Abstract
Objective
To compare the effect of admission cardiotocography and Doppler auscultation of the fetal heart on neonatal outcome and levels of obstetric intervention in a low risk obstetric population.
Design
Randomised controlled trial.
Setting
Obstetric unit of teaching hospital
Participants
Pregnant women who had no obstetric complications that warranted continuous monitoring of fetal heart rate in labour.
Intervention
Women were randomised to receive either cardiotocography or Doppler auscultation of the fetal heart when they were admitted in spontaneous uncomplicated labour.
Main outcome measures
The primary outcome measure was umbilical arterial metabolic acidosis. Secondary outcome measures included other measures of condition at birth and obstetric intervention.
Results
There were no significant differences in the incidence of metabolic acidosis or any other measure of neonatal outcome among women who remained at low risk when they were admitted in labour. However, compared with women who received Doppler auscultation, women who had admission cardiotocography were significantly more likely to have continuous fetal heart rate monitoring in labour (odds ratio 1.49, 95% confidence interval 1.26 to 1.76), augmentation of labour (1.26, 1.02 to 1.56), epidural analgesia (1.33, 1.10 to 1.61), and operative delivery (1.36, 1.12 to 1.65).
Conclusions
Compared with Doppler auscultation of the fetal heart, admission cardiotocography does not benefit neonatal outcome in low risk women. Its use results in increased obstetric intervention, including operative delivery.
What is already known on this topic
The admission cardiotocogram is a short recording of the fetal heart rate immediately after admission to the labour ward
Opinion varies about its value in identifying a potentially compromised fetus
In low risk women, the incidence of intrapartum fetal compromise is low
What this study adds
Compared with Doppler auscultation of the fetal heart, admission cardiotocography has no benefit on neonatal outcome in low risk women
Admission cardiotocography results in increased obstetric intervention, including operative delivery
Introduction
The admission cardiotocogram is a short, usually 20 minute, recording of the fetal heart rate immediately after admission to the labour ward.1 The main justification for admission cardiotocography is that the uterine contractions of labour put stress on the placental circulation; an abnormal tracing might indicate a deficiency and hence identify potential fetal compromise at an early enough stage to allow intervention. Furthermore, a normal admission cardiotocogram offers reassurance. However, the incidence of intrapartum fetal compromise is low in pregnancies that have been uncomplicated before the onset of labour. Thus, labour admission cardiotocography may represent unnecessary intervention. In such low risk cases, confirmation of a normal fetal heart rate by Doppler auscultation should be sufficient.2
Evidence from randomised trials shows that routine electronic fetal monitoring throughout labour results in increased, and probably unnecessary, intervention for apparent fetal distress.3–5 Admission cardiotocography in a low risk obstetric population may therefore result in increased obstetric intervention without fetal and neonatal benefit. We compared the effects of labour admission cardiotocography and Doppler auscultation of the fetal heart on neonatal outcome and levels of obstetric intervention in a low risk obstetric population.
Participants and methods
Women were eligible to join the study if they were booked for hospital delivery, attended a hospital or community based consultant led clinic in the third trimester of pregnancy, and had no obstetric complications at that visit that would warrant continuous intrapartum monitoring of fetal heart rate (pre-eclampsia or hypertension in previous or index pregnancy; essential hypertension; diabetes (insulin dependent or gestational); suspected intrauterine growth restriction; placental abruption or praevia or vaginal bleeding of unknown origin; multiple pregnancy; fetal malformation; previous caesarean section; breech presentation; or rhesus isoimmunisation).
Randomisation procedure and study protocol
A researcher obtained informed consent for the study at the third trimester visit. Women were randomised to the cardiotocography or Doppler group with a commercially available computer randomisation program.6 The allocation was placed in a sealed envelope and attached to the labour admission page of the woman's case records. The women did not know which group they had been randomised to until their admission in labour. An independent observer checked the randomisation process weekly. The data analysts were blind to the randomisation code.
