Abstract
Purpose of the Study: Findings are reported from a study that examined the effects of the Tailored Caregiver Assessment and Referral (TCARE®) protocol, a care management process designed to help family caregivers, on care planning and caregiver outcomes. Design and Methods: A longitudinal, randomized controlled trial was conducted with 97 caregivers enrolled in a demonstration project in Georgia. Data included on care plans pertaining to service recommendations, compliance, and use were reviewed. Caregiver identity discrepancy, objective burden, relationship burden, stress burden, and depressive symptoms were assessed up to 4 times during a 9-month observation period. Chi-square tests, independent samples t tests, random effects regression growth curve analysis, and random intercept regression analysis were conducted. Results: A greater variety of services were recommended to and used by caregivers in the intervention group than in the control group. Caregivers in the intervention group had lower caregiver identity discrepancy, stress burden, and depressive symptoms over time than caregivers in the control group. Implications: Study findings provide initial support for the merits of the TCARE® protocol as a process that can be used to effectively target services to individual caregivers’ needs.
Keywords: Case management, Caregiver stress, Informal caregiving, Caregiver identity discrepancy
Growing recognition of the significant contributions of family caregivers to the long-term care system and the negative consequences that may accrue from caregiving have led to the development of an array of caregiver support services including in-home services, respite programs, assistance with information, counseling, support groups, caregiver education, and supplemental services (Family Caregiver Alliance, 2006; Feinberg, 2002). Although numerous studies of caregiver interventions have been conducted and reviewed over the past decade (e.g., Goy, Freeman, & Kansagara, 2010;Montgomery & Kwak, 2008; Schulz et al., 2002, only a small number of intervention studies (Bass, Clark, Looman, McCarthy, & Eckert, 2003; Gitlin, Reever, Dennis, Mathieu, & Hauck, 2006; Guberman et al., 2003) have examined the effect on caregiver outcomes of a standardized assessment or care planning process designed specifically for caregivers. Consequently, minimal information has been made available to help care managers or other family specialists systematically assess the needs and strengths of caregivers or strategically link caregivers with services. As a result, practitioners tend to offer caregivers the services that are available from the agency for which the practitioner works or the services available in the community about which the practitioner has the most knowledge. Unfortunately, this practice creates the circumstance that many caregiver services go unused or do not fully benefit the caregiver or the care receiver (Montgomery, 2002).
The TCARE® Protocol
The Tailored Caregiver Assessment and Referral (TCARE®) protocol is a manualized care management process designed to help practitioners efficiently triage resources and services available within a community to effectively address caregivers’ needs. The protocol is grounded in the caregiver identity theory, as articulated by Montgomery and Kosloski (2009), and consistent with established norms for effective care management. The protocol incorporates practitioners’ feedback and tools that have been developed after extensive testing on reliability and validity with a large sample of caregivers.
Caregiver Identity Theory
The caregiver identity theory (Montgomery & Kosloski, 2009) builds upon the work of Burke (1991) and his colleagues who considered identity maintenance to be a continuous process in which identity standards are applied to the self in a social role. Identity standards are personal norms that serve as reference points for self-appraisals in a role. Consistency between an individual’s identity standards and an individual’s appraisal of behaviors maintains identity. An inconsistency between identity standards and behaviors challenges identity, resulting in stress and, at times, a transition to a different social role and new identity standard (Burke, 1991).
The caregiver identity theory acknowledges caregiving as a journey that includes a series of transitions that result from changes in the caregiving context and in personal norms that are grounded in familial roles and culture (Gaugler, Kane, Kane, & Newcomer, 2005; Montgomery, Marquis, Schaefer, & Kosloski, 2002). The theory suggests that the caregiving role emerges out of a prior familial role, most often the role of child or spouse. Over time, significant changes in the caregiving context such as declining health and increased dependency of the care receiver lead to changes in caregivers’ behaviors and the manner in which they see their role in relation to the care receiver. That is, their identity within the dyadic relationship changes.
The major tenet of the caregiver identity theory is that identity discrepancy, defined as a disparity between the care activities in which a caregiver is engaging and his or her identity standard, or personal norms, is a major source of caregivers’ stress. This discrepancy can be manifested in at least three distinct areas of burden: objective burden, relationship burden, and stress burden, as well as depression (Savundranayagam & Montgomery, 2010).
