Abstract
Objectives
The Iowa Healthy and Active Minds Study is a four-arm randomised controlled trial of a visual processing speed training programme (Road Tour). This article presents the preplanned interim results immediately after training (6–8 weeks post-randomisation) for the primary outcome.
Design
Within two age strata (50–64 vs ≥65), 681 men and women attending general internal and family medicine clinics were randomised to four training groups: (1) supervised, on-site standard (10 h) dose of Road Tour training; (2) supervised, on-site standard dose of Road Tour training with 4 h of subsequent booster training scheduled to occur at 11 months post-randomisation (ie, no booster training had occurred at the time of this interim analysis); (3) supervised, on-site standard dose of attention control (crossword puzzles) training and (4) self-administered, at-home standard dose of Road Tour training. The primary outcome was the Useful Field of View (UFOV) test. Three intent-to-treat interim analyses were conducted, including (1) multiple linear regression models of composite UFOV scores using Blom rank transformations, (2) general linear mixed effects models and (3) multiple logistic regression models among the 620 participants (91%) with complete data.
Results
In the linear regression analyses of both age strata, random assignment to any Road Tour training group versus the attention control group was significant (p<0.001), with an effect size of −0.558 (adjusted for the Blom rank transformed UFOV score at randomisation). Similar results were obtained for each Road Tour group and within each age stratum and from the general linear and logistic regression models.
Conclusions
Assignment to a standard dose of Road Tour training yielded medium-sized post-training improvements in visual processing speed. Road Tour was equally effective whether administered under laboratory supervision or self-administered in the patient's home and for participants in both age strata (50–64 vs ≥65).
Clinical trial registration number
Article summary
Article focus
Normative age-related declines in cognitive functioning leave a pressing need to identify efficient and effective training interventions for older adults.
The Iowa Healthy and Active Minds Study is a four-arm randomised controlled trial of three modes of delivering a computerised visual speed of processing intervention versus an attention control group.
Key messages
The Iowa Healthy and Active Minds Study is the first randomised controlled trial to evaluate the efficacy and effectiveness of Road Tour, a second-generation computerised visual speed of processing intervention.
Statistically significant medium-sized post-training improvements in visual processing speed were observed regardless of delivery method or age strata.
Strengths and limitations of this study
This randomised controlled trial uses a large sample of men and women aged ≥50 years old and overcomes four of the five important limitations (exclusion of 50–64-year-olds, use of a no-contact control group, adherence-conditioned assignment to booster training and reliance on a supervised cognitive training programme) of a previous multisite trial.
The sample was drawn from just one family care centre in which minorities were underrepresented, participants had to have a home computer and internet access, and data on the primary outcome were available only at randomisation and post-training.
Introduction
It is well established that age-related cognitive decline is a normal part of the ageing process that occurs across many cognitive functions including memory, orientation, attention, abstract thinking and perception.1–4 These age-related cognitive changes can be viewed as the result of physical, behavioural and environmental changes that combine to promote negative brain plasticity and degradations in functioning.5 Fortunately, this capacity for physical and functional brain change across the lifespan is bi-directional.5 6 Indeed, just as brain plasticity can lead towards degradation in cognitive functioning with age, this same plasticity process can also be used to strengthen cognitive abilities.7–9 This is especially important given recent evidence demonstrating that these age-related declines commence as early as age 28 and then continue in a linear fashion throughout the remainder of the life course.9
Many training programmes have been developed to help mitigate these age-related cognitive functioning declines. Although the gains associated with most earlier cognitive training interventions appeared to be highly task and context specific, more recent developments have demonstrated that improving the coordination of executive skills can transfer beyond the testing environment.7 These often involve complex video games, task-switching paradigms or divided attention tasks because these training platforms provide a carefully controlled and well-structured environment. Some of these successful interventions have focused on improving visual information processing speed, which is not surprising given the considerable evidence that supports the role of processing speed in age-related cognitive decline.10–12
Perhaps the most extensively evaluated intervention that targets improving visual processing speed is that developed by Ball and Roenker.4 13 14 Their programme trains users to improve the speed and accuracy with which they identify and locate visual information using a divided attention format. Over time, the difficulty and complexity of each task is systematically increased as users attain specified performance criteria. Manipulations to increase difficulty include decreasing visual stimuli duration, adding visual or auditory distracters, increasing similarity between target and distracter stimuli, and presenting visual targets over a broader spatial expanse. The basic tasks, however, are always the same—central discrimination and peripheral target location. Substantial evidence from the US National Institutes of Health (NIH)-funded multisite randomised controlled trial (RCT) known as ACTIVE (Advanced Cognitive Training for Vital Elderly) has shown the efficacy of Ball and Roenker's visual processing speed intervention on both immediate and distal cognitive functioning, as well as on subsequent health outcomes.15–24
Posit Science Corporation (San Francisco, California, USA) acquired the rights to Ball and Roenker's visual speed of processing training programme in 2007.4 13 14 While all the original tasks were maintained, the delivery platform was modified to be user-friendly and self-administered. Gaming elements were also added to improve user engagement and enhance compliance. The resulting second-generation computerised visual speed of processing training programme is known as Road Tour and has been commercially available since 2009 as part of the Insight visual processing speed suite (which includes four other visual training programmes known as Bird Safari, Jewel Diver, Master Gardenerand Sweep Seeker) or as part of the DriveSharp driving suite (which also includes Jewel Diver and Sweep Seeker) (http://www.positscience.com/our-products).
We designed the Iowa Healthy and Active Minds Study (IHAMS) to evaluate the efficacy and effectiveness of Road Tour. The IHAMS is a four-group parallel RCT (NCT01165463) whose protocol has been described in detail elsewhere.25 In this article, we report on the preplanned interim results immediately after training (6–8 weeks post-randomisation) for the primary outcome. Because standard booster training did not commence until 11 months post-randomisation and because little if any supplemental training beyond 10 h in the at-home group would have occurred until after 6–8 weeks post-randomisation, we hypothesised that participants randomised to any of the three Road Tour training groups (no booster training subsequently scheduled, booster training scheduled to occur much later at 11 months post-randomisation and at-home training with self-dosing allowed after 6–8 weeks post-randomisation) should have significantly and similarly greater improvements in visual processing speed immediately after training than the attention control group. This planned interim post-training analysis represents hypothesis H1 from the original IHAMS protocol25 and can only be evaluated for the primary outcome because the secondary outcomes were not assessed at 6–8 weeks post-randomisation.