When women who were recruited to the study were admitted in spontaneous uncomplicated labour, the admitting midwife opened the trial envelope. Women randomised to the cardiotocography group had 20 minutes of cardiotocography before being given any opiate analgesia. Women randomised to the Doppler group had fetal heart auscultation with a hand held Doppler device during and immediately after at least one contraction. Staff on the labour ward interpreted the fetal heart assessments and took action on the basis of protocols.
Some women developed complications after randomisation that warranted continuous intrapartum monitoring of the fetal heart rate. These women had their admission assessment and labour managed according to the obstetric complication.
At delivery, we obtained umbilical cord blood samples to measure pH and base deficit. When possible both arterial and venous samples were taken. Arterial blood results were included in the analysis only if both an arterial and venous sample had been obtained and the results suggested no errors due to a poor quality sample.
Outcome measures
The primary outcome measure was metabolic acidosis at delivery, defined as an umbilical cord pH<7.20 with a base deficit of >8.0 mmol/l. Secondary outcome measures were other assessments of neonatal outcome (Apgar scores, need for intermittent positive pressure ventilation at resuscitation, admission to neonatal intensive care) and obstetric intervention (use of continuous fetal heart rate monitoring in labour, artificial rupture of membranes, augmentation of labour, monitoring of scalp pH, epidural analgesia, operative delivery).
Sample size and analysis
A final target sample size of 1704 confirmed low risk women was based on an excess of umbilical cord blood metabolic acidosis of 4% in the Doppler group. This gave an α of 0.05 with 80% power. This effect size was chosen as a clinically important difference. In a pilot study in which all women had admission cardiotocography, the incidence of metabolic acidosis was 7%.
During the study the sample size and power calculation were reviewed by the project group and modified. Our original grant application was awarded on the basis of recruiting 3370 low risk women and based on an arbitrary 3% excess of metabolic acidosis in the Doppler group, which we considered clinically important and defined the target power of 90%. As the study progressed, it became clear that recruitment was lower than expected for various justifiable but unalterable reasons and that more women were developing complications that required continuous monitoring than had been predicted. These problems were highlighted in the interim report to the funding body, and we were given a supplementary award to extend the recruitment period. In this application, we stated that the power would be reduced to 80% as this was the conventional level. At that time we believed that we would be able achieve the reduced sample size of 2552.
Just after receiving the supplementary award, we audited the interobserver and intraobserver error in abstracting data from clinical notes. This showed that data on arterial blood gas concentrations were not available in all women, which would create a further shortfall in the number of women available for analysis of the primary outcome variable. Thirteen months before recruitment was due to end the steering group met with two research midwives to discuss the recruitment and viability of the study. At this stage we calculated that at the end of recruitment the number of low risk women on admission in labour with data on arterial blood gas concentrations would be about 1800, a shortfall of 752.
We discussed whether to ask for further funding, review the power calculations, or abandon the study. We dismissed asking for further funding as unrealistic and then reviewed the power calculation. We were not prepared to drop the target power of study below 80%. However, we discussed at length the relevance of the clinical effect size of 3%. Our predicted sample size was sufficient to detect a 4% difference, and our clinical decision at the time was, and remains, that a 4% difference was as relevant as a 3% difference. We therefore agreed to set the effect size at 4% with an 80% power.
Apart from the small audit, no analysis was done until the study was complete and all data had been entered and double checked. All analysis was done blind to the randomisation group.
The whole group analysis was by intention to treat at the time of randomisation. We also did a subgroup analysis on women who were still low risk when they were admitted in labour.