TCARE® as a Triaging Mechanism
The TCARE® protocol empowers family caregivers by providing them with critical information to make informed decisions. In this regard, the protocol is similar to caregiver coaching protocols such as that implemented by Bass and colleagues (2003) and the care management protocol designed by Gitlin and colleagues (2006). The TCARE® protocol differs, however, from these approaches in two major aspects. First, the TCARE® protocol does not assume that caregivers always know which services will be helpful and which will not. Indeed, the persistent finding that many caregivers discontinue service use after a short trial period raises serious questions about this assumption (Montgomery, 2002). Second, the TCARE® protocol expands upon the work of Gitlin and colleagues by first focusing on strategies for helping caregivers achieve intervention goals, rather than a specific set of services options. Indeed, the protocol identifies more than 90 different types of resources or services that could benefit caregivers and are consistent with one or more of the four main support strategies of the protocol.
Development of TCARE® Process
A two-pronged approach was used to develop the protocol over a two-year period. A registry of more than 1,000 caregivers was created to serve as a study sample that would complete a series of questionnaires to develop and refine measures included on the 32-item assessment tool. The process and supporting tools were developed iteratively through collaboration with staff from 10 geographically dispersed organizations that serve family caregivers.
Description of TCARE® Protocol
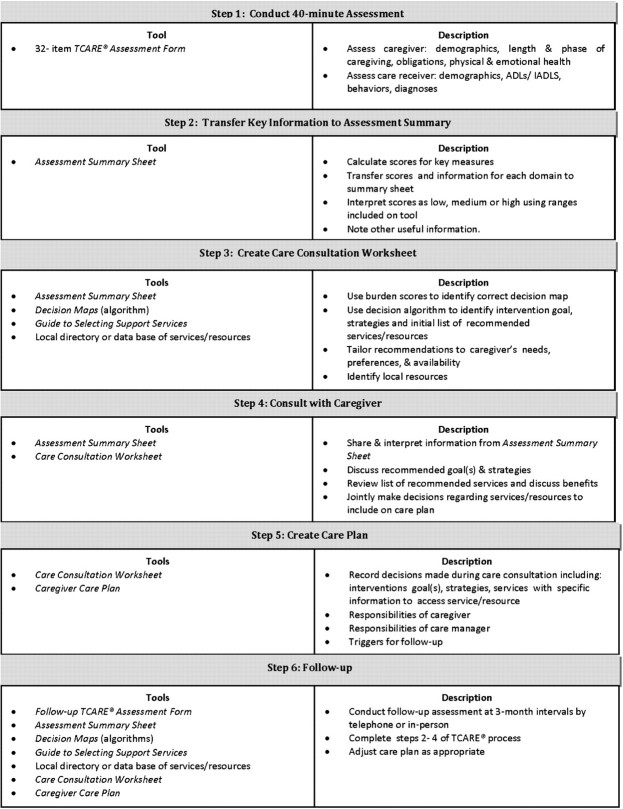
The six-step process, which is briefly described in Figure 1, includes two meetings with caregivers and a structured process for tailoring a care plan to the needs and preferences of the caregiver. A central feature of the TCARE® protocol is a decision algorithm that helps care managers integrate extensive information about the caregiver and care context. The 44 pathways through the decision algorithm reflect various combinations of caregivers’ scores on measures of three types of burden, intentions to place, depression, identity discrepancy, uplifts, and the care manager’s professional judgment regarding the capacity of the caregiver to provide necessary care in a safe manner. The algorithm leads to the identification of (a) an appropriate intervention goal, (b) strategies for reaching that goal, and (c) a generic list of services that is consistent with the identified strategies.
Figure 1.
Six-step TCARE® process.
Reflecting the core assumptions of the caregiver identity theory, one of the three intervention goals is selected to minimize identity discrepancy. The three possible goals for a caregiver are to (a) continue in his or her current identity as a caregiver by “stretching” that identity to include current caregiving activities, (b) reduce the caregiving aspects of his or her identity to bring his or her identity into line with what he or she is actually doing, or (c) further embrace an identity as a caregiver to bring his or her identity into line with what he or she is actually doing. For many caregivers, the algorithm also identifies enhancing the caregiver’s health as a secondary goal. The four possible strategies for achieving the selected goal include (a) changing the caregiver’s personal norms or rules pertaining to care responsibilities and interactions with the care recipient, (b) reducing the work load, (c) enhancing positive self-appraisal, and (d) reducing emotional stress.
