] [PubMed] [Google Scholar]
- 12.Arnold MA, Chang DC, Nabaweesi R, Colombani PM, Fischer AC, Lau HT, et al. Development and validation of a risk stratification index to predict death in gastroschisis. J Pediatr Surg 2007;42:950-6. [DOI] [PubMed] [Google Scholar]
- 13.Caniano DA, Brokaw B, Ginn-Pease ME. An individualized approach to the management of gastroschisis. J Pediatr Surg 1990;25:297-300. [DOI] [PubMed] [Google Scholar]
- 14.Molik KA, Gingalewski CA, West KW, Rescorla FJ, Scherer LR, Engum SA, et al. Gastroschisis: a plea for risk categorization. J Pediatr Surg 2001;36:51-5. [DOI] [PubMed] [Google Scholar]
- 15.Allotey J, Davenport M, Njere I, Charlesworth P, Greenough A, Ade-Ajayi N, et al. Benefit of preformed silos in the management of gastroschisis. Pediatr Surg Int 2007;23:1065-9. [DOI] [PubMed] [Google Scholar]
- 16.Bianchi A, Dickson AP, Alizai NK. Elective delayed midgut reduction-no anesthesia for gastroschisis: selection and conversion criteria. J Pediatr Surg 2002;37:1334-6. [DOI] [PubMed] [Google Scholar]
- 17.Allen RG, Wrenn EL Jr. Silon as a sac in the treatment of omphalocele and gastroschisis. J Pediatr Surg 1969;4:3-8. [DOI] [PubMed] [Google Scholar]
- 18.Fonkalsrud EW, Smith MD, Shaw KS, Borick JM, Shaw A. Selective management of gastroschisis according to the degree of visceroabdominal disproportion. Ann Surg 1993;218:742-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer JD, Chun K, Moores DC, Andrews HG. Gastroschisis: a simple technique for staged silo closure. J Pediatr Surg 1995;30:1169-71. [DOI] [PubMed] [Google Scholar]
- 20.Owen A, Marven S, Jackson L, Antao B, Roberts J, Walker J, et al. Experience of bedside preformed silo staged reduction and closure for gastroschisis. J Pediatr Surg 2006;41:1830-5. [DOI] [PubMed] [Google Scholar]
- 21.Owen A, Marven S, Johnson P, Kurinczuk J, Spark P, Draper ES, et al. Gastroschisis: a national cohort study to describe contemporary surgical strategies and outcomes. J Pediatr Surg 2010;45:1808-16. [DOI] [PubMed] [Google Scholar]
- 22.Minkes RK, Langer JC, Mazziotti MV, Skinner MA, Foglia RP. Routine insertion of a silastic spring-loaded silo for infants with gastroschisis. J Pediatr Surg 2000;35:843-6. [DOI] [PubMed] [Google Scholar]
- 23.Schlatter M, Norris K, Uitvlugt N, DeCou J, Connors R. Improved outcomes in the treatment of gastroschisis using a preformed silo and delayed repair approach. J Pediatr Surg 2003;38:459-64. [DOI] [PubMed] [Google Scholar]
- 24.Banyard D, Ramones T, Phillips SE, Leys CM, Rauth T, Yang EY. Method to our madness: an 18-year retrospective analysis on gastroschisis closure. J Pediatr Surg 2010;45:579-84. [DOI] [PubMed] [Google Scholar]
- 25.Eggink BH, Richardson CJ, Malloy MH, Angel CA. Outcome of gastroschisis: a 20-year case review of infants with gastroschisis born in Galveston, Texas. J Pediatr Surg 2006;41:1103-8. [DOI] [PubMed] [Google Scholar]
- 26.Jager LC, Heij HA. Factors determining outcome in gastroschisis: clinical experience over 18 years. Pediatr Surg Int 2007;23:731-6. [DOI] [PubMed] [Google Scholar]
- 27.Skarsgard ED, Claydon J, Bouchard S, Kim PC, Lee SK, Laberge JM, et al. Canadian Pediatric Surgical Network: a population-based pediatric surgery network and database for analyzing surgical birth defects. The first 100 cases of gastroschisis. J Pediatr Surg 2008;43:30-4. [DOI] [PubMed] [Google Scholar]
- 28.BINOCAR. British Isles network of congenital anomaly registers. www.binocar.org/.
- 29.Knight M, Kurinczuk JJ, Tuffnell D, Brocklehurst P. The UK Obstetric Surveillance System for rare disorders of pregnancy. BJOG 2005;112:263-5. [DOI] [PubMed] [Google Scholar]
- 30.Intestinal Failure Working Group British Society of Paediatric Gastroenterology Hepatology and Nutrition and the British Association of Paediatric Surgeons. Intestinal failure: recommendations for tertiary management of infants and children 2007. www.bspghan.org.uk/Word%20docs%20and%20PDFs/IFWGreportfinalMar2007.pdf.
- 31.Lao OB, Larison C, Garrison MM, Waldhausen JH, Goldin AB. Outcomes in neonates with gastroschisis in US children’s hospitals. Am J Perinatol 2010;27:97-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdullah F, Arnold MA, Nabaweesi R, Fischer AC, Colombani PM, Anderson KD, et al. Gastroschisis in the United States 1988-2003: analysis and risk categorization of 4344 patients. J Perinatol 2007;27:50-5. [DOI] [PubMed] [Google Scholar]
- 33.Mills JA, Lin Y, Macnab YC, Skarsgard ED. Perinatal predictors of outcome in gastroschisis. J Perinatol 2010;30:809-13. [DOI] [PubMed] [Google Scholar]
- 34.Islam S. Clinical care outcomes in abdominal wall defects. Curr Opin Pediatr 2008;20:305-10. [DOI] [PubMed] [Google Scholar]
- 35.Pastor AC, Phillips JD, Fenton SJ, Meyers RL, Lamm AW, Raval MV, et al. Routine use of a SILASTIC spring-loaded silo for infants with gastroschisis: a multicenter randomized controlled trial. J Pediatr Surg 2008;43:1807-12. [DOI] [PubMed] [Google Scholar]