Results
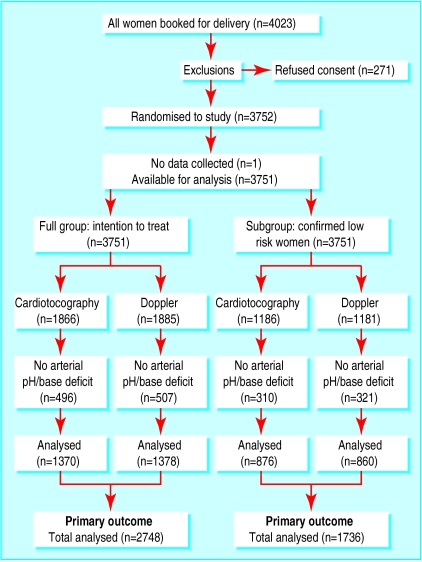
In all, 4023 women met the entry requirements; 271 (7%) did not wish to participate, which left 3752 to be randomised in the third trimester (figure).
Whole group analysis
Comparison between the two groups showed no significant differences in the incidence of metabolic acidosis at delivery. Women in the cardiotocography group were significantly more likely than women in the Doppler group to have continuous monitoring of fetal heart rate during labour, have epidural analgesia, and require an operative delivery. There were no other significant differences (table 1).
Table 1.
Neonatal and obstetric outcomes in whole group analysis after cardiotocography or Doppler auscultation at admission
| Outcome | No in cardiotocography group | No in Doppler group | Odds ratio (95% CI) |
|---|---|---|---|
| Cord arterial blood metabolic acidosis | 252/1370 | 262/1378 | 0.96 (0.79 to 1.17) |
| Apgar score <7 at 5 min | 36/1858 | 34/1868 | 1.07 (0.65 to 1.75) |
| Need for IPPV at resuscitation | 11/1865 | 14/1878 | 0.79 (0.33 to 1.85) |
| Admission to neonatal intensive care | 89/1864 | 105/1878 | 0.85 (0.63 to 1.14) |
| Hypoxic ischaemic encephalopathy | 8/81 | 15/99 | 0.61 (0.22 to 1.65) |
| Continuous fetal heart rate monitoring in labour | 1246/1865 | 1128/1882 | 1.35 (1.17 to 1.54) |
| Artificial rupture of membranes | 1065/1864 | 1031/1879 | 1.10 (0.96 to 1.25) |
| Augmentation of labour | 714/1862 | 692/1878 | 1.07 (0.93 to 1.22) |
| Monitoring of fetal scalp pH | 197/1866 | 177/1885 | 1.14 (0.91 to 1.42) |
| Epidural analgesia in labour | 617/1866 | 565/1885 | 1.15 (1.00 to 1.33) |
| Operative delivery* | 602/1866 | 551/1885 | 1.15 (1.00 to 1.32) |
| Caesarean section | 193/1866 | 165/1885 | 1.20 (0.96 to 1.50) |
IPPV=intermittent positive pressure ventilation.
Caesarean section, forceps, or ventouse.
Subgroup analysis
Between randomisation during the third trimester of pregnancy and admission in labour, 1384 women (37%) developed an obstetric complication that warranted continuous fetal heart rate monitoring in labour (table 2). We did a subgroup analysis after these women were excluded.
Table 2.
Reasons for exclusion after randomisation (some women had more than one reason for exclusion)
| Complication | No (%) of cases |
|---|---|
| Antepartum haemorrhage | 159 (4.2) |
| Raised blood pressure | 271 (7.2) |
| Suspected small for dates | 56 (1.5) |
| Preterm labour | 48 (1.3) |
| Gestational diabetes | 2 (0.1) |
| Fetal anomaly | 2 (0.1) |
| Reduced fetal movements and suspected fetal compromise | 63 (1.7) |
| Meconium stained liquor | 99 (2.6) |
| Intrauterine death | 3 (0.1) |
| Persistent breech | 67 (1.8) |
| Membranes ruptured before labour | 164 (4.4) |
| Induction of labour | 833 (22.2) |
| Baby born before arrival at hospital | 19 (0.5) |
| Elective caesarean section | 61 (1.6) |
| Woman withdrew from trial | 31 (0.8) |
| Other | 44 (1.2) |
| Total | 1384 (36.9) |
Comparison between groups showed no significant differences in the incidence of metabolic acidosis at delivery. Women who had admission cardiotocography were significantly more likely than women in the Doppler group to have continuous fetal heart rate monitoring in labour, augmentation of labour, epidural analgesia, and require an operative delivery. There were no other significant differences (table 3).
