Abstract
Background
Mild cognitive impairment (MCI), a common condition among the elderly, is defined as a deterioration of memory, attention, and cognitive function that exceeds what would be expected for the individual’s age and level of education, yet does not interfere significantly with the activities of daily living. MCI may be a precursor of dementia; the rate of transition from MCI to dementia is 10% to 20% per year. The role of somatic diseases and modifiable risk factors in MCI and dementia needs further study.
Methods
We analyzed pertinent original articles and reviews published 1990 up to December 2010 that were retrieved by a selective search in PubMed and the Cochrane Library.
Results
MCI and dementia are associated with many somatic disorders and modifiable risk factors. MCI has biologically plausible associations with hypertension, diabetes mellitus, and hyperlipidemia, although the interventional trials performed to date have yielded negative results. Recently, chronic renal failure has also been recognized as a risk factor. Insufficient evidence supports a putative benefit on MCI from the substitution of vitamin B12, vitamin D, or testosterone (when these substances are deficient), the treatment of hyperhomocysteinemia or subclinical thyroid dysfunction, or hormone replacement therapy after menopause. Epidemiological data suggest that a Mediterranean diet, physical activity, and moderate alcohol consumption protect against MCI, while cigarette smoking promotes it and should be stopped.
Conclusion
Modifiable risk factors for MCI should be sought (at the very latest) in persons who already have MCI, as their optimal treatment may improve these patients’ cognitive performance or keep the existing deficits from progressing.
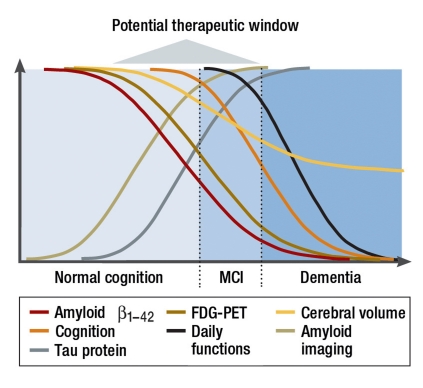
The number of persons affected by dementia is increasing. Therefore, the early detection of possible precursors of dementia and the diagnosis and treatment of modifiable risk factors are assuming increasing importance (1). A central part is played by the concept of mild cognitive impairment (MCI) (Box 1), because in many cases MCI, particularly the amnestic form (affecting memory), represents an early stage of Alzheimer-type dementia. In ca. 10% to 20% of patients with MCI, the mild impairments progress to manifest dementia in the space of 12 months (2). Despite its current pronounced heterogeneity, the concept of MCI permits timely identification of patients at high risk of developing dementia, thus opening a potentially larger therapeutic window and increasing the significance of modifiable risk factors (Figure 1). The importance of this becomes clear when one considers that, to date, all trials of antidementive drugs have had negative results (e1, e2). The data on MCI are sparse compared with dementia, and some studies have drawn no clear line between MCI and dementia or have used other terms (e.g., cognitive decline). The present study is therefore intended to provide an up-to-date overview of the common risk factors for MCI and dementia and of the (ideally prospective) interventional trials carried out to date.
Box 1. Definition of mild cognitive impairment (2, e2).
Absence of dementia
Signs of cognitive decline (medical history provided by doctor or patient)
Demonstration of cognitive disturbance
Ability to perform regular daily functions preserved; no more than minimal impairment of complex activities
Figure 1.
Changes in various parameters during development of dementia (modified from e91). This greatly simplified depiction of the development over time of biomarkers (decreasing levels of amyloid ß1–42 in cerebrospinal fluid, increase in level of tau protein in cerebrospinal fluid as indicator of neurofibrillary degeneration), the findings of nuclear medicine (PET amyloid imaging with increasing cerebral deposition of amyloid ß1–42, FDG-PET with changes in cerebral metabolism) and structural imaging (increasing atrophy on CT or MRI), and clinical symptoms (impairment of cognition and daily function) in patients with dementia clearly shows the importance of early diagnosis and treatment. MCI, mild cognitive impairment
To this end, we conducted a selective literature search of PubMed and the Cochrane Library using the terms “dementia”, “mild cognitive impairment”, and “cognitive decline” and analyzed pertinent original articles and reviews published between 1990 and December 2010.
“Classic” cardiovascular risk factors
Hypertension
Hypertension can lead to vascular-related cognitive impairment through any one of a number of mechanisms (arteriosclerosis, hypoperfusion, leukoaraiosis, cerebral infarction). Numerous cross-sectional analyses of the association between high blood pressure and cognitive impairment have yielded divergent results, while the majority of longitudinal studies have demonstrated an association (3). Seven large randomized, placebo-controlled interventional trials have been performed to date, with conflicting results (Table 1). Five studies revealed no protective action (e3– e7), while two showed a protective effect (e8, e9). The interpretation of these studies was severely restricted by methodological problems, and it is possible—as proposed in a recent Cochrane Review—that more precise results can be yielded only by a meta-analysis on the basis of individual patient data (4). The specific pharmacological mechanisms of action of the different antihypertensive agents could also play an important role.
Table 1. Summarized results of the major placebo-controlled studies on the effect of antihypertensive agents on cognitive impairments (modified from [e87]).