The initial list of generic service types is drawn from the TCARE® Guide for Selecting Services which is a catalogue of more than 90 types of resources, grouped into 15 major categories that have been identified as potentially useful for supporting caregivers. The guide links each type of resource with the strategies that it could support.
Starting with the initial list of generic services and using a directory or database of local resources, care managers follow a structured process to tailor the list of services to reflect preferences and circumstances of the caregiver and the availability of resources within the local community. All of this information is recorded on the Care Consultation Worksheet. During a consultation session, the care manager interprets the caregiver’s scores on key measures and uses the worksheet to discuss the recommended goals and strategies and explains the potential benefits of each recommended service. Decisions regarding a care plan are then jointly made with the caregiver and later recorded on the Care Plan Form and sent to the caregiver. An essential aspect of the TCARE® protocol is a scheduled follow-up, which took place at three-month intervals for the duration of this study.
Study Design and Methods
A small, randomized controlled trial was conducted to assess the feasibility and merits of the TCARE® protocol for serving caregivers of persons with cognitive impairment. The study was approved by the University of Wisconsin-Milwaukee Institutional Review Board on September 27, 2007 (IRB # 08.064).
Hypothesized Outcomes
It was hypothesized that the TCARE® protocol would promote caregiver well-being by altering care management practices. Specifically, we expected that compared with usual practice, the protocol would help care managers gain a more complete understanding of the caregiving context, identify the multiple types of stress and burden that a caregiver might incur, and therefore include a wider variety of services on care plans, many of which are less expensive than respite or in-home services that are most often offered to caregivers. We also hypothesized that strategic selection of support services and the consultation process would lead to greater compliance with recommendations and more use of support services by caregivers. Finally, we hypothesized that the TCARE® protocol would lower caregiver identity discrepancy, caregiver burden, and depressive symptoms over time.
Participants
Organizations and Care Managers.—
The three participating area agencies on aging (AAAs) were selected as pilot sites by the State of Georgia Division of Aging Services. A total of 12 care managers from the three AAAs participated in the study. Each agency designated an equal number of care managers to the intervention and control groups. There were no differences in demographic characteristics between the two care manager groups, and both groups had been employed for an average of 14 years or more in social service industry. However, the mean length of employment by the current agency for the intervention group was seven and half years, whereas it was three and half years for the control group. The six care managers selected to use the TCARE® protocol participated in an initial two-day intensive training session, a one-day practicum training, and a web-based application training. Care managers assigned to the control group followed usual and customary practices to assist caregivers.
Caregivers.—
The sample included 97 family caregivers who contacted the three participating AAAs for services. A short standardized screening tool was used to identify caregivers whose score on one or more of the five major outcome areas (caregiver identity discrepancy, objective burden, relationship burden, stress burden, or depression) was above a pre-set cutoff or they indicated that they “probably would” or “definitely would” place their care receivers in a nursing home in the near future. Cutoff scores were established to be equal to 1 SD below the mean based on analysis of data collected from members of the caregiver registry. Eligible caregivers were randomly assigned to the intervention or control group using a computer-generated algorithm.
Data Collection Procedures
Care plans and service use data for caregivers in both groups were obtained by care managers at baseline and at subsequent follow-up assessment points. Other caregiver outcome data were collected at baseline and at three-month intervals for up to three follow-up interviews. Demographic and outcome data for caregivers in the intervention group were taken from the TCARE® assessment form administered by care managers. Telephone interviews were conducted by trained interviewers using the TCARE® assessment form to obtain data from caregivers in the control group. Data collection was discontinued for caregivers if the care receiver died during the study period.
Of 97 caregivers who completed the initial interview, 74 completed the first follow-up interview, 57 completed the second follow-up interview, and 43 completed the third. The most common reasons for attrition during the study period were death of the care receiver (N = 17), not wanting to continue in the study (N = 7), placement of care receiver into a nursing home (N = 4), and discharge from the care management agency (N = 4). There were no significant differences on any of the baseline characteristics between caregivers who remained enrolled in the study and those who dropped from the study.