Table 3.
Comparison of neonatal and obstetric outcomes in women who remained low risk at labour
| Outcome | No in cardiotocography group | No in Doppler group | Odds ratio (95% CI) |
|---|---|---|---|
| Cord arterial blood metabolic acidosis | 159/876 | 154/860 | 1.02 (0.79 to 1.31) |
| Apgar score <7 at 5 minutes | 25/1181 | 18/1171 | 1.39 (0.72 to 2.66) |
| Need for IPPV at resuscitation | 5/1185 | 4/1178 | 1.24 (0.29 to 5.51) |
| Admission to neonatal intensive care | 46/1185 | 45/1175 | 1.01 (0.65 to 1.57) |
| Hypoxic ischaemic encephalopathy | 6/42 | 5/43 | 1.27 (0.31 to 5.34) |
| Continuous fetal heart rate monitoring in labour | 672/1186 | 551/1178 | 1.49 (1.26 to 1.76) |
| Artificial rupture of membranes | 640/1185 | 614/1175 | 1.07 (0.91 to 1.27) |
| Augmentation of labour | 246/1183 | 202/1175 | 1.26 (1.02 to 1.56) |
| Use of fetal scalp pH | 96/1186 | 76/1181 | 1.28 (0.93 to 1.77) |
| Epidural analgesia in labour | 325/1186 | 261/1181 | 1.33 (1.10 to 1.61) |
| Operative delivery* | 313/1186 | 247/1181 | 1.36 (1.12 to 1.65) |
| Caesarean section | 61/1186 | 43/1181 | 1.43 (0.95 to 2.18) |
IPPV=intermittent positive pressure ventilation.
Caesarean section, forceps, or ventouse.
In this group of confirmed low risk women, 21.5% (255/1186) randomised to have admission cardiotocography were considered to have an abnormal fetal heart trace at the onset of labour compared with 3.6% (42/1181) of women in the Doppler group (P<0.0001). In the cardiotocography group the commonest abnormalities were decelerations (147, 58%) and reduced variability (111, 43%) of cases. In the Doppler group, the commonest abnormalities were a bradycardia and decelerations (both 18 (43%) cases).
Discussion
In our clinical environment, admission cardiotocography had no neonatal benefit, as assessed by metabolic acidosis at delivery, but resulted in increased obstetric intervention. We obtained the same result whether the analysis was for the whole group or just women who remained at low risk when admitted in labour. As the aim of the study was to investigate the effect of admission cardiotocography or Doppler auscultation on the incidence of metabolic acidosis in low risk pregnancies, we felt justified in performing a subgroup analysis in which we excluded women who developed complications between randomisation and the onset of labour. It would have been preferable to obtain women's consent before labour and then wait until they were admitted in labour before randomising them. We could not to do this because of ethical and logistical constraints.
Effect on fetus
Previous descriptive studies have suggested that admission cardiotocography may help identify a compromised fetus when the uterine contractions of early labour act as a functional stress on the placental circulation.1,7,8 These uncontrolled studies, however, do not allow conclusions to be drawn about the clinical usefulness or indeed clinical risks of admission cardiotocography. The assumed benefits are not confirmed by our trial.
We found no neonatal benefit from women having admission cardiotocography, as assessed by the presence of metabolic acidosis at delivery. There were no significant differences in the secondary neonatal outcome measures between the two methods of fetal heart rate assessment. However, our sample size is insufficient to provide definitive information about these outcomes. Many of the confidence intervals were wide and included unity.