| Study | Number of participants | Age (years) | Inclusion criteria (systolic and diastolic blood pressure in mmHg) | Cognitive test | Observation time (years) | Antihypertensive treatment | Result/ effect on cognitive decline |
| MRC trial of hypertension (e3) | 4396 | 70.3 | Hypertension (syst. 160–209; diast. < 115) | Paired-Associate Learning Test, Trail-Making Test Part A | 4.5 | Hydrochlorothiazide | Not significant |
| + amiloride | |||||||
| or atenolol | |||||||
| Syst-Eur Trial (e8, e88) | 2418 | 69.9 | Isolated systolic hypertension (syst. 160–219; diast. < 95) | MMSE | 3.9 | Nitrendipine | HR 0,38 (95% CI 0.23–0.64) ARR 0.41% |
| ± enalapril | |||||||
| ± hydrochlorothiazide | |||||||
| SCOPE (e5) | 4964 | 76.4 | Hypertension (syst. 160–179; diast. 90–99) | MMSE | 3.7 | Candesartan | Not significant |
| ± hydrochlorothiazide | |||||||
| SHEP (e4) | 4736 | 71.6 | Isolated systolic hypertension (syst. 160–219; diast. < 90) | Short Care | 4.5 | Chlorthalidone | Not significant |
| ± atenolol | |||||||
| or reserpine | |||||||
| PROGRESS (e9) | 6105 | 64 | Stroke/TIA | MMSE | 3.9 | Perindopril | RRR 19% (95% CI 4–32%) ARR 0.95% |
| ± indapamide | |||||||
| HYVET-COG (e6) | 3336 | 83.5 | Hypertension (syst. 160–200; diast. < 110) | MMSE | 2.2 | Indapamide | HR 0,86 (95% CI 0.67–1.09) ARR 0.5% |
| ± perindopril | |||||||
| ONTARGET-TRANSCEND (e7) | 31546 | 66.5 | Atherosclerotic disease | MMSE | 3.7 | Telmisartan or ramipril or telmisartan | Not significant |
| + ramipril |
MMSE, Mini Mental Status Examination; HR, hazard ratio; CI, Confidence interval; ARR, absolute risk reduction; RRR, relative risk reduction; TIA, transient ischemic attack; MRC, Medical Research Council; Syst-Eur, Systolic Hypertension in Europe; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; PROGRESS, Perindopril Protection Against Recurrent Stroke Study; HYVET-COG, Hypertension in the Very Elderly Trial Cognitive Function Assessment; ONTARGET, ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial; TRANSCEND, Telmisartan Randomized AssessmeNt Study in ACE iNtolerant subjects with cardiovascular Disease
Diabetes mellitus
The existence of a causal link between diabetes mellitus and cognitive impairments is supported by numerous biochemical (e10, e11), imaging-related (e12, e13), and histopathological (e14) findings. A systematic review of 14 longitudinal studies reported an increased incidence of dementias, although it should be noted that there was often no adjustment for relevant confounding variables (e.g., hypertension or stroke) (5). Recent prospective studies that have taken account of these potential sources of error underline the possible importance of diabetes mellitus as an independent risk factor for cognitive decline (e15– e17). Longer duration of diabetes, lack of antidiabetic medication, and a higher number of hypoglycemic episodes were also associated with an increased risk of cognitive decline (e18– e20). A Cochrane Review in 2002 found no randomized studies investigating the link between the type of treatment for diabetes and the development of MCI or dementia (6). The only randomized study of antidiabetic medications published in the intervening period showed no influence on cognitive performance in mild dementia (e21).
Hyperlipidemia
As early as 2003, autopsy studies described an association between cerebral amyloid deposits and hypercholesterolemia (e22). Large population-based studies then revealed that hyperlipidemia and particularly hypercholesterolemia in middle age are associated with the risk of subsequent occurrence of MCI (e23– e25). In contrast, studies of older subjects (>65 years) showed no association between hypercholesterolemia and cognitive decline (e26– e28). The findings of the majority of prospective observational studies suggested a protective connection between statin intake and cognitive impairment (e25, e29, e30). The Rotterdam Study, for example, with 6992 participants and a mean observation period of 9 years, found that the risk of developing Alzheimer-type dementia was reduced by almost half in those taking statins (hazard ratio [HR] 0.57; 95% confidence interval [CI] 0.37–0.90). This effect was independent of the type of statin but specific to statins, in that other cholesterol-lowering drugs (fibrate, nicotinic acid) showed no such influence (e31). However, two large placebo-controlled trials of persons at high risk of vascular disease did not demonstrate a similar association. Neither the Heart Protection Study (HPS; simvastatin, >20 000 participants, age 40–80 years, observation period 5 years) nor the Pravastatin in Elderly Individuals at Risk of Vascular Disease (PROSPER) trial (pravastatin, almost 6000 participants, age 70–82 years, observation period 3 years) showed a protective effect of statins with regard to cognitive decline. This finding was confirmed by the Cochrane Review based on HPS and PROSPER (7– 9). These negative results may possibly be explained by the fact that neither trial was designed primarily to record cognitive impairments, so there was no baseline assessment of cognitive performance. Any effect of statin intake was therefore not measurable (e32). Furthermore, the age range in the HPS was so wide, encompassing middle-aged as well as elderly persons, that the age-dependent influence of cholesterol may have been neutralized. Moreover, recent findings point to differences in the individual fractions of cholesterol. In analogy to coronary heart disease, a high proportion of HDL cholesterol may have a protective function (e33), and future statin studies should take this into account.
Metabolic factors
Chronic renal failure
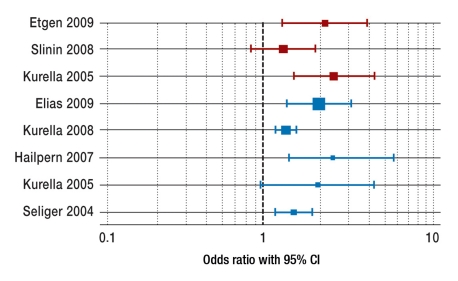
Chronic renal failure represents a new independent risk factor for cognitive decline. Apart from the usual risk factors, other disorders arising in the context of renal failure (e.g., hyperhomocysteinemia, coagulation disorders, inflammation, anemia) may play a part (10). Almost all cross-sectional studies (Figure 2) have demonstrated an increased risk for development of a cognitive impairment, in some cases dependent on the severity of the chronic renal failure (e34– e38). Most longitudinal studies (Figure 2) have confirmed the association between chronic renal failure and cognitive decline, which has been found even in patients with only mild or moderate restriction of renal function (e39– e42). Unfortunately no specific treatment options have yet been identified. For example, high doses of folic acid, vitamin B6 and vitamin B12 for reduction of the elevated homocysteine concentration in patients with chronic renal failure (see below, “Hyperhomocysteinemia”) had no effect on cognition (11).
Figure 2.
The association between chronic renal failure and cognitive impairment: findings of large (> 900 participants) cross-sectional (blue) and longitudinal (red) studies. CI, Confidence interval
Vitamin B12 deficiency
The prevalence of vitamin B12 deficiency increases with age (up to 20% in those over 75 years) (e43), and this could play a significant part in cognitive impairments (e44). Although both cross-sectional and longitudinal studies have shown an association between vitamin B12 deficiency and the development of MCI (e45, e46), none of the randomized double-blind placebo-controlled trials conducted to date have demonstrated a positive effect of vitamin B12 substitution on cognitive status (12– 14).
Vitamin D deficiency
The prevalence of vitamin D deficiency increases to as much as 50% with age, due to reduced sun exposure, reduced vitamin D generation and lower oral intake (e47). Vitamin D plays a part in the synthesis of neurotrophic factors and neurotransmitters (e48) and in receptor regulation in memory-relevant regions of the brain (e49). The results of large cross-sectional studies are inconsistent. No association between low levels of vitamin D and cognitive function was revealed by the 4809 elderly participants in the National Health and Nutrition Examination Survey (NHANES III) (e50). In contrast, three other large studies found that the risk of cognitive impairment was approximately doubled in persons with low vitamin D concentrations (e51– e53). The only large prospective cohort study conducted to date demonstrated no association between vitamin D level and cognitive impairment (15); the study was limited to men, however, and at 20 ng/mL the threshold value for vitamin D deficiency was unusually high.