Fidelity of Implementation.—
To monitor and facilitate accurate implementation of the process, all completed TCARE® forms were reviewed at baseline and the second follow-up by two members of the study team with MSW degrees. Using a 27-item checklist, two scores were created as measures of fidelity. At baseline, the mean score for mechanics, which reflects how accurately information was recorded, was 68% (SD = 18). The mean score for implementation, which indicates how consistent the care plan was with the TCARE® protocol, was 85% (SD = 16.7). The two errors mostly commonly made were failure to complete all questions on the TCARE® Caregiver Assessment Form and incorrect addition of the scores for scales. At six months, the mean scores were 71% (SD = 13.3) for mechanics and 89% (SD = 9.9) for process implementation. Care managers whose average score for completed cases was less than 70% on either dimension of fidelity were offered technical assistance.
Satisfaction of care managers with the protocol was assessed with a 25-item measure that tapped four domains: utility, efficiency, ease of using the protocol, and the utility of matching client services with preferences. All care managers using the TCARE® protocol indicated agreement or strong agreement that protocol was useful, efficient, and easy to use.
Outcome Measures
Service Recommendation, Compliance, and Use.—
The variety of services included on a care plan was measured by counting the number of different types of services listed on the care plan. A dichotomous variable reflecting use (1) or nonuse (0) was created for each of the 22 service types for which data were obtained. Similarly, a dichotomous variable reflecting compliance (1) or noncompliance (0) was created for each service listed on an individual’s care plan.
Identity Discrepancy.—
Caregiver identity discrepancy is defined as the affective psychological state that accrues when there is a disparity between the care activities in which a caregiver is engaging and those activities that would be consistent with his or her identity standard. Identity discrepancy was measured using a 6-point six-item scale with scores ranging 6–36 (α = .80; Savundranayagam & Montgomery, 2010).
Caregiver Burden.—
Caregiver burden was measured using the modified Montgomery Borgatta Caregiver Burden scale (Kosloski, Montgomery, & Youngbauer, 2001; Savundranayagam, Montgomery, & Kosloski, 2010). Objective burden is defined as a negative psychological state that results from the perception that caregiving activities and responsibilities are infringing on other aspects of the caregiver’s life, including time and energy to address other family obligations, leisure activities, and personal needs. It was measured using a 5-point six-item scale with scores ranging 6–30 (α = .86). Relationship burden, measured using a 5-point five-item scale with scores ranging 5–25 (α = .84), is defined as demands for care and attention over and above the level that the caregiver perceives is warranted by the care receiver’s condition. Stress burden is defined as a generalized form of negative affect that results from caregiving and was measured using a 5-point five-item scale with scores ranging 5–25 (α = .87).
Depressive Symptoms.—
Depressive symptoms were measured using a 4-point 10-item short version of the Center for Epidemiological Studies–Depressive Symptoms scale (Andresen, Malmgren, & Cater, 1994). Scores ranged 0–30 (α = .80).
Statistical Analyses
The analyses related to compliance and service use were conducted only for the first three-month period following the initial assessment because new or revised care plans were not created for the majority caregivers (61%) in the control group. Complete data for service recommendations and use were available for 94 caregivers (51 intervention and 43 control) for the first three-month observation period. Independent samples t test and chi-square tests were conducted to examine differences between the groups in the variety of services recommended, compliance and service use. For stress burden and depression as outcomes, we report the results based on the random effects growth curve analysis which estimated the longitudinal trajectories for individual participants at one level, with the intercepts and slopes of these person-specific longitudinal trajectories analyzed as the effects of between-subjects predictors at a higher order second level (Singer & Willett, 2003). For all other outcomes, random intercept regression model analysis was used which estimated the intercept (i.e., mean score) on the basis of the between-subjects predictors at a higher order second level (Singer & Willett, 2003). The final analysis included a total of 243 observations from a nine-month observation period for 97 participants who completed the baseline interview. Predictor variables were group (intervention vs. control), time (measured in months from baseline interview), and a group by time interaction term indicating whether the groups differed from one another with respect to their trajectory of change. Missing data were handled using restricted maximum likelihood estimation as provided by the SAS Proc Mixed procedure (Littell, Milliken, Stroup, & Wolfinger, 1996).
