Abstract
Background/Aim:
Microscopic colitis (MC) is diagnosed when a patient with chronic watery non-bloody diarrhea (CWND) has an endoscopically normal colon, but colonic biopsies show unique inflammatory changes characteristic of lymphocytic or collagenous colitis. MC is a disorder of unknown etiology. Studies comparing the prevalence of the disease in developing countries as compared to developed countries may shed more light on the possibility of a post-infectious etiology. Most data on the incidence and prevalence of MC are from developed countries where it accounts for 4-13% of cases of CWND. There are only a few reports from developing countries. Two studies from Peru and Tunis, with high prevalence of infectious gastroenteritis, revealed MC in 40% and 29.3% of cases of CWND, respectively. The aim of this study was to investigate the prevalence of MC in patients presenting with CWND in Egypt.
Materials and Methods:
A total of 44 patients with CWND of unexplained etiology who had undergone full colonoscopy with no macroscopic abnormalities between January 2000 and January 2010 were assessed retrospectively.
Results:
The histological appearance of MC was identified in 22 (50%) patients. Twelve (55%) patients were male and 10 (45%) female. Mean age was 40 years (range: 20-65 years). Twenty (91%) of MC cases had lymphocytic colitis and 2 (9%) had collagenous colitis.
Conclusions:
The prevalence of MC in Egyptian patients with CWND is high when compared to that in developed countries. MC mainly affects young and middle-aged patients and it is more commonly of the lymphocytic type.
Keywords: Chronic diarrhea, colitis, microscopic
Microscopic colitis (MC) is diagnosed when a patient with chronic watery non-bloody diarrhea (CWND) has an endoscopically normal colon but colonic biopsies show the characteristic inflammatory changes of lymphocytic or collagenous colitis.[1] The predominant symptom is diarrhea (96%). About 3-20 bowel movements can occur per day, often accompanied by abdominal cramping and nocturnal bowel movements. Abdominal pain occurs in around 47% of the cases and weight loss in 41% of cases.[2,3]
MC is a disorder of unknown etiology but several hypotheses on its etiology have been postulated: Gastrointestinal infections, autoimmune diseases, bile acid malabsorption, and various drugs.[4,5] Studies comparing the prevalence of the disease in developing countries as compared to developed countries may shed more light on the possibility of a post-infectious etiology.[4] Most of the data on the incidence or prevalence of MC are from developed countries where it accounts for 4-13% of cases of CWND.[6] There are only few reports of MC from developing countries. A study in Peru, with high prevalence of infectious gastroenteritis, revealed MC in 40% of patients with CWND, more commonly of the lymphocytic type.[5] Another study in Tunis revealed MC in 29.3% of patients with CWND.[7] Bolak Eldakror Hospital is a secondary-care governmental hospital in Giza, Egypt. The gastrointestinal endoscopy unit was formally opened in 1999. The present study was undertaken to determine the prevalence of MC among patients presenting with CWND in a single center in Egypt.
MATERIALS AND METHODS
We retrospectively reviewed all patients who had presented with CWND and who had normal macroscopic appearances at colonoscopy between January 2000 and January 2010. Patients who were passing blood and mucus in their stools were excluded. A detailed clinical history was taken. This included information about stool consistency, number of daily defecations, duration of diarrhea, and other gastrointestinal symptoms such as abdominal pain, weight loss, and previous medication. A thorough physical examination and stool examination was performed and total colonoscopy was done with visualization of the terminal ileum. Biopsies were taken from each segment of the colon and from any abnormal appearing areas. They were immediately placed in separate vials with 10% formalin, processed conventionally in paraffin blocks and cut into 5-μ-thick unstained sections. The slides were stained with Hematoxylin and Eosin (H and E) and Masson's Trichrome dyes. Biopsies were examined separately by two pathologists. Diagnostic criteria for the diagnosis of MC included increased chronic inflammatory infiltration in the lamina propria, increased intraepithelial lymphocytes (IELs), degeneration of surface epithelium, and increased mitosis in crypts.[8] Over 20 IELs per 100 intercryptal epithelial cells (normal <1-5/100) were required for diagnosis of lymphocytic colitis. For collagenous colitis, subepithelial collagen band thickness was measured by ocular micrometer in specimens stained with Masson's Trichrome. Specimen thickness over 10 μm was required for the diagnosis.[8]
A total of 452 patients underwent colonoscopy between January 2000 and January 2010. Of these, 59 (13%) patients with chronic (more than 1 month) non-bloody diarrhea of unexplained etiology were assessed for MC. Among these patients, 15 (25%) were excluded because biopsies had not been obtained during the procedure so 44 patients were included in the study.
