Abstract
Objectives
The study objectives were to develop and objectively assess the therapeutic effect of a novel movement-based complementary and alternative medicine approach for children with an autism-spectrum disorder (ASD).
Design
A within-subject analysis comparing pre- to post-treatment scores on two standard measures of childhood behavioral problems was used.
Settings and location
The intervention and data analysis occurred at a tertiary care, medical school teaching hospital.
Subjects
Twenty-four (24) children aged 3–16 years with a diagnosis of an ASD comprised the study group.
Intervention
The efficacy of an 8-week multimodal yoga, dance, and music therapy program based on the relaxation response (RR) was developed and examined.
Outcome measures
The study outcome was measured using The Behavioral Assessment System for Children, Second Edition (BASC-2) and the Aberrant Behavioral Checklist (ABC).
Results
Robust changes were found on the BASC-2, primarily for 5–12-year-old children. Unexpectedly, the post-treatment scores on the Atypicality scale of the BASC-2, which measures some of the core features of autism, changed significantly (p=0.003).
Conclusions
A movement-based, modified RR program, involving yoga and dance, showed efficacy in treating behavioral and some core features of autism, particularly for latency-age children.
Introduction
Nonpharmacological, complementary and alternative medical (CAM) interventions to treat the behavioral symptoms of patients with an autism spectrum disorder (ASD) offer an important alternative to established pharmacologic treatments.1–3 Such treatments appeal to patients both for “push” factors (dissatisfaction with traditional approaches, such as the side-effect burden of medications4) as well as “pull factors” (an increased sense of agency that patients feel with nontraditional approaches).5
As recently reviewed,6,7 there is limited evidence to evaluate such treatments for children with ASD, but insufficient evidence exists to rule out their potential benefit in most cases.6,7 Movement therapies, such as yoga,7–16 have shown some promise for treating behavioral problems, though most of these studies have not examined patients with ASD. On the other hand, several small, preliminary studies have examined music therapy in children with an ASD17–20 with encouraging initial findings. In light of these preliminary reports on the potential benefit of yoga and music therapies,7–20 the authors developed a combined yoga, dance, and music therapy, based on the critical factors that elicit the relaxation response (RR),21 and examined its effect on the behavioral symptoms of children with an ASD. It was hypothesized that such a highly sensory-based approach might have particular benefit to these children, given the well-documented unusual sensory processes in this population.22
Materials and Methods
Subjects
Subjects were enrolled in the study after referral from two sources: (1) children with a diagnosis of an ASD, ages 3–18, referred for treatment to the outpatient practice of the senior author (JBL), and (2) responses to a list serve notifying parents of children with a diagnosis of an ASD of the program's availability. Subjects ranged in age from 3.6 to 16.5 years (mean=8.9±standard deviation [SD] 3.6). There were 22 (92%) males and 2 (8%) females, consistent with population-wide gender distribution for autism.23 The majority of subjects (n=16) were latency age (5–12), 6 were adolescents (13–16), and 2 were preschoolers (both age 3 years).
For the patients referred from the clinical practice of JBL, all treated patients with a diagnosis of autism during the time period of this study (January 2010–June 2010) were offered the opportunity to participate in the group (n=86). Of these, 36 accepted a referral to the study and 23 were enrolled and consented to participate. Of the approximately 200 individuals who received the list-serve solicitation to participate in the study, 24 responded, and 10 of these were enrolled and consented.
Thus, a total of 33 patients were enrolled in the study from the 60 referred. Of the 33 patients enrolled and consented, 24 completed the study (14 from the 23 enrolled from the practice of JBL and all 10 of the 10 enrolled from the list-serve referral source). Subjects included in the group of study completers were those whose parents completed both the pre- and postscreening questionnaires and who attended a minimum of one session.
Subjects who enrolled in the study but who did not reach criteria for completion were those who never attended any sessions (n=2), had behavioral disruptiveness during the group (n=3), had transportation problems (n=2), did not complete the post-test (n=1), or stopped for unknown reasons (n=1). Of the remaining 24 subjects who completed the study, 10 completed all 8 sessions, 1 attended 7 sessions, 1 attended 6 sessions, 1 attended 5 sessions, 1 attended 4 sessions, 1 attended 3 sessions, 2 attended 2 sessions, and 1 subject attended 1 session. Of the remaining 6 subjects for whom the exact number of sessions was not recorded, it was determined that all 6 attended 5 or more sessions. There were no differences in outcome measures based on the number of sessions attended.