Interpreting cardiotocograms
We found much higher levels of concern about the fetal heart rate after admission cardiotocography than after Doppler auscultation. There is wide intraobserver and interobserver variation in the interpretation of cardiotocograms even among experts.9–13 Fetal heart variability is difficult to interpret visually, and there is a tendency to over report abnormalities.12,14–17 We found a high percentage of admission cardiotocograms were reported as abnormal, with reduced variability and variable decelerations the most commonly reported abnormalities. This high rate of abnormal admission traces is in keeping with findings in other studies.18 Variability in fetal heart rate cannot be assessed in the Doppler group.
Our study was a pragmatic trial in which the midwives and junior obstetric staff interpreted the admission fetal heart assessments. Our findings suggest that when an admission cardiotocogram shows possible reduced baseline variability or mild decelerations, midwives and obstetricians will take defensive action. This starts with continuous monitoring of fetal heart rate, which leads to increased obstetric intervention in the form of augmentation of labour, epidural analgesia, and, ultimately, increased rates of operative delivery. Other randomised trials have also found that routine electronic fetal monitoring in labour results in increased unnecessary intervention for fetal distress.3–5
Maternal outcomes
Perhaps the most important finding is the increased rate of operative delivery in women who had admission cardiotocography. Among women who were low risk at admission, there was an absolute increase of 5.5% in operative delivery and 1.5% increase in caesarean sections. The rising caesarean section rate in the United Kingdom continues to generate much debate and concern.19–23 The increased use of continuous monitoring of fetal heart rate in labour in women who had admission cardiotocography in this study is likely to be a contributing factor.
This study has confirmed that among women with low risk features at the onset of labour, the admission cardiotocogram is no better than Doppler auscultation of the fetal heart in identifying a potentially compromised fetus. Admission cardiotocography was associated with increased obstetric intervention including higher rates of operative delivery. Although caution is needed in generalising conclusions to the whole population, our results point to potential problems with admission cardiotocography. These problems are likely to persist while difficulties remain in interpreting cardiotocograms.
Figure.
Flow chart of trial
Acknowledgments
We thank the research midwives Maureen McLeod and Suzanneke Lucas for recruiting women and collecting data.
Editorial by Goddard
Footnotes
Funding: Chief Scientists Office of the Scottish Executive, Edinburgh.
Competing interests: None declared
References
- 1.Ingemarsson I. Electronic fetal monitoring as a screening test. In: Spencer JAD, Ward RHT, editors. Intrapartum fetal surveillance. London: Royal College of Obstetricians and Gynaecologists; 1993. pp. 45–52. [Google Scholar]
- 2.Prentice A, Lind T. Fetal heart rate monitoring in labour—too frequent intervention, too little benefit? Lancet. 1997;ii:1375–1377. doi: 10.1016/s0140-6736(87)91266-9. [DOI] [PubMed] [Google Scholar]
- 3.Grant AM. Electronic fetal monitoring alone versus intermittent auscultation in labour. In: Enkin MW, Kierse MJNC, Renfrew MJ, Neilson JP, editors. Cochrane pregnancy and childbirth database. Oxford: Update Software; 1993. [Google Scholar]
- 4.Thacker SB, Stroup DF, Peterson HB. Efficacy and safety of intrapartum electronic fetal monitoring: an update. Obstet Gynecol. 1995;86:613–620. [PubMed] [Google Scholar]