RESULTS
The study included 44 (10%) patients who had undergone colonoscopy for the indication of CWND with no apparent cause between January 2000 and January 2010. Of the total number of patients, 52% were women and 48% were men (mean age: 41 years, age range: 16-70 years). In all patients, the feces were clearly loose or liquid. Laboratory investigations revealed no ova or cysts of parasitic origin in the stools, and the stool culture also did not yield any pathogens. Thirty-five (80%) colonoscopies were deemed to be normal macroscopically and 9 (20%) revealed mild hyperemia. Terminal ileum was intubated in 31 (71%) patients and it was macroscopically normal. Biopsy diagnosis of MC was made in 22 (50%), normal histology was found in 10 (22%), nonspecific colitis in 10 (22%), and Bilharzial (Schistosomiasis) colitis in 2 (5%) patients.
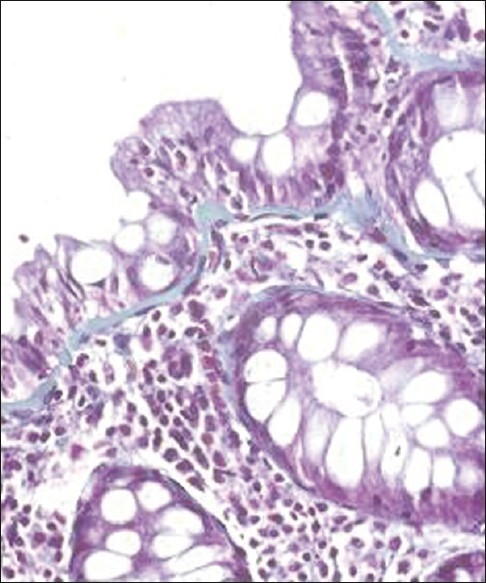
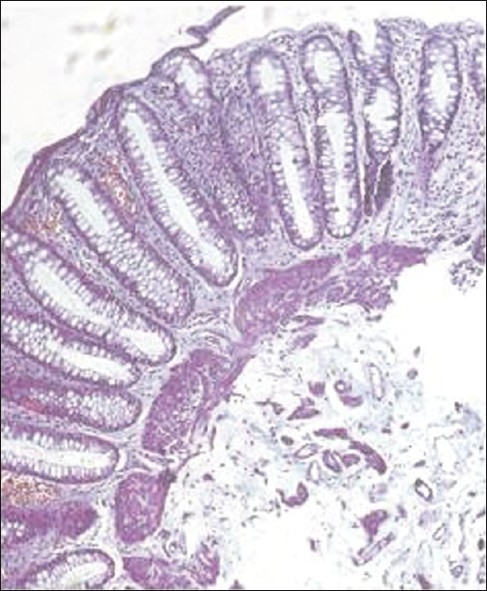
In the 22 (50%) patients diagnosed with MC, 12 (55%) were men and 10 (45%) women. The mean age was 40 years (range: 20-65 years). Fifty percent of the patients were aged less than 40 years. The mean duration of diarrhea was 23 months (range: 2-120 months). Eleven (50%) of these had more than six stools/day. Eighteen (82%) patients had abdominal pain/discomfort and 6 (27%) had weight loss. There was no history of joint pain or swelling, no history of autoimmune diseases, and no history of intake of aspirin, nonsteroidal anti-inflammatory drugs, antibiotics, ranitidine, or proton pump inhibitors. Some patients received 2-3 days course of antimicrobial drugs, including metronidazole, nifuroxazide, tetracycline, or diphenoxylate to treat diarrhea. There was partial response to therapy but without permanent remission. There was no family history of chronic diarrhea. Physical examination did not reveal any abnormality. Twenty (91%) of the MC cases were lymphocytic colitis and 2 (9%) were collagenous colitis. Samples from the cases were digitally photographed through a microscopic camera [Figures 1–4].
Figure 1.
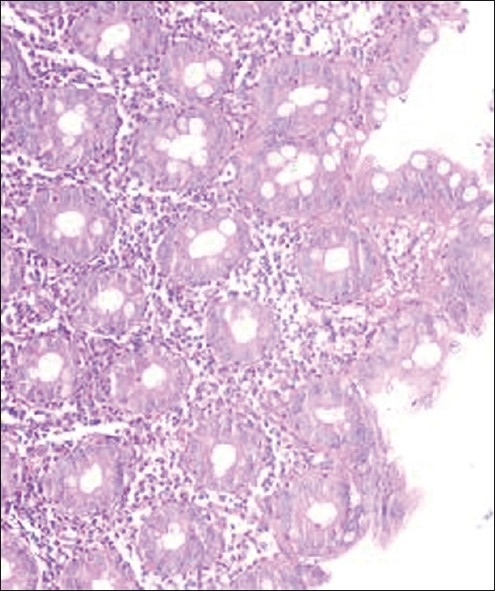
A case of lymphocytic colitis showing marked increase of lymphocytes within the lamina. H and E stain, ×100
Figure 4.