In order to optimize applicability of the study results to clinical practice, all subjects referred to the study were accepted, regardless of comorbid medical, cognitive, or psychiatric conditions, and regardless of autism severity (unless such factors prevented their safe participation in the study). Patients with comorbidities reflect the clinical situation because of the strong association of autism with mental retardation and epilepsy.24,25 Of note, for the group of subjects referred from the list-serve, the institutional review board protocol required that they have primary care physician medical clearance to participate.
To determine whether there was a selection bias based on patients who entered compared to those who were referred to the study, the authors examined the BASC-2 pretest scores of the patients who completed the study in comparison with the established norms on the BASC-2 manual for children with autism, and with recently published26 BASC-2 scores of children with autism (see Measures section below for description of the BASC-2). The mean scores of the total sample and of the subjects with whom the authors had the most robust post-treatment changes on the BASC-2 (subjects aged 5–12, see Results section) were very similar to the manual norms for BASC-2 and to the results of the recent study of the BASC-2 among patients with ASD26 (Table 1).
Table 1.
Comparison of Mean Behavioral Assessment System for Children, Second Edition (BASC-2) Clinical Scores in Current Study, BASC-2 Manual Norms for Autism-Spectrum Disorder (ASD) Patients, and Volker26 BASC-2 Study of Patients with ASD
| Composite clinical scores | Current study mean scores—all ages | Current study mean scores latency age children (5–12) | BASC-2 manual mean scores for patients with ASD | Volker study BASC-2 mean scores for patients with ASD |
|---|---|---|---|---|
| Externalization | 59.62 (11.9) | 59.31 (12.5) | 58.8 (9.9) | 58.65 (10.1) |
| Internalization | 56.25 (15.2) | 55.75 (13.1) | 53.7 (12.7) | 58.18 (11.9) |
| Behavioral Symptom Index | 67.87 (11.2) | 68.81 (11.4) | 69.1 (8.3) | 70.44 (9.2) |
| Clinical subscales | ||||
| Hyperactivity | 65.79 (11.3) | 65.06 (12.6) | 65.3 (8.8) | 66.13 (11.6) |
| Aggression | 52.95 (12.3) | 53 (12.1) | 54.6 (10.4) | 55.47 (11.0) |
| Anxiety | 52.79(14.8) | 52.06 (14.6) | 49.5 (13.1) | 56.94 (10.4) |
| Depression | 59.75 (16.9) | 60.50 (17.0) | 57.6 (11.1) | 63.16 (14.0) |
| Somatization | 52.37 (12.1) | 51.38 (10.4) | 52 (10.8) | 49.77 (12.1) |
| Atypicality | 71.95 (15.7) | 74.81 (13.1) | 74.9 (10.6) | 72.61 (13.6) |
| Withdrawal | 68.25 (14.0) | 69.44 (9.7) | 72.9 (11.7) | 73.76 (13.6) |
| Attention problems | 63.04 (6.5) | 63.19 (6.8) | 64.0 (7.4) | 64.50 (7.1) |
| Conduct problems | 54.39 (10.8) | 54.58 (11.8) | 53.58 (12.1) | 51.79 (11.3) |
Procedure
After a complete description of the procedures, written informed consent was obtained from all participants in accordance with the Saint Francis Hospital and Medical Center's Institutional Review Board. Treatment groups consisted of between 2 and 5 children. All subjects were accompanied by a parent or caregiver, who participated in the activities of the group, and assisted their child when necessary. Groups were of mixed age, although the preschool and adolescent children generally were not placed in the same group.
After an initial orientation and pretesting session, there were eight treatment sessions of 45 minutes, and then a final summary and post-testing session (Fig. 1). The sessions were led by the first author (LER), a licensed clinician with added certification in yoga and dance therapy. Each session followed the same format, to create predictability, familiarity, and to reduce anxiety. Specifically sessions involved (in sequence): breathing techniques of RR (10 minutes), yoga postures (10 minutes), music and dance (20 minutes), and typical yoga relaxation (5 minutes).