Results
Baseline Characteristics
As shown in Table 1, at baseline, the two groups did not differ significantly with respect to demographic characteristics or scores on outcome variables. The majority of caregivers were female (84.5%), married (64.2%), and caring for a parent (53.6%). The average age for caregivers was 63 (SD = 12.37) years. Fifty-four percent of caregivers were White and 42% were Black or African American. Over 70% of care receivers were diagnosed with probable Alzheimer’s disease. Almost half (49%) of caregivers had provided care for five or more years. Caregivers reported that 47.4% of care receivers could not perform two or more activities of daily living (ADLs) without help and 95.9% could not perform two or more instrumental activities of daily living (IADLs) without help.
Table 1.
Caregiver Characteristics at Baseline (N = 97)a
| All (N = 97) | Intervention (N = 53) | Control (N = 44) | |
| Percentage | |||
| Gender | |||
| Male | 15.5 | 9.4 | 22.7 |
| Female | 84.5 | 90.6 | 77.3 |
| Race | |||
| White | 54.6 | 47.2 | 63.6 |
| Black or African American | 42.3 | 50.9 | 31.8 |
| Otherb | 3.1 | 1.9 | 4.6 |
| Relationship to the care recipient | |||
| Spouse/partner | 35.1 | 35.8 | 34.1 |
| Parent | 53.6 | 50.9 | 56.8 |
| Otherc | 11.3 | 13.2 | 9.1 |
| Self-reported health | |||
| Very poor/poor/fair | 46.8 | 46.1 | 47.7 |
| Good/very good | 53.1 | 53.9 | 52.3 |
| Care receiver needs help with 2 or more ADLs | 92.78 | 98.11 | 86.36 |
| Care receiver needs help with 2 or more IADLs | 100.0 | 100.0 | 100.0 |
| M (SD) | |||
| Age in years | 63.09 (12.4) | 62.81 (13.4) | 63.43 (11.2) |
| Identity discrepancy | 18.90 (7.2) | 18.11 (6.84) | 18.16 (6.86) |
| Objective burden | 24.00 (5.0) | 24.04 (6.39) | 24.48 (5.16) |
| Relationship burden | 10.00 (4.9) | 10.17 (5.17) | 11.88 (5.10) |
| Stress burden | 14.00 (4.9) | 14.47 (5.33) | 14.74 (5.33) |
| Depressive symptoms | 12.00 (6.0) | 13.13 (6.27) | 13.91 (6.29) |
Notes: No statistically significant difference between the two groups was found on any of the characteristics shown in table. ADLs = activities of daily living; IADLs = instrumental activities of daily living.
Four caregivers whose care recipients were institutionalized at a point during the study were included in the analysis because caregivers were still involved in caregiving for their care receivers.
Other race refers to caregivers who did not identify as Caucasian or African American or who identified with two or more races or ethnicities.
Other relationships to the care receiver include friends and other relatives.
Service Recommendation, Compliance, and Use
Of the 22 service types for which data were collected only seven were recommended for more than 10% of caregivers in either group (see Table 2). The analysis was restricted to these services. There were significant differences between the two groups in the number of different types of services that were recommended. The mean number of service types included on care plans was 3.4 (SD = 0.806) for the intervention group and 1.4 (SD = 0.623) for the control group, t(92) = −13.504, p < .001.
Table 2.
Service Recommendation, Compliance, and Use by the Intervention Group (N = 51) and Control Group (N = 43)a
| Service category | Recommended |
Compliedb (used when recommended) |
Usedc |
||||||
| Intervention, N (%) | Control, N (%) | χ2 (1, 94) | Intervention, N (%) | Control, N (%) | χ2 (1, 79) | Intervention, N (%) | Control, N (%) | χ2 (1, 94) | |
| In-home services | 42 (82) | 37 (86) | 0.237 | 37 (88) | 33 (89) | 0 | 43 (84) | 37 (86) | 0.055 |
| Medical or behavioral health evaluation | 38 (75) | 1 (2) | 47.146*** | 10 (26) | 0 (NA) | NA | 11 (22) | 0 (0) | 8.520*** |
| Counseling or sociopsychological education | 27 (53) | 11 (26) | 7.251** | 16 (59) | 4 (36) | 1.089 | 19 (37) | 16 (37) | 0 |
| Support group | 31 (61) | 0 (0) | 36.297* | 10 (32) | 0 (NA) | NA | 17 (33) | 3 (7) | 8.166** |
| Education for caregiver that provides information or skills training | 23 (45) | 1 (2) | 20.255*** | 6 (26) | 1 (10) | NA | 27 (53) | 18 (42) | 1.148 |
| Adult day services | 10 (20) | 4 (09) | 1.226 | 4 (40) | 2 (50) | 0 | 7 (14) | 3 (7) | 0.521 |
| Assistive technologies | 4 (8) | 6 (14) | 0.386 | 1 (25) | 5 (83) | 1.406 | 8 (16) | 6 (14) | 0.055 |
Notes: aComplete data on service recommendations and use were available for 94 caregivers (51 intervention, 43 control) for the first three-month observation period.