Hyperhomocysteinemia
Although the level of homocysteine rises with age and with decreasing renal function, it is determined mainly by the nutritional intake or serum concentrations of vitamin B6, vitamin B12, and folic acid. Most of the small cross-sectional studies have demonstrated an association between increased homocysteine concentration and cognitive impairment, but longitudinal studies show inconsistent results (10). The double-blind, randomized, placebo-controlled trials conducted to date have found no clear-cut improvement in cognitive performance despite effective reduction of homocysteine by administration of vitamin B12 and folic acid (16). Another study, however, showed delayed cerebral atrophy in persons with MCI (e54). The problems with these studies include a short study period (≤12 weeks), different homocysteine threshold values, and inhomogeneous study populations (with or without dementia). Sub-study analyses indicate a possible effect in healthy elderly persons with very high levels of homocysteine (16).
Endocrine factors
Testosterone deficiency
Cross-sectional studies on the connection between testosterone deficiency and MCI have had inconsistent results (17). Small studies of patients with testosterone deficiency caused by drug treatment or surgery have found such an association, and in some cases the effect was reversible (e55, e56). The results of the randomized placebo-controlled trials conducted to date on the effect of testosterone substitution are contradictory. However, comparison is hampered by methodological factors (e.g., low numbers of participants [<50 men], variation in type and duration of testosterone administration, and differences in cognitive testing) (17, 18) (Box 2). Testosterone substitution for prevention of cognitive decline is therefore not generally recommended but can be considered after exclusion of other causes and regular urological follow-up in patients with acquired hypogonadism (usually with serum concentration <8–12 nmol/L) and cognitive impairment (e57, e58).
Box 2. Frequent methodological problems.
Different procedures for testing cognition
Varying inclusion criteria
High proportion of actively treated persons in placebo arm of study
High discontinuation rates
Short observation period
Varying clinical endpoints
Inadequate consideration of covariates (e.g., education level, social support)
Subclinical thyroid dysfunction
Manifest dysfunction of the thyroid gland (hypo- or hyperthyroidism) is one of the potentially reversible causes of dementia, so subclinical thyroid dysfunction could play a part in MCI. The prevalence of subclinical hypothyroidism (elevated TSH in the presence of normal thyroxine [T4] and triiodothyronine [T3]) rises with increasing age (>25% in persons over 60) (e59). Early small studies reported an association between cognitive impairment and subclinical hypothyroidism, and in some cases cognitive performance improved after substitution (e60, e61). Subsequent larger or prospective studies have not confirmed this association to date (e62– e64). The prevalence of subclinical hyperthyroidism (low TSH with normal T3 and T4) also increases with age (reaching 7–8% in regions of iodine deficiency) (e63, e65). Two investigations showed that the risk of cognitive impairment was 2 to 3 times higher than normal in the presence of subclinical hyperthyroidism (e66, e67), while another study that took numerous parameters into account found no association (e63).
Estrogens
In animal experiments and cell cultures, estrogens exert a neuroprotective effect by favoring neuronal sprouting, by reducing cerebral amyloid, and by virtue of their anti-inflammatory properties (e68, e69). The results of early cross-sectional analyses were encouraging, but prospective studies showed no positive influence of estrogen administration on cognitive performance. Large randomized placebo-controlled trials demonstrated that postmenopausal hormone replacement therapy increases the risk of developing dementia and does not hinder the development of MCI; purely estrogen-based hormone replacement therapy (without progesterone) actually raises the risk of developing MCI (19, e70, e71). Many different variables may affect the results, e.g., varying age groups, type of menopause (natural or postoperative), mode of substitution (transdermal, oral, or intramuscular), and timing of substitution (time elapsed since menopause, duration) (19, e72, e73). A possible beneficial effect of purely estrogen-based hormone replacement therapy on verbal retentiveness in women under 65 has been discussed (e74), but otherwise hormone replacement therapy should not be administered with the aim of preserving cognitive skills.
Lifestyle factors
Diet
A Mediterranean diet (a high proportion of fish, fruit, vegetables, cereals, and unsaturated fatty acids and a low proportion of dairy products, meat, and saturated fatty acids) could potentially exert a protective effect with regard to cognitive decline via improved carbohydrate metabolism coupled with antioxidative and anti-inflammatory mechanisms (e75).
The only two prospective cohort studies carried out to date differed in some aspects of study design (observation period, composition of diet, etc.), but agreed in suggesting a dose-dependent protective effect of a Mediterranean diet (e76). An American study of 1393 persons with initially normal cognitive function found a 28% reduction in the risk of MCI after 4.5 years among those with a high proportion of Mediterranean-style diet (20). A Cochrane Review of the value of omega-3 fatty acids in the prevention of dementia published in 2006 found insufficient evidence because of the lack of randomized trials at that time.
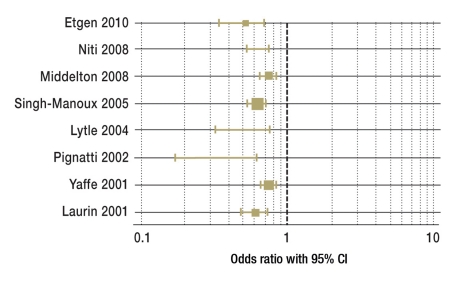
Physical activity
Various mechanisms (reduction of cardiovascular diseases, improved cerebral perfusion, induction of cortical angiogenesis, etc.) have been discussed for the postulated neuroprotective effect of physical activity. Recent cohort studies (Figure 3) have revealed an association between regular exercise and a considerable reduction in the risk of developing MCI (e77– e84). A new meta-analysis of 15 prospective cohort studies embracing a total of 33 816 persons without dementia shows that both intense and moderate exercise reduce the risk of the occurrence of MCI by at least 35% (22). Various interventional trials in recent years have confirmed this effect; however, the numbers of participants were low (<150) and the observation times short (≤1 year) (23). Larger interventional trials are now under way, so more precise recommendations can be expected. It is already clear, however, that not all types of physical activity are suitable; boxing, for example, increases the risk of cognitive impairment (e85).
Figure 3.
The association between exercise and cognitive impairment: findings of large studies (> 1000 participants). CI, Confidence interval
Alcohol consumption
The neurotoxic action of alcohol, exerted via accelerated cerebral atrophy and reduced acetylcholine synthesis, has been clearly confirmed (24). After numerous cohort studies had shown no unambiguous relationship between alcohol consumption and cognitive impairment, the majority of prospective trials revealed a dose-dependent (J- or U-shaped) effect (24). Most investigators report that low (often defined as <12 g of alcohol/day, 0.1 L wine or one glass of beer) to moderate alcohol consumption has a protective influence on cognitive performance. In contrast, a detrimental effect is described for high consumption of alcohol (e75). However, the available data do not permit definitive conclusions with regard to a causal connection. Furthermore, important details (type of alcoholic drink, amount and duration of consumption) have been insufficiently reported.