Methods and analysis
Overview
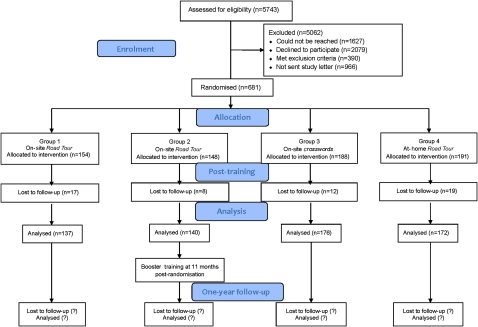
Figure 1 shows the IHAMS study design and participant recruitment results, with additional details available in the article describing the study protocol.25 IHAMS used a 3:3:4:4 allocation ratio and block randomisation separately within two age strata (50–64 (mean=57.2, SD=4.2, range=50–64) vs ≥65 (mean=71.4, SD=5.7, range=65–87)). A total of 681 participants were randomised to one of the following groups: (1) 10 h (a single 2 h session each week over the first 5–6 weeks) of supervised on-site training using Road Tour (N=154), (2) 10 h of supervised on-site training using Road Tour plus 4 h of future booster training at 11 months post-randomisation (N=148), (3) 10 h of supervised on-site attention control using computerised crossword puzzles (Boatload of Crosswords, Boatload Puzzles; LLC, Yorktown Heights, New York, USA) (N=188) or (4) self-administered at-home training using Road Tour for 10 h or more over the next 5–6 weeks without guidance on the number of sessions or their length (N=191), with the option to continue using Road Tour thereafter but not to use any of the four other training programmes from the Insight software suite until the study was over. Post-training assessments occurred at 6–8 weeks post-randomisation, and complete baseline and post-training data were obtained for 620 participants (91%). One year post-randomisation assessments are scheduled to be completed by late November 2011. The IHAMS was sized to provide ≥80% power to detect an effect size of 0.25 in the primary outcome at 1 year post-randomisation with α=0.05.
Figure 1.
IHAMS CONSORT flow diagram.
Sampling frame
We included all patients attending either the general internal or family medicine clinics of the University of Iowa's Family Care Center (FCC) in the IHAMS sampling frame. The electronic medical record was used for initially selecting potentially eligible participants. The initial inclusion criteria were (1) age ≥50 years old, (2) two or more visits to a primary care physician in the FCC in the past year and (3) the absence of diagnostic codes for Alzheimer's or Picks' disease, arteriosclerotic dementia, other senile or pre-senile dementia, dementia due to alcohol or drugs, amnestic syndrome, or dementia due to other organic conditions. A total of 5743 potentially eligible patients were identified. Weekly random replicates of 100–250 of them were sent a letter describing the study and asking them to telephone the project office and indicate whether or not they were interested in participating.
Telephone screening
We attempted to further screen all potentially eligible patients but could not reach 1627. Of the 4116 remaining potentially eligible patients, 2079 declined to participate and 966 had not yet been sent their letter describing the study by the time that study enrolment was closed, leaving 1071 potentially eligible patients. We conducted brief screening interviews to identify who among them met any of the following exclusion criteria: (1) significant cognitive impairment based on three or more errors on a 10-item Mental Status Exam (N=15),26 (2) significant self-reported uncorrected visual acuity problems (N=63), (3) not having a personal computer with a CD-ROM in the home (N=303), (4) not having internet access (N=8) or (5) having previously used a computerised programme for improving cognitive function (N=1). This resulted in the exclusion of 390 potential participants.
Informed consent and baseline interviews
After completing the screening interview, eligible patients were scheduled for a 2 h visit to our laboratory where written informed consent was obtained for the 681 participants who were enrolled between 22 March and 16 November 2010. The 681 enrolees were then administered their baseline (randomisation) interviews by trained research assistants using computer-assisted interviewing protocols. Immediately afterwards, each participant was randomised to one of the four study groups.
Randomisation procedure
The study biostatistician (MPJ) determined the order of assignments using a computer-generated list of random numbers and a 3:3:4:4 allocation ratio because the first two groups can be pooled for some analyses. Sample size was based on a priori power calculations to achieve 80% power at α=0.05 for a two-tailed test with a 0.25 effect size between each training group and the attention control group at 1 year post-randomisation. Block randomisation was used to maintain balance on the two age strata (50–64 and ≥65). Block sizes of 4, 8 and 12 were randomly varied. The assignment for each participant's ID number was recorded on a participant letter and then sealed in an opaque envelope with only the ID number visible. Two age-stratum-specific boxes containing the assignment envelopes were stored in a locked cabinet in the Project Coordinator's office. The Project Coordinator (MMD) had the responsibility of unsealing the envelope (from the appropriate age-stratum box) and revealing each participant's group assignment.
Group training logistics
The three on-site training groups received 10–15 min of individual instruction for either Road Tour or the crossword puzzles programme, depending on their random assignment, in one of two identically configured laboratories. After that, a single ‘monitor’ (usually an undergraduate student trained and certified on both Road Tour and the crossword puzzles programme) was available in one or the other training laboratory (which were adjacent to each other) to provide help with any questions or issues that arose. Thus, although several monitors were needed to accommodate training schedules and specific monitors were not available for the entire enrolment period, at any given training time/session, the monitor was the same. Each of the two primary training laboratories had five workstations. Both Road Tour training arms (with and without subsequently scheduled future booster training) were trained in the same laboratory. A total of five weekly 2 h training sessions were scheduled for the standard training dose. After completing 10 h of training or by 6–8 weeks post-randomisation, whichever came first, participants in the three on-site training groups were invited back to our training laboratories for their post-training assessments on the primary outcome.
Participants randomly assigned to Road Tour training at-home were taken to a third adjacent training laboratory in which they were shown (step-by-step) how to load the software onto a PC. After this, they received about 5–10 min of scripted instruction on how to use Road Tour and then practiced using it for about 10–15 min. The participants in the at-home Road Tour training group were then sent home with the CD containing the Road Tour software to load on their home PCs, as well as a detailed set of step-by-step instructions containing all the screen-shots that they would encounter in doing so. They were also given the phone number and email information for contacting the Project Coordinator (MMD) to answer any questions they might have about loading the software onto their home PCs. These participants were asked to use Road Tour at home for 10 h or more during the next 5–6 weeks without guidance about the number of sessions or their length and were also invited back to our training laboratories at 6–8 weeks post-randomisation for their post-training assessments on the primary outcome.