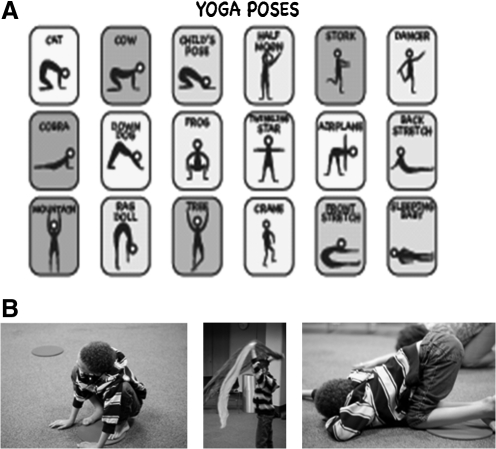
FIG. 1.
A. The diagrams used in program to guide the children in learning the yoga poses. B. One of the study participants engaging in some of the yoga and dance movements.
The program was designed to best engage the unique sensory features of patients with ASD,22 and to incorporate aspects of yoga and music approaches that have shown promise for this population.8–10,17–19 Verbal instructions were complemented by pictures and examples, as shown in Figure 1. Tools such as pinwheels and bubbles were used to help children experience their breath. Competition was de-emphasized and children were given encouragement for whatever they were able to do. By the end of the 8 weeks, most children were able to execute the 18 different postures shown in Figure 1A. Imitation of both the facilitator and each other was encouraged with the goal of enhancing social interaction.
Parents were given a CD of the music from the class as well as guidelines for practicing at home. To view a typical session from the program, please contact the corresponding author.
Measures
BASC–2
This scale (www.pearsonassessments.com/pai/) measures a range of psychiatric functions in children between ages 3 and 21. The authors examined its three clinical composite indices (the Externalizing Scale, Internalizing Scale, and Behavioral Symptom Index or BSI), which comprise nine subscales, which were also examined: (1) Aggression, (2) Anxiety, (3) Attention problems, (4) Atypicality, (5) Conduct problems, (6) Depression, (7) Hyperactivity, (8) Somatization, and (9) Withdrawal subscales. A number of studies have supported the scale's structural and validity properties in children who have disruptive behavior27 and in assessing the unusual thoughts and attention symptoms in children with an ASD,26,28,29 epilepsy,30 and for its use with preschool children.31 The BASC-2 has age-specific child, parent, and teacher self-rating forms. The parent rating scale was used in this study.
The Aberrant Behavioral Checklist (ABC)
The ABC (www.stoeltingco.com/stoelting/2257/1467/1497/Psychological/Aberrant-behavior-Checklist-ABC) is a symptom checklist for assessing problem behaviors of children and adults with mental retardation. It assesses Irritability, lethargy, hyperactivity, stereotypy, and inappropriate speech. Internal structural and validity properties of the test have been well demonstrated in children with developmental delays, including ASD.32–38 Scores on the Irritability scale of the ABC were a priori identified as the scale of interest, as changes on this scale have become the “gold standard” for establishing the efficacy of medications for behavioral symptoms of children with an ASD.32–34
Combined BASC-2 and ABC Irritability scale
Because of (1) the trend toward significance for the ABC Irritability Scale as reviewed in the Results Section below and (2) the importance of this particular scale in the assessment of behavioral changes in autism,36–38 an aggregate score was computed for the ABC Irritability Scale and the BASC-2 Scales that evidenced significant post-treatment changes. This was done by averaging the T-scale value for the combination of the ABC Irritability scale and the scales that significantly changed on the BASC-2 (from Table 2; see Results below). The authors predicted that these aggregate scores would show post-treatment reductions, particularly for the latency-aged children (based on the more robust changes among this age group as discussed in the Results section).
Table 2.
Significant BASC-2 Composite and Subscale Changes by Age Group
| |
All ages |
Latency age |
||||||
|---|---|---|---|---|---|---|---|---|
| BASC-2 scale | Mean pretest | Mean post-test | Mean change | p-Value | Mean pretest | Mean post-test | Mean change | p-Value |
| BSI | 67.87 | 64.70 | −3.17 | 0.04 | 68.81 | 63.43 | −5.38 | 0.013 |
| Externalization | 59.63 | 57.68 | −1.95 | NS | 59.31 | 55.31 | −4.30 | 0.04 |
| Internalization | 56.25 | 53.42 | −2.83 | NS | 55.75 | 50.55 | −5.20 | 0.02 |
| Atypicality | 71.95 | 66.55 | −5.40 | 0.02 | 74.81 | 65.75 | −9.06 | 0.003 |
| Depression | 59.75 | 56.34 | −3.41 | NS | 60.50 | 54.87 | −5.63 | 0.02 |
BASC-2, The Behavioral Assessment System for Children, Second Edition; BSI, Behavioral Symptom Index, NS, not significant.