Smoking
Nicotine, a cholinergic agonist, could counteract the cholinergic dysfunction in cognitive impairment (e86). In contrast, however, cohort studies have indicated a pronounced increase in risk (24). A meta-analysis of 19 prospective studies with a total of 26 374 participants reported that the risk of developing dementia was up to 70% higher in current smokers than in non-smokers (e87). This increase in risk has also been described in recent studies with MCI as endpoint (25). Interpretation of the results is limited by the fact that some studies display deficiencies in the definition and classification of nicotine consumption (amount consumed, duration of consumption/abstinence, passive smoking).
Conclusion
The results of recent studies confirm that the symptoms and course of MCI and dementia can be influenced by somatic illnesses and other modifiable risk factors (Table 2), although the current data originate largely from not entirely conclusive cross-sectional or longitudinal studies. Despite the current lack of positive interventional trials, we are of the opinion that an association with the classic cardiovascular risk factors—hypertension, diabetes mellitus, and hyperlipidemia—is biologically plausible. Measures to ameliorate these factors would simultaneously represent effective prevention of other vascular diseases (myocardial infarction, stroke). In recent years renal failure has also been identified as a somatic risk factor, though no evidence-based treatment strategies have yet emerged. With regard to MCI, the current data do not support the general recommendation of substitution therapy in the case of vitamin B12, vitamin D, or testosterone deficiency, hyperhomocysteinemia, or subclinical thyroid dysfunction. Purely estrogen-based hormone replacement therapy can be contemplated for improvement of verbal retentiveness in women under 65 after careful consideration of potential contraindications, but no other postmenopausal hormone replacement therapy should be given. Epidemiological data indicate a protective action of Mediterranean diet, physical activity, and moderate alcohol consumption, so these can be encouraged or— in the case of alcohol consumption—tolerated. Smoking increases the risk of developing MCI and should be stopped.
Table 2. Modifiable risk factors for mild cognitive impairment and dementia, and recommendation classes for treatment (e89).
| Somatic factor | Change in risk (OR or HR) | Likelihood of relevance | Treatment | Recommendation class*1 |
| Hypertension | 1.24–1.59 (HR) | Probable | Blood pressure reduction | U |
| Diabetes mellitus | 1.34–1.63 (OR) | Certain | Normoglycemia | U |
| Hyperlipidemia | 1.42–1.90 (HR) | Possible | Early treatment | U |
| Chronic renal failure | 1.32–2.43 (OR) | Certain | Optimization | U |
| Vitamin B12 deficiency | 1.50–2.17 (OR) | Unlikely | No substitution | B |
| Vitamin D deficiency | NS-2.3 (OR) | Questionable | No substitution | B |
| Hyperhomocysteinemia | Inconsistent | Unlikely | No substitution | A |
| Testosterone deficiency | Inconsistent | Possible | Substitution in individual cases | C |
| Subclinical thyroid gland dysfunction | Inconsistent | Questionable | No substitution | B |
| Hormone replacement therapy | 1.05–2.05 (HR) | Unlikely | No substitution | A |
| Mediterranean diet | 0.72–1.04 (HR) | Probable | Recommended | B |
| Physical activity | 0.62–0.65 (HR) | Probable | Recommended | B |
| Nicotine consumption | 1.27–1.79 (HR) | Probable | Stop | B |
| Alcohol consumption | 0.28–0.82 (OR) | Possible | Slight to moderate consumption tolerated | B |
The change in risk (as reported in the most important studies) is described in terms of the odds ratio (OR) or hazard ratio (HR). A value > 1.0 shows an increase in risk; a value < 1.0, a reduction in risk. NS, non-significant results;
*1classification of recommendation classes: A, high recommendation based on strong evidence, or on weak evidence with particularly high relevance to patient care; B, moderate recommendation based on moderate evidence, or on weak evidence with high relevance to patient care; C, restricted recommendation based on weak evidence, or on strong evidence with limited relevance to patient care; U, inadequate data, treatment not yet evidence-based
Key Messages.
Mild cognitive impairment and dementia can be influenced by modifiable factors (e.g., Mediterranean diet and physical activity).
Despite the negative results of interventional trials, there is a biologically plausible association with the classic cardiovascular risk factors of hypertension, diabetes mellitus, and hyperlipidemia, so we favor early treatment and optimization.
Chronic renal failure is a newly discovered somatic risk factor, for which no treatment with specific regard to cognitive decline has yet been evaluated.
With regard to mild cognitive impairment, substitution therapy cannot be generally recommended for vitamin B12, vitamin D, or testosterone deficiency, hyperhomocysteinemia, or subclinical thyroid dysfunction; similarly, postmenopausal hormone replacement therapy should generally not be prescribed.
Mediterranean diet and physical activity seem to protect against cognitive decline and should be recommended. Low to moderate alcohol consumption can be tolerated, but smoking should be stopped.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Förstl has received funding from Eisai, General Electric Lundbeck, Pfizer, Merz Janssen, Novartis, AstraZeneca, BMS, GSK, Lilly, Nutricia, Sanofi-Aventis, Schwabe, Servier, and other companies.
Dr. Bickel has received honoraria from Willmar Schwabe.
The remaining authors declare that no conflicts of interest exist.