Primary outcome
The primary outcome in the IHAMS is the Useful Field of View (UFOV) PC mouse version.27 Earlier versions of this test have been used in most prior visual speed of processing studies, including ACTIVE.16 17 The UFOV was administered at randomisation, at post-training (6–8 weeks post-randomisation) and is being administered at the 1 year post-randomisation study end point. The UFOV includes three subtests—stimulus identification, divided attention and selective attention—each of which is scored from 17 to 500 ms reflecting the shortest exposure time at which the participant could correctly perform each subtest 75% of the time, with a composite milliseconds outcome score ranging from 51 to 1500 ms. Consistent with the main reports from the ACTIVE trial,16 17 we used Blom rank transformations28 on the UFOV composite scores at randomisation and post-training to normalise the distributions for the multiple linear regression and general linear mixed effects models. The Blom rank transformations resulted in means of zero and SDs of unity and more nearly Gaussian distributions. Blom transformations are commonly used for distributional normalisation29 and have been shown to yield the most reliable results among a variety of alternatives for violations of the distributional assumptions of both multiple linear regression and general linear mixed effects models.30
Secondary outcomes
Secondary outcomes in the IHAMS include five other neuropsychological assessments, all of which were administered at randomisation and are being administered at the 1 year post-randomisation study end point. These neuropsychological assessments were chosen to evaluate whether the effects of visual speed of processing training transfer to cognitive function domains beyond that represented by the UFOV. The secondary outcomes include (1) the Symbol Digit Modalities Test (SDMT),31 (2) the Trail Making A and B Tests (TMT),32 (3) the Controlled Oral Word Association Test,33 (4) the Digit Vigilance Test34 and (5) the Stroop Color and Word Test (Stroop).35 SDMT captures divided attention and processing speed and is based on how many of 110 possible digit-symbol pairs were scored as correct pairs by the participant in 90 s. TMT assesses visual scanning ability, processing speed and set-shifting/executive functioning and is coded as the number of seconds needed to correctly complete connecting the number and number–letter sets. Controlled Oral Word Association Test assesses verbal fluency based on the number of unique words beginning with the letter C (or F or L in the second and third trials) generated by the participant during 60 s, with a composite score of the number of correct words used across the three letter trials. Digit Vigilance Test assesses sustained attention and psychomotor speed, is performed by crossing out randomly placed number 6's in 59 rows of numbers and is scored as the error and time totals. The Stroop assesses processing speed and executive functioning and is scored as the correct number of words, colours and colour-words identified in 45 s on each subtest.
The Road Tour training programme
Road Tour's basic appearance to the user is shown in figure 2A. After clicking on the start button to initiate training, figure 2B is shown. Here, both the license plate area and the eight circular locations in the near orbit surrounding it are empty. The empty license plate is then replaced, as in figure 2C, with the target vehicle, either a car or a truck. Similarly, the eight empty circular locations surrounding the license plate are then replaced with seven distracter stimuli (rabbit crossing signs) or the target sign (Route 66). The stimuli (car vs truck and rabbit crossing vs Route 66 sign) are presented for a specified time and are then replaced by figure 2D. The amount of time that figure 2C remains on the screen before being replaced by figure 2D is measured in milliseconds. In figure 2E, both target vehicles (the car and truck) are presented in the centre of the screen, one of which was previously shown in figure 2C as the target vehicle. The user first clicks on the correct target vehicle (car or truck) and then on the circular location where the correct peripheral target (Route 66 sign) appeared (figure 2F). The goal is to improve cognitive processing speed by progressively reducing the milliseconds of exposure that figure 2C remains on the screen with subsequent correct identification of both the stimuli (target car or truck) and the target (Route 66) sign. As the user progresses, three changes occur which further increase task difficulty: (1) the target visual field expands by progressing outward from the license plate to add medium and distal orbits, (2) these are accompanied by an increasing number of distracters to fully populate all three orbits (up to 47) and (3) the vehicle pairs morph through nine different stages or pairs to become more similar and thus more difficult to differentiate.
Figure 2.
(A–F) The initial Road Tour sequence.
Analysis
First, one-way analysis of variance for selected participant characteristics, training time, and the primary and secondary outcomes was conducted. To assess the effects of Road Tour training (vs attention control training) on the primary outcome, we used three intent-to-treat analytic approaches, including (1) multiple linear regression of composite UFOV scores using Blom rank transformations for normalisation (the primary analysis specified in the protocol),25 (2) general linear mixed effects models using the Blom rank transformations (as a secondary analysis) and (3) multiple logistic regression analyses of post-training improvements ≥100 ms in the non-transformed UFOV composite (also as a secondary analysis). In each approach, our first model involved the single binary contrast of being randomly assigned to any Road Tour training, adjusting for the value of the UFOV composite at randomisation. We then substituted three mutually exclusive binary indicators for the single binary contrast. These three binary indicators reflect whether the participant was in the on-site speed of processing intervention without boosters, the on-site speed of processing intervention with boosters subsequently scheduled to occur at 11 months post-randomisation or the at-home speed of processing group versus those in the on-site crossword puzzle (attention control) group as the reference or omitted category. We then estimated both the first and the second model separately within each age stratum.
Results
Baseline group comparisons
Table 1 compares the four training groups on selected participant characteristics (including the self-rated health and change in self-rated health from 1-year ago items from the SF-36),36 amount of training (in minutes) received and the five secondary outcome neuropsychological tests at randomisation. No statistically significant differences were found for any of the participant characteristics. Statistically significant differences were observed, however, on the amount of training received. The attention control group received the most training, while the at-home Road Tour training group received the least (despite instructions to the contrary, 37 of them used one or more of the four other programmes in the Insight suite during training, but only 12 did so for >14 min). This is not surprising given the efforts to schedule the five 2 h training sessions for all participants in the three on-site training groups. Moreover, on-site Road Tour participants were allowed to stop their training once they had completed all 81 of the available exercise sets, which occurred about 5% of the time. Finally, although Road Tour directly monitors training in minutes based on actual programme usage, participant training in the attention control group was monitored by project staff based on the completion of 2 h training sessions.
Table 1.