A view of a case of early collagenous colitis showing a superficial mucosal band of deposited collagen; Masson's Trichrome stain ×200
Figure 2.
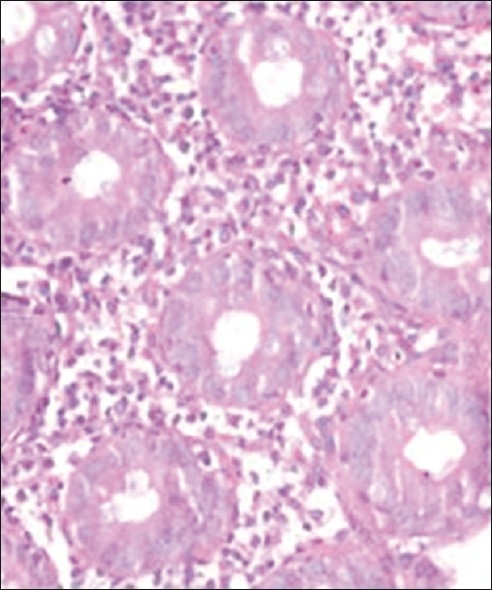
A view of the previous case of lymphocytic colitis showing the lymphocytes invading the crypts; H and E, stain ×200
Figure 3.
A case of lymphocytic colitis showing early superficial collagenous deposition; Masson's Trichrome stain ×100
DISCUSSION
MC is characterized by CWND with normal radiological and endoscopic appearances and is diagnosed by histopathologic examination. The condition that consists of two main subtypes (lymphocytic and collagenous colitis) is a relatively common cause of CWND.[3,6]
MC is a disorder of unknown etiology but several hypotheses on its etiology have been postulated: gastrointestinal infections, autoimmune diseases, bile acid malabsorption, and various drugs.[4,5] The inconclusive nature of the evidence supporting these theories and the variety of clinical settings in which the disease occurs suggest that the syndrome may be the histological endpoint of several different diseases.[4] The association of MC with various autoimmune conditions and markers may support an autoimmune process. Bile acid malabsorption has also been implicated in the pathogenesis of MC. Some drugs have been implicated as possible causes, which include proton pump inhibitors, nonsteroidal anti-inflammatory drugs, histamine-2 receptor blockers, carbamazepine, simvastatin, flutamide, and ticlopidine. There is a possibility that MC may represent the fore end of the spectrum of chronic inflammatory bowel disease (IBD) because there are reports of patients who progressed from MC to IBD.
Another interesting hypothesis is that infectious gastroenteritis may, under certain circumstances, precipitate MC, possibly by an autoimmune reaction.[4] This theory is supported by the finding of acute inflammation on biopsy and a history that suggests acute infection in many patients who are subsequently diagnosed with MC (although no organism has been identified yet). In this regard, the disease is similar to Brainerd diarrhea, which is an acute watery diarrhea associated with mucosal lymphocytosis without crypt distortion, epithelial destruction, or collagen deposition. This condition can last for years and is also thought to be post-infectious. Some patients with MC respond to antimicrobial treatment. Recently, an association has been suggested between infectious gastroenteritis and irritable bowel syndrome with chronic diarrhea; also a striking similarity has been shown between the microscopic lesion observed in this condition and the lesion described in MC.[5]
Studies comparing the prevalence of the disease in developing countries as compared to that in developed countries may shed more light on the possibility of a post-infectious etiology.[4] Studies from different developed countries have reported MC rates of 4%-13% in population cohorts with CWND of unknown origin.[2,3,6,9–11] In this single-center study in Egypt, we found the rate to be 50%, which is similar to the highly prevalence rates reported in other developing countries such as Peru (40%) and Tunis (29.3%).[5,7]
MC (both collagenous colitis and lymphocytic colitis) mainly affects middle-aged and elderly patients.[2] The female to male ratio is reported to be 5:1 in Iceland and 2:1 in Sweden.[9,12] In our study, MC mainly affects younger patients (50% of patients were aged less than 40 years), and there was a male predominance (male:female = 3:2.5).