References
- 1.Förstl H, Bickel H, Frölich L, et al. MCI-plus: leichte kognitive Beeinträchtigung mit rascher Progredienz. Teil I: Prävention und Therapie. Dtsch Med Wochenschr. 2009;134:39–44. doi: 10.1055/s-0028-1105890. [DOI] [PubMed] [Google Scholar]
- 2.Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment–beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 3.Birns J, Kalra L. Cognitive function and hypertension. J Hum Hypertens. 2009;23:86–96. doi: 10.1038/jhh.2008.80. [DOI] [PubMed] [Google Scholar]
- 4.McGuinness B, Todd S, Passmore P, Bullock R. Blood pressure lowering in patients without prior cerebrovascular disease for prevention of cognitive impairment and dementia. Cochrane Database Syst Rev. 2009;4 doi: 10.1002/14651858.CD004034.pub3. CD004034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006;5:64–74. doi: 10.1016/S1474-4422(05)70284-2. [DOI] [PubMed] [Google Scholar]
- 6.Areosa SA, Grimley EV. Effect of the treatment of Type II diabetes mellitus on the development of cognitive impairment and dementia. Cochrane Database Syst Rev. 2002;4 doi: 10.1002/14651858.CD003804. CD003804. [DOI] [PubMed] [Google Scholar]
- 7.McGuinness B, Craig D, Bullock R, Passmore P. Statins for the prevention of dementia. Cochrane Database Syst Rev. 2009;2 doi: 10.1002/14651858.CD003160.pub2. CD003160. [DOI] [PubMed] [Google Scholar]
- 8.Group HPSC. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 9.Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–1630. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 10.Etgen T, Bickel H, Förstl H. Metabolic and endocrine factors in mild cognitive impairment. Ageing Res Rev. 2010;9:280–288. doi: 10.1016/j.arr.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Brady CB, Gaziano JM, Cxypoliski RA, et al. Homocysteine lowering and cognition in CKD: the Veterans Affairs homocysteine study. Am J Kidney Dis. 2009;54:440–449. doi: 10.1053/j.ajkd.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seal EC, Metz J, Flicker L, Melny J. A randomized, double-blind, placebo-controlled study of oral vitamin B12 supplementation in older patients with subnormal or borderline serum vitamin B12 concentrations. J Am Geriatr Soc. 2002;50:146–151. doi: 10.1046/j.1532-5415.2002.50020.x. [DOI] [PubMed] [Google Scholar]
- 13.van Uffelen JG, Chinapaw MJ, van Mechelen W, Hopman-Rock M. Walking or vitamin B for cognition in older adults with mild cognitive impairment? A randomised controlled trial. Br J Sports Med. 2008;42:344–351. doi: 10.1136/bjsm.2007.044735. [DOI] [PubMed] [Google Scholar]
- 14.Aisen PS, Schneider LS, Sano M, et al. High-dose B vitamin supplementation and cognitive decline in Alzheimer disease: a randomized controlled trial. JAMA. 2008;300:1774–1783. doi: 10.1001/jama.300.15.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slinin Y, Paudel ML, Taylor BC, et al. 25-Hydroxyvitamin D levels and cognitive performance and decline in elderly men. Neurology. 2010;74:33–41. doi: 10.1212/WNL.0b013e3181c7197b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malouf R, Grimley Evans J. Folic acid with or without vitamin B12 for the prevention and treatment of healthy elderly and demented people. Cochrane Database Syst Rev. 2008;4 doi: 10.1002/14651858.CD004514.pub2. CD004514. [DOI] [PubMed] [Google Scholar]
- 17.Warren MF, Serby MJ, Roane DM. The effects of testosterone on cognition in elderly men: a review. CNS Spectr. 2008;13:887–897. doi: 10.1017/s1092852900016990. [DOI] [PubMed] [Google Scholar]
- 18.Beauchet O. Testosterone and cognitive function: current clinical evidence of a relationship. Eur J Endocrinol. 2006;155:773–781. doi: 10.1530/eje.1.02306. [DOI] [PubMed] [Google Scholar]
- 19.Lethaby A, Hogervorst E, Richards M, Yesufu A, Yaffe K. Hormone replacement therapy for cognitive function in postmenopausal women. Cochrane Database Syst Rev. 2008;1 doi: 10.1002/14651858.CD003122.pub2. CD003122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scarmeas N, Stern Y, Mayeux R, et al. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66:216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lim WS, Gammack JK, Van Niekerk J, Dangour AD. Omega 3 fatty acid for the prevention of dementia. Cochrane Database Syst Rev. 2006;1 doi: 10.1002/14651858.CD005379.pub2. CD005379. [DOI] [PubMed] [Google Scholar]
- 22.Sofi F, Valecchi D, Bacci D, et al. Physical activity and risk of cognitive decline: a meta-analysis of prospective studies. J Intern Med. 2010;269:107–117. doi: 10.1111/j.1365-2796.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- 23.Lautenschlager NT, Cox KL, Flicker L, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- 24.Bickel H. Rauchen und Alkoholkonsum als Risikofaktoren einer Demenz im Alter. Sucht. 2006;52:48–59. [Google Scholar]
- 25.Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Impact of cardiovascular risk factors on cognitive function: The Tromso study. Eur J Neurol. 2011;18:737–743. doi: 10.1111/j.1468-1331.2010.03263.x. [DOI] [PubMed] [Google Scholar]
- e1.Schneider LS, Insel PS, Weiner MW. Treatment with cholinesterase inhibitors and memantine of patients in the Alzheimer’s Disease Neuroimaging Initiative. Arch Neurol. 2011;68:58–66. doi: 10.1001/archneurol.2010.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e2.Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447–1455. doi: 10.1001/archneurol.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e3.Prince MJ, Bird AS, Blizard RA, Mann AH. Is the cognitive function of older patients affected by antihypertensive treatment? Results from 54 months of the Medical Research Council’s trial of hypertension in older adults. BMJ. 1996;312:801–805. doi: 10.1136/bmj.312.7034.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e4.Applegate WB, Pressel S, Wittes J, et al. Impact of the treatment of isolated systolic hypertension on behavioral variables. Results from the systolic hypertension in the elderly program. Arch Intern Med. 1994;154:2154–2160. [PubMed] [Google Scholar]
- e5.Lithell H, Hansson L, Skoog I, et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21:875–886. doi: 10.1097/00004872-200305000-00011. [DOI] [PubMed] [Google Scholar]
- e6.Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7:683–689. doi: 10.1016/S1474-4422(08)70143-1. [DOI] [PubMed] [Google Scholar]
- e7.Anderson C, Teo K, Gao P, et al. Renin-angiotensin system blockade and cognitive function in patients at high risk of cardiovascular disease: analysis of data from the ONTARGET and TRANSCEND studies. Lancet Neurol. 2011;10:43–53. doi: 10.1016/S1474-4422(10)70250-7. [DOI] [PubMed] [Google Scholar]