Data analysis
The results were analyzed using paired t-test comparisons between pre -and post-test scores. A p-value <0.05 was considered significant for all a priori comparisons. To control for spurious findings due to multiple comparisons, a Bonferroni correction was used to examine nonplanned, a posteriori analyses, to maintain an experiment-wise error rate of 0.05.39 Note that nonplanned comparisons were only examined for subscales of a priori planned comparisons that reached statistical significance. These were the subscales of the BASC-2 Externalizing, Internalizing, and the BSI Composite Scales. Thus, values of 0.025, 0.016, and 0.008 were used for examining these three BASC-2 subscales, respectively.
Results
BASC-2
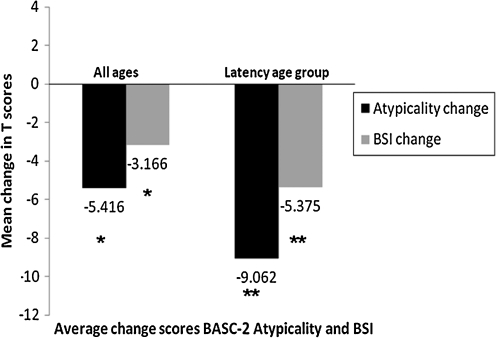
When all subjects were considered, of the three BASC-2 composite clinical scales (BSI, Externalizing, and Internalizing), only the BSI showed improvement (compare row 1 to rows 2 and 3, column 5 in Table 2). Among children in the latency-age group (n=16), all three BASC-2 composite scales were found to be changed (rows 1–3, column 9, Table 2). While the BSI scale changed for all subjects and the latency-aged children, the change was greater for the latency-aged group (compare columns 2 and 4, Fig. 2).
FIG. 2.
Mean changes on the The Behavioral Assessment System for Children, Second Edition (BASC-2) Atypicality Scale and Behavioral Symptom Index by Age Group. The graph shows that while both scales showed significant post-treatment changes (*p<0.05; **p<0.01), the changes were greater for the latency age group (ages 5–12, n=16) and, furthermore, that the Atypicality Scale post-treatment change was greater than the Behavioral Symptom Index (BSI) post-treatment change.
Among the clinical subscales, when all 24 subjects were included, the Atypicality subscale of the BSI composite scale met the established criteria for a posteriori changes comparisons (row 4, column 5, Table 2). Furthermore, as with the overall BSI composite score reported above, this subscale of the BSI evidenced a stronger change among the latency-age children (row 4, column 9, Table 2, and compare columns 1 and 3, Fig. 3). No subscales of the other BASC-2 composite scales reached significance using the Bonferroni correction, for the whole cohort. However, for the latency-aged children, the depression subscale of the internalization composite scale of the BASC-2 changed significantly (row 5, column 9, Table 2).
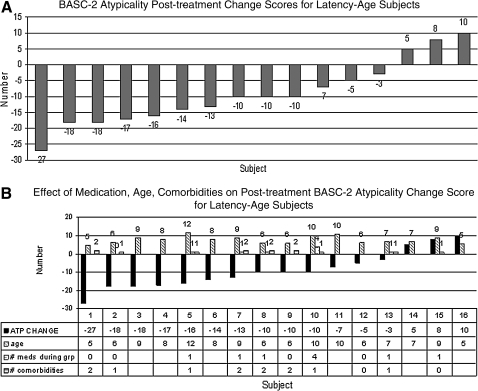
FIG. 3.
Post-treatment change scores by subject on the The Behavioral Assessment System for Children, Second Edition (BASC-2) Atypicality Scale for latency-age subjects (ages 5–12). A. While the overall scores on this scale changed significantly in this age group (Fig. 3, column 3; Table 2, row 4, column 9), there was much variability in these changes when subjects were considered individually. Most subjects showed improvement, but 3 subjects (last three columns) showed worsening (change score standard deviation=10.15). B. The large intrasubject variability in the Atypicality Scale post-treatment change scores (column 1 in graph) did not correspond to differences in age (column 2 in graph and row 2 in table below graph), number of medications (column 3 in graph and row 3 in table below graph), or number of comorbidities (column 4 in graph and row 4 in table below graph). ATP, atypicality. Note: blanks in table below graph refer to missing data, while 0's indicate no medication or comorbidity.