In a Spanish study, the prevalence of lymphocytic colitis was three times that of collagenous colitis.[11] In another study performed in Turkey, lymphocytic colitis was four times more frequent than collagenous colitis.[8] In our study, lymphocytic colitis is 10 times more frequent than collagenous colitis. The etiology of lymphocytic colitis is not well understood. Gastrointestinal infections, autoimmune diseases, and various drugs have been reported to be causative factors.[8] A study was performed by Helal et al. in 2005 to explore the role of bacteria as a possible etiological factor in lymphocytic colitis in Egypt.[13] Twenty patients with a histopathological diagnosis of lymphocytic colitis were included. Colonoscopic biopsies were divided into two parts. A fresh part was incubated on special cultures for bacterial growth. The other was prepared for histological examination. Culture of tissue biopsies revealed bacterial growth in 18 of 20 (90%) patients with lymphocytic colitis. Escherichia coli was detected in 14 cases. Proteus was found only in one case, Klebsiella in two cases, and Staphylococcus aureus in one case.[13]
Undoubtedly, further studies are needed to elucidate the pathogenesis of MC. However, on the basis of our results and the findings of others in Peru and Tunis, we suggest that this condition is an important cause of chronic diarrhea in developing countries. The relatively high prevalence of infectious gastroenteritis in the developing world suggests infectious etiology to be a possible explanation for this. Further studies are required to assess the role of infectious gastroenteritis in the pathogenesis of MC.
This study was carried in a single center in Egypt to assess the prevalence of MC among patients with CWND. Tests to assess the possibility of associated celiac disease are not available. One of the patients, 65-years old, had the tests done in another hospital and was positive for celiac disease. All patients were treated with Sulfasalazine (Salazopyrin) 4 g/day or 5-aminosalicylic acid (Pentasa) 3 g/day, and most of them responded to therapy. Consequently, they received maintenance therapy with Sulfasalazine 3 g/day or 5-aminosalicylic acid 1.5 g/day. Follow-up data are not available.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Butt SK. How alert are we in detecting microscopic colitis? Gut. 2009;58:A92. [Google Scholar]
- 2.Olesen M, Eriksson S, Bohr J, J.rnerot G, Tysk C. Lymphocytic colitis: A retrospective clinical study of 199 Swedish patients. Gut. 2004;53:536–41. doi: 10.1136/gut.2003.023440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohr J, Tysk C, Eriksson S, Abrahamsson H, J.rnerot G. Collagenous colitis: A retrospective study of clinical presentation and treatment in 163 patients. Gut. 1996;39:846–51. doi: 10.1136/gut.39.6.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Otegbayo JA, Otegbeye FM, Rotimi O. Microscopic colitis syndrome. J Natl Med Assoc. 2005;97:678–82. [PMC free article] [PubMed] [Google Scholar]
- 5.Valle Mansilla JL, León Barúa R, Recavarren Arce S, Berendson Seminario R, Biber Poillevard M. Microscopic colitis in patients with chronic diarrhea. Rev Gastroenterol Peru. 2002;22:275–8. [PubMed] [Google Scholar]
- 6.Pardi DS, Smyrk TC, Tremaine WJ, Sandborn WJ. Microscopic colitis: A review. Am J Gastroenterol. 2002;97:794–802. doi: 10.1111/j.1572-0241.2002.05595.x. [DOI] [PubMed] [Google Scholar]
- 7.Essid M, Kallel S, Ben Brahim E, Chatti S, Azzouz MM. Prevalence of the microscopic colitis to the course of the chronic diarrhea: About 150 cases. Tunis Med. 2005;83:284–7. [PubMed] [Google Scholar]
- 8.Erdem L, Yildirim S, Akbayir N, Yilmaz B, Yenice N, Gultekin OS, et al. Prevalence of microscopic colitis in patients with diarrhea of unknown etiology in Turkey. World J Gastroenterol. 2008;14:4319–23. doi: 10.3748/wjg.14.4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agnarsdottir M, Gunnlaugsson O, Orvar KB, Cariglia N, Birgisson S, Bjornsson S, et al. Collagenous and lymphocytic colitis in Iceland. Dig Dis Sci. 2002;47:1122–8. doi: 10.1023/a:1015058611858. [DOI] [PubMed] [Google Scholar]
- 10.Bohr J, Tysk C, Eriksson S, J.rnerot G. Collagenous colitis in Orebro, Sweden, an epidemiological study 1984-1993. Gut. 1995;37:394–7. doi: 10.1136/gut.37.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez-Banares F, Salas A, Forne M, Esteve M, Espin.s J, Vivek JM. Incidence of collagenous and lymphocytic colitis: A 5-year population-based study. Am J Gastroenterol. 1999;94:418–23. doi: 10.1111/j.1572-0241.1999.00870.x. [DOI] [PubMed] [Google Scholar]
- 12.Thijs WJ, van Baarlen J, Kleibeuker JH, Kolkman JJ. Microscopic colitis: Prevalence and distribution throughout the colon in patients with chronic diarrhoea. Neth J Med. 2005;63:137–40. [PubMed] [Google Scholar]
- 13.Helal TE, Ahmed NS, El Fotoh OA. Lymphocytic colitis: a clue to bacterial etiology. World J Gastroenterol. 2005;11:7266–71. doi: 10.3748/wjg.v11.i46.7266. [DOI] [PMC free article] [PubMed] [Google Scholar]