- e8.Forette F, Seux ML, Staessen JA, et al. Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet. 1998;352:1347–1351. doi: 10.1016/s0140-6736(98)03086-4. [DOI] [PubMed] [Google Scholar]
- e9.Tzourio C, Anderson C, Chapman N, et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med. 2003;163:1069–1075. doi: 10.1001/archinte.163.9.1069. [DOI] [PubMed] [Google Scholar]
- e10.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- e11.Farris W, Mansourian S, Chang Y, et al. Insulin-degrading enzyme regulates the levels of insulin, amyloid beta-protein, and the beta-amyloid precursor protein intracellular domain in vivo. Proc Natl Acad Sci USA. 2003;100:4162–4167. doi: 10.1073/pnas.0230450100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e12.den Heijer T, Vermeer SE, van Dijk EJ, et al. Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI. Diabetologia. 2003;46:1604–1610. doi: 10.1007/s00125-003-1235-0. [DOI] [PubMed] [Google Scholar]
- e13.Biessels GJ, Koffeman A, Scheltens P. Diabetes and cognitive impairment. Clinical diagnosis and brain imaging in patients attending a memory clinic. J Neurol. 2006;253:477–482. doi: 10.1007/s00415-005-0036-4. [DOI] [PubMed] [Google Scholar]
- e14.Sonnen JA, Larson EB, Brickell K, et al. Different patterns of cerebral injury in dementia with or without diabetes. Arch Neurol. 2009;66:315–322. doi: 10.1001/archneurol.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e15.Gregg EW, Yaffe K, Cauley JA, et al. Is diabetes associated with cognitive impairment and cognitive decline among older women? Study of Osteoporotic Fractures Research Group. Arch Intern Med. 2000;160:174–180. doi: 10.1001/archinte.160.2.174. [DOI] [PubMed] [Google Scholar]
- e16.Yaffe K, Blackwell T, Kanaya AM, et al. Diabetes, impaired fasting glucose, and development of cognitive impairment in older women. Neurology. 2004;63:658–663. doi: 10.1212/01.wnl.0000134666.64593.ba. [DOI] [PubMed] [Google Scholar]
- e17.Luchsinger JA, Reitz C, Patel B, et al. Relation of diabetes to mild cognitive impairment. Arch Neurol. 2007;64:570–575. doi: 10.1001/archneur.64.4.570. [DOI] [PubMed] [Google Scholar]
- e18.Logroscino G, Kang JH, Grodstein F. Prospective study of type 2 diabetes and cognitive decline in women aged 70-81 years. BMJ. 2004;328 doi: 10.1136/bmj.37977.495729.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e19.Okereke OI, Kang JH, Cook NR, et al. Type 2 diabetes mellitus and cognitive decline in two large cohorts of community-dwelling older adults. J Am Geriatr Soc. 2008;56:1028–1036. doi: 10.1111/j.1532-5415.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- e20.Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP, Jr, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009;301:1565–1572. doi: 10.1001/jama.2009.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e21.Gold M, Alderton C, Zvartau-Hind M, et al. Rosiglitazone monotherapy in mild-to-moderate alzheimer’s disease: results from a randomized, double-blind, placebo-controlled phase III study. Dement Geriatr Cogn Disord. 2010;30:131–146. doi: 10.1159/000318845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e22.Pappolla MA, Bryant-Thomas TK, Herbert D, et al. Mild hypercholesterolemia is an early risk factor for the development of Alzheimer amyloid pathology. Neurology. 2003;61:199–205. doi: 10.1212/01.wnl.0000070182.02537.84. [DOI] [PubMed] [Google Scholar]
- e23.Kivipelto M, Helkala EL, Hanninen T, et al. Midlife vascular risk factors and late-life mild cognitive impairment: A population-based study. Neurology. 2001;56:1683–1689. doi: 10.1212/wnl.56.12.1683. [DOI] [PubMed] [Google Scholar]
- e24.Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005;64:277–281. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- e25.Dufouil C, Richard F, Fievet N, et al. APOE genotype, cholesterol level, lipid-lowering treatment, and dementia: the Three-City Study. Neurology. 2005;64:1531–1538. doi: 10.1212/01.WNL.0000160114.42643.31. [DOI] [PubMed] [Google Scholar]
- e26.Solfrizzi V, Panza F, Colacicco AM, et al. Vascular risk factors, incidence of MCI, and rates of progression to dementia. Neurology. 2004;63:1882–1891. doi: 10.1212/01.wnl.0000144281.38555.e3. [DOI] [PubMed] [Google Scholar]
- e27.Li G, Shofer JB, Kukull WA, et al. Serum cholesterol and risk of Alzheimer disease: a community-based cohort study. Neurology. 2005;65:1045–1050. doi: 10.1212/01.wnl.0000178989.87072.11. [DOI] [PubMed] [Google Scholar]
- e28.Reitz C, Tang MX, Luchsinger J, Mayeux R. Relation of plasma lipids to Alzheimer disease and vascular dementia. Arch Neurol. 2004;61:705–714. doi: 10.1001/archneur.61.5.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e29.Wolozin B, Kellman W, Ruosseau P, Celesia GG, Siegel G. Decreased prevalence of Alzheimer disease associated with 3-hydroxy-3-methyglutaryl coenzyme A reductase inhibitors. Arch Neurol. 2000;57:1439–1443. doi: 10.1001/archneur.57.10.1439. [DOI] [PubMed] [Google Scholar]
- e30.Jick H, Zornberg GL, Jick SS, Seshadri S, Drachman DA. Statins and the risk of dementia. Lancet. 2000;356:1627–1631. doi: 10.1016/s0140-6736(00)03155-x. [DOI] [PubMed] [Google Scholar]
- e31.Haag MD, Hofman A, Koudstaal PJ, Stricker BH, Breteler MM. Statins are associated with a reduced risk of Alzheimer disease regardless of lipophilicity. The Rotterdam Study. J Neurol Neurosurg Psychiatry. 2009;80:13–17. doi: 10.1136/jnnp.2008.150433. [DOI] [PubMed] [Google Scholar]
- e32.Sparks L. Statins and cognitive function. J Neurol Neurosurg Psychiatry. 2009;80:1–2. doi: 10.1136/jnnp.2008.160291. [DOI] [PubMed] [Google Scholar]
- e33.Reitz C, Tang MX, Schupf N, et al. Association of higher levels of high-density lipoprotein cholesterol in elderly individuals and lower risk of late-onset Alzheimer disease. Arch Neurol. 2010;67:1491–1497. doi: 10.1001/archneurol.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e34.Seliger SL, Siscovick DS, Stehman-Breen CO, et al. Moderate renal impairment and risk of dementia among older adults: the Cardiovascular Health Cognition Study. J Am Soc Nephrol. 2004;15:1904–1911. doi: 10.1097/01.asn.0000131529.60019.fa. [DOI] [PubMed] [Google Scholar]
- e35.Kurella M, Yaffe K, Shlipak MG, Wenger NK, Chertow GM. Chronic kidney disease and cognitive impairment in menopausal women. Am J Kidney Dis. 2005;45:66–76. doi: 10.1053/j.ajkd.2004.08.044. [DOI] [PubMed] [Google Scholar]