Although the overall post-treatment T-score changes for the BASC-2 BSI and the Atypicality scales were significant, a subject-by-subject change score analysis revealed much intersubject variability. For example, among the latency-aged children, as shown in Fig. 3A, although 13 subjects showed post-treatment improvements, 3 subjects had worse post-treatment scores (the post-treatment T-score SD on the Atypicality Scale for the 13 subjects shown in Fig. 3A was 10.15).
To determine whether age, medication status, medical or psychiatric comorbidity, or number of sessions attended accounted for the variability in post-treatment change scores shown in Figure 3A, these factors were examined for those subjects for whom such data were available. Though these data were somewhat limited (they were not available for the list-serve referred patients), as shown in Figure 3B, there was no apparent relationship between these variables and the subjects' degree of improvement.
Aberrant Behavioral Checklist (ABC)
For the entire cohort, no scales on the ABC changed. For the latency-aged children, there was a trend toward improvement for the Irritability scale of the ABC (p=0.06). Aggregate T-scores of the ABC Irritability scale and the BASC-2 scales, calculated as described in the Methods section, evidenced significant post-treatment changes for the entire cohort for the ABC Irritability plus the BASC-2 Atypicality score (-6 points, p=0.024). Furthermore, as with the BASC-2 scales considered alone, the latency-aged children showed greater post-treatment changes on the combined ABC plus BASC-2 scores, as shown in Table 3.
Table 3.
Significant Combined Aberrant Behavioral Checklist (ABC) Irritability and The Behavioral Assessment System for Children, Second Edition (BASC-2) Scales for Latency-Aged Children
| ABC scale | BASC-2 scale | Mean change | p-Value |
|---|---|---|---|
| Irritability | Atypicality | −10.75 | 0.002 |
| Irritability | BSI | −7.06 | 0.009 |
| Irritability | Depression | −7.31 | 0.01 |
| Irritability | Externalization | −5.93 | 0.023 |
BSI, Behavioral Symptom Index.
Discussion
This study piloted a novel CAM approach that combines RR21 elicitation with yoga, music, and dance, to treat the behavioral symptoms of children with an ASD. In developing the program, the authors hypothesized that inclusion of movement and auditory modalities would allow the program to target the unique sensory features of patients with ASD.22 Furthermore, previous work suggested that yoga8–10 and music17–19 based CAM therapies have particular utility for similar clinical syndromes.
For the entire cohort, only the BASC-2 BSI composite scale evidenced a post-treatment change in the expected direction, while for the latency-aged group subjects (ages 5–12), all three BASC-2 clinical composite scales (the BSI, Externalizing, and Internalizing Scales) evidenced post-treatment changes in the predicted direction. For the exploratory analyses, corrected for multiple comparisons, only the BASC-2 Atypicality Scale change score was significant. As with the a priori comparisons of the composite scales, the latency-aged group evidenced more post-treatment changes among the exploratory analyses. In this age group, both the Atypicality and Depression Scales evidenced significant changes, after correction for multiple comparisons.
The apparent greater impact of our treatment on latency-aged participants suggests that during this developmental period, patients with ASD may have greater receptivity to the program's unique emphasis on movement and sound. In future studies, we hope to examine whether modifying these components of the intervention would render it more accessible to younger and older patients with ASD.
It is of particular interest that the two BASC-2 scores that changed in both the entire cohort and the latency-aged group (the BSI and the Atypicality Scales) were two of the four BASC-2 scales recently identified as having high sensitivity and specificity for screening patients with ASD.26
If future studies support this finding of a particularly strong response on the BASC-2 Atypicality scale to this RR approach, it suggests that this intervention had an unexpected effect on a core symptom of autism, assessed by the BASC-2 Atypicality scale (peculiar, odd, asocial, and inappropriate behaviors, as well as unusual visual perceptions).26 Of note, the change score was 9 T-score points among the latency-aged children on this scale, rendering this both a statistically and clinically meaningful change.