Means and SDs (in parentheses) of selected participant characteristics and the five secondary outcome neuropsychological tests at randomisation by training group status, N=681
| Variable | Overall N=681 | Road Tour on-site N=154 | Road Tour on-site with future boosters N=148 | Attention control on-site N=188 | Road Tour at-home N=191 |
| Personal characteristics | |||||
| Age (years) | 61.9 (8.2) | 61.4 (8.1) | 62.5 (8.2) | 61.8 (8.7) | 61.9 (7.9) |
| Men (%) | 37.3 (0.5) | 37.2 (0.5) | 32.5 (0.5) | 42.0 (0.5) | 36.7 (0.5) |
| Married (%) | 69.9 (0.5) | 73.0 (0.5) | 61.0 (0.5) | 73.4 (0.4) | 71.2 (0.5) |
| Single (%) | 11.2 (0.3) | 10.1 (0.3) | 14.9 (0.4) | 8.0 (0.3) | 12.0 (0.3) |
| Working (%) | 54.5 (0.5) | 56.8 (0.5) | 53.9 (0.5) | 50.0 (0.5) | 57.6 (0.6) |
| Retired (%) | 35.5 (0.4) | 35.1 (0.5) | 36.4 (0.4) | 34.2 (0.5) | 34.6 (0.3) |
| Income ≤ $35K (%) | 28.3 (0.5) | 24.3 (0.4) | 36.4 (0.5) | 27.7 (0.5) | 25.7 (0.4) |
| Income ≥ $75K (%) | 46.6 (0.5) | 45.3 (0.5) | 41.6 (0.4) | 47.3 (0.5) | 50.8 (0.5) |
| Self-rated health (5=best 1=worst) | 3.8 (0.9) | 3.8 (0.9) | 3.8 (0.8) | 3.7 (0.9) | 3.9 (0.8) |
| One-year change in self-rated health (5=best, 1=worst) | 3.2 (0.8) | 3.3 (0.8) | 3.3 (0.8) | 3.2 (0.8) | 3.3 (0.7) |
| Training time | |||||
| Minutes of training | 469 (217) | 450 (199) | 488 (151) | 535 (154) | 404 (295) |
| Neuropsychological tests | |||||
| SDMT (number of correct) | 50.5 (9.4) | 51.8 (9.0) | 50.5 (9.5) | 48.7 (9.3) | 51.1 (9.6) |
| Trails A (sec) | 41.9 (13.3) | 40.9 (10.9) | 39.8 (12.3) | 45.0 (16.3) | 41.2 (12.0) |
| Trails B (sec) | 66.9 (27.2) | 63.8 (30.8) | 65.8 (23.9) | 71.8 (30.3) | 65.2 (22.1) |
| COWAT composite (number of words) | 42.0 (11.9) | 42.4 (11.0) | 41.9 (12.7) | 40.5 (11.5) | 43.2 (12.4) |
| DVT errors (n) | 8.1 (8.2) | 7.5 (9.6) | 9.0 (7.7) | 7.9 (7.6) | 8.0 (7.8) |
| DVT time (s) | 377.0 (84.1) | 369.0 (82.2) | 374.8 (83.7) | 387.9 (86.5) | 374.5 (83.1) |
| Stroop word (n) | 70.4 (13.1) | 71.2 (13.6) | 71.8 (13.5) | 68.1 (12.8) | 71.1 (12.4) |
| Stroop colour (n) | 97.8 (17.6) | 100.3 (17.3) | 96.5 (18.7) | 95.3 (17.8) | 99.3 (16.5) |
| Stroop colour-word (n) | 38.1 (9.0) | 38.7 (9.5) | 38.0 (8.7) | 37.1 (9.1) | 38.6 (8.9) |
COWAT, Controlled Oral Word Association Test; DVT, Digit Vigilance Test; SDMT, Symbol Digit Modalities Test.
Statistically significant differences between the training groups were also observed for the SDMT, TMT (A and B) and the word and colour subtests of the Stroop. In all cases, the attention control group demonstrated the lowest level of performance. These differences, however, were modest in the absolute, although post-hoc comparisons using Dunnett tests found eight of the 15 group level contrasts involving the attention control group to be statistically significant. The attention control group had significantly lower performance than (1) all three training groups on the TMT-A, (2) the on-site training group without subsequent scheduled boosters on the SDMT, TMT-B and the Stroop colour subtest and (3) the on-site training group without subsequent scheduled boosters and the at-home training group on the Stroop word subtest. Therefore, we will adjust for these differences in all subsequent analyses by including the value of the outcome measure at randomisation.
Table 2 compares the four training groups on the three UFOV subtests—stimulus identification, divided attention and selective attention—as well as the UFOV composite and Blom rank transformed UFOV composites at randomisation and at post-training. No statistically significant differences were observed on the three UFOV subtests, the UFOV composite or the Blom rank transformed UFOV composite scores at randomisation, although the attention control group had the slowest performance in all comparisons. At post-training, however, statistically significant differences were observed on the three UFOV subtests, on the UFOV composite score and on the Blom rank transformed UFOV composite score. Moreover, Dunnett tests indicated that all the training group comparisons involving the attention control group were statistically significant as well.
Table 2.
Means and SDs (in parentheses) of the three UFOV subtests (stimulus identification, divided attention and selective attention), the UFOV Composite and the Blom rank transformed UFOV composite at randomisation and at post-training
| Variable | Overall N=681 | Road Tour on-site N=154 | Road Tour on-site with future boosters N=148 | Attention control on-site N=188 | Road Tour at-home N=191 |
| Randomisation | |||||
| Stimulus identification | 21.5 (20.8) | 19.6 (9.2) | 22.7 (25.5) | 24.4 (29.6) | 21.5 (20.8) |
| Divided attention | 75.2 (89.8) | 79.1 (98.9) | 65.9 (70.2) | 81.4 (94.6) | 73.4 (90.9) |
| Selective attention | 203.3 (103.1) | 202.5 (106.3) | 193.7 (94.7) | 214.1 (108.5) | 200.7 (101.0) |
| UFOV composite | 300.0 (181.6) | 301.2 (192.5) | 282.7 (154.9) | 319.9 (197.1) | 292.8 (175.3) |
| Blom rank transformed UFOV composite | 0.0 (1.0) | −0.0 (1.0) | −0.1 (0.9) | 0.1 (1.0) | −0.0 (1.0) |
| Post-training | Overall N=620 | Road Tour on-site N=138 | Road Tour on-site with future boosters N=142 | Attention control on-site N=176 | Road Tour at-home N=172 |
| Stimulus identification | 18.5 (10.8) | 17.7 (5.8) | 17.3 (4.4) | 20.8 (17.5) | 17.9 (7.8) |
| Divided attention | 45.4 (66.9) | 37.6 (50.3) | 44.7 (64.0) | 63.1 (89.9) | 34.3 (47.4) |
| Selective attention | 157.5 (93.0) | 135.1 (75.9) | 149.1 (87.8) | 201.6 (106.6) | 136.9 (79.0) |
| UFOV composite | 221.6 (147.2) | 190.5 (114.0) | 211.6 (137.6) | 285.5 (182.4) | 189.1 (114.8) |
| Blom rank transformed UFOV composite | 0.0 (0.8) | −0.1 (0.7) | −0.0 (0.9) | 0.4 (0.8) | −0.2 (0.8) |
UFOV, Useful Field of View.