Use of a given service when the service was recommended.
Use of a given service regardless of whether service was recommended.
*p < .05. **p < .01. ***p < .001.
The data in Table 2 provide more in-depth information about differences between the two groups in the types of services that were recommended, compliance with recommendations, and use of these services. For both groups, “in-home services” were the type most frequently recommended, and “assistive technologies” and “adult day services” were least frequently recommended. No significant differences were observed between the groups in frequency of recommendations for these services.
In contrast, there were significant differences between the groups in recommendations for the other four service types. Over half of the care plans for caregivers in the intervention group included recommendations for “medical or behavioral health evaluation” (75%), “support group” (61%), and “education for caregivers that provides information or skills training” (45%). Yet, these three service types were included for only one or no caregivers in the control group. Similarly, more than half of the care plans in the intervention group (53%) included a recommendation of “counseling or sociopsychological education,” but this service was included on only 26% of the care plans for caregivers in the control group.
Two findings are of interest regarding the compliance of caregivers with service recommendations. First, there were no significant differences between the two groups in the rates of compliance for any of the services. However, it must be noted that meaningful comparisons could not be made for three of the service types due to the low frequency of recommendations for persons in the control group. Second, there was substantial variation in the compliance rates across the different types of services. The compliance rates ranged from a high 89% for the control group and 88% for the intervention group for in-home services, which is also the most frequently recommended, to a low of 40% for the control and 25% for the intervention group for assistive technologies.
To a large degree, the pattern of service use by the two groups reflects the pattern of recommendations. In-home services, the service type most frequently recommended, was also the service type used by the largest proportion of caregivers in both groups (84% intervention and 86% control). The other services most commonly used by caregivers were counseling or sociopsychological education (37% of both groups) and education for caregivers that provides information or skills training (53% of the intervention and 42% of the intervention group). The relatively low use of adult day services and assistive technologies among caregivers by both groups is consistent with the small number of persons for whom these services were recommended. Significant differences between the groups in the rate of use were found for only two types of services—medical or behavioral health evaluation and support group. Compared with the control group, a greater proportion of caregivers in the intervention group used both types of services.
Effects of TCARE® Protocol on Caregiver Outcomes
Significant group by time interaction effects were observed for caregiver identity discrepancy, stress burden, and depressive symptoms. Results from random intercept regression models for caregiver identity discrepancy, objective burden, and relationship burden are presented in Table 3, and results from random effects regression growth curve models for stress burden and depressive symptoms are presented in Table 4. Data indicated significant differences between the groups in their trajectory in key outcomes. Over time, scores on caregiver identity discrepancy, stress burden, and depressive symptoms for caregivers in the intervention group decreased, whereas scores for caregivers in the control group increased. However, there was no significant group by time interaction effects for objective burden or relationship burden.
Table 3.
Random Intercept Regression Models of Caregiver Identity Discrepancy, Objective Burden, and Relationship Burden
| Caregiver identity discrepancy |
Objective burden |
Relationship burden |
|||||||
| Estimate | SE | p Value | Estimate | SE | p Value | Estimate | SE | p Value | |
| Intercept | 18.47 | 1.02 | <.0001 | 23.97 | 0.79 | <.0001 | 11.55 | 0.75 | <.0001 |
| Group (0 = control, 1 = TCARE®) | −0.34 | 1.38 | .8045 | 0.15 | 1.07 | .891 | −1.29 | 1.06 | .2248 |
| Time | 0.13 | 0.1 | .1821 | −0.05 | 0.07 | .4404 | 0.02 | 0.06 | .7959 |
| Group × Time | −0.3 | 0.14 | .0309 | 0.01 | 0.09 | .8912 | −0.07 | 0.09 | .4407 |
Table 4.