Although changes were not significant for the ABC Irritability Scale, as predicted, a trend was found in the predicted direction for the latency-aged children (p=0.06). Given the small subject size in this age range (n=16), this trend is important to keep in mind in future larger studies, as it may reflect a real change that the current study was underpowered to detect among the latency-aged subjects. Furthermore, as the baseline scores on the ABC Irritability scale were in the normal range, a floor effect may have limited the ability to detect a change on this measure. Specifically, baseline scores on this scale were highly elevated in the studies that showed a change in this scale after treatment with medication.32–34
Additionally, the aggregate scores of the ABC Irritability scale averaged with the BASC-2 scale scores showed highly significant post-treatment changes. In fact, the degree of change for four of the five BASC-2 scales that showed significant post-treatment changes became more significant when averaged with the ABC Irritability Scale (the exception being the BASC-2 Internalization scale). As all analyses were within subjects, this indicates that irritability, as measured by the ABC, changed in a similar direction for most of the scales on the BASC-2 that had post-treatment changes. Thus, the same subjects who evidenced changes in atypicality overall behavior, externalization, and depression on the BASC-2 also had changes in irritability on the ABC, suggesting an intrasubject congruence on changes in these two different measures. Namely, the subjects who had reduced BASC-2 scores after treatment also had reductions in irritability on the ABC scale (with the exception being the BASC-2 Internalization Scale, which, when combined with the ABC Irritability scale, was not significantly changed).
The analysis of the intersubject variability showed a large variability in treatment responses (Fig. 3). Future studies should therefore be designed to identify whether specific treatment factors account for such individual differences in the response to this treatment approach. Such research should seek to determine whether patients with ASD who have particular characteristics (e.g., those with a greater interest or sensory awareness of music or dance) are most likely to benefit from this CAM approach. Along these lines, while this study was begun with the hypothesis that its benefit would accrue through a general relaxation effect, in observing particular children during the program, the strong role that the sensory components of the program played came to be appreciated. This fits with the well-described unique sensory processing aspects of children with an ASD.22 Further analyses of the role that specific sensory factors offer to this program are thus an important direction for future research, and perhaps in understanding intrasubject response variability.
Study Limitations
The data on comorbid conditions and concomitant medication treatment did not suggest that these factors accounted for the variability of subject responses (nor did age or number of sessions attended). However, this conclusion is tempered by the limited data on medication status and comorbidities for the patients recruited from the list-serv. Future studies examining this intervention will therefore need to examine these factors more systematically. In addition, not enough data were obtained from subjects on the degree to which they practiced the intervention at home to determine whether home practice, as was hypothesized, enhances the efficacy of the intervention. Furthermore, as a relationship was not found between number of sessions attended and treatment outcome, this suggests that either treatment factors other than attendance per se, or possibly non-treatment factors that were not controlled for, could have led to these results. Thus, in future studies, other measures of patient engagement will be employed as well as home practice to determine more conclusively whether, as is hypothesized, degree of participation in this program was in fact a key variable accounting for the very strong treatment effects found.
Conclusions
The results of this pilot study suggest a positive impact of a multimodal relaxation program21 on behavioral and cognitive symptoms in BASC-2. Randomized studies of this intervention are needed to confirm this finding. Such studies should involve a larger number of subjects, additional assessment tools of the treatment effect beyond self-report inventories, and a more systematic analysis of the factors contributing to individual variability in treatment response.
Acknowledgments
This investigation was supported by funds from the Centers for Disease Control and Prevention, Grant number 5R01DP000339, and a grant from the Department of Innovation and Quality Integration, Saint Francis Hospital and Medical Center.
Disclosure Statement
No competing financial interests exist.