- 5.Thacker SB, Stroup DF. Continuous electronic heart rate monitoring for fetal assessment during labor Cochrane Database Syst Rev 2000;(2):CD000063. [DOI] [PubMed]
- 6.Florey C du V. Randomiser. Dundee: University of Dundee; 1995. [Google Scholar]
- 7.Pello LC, Dawes GS, Smith J, Redman CW. Screening of the fetal heart in early labour. Br J Obstet Gynecol. 1988;95:1128–1136. doi: 10.1111/j.1471-0528.1988.tb06790.x. [DOI] [PubMed] [Google Scholar]
- 8.Phelan JP. Labor admission test. Clin Perinatol. 1994;21:879–885. [PubMed] [Google Scholar]
- 9.Hefland M, Marton K, Ueland K. Factors involved in the interpretation of fetal monitor tracings. Am J Obstet Gynecol. 1981;151:737–742. doi: 10.1016/0002-9378(85)90507-1. [DOI] [PubMed] [Google Scholar]
- 10.Beaulieu MD, Fabia J, Leduc B, Brisson J, Bastide A, Bloudin D, et al. The reproducibility of intrapartum cardiotocogram assessments. Can Med J. 1982;127:214–216. [PMC free article] [PubMed] [Google Scholar]
- 11.Nielson PV, Stigsby B, Nickelsoen C, Nim J. Intra and inter observer variability in the assessments of intrapartum cardiotocograms. Acta Obstet Gynecol Scand. 1987;66:421–424. doi: 10.3109/00016348709022046. [DOI] [PubMed] [Google Scholar]
- 12.Borgotta L, Shrout PE, Divon MY. Reliability and reproducibility of non stress test readings. Am J Obstet Gynecol. 1988;159:554–558. doi: 10.1016/s0002-9378(88)80006-1. [DOI] [PubMed] [Google Scholar]
- 13.Lidegaard O, Bottcher LM, Weber T. Description, evaluation and clinical decision making according to various fetal heart rate patterns- interobserver and regional variability. Acta Obstet Gynecol Scand. 1992;71:48–53. doi: 10.3109/00016349209007947. [DOI] [PubMed] [Google Scholar]
- 14.Flynn AM, Kelly J, Matthews R. Predictive value of, and observer variability in, several ways of reporting antenatal cardiotocograms. Br J Obstet Gynecol. 1982;89:434–440. doi: 10.1111/j.1471-0528.1982.tb03632.x. [DOI] [PubMed] [Google Scholar]
- 15.Lotgering FK, Wallenberg HCS, Schouten HJA. Interobserver and intraobserver variation in the assessment of antenatal cardiotocograms. Am J Obstet Gynecol. 1982;144:701–705. doi: 10.1016/0002-9378(82)90440-9. [DOI] [PubMed] [Google Scholar]
- 16.Trimbos JB, Keirse MJNC. Observer variability in the assessment of antenatal cardiotocograms. Br J Obstet Gynecol. 1978;85:900–906. doi: 10.1111/j.1471-0528.1978.tb15851.x. [DOI] [PubMed] [Google Scholar]
- 17.Dawes GS, Lobb M, Moulden M, Redman CWG, Wheeler T. Antenatal cardiotocograms and interpretation using computers. Br J Obstet Gynecol. 1992;99:791–797. doi: 10.1111/j.1471-0528.1992.tb14408.x. [DOI] [PubMed] [Google Scholar]
- 18.Sarno AP, Phelan JP, Ahn MO. Relationship of early intrapartum fetal heart rate patterns to subsequent patterns and fetal outcome. J Reprod Med. 1990;35:239–242. [PubMed] [Google Scholar]
- 19.McIlwaine GM, Cole SK, Macnaughton MC. The rising caesarean section rate—a matter of concern. Health Bull. 1985;43:301–305. [PubMed] [Google Scholar]
- 20.Macfarlane A, Chamberlain G. What is happening to caesarean section rates? Lancet. 1993;342:1005–1006. doi: 10.1016/0140-6736(93)92874-s. [DOI] [PubMed] [Google Scholar]
- 21.Chamberlain G. What is the correct caesarean section rate? Br J Obstet Gynecol. 1993;100:403–404. doi: 10.1111/j.1471-0528.1993.tb15260.x. [DOI] [PubMed] [Google Scholar]
- 22.Treffers PE, Pel M. The rising trend in caesarean birth. BMJ. 1993;307:1017–1018. doi: 10.1136/bmj.307.6911.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilkinson C, McIlwaine G, Boulton-Jones C, Cole S. Is the rising caesarean section rate inevitable? Br J Obstet Gynecol. 1998;105:45–52. doi: 10.1111/j.1471-0528.1998.tb09349.x. [DOI] [PubMed] [Google Scholar]