Random Effects Regression Growth Curve Models for Stress Burden and Depressive Symptoms
| Stress burden |
Depressive symptoms |
|||||
| Estimate | SE | p Value | Estimate | SE | p Value | |
| Intercept | 14.75 | 0.79 | <.0001 | 13.86 | 0.95 | <.0001 |
| Group (0 = control, 1 = TCARE®) | −0.19 | −0.90 | .8599 | −0.90 | 1.29 | .4851 |
| Time | 0.06 | 0.08 | .3918 | 0.08 | 0.10 | .428 |
| Group × Time | −0.24 | −0.32 | .0258 | −0.32 | 0.15 | .0286 |
Discussion
Three important findings emerged from this initial evaluation of the TCARE® protocol that affirm the value of the protocol for supporting family caregivers. First, the differences observed in the types of services included on care plans indicate that the protocol fosters the identification and recommendation of a wider range of services that have the potential to address multiple sources and types of caregiver burden. In addition to recommendations for in-home services that were observed for the vast majority of caregivers in both groups, all of the care plans for the intervention group included other services, most of which were intended to address the emotional and/or physical needs of the caregiver.
Second, although the compliance level for all caregivers was less than desired, the patterns of service use suggest that the recommendation of services by care managers is an important factor affecting use of services. This influence is most striking when examining the patterns of recommendation and service use for medical or behavioral health evaluation or support groups. Very few care plans for caregivers in the control group included these services which were virtually unused by these caregivers. In contrast, these services were included on more than half of the care plans of members of the intervention group and, not surprisingly, a much larger proportion of caregivers in the intervention group used the two services. The impact of including a recommendation for a given service on patterns of service use is further underscored by the fact that, apart from caregiver education, few or none of the individuals in the control group used services that were not included on their care plan.
Lastly, we found that the TCARE® protocol was effective in fostering caregiver well-being as indicated by the observed decrease in caregivers’ scores in the intervention group on identity discrepancy, stress burden, and depressive symptoms over the nine-month observation period.
One interesting outcome is the absence of a difference between the two groups in the level of objective burden. This pattern may reflect the fact that the majority of care plans for both groups included recommendations for in-home services, which was used by the majority of caregivers in both groups. In-home services are generally designed to help caregivers attend to tasks related to ADLs or IADLs for care receivers and/or provide a respite from care obligations. Therefore, these services are most apt to address objective burden, which is the caregiver’s perception that care tasks are interfering with other aspects of their lives, and thus, it is not surprising that we did not observe differences between the two groups.
Two findings from this study, however, are not readily interpretable and indicate a need for further studies. The absence of differences between the two groups in relationship burden deserves further inquiry. Also, the comparable rates of use of caregiver education programs by the two groups despite significant differences in recommendations for these services is an intriguing finding that is worthy of further examination.
It is also important to recognize several limitations of this study that should be addressed in future studies. First, the dichotomous measures of service use and compliance did not allow in-depth examination of the frequency and amount of service use and compliance. Second, we were not able to randomly assign care manager due to practical concerns of participating agencies. Lastly, the study was conducted with a relatively small number of caregivers and care managers from three AAAs participating in a demonstration project in Georgia. Future studies should attempt to replicate the study with a larger sample of diverse caregivers and care managers from various organization settings.
Despite these limitations, the findings from this study are encouraging and consistent with the recent calls by advocacy groups for caregiver assessment (Family Caregiver Alliance, 2006). This early evidence indicates that use of the TCARE® tool by care mangers or family specialist can simultaneously promote the well-being of the family caregivers and efficient use of scarce resources by AAAs. We anticipate that the recent translation of the tool into an electronic web-based version that can be directly linked with regional- or state-wide resource databases will substantially reduce the time necessary to implement the protocol. This improvement along with the positive outcomes provides a solid foundation for advocating the use of this protocol not only by AAAs but also by a wide range of service agencies that work with family caregiver. Clearly, there is a need for this type of tool as greater numbers of families assume the role of primary responsibility for caring for a growing population of older adults with chronic illnesses.
Funding
This project was supported in part by grant number 90AI0006/01 from the U.S. Administration on Aging, U.S. Department of Health and Human Services. Grantees undertaking projects under government sponsorship are encouraged to express their findings and conclusions freely. Points of view or opinions do not, therefore, necessarily represent official Administration on Aging policy.