Multiple linear regression
The first panel of table 3 contains the results from the multiple linear regression analysis of the Blom rank transformed UFOV composite scores at post-training predicted by the Blom rank transformed UFOV composite scores at randomisation and the single binary contrast of being randomly assigned to any Road Tour training for all 620 IHAMS participants with complete data. The second and third panels contain the results from similar analyses stratified on age (50–64 vs ≥65). Because the Blom rank transformed UFOV composite scores have been normalised to have a mean of zero and a SD of unity, the unstandardised b coefficients shown may be directly interpreted as effect size estimates. The effect sizes are −0.558 in the pooled analysis, −0.479 for the ≥65 age stratum and −0.626 for the 50–64 age stratum, with all three p values <0.001. Although the magnitudes of the effect sizes appear larger in the younger age stratum than in the older age stratum, note that all effect sizes are within the 95% CIs of each other and are thus functionally comparable. This was verified by adding a binary marker for age strata and its interaction with having any Road Tour training to the model, neither of which were statistically significant.
Table 3.
Pooled and age-stratum-specific multiple linear regression results for predicting the Blom rank transformed composite UFOV score at 6–8 weeks post-randomisation
| Unstandardised regression coefficient b | p Value | Lower 95% CI | Higher 95% CI | |
| Pooled analysis with both age strata (N=620) | ||||
| Intercept | 0.415 | 0.001 | 0.309 | 0.520 |
| Any Road Tour training (N=444) | 0.558 | 0.001 | −0.433 | −0.683 |
| On-site attention control (N=176) | 0.000 | – | – | – |
| Blom rank transformed UFOV at randomisation | 0.643 | 0.001 | 0.585 | 0.700 |
| R squared | 0.491 | 0.001 | ||
| Separate analysis in the ≥65 age stratum (N=209) | ||||
| Intercept | 0.518 | 0.001 | 0.343 | 0.694 |
| Any Road Tour training (N=154) | −0.479 | 0.001 | −0.290 | −0.668 |
| On-site attention control (N=55) | 0.000 | – | – | – |
| Blom rank transformed UFOV at randomisation | 0.650 | 0.001 | 0.547 | 0.754 |
| R squared | 0.482 | 0.001 | ||
| Separate analysis in the 50–64 age stratum (N=411) | ||||
| Intercept | 0.352 | 0.001 | 0.218 | 0.486 |
| Any Road Tour training (N=292) | −0.626 | 0.001 | −0.467 | −0.785 |
| On-site attention control (N=119) | 0.000 | – | – | – |
| Blom rank transformed UFOV at randomisation | 0.556 | 0.001 | 0.479 | 0.634 |
| R squared | 0.413 | 0.001 | ||
UFOV, Useful Field of View.
Table 4 contains the results from the multiple linear regression analysis of the Blom rank transformed UFOV composite scores when the single binary contrast of being randomly assigned to any Road Tour training is replaced by the set of three binary indicators reflecting each specific Road Tour training group. As in table 3, the first panel of table 4 contains the results for all 620 IHAMS participants with complete data, while the second and third panels contain the results from analyses stratified on age (50–64 vs ≥65). Also as in table 3, all the coefficients shown may be directly interpreted as effect size estimates, and all have p values <0.001. The effect sizes in table 4 for each of the Road Tour training groups are very similar to those shown in table 3 for the pooled markers. Here, too, the magnitude of the effect sizes for each training group appears larger in the younger age stratum than in the older age stratum, but once again, all effect sizes are within the 95% CIs of each other and are thus functionally comparable. Similarly, while the effect sizes within panels appear smallest for the on-site training group not scheduled to receive future booster training, only for the younger age stratum do these lie outside of each other's 95% CIs and then only when compared with the at-home training group. Taken together, the multiple linear regression results contained in tables 3 and 4 support our hypothesis for the post-training effects in all respects.
Table 4.
Pooled and age-stratum-specific multiple linear regression results for predicting the Blom rank transformed composite UFOV score at 6–8 weeks post-randomisation
| Unstandardised regression coefficient b | p Value | Lower 95% CI | Higher 95% CI | |
| Pooled analysis with both age strata (N=620) | ||||
| Intercept | 0.415 | 0.001 | 0.309 | 0.520 |
| Road Tour on-site (N=139) | −0.457 | 0.001 | −0.299 | −0.616 |
| Road Tour on-site with future boosters (N=136) | −0.585 | 0.001 | −0.426 | −0.745 |
| On-site attention control (N=174) | 0.000 | – | – | – |
| Road Tour at home (N=171) | −0.629 | 0.001 | −0.469 | −0.769 |
| Blom rank transformed UFOV at randomisation | 0.642 | 0.001 | 0.585 | 0.699 |
| R squared | 0.495 | 0.001 | ||
| Separate analysis in the ≥65 age stratum (N=209) | ||||
| Intercept | 0.520 | 0.001 | 0.343 | 0.697 |
| Road Tour on-site (N=47) | −0.465 | 0.001 | −0.226 | −0.704 |
| Road Tour on-site with future boosters (N=46) | −0.480 | 0.001 | −0.240 | −0.721 |
| On-site attention control (N=55) | 0.000 | – | – | – |
| Road Tour at home (N=61) | −0.490 | 0.001 | −0.263 | −0.718 |
| Blom rank transformed UFOV at randomisation | 0.648 | 0.001 | 0.542 | 0.697 |
| R squared | 0.482 | 0.001 | ||
| Separate analysis in the 50–64 age stratum (N=411) | ||||
| Intercept | 0.353 | 0.001 | 0.219 | 0.486 |
| Road Tour on-site (N=92) | −0.483 | 0.001 | −0.280 | −0.685 |
| Road Tour on-site with future boosters (N=90) | −0.665 | 0.001 | −0.462 | −0.869 |
| On-site attention control (N=119) | 0.000 | – | – | – |
| Road Tour at home (N=110) | −0.711 | 0.001 | −0.519 | −0.903 |
| Blom rank transformed UFOV at randomisation | 0.560 | 0.001 | 0.483 | 0.638 |
| R squared | 0.421 | 0.001 | ||
UFOV, Useful Field of View.
General linear models with mixed effects
We used general linear models with mixed effects as a secondary analytic approach to adjust for the correlated errors within participants that may arise from the repeated UFOV measurement (which the primary multiple linear regression analyses do not address).37 The results from the general linear mixed effects model for the effect of being randomly assigned to any Road Tour training for all 620 IHAMS participants with complete data revealed (data not shown) a statistically significant (p<0.001) interaction between the Blom rank transformed outcome and any Road Tour training reflecting a standardised mean difference (effect size) of −0.430. When this model was run separately within age strata, the standardised mean difference was −0.378 (p<0.001) in the older stratum and −0.490 (p<0.001) in the younger stratum. Once again, although these effect sizes appear larger in the younger stratum, these differences were not statistically significant, as indicated when the binary marker for age strata and its interaction with any Road Tour training (a group-by-time-by-age stratum interaction) was added to the general linear model for all IHAMS participants.