- e36.Hailpern SM, Melamed ML, Cohen HW, Hostetter TH. Moderate chronic kidney disease and cognitive function in adults 20 to 59 years of age: Third National Health and Nutrition Examination Survey (NHANES III) J Am Soc Nephrol. 2007;18:2205–2213. doi: 10.1681/ASN.2006101165. [DOI] [PubMed] [Google Scholar]
- e37.Kurella Tamura M, Wadley V, Yaffe K, et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2008;52:227–234. doi: 10.1053/j.ajkd.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e38.Elias MF, Elias PK, Seliger SL, et al. Chronic kidney disease, creatinine and cognitive functioning. Nephrol Dial Transplant. 2009;24:2446–2452. doi: 10.1093/ndt/gfp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e39.Kurella M, Chertow GM, Fried LF, et al. Chronic kidney disease and cognitive impairment in the elderly: the health, aging, and body composition study. J Am Soc Nephrol. 2005;16:2127–2133. doi: 10.1681/ASN.2005010005. [DOI] [PubMed] [Google Scholar]
- e40.Etgen T, Sander D, Chonchol M, et al. Chronic kidney disease is associated with incident cognitive impairment in the elderly: the INVADE study. Nephrol Dial Transplant. 2009;24:3144–3150. doi: 10.1093/ndt/gfp230. [DOI] [PubMed] [Google Scholar]
- e41.Khatri M, Nickolas T, Moon YP, et al. CKD associates with cognitive decline. J Am Soc Nephrol. 2009;20:2427–2432. doi: 10.1681/ASN.2008101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e42.Buchman AS, Tanne D, Boyle PA, et al. Kidney function is associated with the rate of cognitive decline in the elderly. Neurology. 2009;73:920–927. doi: 10.1212/WNL.0b013e3181b72629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e43.Clarke R, Refsum H, Birks J, et al. Screening for vitamin B-12 and folate deficiency in older persons. Am J Clin Nutr. 2003;77:1241–1247. doi: 10.1093/ajcn/77.5.1241. [DOI] [PubMed] [Google Scholar]
- e44.Troen AM, Shea-Budgell M, Shukitt-Hale B, et al. B-vitamin deficiency causes hyperhomocysteinemia and vascular cognitive impairment in mice. Proc Natl Acad Sci U S A. 2008;105:12474–12479. doi: 10.1073/pnas.0805350105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e45.Hin H, Clarke R, Sherliker P, et al. Clinical relevance of low serum vitamin B12 concentrations in older people: the Banbury B12 study. Age Ageing. 2006;35:416–422. doi: 10.1093/ageing/afl033. [DOI] [PubMed] [Google Scholar]
- e46.Clarke R, Birks J, Nexo E, et al. Low vitamin B-12 status and risk of cognitive decline in older adults. Am J Clin Nutr. 2007;86:1384–1391. doi: 10.1093/ajcn/86.5.1384. [DOI] [PubMed] [Google Scholar]
- e47.van der Wielen RP, Lowik MR, van den Berg H, et al. Serum vitamin D concentrations among elderly people in Europe. Lancet. 1995;346:207–210. doi: 10.1016/s0140-6736(95)91266-5. [DOI] [PubMed] [Google Scholar]
- e48.Garcion E, Wion-Barbot N, Montero-Menei CN, Berger F, Wion D. New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab. 2002;13:100–105. doi: 10.1016/s1043-2760(01)00547-1. [DOI] [PubMed] [Google Scholar]
- e49.Brewer LD, Thibault V, Chen KC, et al. Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J Neurosci. 2001;21:98–108. doi: 10.1523/JNEUROSCI.21-01-00098.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e50.McGrath J, Scragg R, Chant D, et al. No association between serum 25-hydroxyvitamin D3 level and performance on psychometric tests in NHANES III. Neuroepidemiology. 2007;29:49–54. doi: 10.1159/000108918. [DOI] [PubMed] [Google Scholar]
- e51.Llewellyn DJ, Langa KM, Lang IA. Serum 25-hydroxyvitamin d concentration and cognitive impairment. J Geriatr Psychiatry Neurol. 2009;22:188–195. doi: 10.1177/0891988708327888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e52.Lee DM, Tajar A, Ulubaev A, et al. Association between 25-hydroxyvitamin D levels and cognitive performance in middle-aged and older European men. J Neurol Neurosurg Psychiatry. 2009;80:722–729. doi: 10.1136/jnnp.2008.165720. [DOI] [PubMed] [Google Scholar]
- e53.Annweiler C, Schott AM, Allali G, et al. Association of vitamin D deficiency with cognitive impairment in older women: cross-sectional study. Neurology. 2010;74:27–32. doi: 10.1212/WNL.0b013e3181beecd3. [DOI] [PubMed] [Google Scholar]
- e54.Smith AD, Smith SM, de Jager CA, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PLoS One. 2010;5(9) doi: 10.1371/journal.pone.0012244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e55.Beer TM, Bland LB, Bussiere JR, et al. Testosterone loss and estradiol administration modify memory in men. J Urol. 2006;175:130–135. doi: 10.1016/S0022-5347(05)00049-2. [DOI] [PubMed] [Google Scholar]
- e56.Green HJ, Pakenham KI, Headley BC, et al. Altered cognitive function in men treated for prostate cancer with luteinizing hormone-releasing hormone analogues and cyproterone acetate: a randomized controlled trial. BJU Int. 2002;90:427–432. doi: 10.1046/j.1464-410x.2002.02917.x. [DOI] [PubMed] [Google Scholar]
- e57.Janowsky JS. Thinking with your gonads: testosterone and cognition. Trends Cogn Sci. 2006;10:77–82. doi: 10.1016/j.tics.2005.12.010. [DOI] [PubMed] [Google Scholar]
- e58.Nieschlag E, Swerdloff R, Behre HM, et al. Investigation, treatment and monitoring of late-onset hypogonadism in males. ISA, ISSAM, and EAU recommendations. Eur Urol. 2005;48:1–4. doi: 10.1016/j.eururo.2005.04.027. [DOI] [PubMed] [Google Scholar]
- e59.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526–534. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- e60.Osterweil D, Syndulko K, Cohen SN, et al. Cognitive function in non-demented older adults with hypothyroidism. J Am Geriatr Soc. 1992;40:325–335. doi: 10.1111/j.1532-5415.1992.tb02130.x. [DOI] [PubMed] [Google Scholar]
- e61.Volpato S, Guralnik JM, Fried LP, et al. Serum thyroxine level and cognitive decline in euthyroid older women. Neurology. 2002;58:1055–1061. doi: 10.1212/wnl.58.7.1055. [DOI] [PubMed] [Google Scholar]
- e62.Gussekloo J, van Exel E, de Craen AJ, et al. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004;292:2591–2599. doi: 10.1001/jama.292.21.2591. [DOI] [PubMed] [Google Scholar]
- e63.Roberts LM, Pattison H, Roalfe A, et al. Is subclinical thyroid dysfunction in the elderly associated with depression or cognitive dysfunction? Ann Intern Med. 2006;145:573–581. doi: 10.7326/0003-4819-145-8-200610170-00006. [DOI] [PubMed] [Google Scholar]