Acknowledgments
J. Kwak, R. J. V. Montgomery, and K. Kosloski participated in the planning of the study. J. Kwak conducted the analyses, interpreted the results, and wrote the article. R. J. V. Montgomery and K. Kosloski interpreted the results and wrote the article. J. Lang participated in data analysis and revising the manuscript. All authors approved the final version of the manuscript. Information on this study was presented at the 2009 annual meeting of the Gerontological Society of America.
References
- Andresen EM, Malmgren JA, Cater WB. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Bass D, Clark P, Looman W, McCarthy C, Eckert S. The Cleveland Alzheimer's managed care demonstration: Outcomes after 12 months of implementation. The Gerontologist. 2003;43:73. doi: 10.1093/geront/43.1.73. doi: 10.1093/geront/43.1.73. [DOI] [PubMed] [Google Scholar]
- Burke PJ. Identity processes and social stress. American Sociological Review. 1991;56:836–849. doi:10.2307/2096259. [Google Scholar]
- Family Caregiver Alliance. Caregiver assessment: Voices and views from the field Report from a national consensus development conference. Vol. II. San Francisco: Author; 2006. [Google Scholar]
- Feinberg LF. The state of the art: Caregiver assessment in practice settings. San Francisco: Family Caregiver Alliance; 2002. [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Newcomer R. Early community-based service utilization and its effects on institutionalization in dementia caregiving. The Gerontologist. 2005;45:177–185. doi: 10.1093/geront/45.2.177. doi: 10.1093/geront/45.2.177. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Reever K, Dennis MP, Mathieu E, Hauck WW. Enhancing quality of life of families who use adult day services: Short- and long-term effects of the adult day services plus program. The Gerontologist. 2006;46:630–639. doi: 10.1093/geront/46.5.630. [DOI] [PubMed] [Google Scholar]
- Goy E, Freeman M, Kansagara D. A systematic evidence review of interventions for nonprofessional caregivers of individuals with dementia. Portland: OR: Evidence-based Synthesis Program (ESP) Center, Portland VA Medical Center.; 2010. Veterans Health Administration-Evidence-based Synthesis Program. [PubMed] [Google Scholar]
- Guberman N, Nicholas E, Nolan M, Rembicki D, Lundh U, Keefe J. Impacts on practitioners of using research-based carer assessment tools: Experiences from the UK, Canada and Sweden, with insights from Australia. Health and Social Care in the Community. 2003;11:345–355. doi: 10.1046/j.1365-2524.2003.00434.x. doi:10.1046/j.1365-2524.2003.00434.x. [DOI] [PubMed] [Google Scholar]
- Kosloski K, Montgomery RJV, Youngbauer JG. Utilization of respite services: A comparison of users, seekers, and nonseekers. Journal of Applied Gerontology. 2001;20:111–132. doi:10.1177/073346480102000107. [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Montgomery RJV. A new look at community-based respite programs. New York. Haworth Press. 2002 [Google Scholar]
- Montgomery RJV, Kosloski K. Caregiving as a process of changing identity: Implications for caregiver support. Generations. 2009;33:47–52. [Google Scholar]
- Montgomery RJV, Kwak J. Tailored Caregiver Assessment and Referral (TCARE®) process: An evidence-based model for effectively supporting caregivers. American Journal of Nursing. 2008;108:54–57. doi: 10.1097/01.NAJ.0000336418.50193.74. [DOI] [PubMed] [Google Scholar]
- Montgomery RJV, Marquis J, Schaefer J, Kosloski KD. Profiles of respite use. In: Montgomery RJV, editor. A new look at community-based respite programs. New York: Haworth Press; 2002. pp. 33–64. [Google Scholar]
- Savundranayagam MY, Montgomery RJV. Impact of role discrepancies on caregiver burden among spouses. 2010;32:175–199. Research on Aging. doi:10.1177/0164027509351473. [Google Scholar]
- Savundranayagam MY, Montgomery RJV, Kosloski K. A dimensional analysis of caregiver burden among spouses and adult children. The Gerontologist. 2010 doi: 10.1093/geront/gnq102. Advance online publication. doi:10.1093/geront/gnq102. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, NY: Oxford University Press; 2003. [Google Scholar]
- Schulz R, O’Brien A, Czaja S, Ory M, Norris R, Martire LM, et al. Dementia caregiver intervention research: In search of clinical significance. The Gerontologist. 2002;42:589–602. doi: 10.1093/geront/42.5.589. doi:10.1093/geront/42.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]