When the single binary contrast of being randomly assigned to any Road Tour training was replaced by the set of three binary indicators reflecting each specific Road Tour training group for all IHAMS participants, standardised mean differences (compared with the attention control group) of −0.356, −0.448 and −0.475 were obtained for the on site Road Tour without subsequently scheduled future booster training, on site Road Tour with scheduled future booster training and at-home Road Tour training groups, all of which were statistically significant (p<0.001). Similar results were obtained when this general linear model was estimated within age strata. Once again, no group-by-time-by-age stratum interactions were observed in the general linear mixed effects model for all IHAMS participants. Thus, when taken together, the general linear mixed effects modelling results also support our hypothesis for the post-training effects in all respects.
Multiple logistic regression
The multiple logistic regression analysis was conducted to ensure that both analyses of the Blom rank transformed UFOV composites were not statistical artefacts of the normalisation algorithm. An effect threshold of improvements ≥100 ms was chosen because it represents an effect size of 0.55 based on the non-transformed baseline UFOV composite, which is equivalent to that observed in table 3 for the pooled analysis of assignment to any Road Tour training in the overall IHAMS sample. The adjusted odds ratio for being randomised to any Road Tour training group on achieving a post-training improvement in the UFOV test ≥100 ms was 4.85 (p<0.001). The absolute improvement effect was 12.2% (34.3% of Road Tour subjects improved ≥100 ms vs 23.1% or attention control subjects). This simple model fit the data extremely well (area under the curve (AUC)=0.92). We then replaced the single binary marker with the three indicators for each of the Road Tour training groups and found that while the three Road Tour training groups' adjusted odds ratios varied from 4.01 to 5.52 (p values<0.001; AUC=0.92; absolute improvement effects 10.0%–12.5%), they all fell within the others' CIs, reflecting similar effect sizes. Comparable results were found (not shown) within age strata, although the model for the younger age stratum fit the data slightly better (AUC=0.95 vs AUC=0.86). Thus, when taken together, these multiple logistic regression results also support our hypothesis for the post-training effects in all respects.
Conclusions
Gradual cognitive decline is nearly universal and is well recognised as a normal part of the ageing process. According to Salthouse,38 most age-related cognitive deteriorations are at least partially attributable to declines in information processing speed, which affects episodic and working memory, verbal fluency and reasoning abilities. Previous work, especially the US NIH-funded multisite ACTIVE trial, has led to the development of a promising, second-generation computer-based intervention to improve visual processing speed known as Road Tour. We designed the IHAMS to assess the efficacy and effectiveness of Road Tour.
There are five important aspects of IHAMS that warrant further mention. First, the IHAMS overcomes five major limitations of the previous US NIH-funded ACTIVE multisite RCT, the first three of which we were able to directly evaluate in this article reporting on the post-training results. In addition to participants aged 65 years or older, the IHAMS included 50–64-year-olds to determine whether speed of processing training is efficacious and effective before substantial cognitive decline occurs in the seventh decade.39 If speed of processing training is efficacious in this younger cohort, preventive interventions could focus on improving cognitive functioning before the rapid age-related declination process even begins. The IHAMS also used an attention control group that was trained on computerised crossword puzzles rather than a no-contact control group. This allowed us to directly evaluate the potential that placebo effects cloud the interpretation of the results from ACTIVE.25 By using Road Tour rather than its predecessor, the IHAMS avoids reliance on a supervised training intervention. This allowed us to directly evaluate whether sending participants home with the software to use on their own PCs is efficacious, and if so, whether it was as effective as supervised on-site training, which potentially expands substantially the ability to implement widespread public health interventions. The IHAMS also directly randomised participants to receive or not receive on-site booster training, as opposed to the adherence-conditioned assignment to booster training used in ACTIVE. When the 1-year follow-up data become available, this will allow us to separate the effects associated with standard dosing from those derived from standard dosing plus booster training. The IHAMS also included five additional neuropsychological tests assessed at baseline that will also be assessed at the 1-year follow-up as secondary outcomes. Once the 1-year follow-up data become available, this will allow us to assess the extent to which Road Tour effects on the primary outcome transfer to the other cognitive functions tapped by these neuropsychological tests.
The second important aspect of this study involves the training intervention itself. Road Tour is easy to use on any PC (versions for both PC and Apple platforms are available) at any location. Adherence to training was very good, even in the at-home training group, which did not benefit from the support of weekly scheduling contacts. The targeted standard training dose was just 10 h, although the mean amount of time that it was used in the two on-site training groups was only 7.8 h spread over a 5-week period. The 2 h training sessions were extremely well tolerated, and no discomfort of any kind was reported by any participant during delivery of the standard training dose. In sum, the ability to readily implement Road Tour training in widespread public health interventions is extremely promising from a logistical perspective.
The demonstrated efficacy of Road Tour to improve UFOV scores in these interim analyses is the third important aspect of this study that warrants further mention. Three different analytic approaches—multiple linear regression, general linear mixed effects and multiple logistic regression models—all substantially supported our hypothesis for the post-training effects in all respects. The primary analytic approach was the pooled multiple linear regression of the Blom rank transformed UFOV composite at post-training. When these analyses were done pooling both age strata, the regression coefficient for random assignment to any Road Tour training group versus the attention control group was statistically significant (p<0.001) with an effect size of −0.558 (adjusted for the Blom rank transformed UFOV test at randomisation). Similar results were also obtained when comparing each of the three training groups with the attention control group. That this medium effect size was obtained with an average of <8 h of training suggests that the potential for widespread public health interventions is very promising.
Directly comparing the efficacy of Road Tour obtained in these IHAMS interim analyses to the speed of processing training results obtained from a meta-analysis consisting of ACTIVE and five other visual speed of processing training RCTs with a total enrolment of 907 subjects followed for varying time lengths13 is problematic for at least four reasons. First, most of those RCTs used the touch screen version of the UFOV, which has four subtests and yields a composite score that ranges between 68 and 2000 ms, while IHAMS used the PC mouse version, which has only three subtests and yields a composite score that ranges between 51 and 1500 ms. Second, most of those RCTs used a no-contact control group design that added any potential placebo effect to their training effect estimates. Moreover, IHAMS used an attention control group that was trained using a computerised crossword puzzle programme that may have led to some improvement in processing speed beyond the potential placebo effect. Third, all those RCTs used the predecessor version of the speed of processing software that required supervised on-site training. Fourth, IHAMS used less robust mental status and self-reported visual acuity screening tools than those RCTs for exclusion purposes, which enhances the generalisability of the IHAMS while biasing its effect size estimates towards the null. Taking the four differences noted above into consideration, the effect sizes for those six RCTs are quite comparable to the post-training effect size estimated from our multiple linear regression model of −0.56 and from our general linear mixed effects model of −0.43.