References
- 1.Chavez B. Chavez-Brown M. Sopko MA., Jr Rey JA. Atypical antipsychotics in children with pervasive developmental disorders. Paediatr Drugs. 2007;9:249–266. doi: 10.2165/00148581-200709040-00006. [DOI] [PubMed] [Google Scholar]
- 2.McDougle CJ. Stigler KA. Erickson CA. Posey DJ. Atypical antipsychotics in children and adolescents with autistic and other pervasive developmental disorders. J Clin Psychiatry. 2008;69(suppl 4):15–20. [PubMed] [Google Scholar]
- 3.Aman MG. Lam KS. Van Bourgondien ME. Medication patterns in patients with autism: Temporal, regional, and demographic influences. J Child Adolesc Psychopharmacol. 2005;15:116–126. doi: 10.1089/cap.2005.15.116. [DOI] [PubMed] [Google Scholar]
- 4.Posey DJ. Stigler KA. Erickson CA. McDougle CJ. Antipsychotics in the treatment of autism. J Clin Invest. 2008;118:6–14. doi: 10.1172/JCI32483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bishop FL. Yardley L. Lewith GT. Why consumers maintain complementary and alternative medicine use: A qualitative study. J Altern Complement Med. 2010;16:175–182. doi: 10.1089/acm.2009.0292. [DOI] [PubMed] [Google Scholar]
- 6.Levy SE. Hyman SL. Novel treatments for autistic spectrum disorders. Ment Retard Dev Disabil Res Rev. 2005;11:131–142. doi: 10.1002/mrdd.20062. [DOI] [PubMed] [Google Scholar]
- 7.Levy SE. Hyman SL. Complementary and alternative medicine treatments for children with autism spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2008;17:803–820. doi: 10.1016/j.chc.2008.06.004. ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shannahoff-Khalsa DS. An introduction to Kundalini yoga meditation techniques that are specific for the treatment of psychiatric disorders. J Altern Complement Med. 2004;10:91–101. doi: 10.1089/107555304322849011. [DOI] [PubMed] [Google Scholar]
- 9.Jensen PS. Kenny DT. The effects of yoga on the attention and behavior of boys with attention-deficit/ hyperactivity disorder (ADHD) J Atten Disord. 2004;7:205–216. doi: 10.1177/108705470400700403. [DOI] [PubMed] [Google Scholar]
- 10.Uma K. Nagendra HR. Nagarathna R. Vaidehi S. Seethalakshmi R. The integrated approach of yoga: A therapeutic tool for mentally retarded children. A one-year controlled study. J Ment Defic Res. 1989;33(pt 5):415–421. doi: 10.1111/j.1365-2788.1989.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 11.Levy SE. Mandell DS. Schultz RT. Autism. Lancet. 2009;374:1627–1638. doi: 10.1016/S0140-6736(09)61376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Streeter CC. Jensen JE. Perlmutter RM, et al. Yoga Asana sessions increase brain GABA levels: A pilot study. J Altern Complement Med. 2007;13:419–426. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 13.Streeter CC. Whitfield TH. Owen L, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: A randomized controlled MRS study. J Altern Complement Med. 2010;16:1145–1152. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith C. Hancock H. Blake-Mortimer J. Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15:77–83. doi: 10.1016/j.ctim.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Lavey R. Sherman T. Mueser KT, et al. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399–402. doi: 10.2975/28.2005.399.402. [DOI] [PubMed] [Google Scholar]
- 16.Woolery A. Myers H. Sternlieb B. Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–63. [PubMed] [Google Scholar]
- 17.Gold C. Wigram T. Elefant C. Music therapy for autistic spectrum disorder. Cochrane Database Syst Rev. 2006;2:CD004381. doi: 10.1002/14651858.CD004381.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Kern P. Wolery M. Aldridge D. Use of songs to promote independence in morning greeting routines for young children with autism. J Autism Dev Disord. 2007;37:1264–1271. doi: 10.1007/s10803-006-0272-1. [DOI] [PubMed] [Google Scholar]
- 19.Whipple J. Music in intervention for children and adolescents with autism: A meta-analysis. J Music Ther. 2004;41:90–106. doi: 10.1093/jmt/41.2.90. [DOI] [PubMed] [Google Scholar]
- 20.Kim J. Wigram T. Gold C. Emotional, motivational and interpersonal responsiveness of children with autism in improvisational music therapy. Autism. 2009;13:389–409. doi: 10.1177/1362361309105660. [DOI] [PubMed] [Google Scholar]