- e64.Park YJ, Lee EJ, Lee YJ, et al. Subclinical hypothyroidism (SCH) is not associated with metabolic derangement, cognitive impairment, depression or poor quality of life (QoL) in elderly subjects. Arch Gerontol Geriatr. 2010;50:e68–e73. doi: 10.1016/j.archger.2009.05.015. [DOI] [PubMed] [Google Scholar]
- e65.Aghini-Lombardi F, Antonangeli L, Martino E, et al. The spectrum of thyroid disorders in an iodine-deficient community: the Pescopagano survey. J Clin Endocrinol Metab. 1999;84:561–566. doi: 10.1210/jcem.84.2.5508. [DOI] [PubMed] [Google Scholar]
- e66.Kalmijn S, Mehta KM, Pols HA, et al. Subclinical hyperthyroidism and the risk of dementia. The Rotterdam study. Clin Endocrinol (Oxf) 2000;53:733–737. doi: 10.1046/j.1365-2265.2000.01146.x. [DOI] [PubMed] [Google Scholar]
- e67.Ceresini G, Lauretani F, Maggio M, et al. Thyroid function abnormalities and cognitive impairment in elderly people: results of the Invecchiare in Chianti study. J Am Geriatr Soc. 2009;57:89–93. doi: 10.1111/j.1532-5415.2008.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e68.Goodman Y, Bruce AJ, Cheng B, Mattson MP. Estrogens attenuate and corticosterone exacerbates excitotoxicity, oxidative injury, and amyloid beta-peptide toxicity in hippocampal neurons. J Neurochem. 1996;66:1836–1844. doi: 10.1046/j.1471-4159.1996.66051836.x. [DOI] [PubMed] [Google Scholar]
- e69.McEwen BS, Alves SE, Bulloch K, Weiland NG. Clinically relevant basic science studies of gender differences and sex hormone effects. Psychopharmacol Bull. 1998;34:251–259. [PubMed] [Google Scholar]
- e70.Shumaker SA, Legault C, Kuller L, et al. Conjugated equine estrogens and incidence of probable dementia and mild cognitive impairment in postmenopausal women: Women’s Health Initiative Memory Study. JAMA. 2004;291:2947–2958. doi: 10.1001/jama.291.24.2947. [DOI] [PubMed] [Google Scholar]
- e71.Shumaker SA, Legault C, Rapp SR, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women’s Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003;289:2651–2662. doi: 10.1001/jama.289.20.2651. [DOI] [PubMed] [Google Scholar]
- e72.Henderson VW. Estrogens, episodic memory, and Alzheimer’s disease: a critical update. Semin Reprod Med. 2009;27:283–293. doi: 10.1055/s-0029-1216281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e73.Tierney MC, Oh P, Moineddin R, et al. A randomized double-blind trial of the effects of hormone therapy on delayed verbal recall in older women. Psychoneuroendocrinology. 2009;34:1065–1074. doi: 10.1016/j.psyneuen.2009.02.009. [DOI] [PubMed] [Google Scholar]
- e74.Maki PM, Sundermann E. Hormone therapy and cognitive function. Hum Reprod Update. 2009;15:667–681. doi: 10.1093/humupd/dmp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e75.Solfrizzi V, Capurso C, D’Introno A, et al. Lifestyle-related factors in predementia and dementia syndromes. Expert Rev Neurother. 2008;8:133–158. doi: 10.1586/14737175.8.1.133. [DOI] [PubMed] [Google Scholar]
- e76.Feart C, Samieri C, Barberger-Gateau P. Mediterranean diet and cognitive function in older adults. Curr Opin Clin Nutr Metab Care. 2010;13:14–18. doi: 10.1097/MCO.0b013e3283331fe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e77.Yaffe K, Barnes D, Nevitt M, Lui LY, Covinsky K. A prospective study of physical activity and cognitive decline in elderly women: women who walk. Arch Intern Med. 2001;161:1703–1708. doi: 10.1001/archinte.161.14.1703. [DOI] [PubMed] [Google Scholar]
- e78.Laurin D, Verreault R, Lindsay J, MacPherson K, Rockwood K. Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch Neurol. 2001;58:498–504. doi: 10.1001/archneur.58.3.498. [DOI] [PubMed] [Google Scholar]
- e79.Etgen T, Sander D, Huntgeburth U, et al. Physical activity and incident cognitive impairment in elderly persons: the INVADE study. Arch Intern Med. 2010;170:186–193. doi: 10.1001/archinternmed.2009.498. [DOI] [PubMed] [Google Scholar]
- e80.Pignatti F, Rozzini R, Trabucchi M. Physical activity and cognitive decline in elderly persons. Arch Intern Med. 2002;162:361–362. doi: 10.1001/archinte.162.3.361. [DOI] [PubMed] [Google Scholar]
- e81.Lytle ME, Vander Bilt J, Pandav RS, Dodge HH, Ganguli M. Exercise level and cognitive decline: the MoVIES project. Alzheimer Dis Assoc Disord. 2004;18:57–64. doi: 10.1097/01.wad.0000126614.87955.79. [DOI] [PubMed] [Google Scholar]
- e82.Singh-Manoux A, Hillsdon M, Brunner E, Marmot M. Effects of physical activity on cognitive functioning in middle age: evidence from the Whitehall II prospective cohort study. Am J Public Health. 2005;95:2252–2258. doi: 10.2105/AJPH.2004.055574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e83.Middleton L, Kirkland S, Rockwood K. Prevention of CIND by physical activity: different impact on VCI-ND compared with MCI. J Neurol Sci. 2008;269:80–84. doi: 10.1016/j.jns.2007.04.054. [DOI] [PubMed] [Google Scholar]
- e84.Niti M, Yap KB, Kua EH, Tan CH, Ng TP. Physical, social and productive leisure activities, cognitive decline and interaction with APOE-epsilon 4 genotype in Chinese older adults. Int Psychogeriatr. 2008;20:237–251. doi: 10.1017/S1041610207006655. [DOI] [PubMed] [Google Scholar]
- e85.Förstl H, Haass C, Hemmer B, Meyer B, Halle M. Boxing: Acute complications and late sequelae, from concussion to dementia. Dtsch Arztebl Int. 2010;107(47):835–839. doi: 10.3238/arztebl.2010.0835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e86.Picciotto MR, Zoli M. Nicotinic receptors in aging and dementia. J Neurobiol. 2002;53:641–655. doi: 10.1002/neu.10102. [DOI] [PubMed] [Google Scholar]
- e87.Anstey KJ, von Sanden C, Salim A, O’Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol. 2007;166:367–378. doi: 10.1093/aje/kwm116. [DOI] [PubMed] [Google Scholar]
- e88.Etgen T, Sander D, Bickel H, Sander K, Förstl H. Cognitive Decline: The Relevance of Diabetes, Hyperlipidemia and Hypertension Brit J Diab Vascul Dis 2010; 10: 115-22 [Google Scholar]
- e89.Forette F, Seux ML, Staessen JA, et al. The prevention of dementia with antihypertensive treatment: new evidence from the Systolic Hypertension in Europe (Syst-Eur) study. Arch Intern Med. 2002;162:2046–2052. doi: 10.1001/archinte.162.18.2046. [DOI] [PubMed] [Google Scholar]
- e90.Etgen T, Brönner M, Sander D, et al. Somatische Faktoren bei leichten kognitiven Störungen. Fortschr Neurol Psychiatr. 2009;77:72–82. doi: 10.1055/s-0028-1109116. [DOI] [PubMed] [Google Scholar]
- e91.Jack CR, Jr, Knopman DS, Jagust WJ, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–128. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]