The fourth important aspect of this study that warrants further mention involves the comparison of the on-site versus the at-home training effects in these interim analyses. For the two on-site Road Tour training groups, the effect size estimates from the multiple linear regression model were −0.457 and −0.585, while the effect size estimate for the at-home training group was −0.629. Thus, the effect size was largest for the at-home training group, although all three estimates are within the others' 95% CIs, reflecting their comparability. Therefore, the benefits that accrue from Road Tour training can be achieved using a home PC without supervision, which substantially increases the opportunity to implement speed of processing training in widespread public health interventions.
The final aspect of this study that warrants further mention involves the efficacy equivalence between the two age strata in these interim analyses. Among older adults (≥65 years old), the estimated effect size from the multiple linear regression analysis was −0.479, while it was −0.626 among younger adults (50–64 years old). Moreover, when an interaction term was added to the model in the pooled analysis, no statistical difference in these estimates was observed. This finding of equivalence in the efficacy of Road Tour between the age strata is extremely promising because it suggests that preventive interventions could focus on improving cognitive functioning at an earlier stage of age-related decline.
In conclusion, we note that although our study has numerous strengths, it does have limitations, four of which are worth mentioning. First, although large, the sample was drawn from just one FCC in which minorities were under-represented. Second, to be eligible, participants had to have a home computer and internet access. Third, only one of the five training programmes included in Posit Science's Insight suite (Road Tour) was studied. Finally, only data on the primary outcome were available and then only at randomisation and post-training. The first two of these limitations constrain the generalisability of the IHAMS somewhat, while the last two leave the issues of potential benefits from multifaceted training (using all five of the training programmes in the Insight suite) and the transferability to the five other neuropsychological outcomes unresolved.
Supplementary Material
Acknowledgments
The authors thank Christopher Goerdt, the Medical Director of the University of Iowa Family Care Center (FCC) General Medicine Clinic, and Steven Wolfe, the Medical Director of the FCC Family Medicine Clinic, who cosigned the letters to FCC patients inviting their participation in the study. The authors also acknowledge and applaud the 681 participants from the FCC general internal and family medicine clinics. Without their participation and support, this study would not have been possible. The authors also acknowledge the research assistants, work-study students and other support staff involved in the IHAMS.
Footnotes
To cite: Wolinsky FD, Vander Weg MW, Howren MB, et al. Interim analyses from a randomised controlled trial to improve visual processing speed in older adults: the Iowa Healthy and Active Minds Study. BMJ Open 2011;1:e000225. doi:10.1136/bmjopen-2011-000225
Funding: This study was supported by US National Institutes of Health grant RC1 AG-035546 to FDW.
Competing interests: The Road Tour computerised visual speed of processing intervention used in Iowa Healthy and Active Minds Study (IHAMS) is commercially available from Posit Science Corporation (San Francisco, California, USA). None of the members of the investigative team have any conflicts of interest or commitment involving Posit Science. Specifically, no one on the investigative team will financially profit in any way from the use of Road Tour. Posit Science acquired ownership in October 2007 of Ball and Roenker's original speed of processing intervention that was used in the multisite ACTIVE randomised controlled trial on which FDW was an original co-investigator (at the ACTIVE Indiana University site). In collaboration with Professors Ball and Roenker, Posit Science subsequently developed the second-generation value-added version of the visual speed of processing intervention known as Road Tour and used here in IHAMS. From December 2007 to March 2009, FDW had a limited part time consulting arrangement (15 days, total) with Posit Science to support additional analyses of the first 5 years of the ACTIVE follow-up data that had not been identified in the original ACTIVE protocols nor funded by the various US National Institutes of Health (NIH) grants supporting ACTIVE. This arrangement was approved in advance by the ACTIVE Executive Committee (which included the US NIH project officers) and was sanctioned by the Provost of the University of Iowa. After terminating that consulting arrangement with Posit Science, FDW applied in April 2009 for, and was awarded in September 2009 the US NIH Challenge Grant known as IHAMS. Posit Science provided the 700 copies of Road Tour used in IHAMS at no cost or obligation. Furthermore, in its letter of commitment to IHAMS and the US NIH, Posit Science stated should the results support the efficacy and effectiveness of Road Tour, they will ‘work with agencies at the federal government to make the programme available for wide-scale implementation at only a fraction of the current per-user cost’.
Patient consent: Consent forms approved by the University of Iowa IRB were used, and all subjects signed informed consent documents prior to participation.
Ethics approval: Ethics approval was provided by the University of Iowa Institutional Review Board (IRB-03; IRB protocol number 200908789), initially approved on 12 September 2009 and most recently re-approved on 18 May 2011.
Contributors: FDW is the principal investigator on the study, wrote the original proposal, supervised the trial, conducted all of the analyses and drafted the manuscript. MWVW is co-principal investigator on the study, collaborated on the original proposal, co-supervised the trial and reviewed the analyses reported here as well as the manuscript itself. MBH is a post-doctoral fellow working on the study, trained all of the interviewers, supervised the scoring of the neuropsychological tests and reviewed the manuscript. MPJ is the study biostatistician, devised the randomisation protocol, reviewed all the analyses and reviewed the manuscript. RM is a co-investigator on the study, collaborated on the original proposal, supervised preparation of all the ethics, consent and IRB documents, and reviewed the analyses and the manuscript. TML was a study research assistant who assisted with piloting the interview protocol, conducted randomisation interviews and reviewed the manuscript. KD is the study neuropsychologist, supervised selection of the neuropsychological tests, reviewed the psychometric analyses and reviewed the manuscript. MMD is the Project Coordinator, supervised all logistic operations, assisted in evaluating pilot interviews and revising procedures, conducted randomisation and 1-year follow-up interviews, drafted the exit interviews on the acceptability of the interventions, and reviewed the manuscript.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We plan to deposit a de-identified data set with the Inter-University Consortium for Political and Social Research (http://www.icpsr.umich.edu/icpsrweb/ICPSR/; ICPSR) on or before 1 December 2014. That date corresponds to a 3-year lag after the last interview has been completed. ICPSR is a standard repository for data sets made available for public use.