- 21.Benson H. Beary JF. Carol MP. The relaxation response. Psychiatry. 1974;37:37–46. doi: 10.1080/00332747.1974.11023785. [DOI] [PubMed] [Google Scholar]
- 22.Kern JK. Trivedi MH. Grannemann BD, et al. Sensory correlations in autism. Autism. 2007;11:123–134. doi: 10.1177/1362361307075702. [DOI] [PubMed] [Google Scholar]
- 23.Rutter M. Caspi A. Moffitt TE. Using sex differences in psychopathology to study causal mechanisms: Unifying issues and research strategies. J Child Psychol Psychiatry. 2003;44:1092–1115. doi: 10.1111/1469-7610.00194. [DOI] [PubMed] [Google Scholar]
- 24.el-Hazmi MA. Autism and mental retardation: The genetic relationship and contribution. East Mediterr Health J. 2001;7:536–543. [PubMed] [Google Scholar]
- 25.Depositario-Cabacar DF. Zelleke TG. Treatment of epilepsy in children with developmental disabilities. Dev Disabil Res Rev. 2010;16:239–247. doi: 10.1002/ddrr.116. [DOI] [PubMed] [Google Scholar]
- 26.Volker MA. Lopata C. Smerbeck AM, et al. BASC-2 PRS profiles for students with high-functioning autism spectrum disorders. J Autism Dev Disord. 2010;40:188–199. doi: 10.1007/s10803-009-0849-6. [DOI] [PubMed] [Google Scholar]
- 27.Doyle A. Ostrander R. Skare S, et al. Convergent and criterion-related validity of the Behavior Assessment System for Children-Parent Rating Scale. J Clin Child Psychol. 1997;26:276–284. doi: 10.1207/s15374424jccp2603_6. [DOI] [PubMed] [Google Scholar]
- 28.Kanne SM. Christ SE. Reiersen AM. Psychiatric symptoms and psychosocial difficulties in young adults with autistic traits. J Autism Dev Disord. 2009;39:827–833. doi: 10.1007/s10803-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 29.Vickerstaff S. Heriot S. Wong M, et al. Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. J Autism Dev Disord. 2007;37:1647–1664. doi: 10.1007/s10803-006-0292-x. [DOI] [PubMed] [Google Scholar]
- 30.Allison Bender H. Auciello D. Morrison CE, et al. Comparing the convergent validity and clinical utility of the Behavior Assessment System for Children-Parent Rating Scales and Child Behavior Checklist in children with epilepsy. Epilepsy Behav. 2008;13:237–242. doi: 10.1016/j.yebeh.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 31.Beg MR. Casey JE. Saunders CD. A typology of behavior problems in preschool children. Assessment. 2007;14:111–128. doi: 10.1177/1073191106297463. [DOI] [PubMed] [Google Scholar]
- 32.McCracken JT. McGough J. Shah B, et al. Risperidone in children with autism and serious behavioral problems. NEJM. 2002;347:314–321. doi: 10.1056/NEJMoa013171. [DOI] [PubMed] [Google Scholar]
- 33.Marcus RN. Owen R. Kamen L, et al. A placebo-controlled, fixed-dose study of aripiprazole in children and adolescents with irritability associated with autistic disorder. J Am Acad Child Adolesc Psychiatry. 2009;48:1110–1119. doi: 10.1097/CHI.0b013e3181b76658. [DOI] [PubMed] [Google Scholar]
- 34.Owen R. Sikich L. Marcus RN, et al. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics. 2009 Dec;124(6):1533–40. doi: 10.1542/peds.2008-3782. [DOI] [PubMed] [Google Scholar]
- 35.Karabekiroglu K. Aman MG. Validity of the aberrant behavior checklist in a clinical sample of toddlers. Child Psychiatry Hum Dev. 2009;40:99–110. doi: 10.1007/s10578-008-0108-7. [DOI] [PubMed] [Google Scholar]
- 36.Marshburn EC. Aman MG. Factor validity and norms for the aberrant behavior checklist in a community sample of children with mental retardation. J Autism Dev Disord. 1992;22:357–373. doi: 10.1007/BF01048240. [DOI] [PubMed] [Google Scholar]
- 37.Brown EC. Aman MG. Havercamp SM. Factor analysis and norms for parent ratings on the Aberrant Behavior Checklist-Community for young people in special education. Res Dev Disabil. 2002;23:45–60. doi: 10.1016/s0891-4222(01)00091-9. [DOI] [PubMed] [Google Scholar]
- 38.Brinkley J. Nations L. Abramson RK, et al. Factor analysis of the aberrant behavior checklist in individuals with autism spectrum disorders. J Autism Dev Disord. 2007;37:1949–1459. doi: 10.1007/s10803-006-0327-3. [DOI] [PubMed] [Google Scholar]
- 39.Shaffer JP. Multiple hypothesis testing. Annu Rev Psychol. 1995;46:561–584. [Google Scholar]