References
- 1.Birren JE, Woods AM, Williams MV. Behavioral slowing with age: causes, organization, and consequences of slowing. In: Poon LW, ed. Aging In The 1980s: Psychological Issues. Washington, DC: American Psychological Association, 1980:293–308 [Google Scholar]
- 2.Edwards JD, Wadley VG, Myers RS, et al. Transfer of a speed of processing intervention to near and far cognitive functions. Gerontol 2002;48:329–40 [DOI] [PubMed] [Google Scholar]
- 3.Madden DJ. Four to ten milliseconds per year: age-related slowing of visual word identification. J Gerontol 1992;47:P59–68 [DOI] [PubMed] [Google Scholar]
- 4.Roenker DL, Cissell GM, Ball KK, et al. Speed-of-processing and driving simulator training result in improved driving performance. Hum Factors 2003;45:218–33 [DOI] [PubMed] [Google Scholar]
- 5.Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res 2006;157:81–109 [DOI] [PubMed] [Google Scholar]
- 6.Greenwood PM. Functional plasticity in cognitive aging: review and hypothesis. Neuropsychol 2007;21:657–73 [DOI] [PubMed] [Google Scholar]
- 7.Hertzog C, Kramer AF, Wilson RS, et al. Enrichment effects on adult cognitive development: can the functional capacity of older adults be preserved and enhanced? Psychol Sci Pub Interest 2008;9:1–65 [DOI] [PubMed] [Google Scholar]
- 8.Salthouse TA. Consequences of age-related cognitive declines. Ann Rev Psychol 2012;63 In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salthouse TA. When does age-related cognitive decline begin? Neurobiol Aging 2009;30:507–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clay OJ, Edwards JD, Ross LA, et al. Visual function and cognitive speed of processing mediate age-related decline in memory span and fluid intelligence. J Aging Health 2009;21:547–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lemke U, Zimprich D. Longitudinal changes in memory performance and processing speed in old age. Aging Neuropsychol Cog 2005;12:57–77 [Google Scholar]
- 12.Zimprich DM. Can longitudinal changes in processing speed explain longitudinal changes in fluid intelligence? Psychol Aging 2002;17:690–5 [DOI] [PubMed] [Google Scholar]
- 13.Ball KK, Edwards JD, Ross LA. The impact of speed of processing training on cognitive and everyday functions. J Gerontol B Psychol Sci Soc Sci 2007;62B:19–31 [DOI] [PubMed] [Google Scholar]
- 14.Ball KK, Beard BL, Roenker DL, et al. Age and visual search: expanding the useful field of view. J Optic Soc Amer 1988;5:2210–19 [DOI] [PubMed] [Google Scholar]
- 15.Jobe JB, Smith DM, Ball KK, et al. ACTIVE: a cognitive intervention trial to promote independence in older adults. Controlled Clin Trials 2001;22:453–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ball KK, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA 2002;288:2271–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA 2006;296:2805–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolinsky FD, Mahncke HW, Kosinksi M, et al. The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Serv Res 2009;9:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolinsky FD, Unverzagt FW, Smith DM, et al. The effects of the ACTIVE cognitive training interventions on clinically relevant declines in health-related quality of life. J Gerontol B Psychol Sci Soc Sci 2006;61:S281–7 [DOI] [PubMed] [Google Scholar]
- 20.Wolinsky FD, Unverzagt FW, Smith DM, et al. The ACTIVE cognitive training trial and health-related quality of life: protection that lasts for five years. J Gerontol A Biol Sci Med Sci 2006;61A:1324–9 [DOI] [PubMed] [Google Scholar]
- 21.Wolinsky FD, Vander Weg MW, Martin R, et al. The effect of speed of processing training on depressive symptoms in ACTIVE. J Gerontol A Biol Sci Med Sci 2009;64:468–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolinsky FD, Mahncke HW, Vander Weg MW, et al. The ACTIVE cognitive training interventions and the onset of and recovery from suspected clinical depression. J Gerontol B Psychol Sci Soc Sci 2009;64:577–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolinsky FD, Mahncke HW, Vander Weg MW, et al. Speed of processing training improves self-rated health in older adults: enduring effects observed in the multi-site ACTIVE study. Int Psychogeriatr 2010;22:470–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolinsky FD, Vander Weg MW, Martin R, et al. Cognitive training improves internal locus of control among older adults. J Gerontol: Soc Sci 2010;65B:470–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolinsky FD, Vander Weg MW, Howren MB, et al. Protocol for a randomized controlled trial to improve cognitive functioning in older adults: the Iowa Healthy and Active Minds Study. BMJ Open 2011;1:e000218. doi:10.1136/bmjopen-2011-000218, pages 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pfeiffer EA. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23:433–41 [DOI] [PubMed] [Google Scholar]
- 27.Edwards JD, Vance DE, Wadley VG, et al. Reliability and validity of Useful Field of View test scores as administered by personal computer. J Clin Exper Neuropsychol 2005;27:529–43 [DOI] [PubMed] [Google Scholar]
- 28.Blom G. Statistical Estimates and Transformed Beta-Variables. New York, NY: Wiley, 1958 [Google Scholar]
- 29.Measley TM, Erickson S, Allison DB. Rank-based inverse normal transformations are increasingly used, but are they merited? Behav Genetics 2009;39:580–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kraja AT, Corbett J, Ping A, et al. Rheumatoid arthritis, item response theory, Blom transformation, and mixed models. BMC Proc 2007;1(Suppl 1):S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith A. Symbol Digit Modality Test. Los Angeles, CA: Western Psychological Services, 1982 [Google Scholar]
- 32.Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: Therapy and Clinical Interpretation. Tucson, AZ: Neuropsychological Press, 1985 [Google Scholar]
- 33.Benton AL, Hamsher K, Silvan AB. Multilingual Aphasia Examination. 3rd edn Iowa City, IA: AJA Associates, 1994 [Google Scholar]
- 34.Lewis R, Rennick PM. Manual for the Repeatable Cognitive-Perceptual-Motor Battery. Gross Point, MI: Axon, 1979 [Google Scholar]
- 35.Golden CJ. The Stroop Colour and Word Test. Chicago, IL: Stoelting Company, 1978 [Google Scholar]
- 36.McHorney CA, Ware JE, Raczek R. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31:247–63 [DOI] [PubMed] [Google Scholar]
- 37.Fox J. Applied Regression Analysis and Generalized Linear Models. 2nd edn Newberry Park, CA: Sage, 2008 [Google Scholar]
- 38.Salthouse TA. The processing-speed theory of adult age differences in cognition. Psychol Rev 1996;103:403–28 [DOI] [PubMed] [Google Scholar]
- 39.Salthouse TA. The paradox of cognitive change. J Clin Exper Neuropsychol 2010;332:622–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.